a91858d274472e5ad9edee3963f43593.ppt
- Количество слайдов: 34


TREAT -a Decision Support System for Antibiotic Treatment Supported by an EU 5 th Framework grant Coordinator: Steen Andreassen On behalf of the Treat group: Rabin Medical Centre, Israel Freiburg University Hospital, Germany Universitá Cattolica S. Cuore, Italy Judex Datasystems A/S, Denmark Aalborg University, Denmark
The magnitude of the problem n The mortality associated with severe bacterial infections is ~30%. n A third of patients are prescribed inappropriate empirical antibiotics, and ~20% superfluous drugs (J Intern Med 1998, 244: 379; Chest 2000, 118: 146 ; Scand J Infect Dis 1997, 29: 601; Am J Med Sci 1978, 275: 271). n Inappropriate empirical Rx is associated with an increase in fatality rate: Multi-variable adjusted OR: 1. 6 to 6. 9 (J Intern Med 1998; 244: 379 ); (Chest 2000; 118: 146).
The magnitude of the problem n Maximum empirical antibiotic treatment is not a viable solution. n Antibiotics account for about 20% of drug expenditures: 7 million NIS for Beilinson per year.
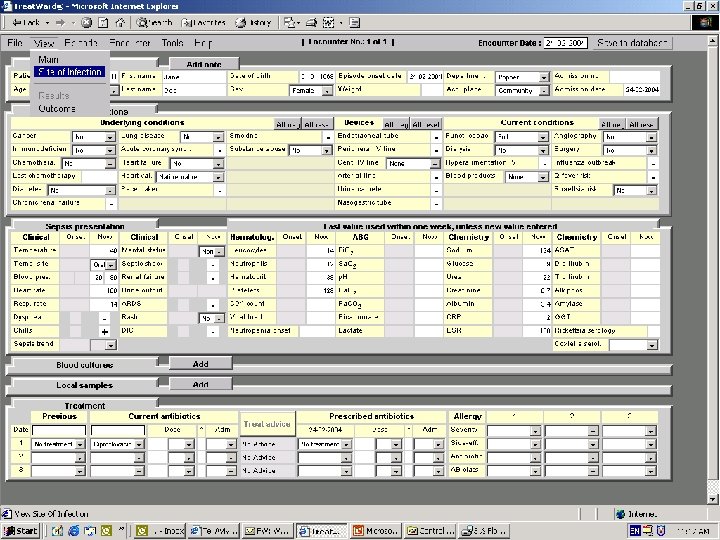
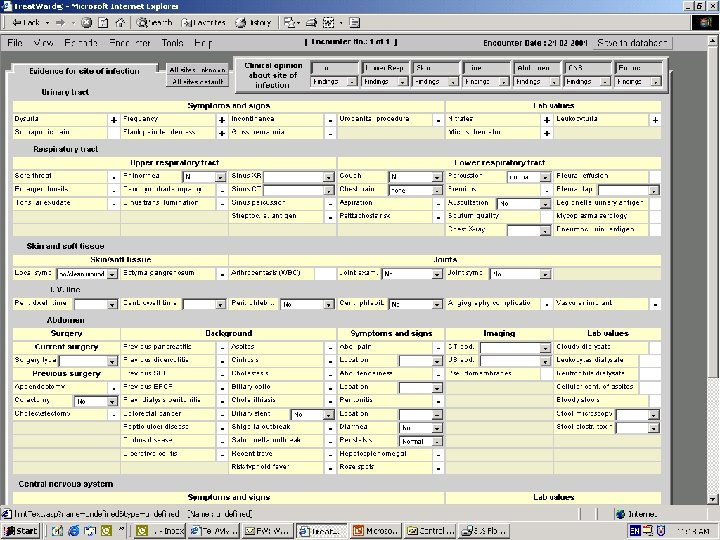
The system n n n Causal probabilistic network for the diagnosis and treatment of infections Treatment based on cost-benefit model Benefit: – Improved survival with appropriate antibiotic treatment – Reduced beddays n Costs: – Direct – Side-effects – Ecological costs
Advantages of a causal probabilistic network (CPN): n n n Natural multiplication of the needed matrices (infection probability X pathogen probability X susceptibilities). Explicit modelling of universal and local factors. The only way to deal with missing data. The only way to combine between knowledge and data from different sources in one system. Cost effectiveness (or benefit) analysis is a natural feature of the system.
A model of infections A (very) simplified version of the TREAT CPN will be used: 1. to demonstrate the concepts of • infection • sepsis • prognosis (sepsis*) • treatment • coverage and • mortality
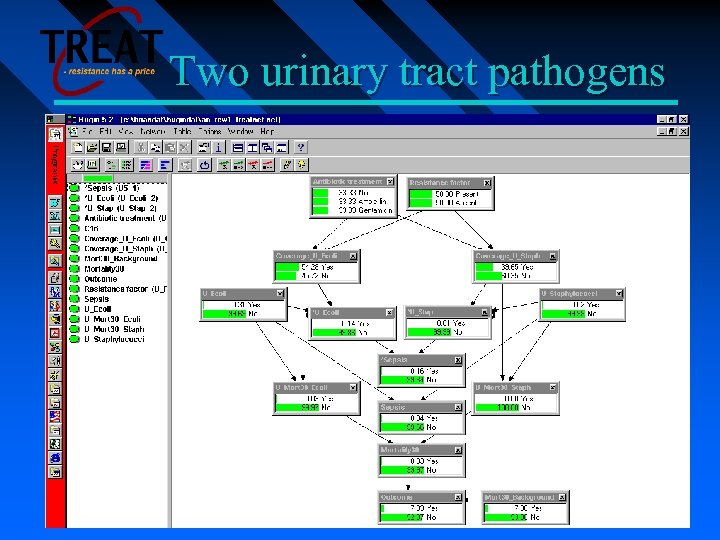
Two urinary tract pathogens

Sepsis = Yes, Treatment = No, Res. Factor = Present (Hosp. Acq. )
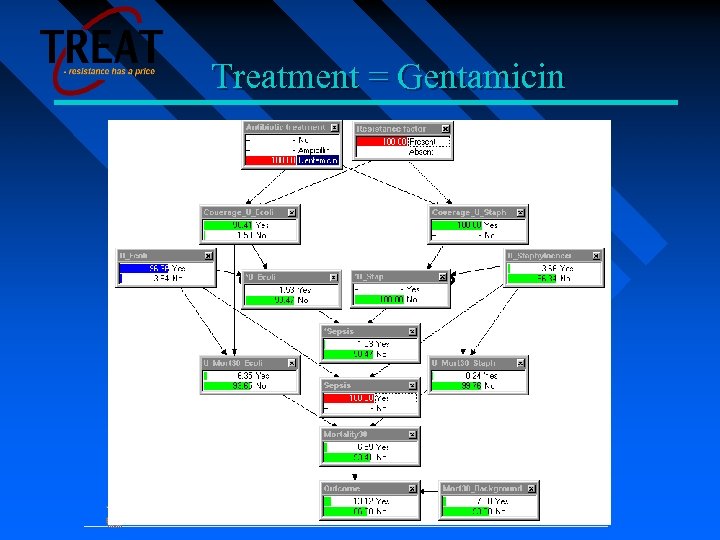
Treatment = Gentamicin
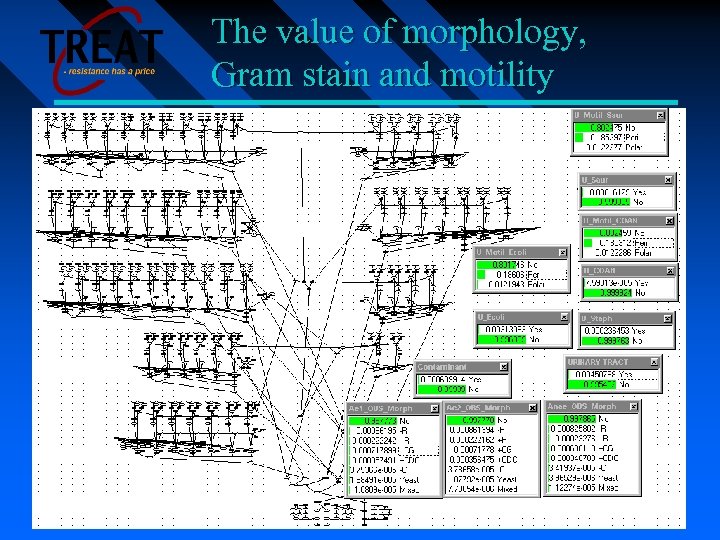
The value of morphology, Gram stain and motility
Databases for local calibrations To adapt the TREAT system to a given hospital, databases are needed for: • Antibiotics and their costs • Resistance of pathogns to antibiotics (hospital vs. community acquired) • Pathogen prevalences
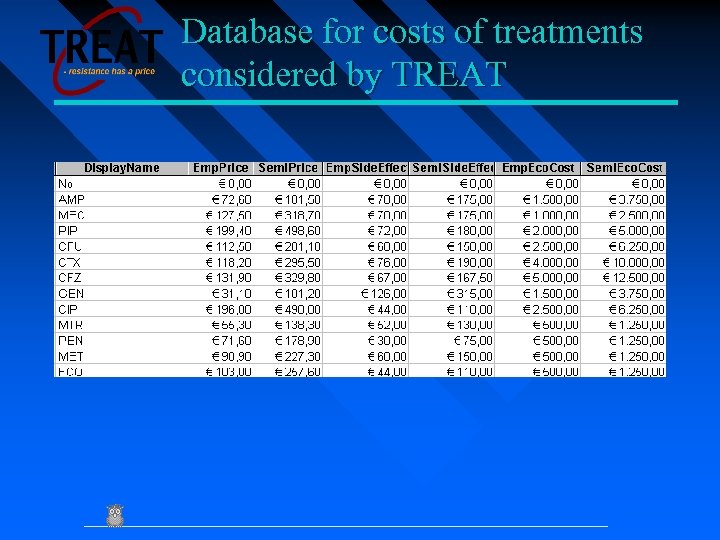
Database for costs of treatments considered by TREAT
Eligible patients 1. 2. 3. 4. 5. 6. All patients for whom antibiotic treatment (but not prophylaxis) is started (whether with a community or hospital acquired disorder). Patients from whom blood cultures are drawn. Patients in whom two or more of the following are present: a. Temperature >38°C or <36°C b. Heart rate >90 beats/min c. Respiratory rate >20 breaths/min or Pa. CO 2 <32 mm. Hg d. WBC >12, 000 cells/mm 3, <4000 cells/mm 3, or >10 percent immature (band) forms Patients with a focus of infection, mainly: a new infiltrate on chest x -ray, urinary complaints and leukocyturia, skin findings compatible with skin or soft tissue infections, etc. Patients with shock compatible with septic shock. Febrile neutropenic patients (single oral temperature ≥ 38. 3 or a temperature of 38 lasting ≥ 1 hour).
Exclusion criteria: n n n n Organ and bone-marrow transplant patients Children<16 years HIV+ Suspected travel infections patients Suspected tuberculosis with sepsis included Pregnancy HIV positive patients with a current suspected or identified opportunistic disease and/or AIDS defining illness currently or within the past 6 months Re-entries
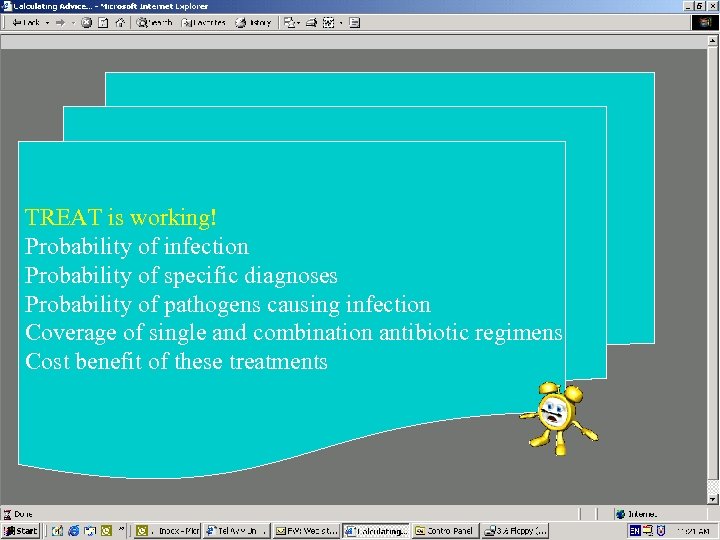
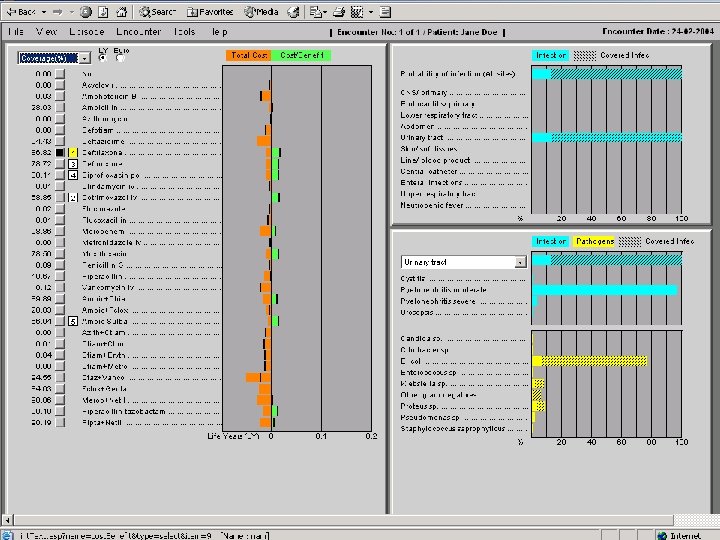
TREAT is working! Probability of infection Probability of specific diagnoses Probability of pathogens causing infection Coverage of single and combination antibiotic regimens Cost benefit of these treatments

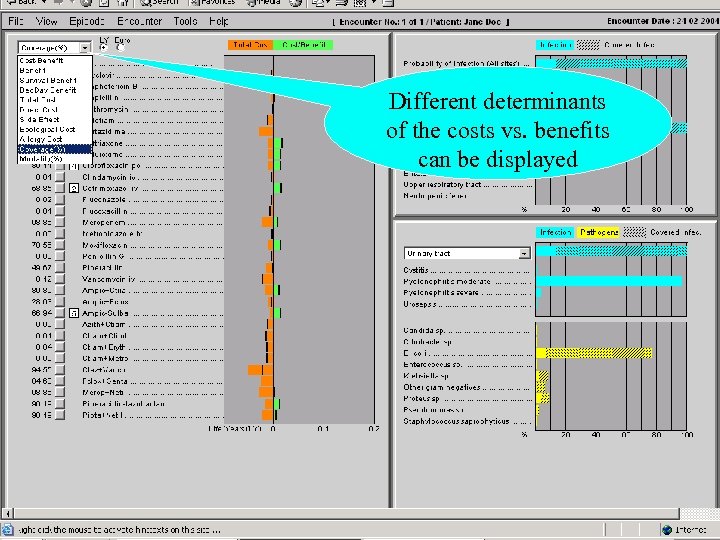
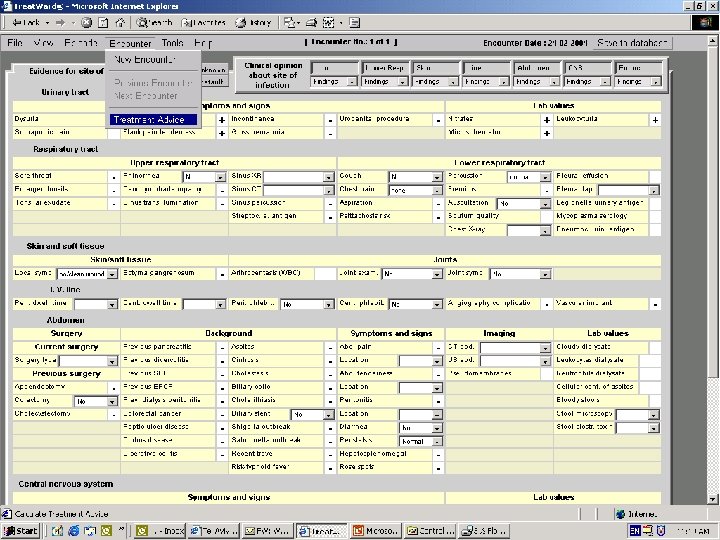
Different determinants of the costs vs. benefits can be displayed
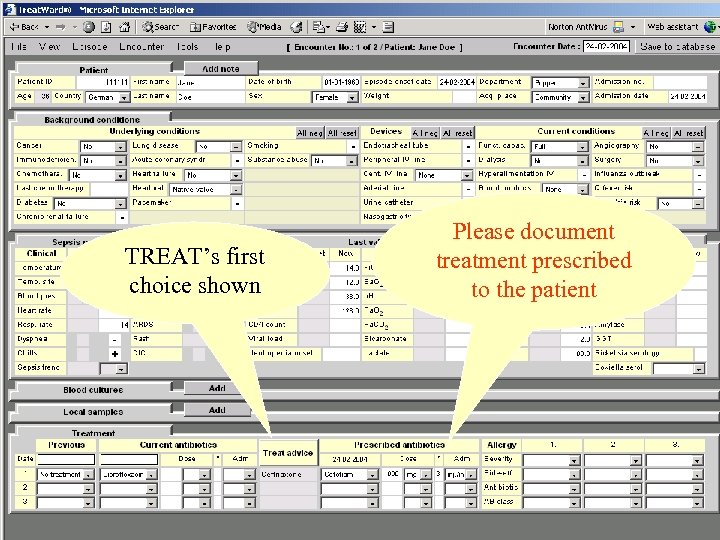
TREAT’s first choice shown Please document treatment prescribed to the patient
TREAT Observational trial 6 -12/2002
Methods and objectives n n n All patients fulfilling inclusion criteria were entered into an observational database Entry, bacteriological, and 30 -day outcome data collected prospectively Each case presented to TREAT advice compared to physician performance Primary outcome: antibiotic treatment matching in -vitro susceptibility of clinically relevant isolates (‘appropriate treatment’)
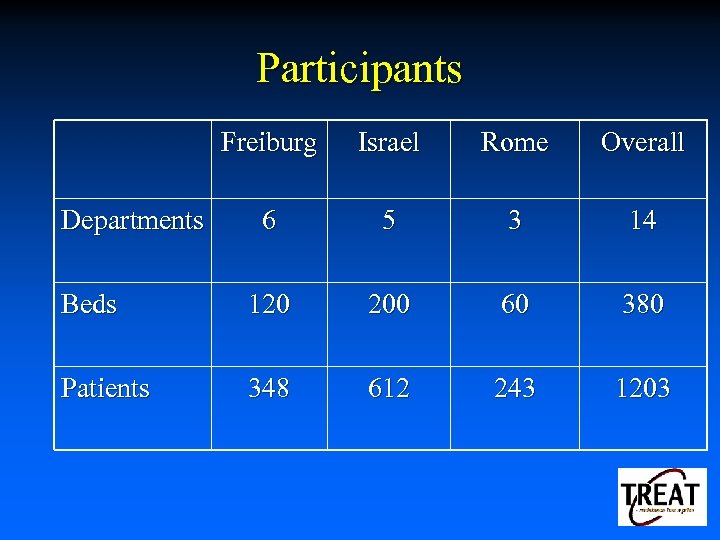
Participants Freiburg Israel Rome Overall 6 5 3 14 Beds 120 200 60 380 Patients 348 612 243 1203 Departments
Primary outcome n n Appropriate antibiotic treatment was prescribed to 58% of patients. TREAT’s advice was appropriate in 70% of cases (p=0. 0001) Increment in the rate of coverage: relative increase of 21% and an absolute increase of 12% The improvement reached statistical significance in Rabin, Freiburg, and overall.
Secondary outcomes TREAT used a lower number of antibiotic regimens than the physician n TREAT preferred narrow spectrum antibiotics to broad spectrum ones. n Overall cost, the overall cost at each site and the costs related by the model to future resistance were significantly reduced by TREAT n
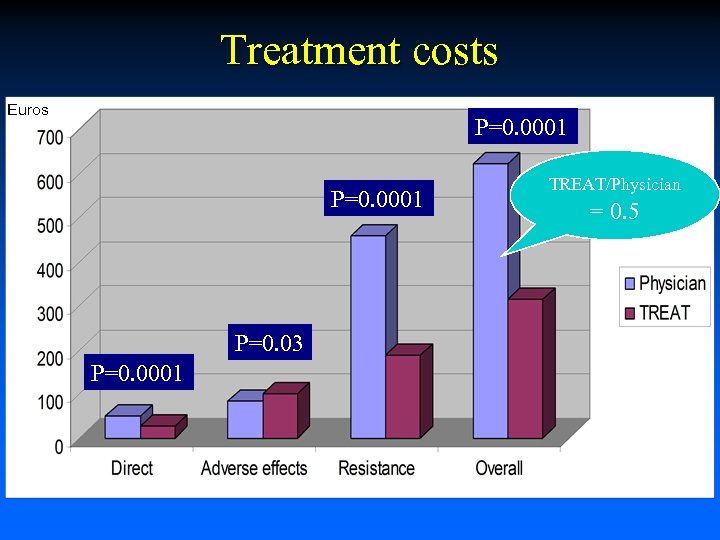
Treatment costs Euros P=0. 0001 P=0. 03 P=0. 0001 TREAT/Physician = 0. 5
Conclusions – observational trial TREAT has the potential of improving significantly on the percentage of appropriate empirical antibiotic treatment while at the same time reducing all components of costs, but mainly the costs assigned by the model to future resistance.
TREAT Intervention
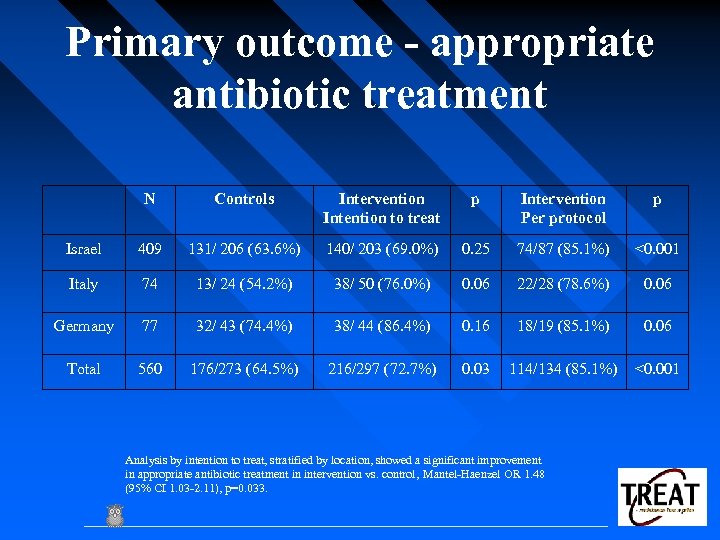
Primary outcome - appropriate antibiotic treatment N Controls Intervention Intention to treat p Intervention Per protocol p Israel 409 131/ 206 (63. 6%) 140/ 203 (69. 0%) 0. 25 74/87 (85. 1%) <0. 001 Italy 74 13/ 24 (54. 2%) 38/ 50 (76. 0%) 0. 06 22/28 (78. 6%) 0. 06 Germany 77 32/ 43 (74. 4%) 38/ 44 (86. 4%) 0. 16 18/19 (85. 1%) 0. 06 Total 560 176/273 (64. 5%) 216/297 (72. 7%) 0. 03 114/134 (85. 1%) <0. 001 Analysis by intention to treat, stratified by location, showed a significant improvement in appropriate antibiotic treatment in intervention vs. control, Mantel-Haenzel OR 1. 48 (95% CI 1. 03 -2. 11), p=0. 033.
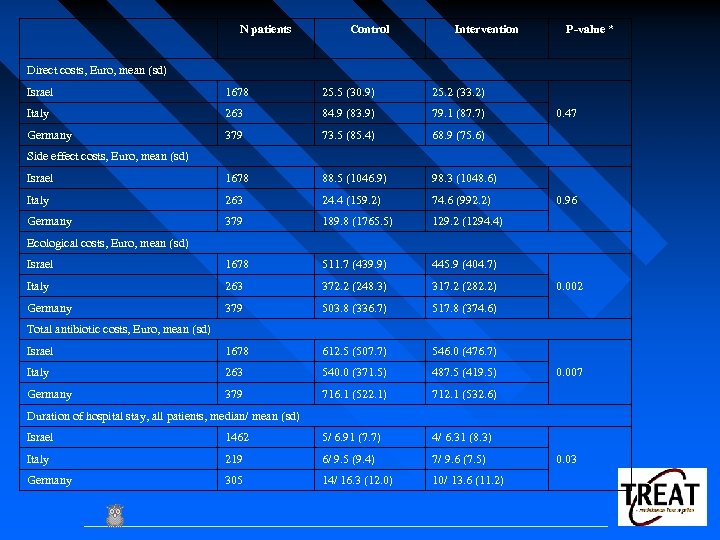
N patients Control Intervention P-value * Direct costs, Euro, mean (sd) Israel 1678 25. 5 (30. 9) 25. 2 (33. 2) Italy 263 84. 9 (83. 9) 79. 1 (87. 7) Germany 379 73. 5 (85. 4) 68. 9 (75. 6) Israel 1678 88. 5 (1046. 9) 98. 3 (1048. 6) Italy 263 24. 4 (159. 2) 74. 6 (992. 2) Germany 379 189. 8 (1765. 5) 129. 2 (1294. 4) Israel 1678 511. 7 (439. 9) 445. 9 (404. 7) Italy 263 372. 2 (248. 3) 317. 2 (282. 2) Germany 379 503. 8 (336. 7) 517. 8 (374. 6) Israel 1678 612. 5 (507. 7) 546. 0 (476. 7) Italy 263 540. 0 (371. 5) 487. 5 (419. 5) Germany 379 716. 1 (522. 1) 712. 1 (532. 6) 0. 47 Side effect costs, Euro, mean (sd) 0. 96 Ecological costs, Euro, mean (sd) 0. 002 Total antibiotic costs, Euro, mean (sd) 0. 007 Duration of hospital stay, all patients, median/ mean (sd) Israel 1462 5/ 6. 91 (7. 7) 4/ 6. 31 (8. 3) Italy 219 6/ 9. 5 (9. 4) 7/ 9. 6 (7. 5) Germany 305 14/ 16. 3 (12. 0) 10/ 13. 6 (11. 2) 0. 03
Thank you
a91858d274472e5ad9edee3963f43593.ppt