d84efddd72d16067209f88d42c061bb8.ppt
- Количество слайдов: 50
Traumatic Brain Injury and Evidence Based Medicine üTBI - What are the problems? üTBI management strategies üTBI treatment in Austria üIntroduction into EBM üHow to use EBM for continuous quality improvement in the care of TBI patients

TBI: Treatment Goals üTO KEEP THE PERMANENT NEURO DEFICIT AT THE LEVEL DEFINED BY THE PRIMARY INJURY üTO AVOID üTO RECOGNIZE IMMEDIATELY üTO TREAT WITHOUT DELAY SECONDARY BRAIN INSULTS
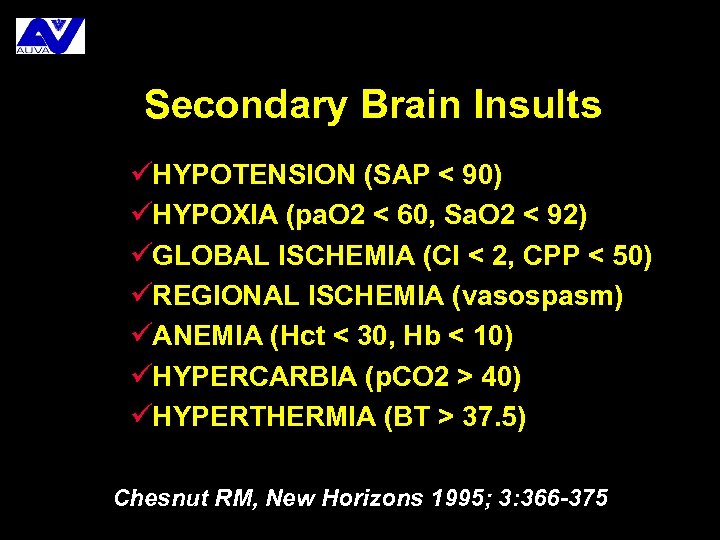
Secondary Brain Insults üHYPOTENSION (SAP < 90) üHYPOXIA (pa. O 2 < 60, Sa. O 2 < 92) üGLOBAL ISCHEMIA (CI < 2, CPP < 50) üREGIONAL ISCHEMIA (vasospasm) üANEMIA (Hct < 30, Hb < 10) üHYPERCARBIA (p. CO 2 > 40) üHYPERTHERMIA (BT > 37. 5) Chesnut RM, New Horizons 1995; 3: 366 -375
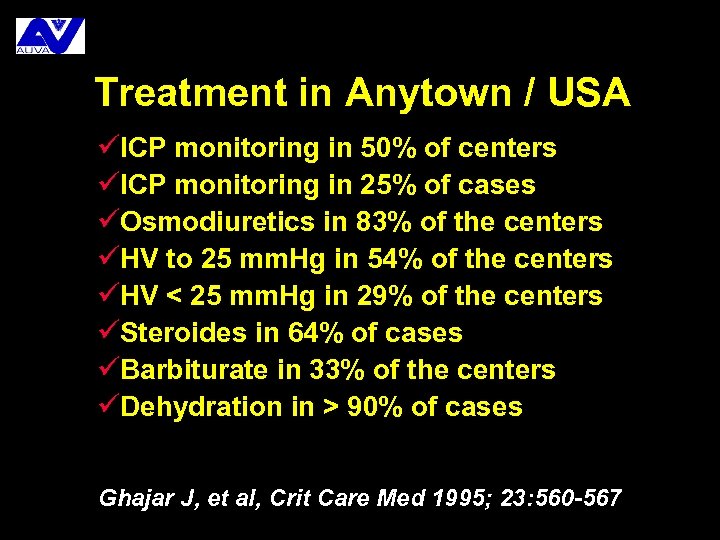
Treatment in Anytown / USA üICP monitoring in 50% of centers üICP monitoring in 25% of cases üOsmodiuretics in 83% of the centers üHV to 25 mm. Hg in 54% of the centers üHV < 25 mm. Hg in 29% of the centers üSteroides in 64% of cases üBarbiturate in 33% of the centers üDehydration in > 90% of cases Ghajar J, et al, Crit Care Med 1995; 23: 560 -567
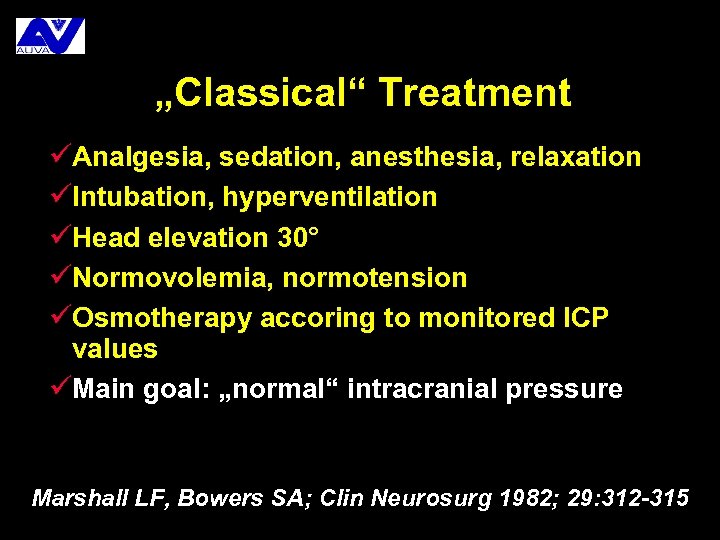
„Classical“ Treatment üAnalgesia, sedation, anesthesia, relaxation üIntubation, hyperventilation üHead elevation 30° üNormovolemia, normotension üOsmotherapy accoring to monitored ICP values üMain goal: „normal“ intracranial pressure Marshall LF, Bowers SA; Clin Neurosurg 1982; 29: 312 -315
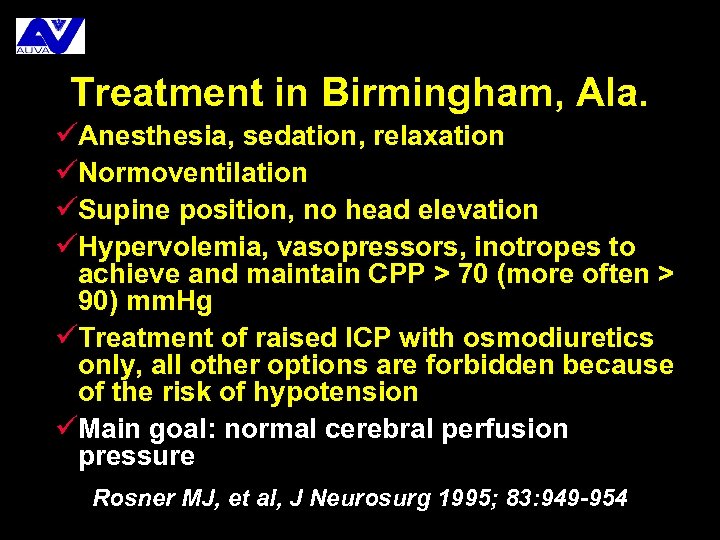
Treatment in Birmingham, Ala. üAnesthesia, sedation, relaxation üNormoventilation üSupine position, no head elevation üHypervolemia, vasopressors, inotropes to achieve and maintain CPP > 70 (more often > 90) mm. Hg üTreatment of raised ICP with osmodiuretics only, all other options are forbidden because of the risk of hypotension üMain goal: normal cerebral perfusion pressure Rosner MJ, et al, J Neurosurg 1995; 83: 949 -954
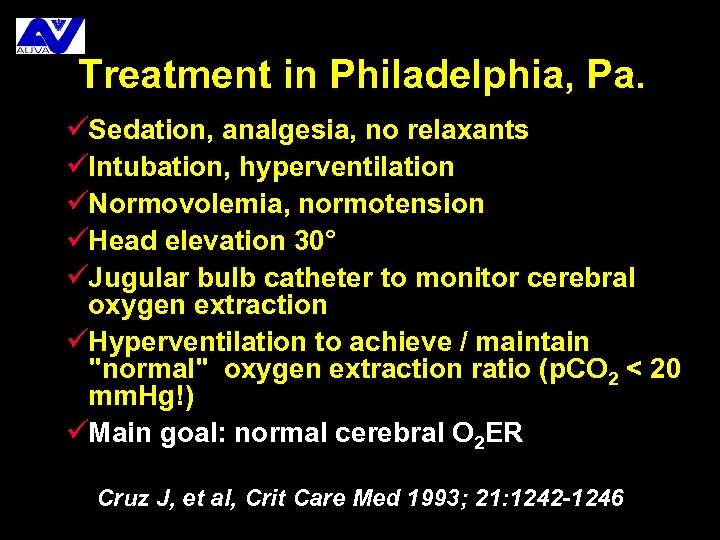
Treatment in Philadelphia, Pa. üSedation, analgesia, no relaxants üIntubation, hyperventilation üNormovolemia, normotension üHead elevation 30° üJugular bulb catheter to monitor cerebral oxygen extraction üHyperventilation to achieve / maintain "normal" oxygen extraction ratio (p. CO 2 < 20 mm. Hg!) üMain goal: normal cerebral O 2 ER Cruz J, et al, Crit Care Med 1993; 21: 1242 -1246
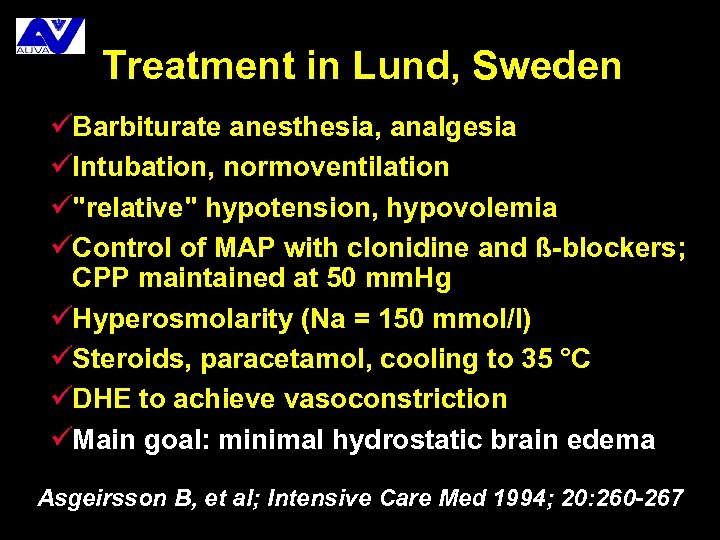
Treatment in Lund, Sweden üBarbiturate anesthesia, analgesia üIntubation, normoventilation ü"relative" hypotension, hypovolemia üControl of MAP with clonidine and ß-blockers; CPP maintained at 50 mm. Hg üHyperosmolarity (Na = 150 mmol/l) üSteroids, paracetamol, cooling to 35 °C üDHE to achieve vasoconstriction üMain goal: minimal hydrostatic brain edema Asgeirsson B, et al; Intensive Care Med 1994; 20: 260 -267
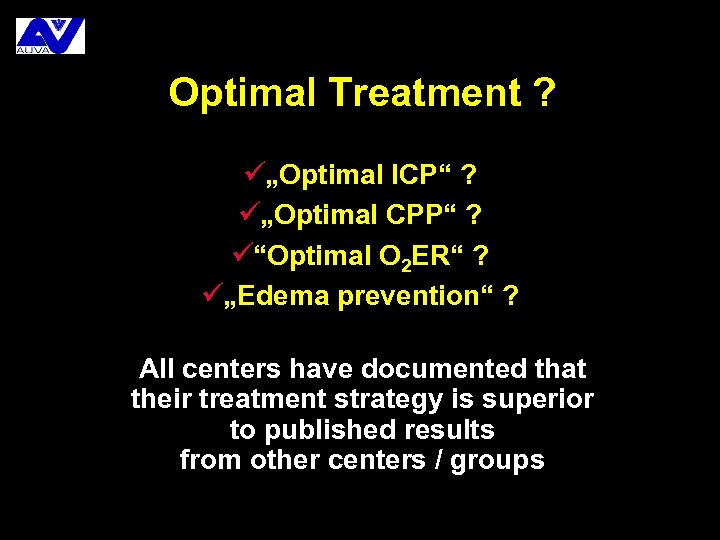
Optimal Treatment ? ü„Optimal ICP“ ? ü„Optimal CPP“ ? ü“Optimal O 2 ER“ ? ü„Edema prevention“ ? All centers have documented that their treatment strategy is superior to published results from other centers / groups

Treatment of severe traumatic brain injury in Austria (1998) H. Drobetz, B. Freudenschuß, E. Kutscha-Lissberg, W. Buchinger, W. Mauritz
Austrian ICUs surveyed (n = 60) üMostly run by anesthesiologists, all contacted by phone (for treatment data) üPhone calls (for patient statistics) to all Departments of üTrauma Surgery üNeurosurgery üSurgery
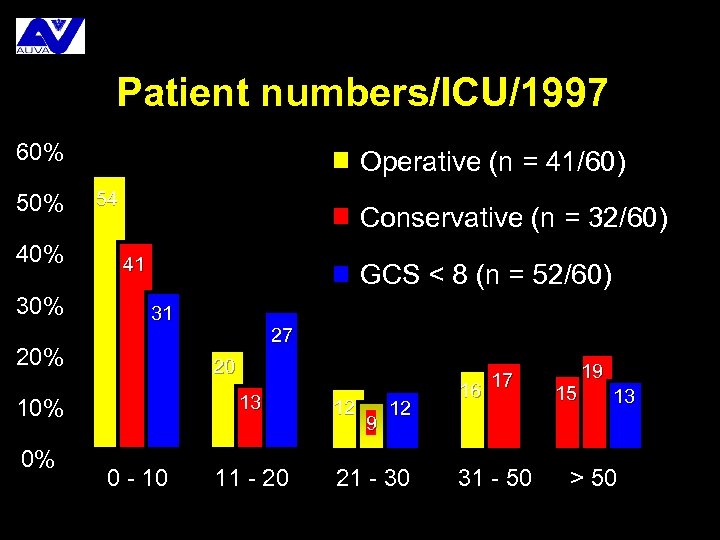
Patient numbers/ICU/1997 60% 50% 40% 30% Operative (n = 41/60) 54 Conservative (n = 32/60) 41 GCS < 8 (n = 52/60) 31 20% 20 13 10% 0% 27 0 - 10 11 - 20 12 9 12 21 - 30 17 16 31 - 50 15 19 13 > 50
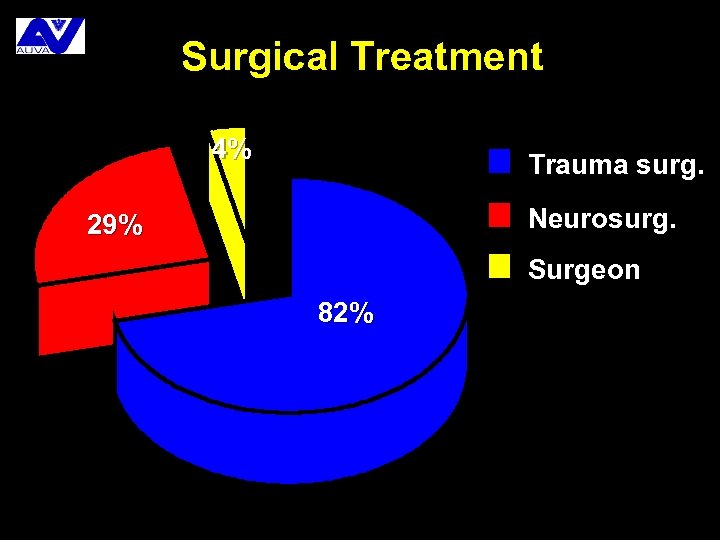
Surgical Treatment 4% Trauma surg. Neurosurg. 29% Surgeon 82%
Prehospital Treatment üGCS 90% (n = 51/60) üMAP, HR, Sa. O 2 100% (n = 44/60) üIntubation 74% (n = 47/60)
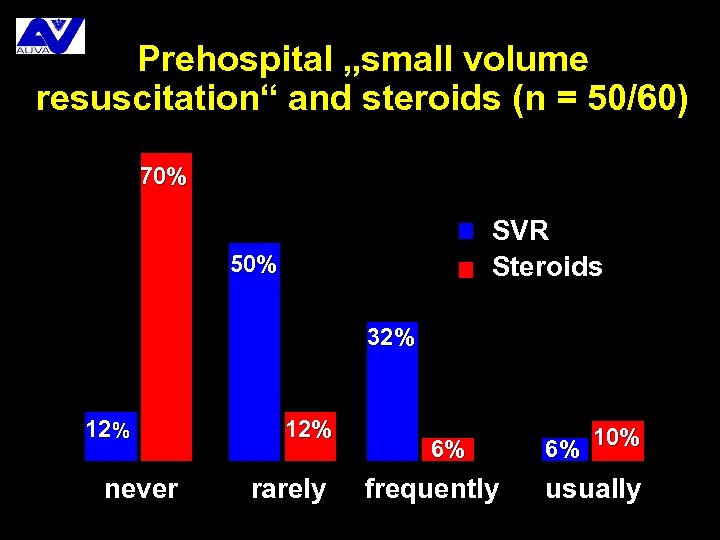
Prehospital „small volume resuscitation“ and steroids (n = 50/60) 70% SVR Steroids 50% 32% 12% never 12% rarely 6% frequently 10% 6% usually
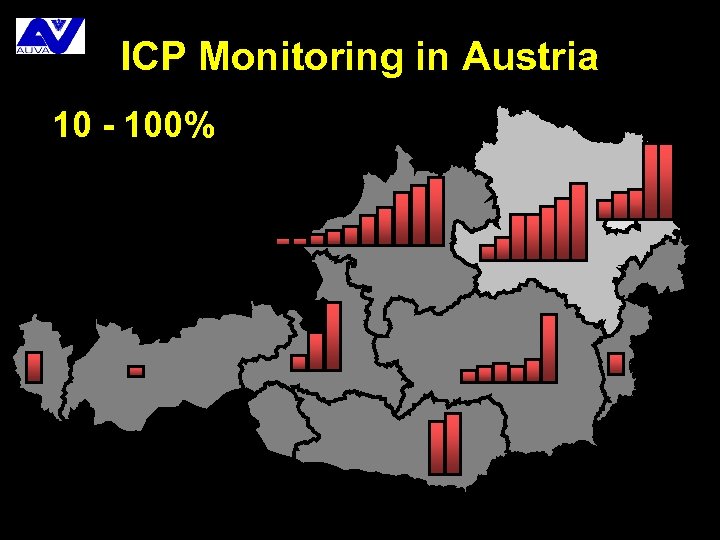
ICP Monitoring in Austria 10 - 100% 1
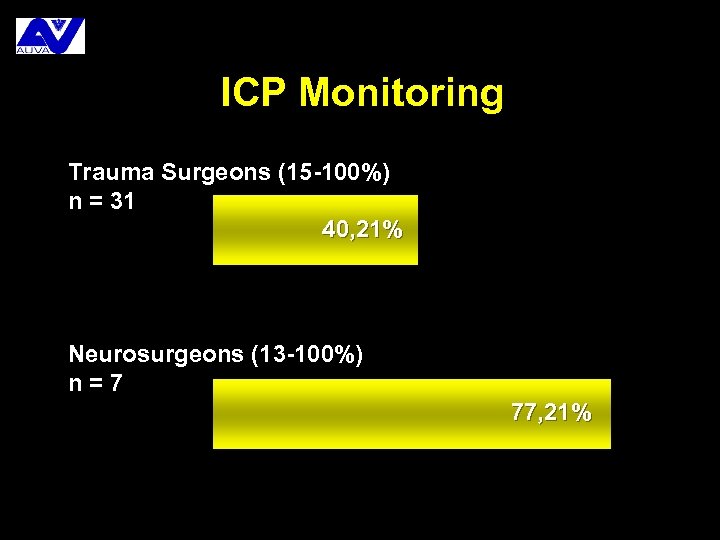
ICP Monitoring Trauma Surgeons (15 -100%) n = 31 40, 21% Neurosurgeons (13 -100%) n=7 77, 21%
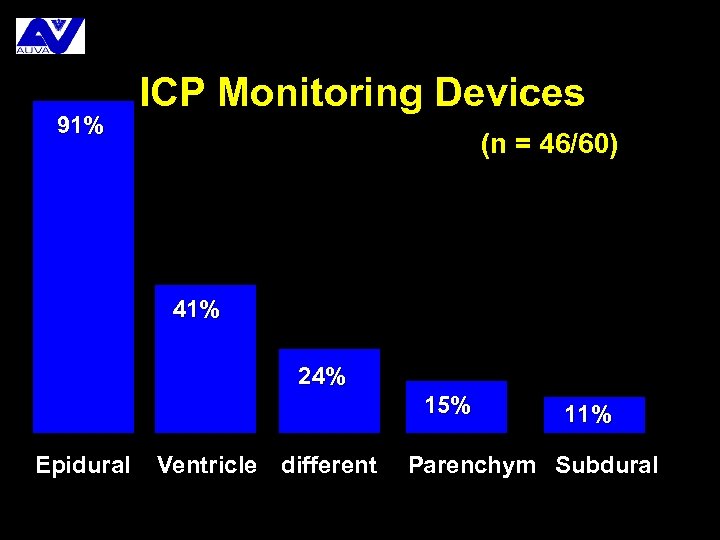
91% ICP Monitoring Devices (n = 46/60) 41% 24% 15% Epidural Ventricle different 11% Parenchym Subdural
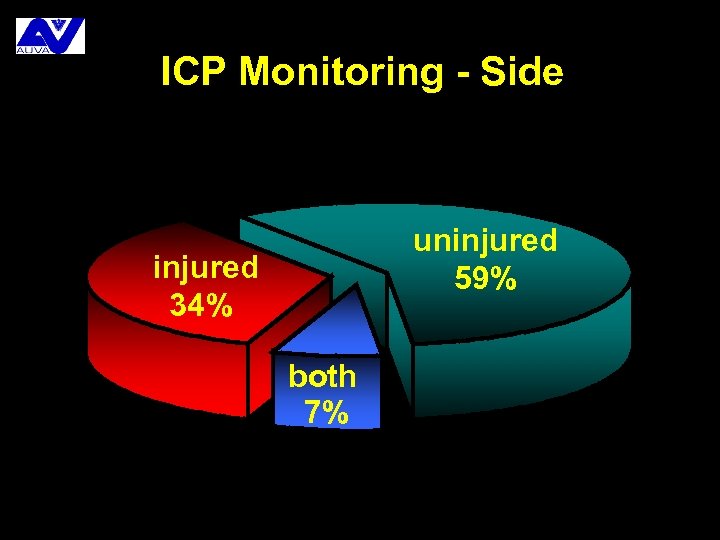
ICP Monitoring - Side uninjured 59% injured 34% both 7%
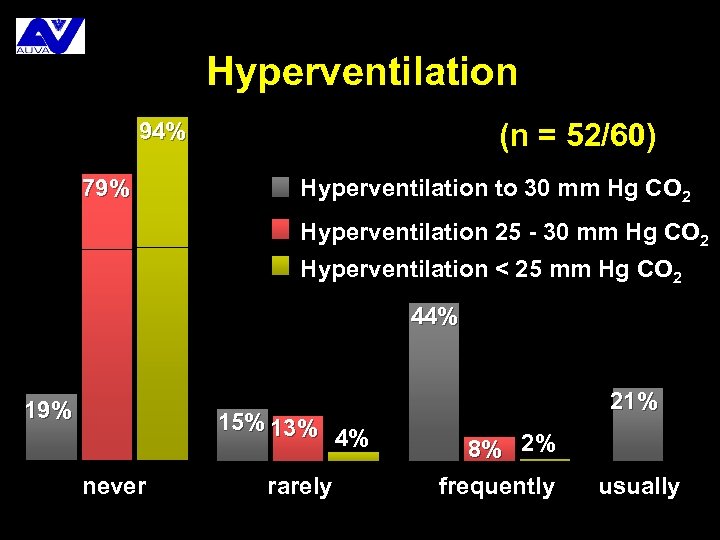
Hyperventilation (n = 52/60) 94% 79% Hyperventilation to 30 mm Hg CO 2 Hyperventilation 25 - 30 mm Hg CO 2 Hyperventilation < 25 mm Hg CO 2 44% 19% 15% 13% never rarely 21% 4% 8% 2% frequently usually
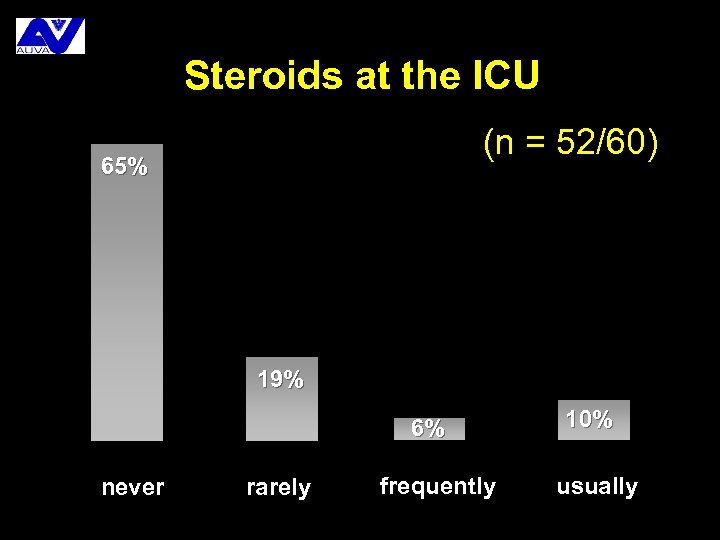
Steroids at the ICU (n = 52/60) 65% 19% 6% never rarely frequently 10% usually
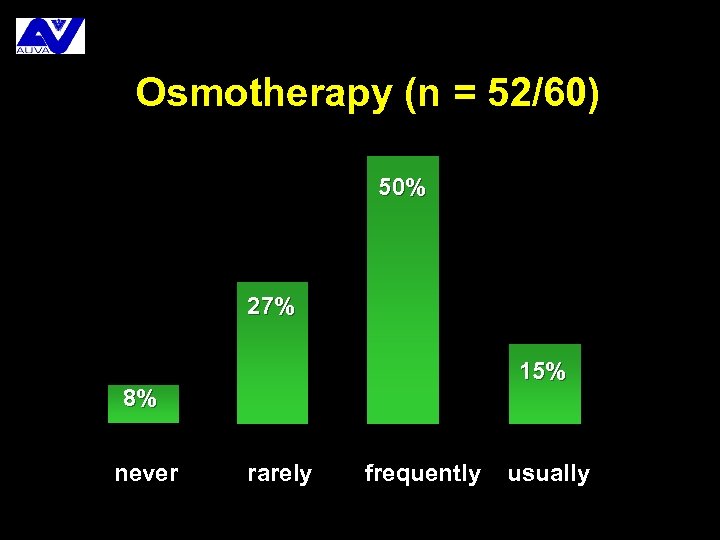
Osmotherapy (n = 52/60) 50% 27% 15% 8% never rarely frequently usually
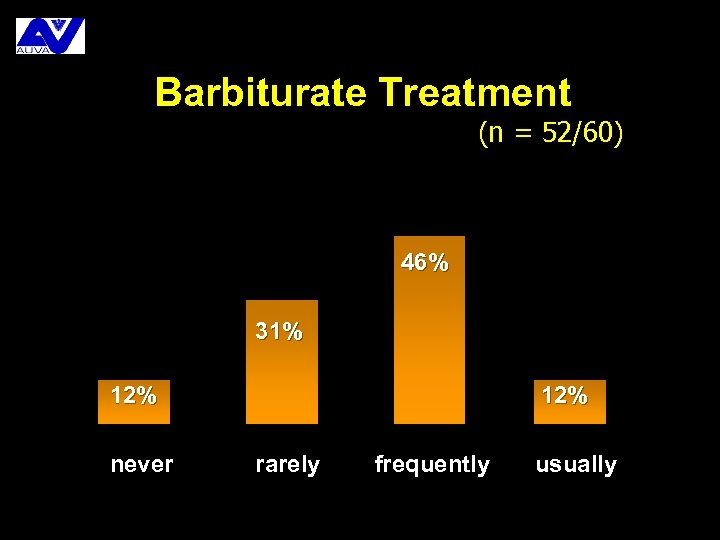
Barbiturate Treatment (n = 52/60) 46% 31% 12% never 12% rarely frequently usually
So what? üEvery center has its own standards üMost centers see only few patients üComparison of results between centers are rare Approach: üCreation of an (inter)national database to collect patient data from different centers üData can be used for quality assurance programs üIntroduction of guidelines and clinical pathways
Available Guidelines ü“Guidelines for the Management of Severe Head Injury” (1995), published in major journals, revised in 1997 üFormulated by the “Joint Section on Neurotrauma and Critical Care” of the AANS and CNS üReviewed & discussed in: üNew Horizons Vol. 3, #3, August 1995 üJ Trauma, Vol. 42, #5, Supplement May 1997
Other Guidelines üEuropean Brain Injury Consortium (EBIC) üScandinavian Guidelines üOther national guidelines Most guidelines were created using the same process (EBM)and the same published evidence, and therefore came to similar conclusions
Evidence Based Medicine üBasis for decisions in medicine ü„clinical experience“, EBM criteria üWhat is EBM? üPrinciple, methods, problems üWhy use EBM? üSafety (? ), quality, standardisation (? ) üHow to use EBM? üIndividual Search Strategies üStandards & Guidelines, Clinical Pathways
Clinical Experience (1) Is the (partially sub-cortically) available summary of üKnowledge of pathophysiology (basic knowledge) üMedical tradition (e. g. Dopamin) üTraining üAnalogies (treatment results in similar cases) which forms the basis for daily decisions.
Clinical Experience (2) üAdvantages: üIncreases with age üAvailable immediately and everywhere üUsually sufficient ü„flexible“ compared to EBM üDisadvantages: üHuge individual differences üErrors may have a long tradition, too üAcceptance of new findings may be slow üEffectivity of treatment overestimated
Evidence Based Medicine üDeveloped by Clinical Epidemiologists from Mc. Master Medical School, Canada, since 1985 üPositioned as alternative to traditional „opinion-based“ medicine ü„best available evidence“ should be the basis for treatment decisions: multi-center PRCT, meta-analysis, guidelines, clinical pathways
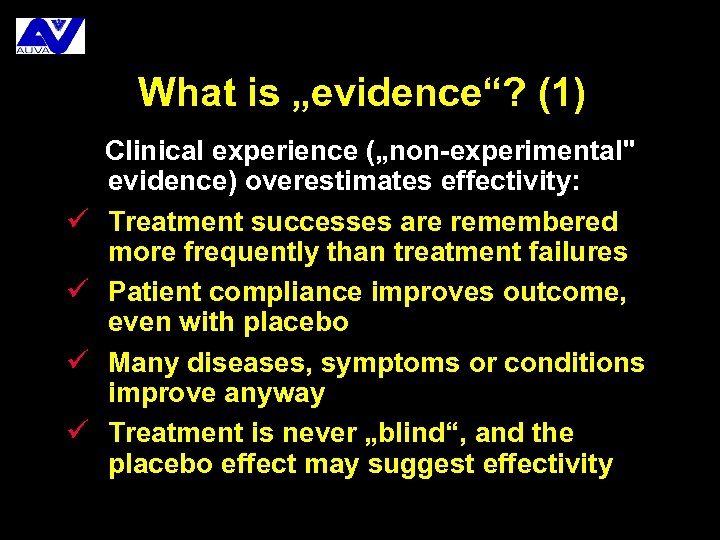
What is „evidence“? (1) ü ü Clinical experience („non-experimental" evidence) overestimates effectivity: Treatment successes are remembered more frequently than treatment failures Patient compliance improves outcome, even with placebo Many diseases, symptoms or conditions improve anyway Treatment is never „blind“, and the placebo effect may suggest effectivity
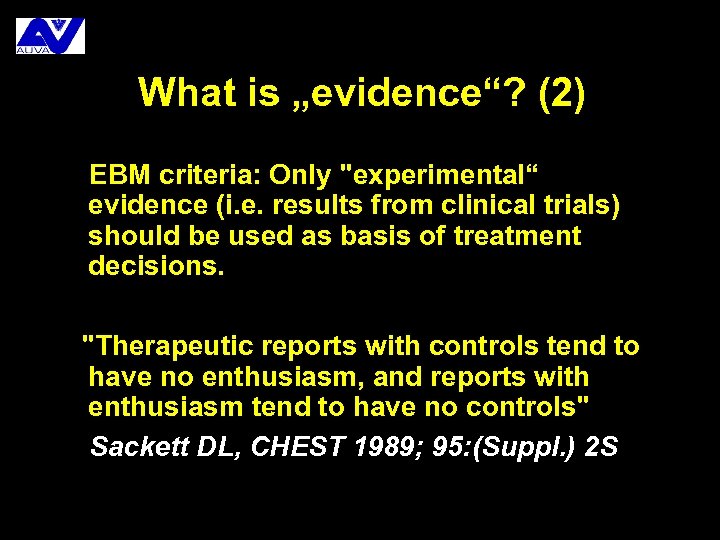
What is „evidence“? (2) EBM criteria: Only "experimental“ evidence (i. e. results from clinical trials) should be used as basis of treatment decisions. "Therapeutic reports with controls tend to have no enthusiasm, and reports with enthusiasm tend to have no controls" Sackett DL, CHEST 1989; 95: (Suppl. ) 2 S
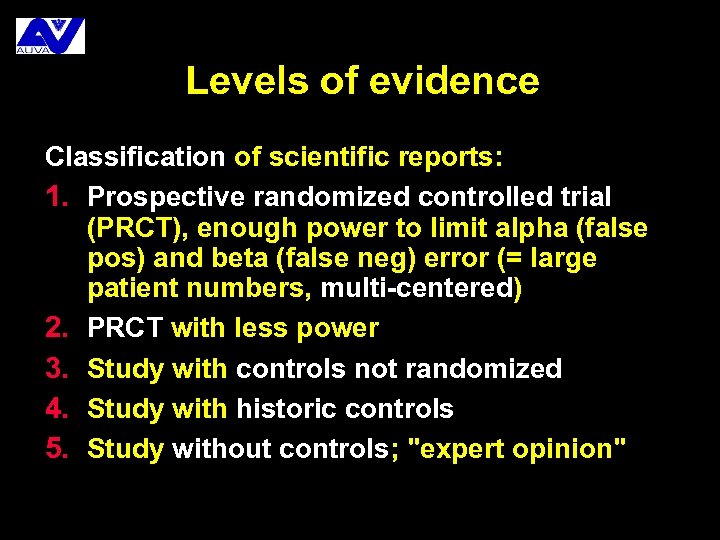
Levels of evidence Classification of scientific reports: 1. Prospective randomized controlled trial (PRCT), enough power to limit alpha (false pos) and beta (false neg) error (= large patient numbers, multi-centered) 2. PRCT with less power 3. Study with controls not randomized 4. Study with historic controls 5. Study without controls; "expert opinion"
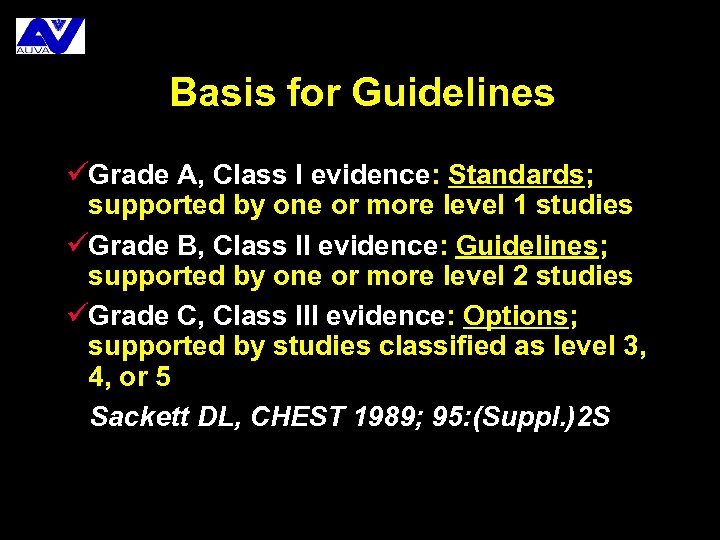
Basis for Guidelines üGrade A, Class I evidence: Standards; supported by one or more level 1 studies üGrade B, Class II evidence: Guidelines; supported by one or more level 2 studies üGrade C, Class III evidence: Options; supported by studies classified as level 3, 4, or 5 Sackett DL, CHEST 1989; 95: (Suppl. )2 S
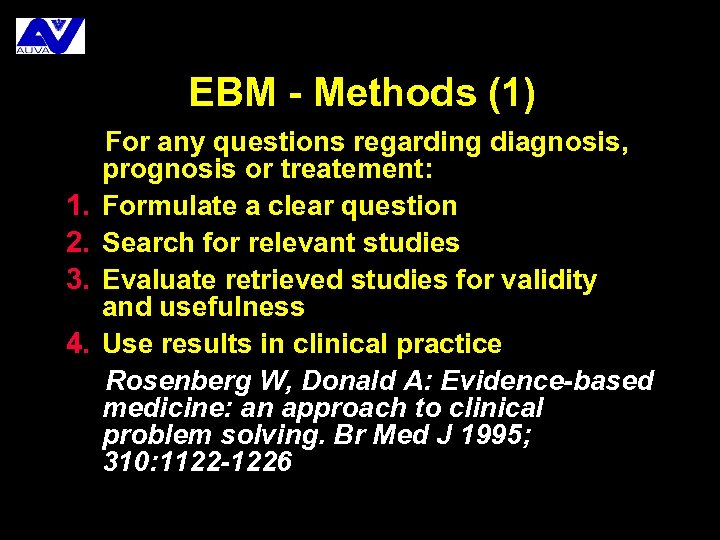
EBM - Methods (1) 1. 2. 3. 4. For any questions regarding diagnosis, prognosis or treatement: Formulate a clear question Search for relevant studies Evaluate retrieved studies for validity and usefulness Use results in clinical practice Rosenberg W, Donald A: Evidence-based medicine: an approach to clinical problem solving. Br Med J 1995; 310: 1122 -1226
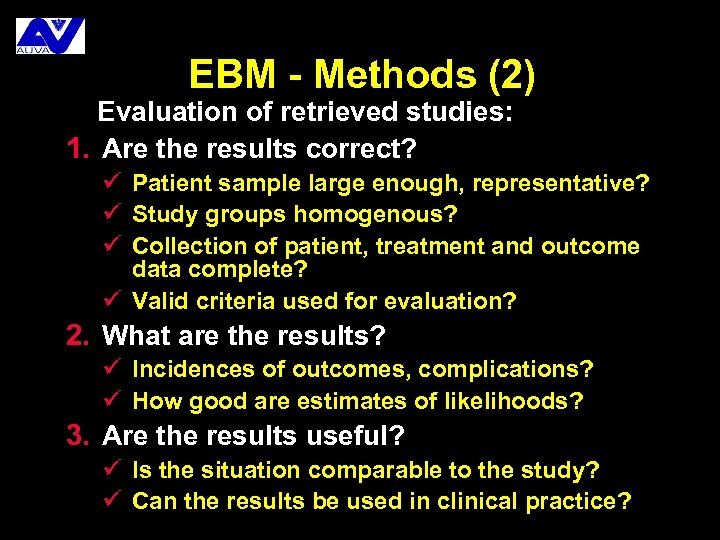
EBM - Methods (2) Evaluation of retrieved studies: 1. Are the results correct? ü Patient sample large enough, representative? ü Study groups homogenous? ü Collection of patient, treatment and outcome data complete? ü Valid criteria used for evaluation? 2. What are the results? ü Incidences of outcomes, complications? ü How good are estimates of likelihoods? 3. Are the results useful? ü Is the situation comparable to the study? ü Can the results be used in clinical practice?
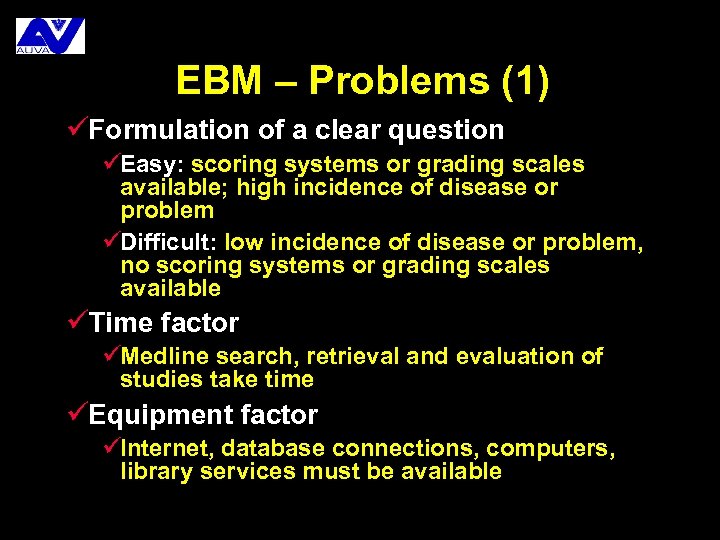
EBM – Problems (1) üFormulation of a clear question üEasy: scoring systems or grading scales available; high incidence of disease or problem üDifficult: low incidence of disease or problem, no scoring systems or grading scales available üTime factor üMedline search, retrieval and evaluation of studies take time üEquipment factor üInternet, database connections, computers, library services must be available
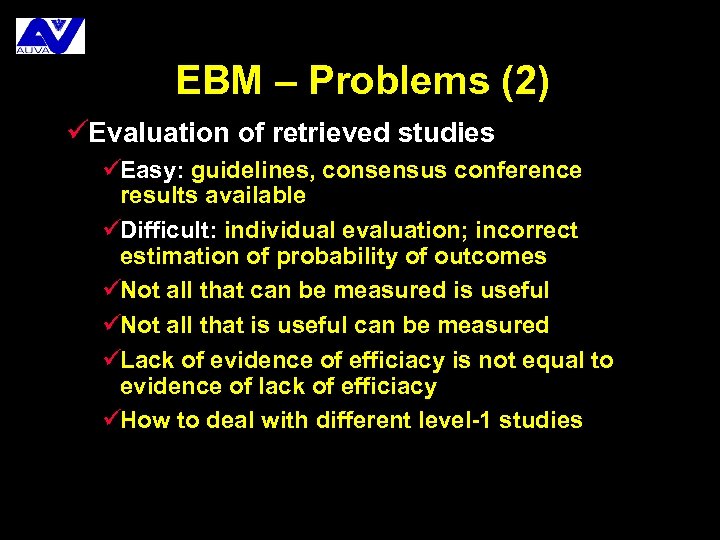
EBM – Problems (2) üEvaluation of retrieved studies üEasy: guidelines, consensus conference results available üDifficult: individual evaluation; incorrect estimation of probability of outcomes üNot all that can be measured is useful üNot all that is useful can be measured üLack of evidence of efficiacy is not equal to evidence of lack of efficiacy üHow to deal with different level-1 studies
EBM - Problems (3) üUse of selected evidence: even use of „best available evidence“ may lead to errors in management due to üIgnorance of local situation üApplication to patients or patient groups who are different from the study group üOveruse of resources in settings where resources are limited
Guidelines üAvailable for frequent problems üDeveloped by Consensus Conferences, Working Groups etc üShould be peer/reviewed üEffect of guideline compliance should be evaluated üShould be updated regularely üNon-compliance may lead to litigation!
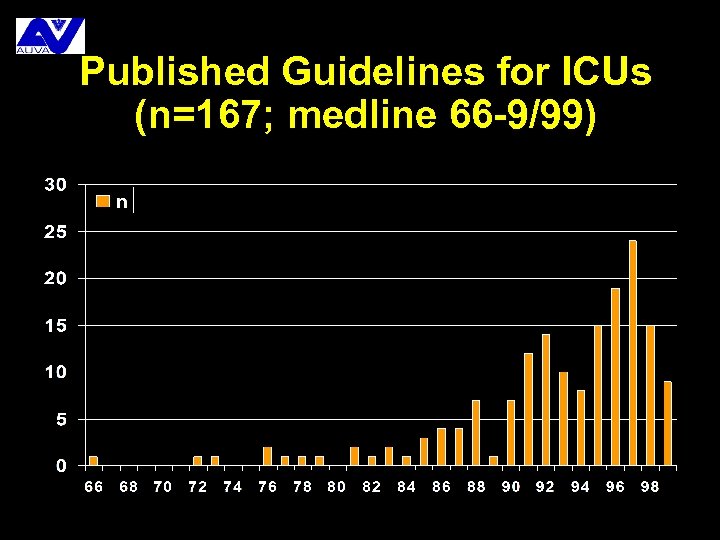
Published Guidelines for ICUs (n=167; medline 66 -9/99)
Why use EBM? üValidity üEBM-Review instead of tradition / opinion üBUT: Application of „best available evidence“ to an individual situation is still a medical decision, and may be wrong üQuality üCritical re-evaluation of clinical practice üScoring systems, grading scales required üStandardisation üTreatment „state of the art“
How to use EBM? üClinical experience should be assisted, not replaced by EBM üUse of EBM requires time, patience, good knowledge of English, computer skills, internet and database connections, and critical intellect üEBM-based solutions for critical situations are available ONLY if the hard work is done before üIndividual search, use of guidelines and clinical pathways possible
Individual Search üIf no guidelines are available üMedline: use different key words for search runs, identify possibly relevant studies üLibrary: retrieve papers üEvaluate, identify relevant papers üCreate treatment algorithm üImplement treatment algorithm üCheck results of algorithm implementation
Guidelines üAvailable for frequent problems üMedline: identify relevant guidelines üLibrary: retrieve original publication üCreate treatment algorithm adapted to local situation (= clinical pathway) üImplement treatment algorithm üCheck results of algorithm implementation
Medicl Decisions (1) üStarting point: Problem with diagnosis, prognosis, treatment üCan the problem be exactly defined? üNO: decision according to „clinical experience“ üYES: üIs the problem exactly defined? üNO: try to define the problem üYES:
Medical Decisions (2) üAre guidelines available? üYES: Creation and implementation of algorithm üNO: üIs experimental evidence (PRCT, MA) available? üYES: decision according EBM criteria üNO: decision according to „clinical experience“ – possible approaches should be tested in clinical study
Ultimate Goal of our Project To improve quality of care for brain trauma patients by using evidence based medicine (EBM) and continuous quality management (CQM)
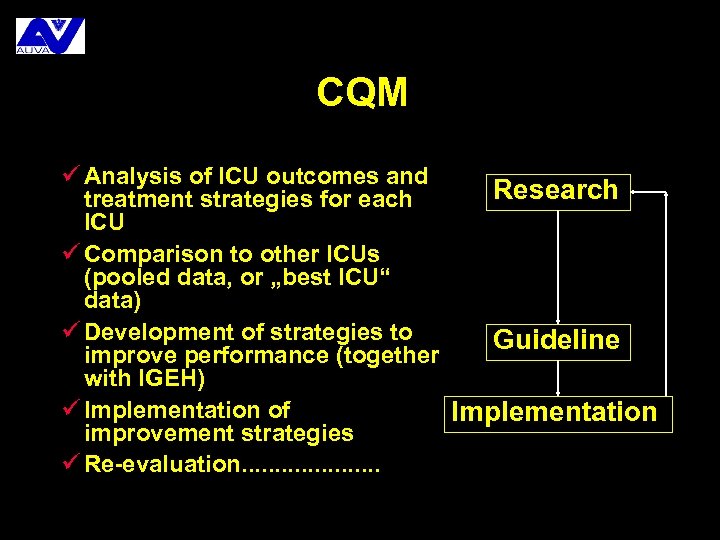
CQM ü Analysis of ICU outcomes and Research treatment strategies for each ICU ü Comparison to other ICUs (pooled data, or „best ICU“ data) ü Development of strategies to Guideline improve performance (together with IGEH) ü Implementation of Implementation improvement strategies ü Re-evaluation. . . . .
Outlook üGuidelines define goals but (usually) DO NOT explain how to reach these goals üOne of the most important steps in our project will be to develop, implement and test „clinical pathways“ üClinical pathways should explain how to reach the goals defined by the guidelines I LOOK FORWARD TO WORK WITH YOU ON THIS FASCINATING PROJECT THANK YOU
d84efddd72d16067209f88d42c061bb8.ppt