feb432a01da68c64d24a1558756f63b3.ppt
- Количество слайдов: 31
 Trauma-Aware Reproductive Care for People Living with HIV and Those Living with Risk Jay Mac. Gillivray, RM Mark H. Yudin, MD, MSc, FRCSC Positive Pregnancy Program (P 3) Toronto, Canada
Trauma-Aware Reproductive Care for People Living with HIV and Those Living with Risk Jay Mac. Gillivray, RM Mark H. Yudin, MD, MSc, FRCSC Positive Pregnancy Program (P 3) Toronto, Canada
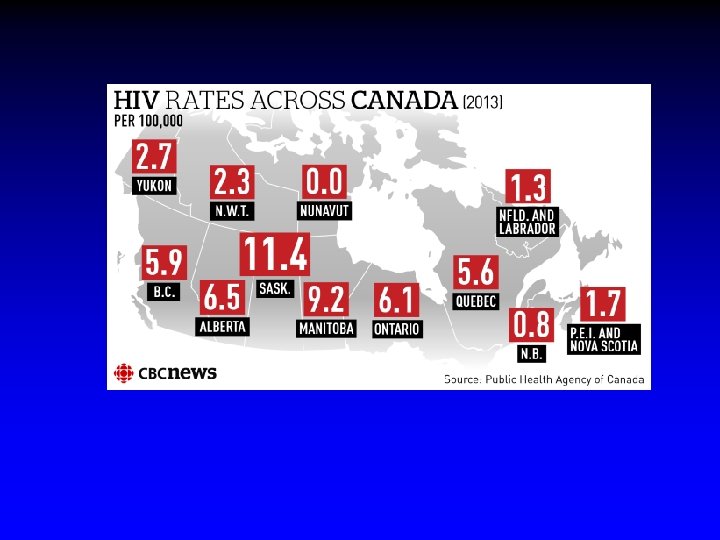
 Background
Background
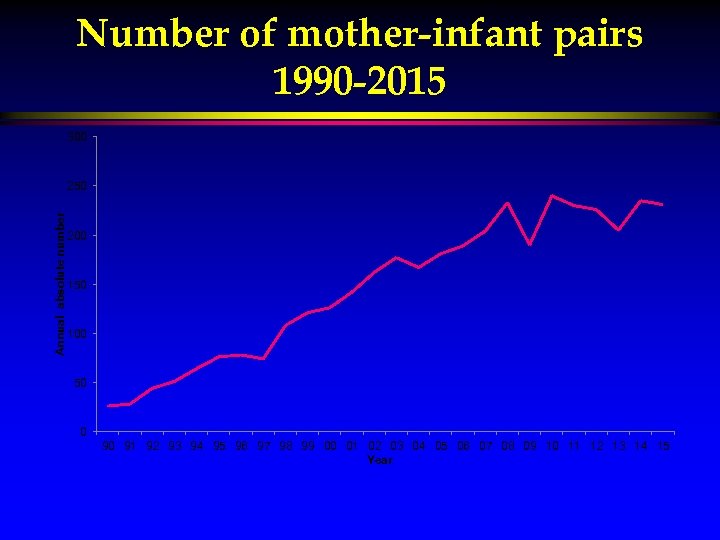 Number of mother-infant pairs 1990 -2015 300 Annual absolute number 250 200 150 100 50 0 90 91 92 93 94 95 96 97 98 99 00 01 02 03 04 05 06 07 08 09 10 11 12 13 14 15 Year
Number of mother-infant pairs 1990 -2015 300 Annual absolute number 250 200 150 100 50 0 90 91 92 93 94 95 96 97 98 99 00 01 02 03 04 05 06 07 08 09 10 11 12 13 14 15 Year
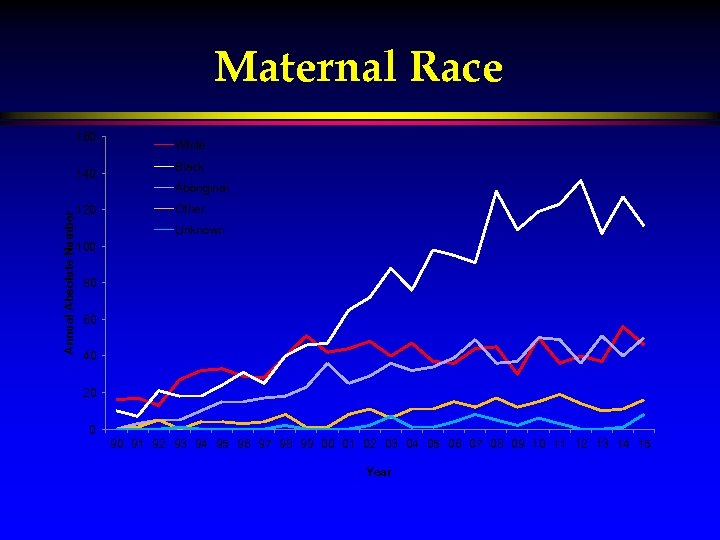 Maternal Race 160 140 White Black Annual Absolute Number Aboriginal 120 Other Unknown 100 80 60 40 20 0 90 91 92 93 94 95 96 97 98 99 00 01 02 03 04 05 06 07 08 09 10 11 12 13 14 15 Year
Maternal Race 160 140 White Black Annual Absolute Number Aboriginal 120 Other Unknown 100 80 60 40 20 0 90 91 92 93 94 95 96 97 98 99 00 01 02 03 04 05 06 07 08 09 10 11 12 13 14 15 Year
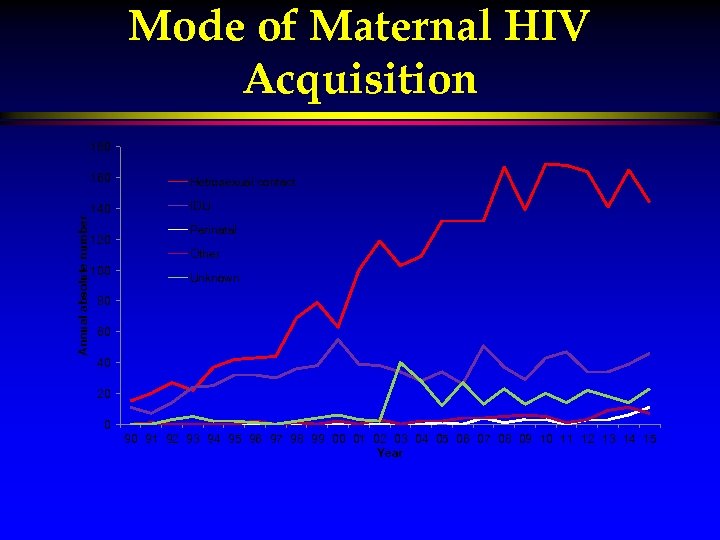 Mode of Maternal HIV Acquisition 180 Annual absolute number 160 Hetrosexual contact 140 IDU 120 Perinatal Other 100 Unknown 80 60 40 20 0 90 91 92 93 94 95 96 97 98 99 00 01 02 03 04 05 06 07 08 09 10 11 12 13 14 15 Year
Mode of Maternal HIV Acquisition 180 Annual absolute number 160 Hetrosexual contact 140 IDU 120 Perinatal Other 100 Unknown 80 60 40 20 0 90 91 92 93 94 95 96 97 98 99 00 01 02 03 04 05 06 07 08 09 10 11 12 13 14 15 Year
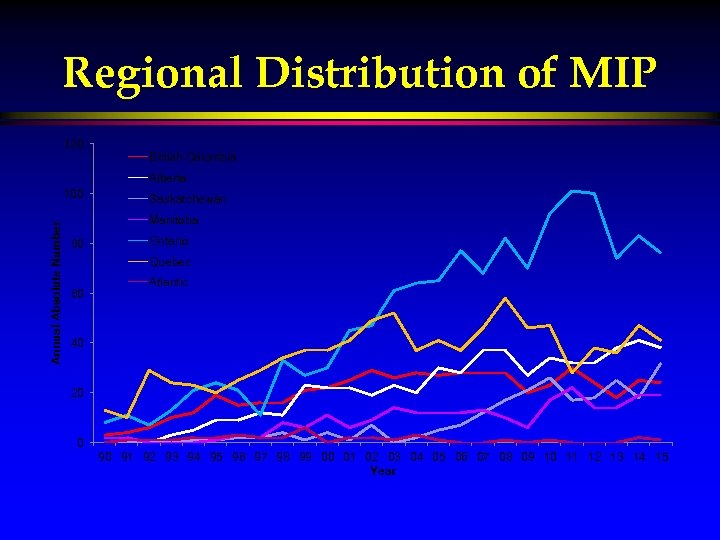 Regional Distribution of MIP 120 British Columbia Alberta Annual Absolute Number 100 Saskatchewan Manitoba 80 Ontario Quebec 60 Atlantic 40 20 0 90 91 92 93 94 95 96 97 98 99 00 01 02 03 04 05 06 07 08 09 10 11 12 13 14 15 Year
Regional Distribution of MIP 120 British Columbia Alberta Annual Absolute Number 100 Saskatchewan Manitoba 80 Ontario Quebec 60 Atlantic 40 20 0 90 91 92 93 94 95 96 97 98 99 00 01 02 03 04 05 06 07 08 09 10 11 12 13 14 15 Year
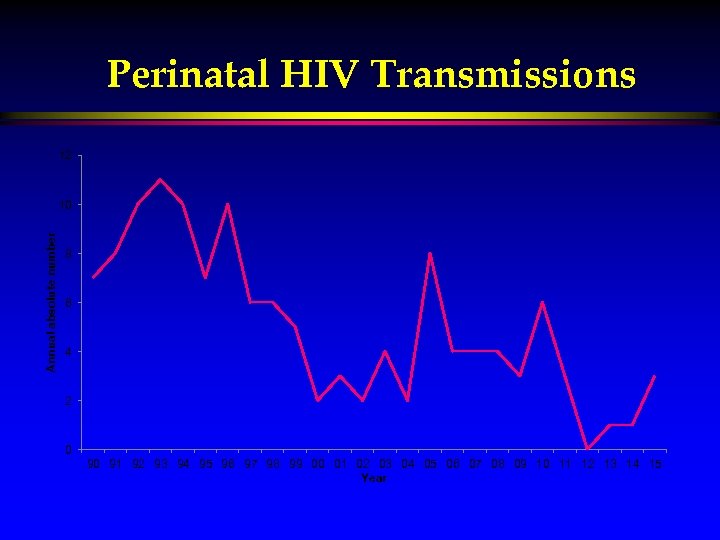 Perinatal HIV Transmissions 12 Annual absolute number 10 8 6 4 2 0 90 91 92 93 94 95 96 97 98 99 00 01 02 03 04 05 06 07 08 09 10 11 12 13 14 15 Year
Perinatal HIV Transmissions 12 Annual absolute number 10 8 6 4 2 0 90 91 92 93 94 95 96 97 98 99 00 01 02 03 04 05 06 07 08 09 10 11 12 13 14 15 Year
 Evolution and Development of P 3
Evolution and Development of P 3
 Positive Pregnancy Program
Positive Pregnancy Program
 Positive Pregnancy Program • Premise of Model A collaborative model providing medical care, health promotion and resources • Midwifery, Obstetrics, Nursing, Social Work, and robust community partnerships • Commitment to clients: respect, confidentiality, dignity, with highest standard of care using latest evidence • Normalizing care for HIV+ community •
Positive Pregnancy Program • Premise of Model A collaborative model providing medical care, health promotion and resources • Midwifery, Obstetrics, Nursing, Social Work, and robust community partnerships • Commitment to clients: respect, confidentiality, dignity, with highest standard of care using latest evidence • Normalizing care for HIV+ community •
 Positive Pregnancy Program • Preparation of Model Out of hospital community consultation • Involved midwifery governing bodies and hospital medical directors in planning • Reviewed literature on care models •
Positive Pregnancy Program • Preparation of Model Out of hospital community consultation • Involved midwifery governing bodies and hospital medical directors in planning • Reviewed literature on care models •
 Positive Pregnancy Program • Community Partnerships • Culturally-based ASOs • Multiple front line agencies • Legal and Housing resources • Peer support services • Settlement services • Medical Partnerships • HIV, Pediatrics, Psychiatry, Pharmacy
Positive Pregnancy Program • Community Partnerships • Culturally-based ASOs • Multiple front line agencies • Legal and Housing resources • Peer support services • Settlement services • Medical Partnerships • HIV, Pediatrics, Psychiatry, Pharmacy
 Strength and Resiliency • • Clients are not victims They are survivors They have remarkable resiliency and wisdom We are not ‘helping’ them- they are truly partners in care
Strength and Resiliency • • Clients are not victims They are survivors They have remarkable resiliency and wisdom We are not ‘helping’ them- they are truly partners in care
 Gender-Based Violence in Conflict Zones • “Forced migration caused by conflict increases the vulnerability of women in every regard but especially to gender-based violence- rape, torture, abduction, forced marriage, slavery, trafficking, and forced pregnancies. ” • Remarks by Judy A. Benjamin, Senior Technical Advisor, Women’s Commission for Refugee Women and Children. Presented at The World Bank, International Women’s Day, March 8, 2001
Gender-Based Violence in Conflict Zones • “Forced migration caused by conflict increases the vulnerability of women in every regard but especially to gender-based violence- rape, torture, abduction, forced marriage, slavery, trafficking, and forced pregnancies. ” • Remarks by Judy A. Benjamin, Senior Technical Advisor, Women’s Commission for Refugee Women and Children. Presented at The World Bank, International Women’s Day, March 8, 2001
 Positive Pregnancy Program • Demographics • Greater than 50% of women living in Canada less than 5 years • Over-representation of Racialized communities, including people of colour and Indigenous communities • Extreme marginalization, infrequent access to care, often lost to f/u
Positive Pregnancy Program • Demographics • Greater than 50% of women living in Canada less than 5 years • Over-representation of Racialized communities, including people of colour and Indigenous communities • Extreme marginalization, infrequent access to care, often lost to f/u
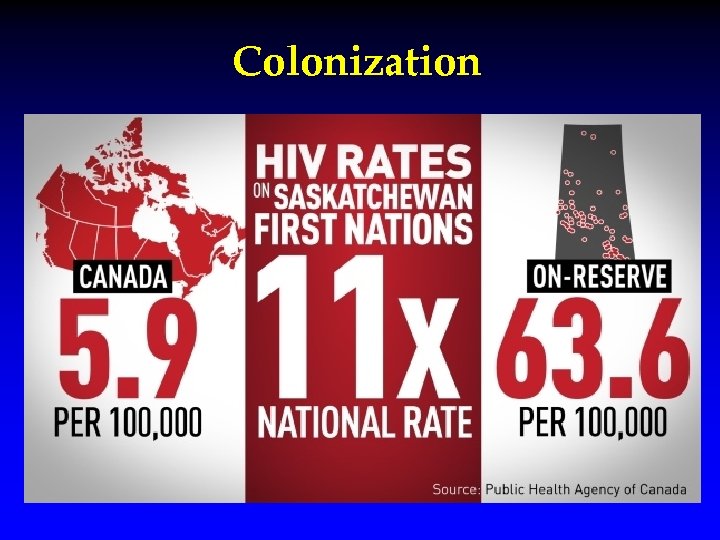 Colonization
Colonization
 P 3 Broad Demographics • • people newly arriving from conflict zones survivors of gender-based violence, migration histories of incarceration street-affected or homeless people in exploited sex work/survival sex people with substance use, mental health issues very few Anglo women of privilege and access Strong theme of trauma, often unresolved, throughout
P 3 Broad Demographics • • people newly arriving from conflict zones survivors of gender-based violence, migration histories of incarceration street-affected or homeless people in exploited sex work/survival sex people with substance use, mental health issues very few Anglo women of privilege and access Strong theme of trauma, often unresolved, throughout
 Trauma, Substance use, Exploited sex work, Street life and Pregnancy: Living with increased risk of HIV
Trauma, Substance use, Exploited sex work, Street life and Pregnancy: Living with increased risk of HIV
 Interconnected truths • • Pregnancy isn’t always planned- sometimes it is Substance use in pregnancy doesn’t just happen Trauma isn’t self-inflicted HIV is unintended Harm reduction works Respect is essential Racism in health care and its affects are real
Interconnected truths • • Pregnancy isn’t always planned- sometimes it is Substance use in pregnancy doesn’t just happen Trauma isn’t self-inflicted HIV is unintended Harm reduction works Respect is essential Racism in health care and its affects are real
 Street Realities Approximately 1, 000 women of childbearing age will sleep in the streets of Toronto on any given night. Cheung 2004
Street Realities Approximately 1, 000 women of childbearing age will sleep in the streets of Toronto on any given night. Cheung 2004
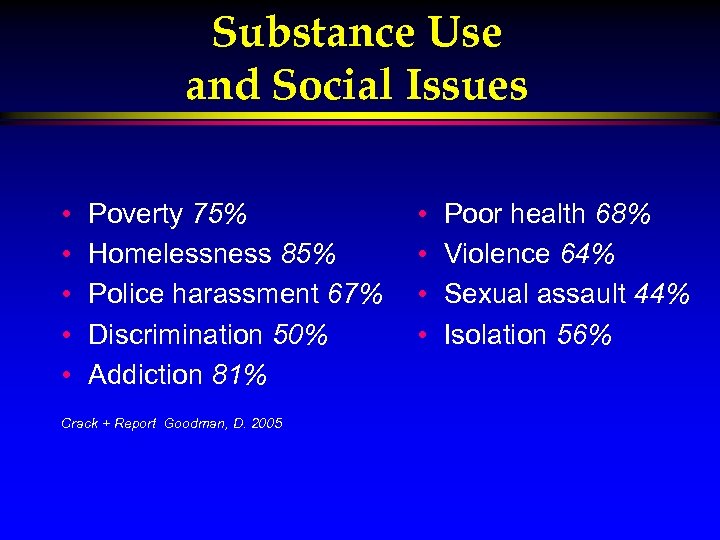 Substance Use and Social Issues • • • Poverty 75% Homelessness 85% Police harassment 67% Discrimination 50% Addiction 81% Crack + Report Goodman, D. 2005 • • Poor health 68% Violence 64% Sexual assault 44% Isolation 56%
Substance Use and Social Issues • • • Poverty 75% Homelessness 85% Police harassment 67% Discrimination 50% Addiction 81% Crack + Report Goodman, D. 2005 • • Poor health 68% Violence 64% Sexual assault 44% Isolation 56%
 Exploited ‘Sex’ Whilst Pregnant • Often cant negotiate safer sex=violence, low self esteem, lack of power • People worth more on street when pregnant • Being run by someone else • May be someone else’s for-profit income
Exploited ‘Sex’ Whilst Pregnant • Often cant negotiate safer sex=violence, low self esteem, lack of power • People worth more on street when pregnant • Being run by someone else • May be someone else’s for-profit income
 Harm Reduction: clients must lead • • • K. B. - 34 years old. G 2 p 1. one previous term vaginal birth 10 months earlier=child apprehended. Brought into care by street team at 32 weeks. Blasting an H point 3 x/day. First appointment: =“do you have any screens? ” Keep harm reduction bags at work and in my car=Gave screen without comment. Opened discussion of use pattern and related issues, strategies for harm reduction. “I'm comin’ back here”.
Harm Reduction: clients must lead • • • K. B. - 34 years old. G 2 p 1. one previous term vaginal birth 10 months earlier=child apprehended. Brought into care by street team at 32 weeks. Blasting an H point 3 x/day. First appointment: =“do you have any screens? ” Keep harm reduction bags at work and in my car=Gave screen without comment. Opened discussion of use pattern and related issues, strategies for harm reduction. “I'm comin’ back here”.
 Care Providers’ Judgements as Barriers to Care • Do clients have the autonomy to decide on appointments? • The great divide: I drove to clinic from the house I own; how did she get there and from where? Acknowledge my privilege. • Lack of awareness of true issues. Where is she going to get prenatal vitamins if she has no money, no bathroom to put them in, hasn’t eaten for a day and a half and she is drug sick? • Social determinants of health are real.
Care Providers’ Judgements as Barriers to Care • Do clients have the autonomy to decide on appointments? • The great divide: I drove to clinic from the house I own; how did she get there and from where? Acknowledge my privilege. • Lack of awareness of true issues. Where is she going to get prenatal vitamins if she has no money, no bathroom to put them in, hasn’t eaten for a day and a half and she is drug sick? • Social determinants of health are real.
 Trauma and Care Considerations • Often a time clients reflect on their history • Give consent too easily, be aware of power imbalance and gender-based fear. (watch for ‘trauma influenced consent’, Jay’s phrase) • Assume that any labour supports are unaware of status (eg. take charts out of room) • Sit down when talking, doing a vaginal exam or delivering the baby • Ask for permission before any touching
Trauma and Care Considerations • Often a time clients reflect on their history • Give consent too easily, be aware of power imbalance and gender-based fear. (watch for ‘trauma influenced consent’, Jay’s phrase) • Assume that any labour supports are unaware of status (eg. take charts out of room) • Sit down when talking, doing a vaginal exam or delivering the baby • Ask for permission before any touching
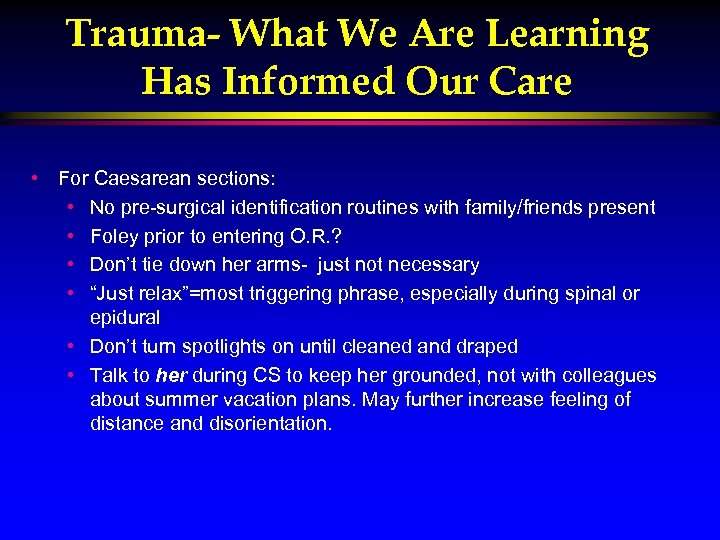 Trauma- What We Are Learning Has Informed Our Care • For Caesarean sections: • No pre-surgical identification routines with family/friends present • Foley prior to entering O. R. ? • Don’t tie down her arms- just not necessary • “Just relax”=most triggering phrase, especially during spinal or epidural • Don’t turn spotlights on until cleaned and draped • Talk to her during CS to keep her grounded, not with colleagues about summer vacation plans. May further increase feeling of distance and disorientation.
Trauma- What We Are Learning Has Informed Our Care • For Caesarean sections: • No pre-surgical identification routines with family/friends present • Foley prior to entering O. R. ? • Don’t tie down her arms- just not necessary • “Just relax”=most triggering phrase, especially during spinal or epidural • Don’t turn spotlights on until cleaned and draped • Talk to her during CS to keep her grounded, not with colleagues about summer vacation plans. May further increase feeling of distance and disorientation.
 What We Have Learned; So Far
What We Have Learned; So Far
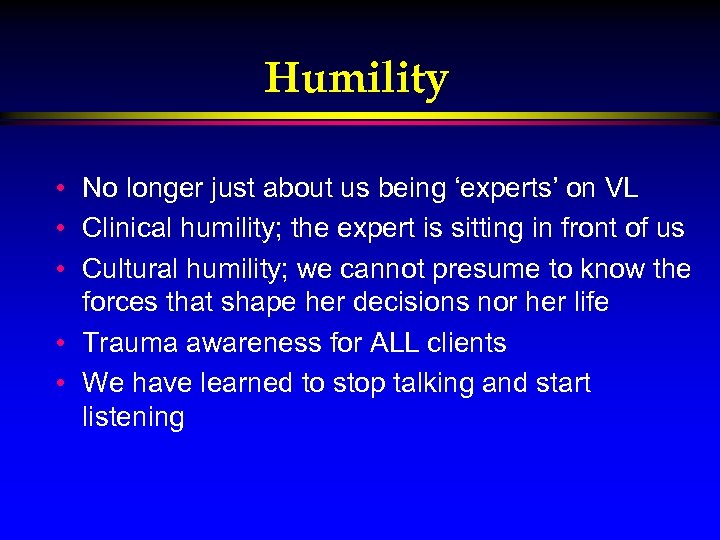 Humility • No longer just about us being ‘experts’ on VL • Clinical humility; the expert is sitting in front of us • Cultural humility; we cannot presume to know the forces that shape her decisions nor her life • Trauma awareness for ALL clients • We have learned to stop talking and start listening
Humility • No longer just about us being ‘experts’ on VL • Clinical humility; the expert is sitting in front of us • Cultural humility; we cannot presume to know the forces that shape her decisions nor her life • Trauma awareness for ALL clients • We have learned to stop talking and start listening
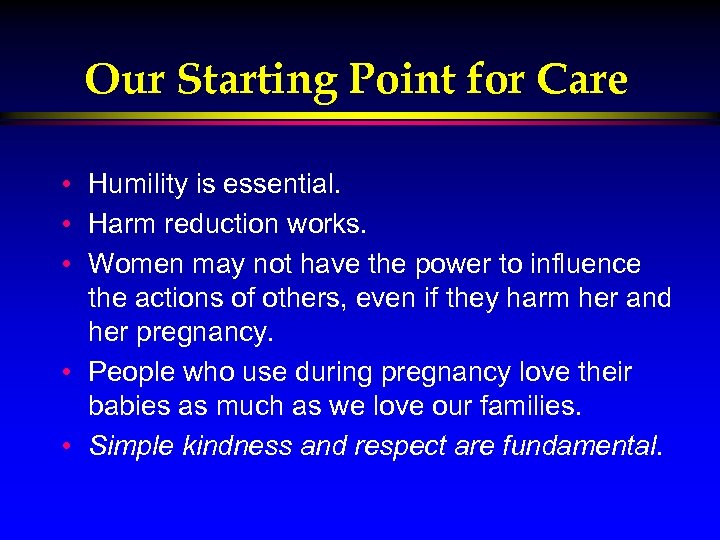 Our Starting Point for Care • Humility is essential. • Harm reduction works. • Women may not have the power to influence the actions of others, even if they harm her and her pregnancy. • People who use during pregnancy love their babies as much as we love our families. • Simple kindness and respect are fundamental.
Our Starting Point for Care • Humility is essential. • Harm reduction works. • Women may not have the power to influence the actions of others, even if they harm her and her pregnancy. • People who use during pregnancy love their babies as much as we love our families. • Simple kindness and respect are fundamental.


