5fc789459d8ce6e1f5d7fc3045dfecf3.ppt
- Количество слайдов: 57
 Transfusion Third Year Medical Student Teaching Friday 11 th March 2016 Dr Dawn Swan – Haematology ST 4 Registrar Dr Holly Owen – Foundation Year Two Slides by Dr Jayne Peters- Haematology ST 5 Registrar
Transfusion Third Year Medical Student Teaching Friday 11 th March 2016 Dr Dawn Swan – Haematology ST 4 Registrar Dr Holly Owen – Foundation Year Two Slides by Dr Jayne Peters- Haematology ST 5 Registrar
 Overview • The Journey of Blood • Matching blood • Team learning session • Review of answers • Summary and questions
Overview • The Journey of Blood • Matching blood • Team learning session • Review of answers • Summary and questions
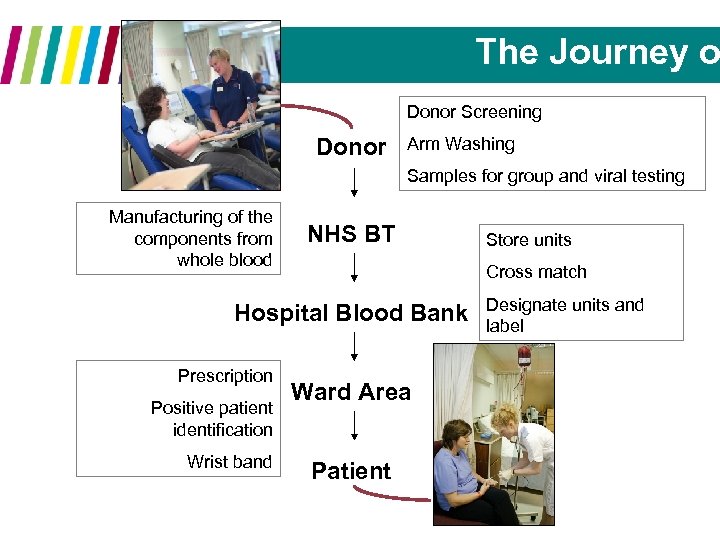 The Journey o Donor Screening Donor Arm Washing Samples for group and viral testing Manufacturing of the components from whole blood NHS BT Cross match Hospital Blood Bank Prescription Positive patient identification Wrist band Store units Ward Area Patient Designate units and label
The Journey o Donor Screening Donor Arm Washing Samples for group and viral testing Manufacturing of the components from whole blood NHS BT Cross match Hospital Blood Bank Prescription Positive patient identification Wrist band Store units Ward Area Patient Designate units and label
 Blood Collectio
Blood Collectio
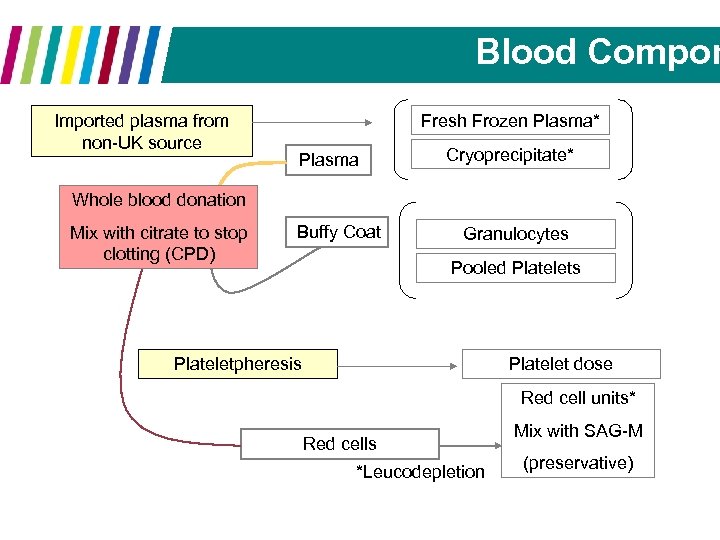 Blood Compon Imported plasma from non-UK source Fresh Frozen Plasma* Plasma Cryoprecipitate* Whole blood donation Mix with citrate to stop clotting (CPD) Buffy Coat Granulocytes Pooled Platelets Plateletpheresis Platelet dose Red cell units* Red cells *Leucodepletion Mix with SAG-M (preservative)
Blood Compon Imported plasma from non-UK source Fresh Frozen Plasma* Plasma Cryoprecipitate* Whole blood donation Mix with citrate to stop clotting (CPD) Buffy Coat Granulocytes Pooled Platelets Plateletpheresis Platelet dose Red cell units* Red cells *Leucodepletion Mix with SAG-M (preservative)
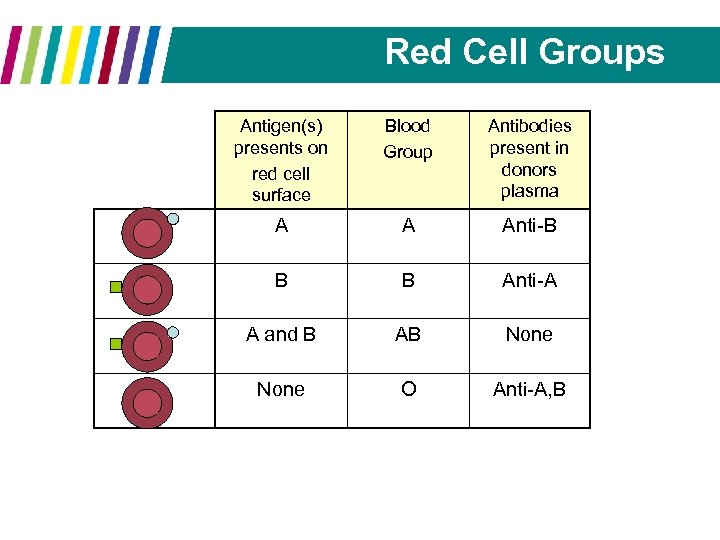 Red Cell Groups Antigen(s) presents on red cell surface Blood Group Antibodies present in donors plasma A A Anti-B B B Anti-A A and B AB None O Anti-A, B
Red Cell Groups Antigen(s) presents on red cell surface Blood Group Antibodies present in donors plasma A A Anti-B B B Anti-A A and B AB None O Anti-A, B
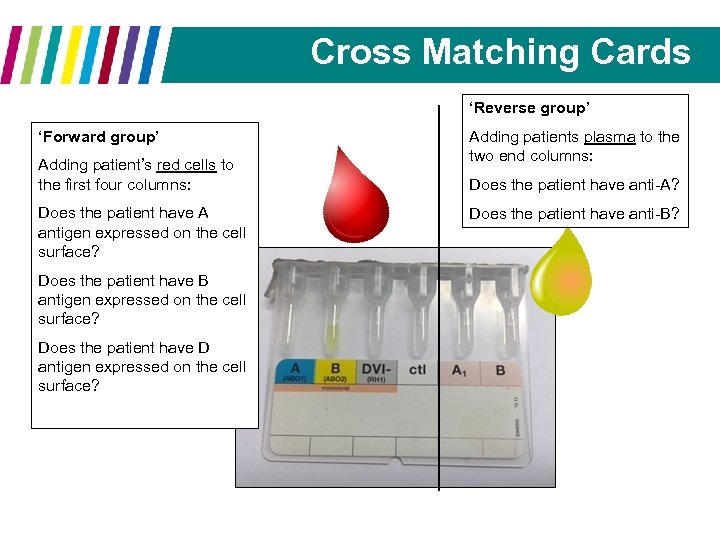 Cross Matching Cards ‘Reverse group’ ‘Forward group’ Adding patient’s red cells to the first four columns: Does the patient have A antigen expressed on the cell surface? Does the patient have B antigen expressed on the cell surface? Does the patient have D antigen expressed on the cell surface? Adding patients plasma to the two end columns: Does the patient have anti-A? Does the patient have anti-B?
Cross Matching Cards ‘Reverse group’ ‘Forward group’ Adding patient’s red cells to the first four columns: Does the patient have A antigen expressed on the cell surface? Does the patient have B antigen expressed on the cell surface? Does the patient have D antigen expressed on the cell surface? Adding patients plasma to the two end columns: Does the patient have anti-A? Does the patient have anti-B?
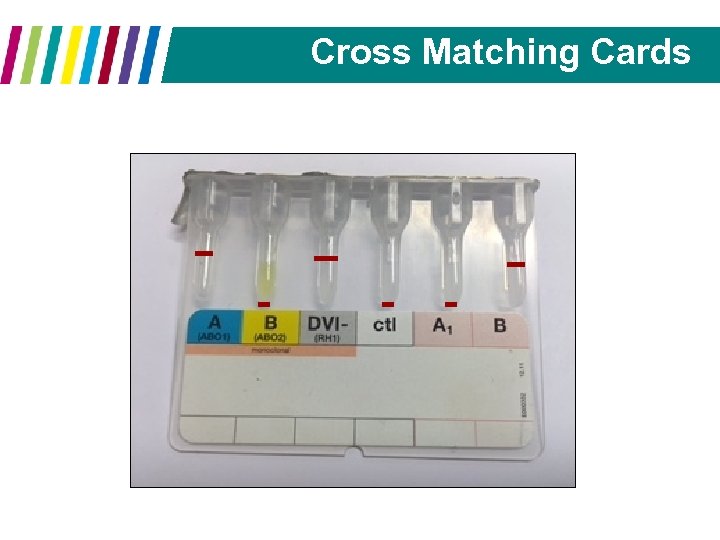 Cross Matching Cards
Cross Matching Cards
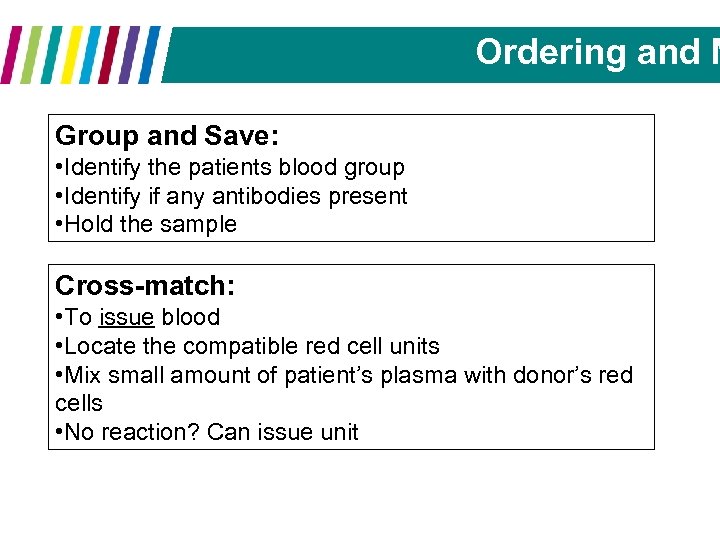 Ordering and M Group and Save: • Identify the patients blood group • Identify if any antibodies present • Hold the sample Cross-match: • To issue blood • Locate the compatible red cell units • Mix small amount of patient’s plasma with donor’s red cells • No reaction? Can issue unit
Ordering and M Group and Save: • Identify the patients blood group • Identify if any antibodies present • Hold the sample Cross-match: • To issue blood • Locate the compatible red cell units • Mix small amount of patient’s plasma with donor’s red cells • No reaction? Can issue unit
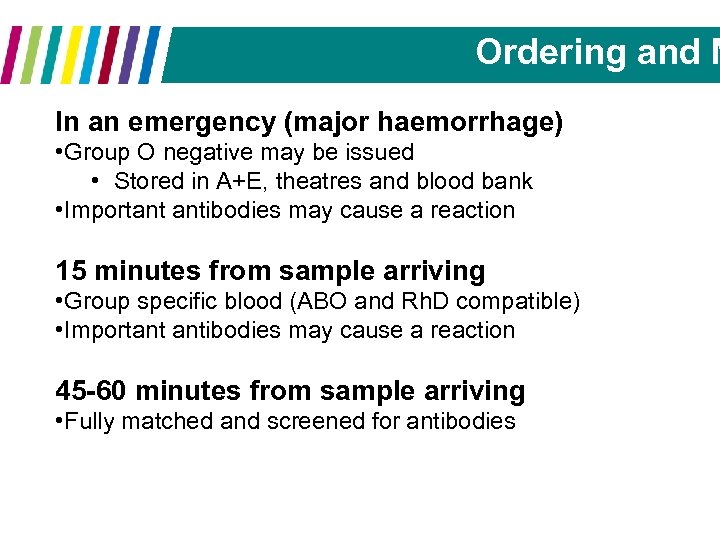 Ordering and M In an emergency (major haemorrhage) • Group O negative may be issued • Stored in A+E, theatres and blood bank • Important antibodies may cause a reaction 15 minutes from sample arriving • Group specific blood (ABO and Rh. D compatible) • Important antibodies may cause a reaction 45 -60 minutes from sample arriving • Fully matched and screened for antibodies
Ordering and M In an emergency (major haemorrhage) • Group O negative may be issued • Stored in A+E, theatres and blood bank • Important antibodies may cause a reaction 15 minutes from sample arriving • Group specific blood (ABO and Rh. D compatible) • Important antibodies may cause a reaction 45 -60 minutes from sample arriving • Fully matched and screened for antibodies
 Team Learning: Discuss your answers as a small group using the materials provided to help guide your decisions.
Team Learning: Discuss your answers as a small group using the materials provided to help guide your decisions.
 Red Cells Questions 1 and 4
Red Cells Questions 1 and 4
 Question 1: A GP refers in an asymptomatic 30 year old female with a history of menorrhagia and a Hb 44 g/L. Initial treatment should include a 2 unit transfusion of packed red cells. True or false?
Question 1: A GP refers in an asymptomatic 30 year old female with a history of menorrhagia and a Hb 44 g/L. Initial treatment should include a 2 unit transfusion of packed red cells. True or false?
 Question 1: A GP refers in an asymptomatic 30 year old female with a history of menorrhagia and a Hb 44 g/L. Initial treatment should include a 2 unit transfusion of packed red cells. True or false?
Question 1: A GP refers in an asymptomatic 30 year old female with a history of menorrhagia and a Hb 44 g/L. Initial treatment should include a 2 unit transfusion of packed red cells. True or false?
 Question 4: An 82 year old male with known diabetes and hypertension has a repeat Hb of 101 g/L following admission for recurrent chest pain. It is appropriate to transfuse him packed red cells. True or false?
Question 4: An 82 year old male with known diabetes and hypertension has a repeat Hb of 101 g/L following admission for recurrent chest pain. It is appropriate to transfuse him packed red cells. True or false?
 Question 4: An 82 year old male with known diabetes and hypertension has a repeat Hb of 101 g/L following admission for recurrent chest pain. It is appropriate to transfuse him packed red cells. True or false?
Question 4: An 82 year old male with known diabetes and hypertension has a repeat Hb of 101 g/L following admission for recurrent chest pain. It is appropriate to transfuse him packed red cells. True or false?
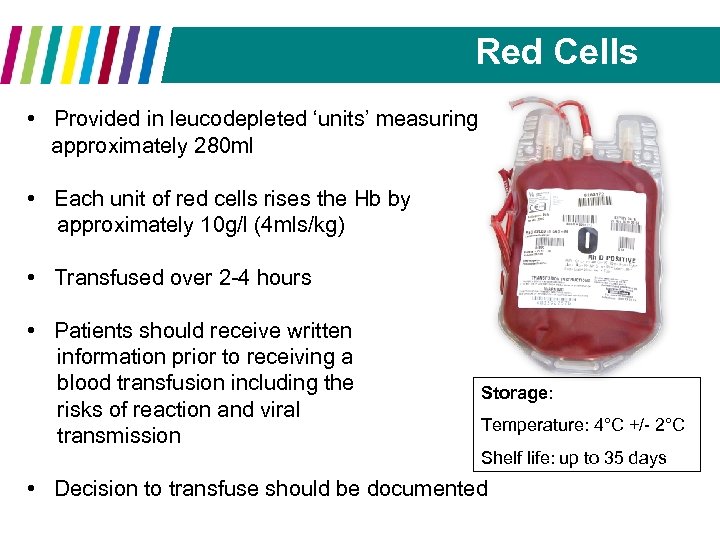 Red Cells • Provided in leucodepleted ‘units’ measuring approximately 280 ml • Each unit of red cells rises the Hb by approximately 10 g/l (4 mls/kg) • Transfused over 2 -4 hours • Patients should receive written information prior to receiving a blood transfusion including the risks of reaction and viral transmission Storage: Temperature: 4°C +/- 2°C Shelf life: up to 35 days • Decision to transfuse should be documented
Red Cells • Provided in leucodepleted ‘units’ measuring approximately 280 ml • Each unit of red cells rises the Hb by approximately 10 g/l (4 mls/kg) • Transfused over 2 -4 hours • Patients should receive written information prior to receiving a blood transfusion including the risks of reaction and viral transmission Storage: Temperature: 4°C +/- 2°C Shelf life: up to 35 days • Decision to transfuse should be documented
 Red Cells • No universal trigger for transfusion • Decision to transfuse should be based on clinical judgement • Asymptomatic patients with chronic anaemia secondary to iron deficiency may benefit from iron replacement rather than transfusion • Always assess haemotinics if not already done so for a patient presenting in an anaemic state • Is the result in keeping with what is expected? • ? dilutional or from a different patient
Red Cells • No universal trigger for transfusion • Decision to transfuse should be based on clinical judgement • Asymptomatic patients with chronic anaemia secondary to iron deficiency may benefit from iron replacement rather than transfusion • Always assess haemotinics if not already done so for a patient presenting in an anaemic state • Is the result in keeping with what is expected? • ? dilutional or from a different patient
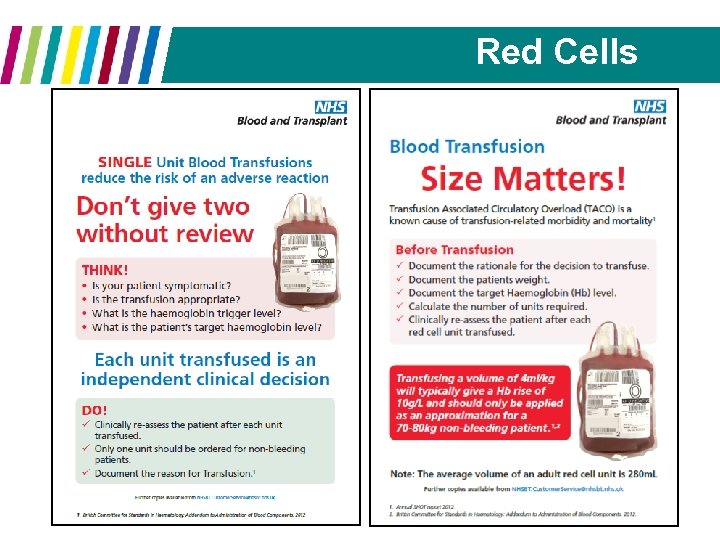 Red Cells
Red Cells
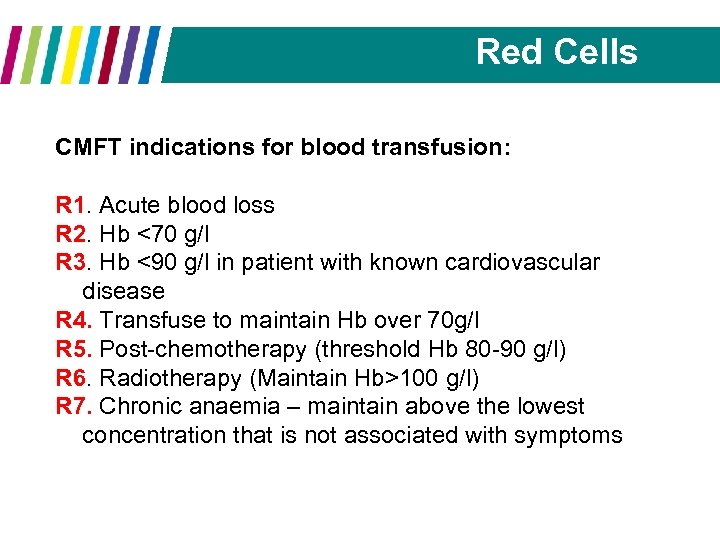 Red Cells CMFT indications for blood transfusion: R 1. Acute blood loss R 2. Hb <70 g/l R 3. Hb <90 g/l in patient with known cardiovascular disease R 4. Transfuse to maintain Hb over 70 g/l R 5. Post-chemotherapy (threshold Hb 80 -90 g/l) R 6. Radiotherapy (Maintain Hb>100 g/l) R 7. Chronic anaemia – maintain above the lowest concentration that is not associated with symptoms
Red Cells CMFT indications for blood transfusion: R 1. Acute blood loss R 2. Hb <70 g/l R 3. Hb <90 g/l in patient with known cardiovascular disease R 4. Transfuse to maintain Hb over 70 g/l R 5. Post-chemotherapy (threshold Hb 80 -90 g/l) R 6. Radiotherapy (Maintain Hb>100 g/l) R 7. Chronic anaemia – maintain above the lowest concentration that is not associated with symptoms
 FFP (Fresh Frozen Plasma) Questions 2 and 6
FFP (Fresh Frozen Plasma) Questions 2 and 6
 Question 2: A 45 year old male with alcoholic liver disease presents with gross ascites. You are asked to do a diagnostic tap, however note that the clotting screen is abnormal; PT 17. 2 (11 -14), APTT 26 (22 -28). It is recommended to administer FFP prior to proceeding True or false?
Question 2: A 45 year old male with alcoholic liver disease presents with gross ascites. You are asked to do a diagnostic tap, however note that the clotting screen is abnormal; PT 17. 2 (11 -14), APTT 26 (22 -28). It is recommended to administer FFP prior to proceeding True or false?
 Question 2: A 45 year old male with alcoholic liver disease presents with gross ascites. You are asked to do a diagnostic tap, however note that the clotting screen is abnormal; PT 17. 2 (11 -14), APTT 26 (22 -28). It is recommended to administer FFP prior to proceeding True or false?
Question 2: A 45 year old male with alcoholic liver disease presents with gross ascites. You are asked to do a diagnostic tap, however note that the clotting screen is abnormal; PT 17. 2 (11 -14), APTT 26 (22 -28). It is recommended to administer FFP prior to proceeding True or false?
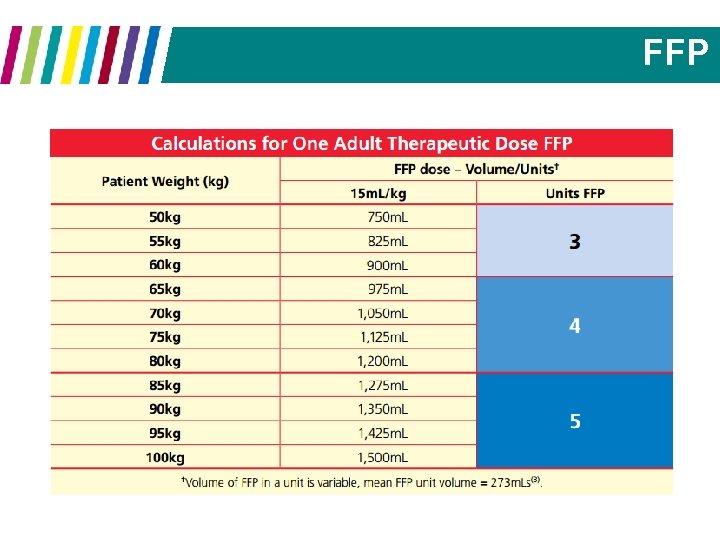
 Question 6: FFP is dosed according to patient weight. When clinically indicated, the average sized adult requires 2 units of FFP True or false?
Question 6: FFP is dosed according to patient weight. When clinically indicated, the average sized adult requires 2 units of FFP True or false?
 Question 6: FFP is dosed according to patient weight. When clinically indicated, the average sized adult requires 2 units of FFP True or false?
Question 6: FFP is dosed according to patient weight. When clinically indicated, the average sized adult requires 2 units of FFP True or false?
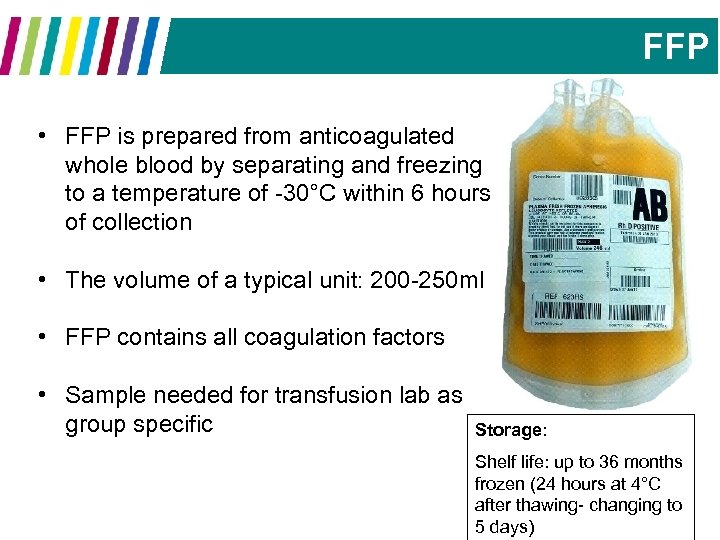 FFP • FFP is prepared from anticoagulated whole blood by separating and freezing to a temperature of -30°C within 6 hours of collection • The volume of a typical unit: 200 -250 ml • FFP contains all coagulation factors • Sample needed for transfusion lab as group specific Storage: Shelf life: up to 36 months frozen (24 hours at 4°C after thawing- changing to 5 days)
FFP • FFP is prepared from anticoagulated whole blood by separating and freezing to a temperature of -30°C within 6 hours of collection • The volume of a typical unit: 200 -250 ml • FFP contains all coagulation factors • Sample needed for transfusion lab as group specific Storage: Shelf life: up to 36 months frozen (24 hours at 4°C after thawing- changing to 5 days)
 Octoplas • Octaplas is a solvent detergent treated, prion reduced human plasma product • It has standardised coagulation factors content and is available in 200 ml bags with A, B, O and AB groups • Patients born on or after 1 st January 1996 should receive plasma from a country with a low risk of v. CJD • This product is also used for plasma exchanges for certain diagnoses such as thrombotic thrombocytopenic purpura
Octoplas • Octaplas is a solvent detergent treated, prion reduced human plasma product • It has standardised coagulation factors content and is available in 200 ml bags with A, B, O and AB groups • Patients born on or after 1 st January 1996 should receive plasma from a country with a low risk of v. CJD • This product is also used for plasma exchanges for certain diagnoses such as thrombotic thrombocytopenic purpura
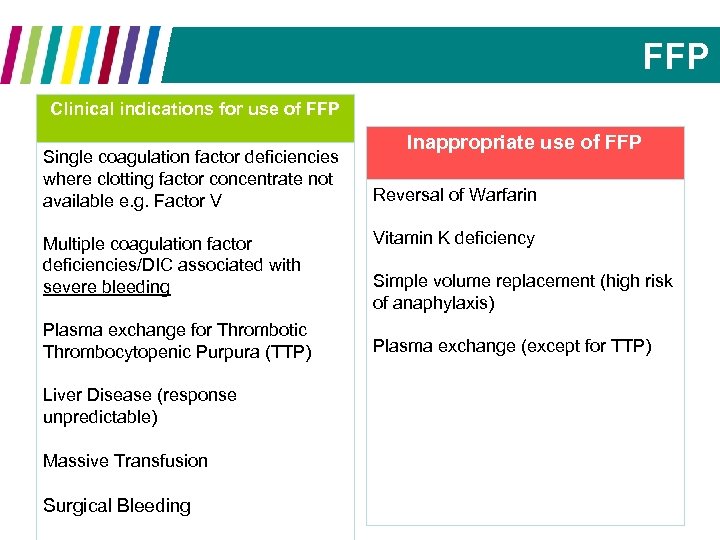 FFP Clinical indications for use of FFP Single coagulation factor deficiencies where clotting factor concentrate not available e. g. Factor V Multiple coagulation factor deficiencies/DIC associated with severe bleeding Plasma exchange for Thrombotic Thrombocytopenic Purpura (TTP) Liver Disease (response unpredictable) Massive Transfusion Surgical Bleeding Inappropriate use of FFP Reversal of Warfarin Vitamin K deficiency Simple volume replacement (high risk of anaphylaxis) Plasma exchange (except for TTP)
FFP Clinical indications for use of FFP Single coagulation factor deficiencies where clotting factor concentrate not available e. g. Factor V Multiple coagulation factor deficiencies/DIC associated with severe bleeding Plasma exchange for Thrombotic Thrombocytopenic Purpura (TTP) Liver Disease (response unpredictable) Massive Transfusion Surgical Bleeding Inappropriate use of FFP Reversal of Warfarin Vitamin K deficiency Simple volume replacement (high risk of anaphylaxis) Plasma exchange (except for TTP)
 FFP
FFP
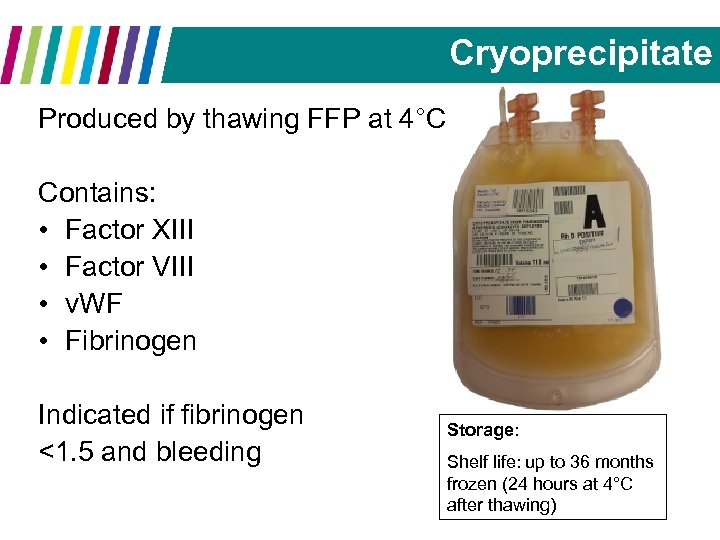 Cryoprecipitate Produced by thawing FFP at 4°C Contains: • Factor XIII • Factor VIII • v. WF • Fibrinogen Indicated if fibrinogen <1. 5 and bleeding Storage: Shelf life: up to 36 months frozen (24 hours at 4°C after thawing)
Cryoprecipitate Produced by thawing FFP at 4°C Contains: • Factor XIII • Factor VIII • v. WF • Fibrinogen Indicated if fibrinogen <1. 5 and bleeding Storage: Shelf life: up to 36 months frozen (24 hours at 4°C after thawing)
 Platelets Questions 3, 5 and 7
Platelets Questions 3, 5 and 7
 Question 3: During massive haemorrhage secondary to GI bleeding, it is advisable to keep the platelet count above 100 x 109/L? True or false?
Question 3: During massive haemorrhage secondary to GI bleeding, it is advisable to keep the platelet count above 100 x 109/L? True or false?
 Question 3: During massive haemorrhage secondary to GI bleeding, it is advisable to keep the platelet count above 100 x 109/L? True or false?
Question 3: During massive haemorrhage secondary to GI bleeding, it is advisable to keep the platelet count above 100 x 109/L? True or false?
 Question 5: A full blood count states the platelet count to be ‘ 6 x 109/l’ with an associated peripheral blood film comment of ‘platelet clumping seen. A prophylactic platelet transfusion (1 ATD) is indicated as the platelet count is <10 x 109/l? True or false?
Question 5: A full blood count states the platelet count to be ‘ 6 x 109/l’ with an associated peripheral blood film comment of ‘platelet clumping seen. A prophylactic platelet transfusion (1 ATD) is indicated as the platelet count is <10 x 109/l? True or false?
 Question 5: A full blood count states the platelet count to be ‘ 6 x 109/l’ with an associated peripheral blood film comment of ‘platelet clumping seen. A prophylactic platelet transfusion (1 ATD) is indicated as the platelet count is <10 x 109/l? True or false?
Question 5: A full blood count states the platelet count to be ‘ 6 x 109/l’ with an associated peripheral blood film comment of ‘platelet clumping seen. A prophylactic platelet transfusion (1 ATD) is indicated as the platelet count is <10 x 109/l? True or false?
 Question 7: A patient with thrombocytopenia secondary to sepsis has a repeat platelet count of 70 x 109/L and requires neurosurgery. You should give 1 ATD (adult treatment dose) of platelets then recheck the FBC. True or false?
Question 7: A patient with thrombocytopenia secondary to sepsis has a repeat platelet count of 70 x 109/L and requires neurosurgery. You should give 1 ATD (adult treatment dose) of platelets then recheck the FBC. True or false?
 Question 7: A patient with thrombocytopenia secondary to sepsis has a repeat platelet count of 70 x 109/L and requires neurosurgery. You should give 1 ATD (adult treatment dose) of platelets then recheck the FBC. True or false?
Question 7: A patient with thrombocytopenia secondary to sepsis has a repeat platelet count of 70 x 109/L and requires neurosurgery. You should give 1 ATD (adult treatment dose) of platelets then recheck the FBC. True or false?
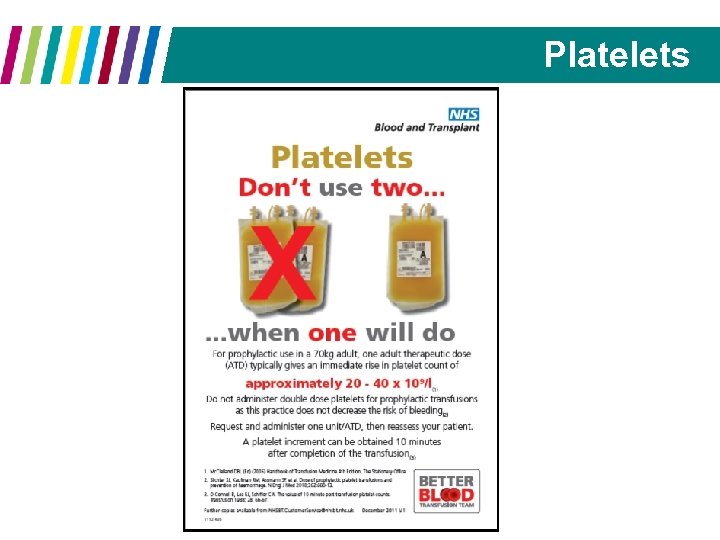
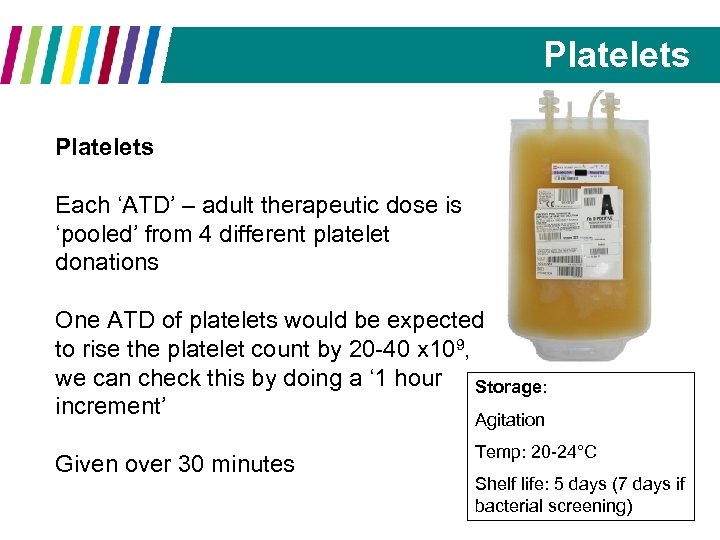 Platelets Each ‘ATD’ – adult therapeutic dose is ‘pooled’ from 4 different platelet donations One ATD of platelets would be expected to rise the platelet count by 20 -40 x 109, we can check this by doing a ‘ 1 hour Storage: increment’ Agitation Given over 30 minutes Temp: 20 -24°C Shelf life: 5 days (7 days if bacterial screening)
Platelets Each ‘ATD’ – adult therapeutic dose is ‘pooled’ from 4 different platelet donations One ATD of platelets would be expected to rise the platelet count by 20 -40 x 109, we can check this by doing a ‘ 1 hour Storage: increment’ Agitation Given over 30 minutes Temp: 20 -24°C Shelf life: 5 days (7 days if bacterial screening)
 Platelets
Platelets
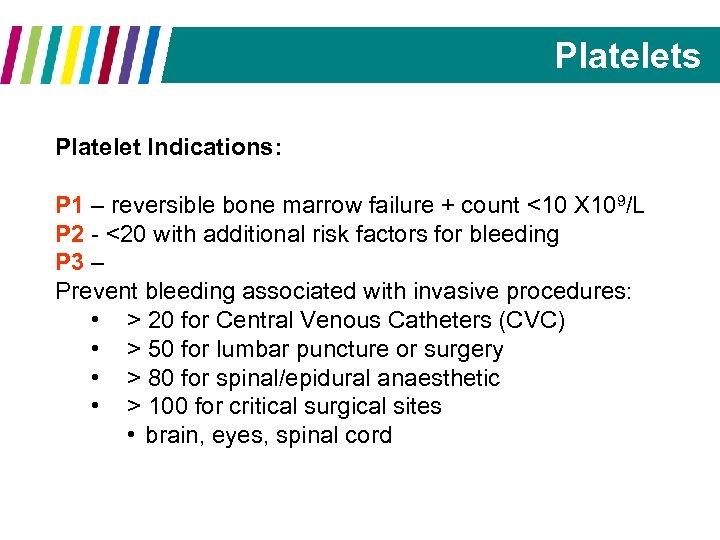 Platelets Platelet Indications: P 1 – reversible bone marrow failure + count <10 X 109/L P 2 - <20 with additional risk factors for bleeding P 3 – Prevent bleeding associated with invasive procedures: • > 20 for Central Venous Catheters (CVC) • > 50 for lumbar puncture or surgery • > 80 for spinal/epidural anaesthetic • > 100 for critical surgical sites • brain, eyes, spinal cord
Platelets Platelet Indications: P 1 – reversible bone marrow failure + count <10 X 109/L P 2 - <20 with additional risk factors for bleeding P 3 – Prevent bleeding associated with invasive procedures: • > 20 for Central Venous Catheters (CVC) • > 50 for lumbar puncture or surgery • > 80 for spinal/epidural anaesthetic • > 100 for critical surgical sites • brain, eyes, spinal cord
 Platelets Platelet Indications: P 4 – massive blood transfusion (after 1 circulating blood volume) P 5 – acquired platelet dysfunction P 6 – acute DIC and bleeding P 7 – inherited platelet dysfunction P 8 – primary immune thrombocytopenia for emergency treatment in advance of surgery or in major haemorrhage P 9 – post-transfusion purpura in the presence of major haemorrhage P 10 – Neonatal alloimmune thrombocytopenia (bleeding or prophylaxis, maintain >30)
Platelets Platelet Indications: P 4 – massive blood transfusion (after 1 circulating blood volume) P 5 – acquired platelet dysfunction P 6 – acute DIC and bleeding P 7 – inherited platelet dysfunction P 8 – primary immune thrombocytopenia for emergency treatment in advance of surgery or in major haemorrhage P 9 – post-transfusion purpura in the presence of major haemorrhage P 10 – Neonatal alloimmune thrombocytopenia (bleeding or prophylaxis, maintain >30)
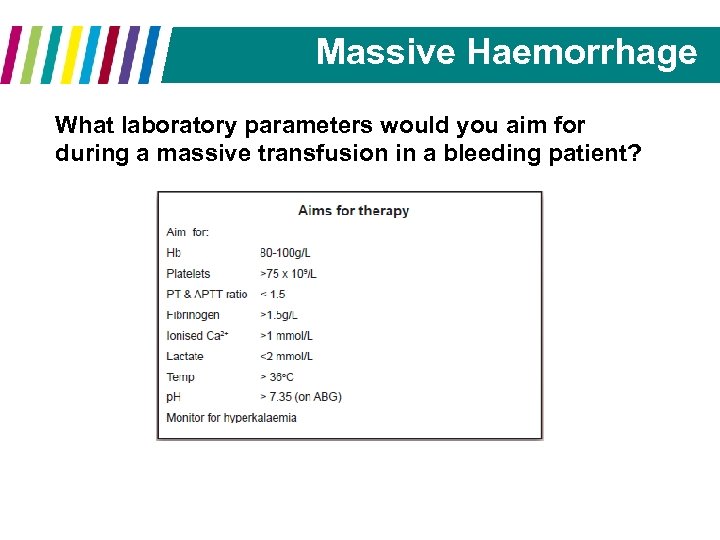 Massive Haemorrhage What laboratory parameters would you aim for during a massive transfusion in a bleeding patient?
Massive Haemorrhage What laboratory parameters would you aim for during a massive transfusion in a bleeding patient?
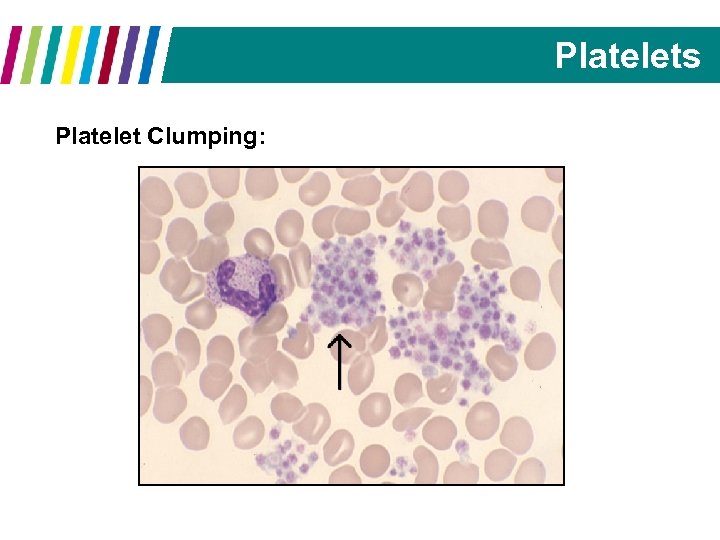 Platelets Platelet Clumping:
Platelets Platelet Clumping:
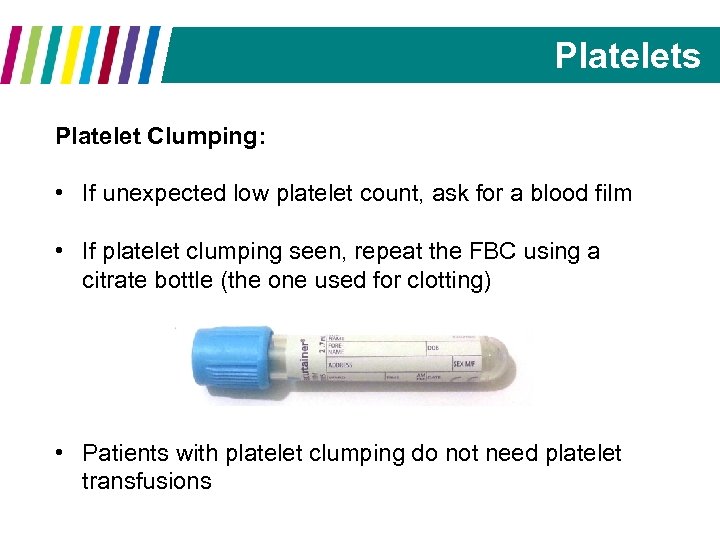 Platelets Platelet Clumping: • If unexpected low platelet count, ask for a blood film • If platelet clumping seen, repeat the FBC using a citrate bottle (the one used for clotting) • Patients with platelet clumping do not need platelet transfusions
Platelets Platelet Clumping: • If unexpected low platelet count, ask for a blood film • If platelet clumping seen, repeat the FBC using a citrate bottle (the one used for clotting) • Patients with platelet clumping do not need platelet transfusions
 Warfarin Reversal Question 8
Warfarin Reversal Question 8
 Question 8: Fresh Frozen Plasma (FFP) is the optimal treatment available to treat life threatening bleeding in patients on warfarin True or false?
Question 8: Fresh Frozen Plasma (FFP) is the optimal treatment available to treat life threatening bleeding in patients on warfarin True or false?
 Question 8: Fresh Frozen Plasma (FFP) is the optimal treatment available to treat life threatening bleeding in patients on warfarin True or false?
Question 8: Fresh Frozen Plasma (FFP) is the optimal treatment available to treat life threatening bleeding in patients on warfarin True or false?
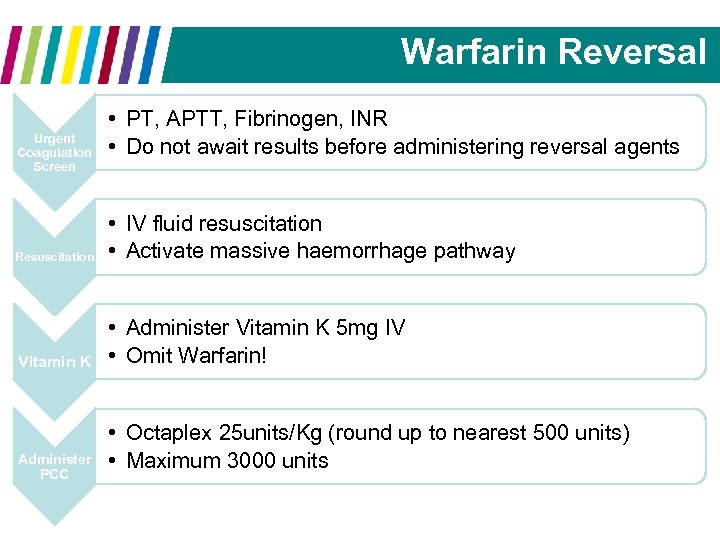 Warfarin Reversal Urgent Coagulation Screen • PT, APTT, Fibrinogen, INR • Do not await results before administering reversal agents Resuscitation • IV fluid resuscitation • Activate massive haemorrhage pathway Vitamin K • Administer Vitamin K 5 mg IV • Omit Warfarin! Administer PCC • Octaplex 25 units/Kg (round up to nearest 500 units) • Maximum 3000 units
Warfarin Reversal Urgent Coagulation Screen • PT, APTT, Fibrinogen, INR • Do not await results before administering reversal agents Resuscitation • IV fluid resuscitation • Activate massive haemorrhage pathway Vitamin K • Administer Vitamin K 5 mg IV • Omit Warfarin! Administer PCC • Octaplex 25 units/Kg (round up to nearest 500 units) • Maximum 3000 units
 Patients who refuse blood products Question 9
Patients who refuse blood products Question 9
 Question 9: Jehovah’s Witnesses do not accept red blood cell transfusions but on the whole are happy to accept platelets or plasma True or false?
Question 9: Jehovah’s Witnesses do not accept red blood cell transfusions but on the whole are happy to accept platelets or plasma True or false?
 Question 9: Jehovah’s Witnesses do not accept red blood cell transfusions but on the whole are happy to accept platelets or plasma True or false?
Question 9: Jehovah’s Witnesses do not accept red blood cell transfusions but on the whole are happy to accept platelets or plasma True or false?
 Patients who refuse blood Patients can refuse blood products for personal reasons not only religious regions Assess capacity to make decision Spend time exploring the patient’s reasoning • Ideally the patient should be alone, away from influence of family/friends • Accompany with nurse specialist
Patients who refuse blood Patients can refuse blood products for personal reasons not only religious regions Assess capacity to make decision Spend time exploring the patient’s reasoning • Ideally the patient should be alone, away from influence of family/friends • Accompany with nurse specialist
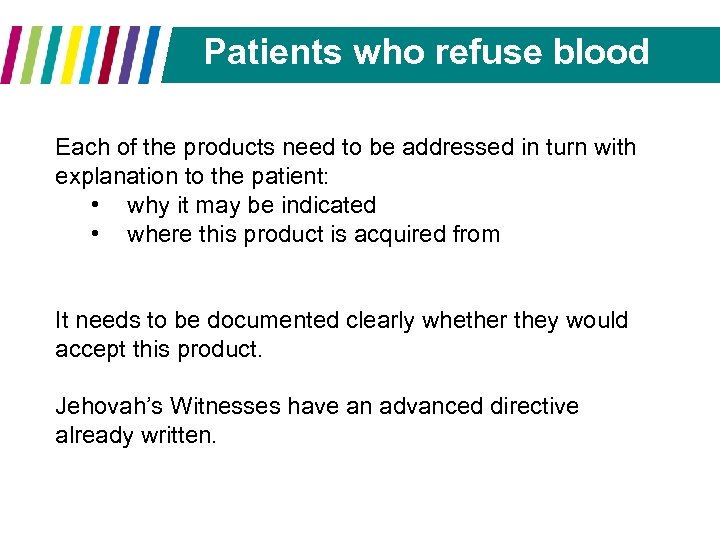 Patients who refuse blood Each of the products need to be addressed in turn with explanation to the patient: • why it may be indicated • where this product is acquired from It needs to be documented clearly whether they would accept this product. Jehovah’s Witnesses have an advanced directive already written.
Patients who refuse blood Each of the products need to be addressed in turn with explanation to the patient: • why it may be indicated • where this product is acquired from It needs to be documented clearly whether they would accept this product. Jehovah’s Witnesses have an advanced directive already written.
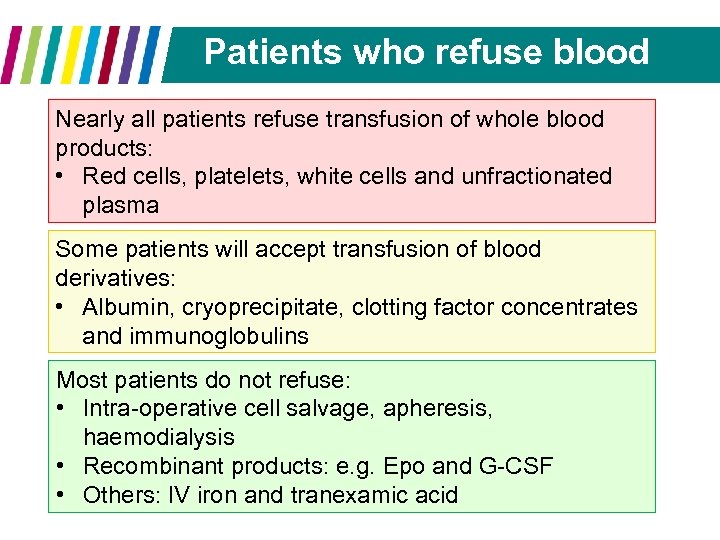 Patients who refuse blood Nearly all patients refuse transfusion of whole blood products: • Red cells, platelets, white cells and unfractionated plasma Some patients will accept transfusion of blood derivatives: • Albumin, cryoprecipitate, clotting factor concentrates and immunoglobulins Most patients do not refuse: • Intra-operative cell salvage, apheresis, haemodialysis • Recombinant products: e. g. Epo and G-CSF • Others: IV iron and tranexamic acid
Patients who refuse blood Nearly all patients refuse transfusion of whole blood products: • Red cells, platelets, white cells and unfractionated plasma Some patients will accept transfusion of blood derivatives: • Albumin, cryoprecipitate, clotting factor concentrates and immunoglobulins Most patients do not refuse: • Intra-operative cell salvage, apheresis, haemodialysis • Recombinant products: e. g. Epo and G-CSF • Others: IV iron and tranexamic acid
 Summary Transfusion of blood products can save lives, before you prescribe, ask yourself: • Does this patient need blood product support? • Are there alternatives? • Is it the correct blood product? • Is it the correct amount? • Think of the reasons behind the abnormality, how can this be investigated and managed?
Summary Transfusion of blood products can save lives, before you prescribe, ask yourself: • Does this patient need blood product support? • Are there alternatives? • Is it the correct blood product? • Is it the correct amount? • Think of the reasons behind the abnormality, how can this be investigated and managed?
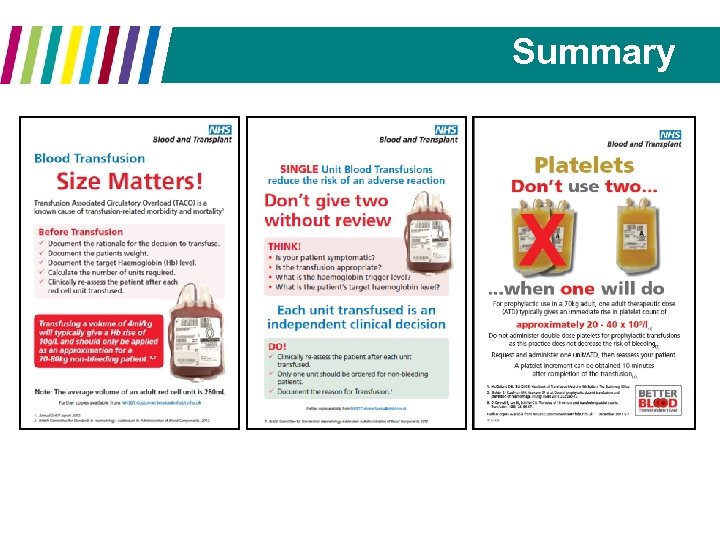 Summary
Summary
 Thank you for listening Any Questions? If you would like any further information, suggest future transfusion and blood teaching sessions or help us with future blood management projects, email me on: dawn. swan@cmft. nhs. uk
Thank you for listening Any Questions? If you would like any further information, suggest future transfusion and blood teaching sessions or help us with future blood management projects, email me on: dawn. swan@cmft. nhs. uk


