01f6f205501acd2525344e15b8ee90cf.ppt
- Количество слайдов: 27
Transforming community services: the Productive series Helen Bevan
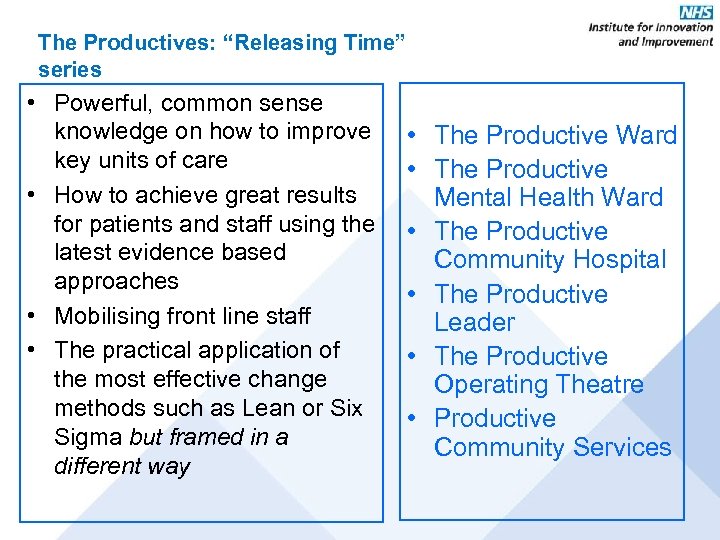
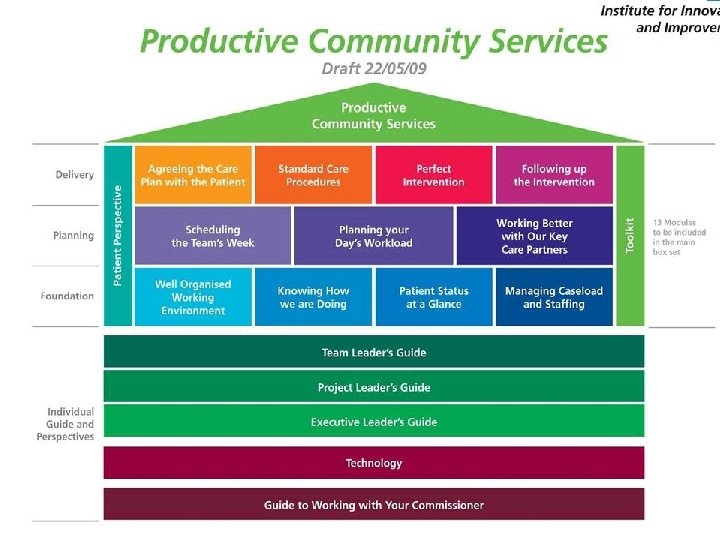
The Productives: “Releasing Time” series • Powerful, common sense knowledge on how to improve key units of care • How to achieve great results for patients and staff using the latest evidence based approaches • Mobilising front line staff • The practical application of the most effective change methods such as Lean or Six Sigma but framed in a different way • The Productive Ward • The Productive Mental Health Ward • The Productive Community Hospital • The Productive Leader • The Productive Operating Theatre • Productive Community Services
What we are learning from Releasing time to care How much energy can be unleashed by encouraging front line teams to question how they work and providing simple tools and skills to do this
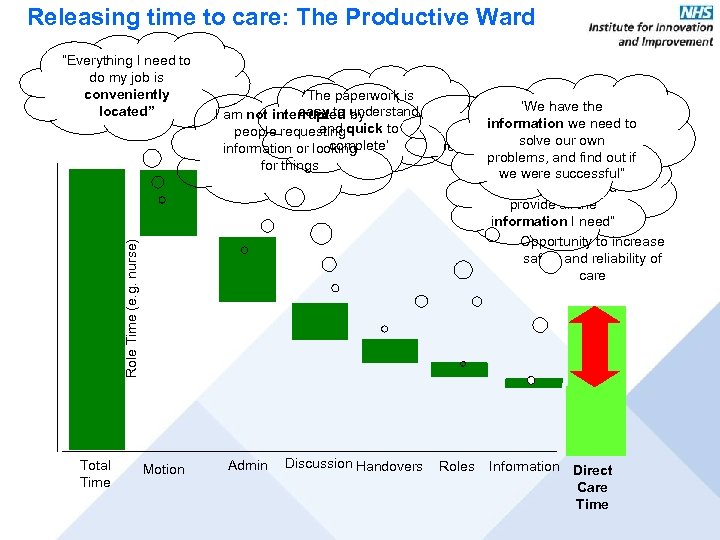
Releasing time to care: The Productive Ward ‘The paperwork is easy to understand I am not interrupted by and quick to people requesting complete’ information or looking for things Role Time (e. g. nurse) “Everything I need to do my job is conveniently located” Total Time Motion Admin Discussion Handovers ‘We have the ‘It is clear to information everyone who is we need to solve our own responsible for what” problems, and find out if ‘’Handovers are we were successful” concise, timely and provide all the information I need” Opportunity to increase safety and reliability of care Roles Information Direct Care Time
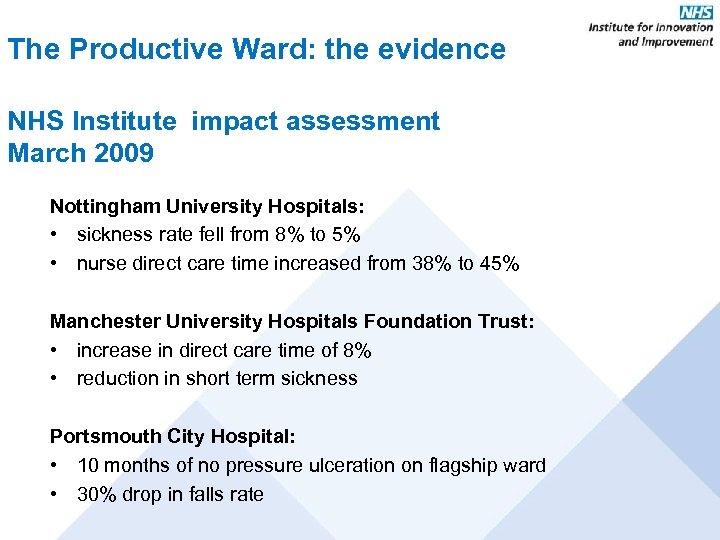
The Productive Ward: the evidence NHS Institute impact assessment March 2009 Nottingham University Hospitals: • sickness rate fell from 8% to 5% • nurse direct care time increased from 38% to 45% Manchester University Hospitals Foundation Trust: • increase in direct care time of 8% • reduction in short term sickness Portsmouth City Hospital: • 10 months of no pressure ulceration on flagship ward • 30% drop in falls rate
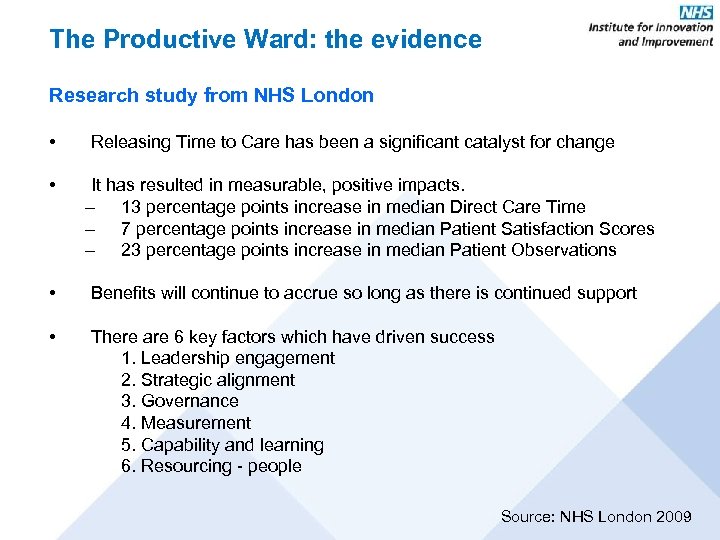
The Productive Ward: the evidence Research study from NHS London • • Releasing Time to Care has been a significant catalyst for change It has resulted in measurable, positive impacts. – 13 percentage points increase in median Direct Care Time – 7 percentage points increase in median Patient Satisfaction Scores – 23 percentage points increase in median Patient Observations • Benefits will continue to accrue so long as there is continued support • There are 6 key factors which have driven success 1. Leadership engagement 2. Strategic alignment 3. Governance 4. Measurement 5. Capability and learning 6. Resourcing - people Source: NHS London 2009
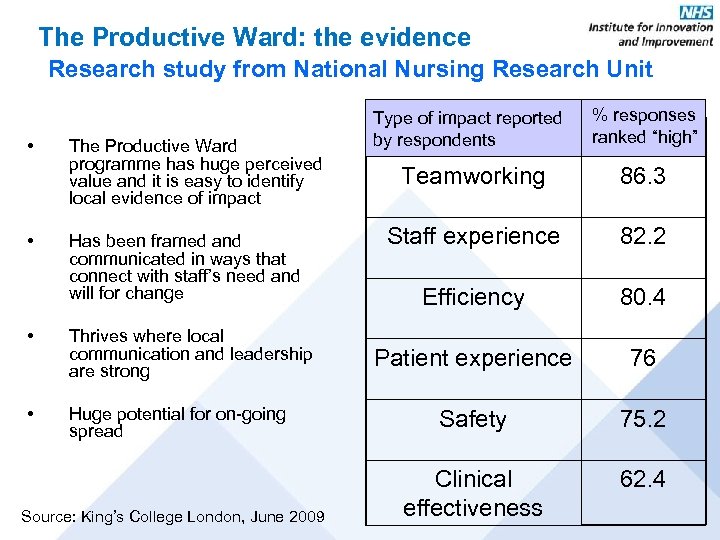
The Productive Ward: the evidence Research study from National Nursing Research Unit • • The Productive Ward programme has huge perceived value and it is easy to identify local evidence of impact Has been framed and communicated in ways that connect with staff’s need and will for change • Thrives where local communication and leadership are strong • Huge potential for on-going spread Source: King’s College London, June 2009 Type of impact reported by respondents % responses ranked “high” Teamworking 86. 3 Staff experience 82. 2 Efficiency 80. 4 Patient experience 76 Safety 75. 2 Clinical effectiveness 62. 4
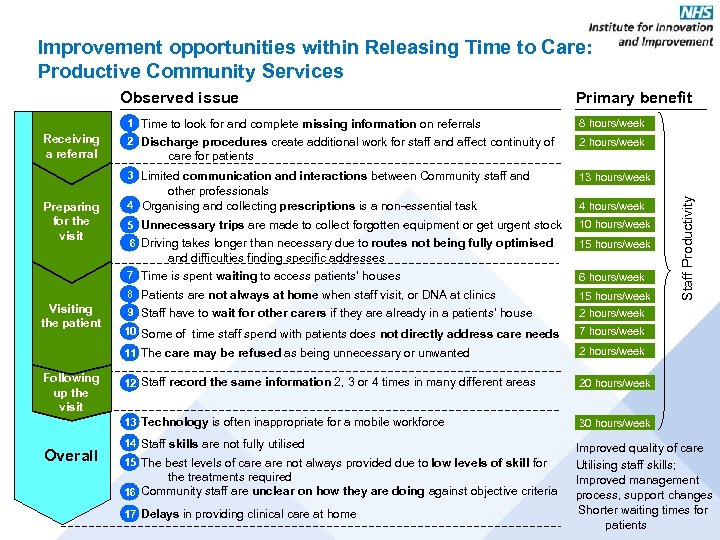
Improvement opportunities within Releasing Time to Care: Productive Community Services Observed issue Primary benefit 1 Time to look for and complete missing information on referrals 2 Discharge procedures create additional work for staff and affect continuity of 2 hours/week care for patients 3 Limited communication and interactions between Community staff and Preparing for the visit 13 hours/week other professionals 4 Organising and collecting prescriptions is a non-essential task 4 hours/week 5 Unnecessary trips are made to collect forgotten equipment or get urgent stock 10 hours/week 6 Driving takes longer than necessary due to routes not being fully optimised 15 hours/week and difficulties finding specific addresses 7 Time is spent waiting to access patients’ houses 8 Patients are not always at home when staff visit, or DNA at clinics Overall 9 Staff have to wait for other carers if they are already in a patients’ house 2 hours/week 10 Some of time staff spend with patients does not directly address care needs 7 hours/week 2 hours/week 12 Staff record the same information 2, 3 or 4 times in many different areas 20 hours/week 13 Technology is often inappropriate for a mobile workforce Following up the visit 15 hours/week 11 The care may be refused as being unnecessary or unwanted Visiting the patient 6 hours/week Staff Productivity Receiving a referral 8 hours/week 30 hours/week 14 Staff skills are not fully utilised 15 The best levels of care not always provided due to low levels of skill for the treatments required 16 Community staff are unclear on how they are doing against objective criteria 17 Delays in providing clinical care at home Improved quality of care Utilising staff skills; Improved management process, support changes Shorter waiting times for patients
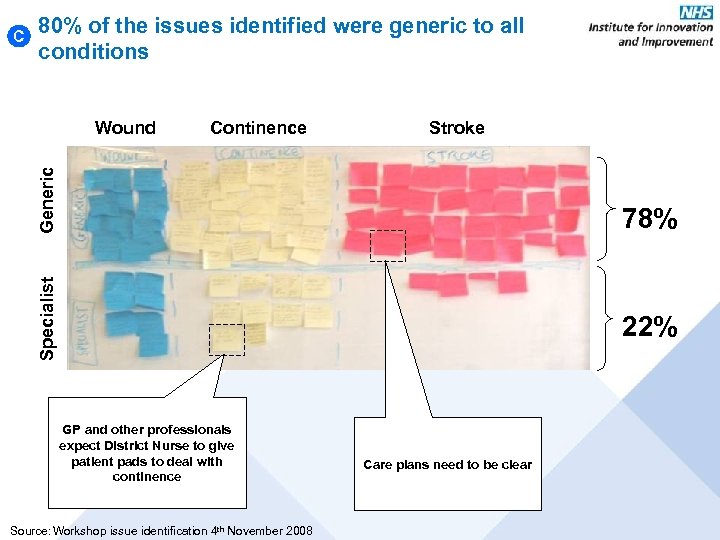
C 80% of the issues identified were generic to all conditions Continence Stroke Generic Wound Specialist 78% 22% GP and other professionals expect District Nurse to give patient pads to deal with continence Source: Workshop issue identification 4 th November 2008 Care plans need to be clear
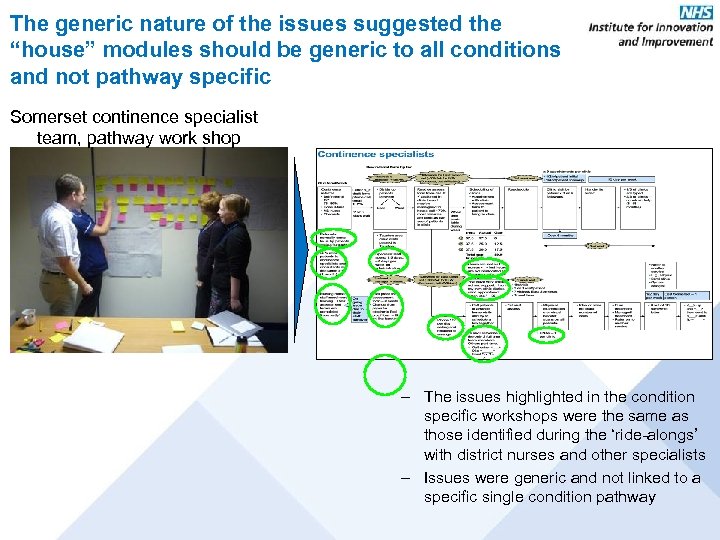
The generic nature of the issues suggested the “house” modules should be generic to all conditions and not pathway specific Somerset continence specialist team, pathway work shop – The issues highlighted in the condition specific workshops were the same as those identified during the ‘ride-alongs’ with district nurses and other specialists – Issues were generic and not linked to a specific single condition pathway
Development so far Focussed on field work services Concentrated on the ‘how to’ Developed tools to help staff Built and tested by staff in the community
Productive Community Services will… Increase patient-facing contact time, Reduce inefficient work practices, Improve the quality and safety of care. Re-vitalise the workforce Put staff at the forefront of redesigning their own services
Our plans for launch… Autumn 2009 – Foundation Modules Spring 2010 – Planning and Delivery Modules
Well Organised Working Environment. . . …helps front line teams to analyse their current activities and to develop and test more effective working systems.
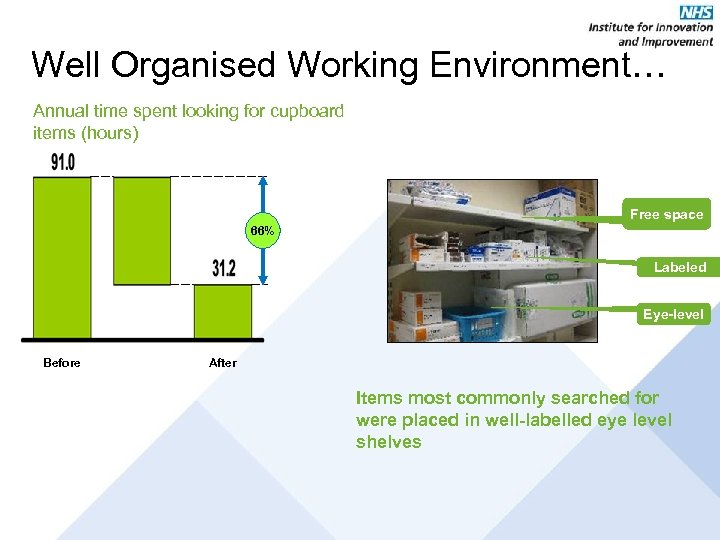
Well Organised Working Environment… Annual time spent looking for cupboard items (hours) Free space 66% Labeled Eye-level Before After Items most commonly searched for were placed in well-labelled eye level shelves
Patient Status at a glance. . . …enables multi-professional and multi- location teams to understand the status of every patient, using the most up-to-date “visual management” techniques.
Patient Status at a Glance. . …is a good idea! I have more awareness of what’s going on. …acts as a guide to discuss patients while prompting us to follow things up. …breaks down a problem and has given us purpose and power. . . say District Nurses
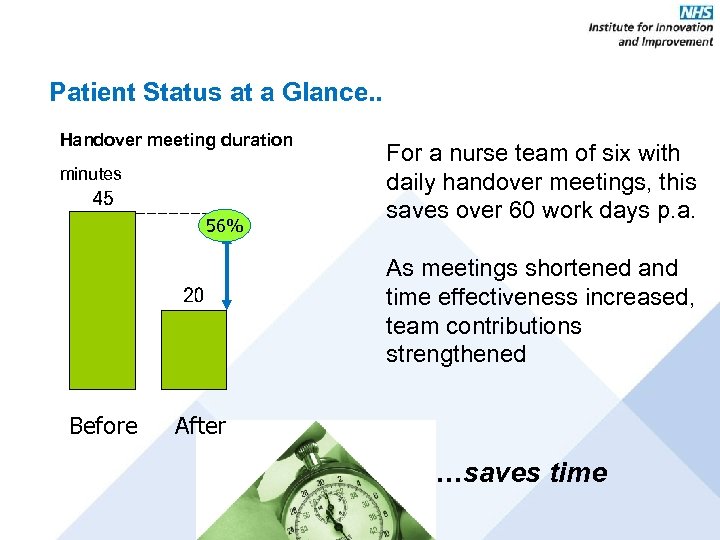
Patient Status at a Glance. . Handover meeting duration minutes 56% For a nurse team of six with daily handover meetings, this saves over 60 work days p. a. As meetings shortened and time effectiveness increased, team contributions strengthened Before After …saves time
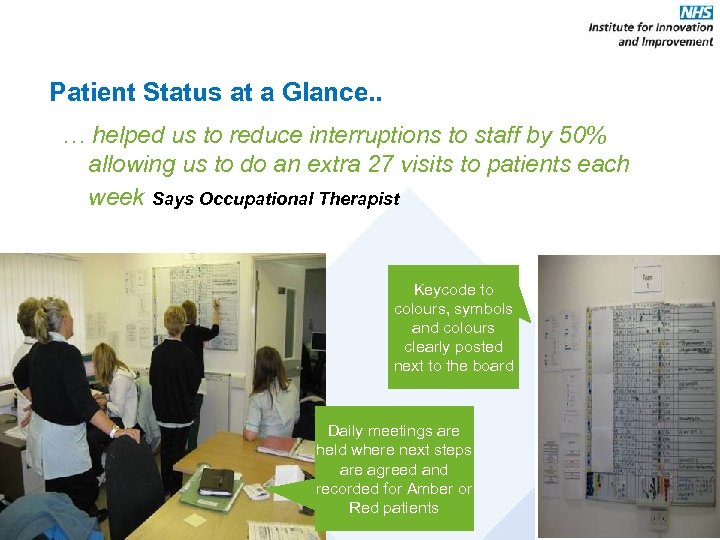
Patient Status at a Glance. . … helped us to reduce interruptions to staff by 50% allowing us to do an extra 27 visits to patients each week Says Occupational Therapist Keycode to colours, symbols and colours clearly posted next to the board Daily meetings are held where next steps are agreed and recorded for Amber or Red patients
Managing Caseload and Staffing. . . …gets the most out of the people and avoids bottlenecks by managing caseloads better and planning staff activity more effectively.
Managing Caseload and Staffing… We’re surprised by how much time is spent on travel/admin/meetings. Only 35% spent with patients. Our current understanding of demand capacity is inadequate to manage our service well. Evidence-based decision making is possible with the tools from this module. The key to balancing demand capacity is to smooth out staff availability and/or demand for the service. say frontline staff … increases patient-facing time
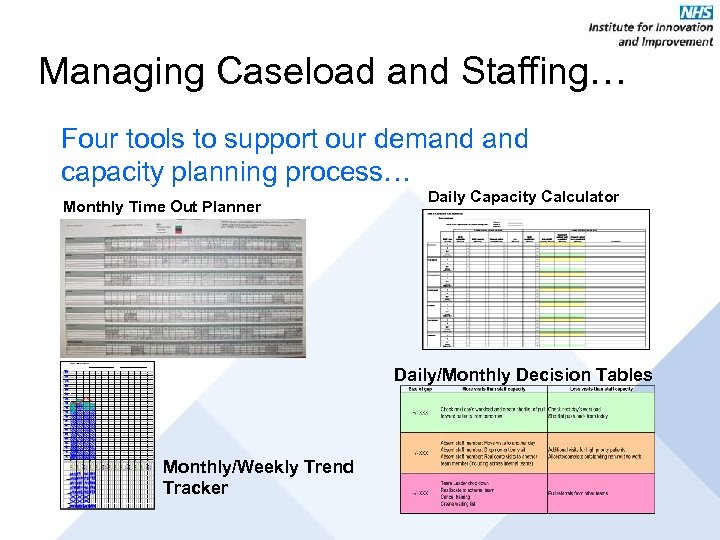
Managing Caseload and Staffing… Four tools to support our demand capacity planning process… Monthly Time Out Planner Daily Capacity Calculator Daily/Monthly Decision Tables Monthly/Weekly Trend Tracker
Knowing How We are Doing. . . …enables local teams to understand team performance and set team improvement goals in areas such as safety, quality, productivity, patient experience and staff experience.
Knowing How We are Doing. . . …has helped us to move us from a disjointed, demoralised, self doubting team, to one which is excited/motivated by the goals and opportunities we have to impact change within our PCT … says Nurse Team Leader
Our testing and development to date suggests that PCS could fundamentally change the way you deliver healthcare • Fits strategy with service design and reshapes the channels for delivering care • Aligns teams in traditional silos on a single agenda like never before • Potentially doubles the amount of patient care time delivered by the same staff • Increases management skills such as planning and performance management • Lifts the confidence and morale of the workforce • Transforms the culture to fact-based and data driven, able to take improvement actions • Explores the possibility of real time data tracking for staff • Provides an opportunity to explore electronic medial records that allow better access and mobility

For more information http: //www. institute. nhs. uk
01f6f205501acd2525344e15b8ee90cf.ppt