56cc6c259e4b9c6ea26cb565b403b85b.ppt
- Количество слайдов: 42
Training on Outbreak Management for Kala-azar in Bangladesh Kala-azar Situation in Bangladesh Presenter: Dr. Mohammad Sohel Shomik Deputy Project Coordinator icddr, b
Leishmaniasis A group of diseases, caused by the Leishmania parasites and transmitted by the sandfly
Types of Leishmaniasis Ø Visceral Leishmaniasis (VL)/ Kala-azar It is characterized by irregular bouts of fever, weight loss, enlargement of the spleen and liver, and anaemia. It is fatal if left untreated. Ø Cutaneous/ mucocutaneous Leishmaniasis It is the most common form of leishmaniasis and causes skin lesions, mainly ulcers, on exposed parts of the body, leaving life-long scars and serious disability.
Post Kala-azar Dermal Leishmaniasis (PKDL) PKDL is a sequel of visceral leishmaniasis that appears as macular, papular or nodular rash usually on face, upper arms, trunks and other parts of the body. People with PKDL are considered to be a potential source of kala-azar infection.
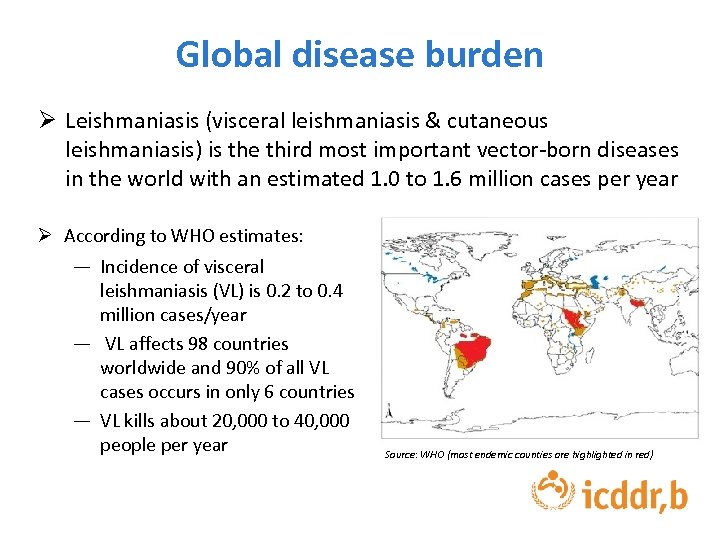
Global disease burden Ø Leishmaniasis (visceral leishmaniasis & cutaneous leishmaniasis) is the third most important vector-born diseases in the world with an estimated 1. 0 to 1. 6 million cases per year Ø According to WHO estimates: ― Incidence of visceral leishmaniasis (VL) is 0. 2 to 0. 4 million cases/year ― VL affects 98 countries worldwide and 90% of all VL cases occurs in only 6 countries ― VL kills about 20, 000 to 40, 000 people per year Source: WHO (most endemic counties are highlighted in red)
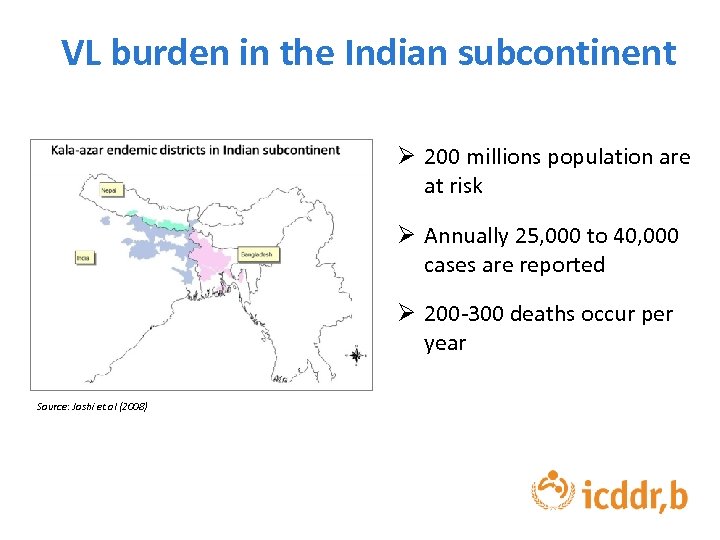
VL burden in the Indian subcontinent Ø 200 millions population are at risk Ø Annually 25, 000 to 40, 000 cases are reported Ø 200 -300 deaths occur per year Source: Joshi et. al (2008)
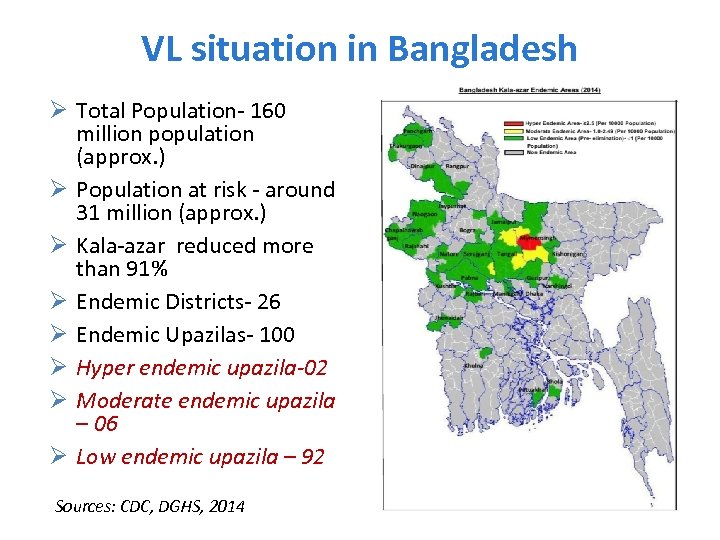
VL situation in Bangladesh Ø Total Population- 160 million population (approx. ) Ø Population at risk - around 31 million (approx. ) Ø Kala-azar reduced more than 91% Ø Endemic Districts- 26 Ø Endemic Upazilas- 100 Ø Hyper endemic upazila-02 Ø Moderate endemic upazila – 06 Ø Low endemic upazila – 92 Sources: CDC, DGHS, 2014
Unique epidemiological features of VL in the Indian subcontinent Ø Human are the only reservoir/host Ø Female Phlebotomas argentipes sand fly is the only vector Ø Leishmania donovani is the only species responsible for VL Ø The disease is highly clustered Visceral leishmaniasis VL patient/host Sand fly Vector Case fatality rate is 100% if VL is not treated properly
VL Elimination Program in the Indian subcontinent Ø The Government of Bangladesh, India and Nepal committed to eliminate VL from the Indian sub-continent by 2015. Ø The elimination target is to reduce VL case less than one per 10, 000 people at sub-district level in Bangladesh • Recently the elimination target time is extended up to 2017 and two new countries (Bhutan and Thailand) joined in this initiative
Strategy of National Kala-azar Elimination Program in Bangladesh 1. 2. 3. 4. Early diagnosis and complete treatment Integrated vector management (IVM) Effective disease surveillance Social mobilization and building partnerships 5. Operational research
Strategy -1: Early diagnosis and complete treatment
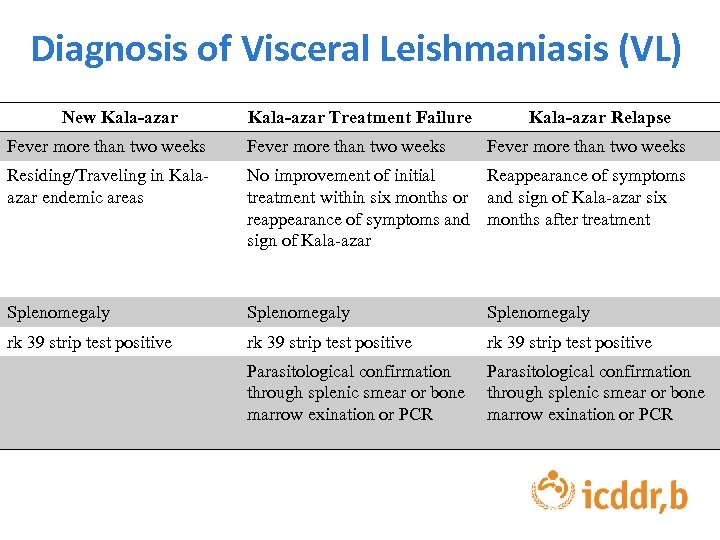
Diagnosis of Visceral Leishmaniasis (VL) New Kala-azar Treatment Failure Kala-azar Relapse Fever more than two weeks Residing/Traveling in Kalaazar endemic areas No improvement of initial Reappearance of symptoms treatment within six months or and sign of Kala-azar six reappearance of symptoms and months after treatment sign of Kala-azar Splenomegaly rk 39 strip test positive Parasitological confirmation through splenic smear or bone marrow exination or PCR
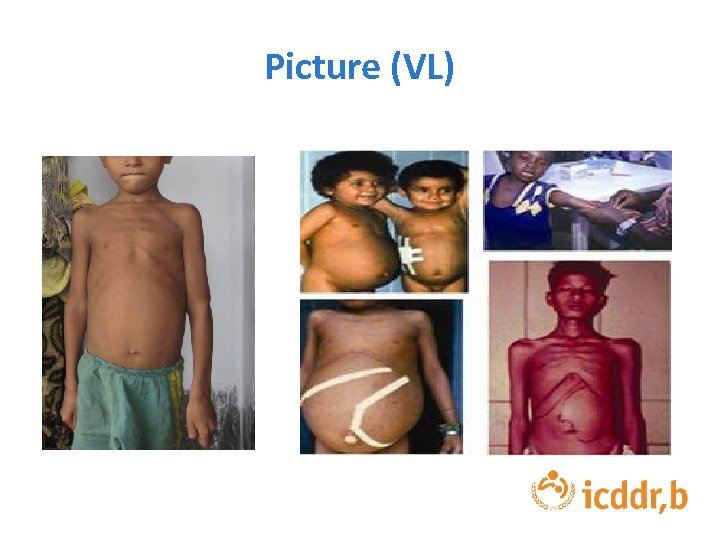
Picture (VL)
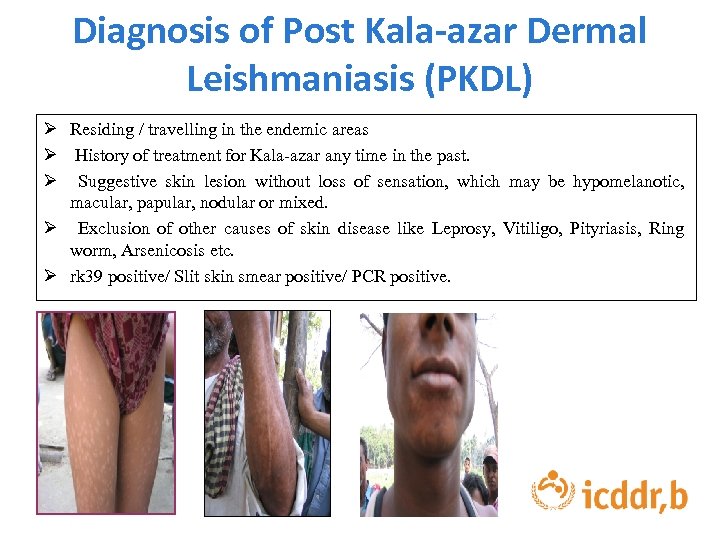
Diagnosis of Post Kala-azar Dermal Leishmaniasis (PKDL) Ø Residing / travelling in the endemic areas Ø History of treatment for Kala-azar any time in the past. Ø Suggestive skin lesion without loss of sensation, which may be hypomelanotic, macular, papular, nodular or mixed. Ø Exclusion of other causes of skin disease like Leprosy, Vitiligo, Pityriasis, Ring worm, Arsenicosis etc. Ø rk 39 positive/ Slit skin smear positive/ PCR positive.
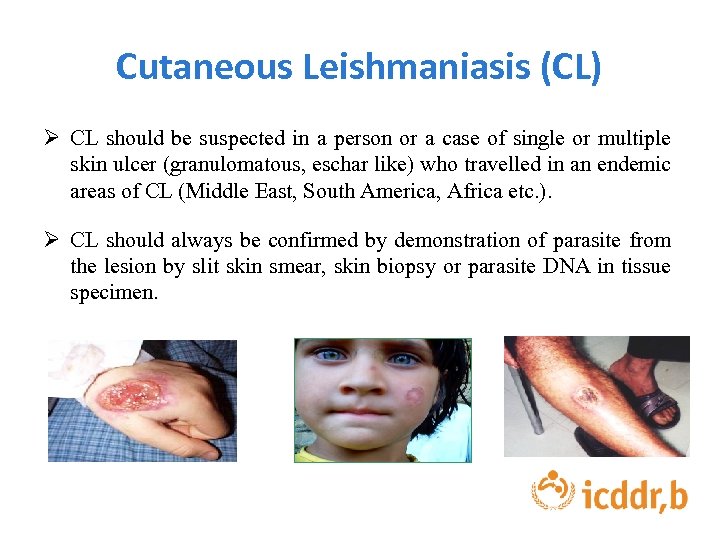
Cutaneous Leishmaniasis (CL) Ø CL should be suspected in a person or a case of single or multiple skin ulcer (granulomatous, eschar like) who travelled in an endemic areas of CL (Middle East, South America, Africa etc. ). Ø CL should always be confirmed by demonstration of parasite from the lesion by slit skin smear, skin biopsy or parasite DNA in tissue specimen.
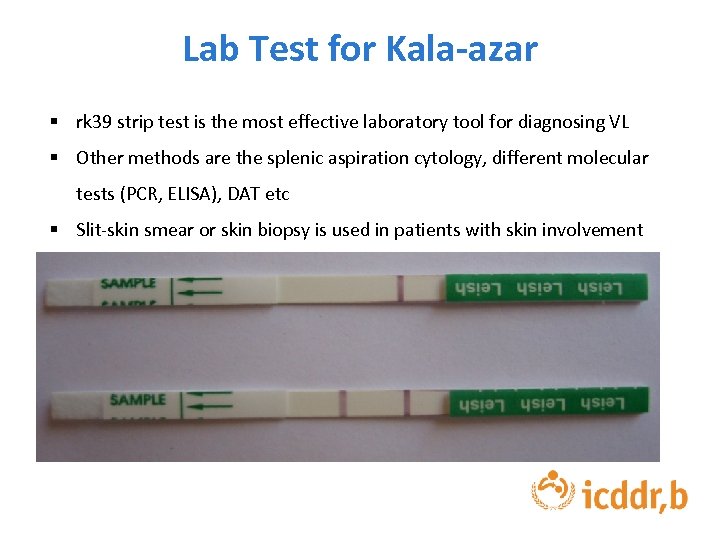
Lab Test for Kala-azar § rk 39 strip test is the most effective laboratory tool for diagnosing VL § Other methods are the splenic aspiration cytology, different molecular tests (PCR, ELISA), DAT etc § Slit-skin smear or skin biopsy is used in patients with skin involvement
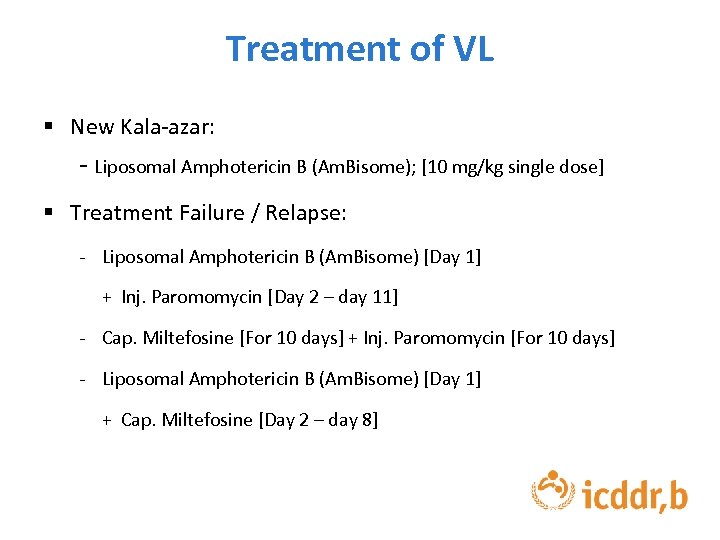
Treatment of VL § New Kala-azar: - Liposomal Amphotericin B (Am. Bisome); [10 mg/kg single dose] § Treatment Failure / Relapse: - Liposomal Amphotericin B (Am. Bisome) [Day 1] + Inj. Paromomycin [Day 2 – day 11] - Cap. Miltefosine [For 10 days] + Inj. Paromomycin [For 10 days] - Liposomal Amphotericin B (Am. Bisome) [Day 1] + Cap. Miltefosine [Day 2 – day 8]
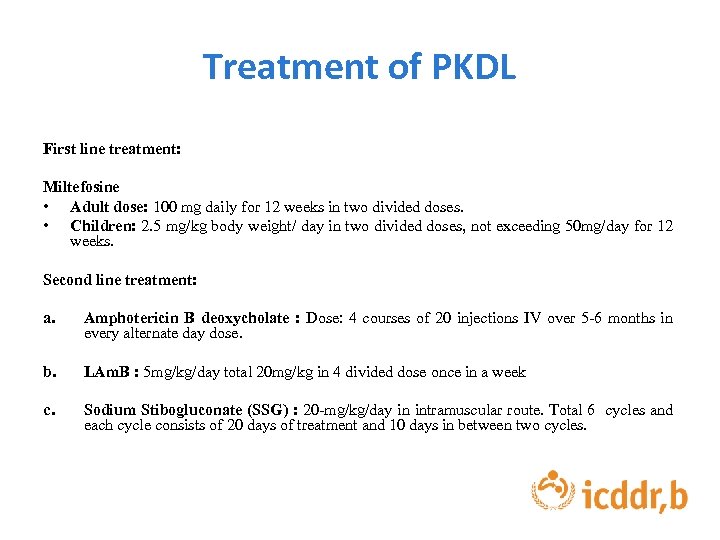
Treatment of PKDL First line treatment: Miltefosine • Adult dose: 100 mg daily for 12 weeks in two divided doses. • Children: 2. 5 mg/kg body weight/ day in two divided doses, not exceeding 50 mg/day for 12 weeks. Second line treatment: a. Amphotericin B deoxycholate : Dose: 4 courses of 20 injections IV over 5 -6 months in every alternate day dose. b. LAm. B : 5 mg/kg/day total 20 mg/kg in 4 divided dose once in a week c. Sodium Stibogluconate (SSG) : 20 -mg/kg/day in intramuscular route. Total 6 cycles and each cycle consists of 20 days of treatment and 10 days in between two cycles.

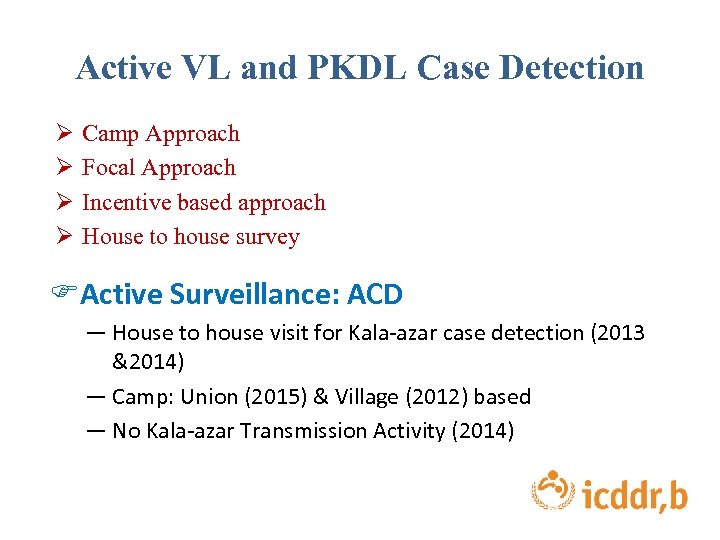
Active VL and PKDL Case Detection Ø Ø Camp Approach Focal Approach Incentive based approach House to house survey FActive Surveillance: ACD ― House to house visit for Kala-azar case detection (2013 &2014) ― Camp: Union (2015) & Village (2012) based ― No Kala-azar Transmission Activity (2014)

Strategy-2: Integrated vector management (IVM)
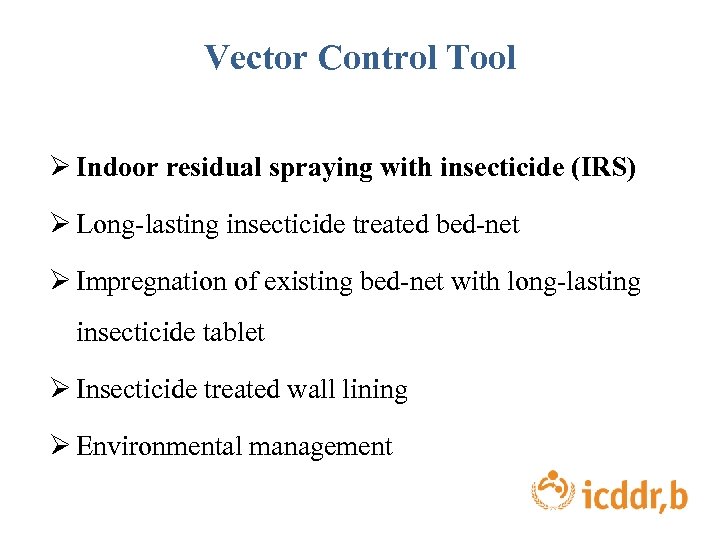
Vector Control Tool Ø Indoor residual spraying with insecticide (IRS) Ø Long-lasting insecticide treated bed-net Ø Impregnation of existing bed-net with long-lasting insecticide tablet Ø Insecticide treated wall lining Ø Environmental management

Integrated Vector Management (IVM) Indoor Residual Spraying Larvicide Spraying
WALL LINING Bed-net Impregnation
Risk Factor for VL § Socioeconomic condition § Malnutrition § Population mobility § Environmental changes § Climate changes Source: WHO (http: //www. who. int/mediacentre/factsheets/fs 375/en/)
Strategy -3: Effective Disease Surveillance
Kala-azar Surveillance in Bangladesh Ø Kala-azar surveillance is a part of web-based national disease surveillance system centrally managed by Kalaazar Elimination Programme, Disease control Unit, DGHS. Ø Kala-azar elimination program-specific indicators is incorporated in the reporting format. Ø In order to strengthen Kala-azar surveillance, KA surveillance units is set up at upazila and district level. Ø KEP has access to surveillance data in real time
Kala-azar Surveillance in Bangladesh: A Modern Surveillance ü National Kala-azar Elimination Program is using both: 1. Passive Surveillance & 2. Active Surveillance
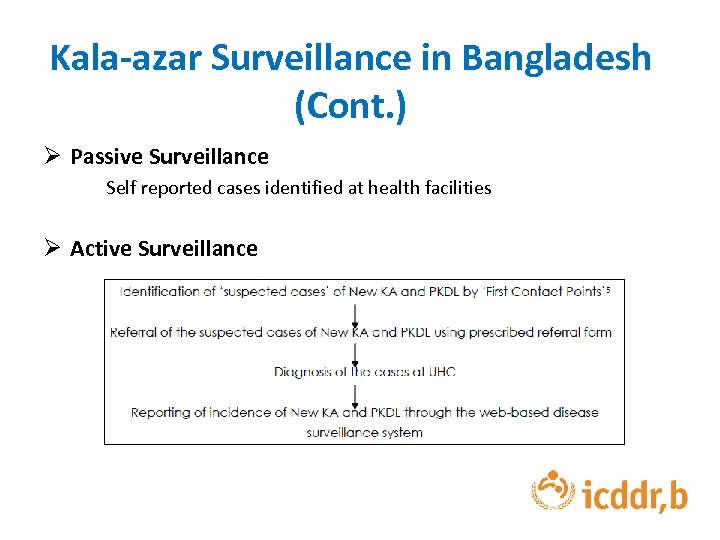
Kala-azar Surveillance in Bangladesh (Cont. ) Ø Passive Surveillance Self reported cases identified at health facilities Ø Active Surveillance
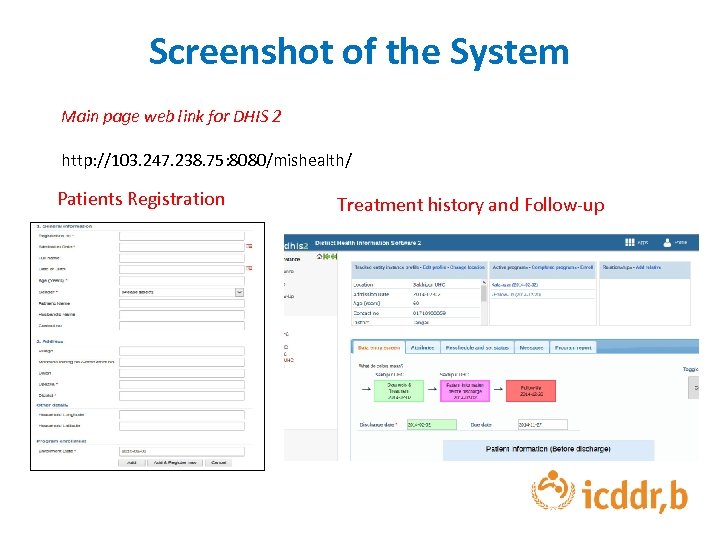
Screenshot of the System Main page web link for DHIS 2 http: //103. 247. 238. 75: 8080/mishealth/ Patients Registration Treatment history and Follow-up
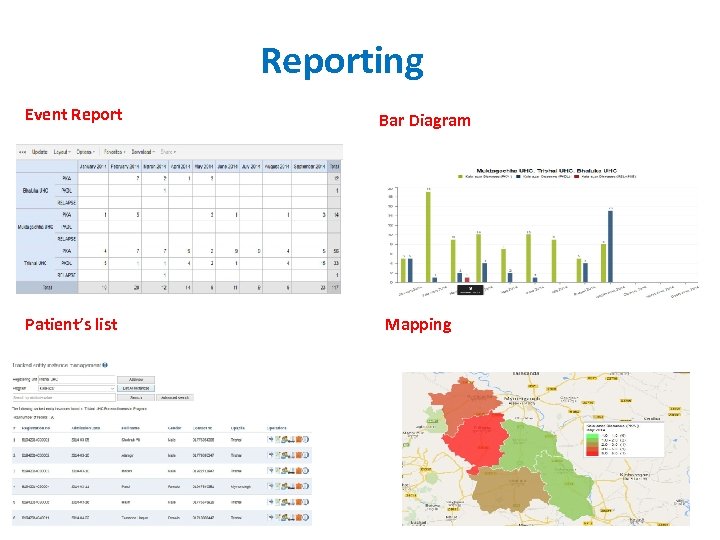
Reporting Event Report Patient’s list Bar Diagram Mapping

Strategy-4: Social mobilization and building partnerships

Social Mobilization and Partnership Folk song on Kala-azar sung at market places Folk song on Kala-azar sung at school premises Kala-azar Billboard

Some Newly Introduced IEC / BCC Materials by NKEP Poster Flipchart
Pen-Holder Sticker
Strategy -5: Operational research
Clinical and operational research Clinical trials with miltefosine , combination drug therapy, and feasibility studies for single-dose Am. Bisome at the sub-district level Trials have also been conducted with different vector control methods and studies for better diagnostic tools for VL and PKDL. Another major success of the program is the establishment of a Kala-azar research center at the Surja Kanta (SK) Hospital The research center at the SK Hospital is open to all researchers who are interested in conducting studies on VL and PKDL.
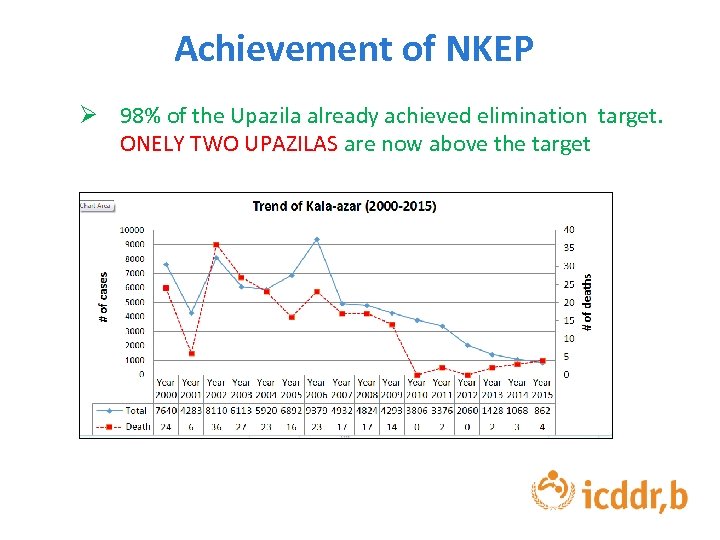
Achievement of NKEP Ø 98% of the Upazila already achieved elimination target. ONELY TWO UPAZILAS are now above the target
Challenges of Kala-azar Elimination Program § Establishing an effective surveillance system § Health seeking behavior § Effective community mobilization § Ignorance on PKDL § Drug resistance § Proper vector management § Cross border collaboration § Sporadic cases are reported from both non-endemic and from eliminated Upazilas
Information on Kala-azar available www. kalacorebd. com

Acknowledgement

THANK YOU
56cc6c259e4b9c6ea26cb565b403b85b.ppt