f9f28fe00db71d56d733b1ec74291bbb.ppt
- Количество слайдов: 42
 Toxicology WEEK 6
Toxicology WEEK 6
 Toxicants and Toxins Proper and prompt tx of poisonings, including stabilization and decontamination, is essential Toxicants- of biologic origin, manufactured chemicals, or naturally occurring chemicals Any substance that when introduced into or applied to the body can interfere with the life processes of cells of the organism. Toxin- noxious or poisonous substance that is formed or elaborated during the metabolism and growth of certain microorganisms and some higher plant and animal species
Toxicants and Toxins Proper and prompt tx of poisonings, including stabilization and decontamination, is essential Toxicants- of biologic origin, manufactured chemicals, or naturally occurring chemicals Any substance that when introduced into or applied to the body can interfere with the life processes of cells of the organism. Toxin- noxious or poisonous substance that is formed or elaborated during the metabolism and growth of certain microorganisms and some higher plant and animal species
 You as a technician Should be able to recognize what constitutes a toxicological emergency and what does not Be able to give basic first aid advice, and provide clear directions to the hospital Can prepare for arrival with necessary equipment and medication Investigate the toxicant Direct owner to contact the ASPCA poison control center (888 -426 -4435)
You as a technician Should be able to recognize what constitutes a toxicological emergency and what does not Be able to give basic first aid advice, and provide clear directions to the hospital Can prepare for arrival with necessary equipment and medication Investigate the toxicant Direct owner to contact the ASPCA poison control center (888 -426 -4435)
 Questions to ask when the owner calls What is the current clinical status of the animal What was the animal exposed to and through what route Has the owner taken any steps to treat the animal Age and weight of animal How much was ingested When was the exposure Male or female; if female, lactating or pregnant Any Hx of health problems On any current medication Had any recent Sx
Questions to ask when the owner calls What is the current clinical status of the animal What was the animal exposed to and through what route Has the owner taken any steps to treat the animal Age and weight of animal How much was ingested When was the exposure Male or female; if female, lactating or pregnant Any Hx of health problems On any current medication Had any recent Sx
 Assesment 1 st thing is assess animals condition Performed quickly and includes: examination of RR, CRT, MM color, HR, and temp Unconscious, in shock, seizuring, or cardiovasular or resp distress must be conducted simultaneously with stabilization measures Look for any evidence of hemorrhaging
Assesment 1 st thing is assess animals condition Performed quickly and includes: examination of RR, CRT, MM color, HR, and temp Unconscious, in shock, seizuring, or cardiovasular or resp distress must be conducted simultaneously with stabilization measures Look for any evidence of hemorrhaging
 Stabilization General rule: treat the patient not the poison Establish and maintain patient airway Cardiovascular system should be monitored Apply O 2 or artificial respirations if needed Place an indwelling IV catheter for administration of any necessary injections
Stabilization General rule: treat the patient not the poison Establish and maintain patient airway Cardiovascular system should be monitored Apply O 2 or artificial respirations if needed Place an indwelling IV catheter for administration of any necessary injections
 Decontamination Must know patients: Age Weight Previous medical Hx Treat appropriately
Decontamination Must know patients: Age Weight Previous medical Hx Treat appropriately
 External exposures Ocular irrigation Eyes flushed repeatedly with water or saline for a minimum of 20 -30 minutes and treat with lubricant ointment Corrosive agents considered an emergency Examination for corneal damage and monitor for excessive redness, lacrimation or pain Never use topical steroids with ocular scratches/ulcerations Bathing Dermal exposures Use mild liquid dishwashing detergent Rinse well Towel dry
External exposures Ocular irrigation Eyes flushed repeatedly with water or saline for a minimum of 20 -30 minutes and treat with lubricant ointment Corrosive agents considered an emergency Examination for corneal damage and monitor for excessive redness, lacrimation or pain Never use topical steroids with ocular scratches/ulcerations Bathing Dermal exposures Use mild liquid dishwashing detergent Rinse well Towel dry
 Oral ingestion Types of tx: Dilution Emesis Activated charcoal Cathartics Enemas Gastric lavage Supportive care
Oral ingestion Types of tx: Dilution Emesis Activated charcoal Cathartics Enemas Gastric lavage Supportive care
 Emesis Vomiting Patient’s species, time past ingestion, previous and current Hx, and type of poison can effect decision Best results within 2 -3 hours postexposure Contraindicated in: rodents, rabbits, birds, horses, and ruminants Contraindicated with previous Hx of heart abnormalities, epilepsy, or abdominal Sx, corrosive material Feeding small meal prior increases adequate emesis
Emesis Vomiting Patient’s species, time past ingestion, previous and current Hx, and type of poison can effect decision Best results within 2 -3 hours postexposure Contraindicated in: rodents, rabbits, birds, horses, and ruminants Contraindicated with previous Hx of heart abnormalities, epilepsy, or abdominal Sx, corrosive material Feeding small meal prior increases adequate emesis
 Agents 3% H 2 O 2: 1 teaspoon per 5 lbs Repeat if no vomiting within 15 -20 minutes H 2 O 2 must be fresh Do not exceed 3 tbsp Apomorphine: Preferred emetic Available in injectable or capsule Capsule admin in the conjuctiva
Agents 3% H 2 O 2: 1 teaspoon per 5 lbs Repeat if no vomiting within 15 -20 minutes H 2 O 2 must be fresh Do not exceed 3 tbsp Apomorphine: Preferred emetic Available in injectable or capsule Capsule admin in the conjuctiva
 Activated charcoal Absorbs a chemical or toxicant and facilitates its excretion via the feces Dose 1 -3 g/kg of body weight, repeated every 4 -8 hours at ½ the original dose Administered orally or through stomach tube Not used in animals that ingested caustic materials Very messy to administer
Activated charcoal Absorbs a chemical or toxicant and facilitates its excretion via the feces Dose 1 -3 g/kg of body weight, repeated every 4 -8 hours at ½ the original dose Administered orally or through stomach tube Not used in animals that ingested caustic materials Very messy to administer
 Cathartics Used to enhance elimination of activated charcoal and absorbed toxicant Contraindicated with patients with: Diarrhea Dehydration Enemas are a type of cathartic Helpful in elimination of toxicants from the lower GI tract Use warm plain water or warm soapy water Premixed solutions have potential for electrolyte and/or acid-base imbalance
Cathartics Used to enhance elimination of activated charcoal and absorbed toxicant Contraindicated with patients with: Diarrhea Dehydration Enemas are a type of cathartic Helpful in elimination of toxicants from the lower GI tract Use warm plain water or warm soapy water Premixed solutions have potential for electrolyte and/or acid-base imbalance
 Gastric Lavage Gently pumping out of the stomach contents Usually performed under general anesthesia Pumped repeatedly with body temp water until it comes out clear Enterogastric lavage: occasionally done after gastric lavage Leave stomach tube in place Perform an enema Distal end of enema tube is attached to a water faucet and body temp water is ran trough until it comes out of the stomach tube, repeat until clear Considered the “through and through” method
Gastric Lavage Gently pumping out of the stomach contents Usually performed under general anesthesia Pumped repeatedly with body temp water until it comes out clear Enterogastric lavage: occasionally done after gastric lavage Leave stomach tube in place Perform an enema Distal end of enema tube is attached to a water faucet and body temp water is ran trough until it comes out of the stomach tube, repeat until clear Considered the “through and through” method
 Supportive Care Tech plays critical role in routinely evaluating vital signs and parameters poss. Affected by toxicants Check hydration Blood samples Watch for overhydration Diuresis may be beneficial for exposures to toxicants that can cause kidney damage Nutrition can be key component in recovery Tech should educate owners on dangers of toxicants
Supportive Care Tech plays critical role in routinely evaluating vital signs and parameters poss. Affected by toxicants Check hydration Blood samples Watch for overhydration Diuresis may be beneficial for exposures to toxicants that can cause kidney damage Nutrition can be key component in recovery Tech should educate owners on dangers of toxicants
 Topical Insecticides Some common topical insecticides can produce topical allergic reactions. Imidacloprid (_____) In Fipronil (_____) Selamectin (_____) Methoprene (Hartz) In combination with permethrin for ticks- K 9 Advantix combination with Fipronil is Frontline Plus Pyrethroids Most commonly see toxicity due to “piggyback” use causing overdose. May see neurologic signs. Tx by bathing
Topical Insecticides Some common topical insecticides can produce topical allergic reactions. Imidacloprid (_____) In Fipronil (_____) Selamectin (_____) Methoprene (Hartz) In combination with permethrin for ticks- K 9 Advantix combination with Fipronil is Frontline Plus Pyrethroids Most commonly see toxicity due to “piggyback” use causing overdose. May see neurologic signs. Tx by bathing
 Topical Insecticides Permethrin toxicity A synthetic pyrethroid compound with insecticidal properties Used in the control of fleas and ticks Clinical signs of toxicity Generalized tremors, muscle fasciculations, and seizures Most common in cats due to the misapplication of products intended for dogs
Topical Insecticides Permethrin toxicity A synthetic pyrethroid compound with insecticidal properties Used in the control of fleas and ticks Clinical signs of toxicity Generalized tremors, muscle fasciculations, and seizures Most common in cats due to the misapplication of products intended for dogs
 Topical Insecticides Permethrin toxicity diagnosis History of exposure and subsequent development of clinical signs Permethrin toxicity treatment Decontamination of the skin via bathing Bathing symptomatic cats may be difficult, but is important in preventing further uptake of the toxin Muscle relaxants, anti-convulsants and sedative drugs can be useful in the symptomatic treatment of seizures, tremors, and muscle fasciculation
Topical Insecticides Permethrin toxicity diagnosis History of exposure and subsequent development of clinical signs Permethrin toxicity treatment Decontamination of the skin via bathing Bathing symptomatic cats may be difficult, but is important in preventing further uptake of the toxin Muscle relaxants, anti-convulsants and sedative drugs can be useful in the symptomatic treatment of seizures, tremors, and muscle fasciculation
 Topical Insecticides Permethrin toxicity fluid therapy Indicated to correct dehydration that develops from hypersalivation and protracted muscle activity Fluid therapy and bathing are helpful in managing potential hyperthermia Overall prognosis for cats that receive prompt treatment is good
Topical Insecticides Permethrin toxicity fluid therapy Indicated to correct dehydration that develops from hypersalivation and protracted muscle activity Fluid therapy and bathing are helpful in managing potential hyperthermia Overall prognosis for cats that receive prompt treatment is good
 Household cleaning agents Acids Alkali Bleaches Detergents
Household cleaning agents Acids Alkali Bleaches Detergents
 Misc Household items Ant baits Silica gel packets Toilet water with tank cleaning drop-in tablets Glow necklaces Liquid potpourri Batteries Cigarettes Pennies Mothballs Moldy food Ice and snow melts
Misc Household items Ant baits Silica gel packets Toilet water with tank cleaning drop-in tablets Glow necklaces Liquid potpourri Batteries Cigarettes Pennies Mothballs Moldy food Ice and snow melts
 Dangerous Foods Moldy food Chocolate- dark more toxic than milk, unsweetened baking more toxic than dark Onions- causes damage to RBCs causing hemolysis Uncooked more toxic than cooked. Onion powder can also be toxic Macadamia Nuts- dogs Rising bread dough Grapes and raisins- kidney failure in dogs Tobacco Xylitol- most commonly found in gum and pop Causes hypoglycemia
Dangerous Foods Moldy food Chocolate- dark more toxic than milk, unsweetened baking more toxic than dark Onions- causes damage to RBCs causing hemolysis Uncooked more toxic than cooked. Onion powder can also be toxic Macadamia Nuts- dogs Rising bread dough Grapes and raisins- kidney failure in dogs Tobacco Xylitol- most commonly found in gum and pop Causes hypoglycemia
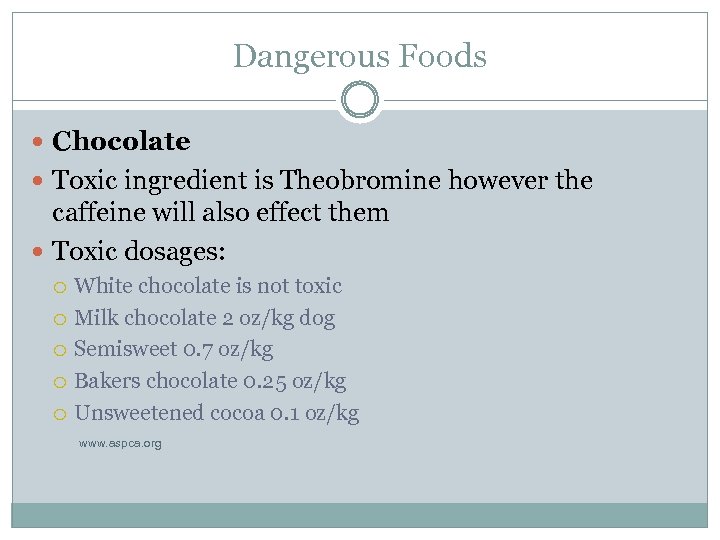 Dangerous Foods Chocolate Toxic ingredient is Theobromine however the caffeine will also effect them Toxic dosages: White chocolate is not toxic Milk chocolate 2 oz/kg dog Semisweet 0. 7 oz/kg Bakers chocolate 0. 25 oz/kg Unsweetened cocoa 0. 1 oz/kg www. aspca. org
Dangerous Foods Chocolate Toxic ingredient is Theobromine however the caffeine will also effect them Toxic dosages: White chocolate is not toxic Milk chocolate 2 oz/kg dog Semisweet 0. 7 oz/kg Bakers chocolate 0. 25 oz/kg Unsweetened cocoa 0. 1 oz/kg www. aspca. org
 Dangerous Foods Chocolate Signs V and D, hyperactivity, muscle tremors, tachycardia, hypertension, +/- seizures Treatment Induce vomiting, gastric lavage may be necessary Activated charcoal given after IV fluids, +/- oxygen therapy
Dangerous Foods Chocolate Signs V and D, hyperactivity, muscle tremors, tachycardia, hypertension, +/- seizures Treatment Induce vomiting, gastric lavage may be necessary Activated charcoal given after IV fluids, +/- oxygen therapy
 Dangerous Foods Grapes/Raisins Effects dogs, unknown reason or cause Side effects Kidney failure Treatment Symptomatic and supportive care
Dangerous Foods Grapes/Raisins Effects dogs, unknown reason or cause Side effects Kidney failure Treatment Symptomatic and supportive care
 Dangerous Foods Xylitol Signs GI symptoms, weakness, PU/PD, elevated liver enzymes with acute renal failure, hemorrhage, DIC Treatment Induce vomiting Symptomatic and supportive care
Dangerous Foods Xylitol Signs GI symptoms, weakness, PU/PD, elevated liver enzymes with acute renal failure, hemorrhage, DIC Treatment Induce vomiting Symptomatic and supportive care
 Dangerous plants Rhododendron species Can lead to cardiovascular dysfunction Signs- v and d, abdominal pain, weakness, depression, cardiac arrythmias, hypotension, shock, dyspnea, CNS depression, seizures Cardiac Glycoside- containing plants Signs involve GI tract and cardio system. Toxic in very small amounts Castor beans Most potent plant toxic known- Ricin- Potentially lethal Cycad palms Effects hepatic and GI systems, results in liver failure and death in dogs
Dangerous plants Rhododendron species Can lead to cardiovascular dysfunction Signs- v and d, abdominal pain, weakness, depression, cardiac arrythmias, hypotension, shock, dyspnea, CNS depression, seizures Cardiac Glycoside- containing plants Signs involve GI tract and cardio system. Toxic in very small amounts Castor beans Most potent plant toxic known- Ricin- Potentially lethal Cycad palms Effects hepatic and GI systems, results in liver failure and death in dogs
 Dangerous Plants Lilies Acute renal failure and death in cats Calcium oxalate- containing plants Calcium oxalate crystals present in plant material causing painful oropharyngeal edema. Airway compromised from tissue swelling, can be life-threatening
Dangerous Plants Lilies Acute renal failure and death in cats Calcium oxalate- containing plants Calcium oxalate crystals present in plant material causing painful oropharyngeal edema. Airway compromised from tissue swelling, can be life-threatening
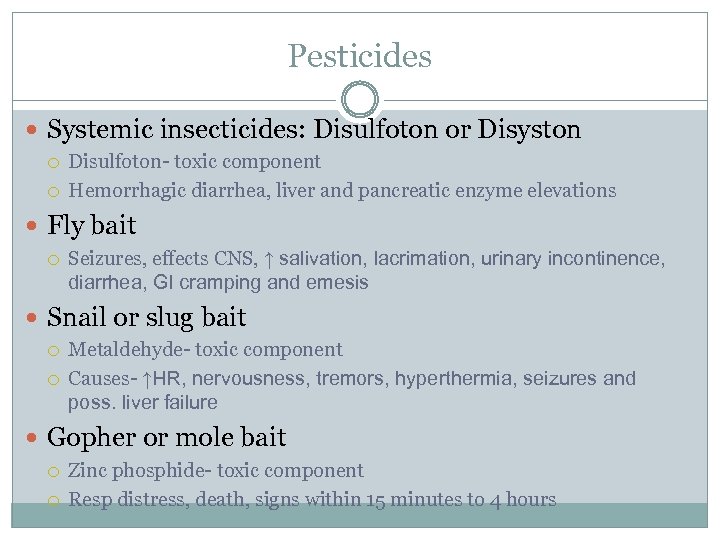 Pesticides Systemic insecticides: Disulfoton or Disyston Disulfoton- toxic component Hemorrhagic diarrhea, liver and pancreatic enzyme elevations Fly bait Seizures, effects CNS, ↑ salivation, lacrimation, urinary incontinence, diarrhea, GI cramping and emesis Snail or slug bait Metaldehyde- toxic component Causes- ↑HR, nervousness, tremors, hyperthermia, seizures and poss. liver failure Gopher or mole bait Zinc phosphide- toxic component Resp distress, death, signs within 15 minutes to 4 hours
Pesticides Systemic insecticides: Disulfoton or Disyston Disulfoton- toxic component Hemorrhagic diarrhea, liver and pancreatic enzyme elevations Fly bait Seizures, effects CNS, ↑ salivation, lacrimation, urinary incontinence, diarrhea, GI cramping and emesis Snail or slug bait Metaldehyde- toxic component Causes- ↑HR, nervousness, tremors, hyperthermia, seizures and poss. liver failure Gopher or mole bait Zinc phosphide- toxic component Resp distress, death, signs within 15 minutes to 4 hours
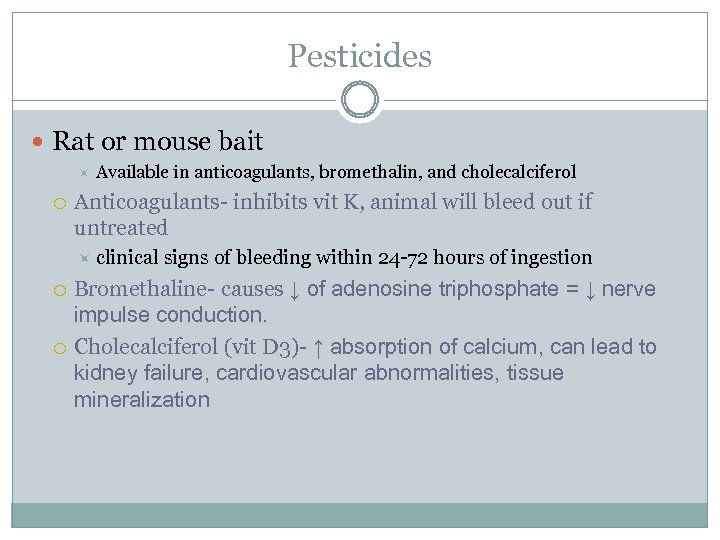 Pesticides Rat or mouse bait Available in anticoagulants, bromethalin, and cholecalciferol Anticoagulants- inhibits vit K, animal will bleed out if untreated clinical signs of bleeding within 24 -72 hours of ingestion Bromethaline- causes ↓ of adenosine triphosphate = ↓ nerve impulse conduction. Cholecalciferol (vit D 3)- ↑ absorption of calcium, can lead to kidney failure, cardiovascular abnormalities, tissue mineralization
Pesticides Rat or mouse bait Available in anticoagulants, bromethalin, and cholecalciferol Anticoagulants- inhibits vit K, animal will bleed out if untreated clinical signs of bleeding within 24 -72 hours of ingestion Bromethaline- causes ↓ of adenosine triphosphate = ↓ nerve impulse conduction. Cholecalciferol (vit D 3)- ↑ absorption of calcium, can lead to kidney failure, cardiovascular abnormalities, tissue mineralization
 Pesticides Diagnosis Patient history Prothrombin time (PT) and activated partial thromboplastin time (PTT) Both become prolonged with rodenticide toxicity Countertop analyzers are available for rapid in-house assessment of clotting times- very pricey to own.
Pesticides Diagnosis Patient history Prothrombin time (PT) and activated partial thromboplastin time (PTT) Both become prolonged with rodenticide toxicity Countertop analyzers are available for rapid in-house assessment of clotting times- very pricey to own.
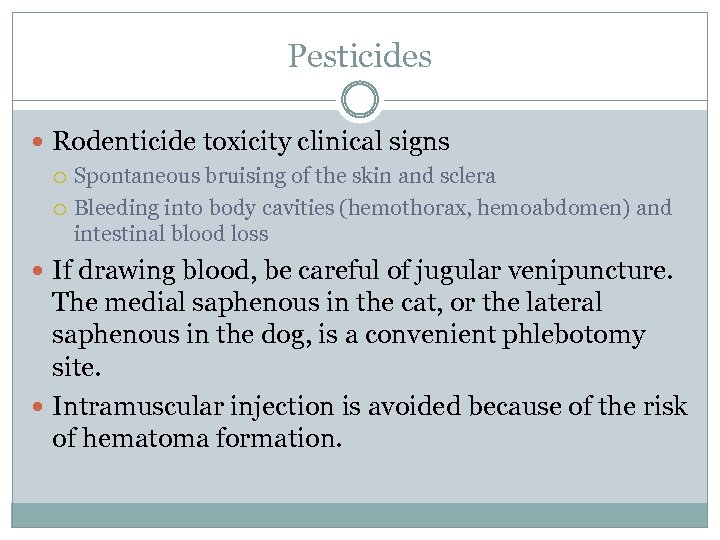 Pesticides Rodenticide toxicity clinical signs Spontaneous bruising of the skin and sclera Bleeding into body cavities (hemothorax, hemoabdomen) and intestinal blood loss If drawing blood, be careful of jugular venipuncture. The medial saphenous in the cat, or the lateral saphenous in the dog, is a convenient phlebotomy site. Intramuscular injection is avoided because of the risk of hematoma formation.
Pesticides Rodenticide toxicity clinical signs Spontaneous bruising of the skin and sclera Bleeding into body cavities (hemothorax, hemoabdomen) and intestinal blood loss If drawing blood, be careful of jugular venipuncture. The medial saphenous in the cat, or the lateral saphenous in the dog, is a convenient phlebotomy site. Intramuscular injection is avoided because of the risk of hematoma formation.
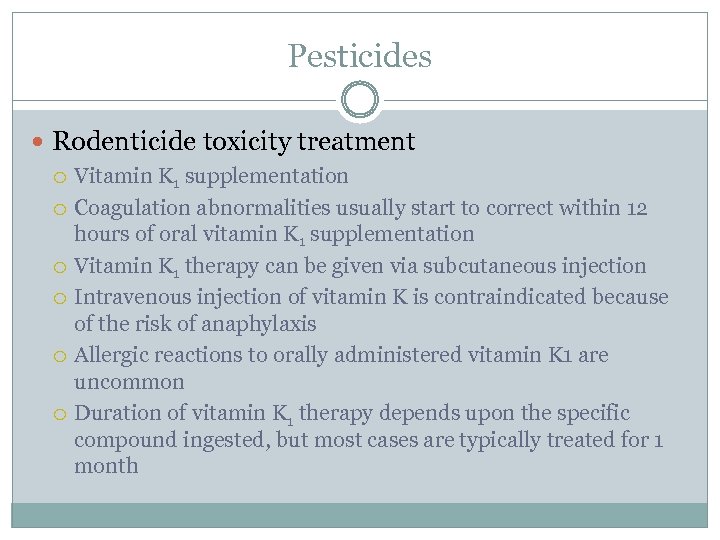 Pesticides Rodenticide toxicity treatment Vitamin K 1 supplementation Coagulation abnormalities usually start to correct within 12 hours of oral vitamin K 1 supplementation Vitamin K 1 therapy can be given via subcutaneous injection Intravenous injection of vitamin K is contraindicated because of the risk of anaphylaxis Allergic reactions to orally administered vitamin K 1 are uncommon Duration of vitamin K 1 therapy depends upon the specific compound ingested, but most cases are typically treated for 1 month
Pesticides Rodenticide toxicity treatment Vitamin K 1 supplementation Coagulation abnormalities usually start to correct within 12 hours of oral vitamin K 1 supplementation Vitamin K 1 therapy can be given via subcutaneous injection Intravenous injection of vitamin K is contraindicated because of the risk of anaphylaxis Allergic reactions to orally administered vitamin K 1 are uncommon Duration of vitamin K 1 therapy depends upon the specific compound ingested, but most cases are typically treated for 1 month
 Antifreeze products Methanol Causes metabolic acidosis Minimum toxic dose in dogs (8. 0 g/kg) Propylene glycol 3 x less toxic than ethylene glycol Acidosis, liver damage, renal insufficiency and seizures are possible Ethylene glycol Active ingredient of most automotive antifreeze solutions Most dangerous form- min dose dogs (4. 4 -6. 6 ml/kg) cat (1. 4 ml/kg) Causes metabolic acidosis and renal tubular necrosis Emesis if recent ingestion (<1 hr), Fomepizole admin in dogs, ethanol in dogs or cats
Antifreeze products Methanol Causes metabolic acidosis Minimum toxic dose in dogs (8. 0 g/kg) Propylene glycol 3 x less toxic than ethylene glycol Acidosis, liver damage, renal insufficiency and seizures are possible Ethylene glycol Active ingredient of most automotive antifreeze solutions Most dangerous form- min dose dogs (4. 4 -6. 6 ml/kg) cat (1. 4 ml/kg) Causes metabolic acidosis and renal tubular necrosis Emesis if recent ingestion (<1 hr), Fomepizole admin in dogs, ethanol in dogs or cats
 Ethylene Glycol Ethylene glycol ingestion clinical signs “Early” signs occur within 30 minutes to 12 hours postingestion Signs include vomiting, lethargy, excessive drinking/urination, incoordination Neurological signs Ataxia, proprioceptive deficits, seizures Initial neurological signs often diminish as ethylene glycol is metabolized, leading to a false sense of recovery
Ethylene Glycol Ethylene glycol ingestion clinical signs “Early” signs occur within 30 minutes to 12 hours postingestion Signs include vomiting, lethargy, excessive drinking/urination, incoordination Neurological signs Ataxia, proprioceptive deficits, seizures Initial neurological signs often diminish as ethylene glycol is metabolized, leading to a false sense of recovery
 Ethylene Glycol Metabolites of ethylene glycol soon cause acute renal failure in both cats and dogs Kidney failure generally develops within 12 -24 hours in cats Kidney failure with 48 -72 hours in dogs “Late” clinical signs of ethylene glycol poisoning include renewed neurological signs from severe kidney failure Oliguria/anuria, severe lethargy, vomiting, and dehydration Seizures, coma, and death
Ethylene Glycol Metabolites of ethylene glycol soon cause acute renal failure in both cats and dogs Kidney failure generally develops within 12 -24 hours in cats Kidney failure with 48 -72 hours in dogs “Late” clinical signs of ethylene glycol poisoning include renewed neurological signs from severe kidney failure Oliguria/anuria, severe lethargy, vomiting, and dehydration Seizures, coma, and death
 Ethylene Glycol Ingestion diagnosis: Blood levels peak at 12 hours post-ingestion in dogs, 3 -6 hours post-ingestion in cats and then diminish rapidly Definitive diagnosis requires either witnessed ingestion or demonstration of ethylene glycol in blood or urine Ethylene glycol assays commercially available Thereafter, investigate ethylene glycol levels in the urine, where the compound is excreted Isosthenuria and calcium oxalate monohydrate crystals in the urine may be seen within hours of ingestion and can be important supporting evidence in the diagnosis of toxicity
Ethylene Glycol Ingestion diagnosis: Blood levels peak at 12 hours post-ingestion in dogs, 3 -6 hours post-ingestion in cats and then diminish rapidly Definitive diagnosis requires either witnessed ingestion or demonstration of ethylene glycol in blood or urine Ethylene glycol assays commercially available Thereafter, investigate ethylene glycol levels in the urine, where the compound is excreted Isosthenuria and calcium oxalate monohydrate crystals in the urine may be seen within hours of ingestion and can be important supporting evidence in the diagnosis of toxicity
 Ethylene Glycol Ethylene glycol ingestion treatment Varies with the level of available care and the timing of diagnosis Witnessed ingestion should be managed with standard detoxification procedures including induction of vomiting and administration of activated charcoal within 1 -2 hours of ingestion IV fluids, peritoneal dialysis and cathartics are recommended. (monitor fluid overload!) Standard treatment is focused on preventing metabolism of the toxin
Ethylene Glycol Ethylene glycol ingestion treatment Varies with the level of available care and the timing of diagnosis Witnessed ingestion should be managed with standard detoxification procedures including induction of vomiting and administration of activated charcoal within 1 -2 hours of ingestion IV fluids, peritoneal dialysis and cathartics are recommended. (monitor fluid overload!) Standard treatment is focused on preventing metabolism of the toxin
 Ethylene Glycol Ethylene glycol ingestion treatment (cont’d) Metabolism of ethylene glycol may be inhibited by administration of fomepizole (Antizol-Vet, Orphan Medical) Medical-grade ethanol can also be used to competitively inhibit the enzymes responsible for ethylene glycol metabolism
Ethylene Glycol Ethylene glycol ingestion treatment (cont’d) Metabolism of ethylene glycol may be inhibited by administration of fomepizole (Antizol-Vet, Orphan Medical) Medical-grade ethanol can also be used to competitively inhibit the enzymes responsible for ethylene glycol metabolism
 Dangerous Human Medications Acetaminophen- toxic metabolite is N-acetyl- parabenzequinoneimine Ibuprofen Aspirin Ma Huang, pseudoephedrine, and Ephedrine: sympathomimetic alkaloids Isoniazid Used in tx of TB Calcipotriene: Vit D derivatives Tx of psoriasis 5 -Fluorouracil: antimetabolites Anticancer topical cream
Dangerous Human Medications Acetaminophen- toxic metabolite is N-acetyl- parabenzequinoneimine Ibuprofen Aspirin Ma Huang, pseudoephedrine, and Ephedrine: sympathomimetic alkaloids Isoniazid Used in tx of TB Calcipotriene: Vit D derivatives Tx of psoriasis 5 -Fluorouracil: antimetabolites Anticancer topical cream
 Toxicities Acetaminophen (Tylenol) Extremely dangerous in cats (1 tablet can be fatal!) Side effects Seen 1 -2 hours post ingestion: dyspnea, salivation, vomiting, brown or cyanotic MM, dark or chocolate colored blood, edema, liver signs. May see death in cats within 1 hour of ingestion.
Toxicities Acetaminophen (Tylenol) Extremely dangerous in cats (1 tablet can be fatal!) Side effects Seen 1 -2 hours post ingestion: dyspnea, salivation, vomiting, brown or cyanotic MM, dark or chocolate colored blood, edema, liver signs. May see death in cats within 1 hour of ingestion.
 Toxicities Acetaminophen treatment Induce vomiting if <1 hour post ingestion Activated charcoal given after IV fluids and oxygen recommended if tachypnea is not present.
Toxicities Acetaminophen treatment Induce vomiting if <1 hour post ingestion Activated charcoal given after IV fluids and oxygen recommended if tachypnea is not present.


