e01278a8c53cbae48d5ce60e131790ca.ppt
- Количество слайдов: 17
 Towards Innovative Healthcare Financing Ghana NHIS 10 th Anniversary Conference WHO Consultant Sheila O’Dougherty November 2013
Towards Innovative Healthcare Financing Ghana NHIS 10 th Anniversary Conference WHO Consultant Sheila O’Dougherty November 2013
 Outline of Presentation • International trend: from opposing camps to disappearing dichotomies • Innovation and efficiency gains: the relationship between three health financing functions of revenue collection, pooling of funds and health purchasing
Outline of Presentation • International trend: from opposing camps to disappearing dichotomies • Innovation and efficiency gains: the relationship between three health financing functions of revenue collection, pooling of funds and health purchasing
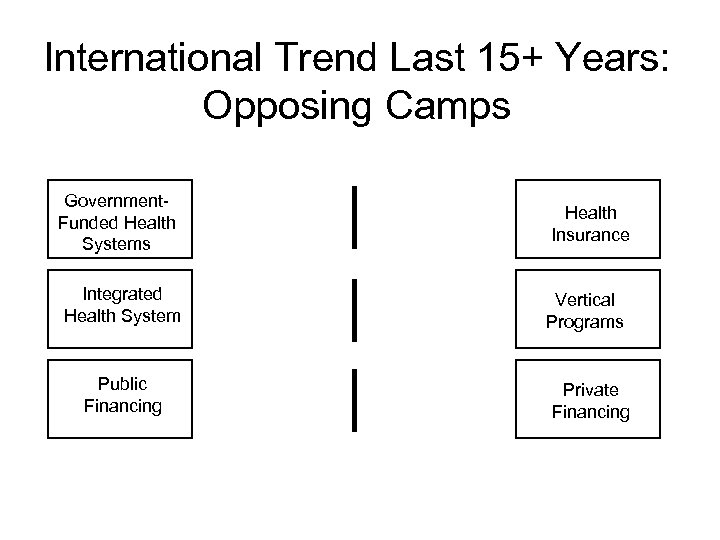 International Trend Last 15+ Years: Opposing Camps Government. Funded Health Systems Integrated Health System Public Financing Health Insurance Vertical Programs Private Financing
International Trend Last 15+ Years: Opposing Camps Government. Funded Health Systems Integrated Health System Public Financing Health Insurance Vertical Programs Private Financing
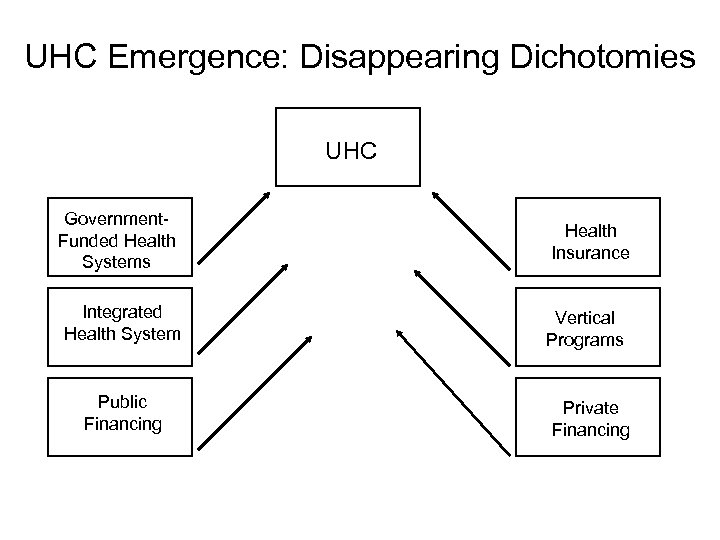 UHC Emergence: Disappearing Dichotomies UHC Government. Funded Health Systems Integrated Health System Public Financing Health Insurance Vertical Programs Private Financing
UHC Emergence: Disappearing Dichotomies UHC Government. Funded Health Systems Integrated Health System Public Financing Health Insurance Vertical Programs Private Financing
 Universal Health Coverage • "Financing systems need to be specifically designed to: – Provide all people with access to needed health services (including prevention, promotion, treatment and rehabilitation) of sufficient quality to be effective; – Ensure that the use of these services does not expose the user to financial hardship“ – World Health Report 2010, p. 6 – More a journey than a destination
Universal Health Coverage • "Financing systems need to be specifically designed to: – Provide all people with access to needed health services (including prevention, promotion, treatment and rehabilitation) of sufficient quality to be effective; – Ensure that the use of these services does not expose the user to financial hardship“ – World Health Report 2010, p. 6 – More a journey than a destination
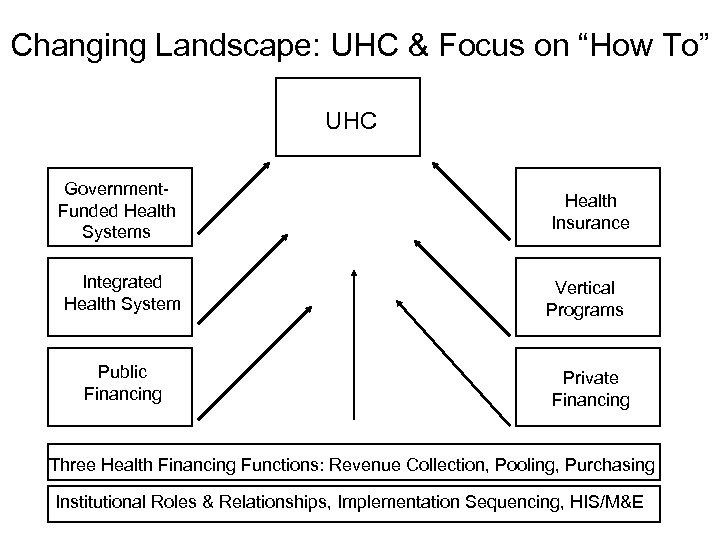 Changing Landscape: UHC & Focus on “How To” UHC Government. Funded Health Systems Integrated Health System Public Financing Health Insurance Vertical Programs Private Financing Three Health Financing Functions: Revenue Collection, Pooling, Purchasing Institutional Roles & Relationships, Implementation Sequencing, HIS/M&E
Changing Landscape: UHC & Focus on “How To” UHC Government. Funded Health Systems Integrated Health System Public Financing Health Insurance Vertical Programs Private Financing Three Health Financing Functions: Revenue Collection, Pooling, Purchasing Institutional Roles & Relationships, Implementation Sequencing, HIS/M&E
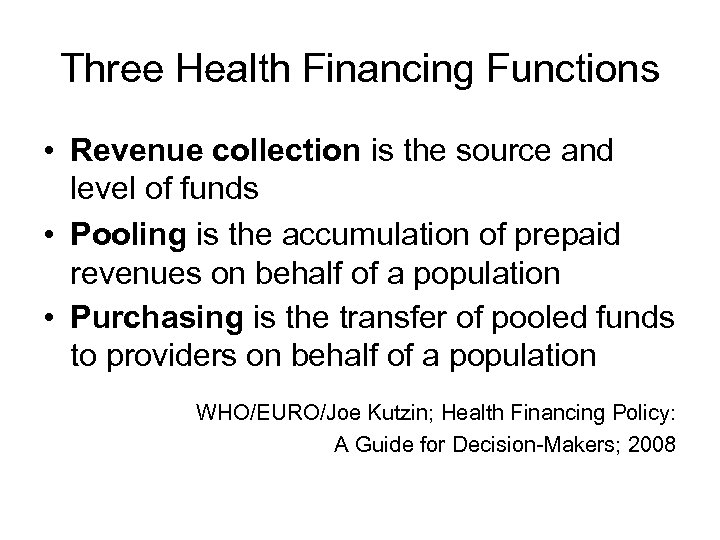 Three Health Financing Functions • Revenue collection is the source and level of funds • Pooling is the accumulation of prepaid revenues on behalf of a population • Purchasing is the transfer of pooled funds to providers on behalf of a population WHO/EURO/Joe Kutzin; Health Financing Policy: A Guide for Decision-Makers; 2008
Three Health Financing Functions • Revenue collection is the source and level of funds • Pooling is the accumulation of prepaid revenues on behalf of a population • Purchasing is the transfer of pooled funds to providers on behalf of a population WHO/EURO/Joe Kutzin; Health Financing Policy: A Guide for Decision-Makers; 2008
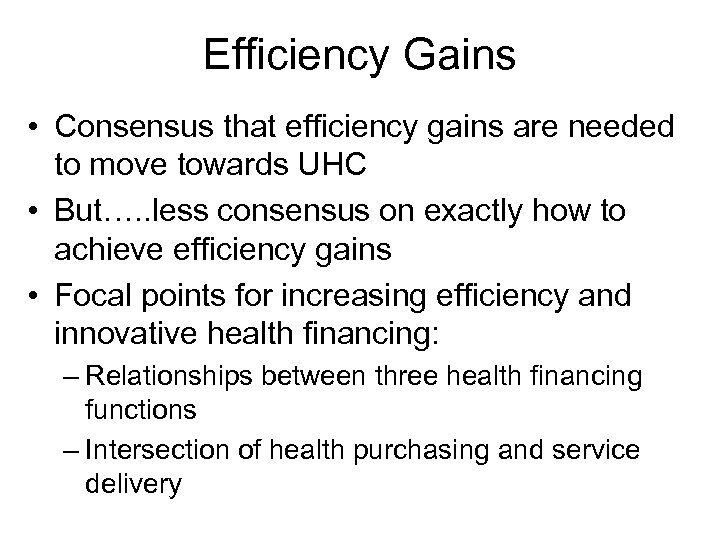 Efficiency Gains • Consensus that efficiency gains are needed to move towards UHC • But…. . less consensus on exactly how to achieve efficiency gains • Focal points for increasing efficiency and innovative health financing: – Relationships between three health financing functions – Intersection of health purchasing and service delivery
Efficiency Gains • Consensus that efficiency gains are needed to move towards UHC • But…. . less consensus on exactly how to achieve efficiency gains • Focal points for increasing efficiency and innovative health financing: – Relationships between three health financing functions – Intersection of health purchasing and service delivery
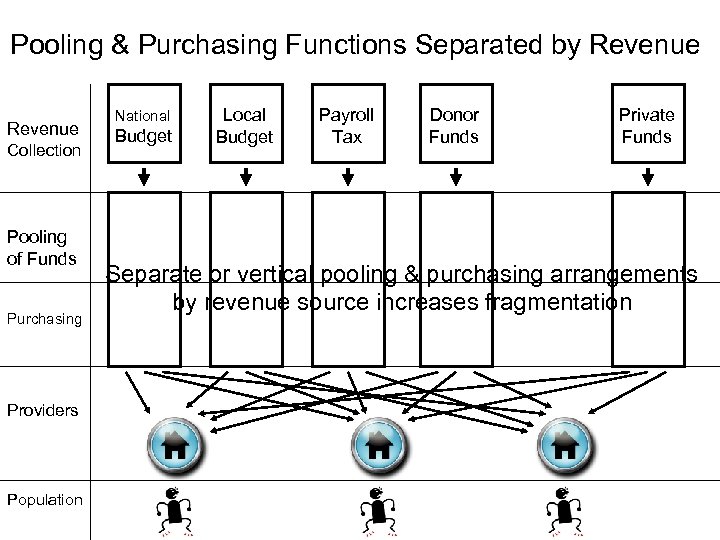 Pooling & Purchasing Functions Separated by Revenue Collection Pooling of Funds Purchasing Providers Population National Budget Local Budget Payroll Tax Donor Funds Private Funds Separate or vertical pooling & purchasing arrangements by revenue source increases fragmentation
Pooling & Purchasing Functions Separated by Revenue Collection Pooling of Funds Purchasing Providers Population National Budget Local Budget Payroll Tax Donor Funds Private Funds Separate or vertical pooling & purchasing arrangements by revenue source increases fragmentation
 Summary (Chart 1) • Common perception that each revenue source is standalone or requires it’s own separate pooling and purchasing arrangements – National budget, local government budget, payroll tax (SHI), other types of taxes, donors, private, etc. • Can lead to health financing fragmentation and inefficiencies: – Less than optimal pooling of funds – Less than optimal service or benefit package and provider payment system specification – At provider level, conflicting financial incentives in payment systems (mess of arrows in payment to providers) – Not achieving service delivery improvement objectives – Not level playing field across types of providers – Harder for people to access covered & appropriate services
Summary (Chart 1) • Common perception that each revenue source is standalone or requires it’s own separate pooling and purchasing arrangements – National budget, local government budget, payroll tax (SHI), other types of taxes, donors, private, etc. • Can lead to health financing fragmentation and inefficiencies: – Less than optimal pooling of funds – Less than optimal service or benefit package and provider payment system specification – At provider level, conflicting financial incentives in payment systems (mess of arrows in payment to providers) – Not achieving service delivery improvement objectives – Not level playing field across types of providers – Harder for people to access covered & appropriate services
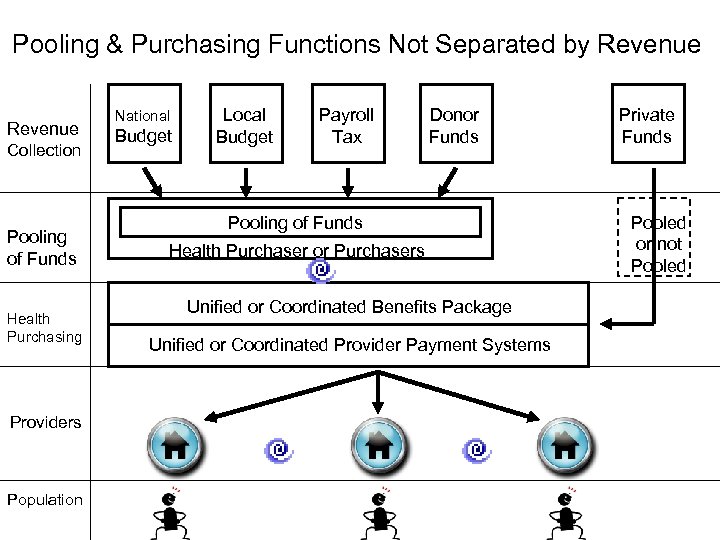 Pooling & Purchasing Functions Not Separated by Revenue Collection Pooling of Funds Health Purchasing Providers Population National Budget Local Budget Payroll Tax Donor Funds Pooling of Funds Health Purchaser or Purchasers Unified or Coordinated Benefits Package Unified or Coordinated Provider Payment Systems Private Funds Pooled or not Pooled
Pooling & Purchasing Functions Not Separated by Revenue Collection Pooling of Funds Health Purchasing Providers Population National Budget Local Budget Payroll Tax Donor Funds Pooling of Funds Health Purchaser or Purchasers Unified or Coordinated Benefits Package Unified or Coordinated Provider Payment Systems Private Funds Pooled or not Pooled
 Purchasing with Health Budget Funds • Input-based line item budgets funding public facilities can be problematic if low budget level doesn’t fund all services provided in health facility – Not clear to provider what services funded and what not funded • Health budget purchasing better targeting or matching priority services & poor populations – Output-based provider payment systems • Key is unit of service—not building but services for people – Financial incentives for desired service delivery improvements – Align rather than fragment health purchasing – Better targeting budget funds to priority services opens space or clear role for private funds
Purchasing with Health Budget Funds • Input-based line item budgets funding public facilities can be problematic if low budget level doesn’t fund all services provided in health facility – Not clear to provider what services funded and what not funded • Health budget purchasing better targeting or matching priority services & poor populations – Output-based provider payment systems • Key is unit of service—not building but services for people – Financial incentives for desired service delivery improvements – Align rather than fragment health purchasing – Better targeting budget funds to priority services opens space or clear role for private funds
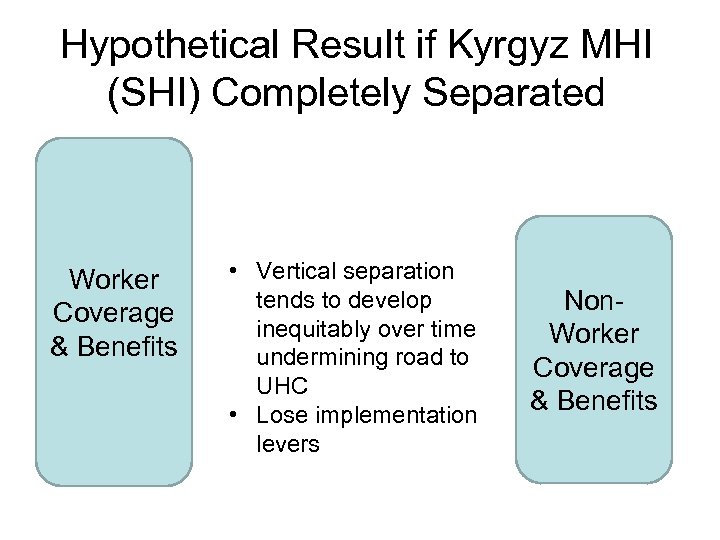 Hypothetical Result if Kyrgyz MHI (SHI) Completely Separated Worker Coverage & Benefits • Vertical separation tends to develop inequitably over time undermining road to UHC • Lose implementation levers Non. Worker Coverage & Benefits
Hypothetical Result if Kyrgyz MHI (SHI) Completely Separated Worker Coverage & Benefits • Vertical separation tends to develop inequitably over time undermining road to UHC • Lose implementation levers Non. Worker Coverage & Benefits
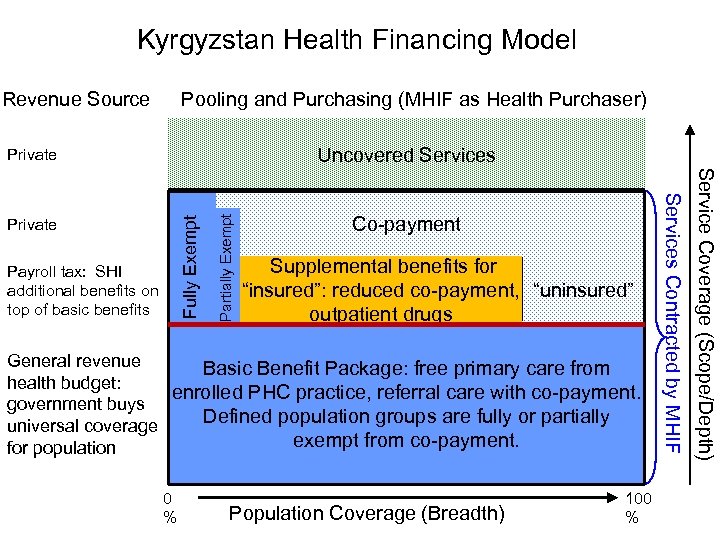 Kyrgyzstan Health Financing Model Revenue Source Pooling and Purchasing (MHIF as Health Purchaser) Payroll tax: SHI additional benefits on top of basic benefits Partially Exempt Co-payment Fully Exempt Private Supplemental benefits for “insured”: reduced co-payment, “uninsured” outpatient drugs General revenue Basic Benefit Package: free primary care from health budget: enrolled PHC practice, referral care with co-payment. government buys Defined population groups are fully or partially universal coverage exempt from co-payment. for population 0 % Population Coverage (Breadth) 100 % Service Coverage (Scope/Depth) Uncovered Services Contracted by MHIF Private
Kyrgyzstan Health Financing Model Revenue Source Pooling and Purchasing (MHIF as Health Purchaser) Payroll tax: SHI additional benefits on top of basic benefits Partially Exempt Co-payment Fully Exempt Private Supplemental benefits for “insured”: reduced co-payment, “uninsured” outpatient drugs General revenue Basic Benefit Package: free primary care from health budget: enrolled PHC practice, referral care with co-payment. government buys Defined population groups are fully or partially universal coverage exempt from co-payment. for population 0 % Population Coverage (Breadth) 100 % Service Coverage (Scope/Depth) Uncovered Services Contracted by MHIF Private
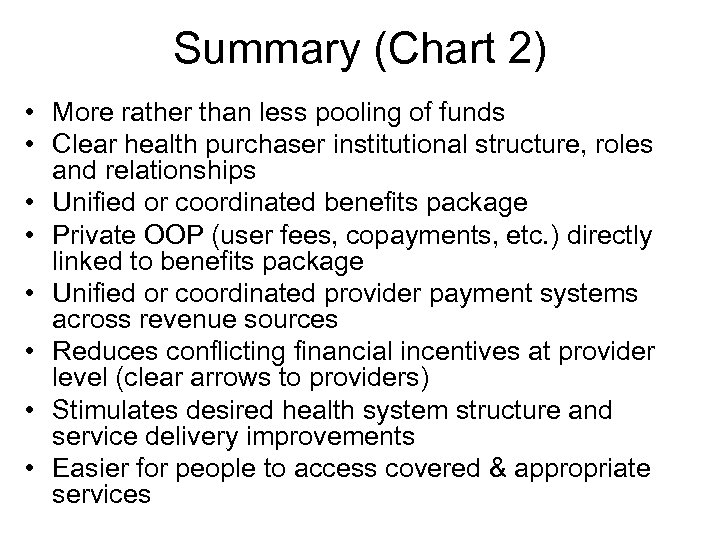 Summary (Chart 2) • More rather than less pooling of funds • Clear health purchaser institutional structure, roles and relationships • Unified or coordinated benefits package • Private OOP (user fees, copayments, etc. ) directly linked to benefits package • Unified or coordinated provider payment systems across revenue sources • Reduces conflicting financial incentives at provider level (clear arrows to providers) • Stimulates desired health system structure and service delivery improvements • Easier for people to access covered & appropriate services
Summary (Chart 2) • More rather than less pooling of funds • Clear health purchaser institutional structure, roles and relationships • Unified or coordinated benefits package • Private OOP (user fees, copayments, etc. ) directly linked to benefits package • Unified or coordinated provider payment systems across revenue sources • Reduces conflicting financial incentives at provider level (clear arrows to providers) • Stimulates desired health system structure and service delivery improvements • Easier for people to access covered & appropriate services
 Possible Relevance to Ghana • Ghana doing excellent job moving toward UHC • Innovations could consider: – More unification or coordination of MOH services/programs and NHIS benefit package • Tied together by health worker salaries – Potential for efficiency gains and reducing conflicting financial incentives in payment systems for variable costs of direct patient care (input-based line item budget, fee-for-service, DRGs, per capita, donor mechanisms) – Ensure health purchasing and financial incentives drive desired service delivery improvements
Possible Relevance to Ghana • Ghana doing excellent job moving toward UHC • Innovations could consider: – More unification or coordination of MOH services/programs and NHIS benefit package • Tied together by health worker salaries – Potential for efficiency gains and reducing conflicting financial incentives in payment systems for variable costs of direct patient care (input-based line item budget, fee-for-service, DRGs, per capita, donor mechanisms) – Ensure health purchasing and financial incentives drive desired service delivery improvements
 Conclusions • Emergence of UHC as goal can be: – Problem: creates unrealistic expectations – Opportunity: disappearing dichotomies open avenues for innovation • Relationships between three health financing functions and link to service delivery can drive innovation and efficiency gains • Health purchasing for health budget funds better targeting priority services and poor populations – Maximize impact of health budget – Align pooling & purchasing for all revenue sources – Create clarity and space for private financing
Conclusions • Emergence of UHC as goal can be: – Problem: creates unrealistic expectations – Opportunity: disappearing dichotomies open avenues for innovation • Relationships between three health financing functions and link to service delivery can drive innovation and efficiency gains • Health purchasing for health budget funds better targeting priority services and poor populations – Maximize impact of health budget – Align pooling & purchasing for all revenue sources – Create clarity and space for private financing


