20a573a8ed9f974568e5306a787834ef.ppt
- Количество слайдов: 33
TORTORA • FUNKE • CASE Microbiology AN INTRODUCTION B. E Pruitt & Jane J. Stein Chapter 19, part A Disorders Associated with the Immune System
Disorders Associated with the Immune System The Immune system does not always run perfectly • It may over respond - hypersensitivities • Hypersensitivities ~ allergy • 4 types • I, II and III - are humoral • IV is cellular • It may react to your own cells - Autoimmune • Immune Deficiencies - unable to response to new pathogens
Hypersensitivity Reactions • Response to antigens (allergens) leading to damage • First exposure to antigen called “allergen” sensitized, second over reaction • Skin testing
Hypersensitivities • Type I — Anaphylaxis. Mast cells degranulate when Ig. E antibodies on surface bind to pathogens or allergens (antigens that invoke too strong a reaction) • Type II — Antibodies react with cell-surface antigens or cells you own or that have been put in you • Type III (Immune Complex) — Ig. M, Ig. G, complement immune complexes deposit in tissues • Type IV — Delayed Cell mediated by TD (CD 4+ Th 1 cells) release IL-2 to stimulate more Th 1 cells, CD 8 Tc cells and MΦ
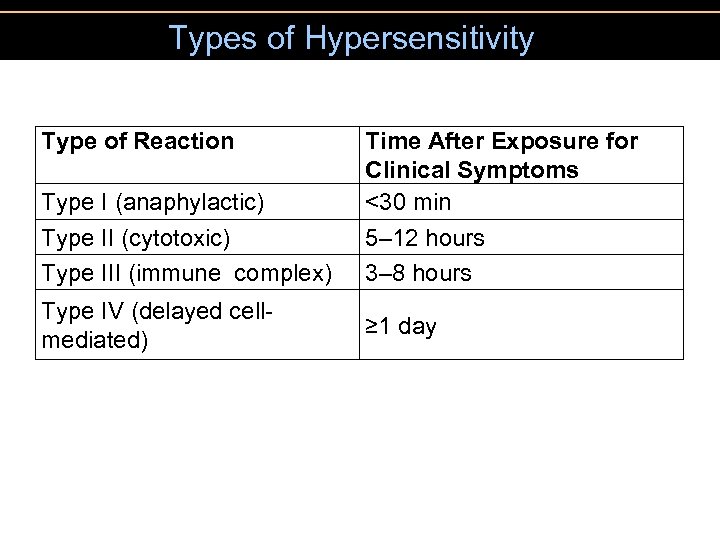
Types of Hypersensitivity Type of Reaction Type I (anaphylactic) Type II (cytotoxic) Type III (immune complex) Type IV (delayed cellmediated) Time After Exposure for Clinical Symptoms <30 min 5– 12 hours 3– 8 hours ≥ 1 day
Type I (Anaphylactic) Reactions Type I • anaphylaxis - against protection • May be localized or systemic Figure 19. 3
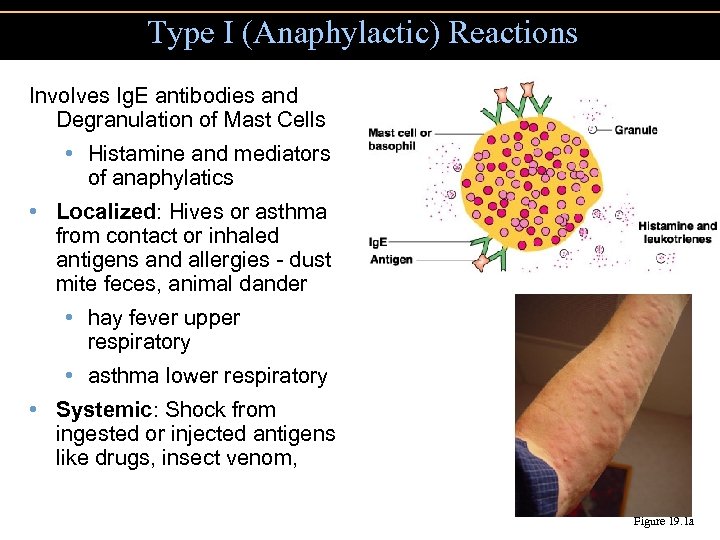
Type I (Anaphylactic) Reactions Involves Ig. E antibodies and Degranulation of Mast Cells • Histamine and mediators of anaphylatics • Localized: Hives or asthma from contact or inhaled antigens and allergies - dust mite feces, animal dander • hay fever upper respiratory • asthma lower respiratory • Systemic: Shock from ingested or injected antigens like drugs, insect venom, Figure 19. 1 a
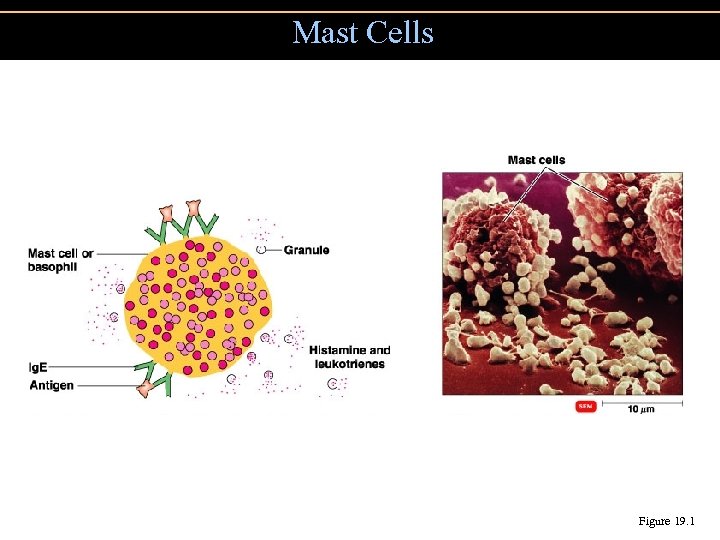
Mast Cells Figure 19. 1
Type I (Anaphylactic) Reactions • Systemic anaphylaxis • May result in circulatory collapse and death • Localized anaphylaxis • Hives, hay fever, and asthma
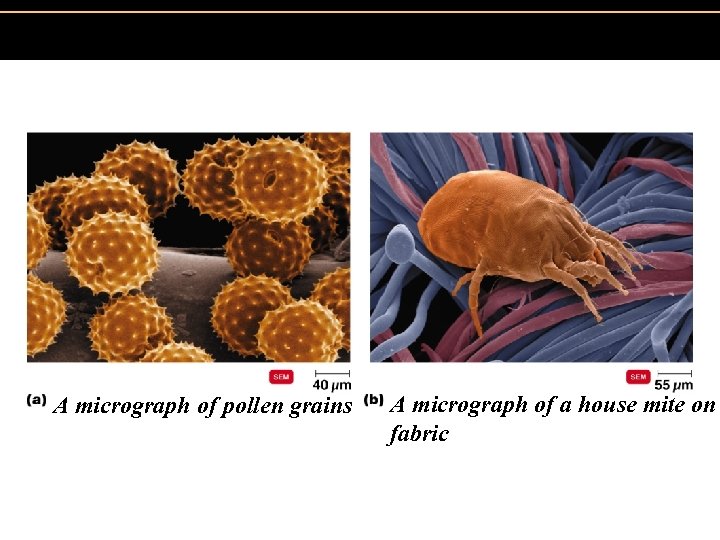
Figure 19. 2 Localized anaphylaxis. A micrograph of pollen grains A micrograph of a house mite on fabric
Figure 19. 3 A skin test to identify allergens. Desensitization can help improve reaction in about 70% of individuals. Produce Ig. G to antigen (allergen) and hide it from Mast cells and Ig. E’s
Preventing Anaphylactic Reactions • Desensitizing injections of antigen • Cause production of Ig. G, so that Ig. G antibodies will act as blocking antibodies
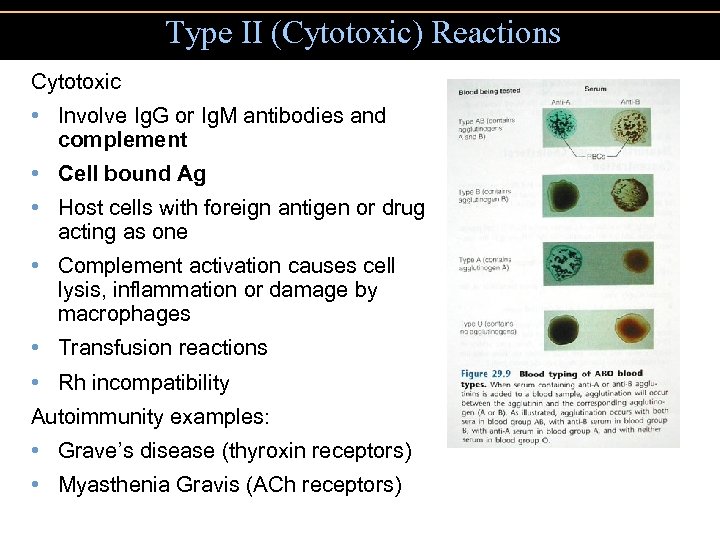
Type II (Cytotoxic) Reactions Cytotoxic • Involve Ig. G or Ig. M antibodies and complement • Cell bound Ag • Host cells with foreign antigen or drug acting as one • Complement activation causes cell lysis, inflammation or damage by macrophages • Transfusion reactions • Rh incompatibility Autoimmunity examples: • Grave’s disease (thyroxin receptors) • Myasthenia Gravis (ACh receptors)
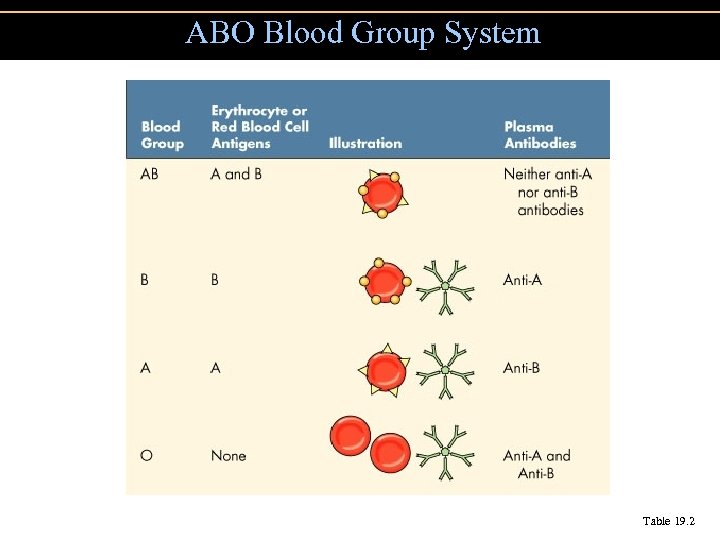
ABO Blood Group System Table 19. 2
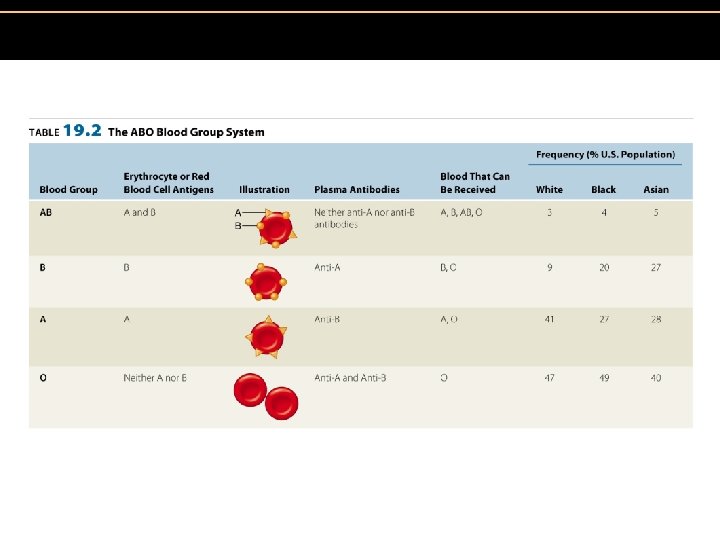
Table 19. 2 The ABO Blood Group System Insert Table 19. 2
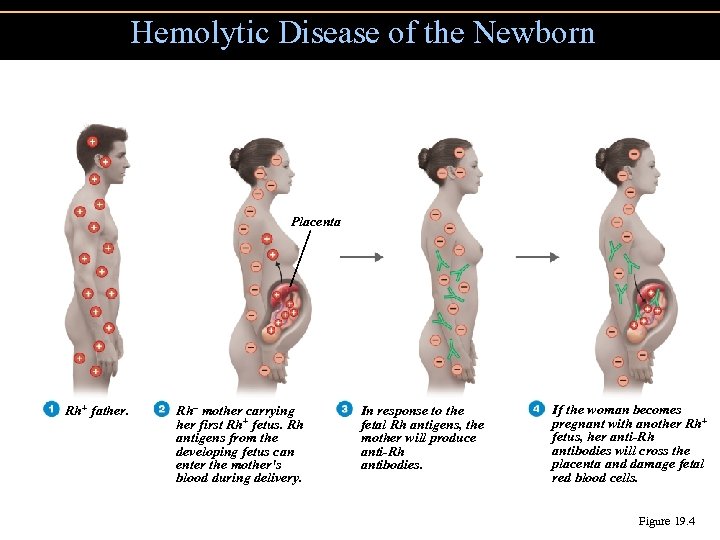
Hemolytic Disease of the Newborn Placenta Rh+ father. Rh– mother carrying her first Rh+ fetus. Rh antigens from the developing fetus can enter the mother's blood during delivery. In response to the fetal Rh antigens, the mother will produce anti-Rh antibodies. If the woman becomes pregnant with another Rh+ fetus, her anti-Rh antibodies will cross the placenta and damage fetal red blood cells. Figure 19. 4
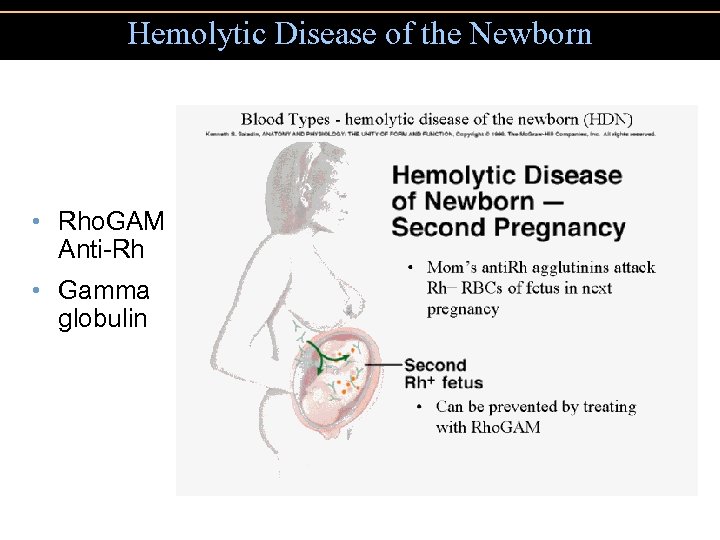
Hemolytic Disease of the Newborn • Rho. GAM Anti-Rh • Gamma globulin
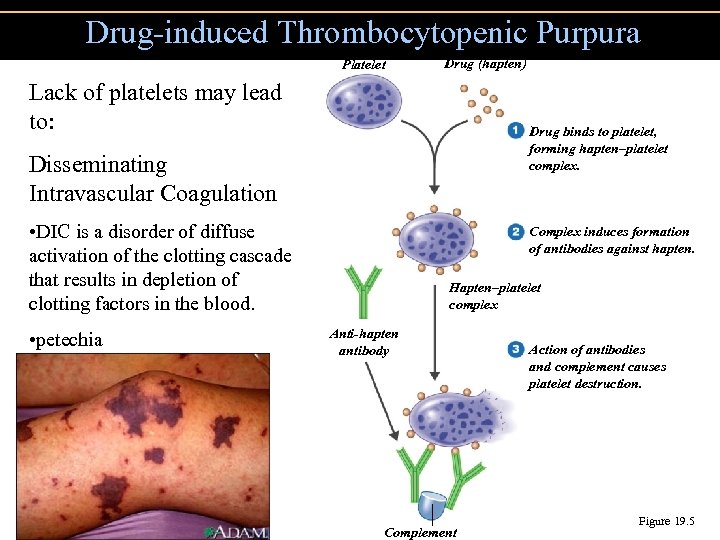
Drug-induced Thrombocytopenic Purpura Platelet Drug (hapten) Lack of platelets may lead to: Drug binds to platelet, forming hapten–platelet complex. Disseminating Intravascular Coagulation • DIC is a disorder of diffuse activation of the clotting cascade that results in depletion of clotting factors in the blood. • petechia Complex induces formation of antibodies against hapten. Hapten–platelet complex Anti-hapten antibody Complement Action of antibodies and complement causes platelet destruction. Figure 19. 5
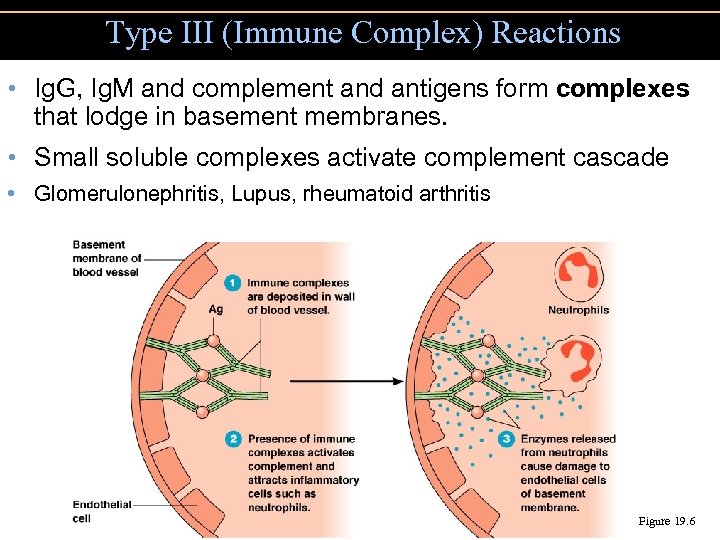
Type III (Immune Complex) Reactions • Ig. G, Ig. M and complement and antigens form complexes that lodge in basement membranes. • Small soluble complexes activate complement cascade • Glomerulonephritis, Lupus, rheumatoid arthritis Figure 19. 6
Type IV (Cell-Mediated) Reactions • Delayed-type hypersensitivities due to T cells • Cytokines attract macrophages and TC cells • Initiate tissue damage
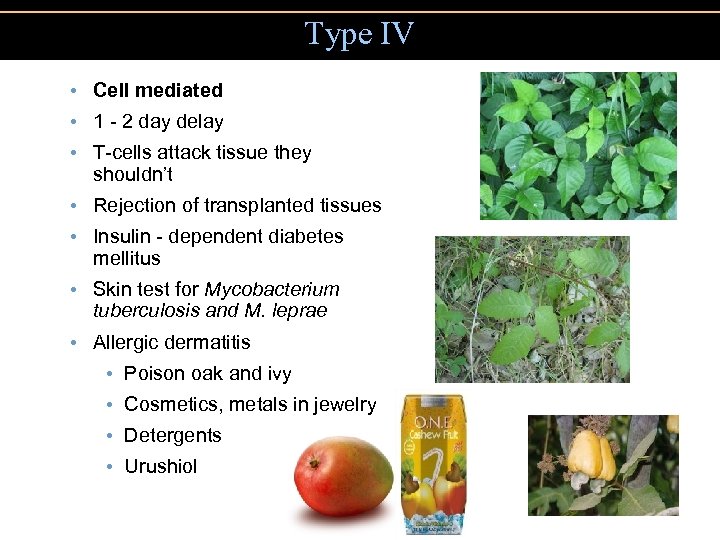
Type IV • Cell mediated • 1 - 2 day delay • T-cells attack tissue they shouldn’t • Rejection of transplanted tissues • Insulin - dependent diabetes mellitus • Skin test for Mycobacterium tuberculosis and M. leprae • Allergic dermatitis • Poison oak and ivy • Cosmetics, metals in jewelry • Detergents • Urushiol
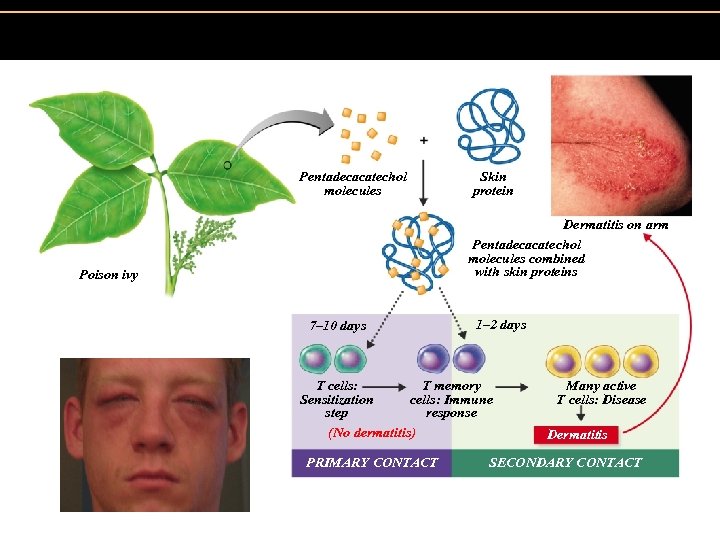
Figure 19. 7 The development of an allergy (allergic contact dermatitis) to catechols from the poison ivy plant. Pentadecacatechol molecules Skin protein Dermatitis on arm Pentadecacatechol molecules combined with skin proteins Poison ivy 7– 10 days 1– 2 days T cells: T memory Sensitization cells: Immune step response (No dermatitis) PRIMARY CONTACT Many active T cells: Disease Dermatitis SECONDARY CONTACT
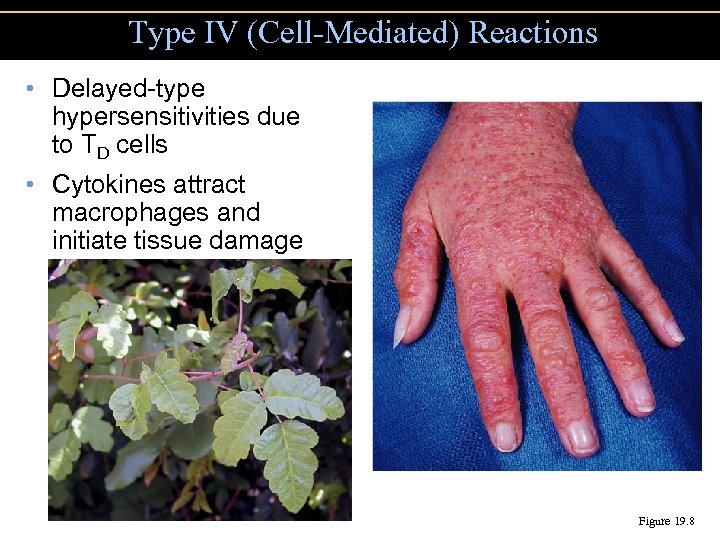
Type IV (Cell-Mediated) Reactions • Delayed-type hypersensitivities due to TD cells • Cytokines attract macrophages and initiate tissue damage Figure 19. 8
Autoimmune Diseases • Clonal deletion during lymphocyte development ensures self-tolerance • Autoimmunity is loss of self-tolerance
Reactions Related to the Human Leukocyte Antigen (HLA) Complex • Histocompatibility antigens: Self antigens on cell surfaces • Major histocompatibility complex (MHC): Genes encoding histocompatibility antigens • Human leukocyte antigen (HLA) complex: The group of MHC genes on leukocytes
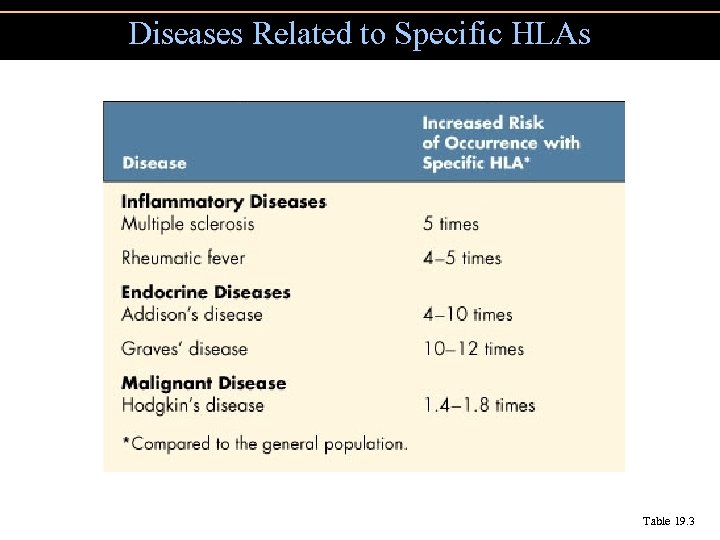
Diseases Related to Specific HLAs Table 19. 3
Reactions to Transplantation • Transplants may be attacked by T cells, macrophages, and complement-fixing antibodies. • Transplants to privileged sites do not cause an immune response. • Cornea, testes, brain, heart valves and fetal tissue • Stem cells may allow therapeutic cloning to avoid rejection. Organ rejection
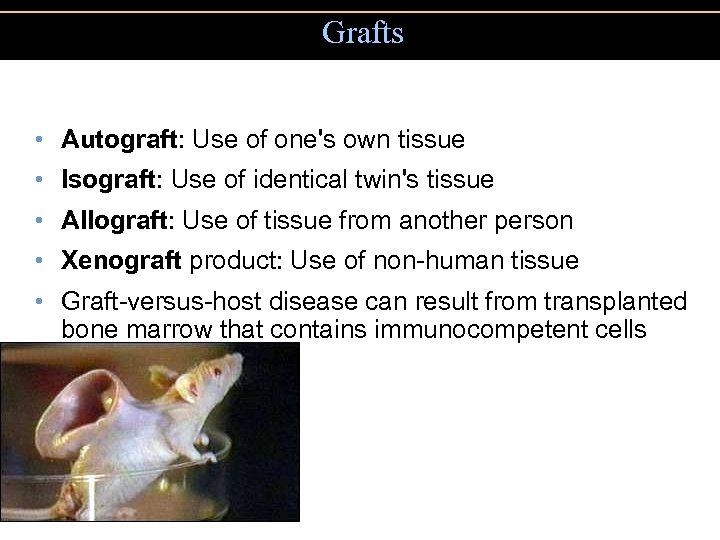
Grafts • Autograft: Use of one's own tissue • Isograft: Use of identical twin's tissue • Allograft: Use of tissue from another person • Xenograft product: Use of non-human tissue • Graft-versus-host disease can result from transplanted bone marrow that contains immunocompetent cells
Immunosuppression prevents an immune response to transplanted tissues • Cyclosporine suppresses IL-2 • Mycophenolate mofetil inhibits T cell and B cell reproduction • Sirolimus blocks IL-2
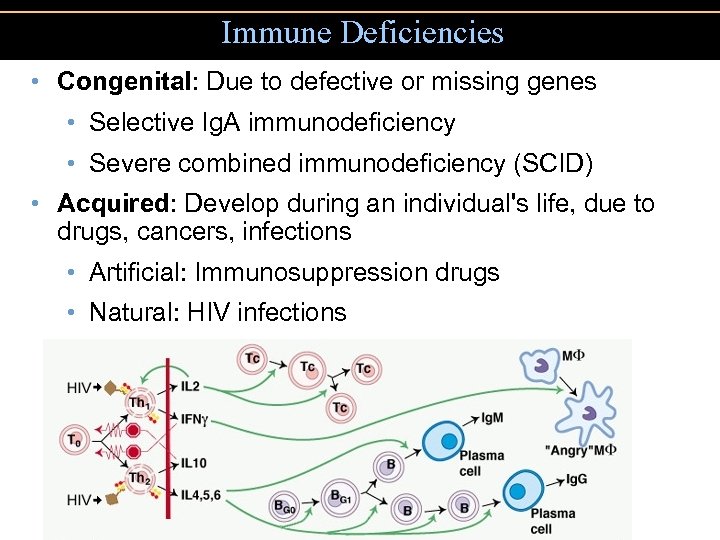
Immune Deficiencies • Congenital: Due to defective or missing genes • Selective Ig. A immunodeficiency • Severe combined immunodeficiency (SCID) • Acquired: Develop during an individual's life, due to drugs, cancers, infections • Artificial: Immunosuppression drugs • Natural: HIV infections
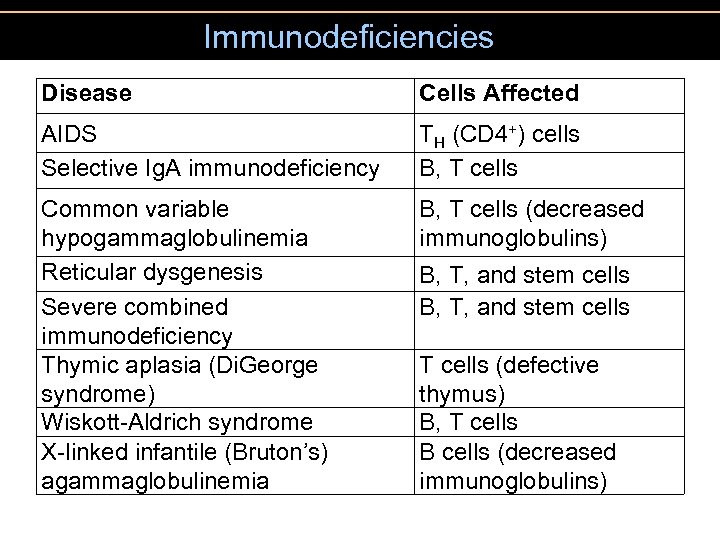
Immunodeficiencies Disease Cells Affected AIDS Selective Ig. A immunodeficiency TH (CD 4+) cells B, T cells Common variable hypogammaglobulinemia Reticular dysgenesis Severe combined immunodeficiency Thymic aplasia (Di. George syndrome) Wiskott-Aldrich syndrome X-linked infantile (Bruton’s) agammaglobulinemia B, T cells (decreased immunoglobulins) B, T, and stem cells T cells (defective thymus) B, T cells B cells (decreased immunoglobulins)
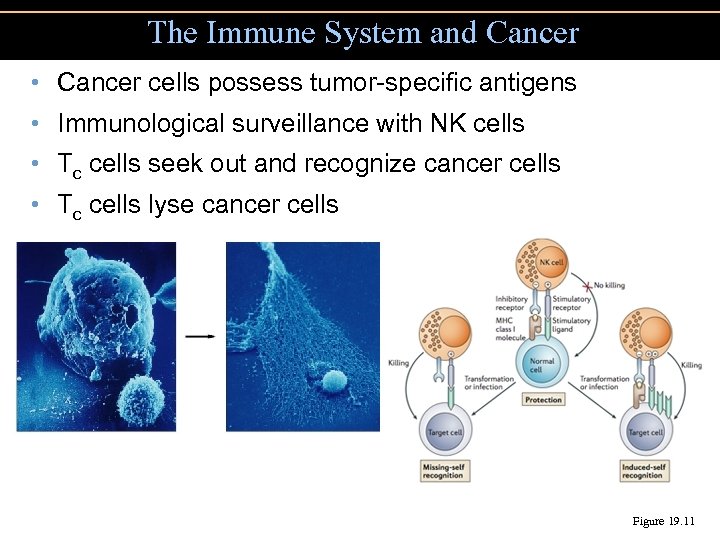
The Immune System and Cancer • Cancer cells possess tumor-specific antigens • Immunological surveillance with NK cells • Tc cells seek out and recognize cancer cells • Tc cells lyse cancer cells Figure 19. 11
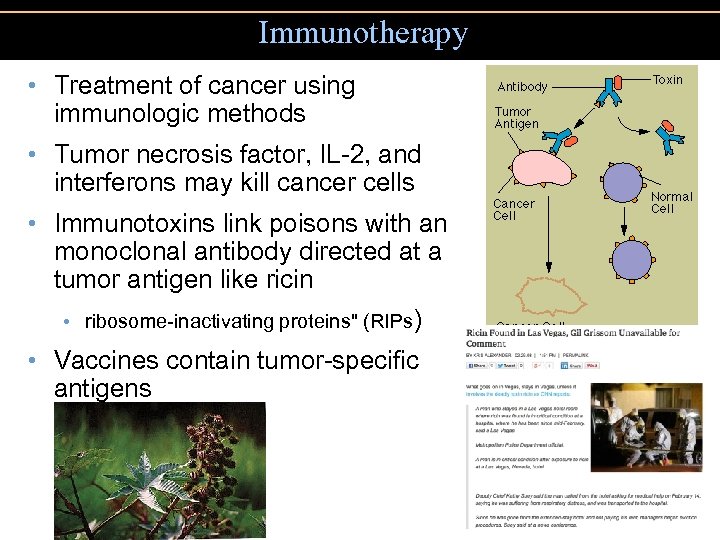
Immunotherapy • Treatment of cancer using immunologic methods • Tumor necrosis factor, IL-2, and interferons may kill cancer cells • Immunotoxins link poisons with an monoclonal antibody directed at a tumor antigen like ricin • ribosome-inactivating proteins" (RIPs) • Vaccines contain tumor-specific antigens
20a573a8ed9f974568e5306a787834ef.ppt