Topics • • • 10 facts about TB Epidemiology of TB Transmission of TB infection Pathogenesis of primary TB Stages of TB infection (throughout live) Diagnosis of TB
Tuberculosis TB – is a common systemic infectious disease caused by Mycobacterium tuberculosis with dominant localization in lungs, leading to development of caseouse inflammation in lung tissue and other organs
10 facts about tuberculosis Fact 1 Tuberculosis (TB) is contagious and spreads through the air. If not treated, each person with active TB can infect on average 10 to 15 people a year.
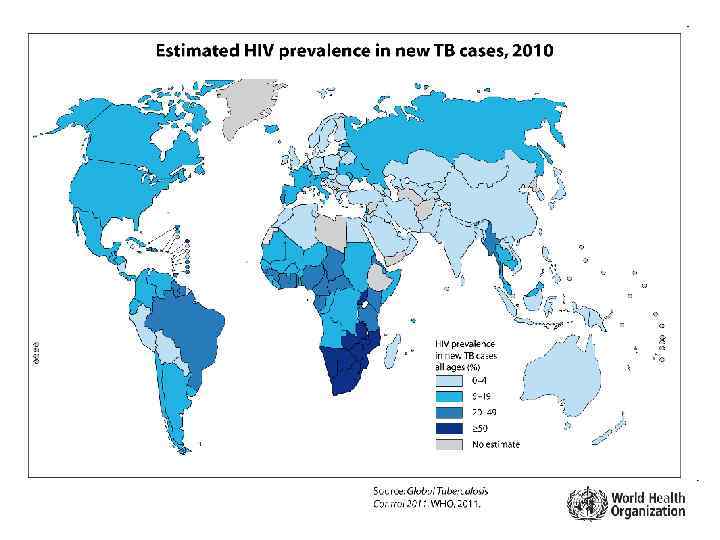
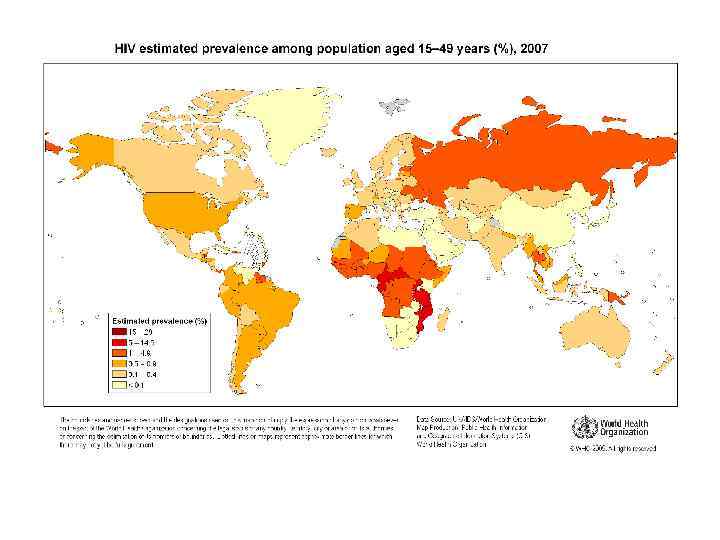
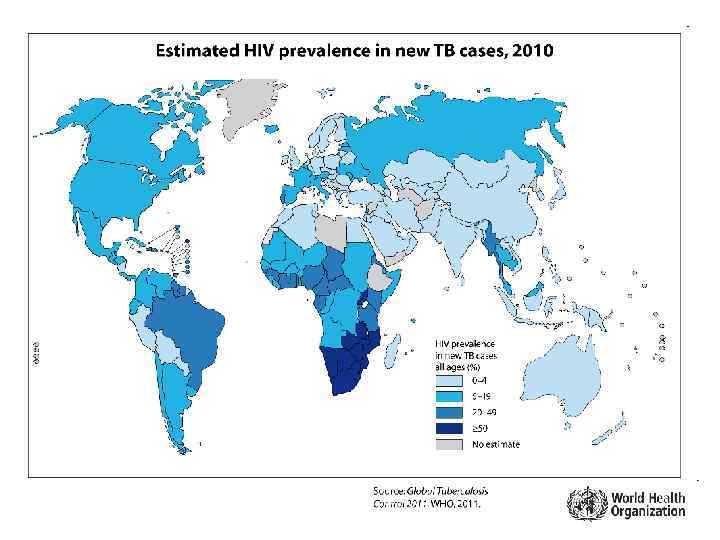
10 facts about tuberculosis Fact 2 More than two billion people, equal to one third of the world’s total population, are infected with TB bacilli, the microbes that cause TB. One in every 10 of those people will become sick with active TB in his or her lifetime. People living with HIV are at a much greater risk.
10 facts about tuberculosis Fact 3 A total of 1. 77 million people died from TB in 2007 (including 456 000 people with HIV), equal to about 4800 deaths a day. TB is a disease of poverty, affecting mostly young adults in their most productive years. The vast majority of TB deaths are in the developing world, with more than half occurring in Asia.
10 facts about tuberculosis Fact 4 TB is a leading killer among people living with HIV, who have weakened immune systems.
10 facts about tuberculosis Fact 5 There were 9. 27 million new TB cases in 2007, of which 80% were in just 22 countries. Per capita, the global TB incidence rate is falling, but the rate of decline is very slow - less than 1%.
10 facts about tuberculosis Fact 6 TB is a worldwide pandemic. Among the 15 countries with the highest estimated TB incidence rates, 13 are in Africa, while half of all new cases are in six Asian countries (Bangladesh, China, India, Indonesia, Pakistan and the Philippines).
10 facts about tuberculosis Fact 7 Multidrug-resistant TB (MDR-TB) is a form of TB that does not respond to the standard treatments using first-line drugs. MDR-TB is present in virtually all countries surveyed by WHO and its partners.
10 facts about tuberculosis Fact 8 There were an estimated 511 000 new MDR-TB cases in 2007 with three countries accounting for 56% of all cases globally: China, India and the Russian Federation. Extensively drug-resistant TB (XDR-TB) occurs when resistance to second-line drugs develops. It is extremely difficult to treat and cases have been confirmed in more than 50 countries.
10 facts about tuberculosis Fact 9 WHO’s Stop TB Strategy aims to reach all patients and achieve the target under the Millennium Development Goals (MDG): to reduce by 2015 the prevalence of and deaths due to TB by 50% relative to 1990 and reverse the trend in incidence. The strategy emphasizes the need for proper health systems and the importance of effective primary health care to address the TB epidemic.
10 facts about tuberculosis Fact 10 The Global Plan to Stop TB 2006 -2015, launched January 2006, aims to achieve the MDG target with an investment of US$ 67 billion. This represents more than a three-fold increase in investment from 2005. The estimated funding gap is US$ 40 billion.
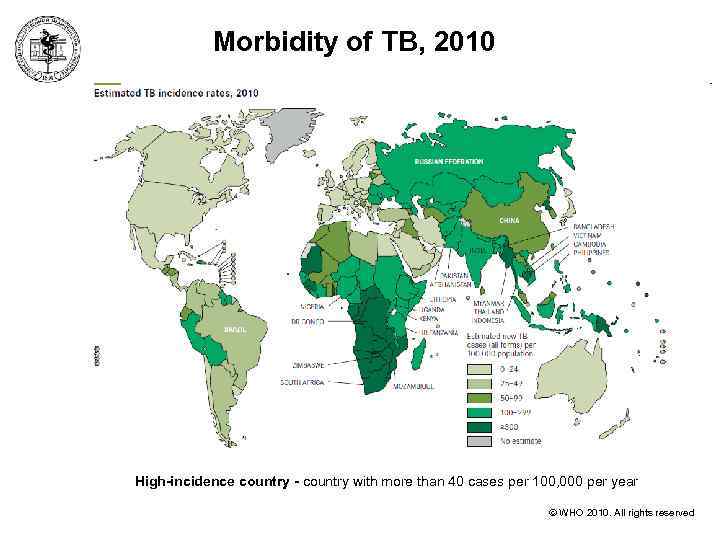
Morbidity of ТВ, 2010 High-incidence country - country with more than 40 cases per 100, 000 per year WHO 2010. All rights reserved
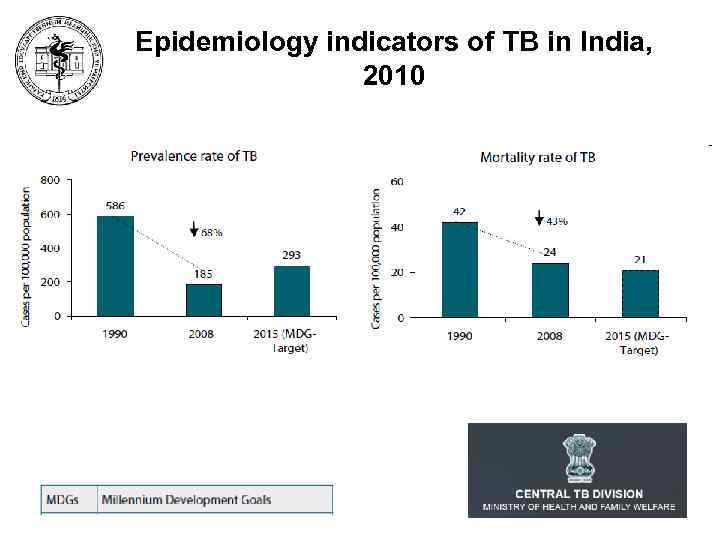
Epidemiology indicators of ТВ in India, 2010
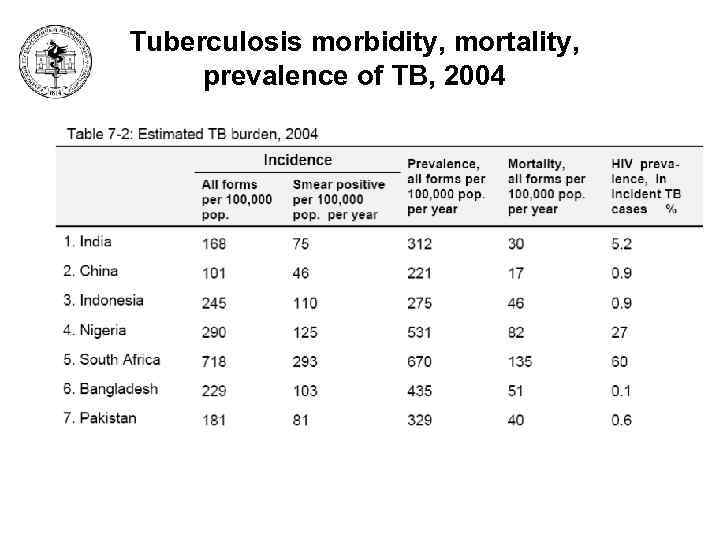
Tuberculosis morbidity, mortality, prevalence of TB, 2004
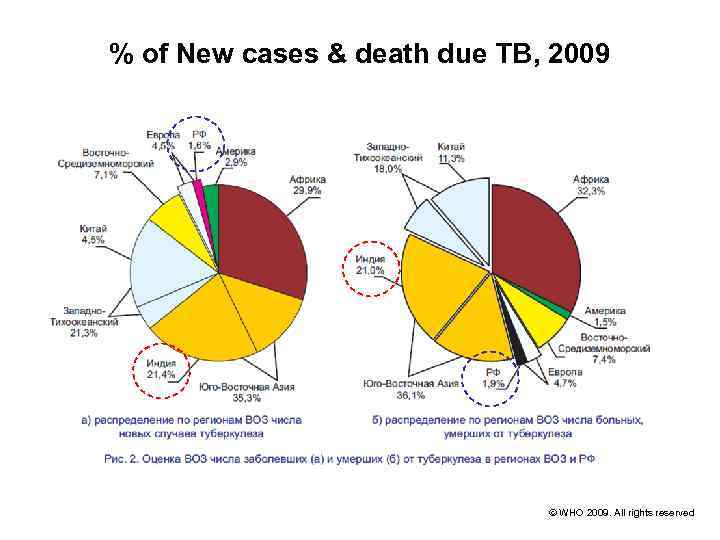
% of New cases & death due ТВ, 2009 WHO 2009. All rights reserved
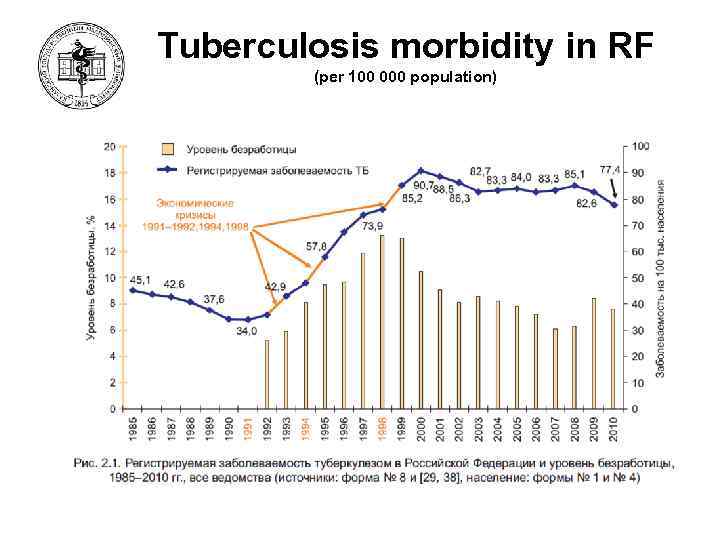
Tuberculosis morbidity in RF (per 100 000 population) 17
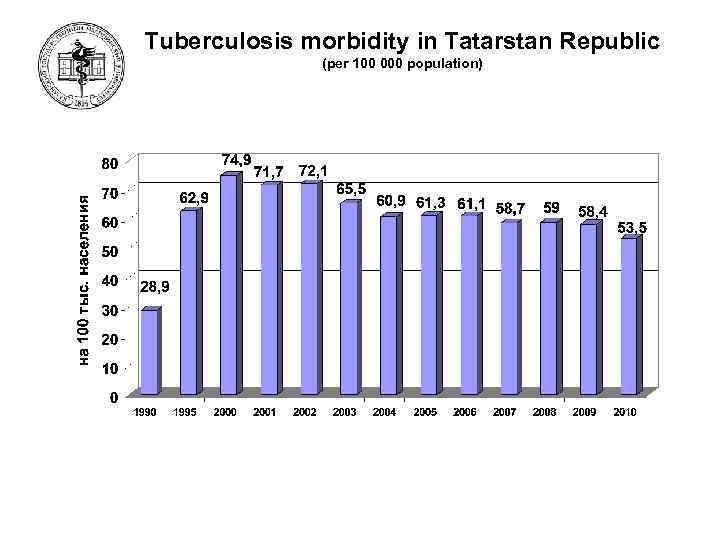
Tuberculosis morbidity in Tatarstan Republic (per 100 000 population) 18
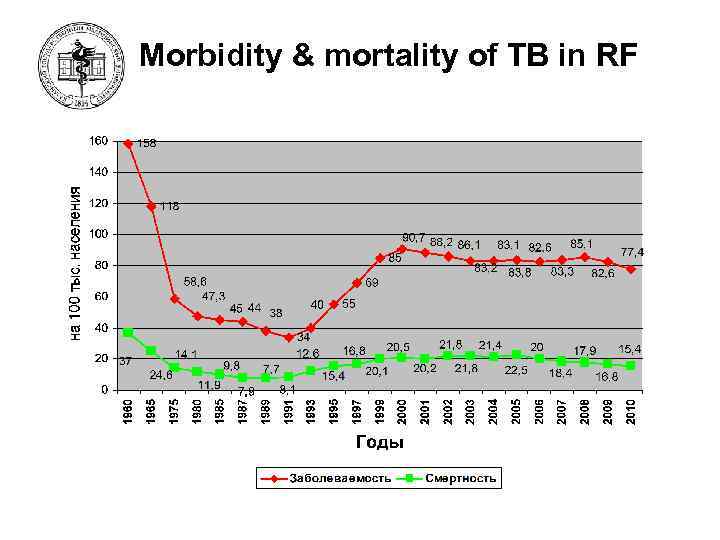
Morbidity & mortality of TB in RF 19
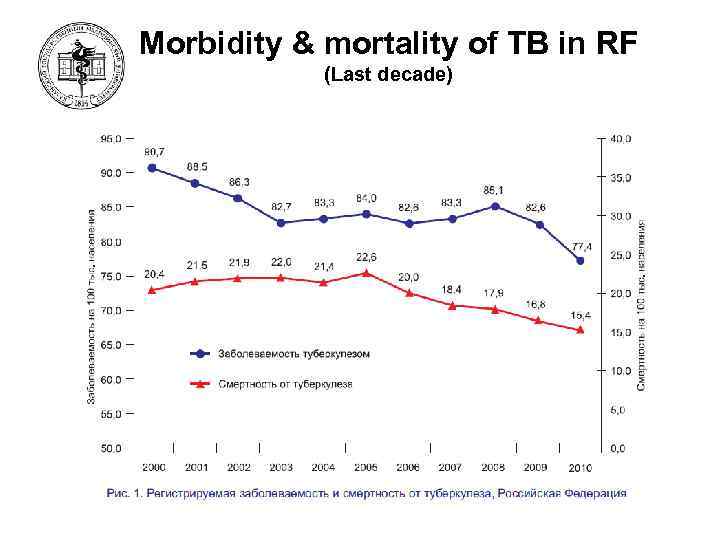
Morbidity & mortality of TB in RF (Last decade) 20

Respiratory and Non-respiratory TB in RF 21 Туберкулез в Российской Федерации, 2007 г. , Аналитический обзор основных статистических показателей по туберкулезу, используемых в Российской Федерации, (под ред. М. И. Перельмана и Ю. В. Михайловой) М. , 2007.
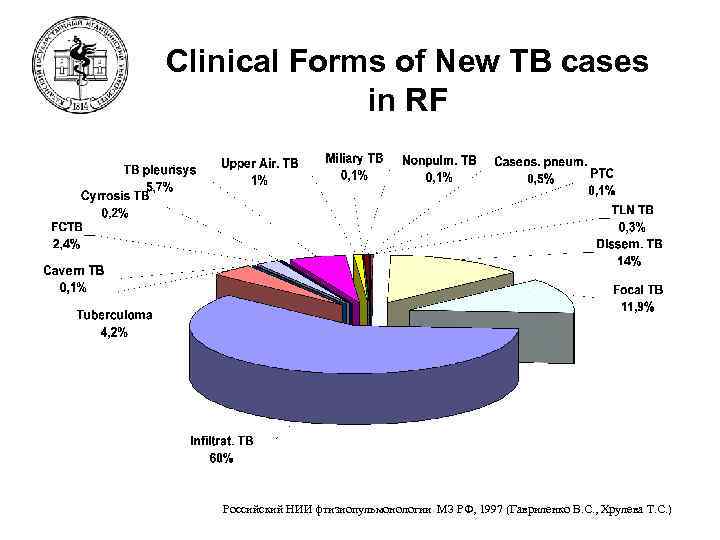
Clinical Forms of New TB cases in RF Российский НИИ фтизиопульмонологии МЗ РФ, 1997 (Гавриленко В. С. , Хрулева Т. С. )
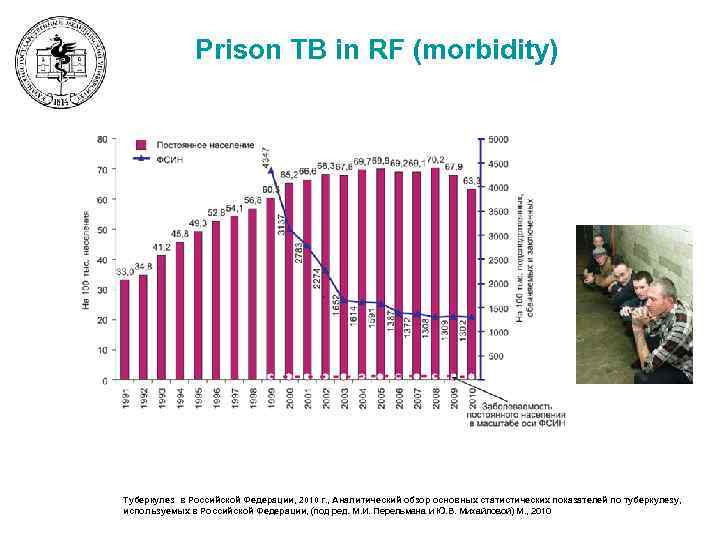
Prison TB in RF (morbidity) 25 Туберкулез в Российской Федерации, 2010 г. , Аналитический обзор основных статистических показателей по туберкулезу, используемых в Российской Федерации, (под ред. М. И. Перельмана и Ю. В. Михайловой) М. , 2010
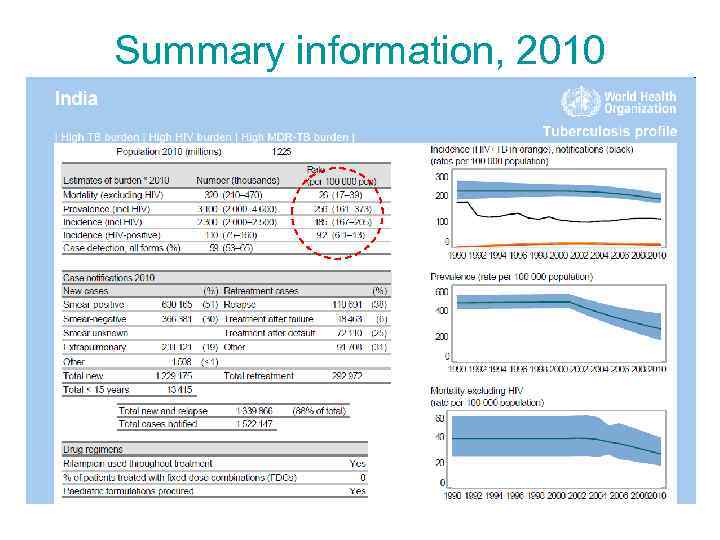
Summary information, 2010 26
Epidemiology of TB • Ways of transmission of infection: – Airborne (main): • 1) through the droplets of sputum from active TB patients (contacts, foci of TB infection (living, staying or working places of SSP TB patient) • 2) through the dust (dry sputum particles) – Alimentary (rare): • consumption of milk from the TB ill cows (M. bovis) • pasteurization of milk – Contact-associated (through the skin) (rare): • through the personal things of SSP TB patient • pathologists, forensic physicians, bacteriologists – Vertical (from mother to child) (very rare)
Factors of transmission of MBT 1. 2. 3. 4. The number of organisms being expelled into the air The concentration of organisms in the determined volume of the space and it’s ventilation The length of time an exposed person breathes the contaminated air The immune status of the exposed individual
Methods of reduction of transmission MBT 1. Ventilation with fresh air: >= 6 room-air changes an hour 2. Ultraviolet irradiation of air in the room 3. Using of masks 4. Isolation of the SSP patients in hospital 5. Treatment SSP TB patients 6. Early diagnosis of TB (TST, Microscopy of sputum, CXR)
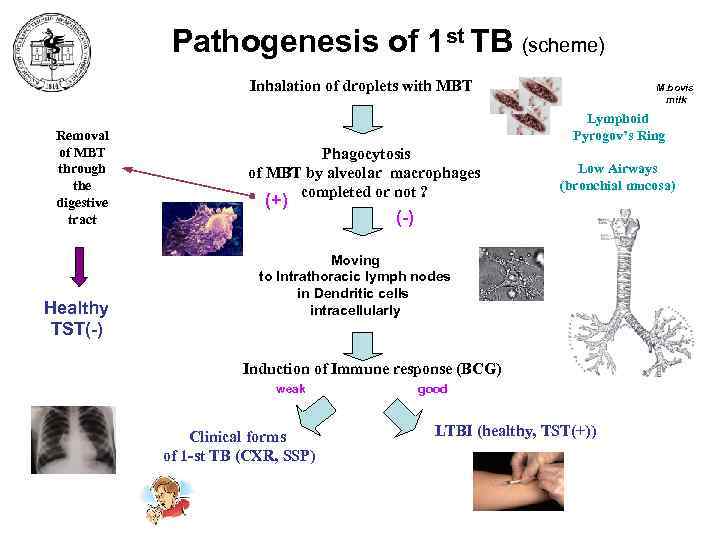
Pathogenesis of 1 st TB (scheme) Inhalation of droplets with MBT Removal of MBT through the digestive tract Healthy TST(-) M. bovis milk Lymphoid Pyrogov’s Ring Phagocytosis of MBT by alveolar macrophages completed or not ? (+) Low Airways (bronchial mucosa) (-) Moving to Intrathoracic lymph nodes in Dendritic cells intracellularly Induction of Immune response (BCG) weak Clinical forms of 1 -st TB (CXR, SSP) good LTBI (healthy, TST(+))
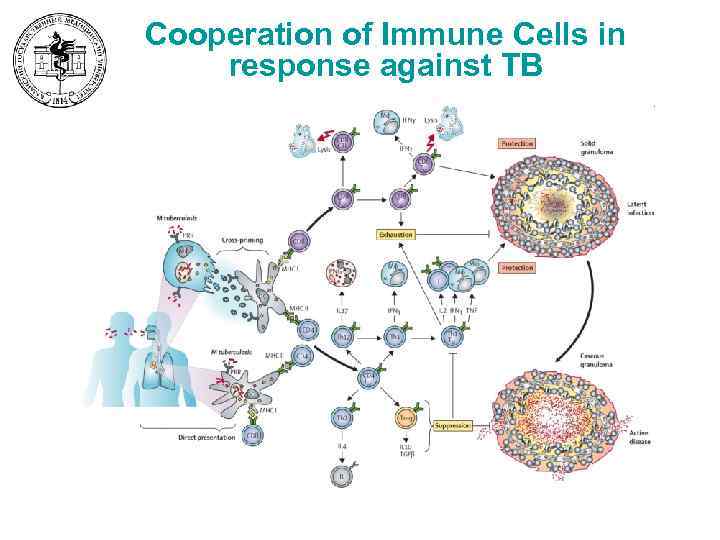
Cooperation of Immune Cells in response against TB
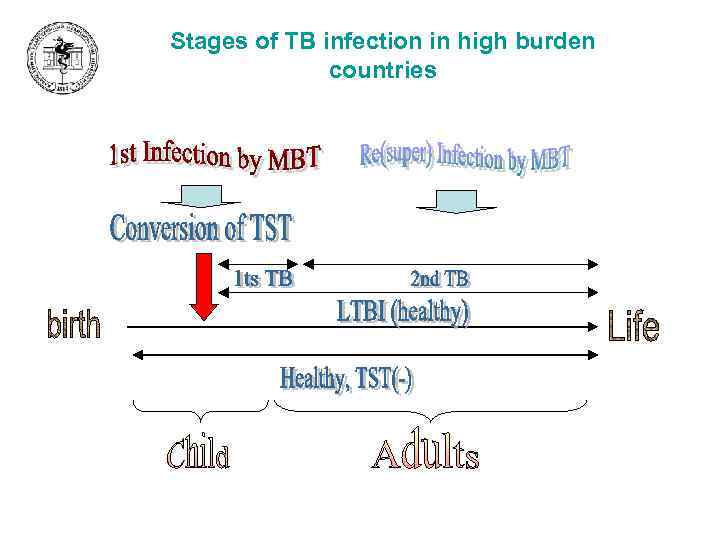
Stages of TB infection in high burden countries
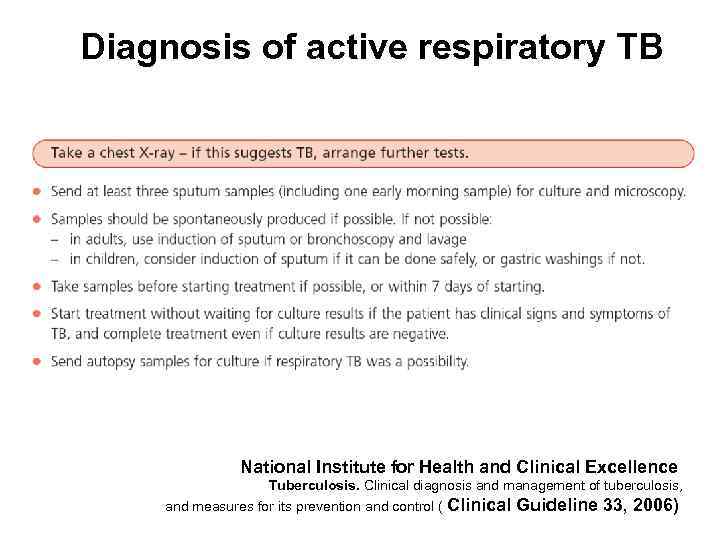
Diagnosis of active respiratory TB National Institute for Health and Clinical Excellence Tuberculosis. Clinical diagnosis and management of tuberculosis, and measures for its prevention and control ( Clinical Guideline 33, 2006)
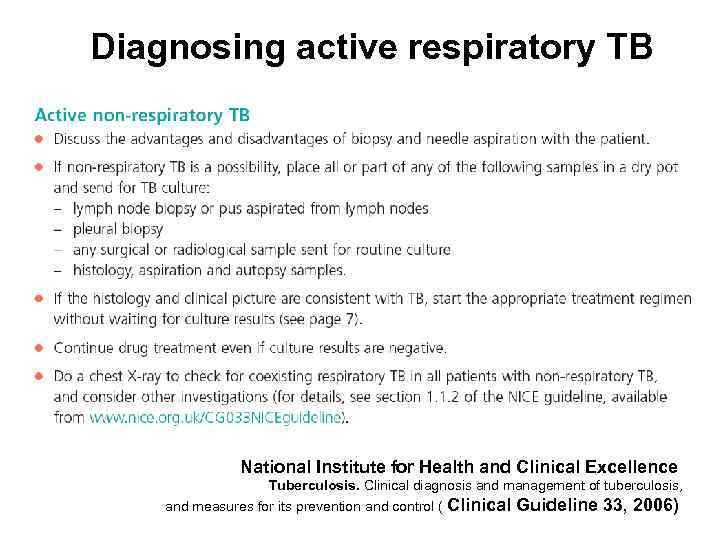
Diagnosing active respiratory TB National Institute for Health and Clinical Excellence Tuberculosis. Clinical diagnosis and management of tuberculosis, and measures for its prevention and control ( Clinical Guideline 33, 2006)
What does it mean for practitioners? ? ? – 1. if this suggests TB, 2. arrange further tests. Take a chest X-ray The point of the Lecture “Diagnosis of TB”
TB Diagnosis – General aspects • • • TB – infectious disease (microbiology investigation) TB localization (dominantly in lung – CXR investigation) Variety of clinical forms (features of clinical manifestation) Age features (primary TB < 5%) Diagnosis of 1 st and 2 nd TB (TST and chest X-ray) Groups at Risk for TB (Who is ill more often? )
Diagnosis of TB • Patient’s history (clinical features) – Anamnesis – Symptoms • Physical examination – auscultation, percussion, palpation • • • Chest X-ray (fluorography, tomography) Microbiology examination Full blood count Tuberculin skin test, Gamma-Interferon test Lung Function Tests Histology investigation
Anamnesis (aspects) • Symptoms • History of Disease – – – onset (acute, subacute (gradual), asymptomatic) duration of disease method of revealing diagnostic path (Where? When? Who? ) previous treatment • Masks of TB (chronic cough) • Epidemiologic anamnesis • Group of high risk

Clinical Forms of New TB cases in RF Российский НИИ фтизиопульмонологии МЗ РФ, 1997 (Гавриленко В. С. , Хрулева Т. С. )
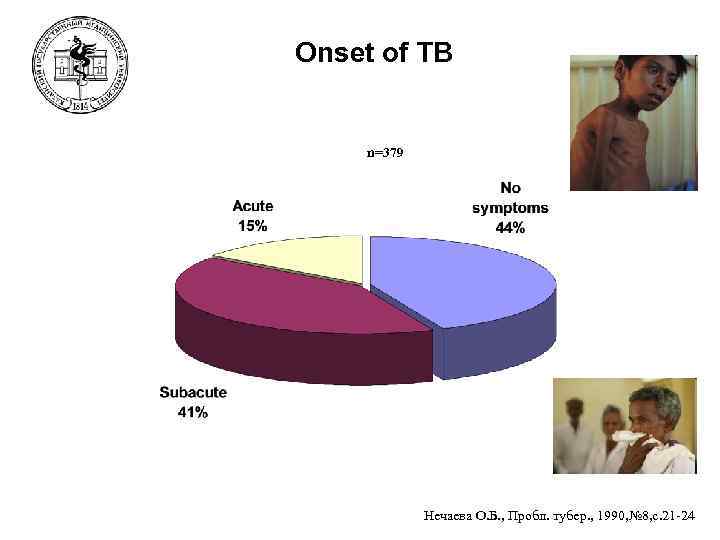
Onset of TB n=379 Нечаева О. Б. , Пробл. тубер. , 1990, № 8, с. 21 -24
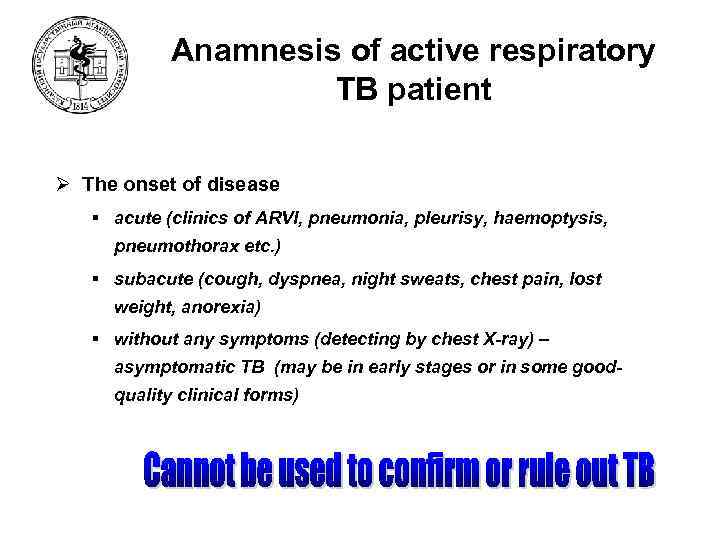
Anamnesis of active respiratory TB patient Ø The onset of disease § acute (clinics of ARVI, pneumonia, pleurisy, haemoptysis, pneumothorax etc. ) § subacute (cough, dyspnea, night sweats, chest pain, lost weight, anorexia) § without any symptoms (detecting by chest X-ray) – asymptomatic TB (may be in early stages or in some goodquality clinical forms)
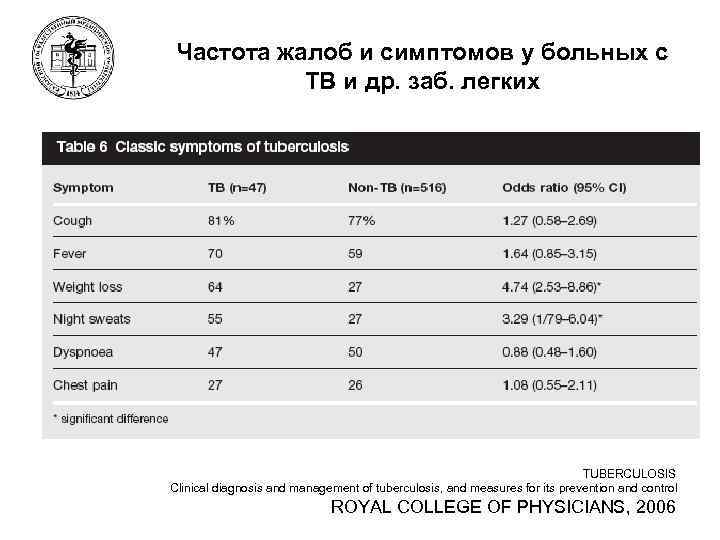
Частота жалоб и симптомов у больных с ТВ и др. заб. легких TUBERCULOSIS Clinical diagnosis and management of tuberculosis, and measures for its prevention and control ROYAL COLLEGE OF PHYSICIANS, 2006
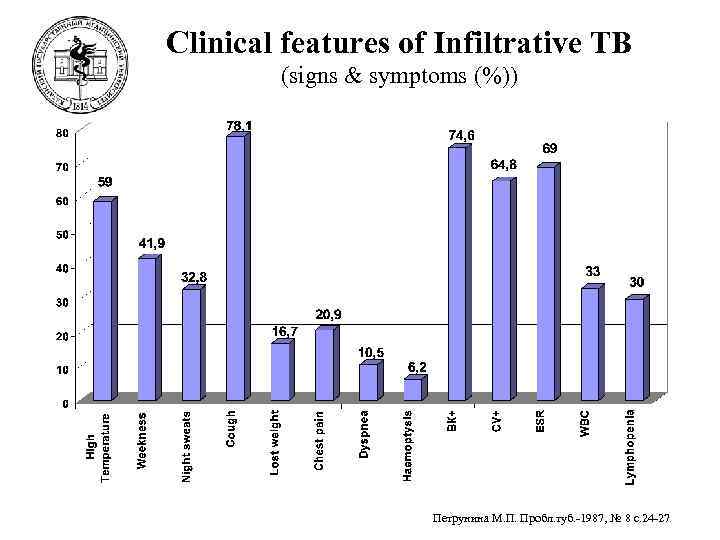
Clinical features of Infiltrative TB (signs & symptoms (%)) Петрунина М. П. Пробл. туб. -1987, № 8 с. 24 -27
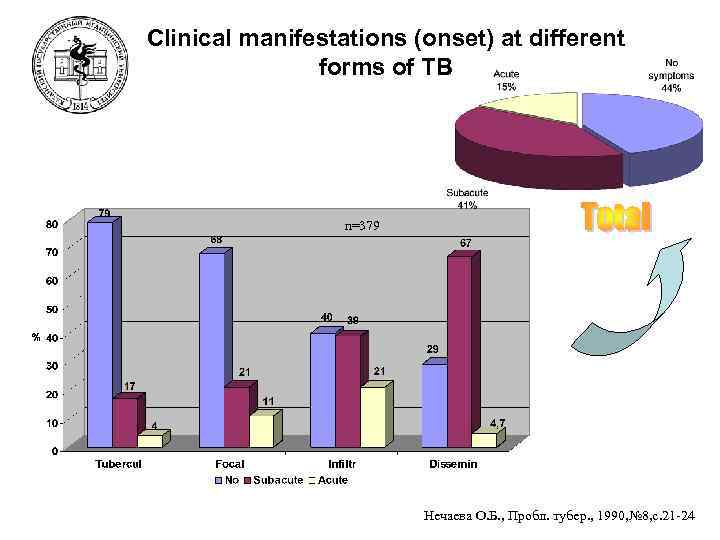
Clinical manifestations (onset) at different forms of TB n=379 Нечаева О. Б. , Пробл. тубер. , 1990, № 8, с. 21 -24
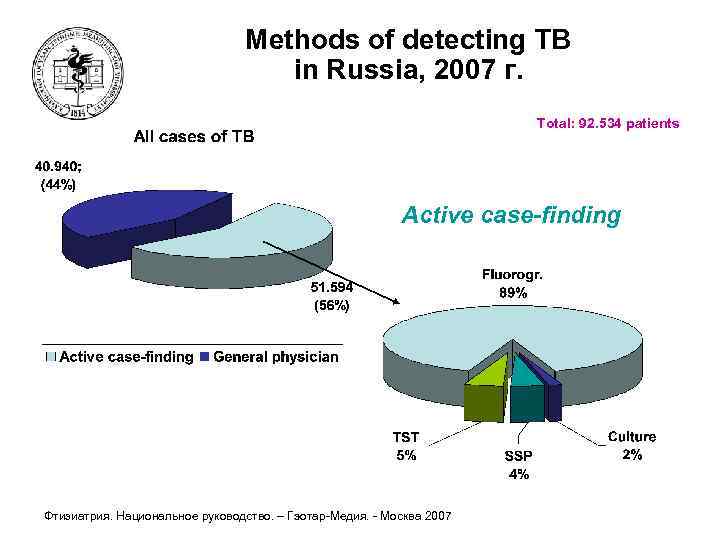
Methods of detecting TB in Russia, 2007 г. Total: 92. 534 patients Active case-finding Фтизиатрия. Национальное руководство. – Гэотар-Медия. - Москва 2007
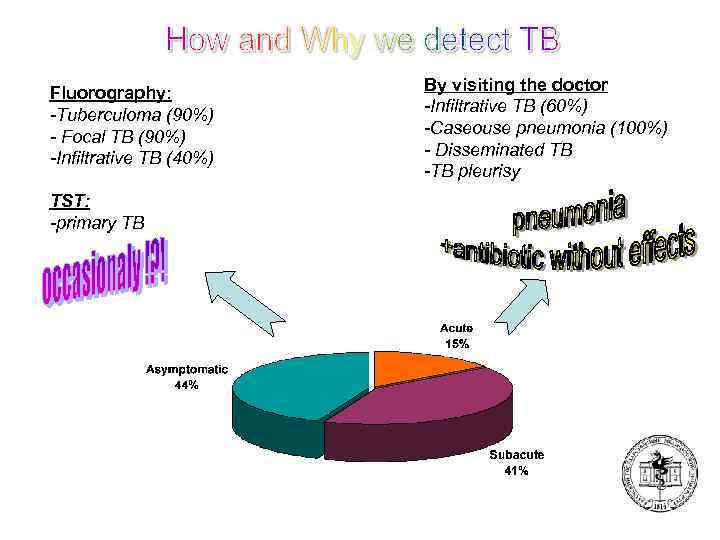
Fluorography: -Tuberculoma (90%) - Focal TB (90%) -Infiltrative TB (40%) TST: -primary TB By visiting the doctor -Infiltrative TB (60%) -Caseouse pneumonia (100%) - Disseminated TB -TB pleurisy
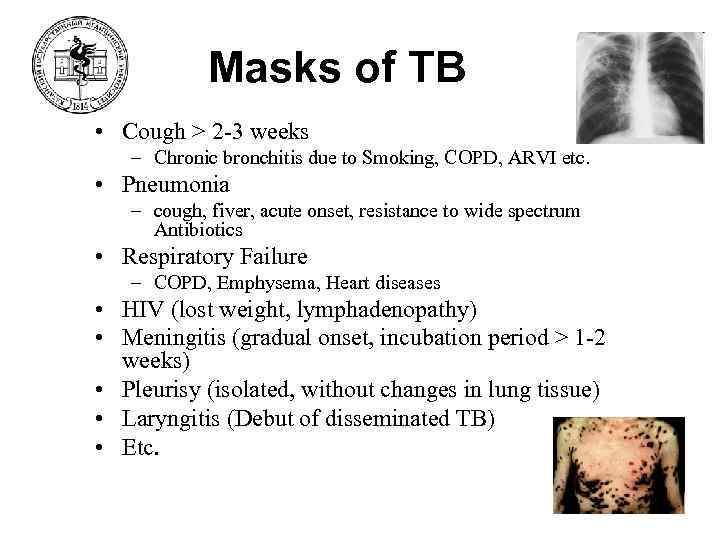
Masks of TB • Cough > 2 -3 weeks – Chronic bronchitis due to Smoking, COPD, ARVI etc. • Pneumonia – cough, fiver, acute onset, resistance to wide spectrum Antibiotics • Respiratory Failure – COPD, Emphysema, Heart diseases • HIV (lost weight, lymphadenopathy) • Meningitis (gradual onset, incubation period > 1 -2 weeks) • Pleurisy (isolated, without changes in lung tissue) • Laryngitis (Debut of disseminated TB) • Etc.
Groups of high risk • Are the students of KSMU in group of risk for TB ? – – – 1 -2 New cases of TB per year Number of students in KSMU = 4. 000 Morbidity = number NCTB /100 000 population Morbidity in RT - 50 per 100 000 pop. Morbidity ? 100. 000 / 4. 000 = 25 (1 -2) * 25 = (25 -50) per 100 000 students – No!!!
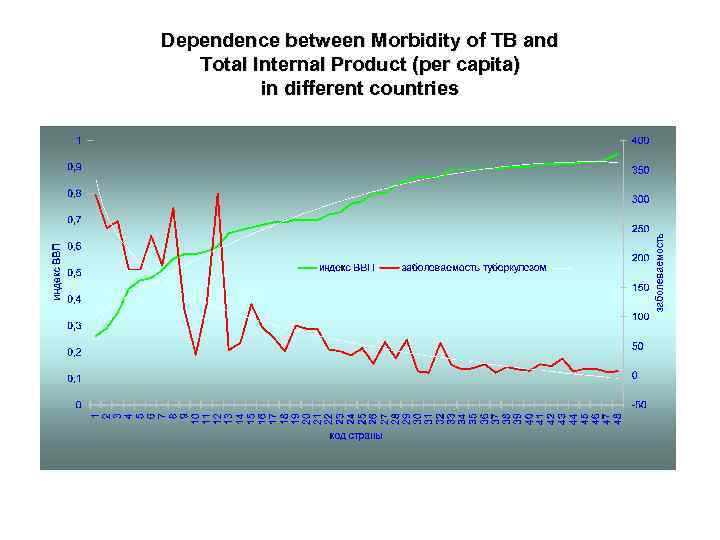
Dependence between Morbidity of TB and Total Internal Product (per capita) in different countries
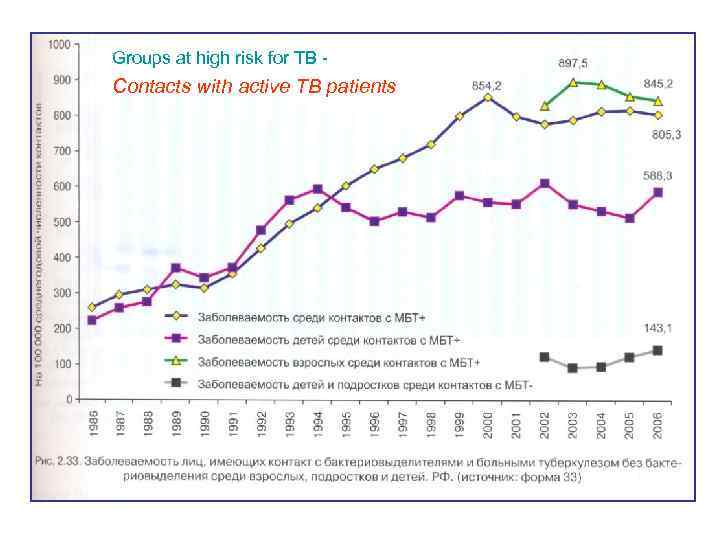
Groups at high risk for TB - Contacts with active TB patients
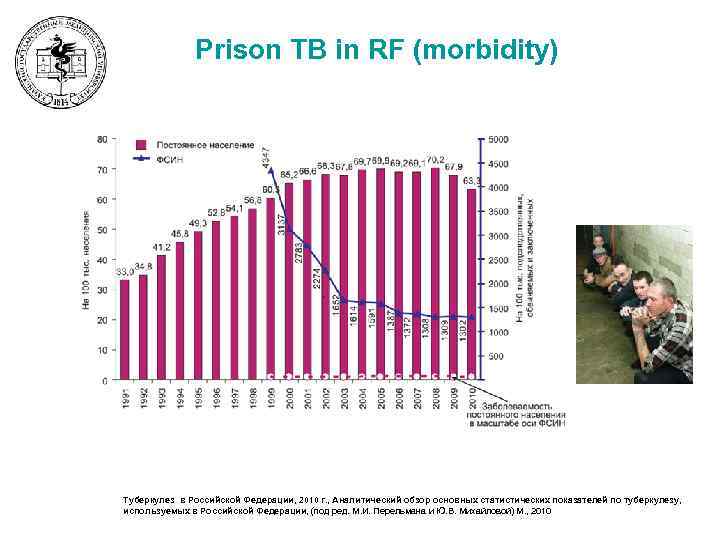
Prison TB in RF (morbidity) 51 Туберкулез в Российской Федерации, 2010 г. , Аналитический обзор основных статистических показателей по туберкулезу, используемых в Российской Федерации, (под ред. М. И. Перельмана и Ю. В. Михайловой) М. , 2010
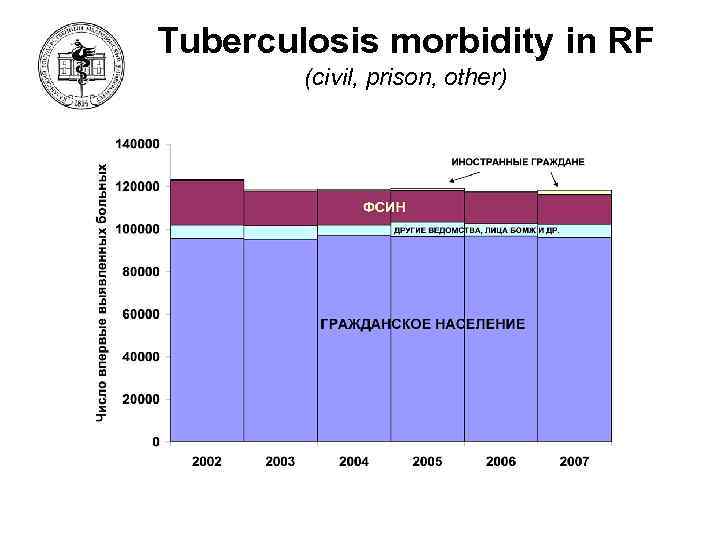
Tuberculosis morbidity in RF (civil, prison, other) 52
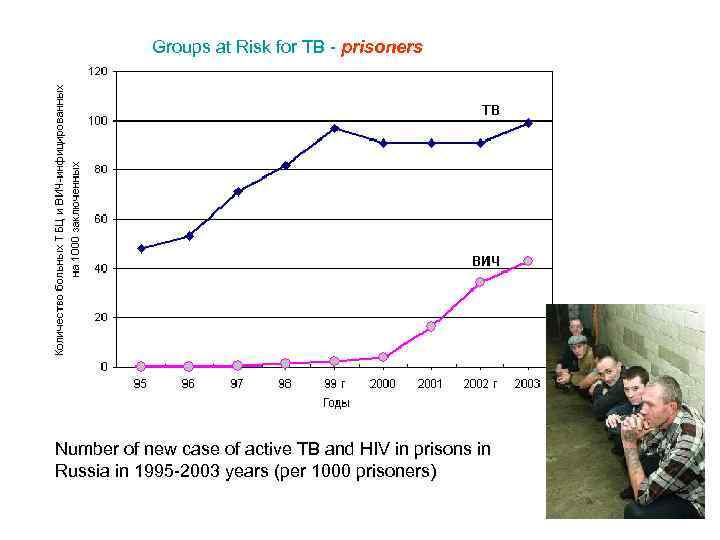
Groups at Risk for TB - prisoners Number of new case of active TB and HIV in prisons in Russia in 1995 -2003 years (per 1000 prisoners)
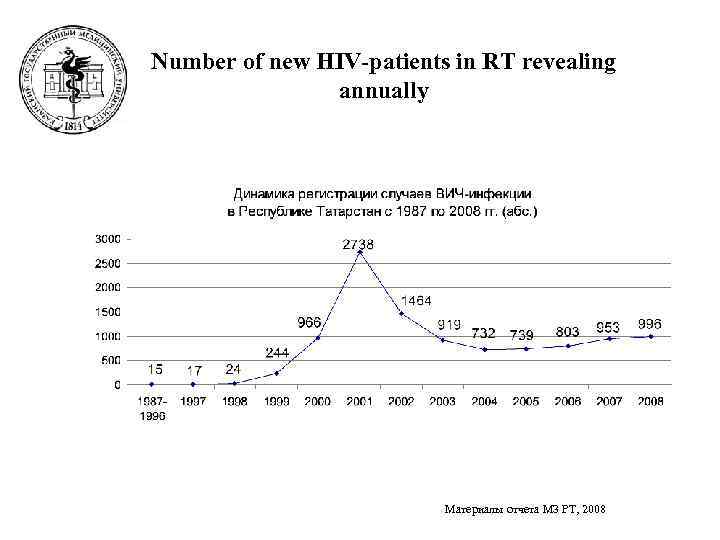
Number of new HIV-patients in RT revealing annually Материалы отчета МЗ РТ, 2008
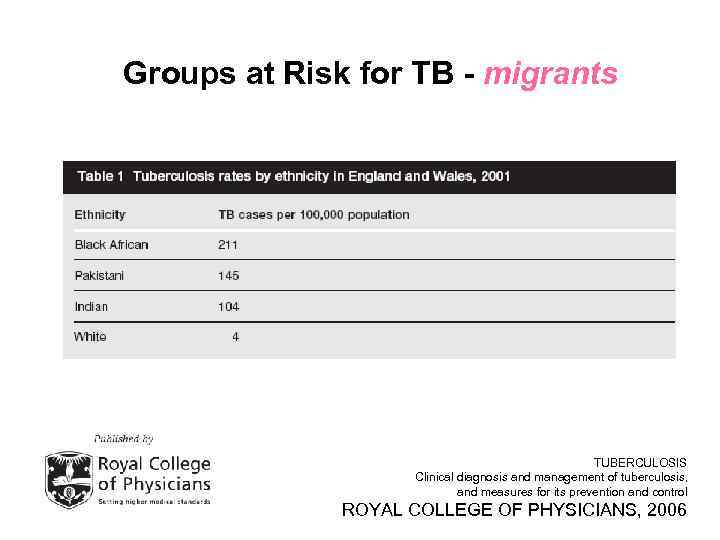
Groups at Risk for TB - migrants TUBERCULOSIS Clinical diagnosis and management of tuberculosis, and measures for its prevention and control ROYAL COLLEGE OF PHYSICIANS, 2006
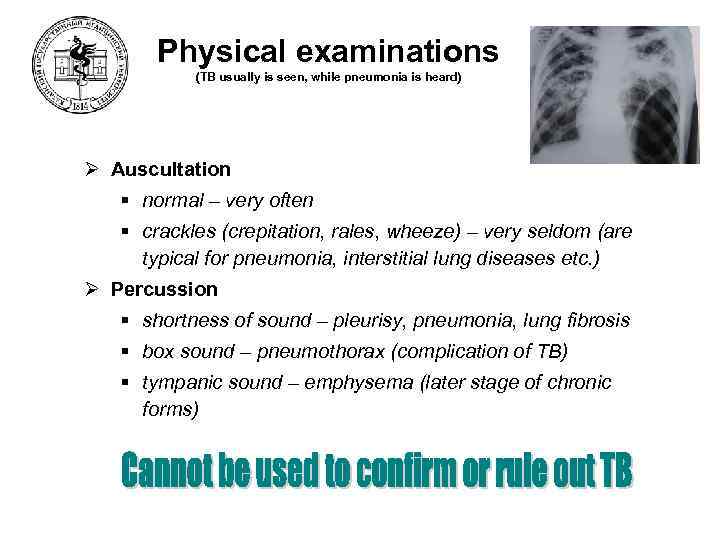
Physical examinations (TB usually is seen, while pneumonia is heard) Ø Auscultation § normal – very often § crackles (crepitation, rales, wheeze) – very seldom (are typical for pneumonia, interstitial lung diseases etc. ) Ø Percussion § shortness of sound – pleurisy, pneumonia, lung fibrosis § box sound – pneumothorax (complication of TB) § tympanic sound – emphysema (later stage of chronic forms)
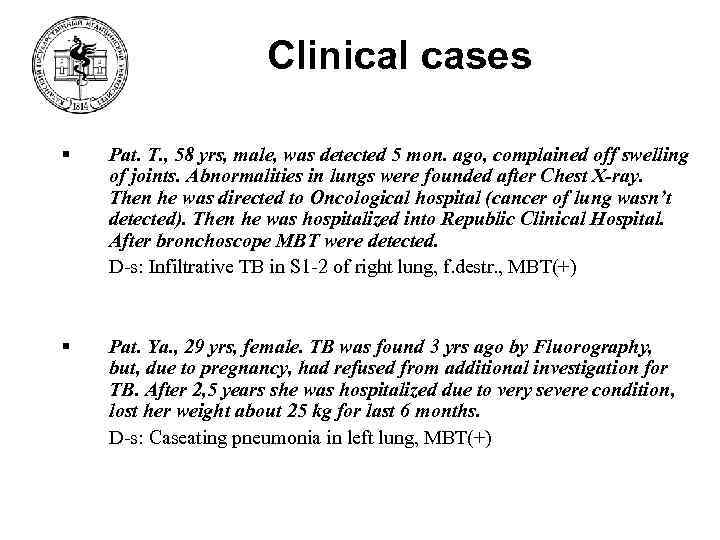
Clinical cases § Pat. Т. , 58 yrs, male, was detected 5 mon. ago, complained off swelling of joints. Abnormalities in lungs were founded after Chest X-ray. Then he was directed to Oncological hospital (cancer of lung wasn’t detected). Then he was hospitalized into Republic Clinical Hospital. After bronchoscope MBT were detected. D-s: Infiltrative TB in S 1 -2 of right lung, f. destr. , MBT(+) § Pat. Ya. , 29 yrs, female. TB was found 3 yrs ago by Fluorography, but, due to pregnancy, had refused from additional investigation for TB. After 2, 5 years she was hospitalized due to very severe condition, lost her weight about 25 kg for last 6 months. D-s: Caseating pneumonia in left lung, MBT(+)
Clinical cases § Pat. С. , 40 yrs, male, was detected by fluorography. Any of clinical manifestations of TB were absent. D-s: Infiltrative TB in S 1 -2 of right lung § Pat. С. , 52 yrs, male, was detected due to occasional haemoptysis, cough, pleuritic pain. After Chest X-ray he was directed to TB hospital. D-s: Disseminative TB of lungs, secondary TB pleurisy
Clinical cases § Pat. M. , 30 yrs, male. TB was found by prophylactic fluorography due to employment. Was hospitalized into Central District Hospital with diagnosis Communityacquired Pneumonia. He was treated by antibiotics for 2 weeks without any clinical effects. Then he was directed to Republic TB Hospital. Complaint off a cough, fatigue. D-s: Infiltrative TB in S 6 of right lung, f. destr. , MBT(+) § Pat. D, 55 yrs, nurse in TB Hospital. TB was found by prophylactic fluorography 13 mon. ago (Tuberculoma in S 2 of left lung). Symptoms of TB were absent. 12 mon. after mass in lung was enlarged. D-s: Tuberculoma in S 6 of left lung, f. destr.
Clinical cases • Pat. M. , 35 yrs, male. TB was found 7 mon. ago due to complaints off dyspnea for 1 yrs, haemoptysis, weight lost. Chest X-ray wasn’t performed for more then 5 yrs. D-s: infiltrative TB in left and right lungs, f. destr, MBT(+) • Pat. Ch. , 49 yrs, female. She was detected due to fever (38, 5 С), dyspnea. Fluorography was performed 1, 5 yrs ago. Out-patient doctor administered aspirin, biseptol (without any clinical effect). After treatment TB was found by Chest X-ray. D-s: infiltrative TB in S 1 of right lung
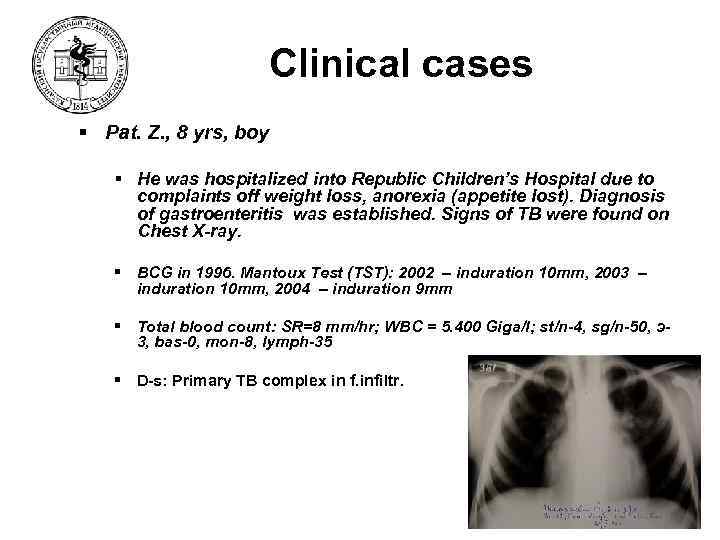
Clinical cases § Pat. Z. , 8 yrs, boy § He was hospitalized into Republic Children’s Hospital due to complaints off weight loss, anorexia (appetite lost). Diagnosis of gastroenteritis was established. Signs of TB were found on Chest X-ray. § BCG in 1996. Mantoux Test (TST): 2002 – induration 10 mm, 2003 – induration 10 mm, 2004 – induration 9 mm § Total blood count: SR=8 mm/hr; WBC = 5. 400 Giga/l; st/n-4, sg/n-50, э3, bas-0, mon-8, lymph-35 § D-s: Primary TB complex in f. infiltr.
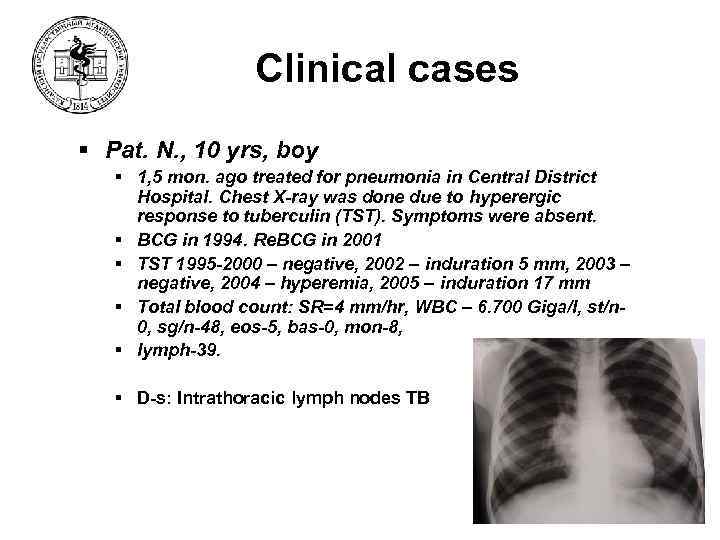
Clinical cases § Pat. N. , 10 yrs, boy § 1, 5 mon. ago treated for pneumonia in Central District Hospital. Chest X-ray was done due to hyperergic response to tuberculin (TST). Symptoms were absent. § BCG in 1994. Re. BCG in 2001 § TST 1995 -2000 – negative, 2002 – induration 5 mm, 2003 – negative, 2004 – hyperemia, 2005 – induration 17 mm § Total blood count: SR=4 mm/hr, WBC – 6. 700 Giga/l, st/n 0, sg/n-48, eos-5, bas-0, mon-8, § lymph-39. § D-s: Intrathoracic lymph nodes TB
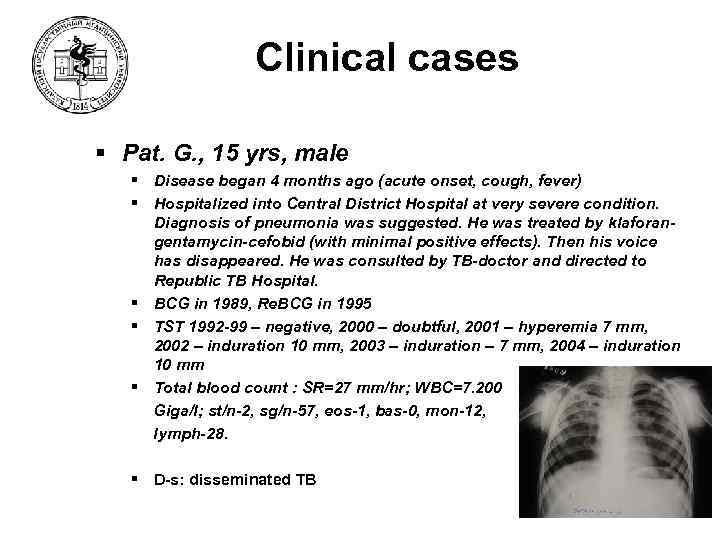
Clinical cases § Pat. G. , 15 yrs, male § Disease began 4 months ago (acute onset, cough, fever) § Hospitalized into Central District Hospital at very severe condition. Diagnosis of pneumonia was suggested. He was treated by klaforangentamycin-cefobid (with minimal positive effects). Then his voice has disappeared. He was consulted by TB-doctor and directed to Republic TB Hospital. § BCG in 1989, Re. BCG in 1995 § TST 1992 -99 – negative, 2000 – doubtful, 2001 – hyperemia 7 mm, 2002 – induration 10 mm, 2003 – induration – 7 mm, 2004 – induration 10 mm § Total blood count : SR=27 mm/hr; WBC=7. 200 Giga/l; st/n-2, sg/n-57, eos-1, bas-0, mon-12, lymph-28. § D-s: disseminated TB
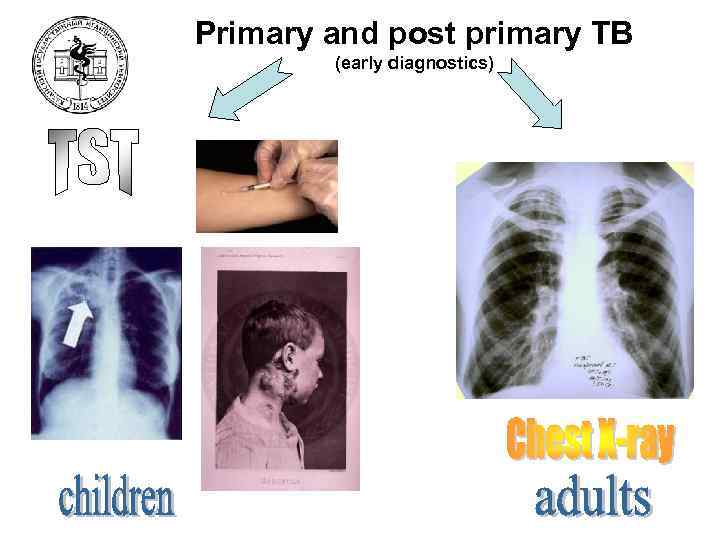
Primary and post primary TB (early diagnostics)
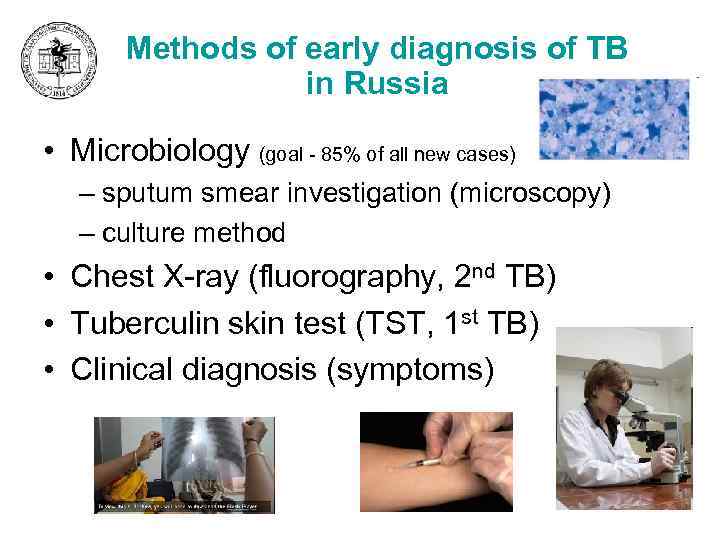
Methods of early diagnosis of TB in Russia • Microbiology (goal - 85% of all new cases) – sputum smear investigation (microscopy) – culture method • Chest X-ray (fluorography, 2 nd TB) • Tuberculin skin test (TST, 1 st TB) • Clinical diagnosis (symptoms)
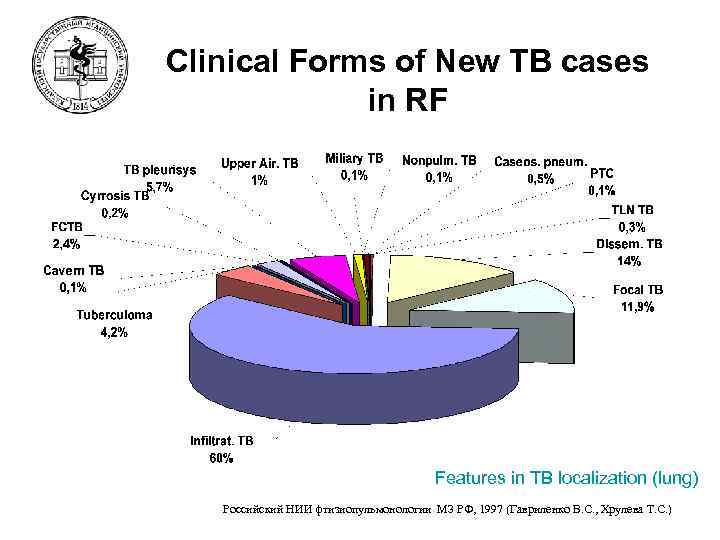
Clinical Forms of New TB cases in RF Features in TB localization (lung) Российский НИИ фтизиопульмонологии МЗ РФ, 1997 (Гавриленко В. С. , Хрулева Т. С. )
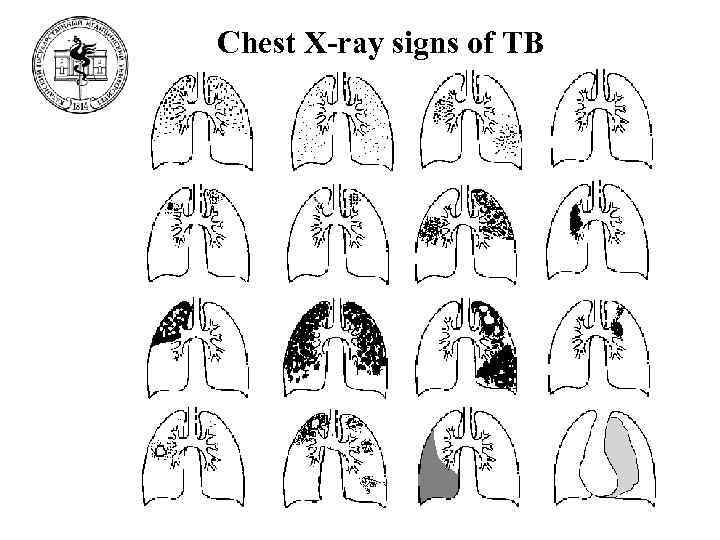
Chest X-ray signs of TB
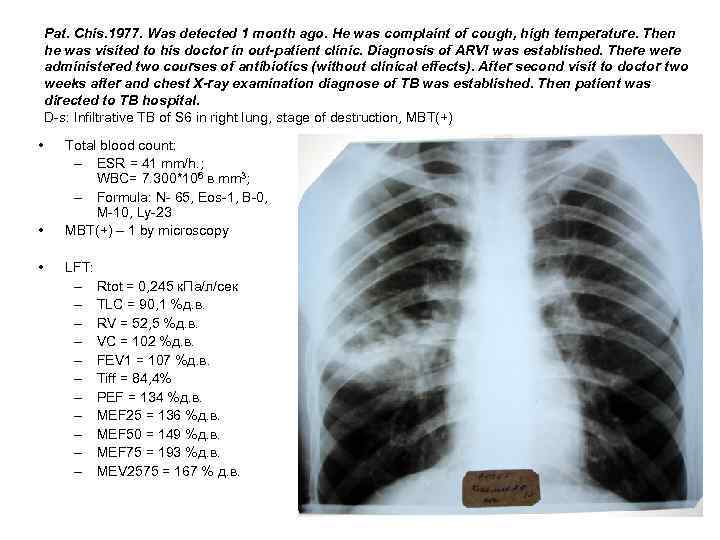
Pat. Chis. 1977. Was detected 1 month ago. He was complaint of cough, high temperature. Then he was visited to his doctor in out-patient clinic. Diagnosis of ARVI was established. There were administered two courses of antibiotics (without clinical effects). After second visit to doctor two weeks after and chest X-ray examination diagnose of TB was established. Then patient was directed to TB hospital. D-s: Infiltrative TB of S 6 in right lung, stage of destruction, MBT(+) • • • Total blood count: – ESR = 41 mm/h. ; WBC= 7. 300*106 в mm 3; – Formula: N- 65, Eos-1, B-0, М-10, Ly-23 MBT(+) – 1 by microscopy LFT: – Rtot = 0, 245 к. Па/л/сек – TLC = 90, 1 %д. в. – RV = 52, 5 %д. в. – VC = 102 %д. в. – FEV 1 = 107 %д. в. – Tiff = 84, 4% – PEF = 134 %д. в. – MEF 25 = 136 %д. в. – MEF 50 = 149 %д. в. – MEF 75 = 193 %д. в. – MEV 2575 = 167 % д. в.
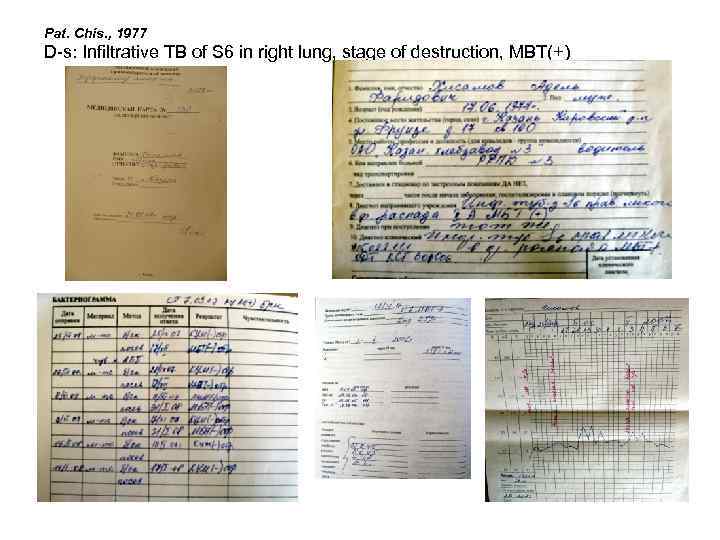
Pat. Chis. , 1977 D-s: Infiltrative TB of S 6 in right lung, stage of destruction, MBT(+)
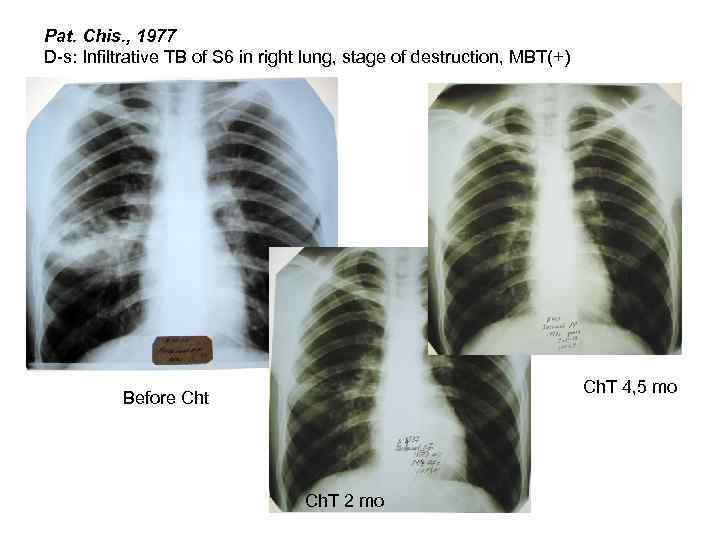
Pat. Chis. , 1977 D-s: Infiltrative TB of S 6 in right lung, stage of destruction, MBT(+) Ch. T 4, 5 mo Before Cht Ch. Т 2 mo
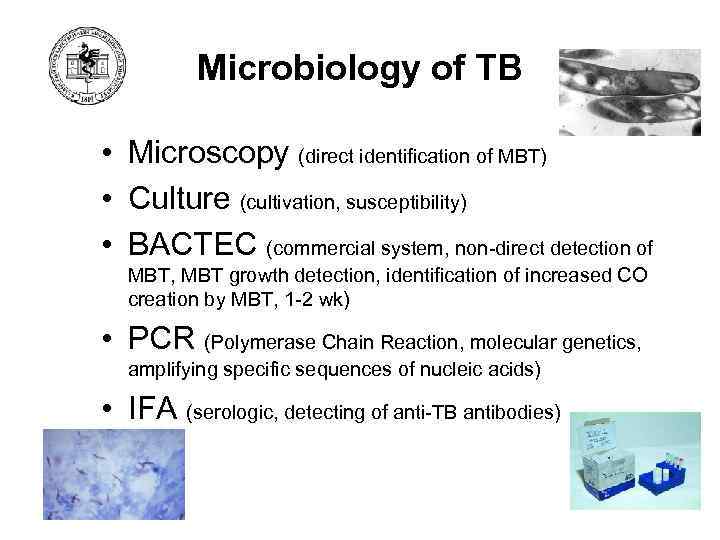
Microbiology of TB • Microscopy (direct identification of MBT) • Culture (cultivation, susceptibility) • BACTEC (commercial system, non-direct detection of MBT, MBT growth detection, identification of increased CO creation by MBT, 1 -2 wk) • PCR (Polymerase Chain Reaction, molecular genetics, amplifying specific sequences of nucleic acids) • IFA (serologic, detecting of anti-TB antibodies)
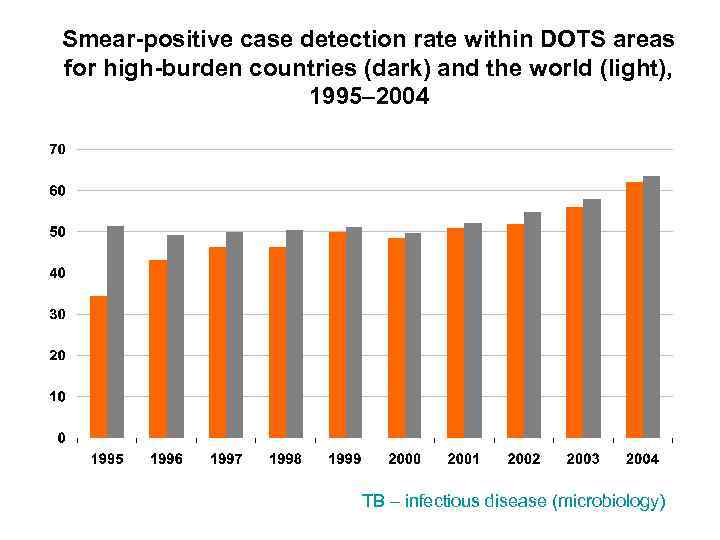
Smear-positive case detection rate within DOTS areas for high-burden countries (dark) and the world (light), 1995– 2004 TB – infectious disease (microbiology)
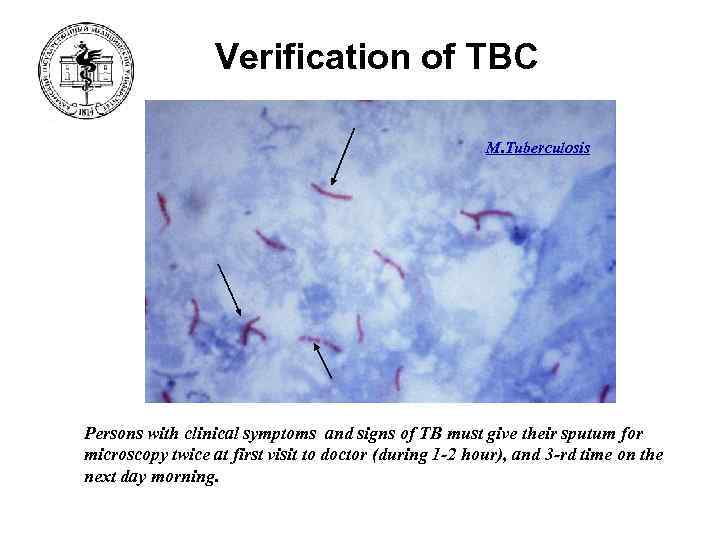
Verification of ТВС M. Tuberculosis Persons with clinical symptoms and signs of TB must give their sputum for microscopy twice at first visit to doctor (during 1 -2 hour), and 3 -rd time on the next day morning.
M. tuberculosis complex • M. tuberculosis (humanus) – human type, causes 85% of all new cases of TB in humans, is transmittes through the airborne route and there are no known animal reservoirs. • M. bovis – bovinus type, causes 10 -15% of all new cases of TB, localization in gastrointestinal tract and lymph nodes. Penetration through the mucosa of oropharynx when ingested in milk containing large number of organism. The origin of BCG-vaccine strain. • M. africanum – the reason of 90% of new cases of TB in South Africa. • M. microti – mouse type. Very rarely in humans. • M. cannetti
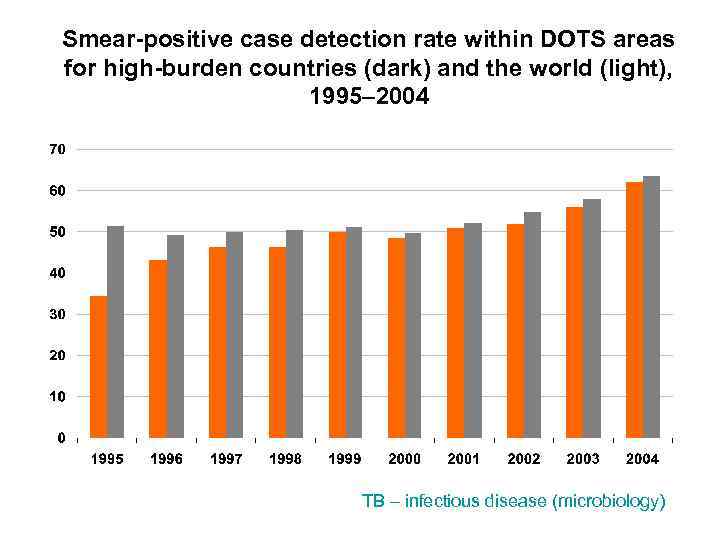
Smear-positive case detection rate within DOTS areas for high-burden countries (dark) and the world (light), 1995– 2004 TB – infectious disease (microbiology)
Sputum Microscopy (general ideas) • M. tuberculosis & DOTS (program of WHO against TB) – dependence between Morbidity of TB & number of SSP TB persons – all attention should be pay to SSP patients – main microbiology method is Microscopy of MBT • Only 60 -70% of TB patients are SSP • At least 3 samples (not saliva, by productive cough) • Bronchial washings, BAL (bronchoalveolar lavage) • Induced sputum (inhalation of hypertonic saline, (Na. Cl 315% solution) by ultrasonic nebulizer)
Sputum Microscopy (Ziehl-Neelsen) • Advantages – – Simple Inexpensive Fast (half an hour) High Clinical value • Disadvantages – Limited sensitivity (5. 000 -10. 000 BK / ml sputum) • At least 3 samples (not saliva, productive cough) • Bronchial washings, BAL (broncho-alveolar lavage) • Induced sputum (inhalation of hypertonic saline, (Na. Cl 3 -15% solution) by ultrasonic nebulizer)
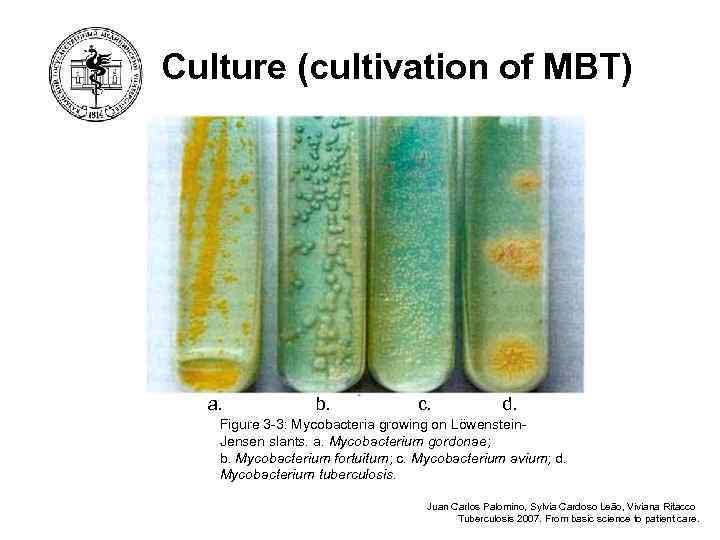
Culture (cultivation of MBT) a. b. c. d. Figure 3 -3: Mycobacteria growing on Löwenstein. Jensen slants. a. Mycobacterium gordonae; b. Mycobacterium fortuitum; c. Mycobacterium avium; d. Mycobacterium tuberculosis. Juan Carlos Palomino, Sylvia Cardoso Leão, Viviana Ritacco Tuberculosis 2007. From basic science to patient care.
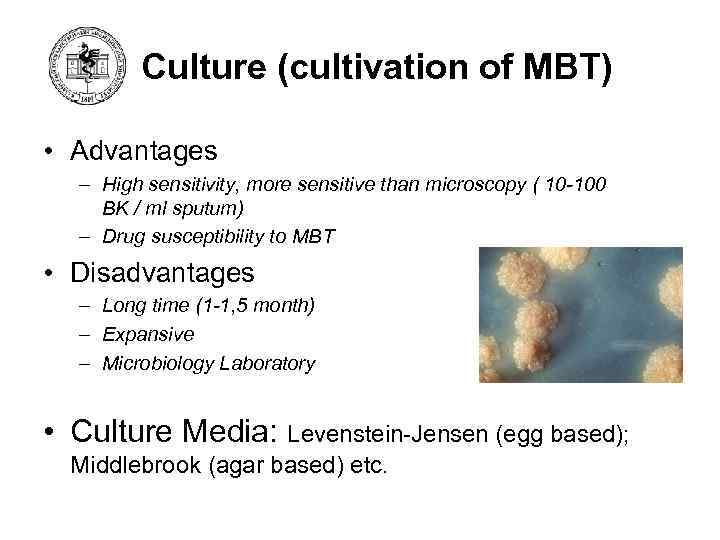
Culture (cultivation of MBT) • Advantages – High sensitivity, more sensitive than microscopy ( 10 -100 BK / ml sputum) – Drug susceptibility to MBT • Disadvantages – Long time (1 -1, 5 month) – Expansive – Microbiology Laboratory • Culture Media: Levenstein-Jensen (egg based); Middlebrook (agar based) etc.
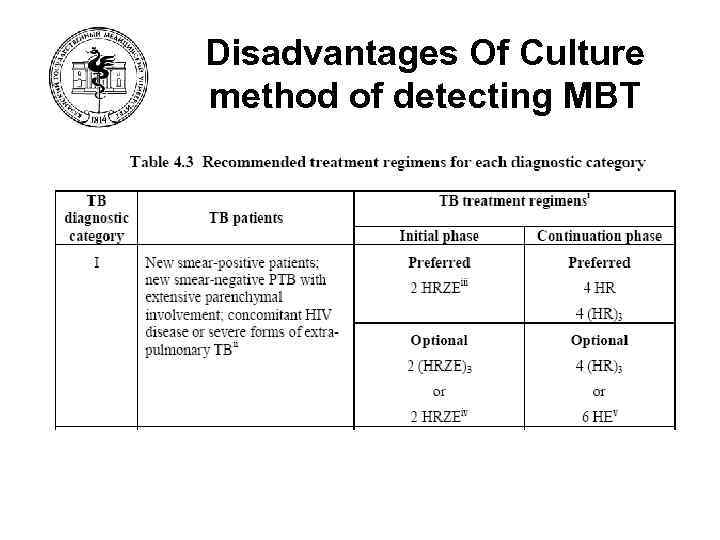
Disadvantages Of Culture method of detecting MBT
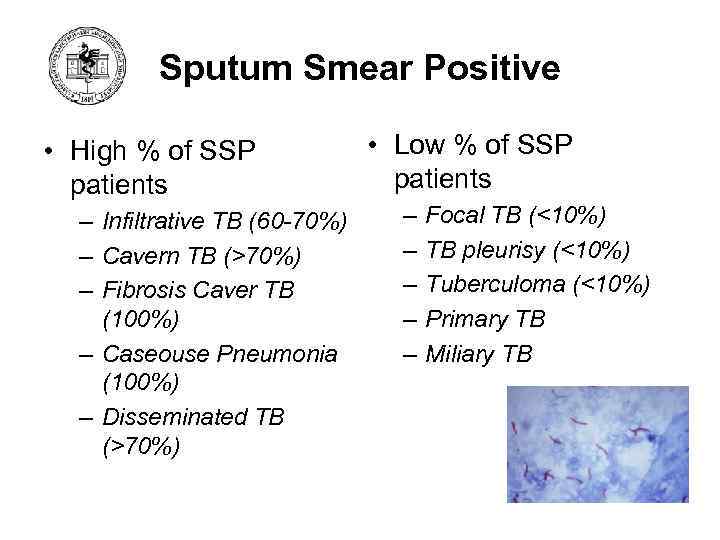
Sputum Smear Positive • High % of SSP patients – Infiltrative TB (60 -70%) – Cavern TB (>70%) – Fibrosis Caver TB (100%) – Caseouse Pneumonia (100%) – Disseminated TB (>70%) • Low % of SSP patients – – – Focal TB (<10%) TB pleurisy (<10%) Tuberculoma (<10%) Primary TB Miliary TB
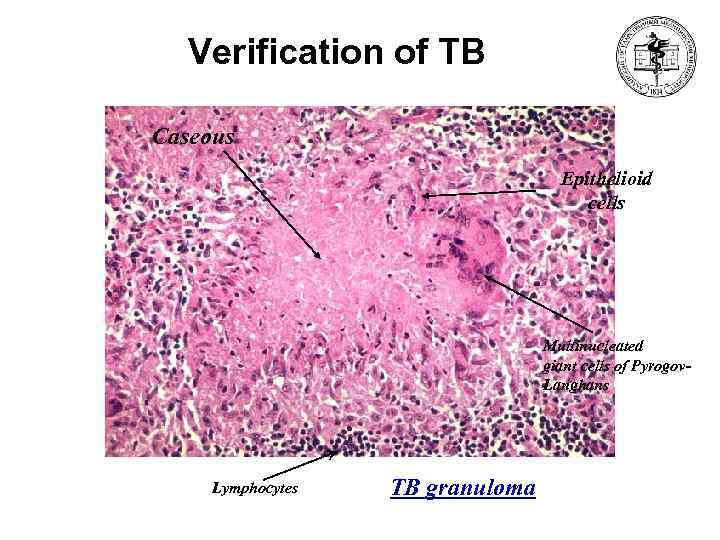
Verification of TB Caseous Epithelioid cells Multinucleated giant cells of Pyrogov. Langhans Lymphocytes TB granuloma
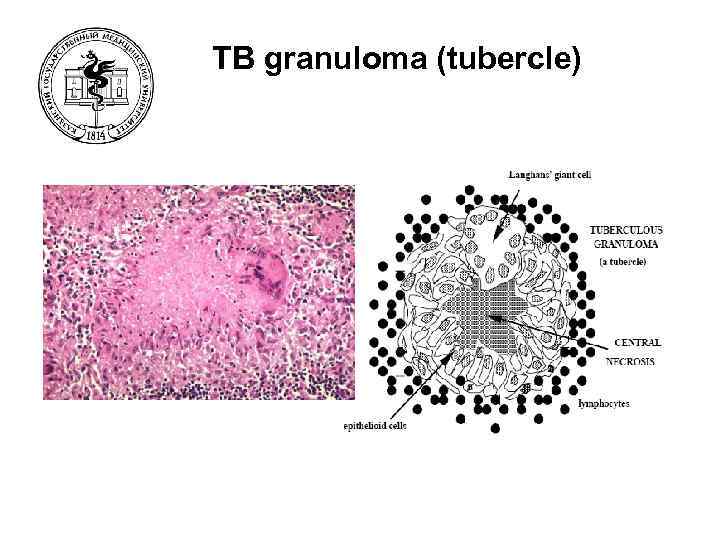
TB granuloma (tubercle)
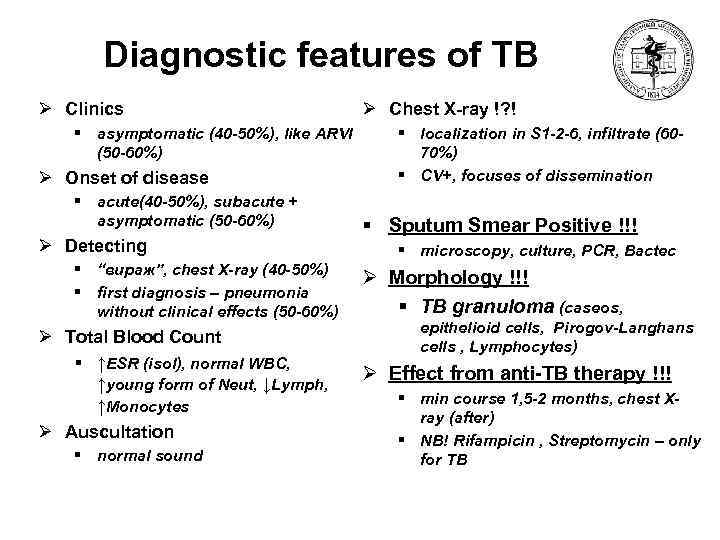
Diagnostic features of TB Ø Clinics § asymptomatic (40 -50%), like ARVI (50 -60%) Ø Onset of disease § acute(40 -50%), subacute + asymptomatic (50 -60%) Ø Detecting § “вираж”, chest X-ray (40 -50%) § first diagnosis – pneumonia without clinical effects (50 -60%) Ø Total Blood Count § ↑ESR (isol), normal WBC, ↑young form of Neut, ↓Lymph, ↑Monocytes Ø Auscultation § normal sound Ø Chest X-ray !? ! § localization in S 1 -2 -6, infiltrate (6070%) § CV+, focuses of dissemination § Sputum Smear Positive !!! § microscopy, culture, PCR, Bactec Ø Morphology !!! § TB granuloma (caseos, epithelioid cells, Pirogov-Langhans cells , Lymphocytes) Ø Effect from anti-TB therapy !!! § min course 1, 5 -2 months, chest Xray (after) § NB! Rifampicin , Streptomycin – only for TB
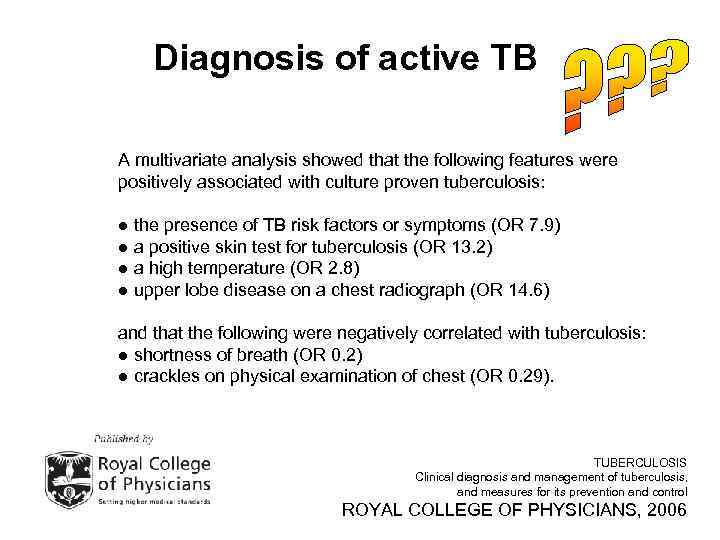
Diagnosis of active TB A multivariate analysis showed that the following features were positively associated with culture proven tuberculosis: ● the presence of TB risk factors or symptoms (OR 7. 9) ● a positive skin test for tuberculosis (OR 13. 2) ● a high temperature (OR 2. 8) ● upper lobe disease on a chest radiograph (OR 14. 6) and that the following were negatively correlated with tuberculosis: ● shortness of breath (OR 0. 2) ● crackles on physical examination of chest (OR 0. 29). TUBERCULOSIS Clinical diagnosis and management of tuberculosis, and measures for its prevention and control ROYAL COLLEGE OF PHYSICIANS, 2006
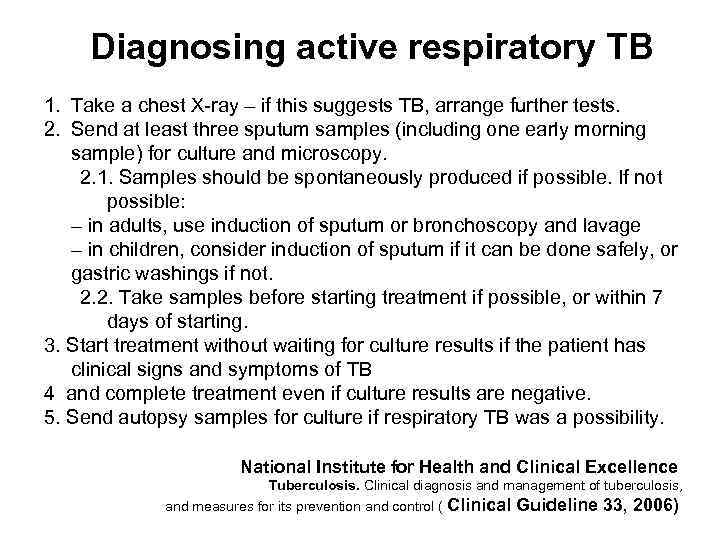
Diagnosing active respiratory TB 1. Take a chest X-ray – if this suggests TB, arrange further tests. 2. Send at least three sputum samples (including one early morning sample) for culture and microscopy. 2. 1. Samples should be spontaneously produced if possible. If not possible: – in adults, use induction of sputum or bronchoscopy and lavage – in children, consider induction of sputum if it can be done safely, or gastric washings if not. 2. 2. Take samples before starting treatment if possible, or within 7 days of starting. 3. Start treatment without waiting for culture results if the patient has clinical signs and symptoms of TB 4 and complete treatment even if culture results are negative. 5. Send autopsy samples for culture if respiratory TB was a possibility. National Institute for Health and Clinical Excellence Tuberculosis. Clinical diagnosis and management of tuberculosis, and measures for its prevention and control ( Clinical Guideline 33, 2006)
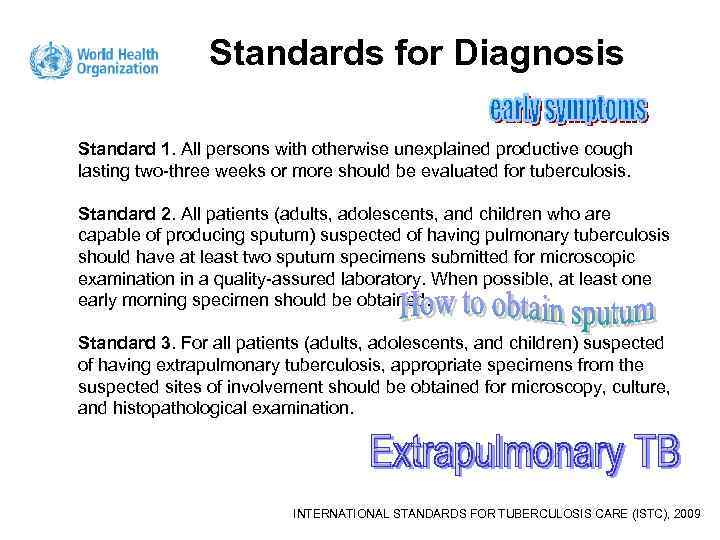
Standards for Diagnosis Standard 1. All persons with otherwise unexplained productive cough lasting two-three weeks or more should be evaluated for tuberculosis. Standard 2. All patients (adults, adolescents, and children who are capable of producing sputum) suspected of having pulmonary tuberculosis should have at least two sputum specimens submitted for microscopic examination in a quality-assured laboratory. When possible, at least one early morning specimen should be obtained. Standard 3. For all patients (adults, adolescents, and children) suspected of having extrapulmonary tuberculosis, appropriate specimens from the suspected sites of involvement should be obtained for microscopy, culture, and histopathological examination. INTERNATIONAL STANDARDS FOR TUBERCULOSIS CARE (ISTC), 2009
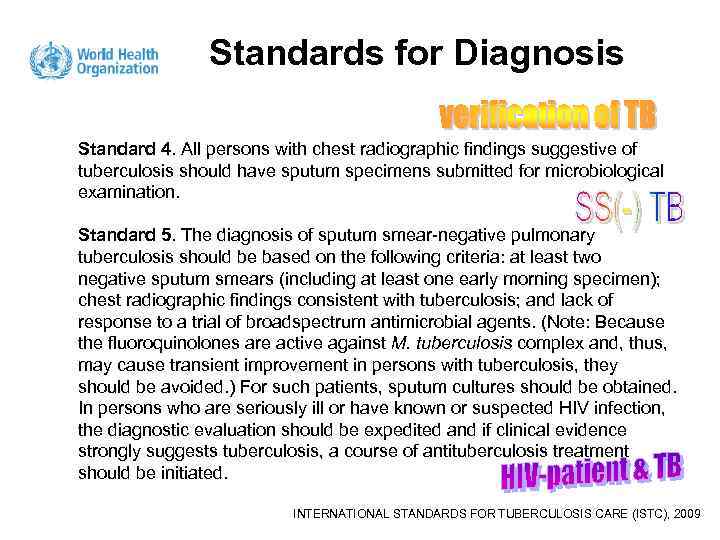
Standards for Diagnosis Standard 4. All persons with chest radiographic findings suggestive of tuberculosis should have sputum specimens submitted for microbiological examination. Standard 5. The diagnosis of sputum smear-negative pulmonary tuberculosis should be based on the following criteria: at least two negative sputum smears (including at least one early morning specimen); chest radiographic findings consistent with tuberculosis; and lack of response to a trial of broadspectrum antimicrobial agents. (Note: Because the fluoroquinolones are active against M. tuberculosis complex and, thus, may cause transient improvement in persons with tuberculosis, they should be avoided. ) For such patients, sputum cultures should be obtained. In persons who are seriously ill or have known or suspected HIV infection, the diagnostic evaluation should be expedited and if clinical evidence strongly suggests tuberculosis, a course of antituberculosis treatment should be initiated. INTERNATIONAL STANDARDS FOR TUBERCULOSIS CARE (ISTC), 2009
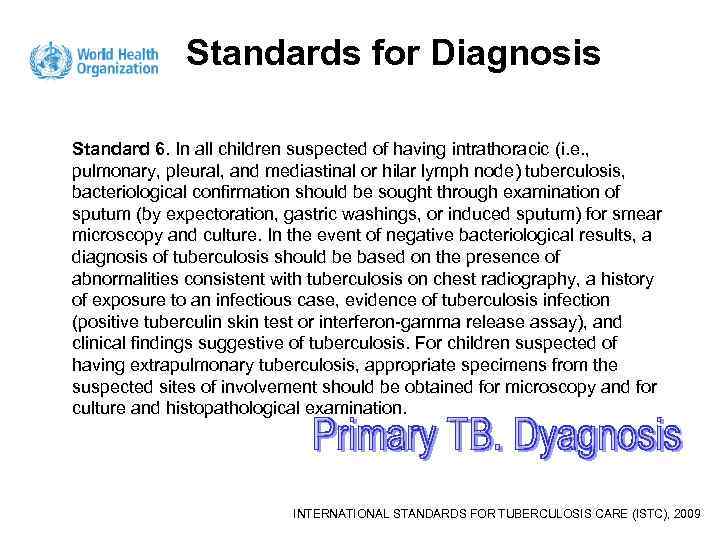
Standards for Diagnosis Standard 6. In all children suspected of having intrathoracic (i. e. , pulmonary, pleural, and mediastinal or hilar lymph node) tuberculosis, bacteriological confirmation should be sought through examination of sputum (by expectoration, gastric washings, or induced sputum) for smear microscopy and culture. In the event of negative bacteriological results, a diagnosis of tuberculosis should be based on the presence of abnormalities consistent with tuberculosis on chest radiography, a history of exposure to an infectious case, evidence of tuberculosis infection (positive tuberculin skin test or interferon-gamma release assay), and clinical findings suggestive of tuberculosis. For children suspected of having extrapulmonary tuberculosis, appropriate specimens from the suspected sites of involvement should be obtained for microscopy and for culture and histopathological examination. INTERNATIONAL STANDARDS FOR TUBERCULOSIS CARE (ISTC), 2009
Medical history of active TB Ø The Aims of Interview § to obtain information to make an accurate diagnosis § to make a differential diagnosis § to create the further diagnostic plan for patient § to create a plan for treatment (if it’s possible)
The Seven Level Model of whole-person medicine • • • Social effects (for instance – family’s anxiety, must change my work) Disability (for instance – unable to work) Symptoms (for instance – cough and breathlessness) Signs (for instance – fever, hyperventilation) Disorders structure & Functions (for instance – infiltrate on chest X-ray) • Pathology (for instance – pneumonia, TB) • Causes (for instance – smoking, contact with active TB patient)
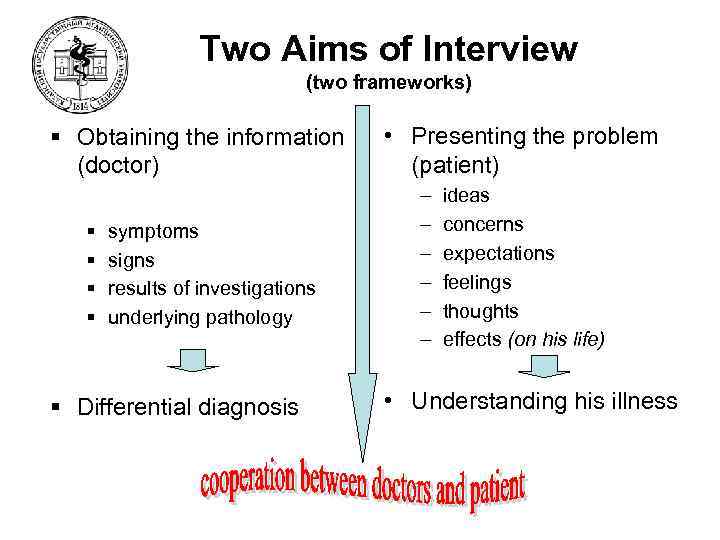
Two Aims of Interview (two frameworks) § Obtaining the information (doctor) § § symptoms signs results of investigations underlying pathology § Differential diagnosis • Presenting the problem (patient) – – – ideas concerns expectations feelings thoughts effects (on his life) • Understanding his illness
Medical history of active respiratory TB Ø Symptoms and signs § Intoxication syndrome § malaise, fever, chills, fatigue, weakness, night sweats, lost weight, anorexia (decrease of appetite) § Chest syndrome § prolonged cough more than 2 weeks (initially dry and may later become productive), decreased an ability to perform physical exercise, haemoptysis, lung bleeding, dyspnea, chest pain
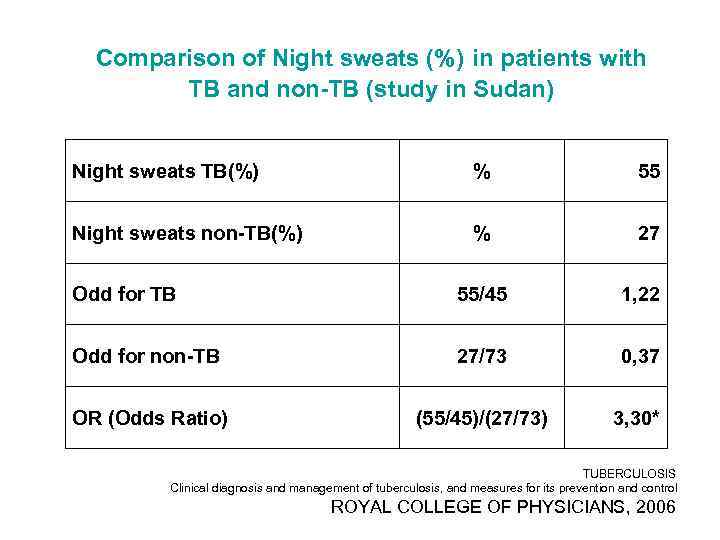
Comparison of Night sweats (%) in patients with TB and non-TB (study in Sudan) Night sweats TB(%) % 55 Night sweats non-TB(%) % 27 Odd for TB 55/45 1, 22 Odd for non-TB 27/73 0, 37 OR (Odds Ratio) (55/45)/(27/73) 3, 30* TUBERCULOSIS Clinical diagnosis and management of tuberculosis, and measures for its prevention and control ROYAL COLLEGE OF PHYSICIANS, 2006
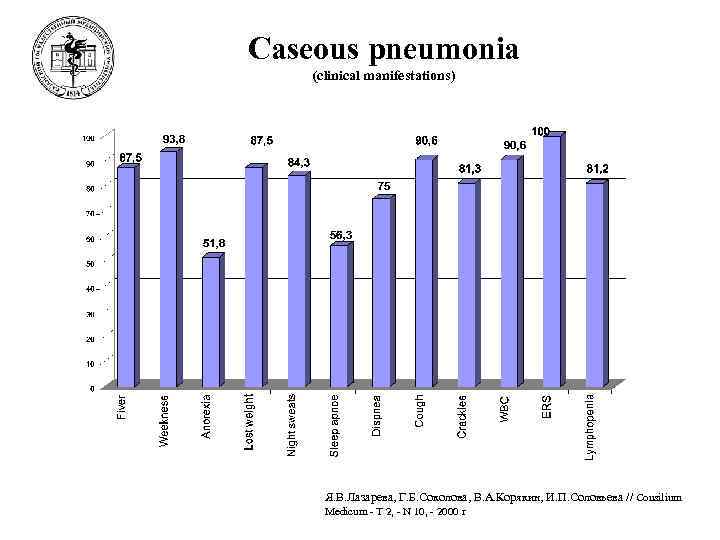
Caseous pneumonia (clinical manifestations) Я. В. Лазарева, Г. Б. Соколова, В. А. Корякин, И. П. Соловьева // Consilium Medicum - T 2, - N 10, - 2000 г