80f1a7d70ffc376dd9bf2ec6d985ecc0.ppt
- Количество слайдов: 72
 Topic review
Topic review
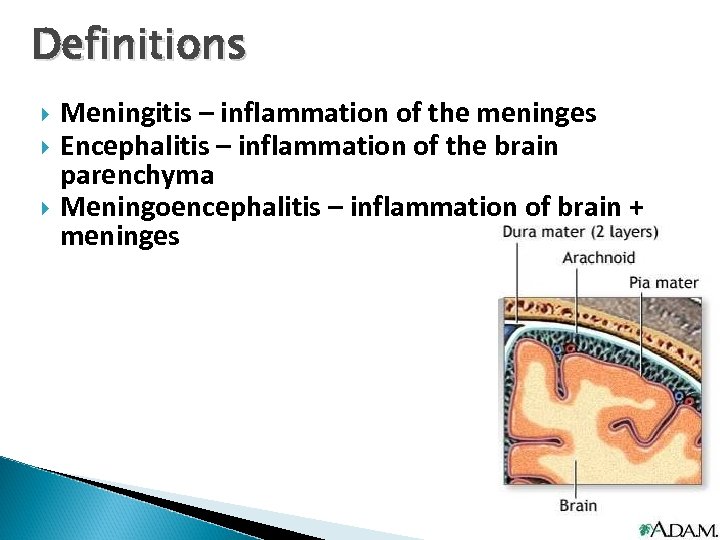 Definitions Meningitis – inflammation of the meninges Encephalitis – inflammation of the brain parenchyma Meningoencephalitis – inflammation of brain + meninges
Definitions Meningitis – inflammation of the meninges Encephalitis – inflammation of the brain parenchyma Meningoencephalitis – inflammation of brain + meninges
 Definitions Meningitis is a clinical syndrome characterized by inflammation of the meninges There are numerous infectious and noninfectious causes of meningitis (common noninfectious causes eg, medications and carcinomatosis) may be classified as acute or chronic Acute meningitis -hours to several days Chronic meningitis -at least 4 weeks.
Definitions Meningitis is a clinical syndrome characterized by inflammation of the meninges There are numerous infectious and noninfectious causes of meningitis (common noninfectious causes eg, medications and carcinomatosis) may be classified as acute or chronic Acute meningitis -hours to several days Chronic meningitis -at least 4 weeks.
 Classification 1. acute bacterial meningitis 2. acute aseptic meningitis 3. chronic meningitis 4. other (depend on specific pathogen); fungal meningitis, parasitic meningitis i. e
Classification 1. acute bacterial meningitis 2. acute aseptic meningitis 3. chronic meningitis 4. other (depend on specific pathogen); fungal meningitis, parasitic meningitis i. e
 Pathophysiology Three major pathways which an infectious agent gains access to the CNS and causes meningeal disease Hematogenous (eg, from bacteremia, viremia, fungemia) Retrograde neuronal pathway (eg, Naegleria fowleri, Direct contiguous spread (eg, sinusitis, otitis media, rabies, HSV, VZV) congenital malformations, trauma, direct inoculation during intracranial manipulation)
Pathophysiology Three major pathways which an infectious agent gains access to the CNS and causes meningeal disease Hematogenous (eg, from bacteremia, viremia, fungemia) Retrograde neuronal pathway (eg, Naegleria fowleri, Direct contiguous spread (eg, sinusitis, otitis media, rabies, HSV, VZV) congenital malformations, trauma, direct inoculation during intracranial manipulation)
 Clinical manifestation Fever , malaise Headache nausea, vomiting photophobia Hyperirritability neck stiffness changes in mental status Seizure occur in approximately 30% of patients
Clinical manifestation Fever , malaise Headache nausea, vomiting photophobia Hyperirritability neck stiffness changes in mental status Seizure occur in approximately 30% of patients
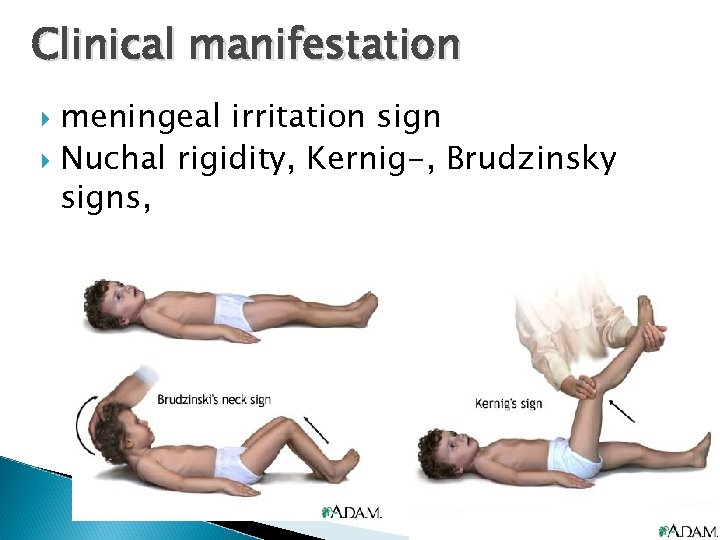 Clinical manifestation meningeal irritation sign Nuchal rigidity, Kernig-, Brudzinsky signs,
Clinical manifestation meningeal irritation sign Nuchal rigidity, Kernig-, Brudzinsky signs,
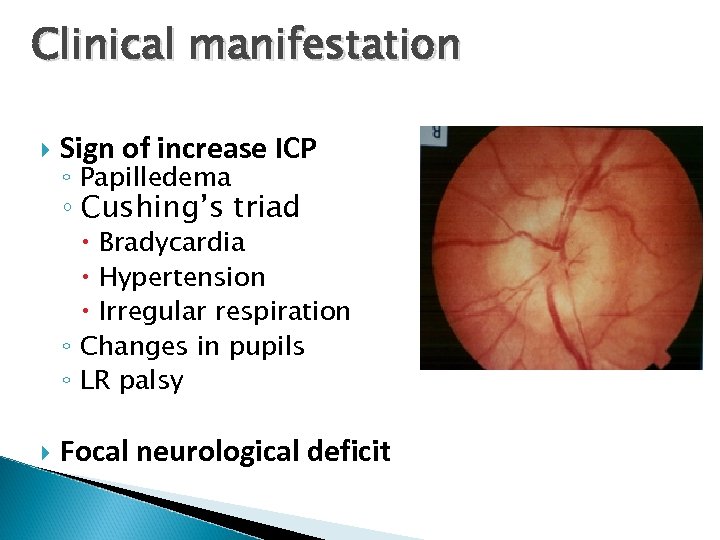 Clinical manifestation Sign of increase ICP ◦ Papilledema ◦ Cushing’s triad Bradycardia Hypertension Irregular respiration ◦ Changes in pupils ◦ LR palsy Focal neurological deficit
Clinical manifestation Sign of increase ICP ◦ Papilledema ◦ Cushing’s triad Bradycardia Hypertension Irregular respiration ◦ Changes in pupils ◦ LR palsy Focal neurological deficit
 Clinical manifestation Atypical presentation may be observed in certain groups ◦ Elderly, especially with underlying comorbidities (eg, diabetes, renal and liver disease), may present with lethargy and an absence of meningeal symptoms. ◦ Patients with neutropenia may present with subtle symptoms of meningeal irritation. ◦ Other ; immunocompromised hosts, including organ and tissue transplant recipients and patients with HIV and AIDS patients with aseptic meningitis syndrome usually appear clinically nontoxic with no vascular instability.
Clinical manifestation Atypical presentation may be observed in certain groups ◦ Elderly, especially with underlying comorbidities (eg, diabetes, renal and liver disease), may present with lethargy and an absence of meningeal symptoms. ◦ Patients with neutropenia may present with subtle symptoms of meningeal irritation. ◦ Other ; immunocompromised hosts, including organ and tissue transplant recipients and patients with HIV and AIDS patients with aseptic meningitis syndrome usually appear clinically nontoxic with no vascular instability.
 Clinical manifestation sexual contact and high-risk behavior: HSV meningitis is associated with primary genital HSV infection and HIV infection exposure to a patient with a similar illness is an important epidemiological clue when determining etiology (eg, meningococcemia). intake of unpasteurized milk predisposes to brucellosis and L monocytogenes infection. Animal contacts rabies (LCM) virus Leptospira History of neurosurgery eg, ventriculoperitoneal shunt cochlear implants
Clinical manifestation sexual contact and high-risk behavior: HSV meningitis is associated with primary genital HSV infection and HIV infection exposure to a patient with a similar illness is an important epidemiological clue when determining etiology (eg, meningococcemia). intake of unpasteurized milk predisposes to brucellosis and L monocytogenes infection. Animal contacts rabies (LCM) virus Leptospira History of neurosurgery eg, ventriculoperitoneal shunt cochlear implants
 Clinical manifestation Sinusitis or otitis suggests direct extension into the meninges, usually with S pneumoniae and H influenzae Rhinorrhea or otorrhea suggests a CSF leak from a basilar skull fracture, with meningitis most commonly caused by S pneumoniae. petechiae are seen in meningococcal disease with or without meningitis The presence of a murmur suggests infective endocarditis with secondary bacterial seeding of the meninges
Clinical manifestation Sinusitis or otitis suggests direct extension into the meninges, usually with S pneumoniae and H influenzae Rhinorrhea or otorrhea suggests a CSF leak from a basilar skull fracture, with meningitis most commonly caused by S pneumoniae. petechiae are seen in meningococcal disease with or without meningitis The presence of a murmur suggests infective endocarditis with secondary bacterial seeding of the meninges
 Clinical manifestation Hepatosplenomegaly and lymphadenopathy suggest a systemic disease, including viral (eg, mononucleosislike syndrome in EBV, CMV, and HIV) and fungal (eg, disseminated histoplasmosis) disease. Vesicular lesions in a dermatomal distribution suggest varicella-zoster virus. Genital vesicles suggest HSV-2 meningitis
Clinical manifestation Hepatosplenomegaly and lymphadenopathy suggest a systemic disease, including viral (eg, mononucleosislike syndrome in EBV, CMV, and HIV) and fungal (eg, disseminated histoplasmosis) disease. Vesicular lesions in a dermatomal distribution suggest varicella-zoster virus. Genital vesicles suggest HSV-2 meningitis
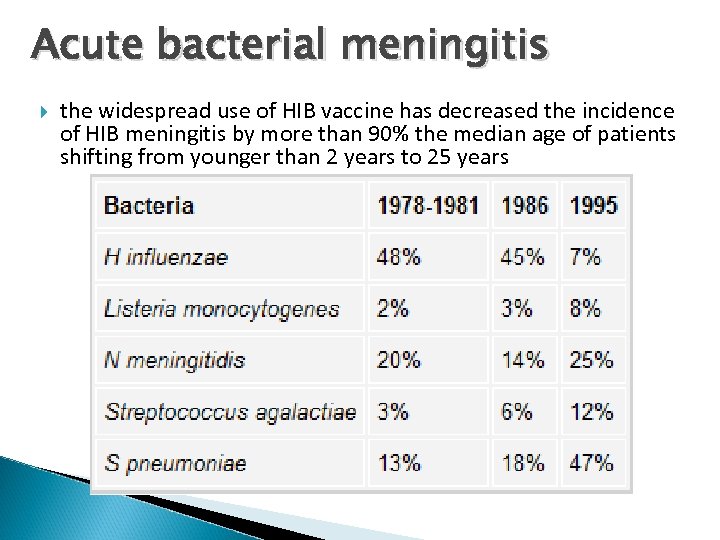 Acute bacterial meningitis the widespread use of HIB vaccine has decreased the incidence of HIB meningitis by more than 90% the median age of patients shifting from younger than 2 years to 25 years
Acute bacterial meningitis the widespread use of HIB vaccine has decreased the incidence of HIB meningitis by more than 90% the median age of patients shifting from younger than 2 years to 25 years
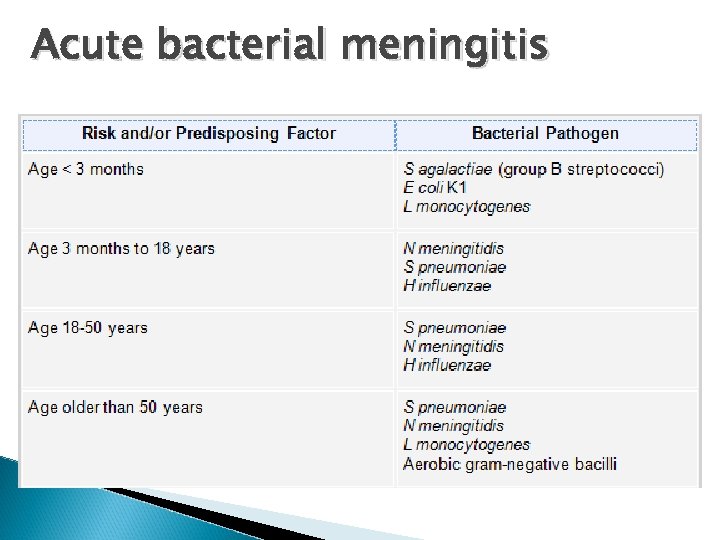 Acute bacterial meningitis
Acute bacterial meningitis
 Acute bacterial meningitis
Acute bacterial meningitis
 S. pneumoniae ◦ gram-positive cocci, colonize at human nasopharynx. ◦ most common bacterial cause of meningitis, accounting for 47% of cases with mortality rates 19 -26% ◦ Mechanism: hematogenous or direct extension from sinusitis or otitis media ◦ Risk factor basilar skull fracture and CSF leak. Patients with hyposplenism or splenectomy hypogammaglobulinemia, multiple myeloma glucocorticoid treatment diabetes mellitus, renal insufficiency, alcoholism, malnutrition, and chronic liver disease
S. pneumoniae ◦ gram-positive cocci, colonize at human nasopharynx. ◦ most common bacterial cause of meningitis, accounting for 47% of cases with mortality rates 19 -26% ◦ Mechanism: hematogenous or direct extension from sinusitis or otitis media ◦ Risk factor basilar skull fracture and CSF leak. Patients with hyposplenism or splenectomy hypogammaglobulinemia, multiple myeloma glucocorticoid treatment diabetes mellitus, renal insufficiency, alcoholism, malnutrition, and chronic liver disease
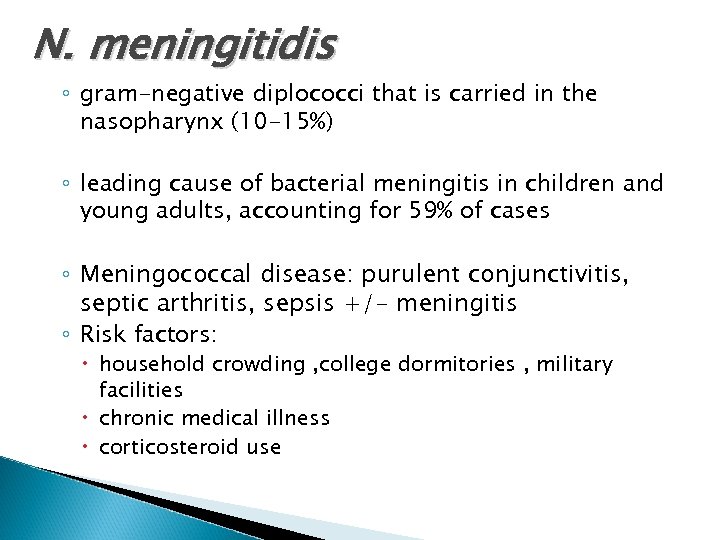 N. meningitidis ◦ gram-negative diplococci that is carried in the nasopharynx (10 -15%) ◦ leading cause of bacterial meningitis in children and young adults, accounting for 59% of cases ◦ Meningococcal disease: purulent conjunctivitis, septic arthritis, sepsis +/- meningitis ◦ Risk factors: household crowding , college dormitories , military facilities chronic medical illness corticosteroid use
N. meningitidis ◦ gram-negative diplococci that is carried in the nasopharynx (10 -15%) ◦ leading cause of bacterial meningitis in children and young adults, accounting for 59% of cases ◦ Meningococcal disease: purulent conjunctivitis, septic arthritis, sepsis +/- meningitis ◦ Risk factors: household crowding , college dormitories , military facilities chronic medical illness corticosteroid use
 N. meningitidis
N. meningitidis
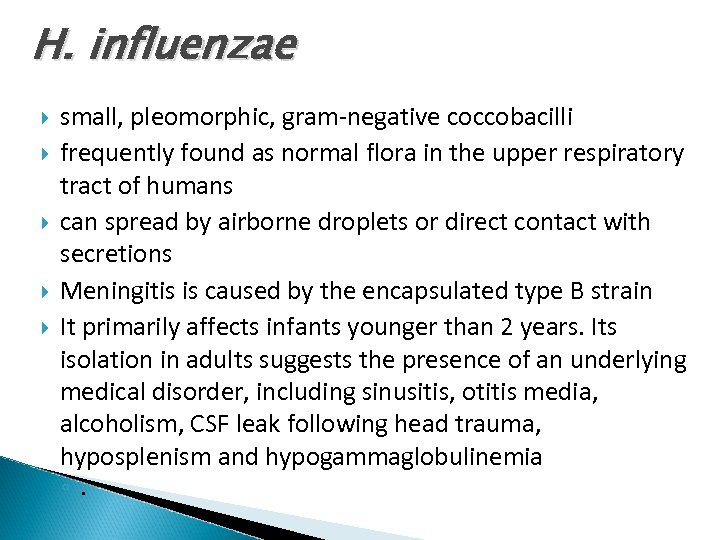 H. influenzae small, pleomorphic, gram-negative coccobacilli frequently found as normal flora in the upper respiratory tract of humans can spread by airborne droplets or direct contact with secretions Meningitis is caused by the encapsulated type B strain It primarily affects infants younger than 2 years. Its isolation in adults suggests the presence of an underlying medical disorder, including sinusitis, otitis media, alcoholism, CSF leak following head trauma, hyposplenism and hypogammaglobulinemia ◦.
H. influenzae small, pleomorphic, gram-negative coccobacilli frequently found as normal flora in the upper respiratory tract of humans can spread by airborne droplets or direct contact with secretions Meningitis is caused by the encapsulated type B strain It primarily affects infants younger than 2 years. Its isolation in adults suggests the presence of an underlying medical disorder, including sinusitis, otitis media, alcoholism, CSF leak following head trauma, hyposplenism and hypogammaglobulinemia ◦.
 L. monocytogenes ◦ small gram-positive bacillus ◦ one of the highest mortality rates (22%). ◦ Most human cases appear food-borne: coleslaw, milk, cheese i. e ◦ Risk factor: infants and children, elderly (>60 y) pregnant women Alcoholism Patients with CMI defect immunocompromised
L. monocytogenes ◦ small gram-positive bacillus ◦ one of the highest mortality rates (22%). ◦ Most human cases appear food-borne: coleslaw, milk, cheese i. e ◦ Risk factor: infants and children, elderly (>60 y) pregnant women Alcoholism Patients with CMI defect immunocompromised

 Aseptic meningitis syndrome most common infectious syndrome affecting the CNS acute onset of meningeal symptoms, fever, and cerebrospinal pleocytosis (usually prominently lymphocytic) with negative bacterial microbiologic data Most episodes are caused by a viral pathogen but they can also be caused by bacteria, fungi, or parasites
Aseptic meningitis syndrome most common infectious syndrome affecting the CNS acute onset of meningeal symptoms, fever, and cerebrospinal pleocytosis (usually prominently lymphocytic) with negative bacterial microbiologic data Most episodes are caused by a viral pathogen but they can also be caused by bacteria, fungi, or parasites
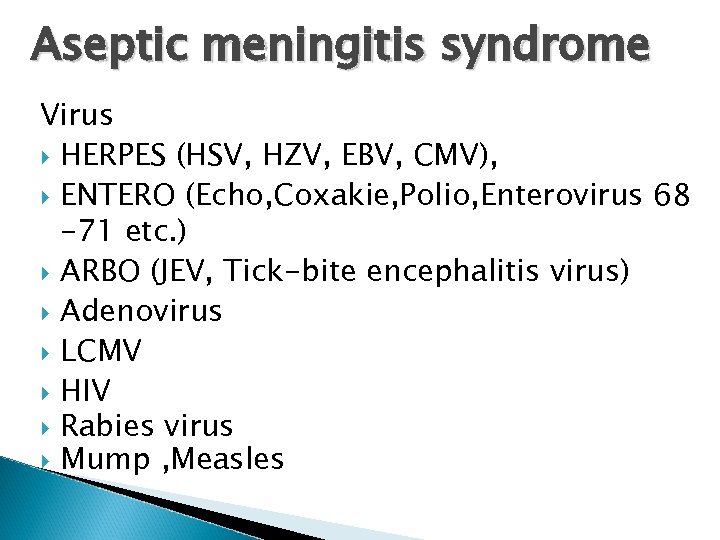 Aseptic meningitis syndrome Virus HERPES (HSV, HZV, EBV, CMV), ENTERO (Echo, Coxakie, Polio, Enterovirus 68 -71 etc. ) ARBO (JEV, Tick-bite encephalitis virus) Adenovirus LCMV HIV Rabies virus Mump , Measles
Aseptic meningitis syndrome Virus HERPES (HSV, HZV, EBV, CMV), ENTERO (Echo, Coxakie, Polio, Enterovirus 68 -71 etc. ) ARBO (JEV, Tick-bite encephalitis virus) Adenovirus LCMV HIV Rabies virus Mump , Measles
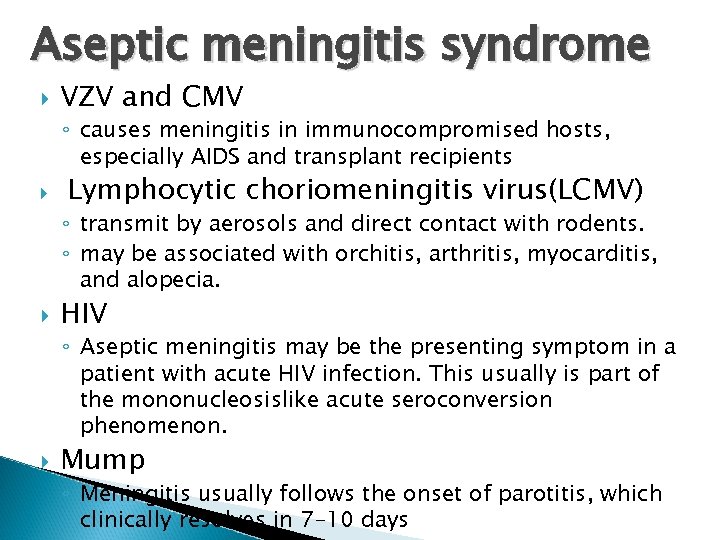 Aseptic meningitis syndrome VZV and CMV ◦ causes meningitis in immunocompromised hosts, especially AIDS and transplant recipients Lymphocytic choriomeningitis virus(LCMV) ◦ transmit by aerosols and direct contact with rodents. ◦ may be associated with orchitis, arthritis, myocarditis, and alopecia. HIV ◦ Aseptic meningitis may be the presenting symptom in a patient with acute HIV infection. This usually is part of the mononucleosislike acute seroconversion phenomenon. Mump ◦ Meningitis usually follows the onset of parotitis, which clinically resolves in 7 -10 days
Aseptic meningitis syndrome VZV and CMV ◦ causes meningitis in immunocompromised hosts, especially AIDS and transplant recipients Lymphocytic choriomeningitis virus(LCMV) ◦ transmit by aerosols and direct contact with rodents. ◦ may be associated with orchitis, arthritis, myocarditis, and alopecia. HIV ◦ Aseptic meningitis may be the presenting symptom in a patient with acute HIV infection. This usually is part of the mononucleosislike acute seroconversion phenomenon. Mump ◦ Meningitis usually follows the onset of parotitis, which clinically resolves in 7 -10 days
 Aseptic meningitis syndrome Bacteria ◦ ◦ ◦ Partially-treated bacterial meningitis L monocytogenes Brucella species Rickettsia rickettsii Ehrlichia species Mycoplasma pneumoniae B burgdorferi Treponema pallidum Leptospira species Mycobacterium tuberculosis Nocardia species
Aseptic meningitis syndrome Bacteria ◦ ◦ ◦ Partially-treated bacterial meningitis L monocytogenes Brucella species Rickettsia rickettsii Ehrlichia species Mycoplasma pneumoniae B burgdorferi Treponema pallidum Leptospira species Mycobacterium tuberculosis Nocardia species
 Aseptic meningitis syndrome Parasites ◦ ◦ ◦ ◦ N fowleri Acanthamoeba species Balamuthia species Angiostrongylus cantonensis G spinigerum Baylisascaris procyonis S stercoralis Taenia solium (cysticercosis)
Aseptic meningitis syndrome Parasites ◦ ◦ ◦ ◦ N fowleri Acanthamoeba species Balamuthia species Angiostrongylus cantonensis G spinigerum Baylisascaris procyonis S stercoralis Taenia solium (cysticercosis)
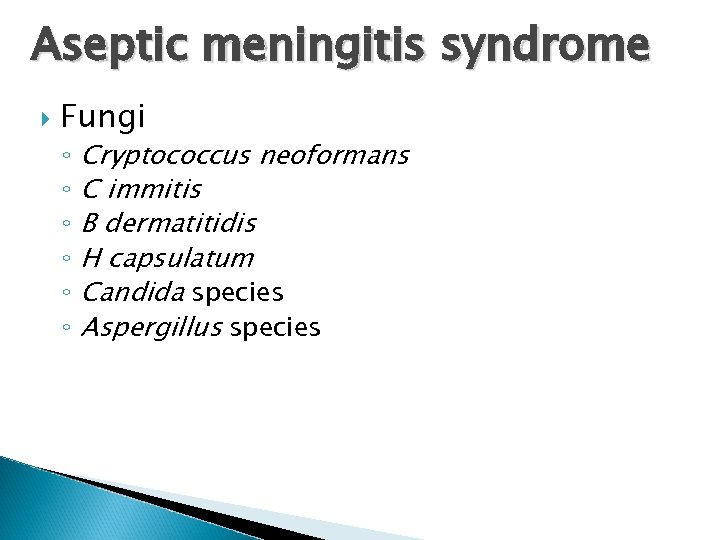 Aseptic meningitis syndrome Fungi ◦ ◦ ◦ Cryptococcus neoformans C immitis B dermatitidis H capsulatum Candida species Aspergillus species
Aseptic meningitis syndrome Fungi ◦ ◦ ◦ Cryptococcus neoformans C immitis B dermatitidis H capsulatum Candida species Aspergillus species
 Chronic meningitis constellation of signs and symptoms of meningeal irritation associated with CSF pleocytosis that persists for longer than 4 weeks.
Chronic meningitis constellation of signs and symptoms of meningeal irritation associated with CSF pleocytosis that persists for longer than 4 weeks.
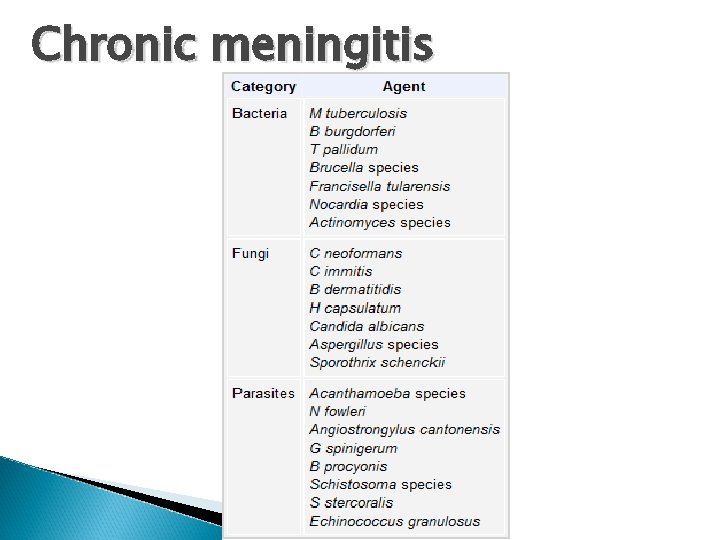 Chronic meningitis
Chronic meningitis
 Tuberculous meningitis ◦ acid-fast bacilli ◦ spread through airborne, droplet ◦ The presentation may be acute, but the classic presentation is subacute and spans weeks ◦ Patients generally have a prodrome of fever of varying degrees, malaise, and intermittent headaches ◦ Patients often develop central nerve palsies (III, IV, V, VI, and VII), suggesting basilar meningeal involvement
Tuberculous meningitis ◦ acid-fast bacilli ◦ spread through airborne, droplet ◦ The presentation may be acute, but the classic presentation is subacute and spans weeks ◦ Patients generally have a prodrome of fever of varying degrees, malaise, and intermittent headaches ◦ Patients often develop central nerve palsies (III, IV, V, VI, and VII), suggesting basilar meningeal involvement
 Tuberculous meningitis clinical staging of meningeal tuberculosis is based on neurologic status ◦ Stage 1 - no change in mental function with no deficits and no hydrocephalus ◦ Stage 2 - confusion and evidence of neurologic deficit ◦ Stage 3 - stupor and lethargy Always consider tuberculous meningitis in the differential diagnoses of patients with aseptic meningitis or chronic meningitis syndromes
Tuberculous meningitis clinical staging of meningeal tuberculosis is based on neurologic status ◦ Stage 1 - no change in mental function with no deficits and no hydrocephalus ◦ Stage 2 - confusion and evidence of neurologic deficit ◦ Stage 3 - stupor and lethargy Always consider tuberculous meningitis in the differential diagnoses of patients with aseptic meningitis or chronic meningitis syndromes
 Spirochetal meningitis T pallidum modes of transmission: ◦ ◦ sexual contact direct contact with an active lesion passage through the placenta blood transfusion (rare) Three stages of disease are described, and involvement of the CNS can occur during any of these stages. Syphilitic meningitis usually occurs during the primary or secondary stage. Its presentation is similar to other agents of aseptic meningitis
Spirochetal meningitis T pallidum modes of transmission: ◦ ◦ sexual contact direct contact with an active lesion passage through the placenta blood transfusion (rare) Three stages of disease are described, and involvement of the CNS can occur during any of these stages. Syphilitic meningitis usually occurs during the primary or secondary stage. Its presentation is similar to other agents of aseptic meningitis
 Spirochetal meningitis Other CNS syphilitic syndromes include ◦ meningovascular syphilis ◦ parenchymatous neurosyphilis ◦ gummatous neurosyphilis and the symptoms are dominated by focal syphilitic arteritis (ie, focal neurologic symptoms associated with signs of meningeal irritation)
Spirochetal meningitis Other CNS syphilitic syndromes include ◦ meningovascular syphilis ◦ parenchymatous neurosyphilis ◦ gummatous neurosyphilis and the symptoms are dominated by focal syphilitic arteritis (ie, focal neurologic symptoms associated with signs of meningeal irritation)
 Fungal meningitis C. neoformans an encapsulated yeast-like fungus that found in high concentrations in aged pigeon droppings 50 -80% of cases occur in immunocompromised hosts The infection is characterized by the gradual onset of symptoms, the most common of which is headache. The onset may be acute, especially among patients with AIDS
Fungal meningitis C. neoformans an encapsulated yeast-like fungus that found in high concentrations in aged pigeon droppings 50 -80% of cases occur in immunocompromised hosts The infection is characterized by the gradual onset of symptoms, the most common of which is headache. The onset may be acute, especially among patients with AIDS
 Parasitic meningitis Free-living amoebas (ie, Acanthamoeba, Balamuthia, Naegleria) ◦ infrequent but often life-threatening illness ◦ N fowleri is the agent of primary amebic meningoencephalitis (PAM) ◦ Infection occurs when swimming or playing in the contaminated water ◦ invade the CNS through the nasal mucosa and cribriform plate.
Parasitic meningitis Free-living amoebas (ie, Acanthamoeba, Balamuthia, Naegleria) ◦ infrequent but often life-threatening illness ◦ N fowleri is the agent of primary amebic meningoencephalitis (PAM) ◦ Infection occurs when swimming or playing in the contaminated water ◦ invade the CNS through the nasal mucosa and cribriform plate.
 Parasitic meningitis ◦ PAM occurs in 2 forms. an acute onset of high fever, photophobia, headache, and change in mental status, similar to bacterial meningitis with involvement of the olfactory nerves sensation. Death occurs in 3 days in patients who are not treated. subacute or chronic form, is an insidious onset of low-grade fever, headache, and focal neurologic signs. Acanthamoeba and Balamuthia cause granulomatous amebic encephalitis, which spreads hematogenously from the primary site of infection (skin or lungs)
Parasitic meningitis ◦ PAM occurs in 2 forms. an acute onset of high fever, photophobia, headache, and change in mental status, similar to bacterial meningitis with involvement of the olfactory nerves sensation. Death occurs in 3 days in patients who are not treated. subacute or chronic form, is an insidious onset of low-grade fever, headache, and focal neurologic signs. Acanthamoeba and Balamuthia cause granulomatous amebic encephalitis, which spreads hematogenously from the primary site of infection (skin or lungs)
 Helminthic eosinophilic meningitis A cantonensis G spinigerum ◦ cause eosinophilic meningitis (pleocytosis with >10% eosinophils) ◦ acquire the infection by ingesting raw mollusks. ◦ present with nonspecific and self-limited abdominal pain caused by larval migration into the bowel wall. ◦ On rare occasions, the larva can migrate into the CNS and cause eosinophilic meningitis ◦ cause eosinophilic meningoencephalitis ◦ acquire the infection following ingestion of undercooked infected fish and poultry.
Helminthic eosinophilic meningitis A cantonensis G spinigerum ◦ cause eosinophilic meningitis (pleocytosis with >10% eosinophils) ◦ acquire the infection by ingesting raw mollusks. ◦ present with nonspecific and self-limited abdominal pain caused by larval migration into the bowel wall. ◦ On rare occasions, the larva can migrate into the CNS and cause eosinophilic meningitis ◦ cause eosinophilic meningoencephalitis ◦ acquire the infection following ingestion of undercooked infected fish and poultry.
 Differential diagnosis Encephalitis Brain Abscess Noninfectious meningitis, including medicationinduced meningeal inflammation Meningeal carcinomatosis Stroke CNS vasculitis
Differential diagnosis Encephalitis Brain Abscess Noninfectious meningitis, including medicationinduced meningeal inflammation Meningeal carcinomatosis Stroke CNS vasculitis
 Lumbar puncture for CSF examination is urgently warranted in individuals in whom meningitis is clinically suspected CSF for ◦ Chemistry (glucose & protein) ◦ cell count & diff ◦ Gram stain , AFB stain ◦ Culture for pathogens ◦ Other : India ink , serology , PCR , Ag Identification , cytology i. e
Lumbar puncture for CSF examination is urgently warranted in individuals in whom meningitis is clinically suspected CSF for ◦ Chemistry (glucose & protein) ◦ cell count & diff ◦ Gram stain , AFB stain ◦ Culture for pathogens ◦ Other : India ink , serology , PCR , Ag Identification , cytology i. e
 Lumbar puncture Between L 3 -L 4(iliac crest level) or L 4 -L 5
Lumbar puncture Between L 3 -L 4(iliac crest level) or L 4 -L 5
 Lumbar puncture Contraindications: ◦ increase risk of herniation(suspected space occupying lesion in CNS) ◦ Skin & soft tissue infection at area of tap ◦ Bleeding disorder ◦ Respiratory distress (positioning) Complications ◦ Cerebral herniation ◦ Postdural puncture headache ◦ Traumatic tap , Spinal trauma
Lumbar puncture Contraindications: ◦ increase risk of herniation(suspected space occupying lesion in CNS) ◦ Skin & soft tissue infection at area of tap ◦ Bleeding disorder ◦ Respiratory distress (positioning) Complications ◦ Cerebral herniation ◦ Postdural puncture headache ◦ Traumatic tap , Spinal trauma

 Laboratory investigation CBC BS Anti-HIV H/C cultures from other possible sites of infection
Laboratory investigation CBC BS Anti-HIV H/C cultures from other possible sites of infection
 Imaging study CT or MRI of the brain indicated in patients with ◦ ◦ ◦ focal neurologic deficit increased ICP suspicious for space-occupying lesions suspected basilar fracture diagnosis is unclear Helpful in the detection of CNS complications of bacterial meningitis, such as hydrocephalus, cerebral infarct, brain abscess, subdural empyema, and venous sinus thrombosis
Imaging study CT or MRI of the brain indicated in patients with ◦ ◦ ◦ focal neurologic deficit increased ICP suspicious for space-occupying lesions suspected basilar fracture diagnosis is unclear Helpful in the detection of CNS complications of bacterial meningitis, such as hydrocephalus, cerebral infarct, brain abscess, subdural empyema, and venous sinus thrombosis
 Treatment : Bacterial meningitis is a neurological emergency that is associated with significant morbidity and mortality. The initiation of empiric antibacterial therapy is therefore essential for better outcome usually based on the known predisposing factors and/or initial CSF Gram-stain results. delays in instituting antimicrobial treatment in individuals with bacterial meningitis could lead to significant morbidity and mortality
Treatment : Bacterial meningitis is a neurological emergency that is associated with significant morbidity and mortality. The initiation of empiric antibacterial therapy is therefore essential for better outcome usually based on the known predisposing factors and/or initial CSF Gram-stain results. delays in instituting antimicrobial treatment in individuals with bacterial meningitis could lead to significant morbidity and mortality
 Treatment : Bacterial meningitis penicillins, certain cephalosporins (ie, thirdand fourth-generation cephalosporins), the carbapenems, fluoroquinolones, and rifampin provide high CSF levels Once the pathogen has been identified antimicrobial susceptibilities determined, the antibiotics may be modified for optimal targetted treatment
Treatment : Bacterial meningitis penicillins, certain cephalosporins (ie, thirdand fourth-generation cephalosporins), the carbapenems, fluoroquinolones, and rifampin provide high CSF levels Once the pathogen has been identified antimicrobial susceptibilities determined, the antibiotics may be modified for optimal targetted treatment

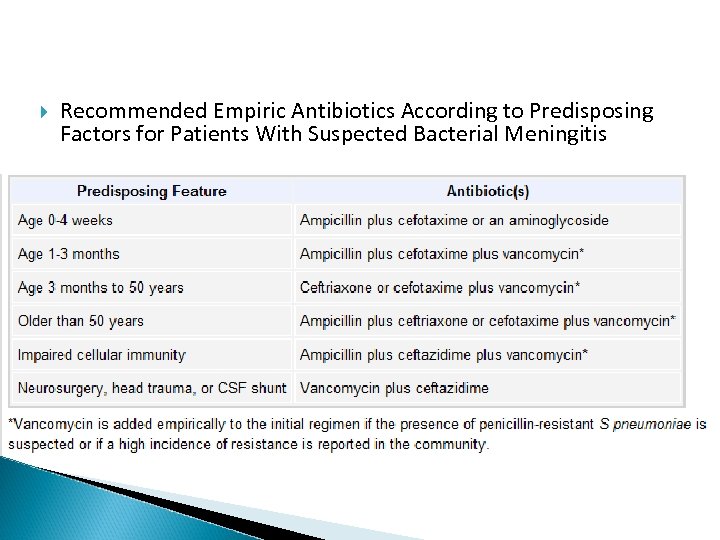 Recommended Empiric Antibiotics According to Predisposing Factors for Patients With Suspected Bacterial Meningitis
Recommended Empiric Antibiotics According to Predisposing Factors for Patients With Suspected Bacterial Meningitis
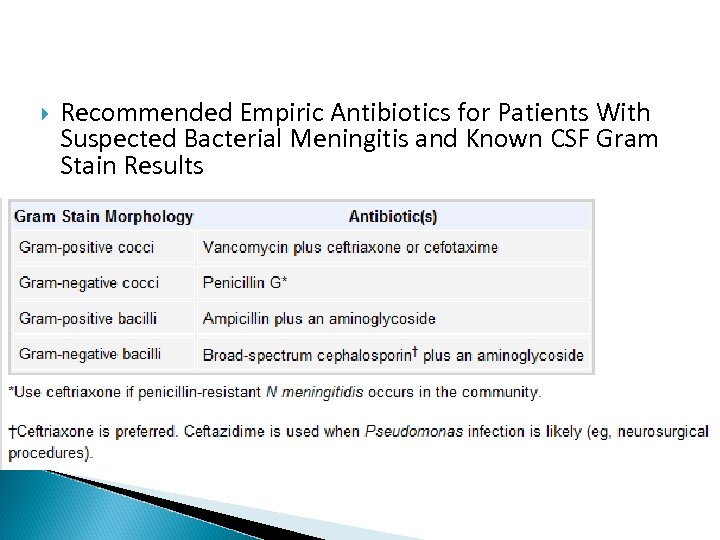 Recommended Empiric Antibiotics for Patients With Suspected Bacterial Meningitis and Known CSF Gram Stain Results
Recommended Empiric Antibiotics for Patients With Suspected Bacterial Meningitis and Known CSF Gram Stain Results
 Specific Antibiotics and Duration of Therapy for Patients With Acute Bacterial Meningitis
Specific Antibiotics and Duration of Therapy for Patients With Acute Bacterial Meningitis
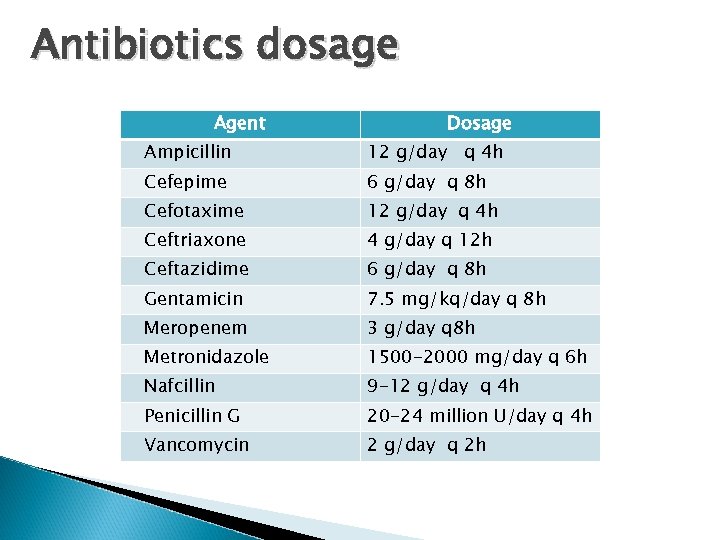 Antibiotics dosage Agent Dosage Ampicillin 12 g/day q 4 h Cefepime 6 g/day q 8 h Cefotaxime 12 g/day q 4 h Ceftriaxone 4 g/day q 12 h Ceftazidime 6 g/day q 8 h Gentamicin 7. 5 mg/kq/day q 8 h Meropenem 3 g/day q 8 h Metronidazole 1500 -2000 mg/day q 6 h Nafcillin 9 -12 g/day q 4 h Penicillin G 20 -24 million U/day q 4 h Vancomycin 2 g/day q 2 h
Antibiotics dosage Agent Dosage Ampicillin 12 g/day q 4 h Cefepime 6 g/day q 8 h Cefotaxime 12 g/day q 4 h Ceftriaxone 4 g/day q 12 h Ceftazidime 6 g/day q 8 h Gentamicin 7. 5 mg/kq/day q 8 h Meropenem 3 g/day q 8 h Metronidazole 1500 -2000 mg/day q 6 h Nafcillin 9 -12 g/day q 4 h Penicillin G 20 -24 million U/day q 4 h Vancomycin 2 g/day q 2 h
 Use of corticosteroid The use of corticosteroids such as dexamethasone as adjunctive treatment was significantly associated with a reduction in case-fatality rate and neurologic sequelae Strongly consider in patients with certain types of bacterial meninigitis, such as H influenzae, tuberculous, and pneumococcal meningitis should be administered prior to or during the administration of antimicrobial therapy May associate with decreased penetration into the CSF of some antimicrobials, such as vancomycin Dexamethasone (0. 15 mg/kg per dose q 6 h for 2 -4 d)
Use of corticosteroid The use of corticosteroids such as dexamethasone as adjunctive treatment was significantly associated with a reduction in case-fatality rate and neurologic sequelae Strongly consider in patients with certain types of bacterial meninigitis, such as H influenzae, tuberculous, and pneumococcal meningitis should be administered prior to or during the administration of antimicrobial therapy May associate with decreased penetration into the CSF of some antimicrobials, such as vancomycin Dexamethasone (0. 15 mg/kg per dose q 6 h for 2 -4 d)
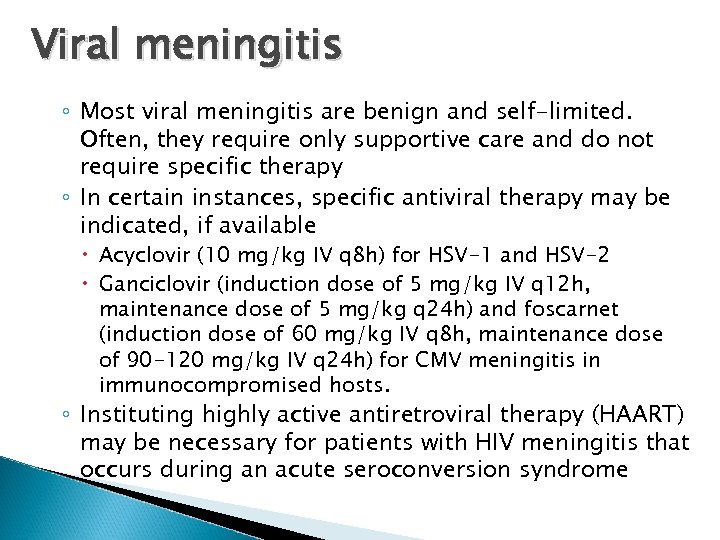 Viral meningitis ◦ Most viral meningitis are benign and self-limited. Often, they require only supportive care and do not require specific therapy ◦ In certain instances, specific antiviral therapy may be indicated, if available Acyclovir (10 mg/kg IV q 8 h) for HSV-1 and HSV-2 Ganciclovir (induction dose of 5 mg/kg IV q 12 h, maintenance dose of 5 mg/kg q 24 h) and foscarnet (induction dose of 60 mg/kg IV q 8 h, maintenance dose of 90 -120 mg/kg IV q 24 h) for CMV meningitis in immunocompromised hosts. ◦ Instituting highly active antiretroviral therapy (HAART) may be necessary for patients with HIV meningitis that occurs during an acute seroconversion syndrome
Viral meningitis ◦ Most viral meningitis are benign and self-limited. Often, they require only supportive care and do not require specific therapy ◦ In certain instances, specific antiviral therapy may be indicated, if available Acyclovir (10 mg/kg IV q 8 h) for HSV-1 and HSV-2 Ganciclovir (induction dose of 5 mg/kg IV q 12 h, maintenance dose of 5 mg/kg q 24 h) and foscarnet (induction dose of 60 mg/kg IV q 8 h, maintenance dose of 90 -120 mg/kg IV q 24 h) for CMV meningitis in immunocompromised hosts. ◦ Instituting highly active antiretroviral therapy (HAART) may be necessary for patients with HIV meningitis that occurs during an acute seroconversion syndrome
 Tuberculous meningitis The demonstration of the acid-fast in the CSF is difficult and usually requires a large volume of CSF The culture for Mycobacterium usually takes several weeks and may delay definitive diagnosis. Nucleic acid amplification for. M tuberculosis have the advantage of a rapid, sensitive, and specific The need for mycobacterial growth in cultures remains because this offers the advantage of performing drug susceptibility assays.
Tuberculous meningitis The demonstration of the acid-fast in the CSF is difficult and usually requires a large volume of CSF The culture for Mycobacterium usually takes several weeks and may delay definitive diagnosis. Nucleic acid amplification for. M tuberculosis have the advantage of a rapid, sensitive, and specific The need for mycobacterial growth in cultures remains because this offers the advantage of performing drug susceptibility assays.
 Tuberculous meningitis ◦ Isoniazid (INH) and pyrazinamide (PZA) attain good CSF levels (approximate blood levels). Rifampin (RIF) penetrates the BBB less efficiently but still attains adequate CSF levels. ◦ use the combination of the first-line drugs (ie, INH, RIF, PZA, ethambutol, streptomycin. ◦ The dosage is similar to what is used for pulmonary tuberculosis (ie, INH 300 mg qd, RIF 600 mg qd, PZA 15 -30 mg/kg qd, ethambutol 15 -25 mg/kg qd, streptomycin 7. 5 mg/kg q 12 h).
Tuberculous meningitis ◦ Isoniazid (INH) and pyrazinamide (PZA) attain good CSF levels (approximate blood levels). Rifampin (RIF) penetrates the BBB less efficiently but still attains adequate CSF levels. ◦ use the combination of the first-line drugs (ie, INH, RIF, PZA, ethambutol, streptomycin. ◦ The dosage is similar to what is used for pulmonary tuberculosis (ie, INH 300 mg qd, RIF 600 mg qd, PZA 15 -30 mg/kg qd, ethambutol 15 -25 mg/kg qd, streptomycin 7. 5 mg/kg q 12 h).
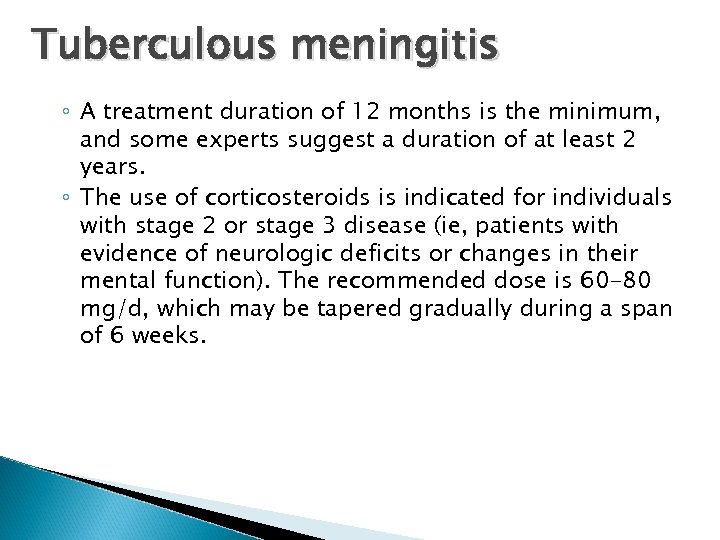 Tuberculous meningitis ◦ A treatment duration of 12 months is the minimum, and some experts suggest a duration of at least 2 years. ◦ The use of corticosteroids is indicated for individuals with stage 2 or stage 3 disease (ie, patients with evidence of neurologic deficits or changes in their mental function). The recommended dose is 60 -80 mg/d, which may be tapered gradually during a span of 6 weeks.
Tuberculous meningitis ◦ A treatment duration of 12 months is the minimum, and some experts suggest a duration of at least 2 years. ◦ The use of corticosteroids is indicated for individuals with stage 2 or stage 3 disease (ie, patients with evidence of neurologic deficits or changes in their mental function). The recommended dose is 60 -80 mg/d, which may be tapered gradually during a span of 6 weeks.
 cryptococcal meningitis Diagnosis : identification of the pathogen in the CSF C neoformans culture from CSF India ink preparation : sensitivity of only 50%, but highly diagnostic if positive CSF cryptococcal antigen : sensitivity of greater than 90% blood cultures and serum cryptococcal antigen to determine if cryptococcal fungemia is present
cryptococcal meningitis Diagnosis : identification of the pathogen in the CSF C neoformans culture from CSF India ink preparation : sensitivity of only 50%, but highly diagnostic if positive CSF cryptococcal antigen : sensitivity of greater than 90% blood cultures and serum cryptococcal antigen to determine if cryptococcal fungemia is present
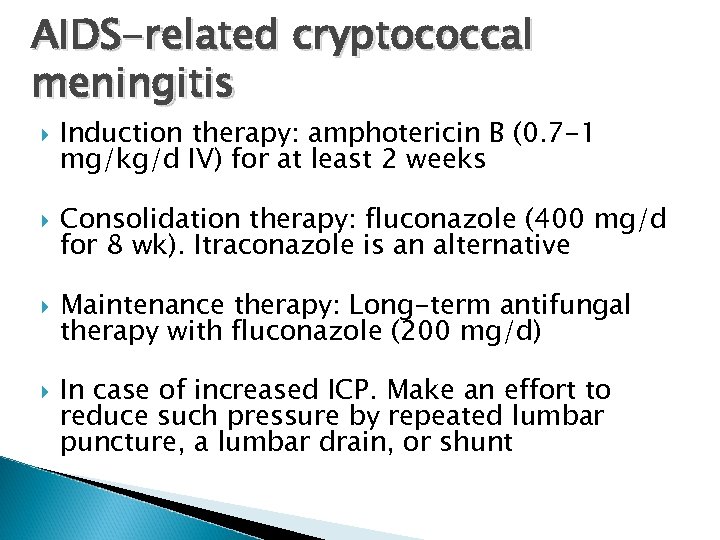 AIDS-related cryptococcal meningitis Induction therapy: amphotericin B (0. 7 -1 mg/kg/d IV) for at least 2 weeks Consolidation therapy: fluconazole (400 mg/d for 8 wk). Itraconazole is an alternative Maintenance therapy: Long-term antifungal therapy with fluconazole (200 mg/d) In case of increased ICP. Make an effort to reduce such pressure by repeated lumbar puncture, a lumbar drain, or shunt
AIDS-related cryptococcal meningitis Induction therapy: amphotericin B (0. 7 -1 mg/kg/d IV) for at least 2 weeks Consolidation therapy: fluconazole (400 mg/d for 8 wk). Itraconazole is an alternative Maintenance therapy: Long-term antifungal therapy with fluconazole (200 mg/d) In case of increased ICP. Make an effort to reduce such pressure by repeated lumbar puncture, a lumbar drain, or shunt
 cryptococcal meningitis in patients without AIDS Induction/consolidation: Administer amphotericin B (0. 7 -1 mg/kg/d) plus flucytosine (100 mg/kg/d) for 2 weeks. Then, administer fluconazole (400 mg/d) for a minimum of 10 weeks. A lumbar puncture is recommended after 2 weeks to document sterilization of the CSF. If the infection persists, longer therapy is recommended. Solid organ transplant recipients require prolonged therapy.
cryptococcal meningitis in patients without AIDS Induction/consolidation: Administer amphotericin B (0. 7 -1 mg/kg/d) plus flucytosine (100 mg/kg/d) for 2 weeks. Then, administer fluconazole (400 mg/d) for a minimum of 10 weeks. A lumbar puncture is recommended after 2 weeks to document sterilization of the CSF. If the infection persists, longer therapy is recommended. Solid organ transplant recipients require prolonged therapy.
 Fungal meningitis ◦ C. immitis oral fluconazole (400 mg/d) or Itraconazole (400 -600 mg/d) Duration of treatment usually is life long. ◦ H capsulatum Amphotericin B at 0. 7 -1 mg/kg/d to complete a total dose of 35 mg/kg Fluconazole (800 mg/d) for an additional 9 -12 months may be used to prevent relapse. ◦ Candida species amphotericin B (0. 7 mg/kg/d)+/- Flucytosine (25 mg/kg qid)
Fungal meningitis ◦ C. immitis oral fluconazole (400 mg/d) or Itraconazole (400 -600 mg/d) Duration of treatment usually is life long. ◦ H capsulatum Amphotericin B at 0. 7 -1 mg/kg/d to complete a total dose of 35 mg/kg Fluconazole (800 mg/d) for an additional 9 -12 months may be used to prevent relapse. ◦ Candida species amphotericin B (0. 7 mg/kg/d)+/- Flucytosine (25 mg/kg qid)
 Syphilitic meningitis The CSF is characterized by mild lymphocytic pleocytosis. elevated CSF protein levels & decreased glucose levels may be observed in 10 -70% of cases. Demonstrate the spirochete by using dark-field or phasecontrast microscopy on specimens collected from skin lesions (eg, chancres and other syphilitic lesions). CSF VDRL : sensitivity of 30 -70% (a negative result does not rule out syphilitic meningitis) and a high specificity (a positive test result suggests the disease). serologic tests to detect syphilis : VDRL test , FTA-Abs , TPHA
Syphilitic meningitis The CSF is characterized by mild lymphocytic pleocytosis. elevated CSF protein levels & decreased glucose levels may be observed in 10 -70% of cases. Demonstrate the spirochete by using dark-field or phasecontrast microscopy on specimens collected from skin lesions (eg, chancres and other syphilitic lesions). CSF VDRL : sensitivity of 30 -70% (a negative result does not rule out syphilitic meningitis) and a high specificity (a positive test result suggests the disease). serologic tests to detect syphilis : VDRL test , FTA-Abs , TPHA
 Syphilitic meningitis penicillin G (2 -4 million U/d IV q 4 h) for 10 -14 days, often followed with benzathine penicillin G 2. 4 million U IM. Alternative : administer procaine penicillin G (2. 4 million U/d IM) plus probenecid (500 mg PO qid) for 14 days, followed by IM benzathine penicillin G (2. 4 million U). Repeat CSF examination : cell count , serologic titers Because penicillin G is treatment of choice, patients who are allergic to penicillin should undergo penicillin desensitization
Syphilitic meningitis penicillin G (2 -4 million U/d IV q 4 h) for 10 -14 days, often followed with benzathine penicillin G 2. 4 million U IM. Alternative : administer procaine penicillin G (2. 4 million U/d IM) plus probenecid (500 mg PO qid) for 14 days, followed by IM benzathine penicillin G (2. 4 million U). Repeat CSF examination : cell count , serologic titers Because penicillin G is treatment of choice, patients who are allergic to penicillin should undergo penicillin desensitization
 Complications : Early increased intracranial pressure (ICP) venous sinus thrombosis subdural empyema brain abscess cranial nerve palsies cerebral infarction result from impaired cerebral blood flow
Complications : Early increased intracranial pressure (ICP) venous sinus thrombosis subdural empyema brain abscess cranial nerve palsies cerebral infarction result from impaired cerebral blood flow
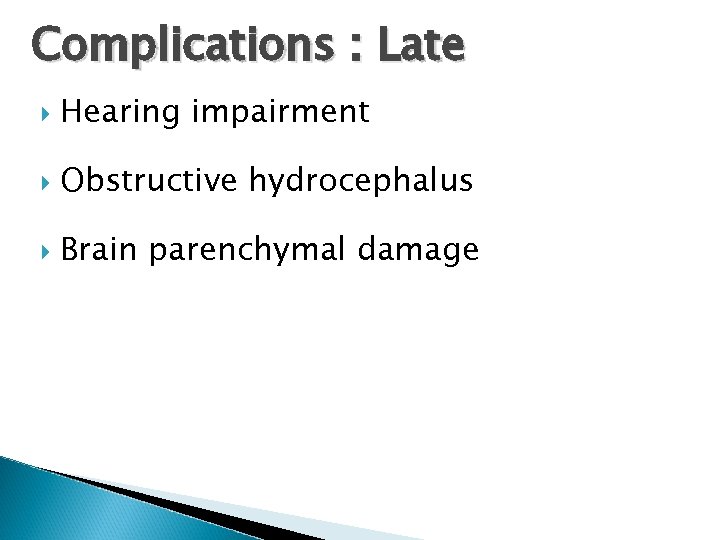 Complications : Late Hearing impairment Obstructive hydrocephalus Brain parenchymal damage
Complications : Late Hearing impairment Obstructive hydrocephalus Brain parenchymal damage
 Further Inpatient Care Monitor the clinical course & response to medical treatment surveillance for the development of complications Seizure precautions are indicated, especially for patients with impaired mental function Proper isolation precautions in cases of invasive meningococcal disease
Further Inpatient Care Monitor the clinical course & response to medical treatment surveillance for the development of complications Seizure precautions are indicated, especially for patients with impaired mental function Proper isolation precautions in cases of invasive meningococcal disease
 Further Inpatient Care Monitor patients for potential adverse effects of medications, such as hypersensitivity reactions, cytopenia, or drug toxicity Drug-level monitoring for some antibiotics such as vancomycin and aminoglycosides
Further Inpatient Care Monitor patients for potential adverse effects of medications, such as hypersensitivity reactions, cytopenia, or drug toxicity Drug-level monitoring for some antibiotics such as vancomycin and aminoglycosides
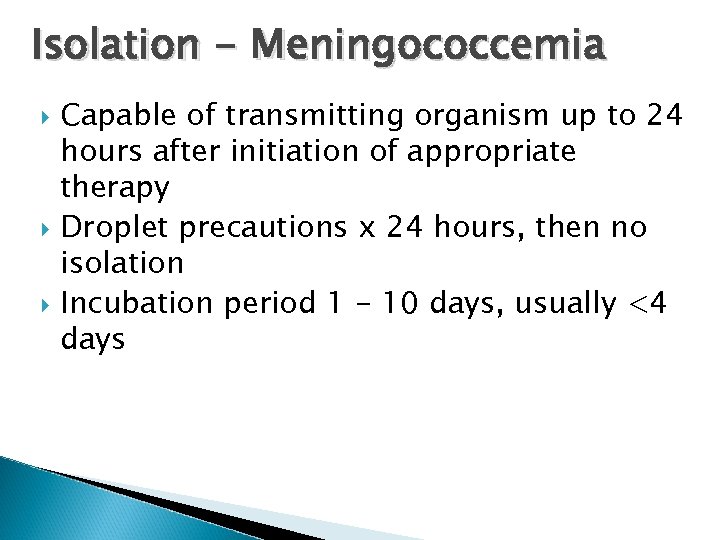 Isolation - Meningococcemia Capable of transmitting organism up to 24 hours after initiation of appropriate therapy Droplet precautions x 24 hours, then no isolation Incubation period 1 - 10 days, usually <4 days
Isolation - Meningococcemia Capable of transmitting organism up to 24 hours after initiation of appropriate therapy Droplet precautions x 24 hours, then no isolation Incubation period 1 - 10 days, usually <4 days
 Meningococcemia - Prophylaxis Persons who have had “intimate contact” w/ oral secretions prior & during 1 st 24 h of antibiotics “Intimate contact” – 300 -800 x risk (kissing, eating/ drinking utensils, mouth-to-mouth, suctioning, intubating) Treat within 24 hours of exposure
Meningococcemia - Prophylaxis Persons who have had “intimate contact” w/ oral secretions prior & during 1 st 24 h of antibiotics “Intimate contact” – 300 -800 x risk (kissing, eating/ drinking utensils, mouth-to-mouth, suctioning, intubating) Treat within 24 hours of exposure
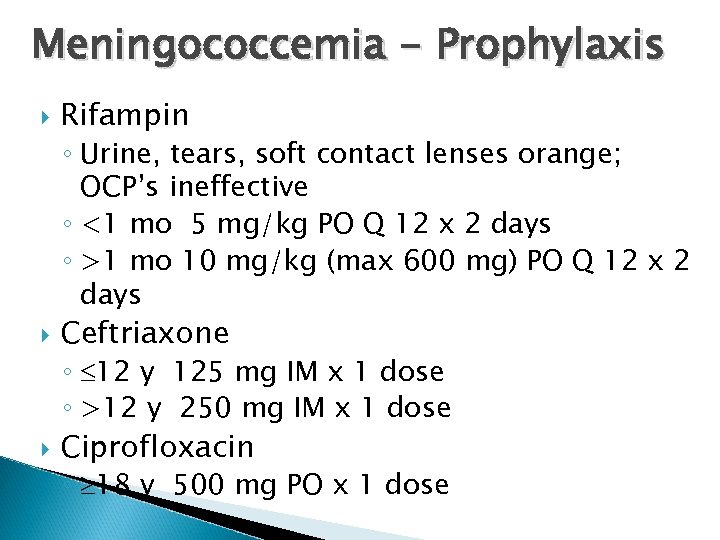 Meningococcemia - Prophylaxis Rifampin ◦ Urine, tears, soft contact lenses orange; OCP’s ineffective ◦ <1 mo 5 mg/kg PO Q 12 x 2 days ◦ >1 mo 10 mg/kg (max 600 mg) PO Q 12 x 2 days Ceftriaxone ◦ 12 y 125 mg IM x 1 dose ◦ >12 y 250 mg IM x 1 dose Ciprofloxacin ◦ 18 y 500 mg PO x 1 dose
Meningococcemia - Prophylaxis Rifampin ◦ Urine, tears, soft contact lenses orange; OCP’s ineffective ◦ <1 mo 5 mg/kg PO Q 12 x 2 days ◦ >1 mo 10 mg/kg (max 600 mg) PO Q 12 x 2 days Ceftriaxone ◦ 12 y 125 mg IM x 1 dose ◦ >12 y 250 mg IM x 1 dose Ciprofloxacin ◦ 18 y 500 mg PO x 1 dose
 Prognosis viral meningitis usually have a good prognosis for recovery. The prognosis is worse for patients at the extremes of age (ie, <2 y, >60 y) and with significant comorbidities and underlying immunodeficiency. Patients presenting with an impaired level of consciousness are at increased risk for developing neurologic sequelae or dying. A seizure during an episode of meningitis also is a risk factor for mortality or neurologic sequelae. The presence of low-level pleocytosis (<20 cells) in patients with bacterial meningitis suggests a poorer outcome.
Prognosis viral meningitis usually have a good prognosis for recovery. The prognosis is worse for patients at the extremes of age (ie, <2 y, >60 y) and with significant comorbidities and underlying immunodeficiency. Patients presenting with an impaired level of consciousness are at increased risk for developing neurologic sequelae or dying. A seizure during an episode of meningitis also is a risk factor for mortality or neurologic sequelae. The presence of low-level pleocytosis (<20 cells) in patients with bacterial meningitis suggests a poorer outcome.
 Prognosis Delay in instituting effective antimicrobial therapy for Acute bacterial meningitis result in increased morbidity and mortality Meningitis caused by S pneumoniae, L monocytogenes, and gram-negative bacilli has a higher case-fatality rate compared to meningitis caused by other bacterial agents. Prognosis of meningitis caused by opportunistic pathogens depends on the underlying immune function of the host. Many of the survivors require lifelong suppressive therapy (eg, long-term fluconazole for suppression in patients with HIV-associated cryptococcal meningitis).
Prognosis Delay in instituting effective antimicrobial therapy for Acute bacterial meningitis result in increased morbidity and mortality Meningitis caused by S pneumoniae, L monocytogenes, and gram-negative bacilli has a higher case-fatality rate compared to meningitis caused by other bacterial agents. Prognosis of meningitis caused by opportunistic pathogens depends on the underlying immune function of the host. Many of the survivors require lifelong suppressive therapy (eg, long-term fluconazole for suppression in patients with HIV-associated cryptococcal meningitis).



