1 регуляция дыхания а 2014-2015 англ лекц.ppt
- Количество слайдов: 110
 Topic: " Regulation of respiration. Peculiarities of respiration under various conditions. Features of breath in children " 16. 02. 2018 1
Topic: " Regulation of respiration. Peculiarities of respiration under various conditions. Features of breath in children " 16. 02. 2018 1
 Purpose: • to Show adaptive activity of respiratory system to various requirements of an organism for maintenance of optimum pressure of gases in blood and tissues according to intensity of a metabolism.
Purpose: • to Show adaptive activity of respiratory system to various requirements of an organism for maintenance of optimum pressure of gases in blood and tissues according to intensity of a metabolism.
 • Pulmonary ventilation is the inflow and outflow of air between the lungs and atmospheric air, which occurs due to rhythmic contractions of respiratory muscles. • The rate, force and pattern of these contractions are adjusted so as to meet body requirements.
• Pulmonary ventilation is the inflow and outflow of air between the lungs and atmospheric air, which occurs due to rhythmic contractions of respiratory muscles. • The rate, force and pattern of these contractions are adjusted so as to meet body requirements.
 16. 02. 2018 4
16. 02. 2018 4
 Brief contents: • 1. Breath regulation. • 2. Methods of studying of functions of the respiratory centers. • 3. The central nervous regulation. • 4. Sensor receptors. Hering-Breuer reflex. • 5. Humoral breath regulation. Central and peripheral chemoreceptors, their value in maintenance of a gas homeostasis. • 6. Regulation of breath at newborns. • 7. Feature regulation of breath at children.
Brief contents: • 1. Breath regulation. • 2. Methods of studying of functions of the respiratory centers. • 3. The central nervous regulation. • 4. Sensor receptors. Hering-Breuer reflex. • 5. Humoral breath regulation. Central and peripheral chemoreceptors, their value in maintenance of a gas homeostasis. • 6. Regulation of breath at newborns. • 7. Feature regulation of breath at children.
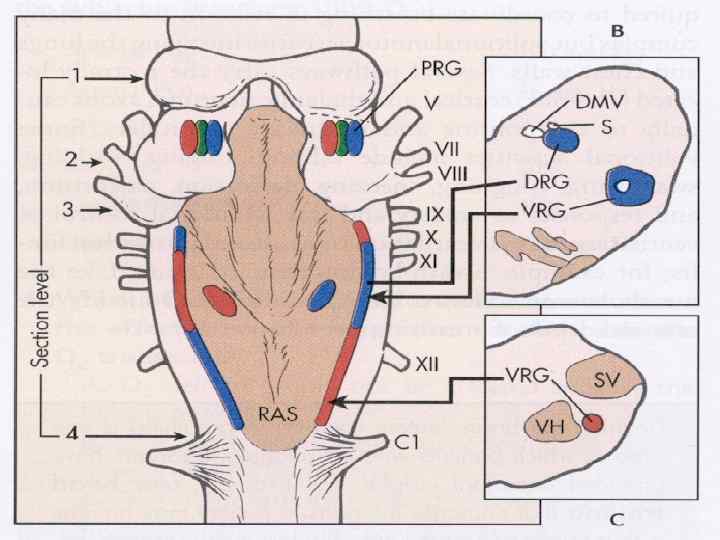
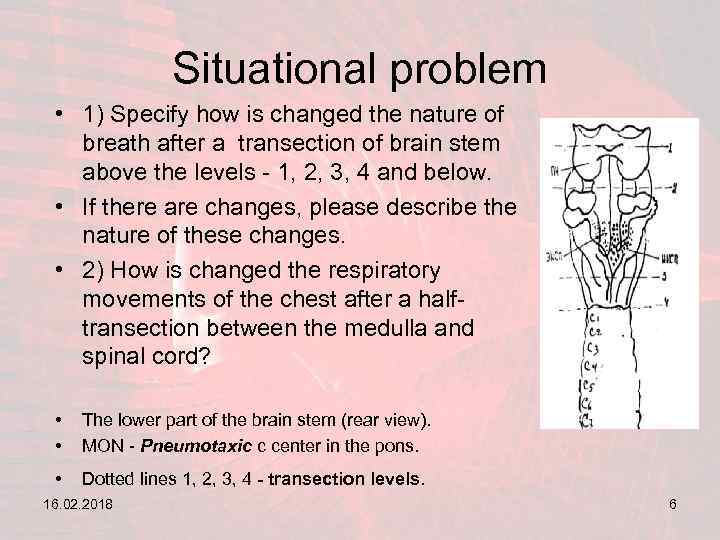 Situational problem • 1) Specify how is changed the nature of breath after a transection of brain stem above the levels - 1, 2, 3, 4 and below. • If there are changes, please describe the nature of these changes. • 2) How is changed the respiratory movements of the chest after a halftransection between the medulla and spinal cord? • • The lower part of the brain stem (rear view). MON - Pneumotaxic c center in the pons. • Dotted lines 1, 2, 3, 4 - transection levels. 16. 02. 2018 6
Situational problem • 1) Specify how is changed the nature of breath after a transection of brain stem above the levels - 1, 2, 3, 4 and below. • If there are changes, please describe the nature of these changes. • 2) How is changed the respiratory movements of the chest after a halftransection between the medulla and spinal cord? • • The lower part of the brain stem (rear view). MON - Pneumotaxic c center in the pons. • Dotted lines 1, 2, 3, 4 - transection levels. 16. 02. 2018 6
 REGULATION OF RESPIRATION
REGULATION OF RESPIRATION
 The pattern of respiration is regulated by two mechanisms namely I Nervous or neural mechanism 16. 02. 2018 II. Chemical mechanism 8
The pattern of respiration is regulated by two mechanisms namely I Nervous or neural mechanism 16. 02. 2018 II. Chemical mechanism 8
 16. 02. 2018 9
16. 02. 2018 9
 I Nervous or neural mechanism 16. 02. 2018 10
I Nervous or neural mechanism 16. 02. 2018 10
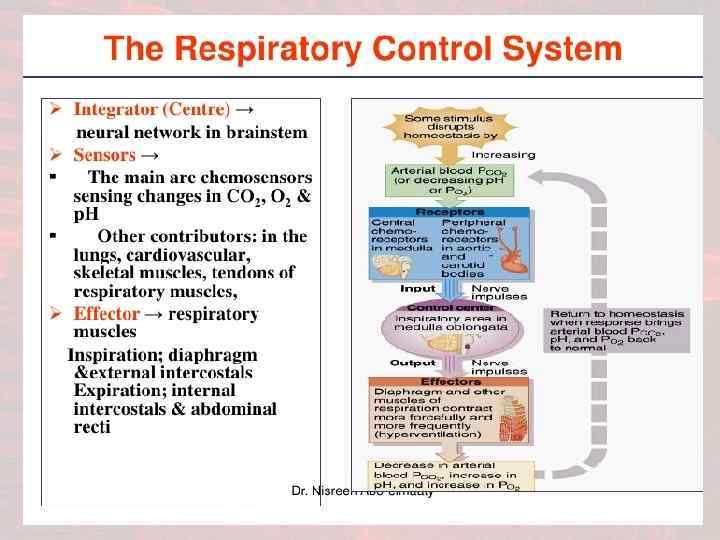
 Neurogenic Regulation • Nervous system maintains a constant homeostatic arterial partial pressure of oxygen & carbon dioxide • Adjustments in rate of alveolar ventilation • Arterial blood gas concentrations hardly altered by exercise or stress
Neurogenic Regulation • Nervous system maintains a constant homeostatic arterial partial pressure of oxygen & carbon dioxide • Adjustments in rate of alveolar ventilation • Arterial blood gas concentrations hardly altered by exercise or stress
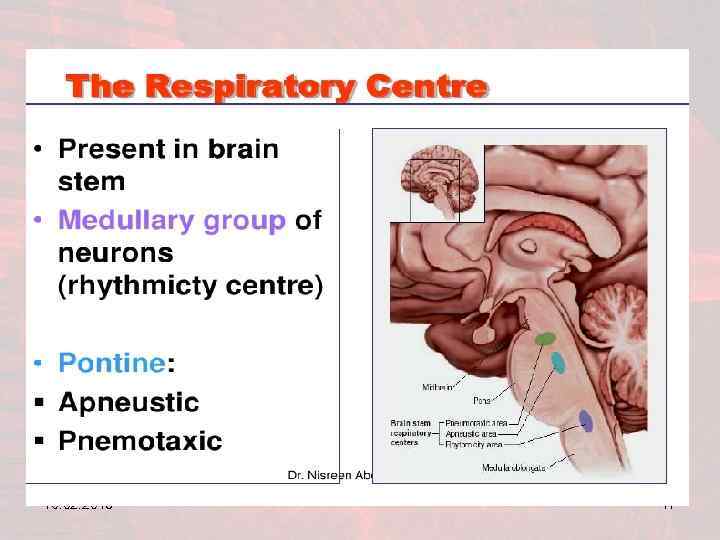
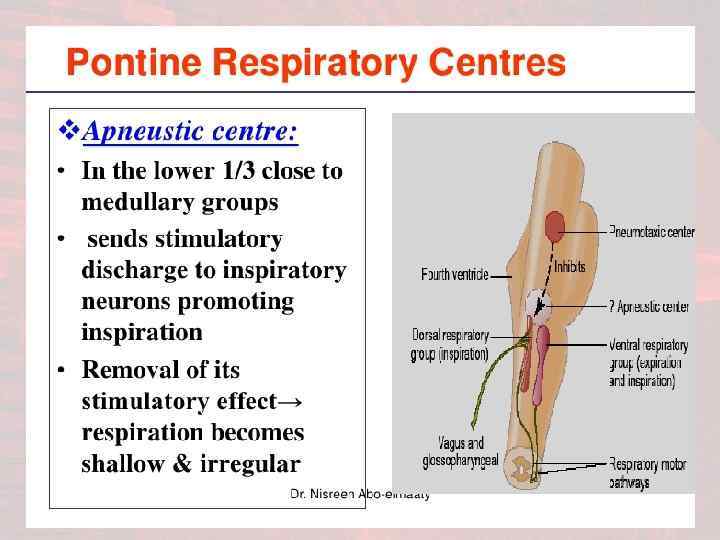
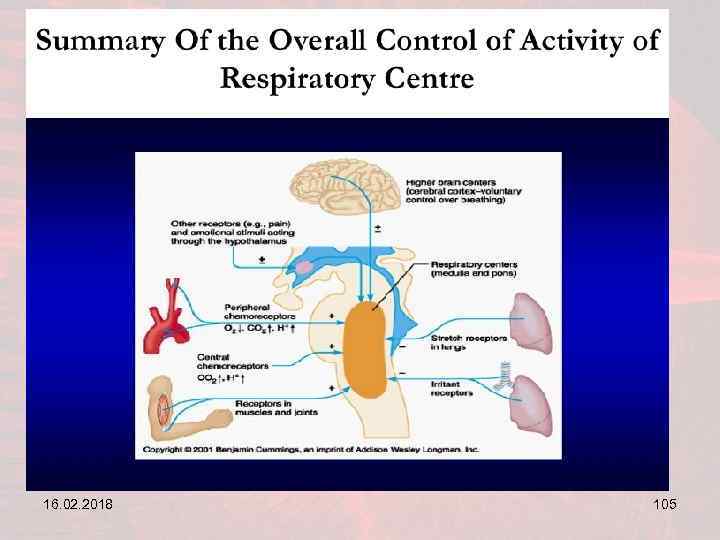
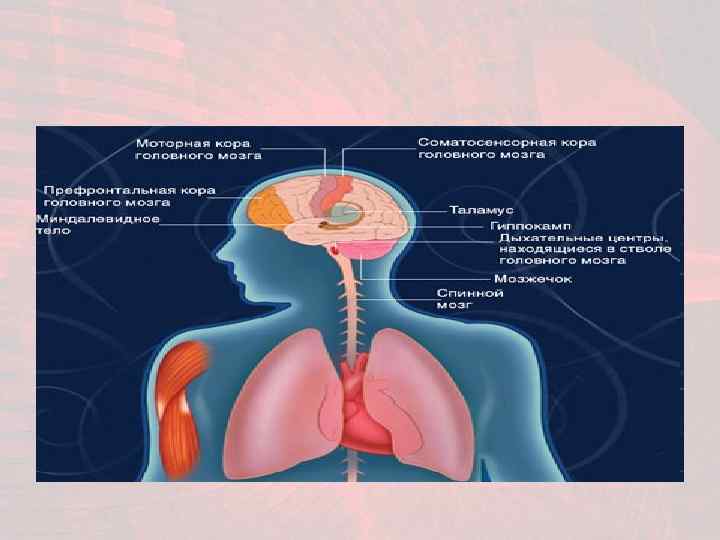
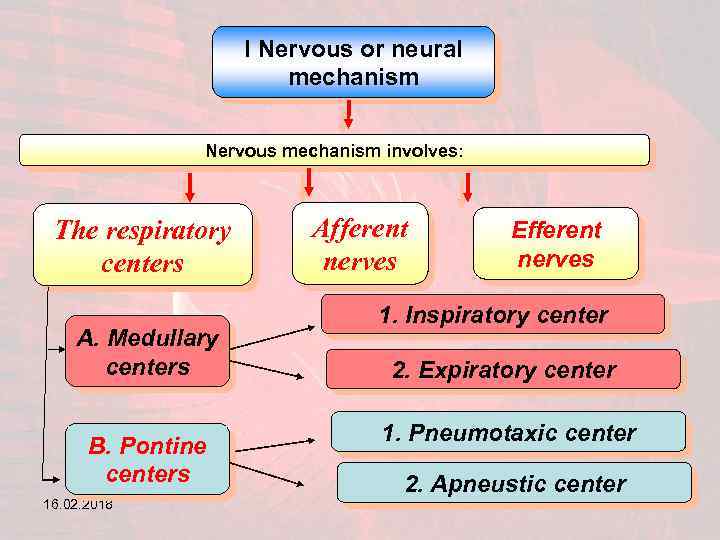 I Nervous or neural mechanism Nervous mechanism involves: The respiratory centers A. Medullary centers B. Pontine centers 16. 02. 2018 Afferent nerves Efferent nerves 1. Inspiratory center 2. Expiratory center 1. Pneumotaxic center 2. Apneustic center 12
I Nervous or neural mechanism Nervous mechanism involves: The respiratory centers A. Medullary centers B. Pontine centers 16. 02. 2018 Afferent nerves Efferent nerves 1. Inspiratory center 2. Expiratory center 1. Pneumotaxic center 2. Apneustic center 12
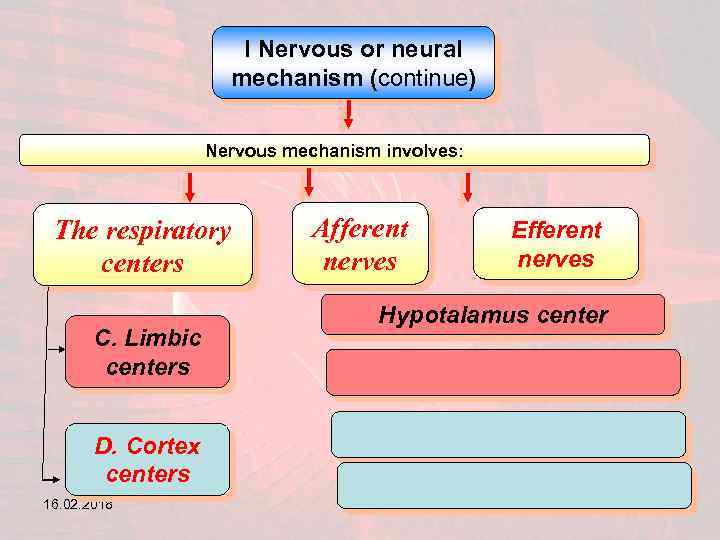 I Nervous or neural mechanism (continue) Nervous mechanism involves: The respiratory centers C. Limbic centers Afferent nerves Efferent nerves Hypotalamus center D. Cortex centers 16. 02. 2018 13
I Nervous or neural mechanism (continue) Nervous mechanism involves: The respiratory centers C. Limbic centers Afferent nerves Efferent nerves Hypotalamus center D. Cortex centers 16. 02. 2018 13
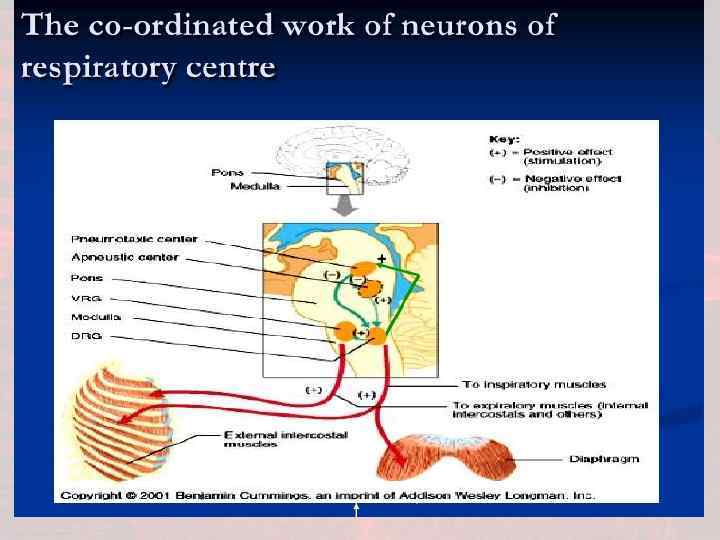
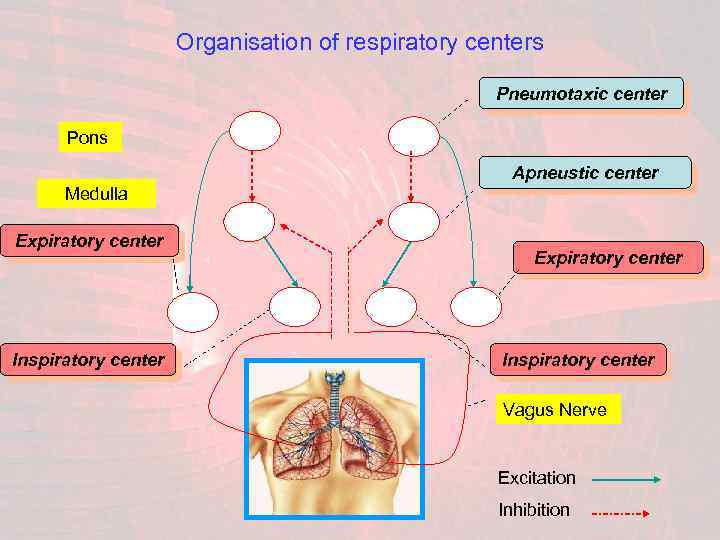 Organisation of respiratory centers Pneumotaxic center Pons Apneustic center Medulla Expiratory center Inspiratory center Vagus Nerve Excitation Inhibition
Organisation of respiratory centers Pneumotaxic center Pons Apneustic center Medulla Expiratory center Inspiratory center Vagus Nerve Excitation Inhibition
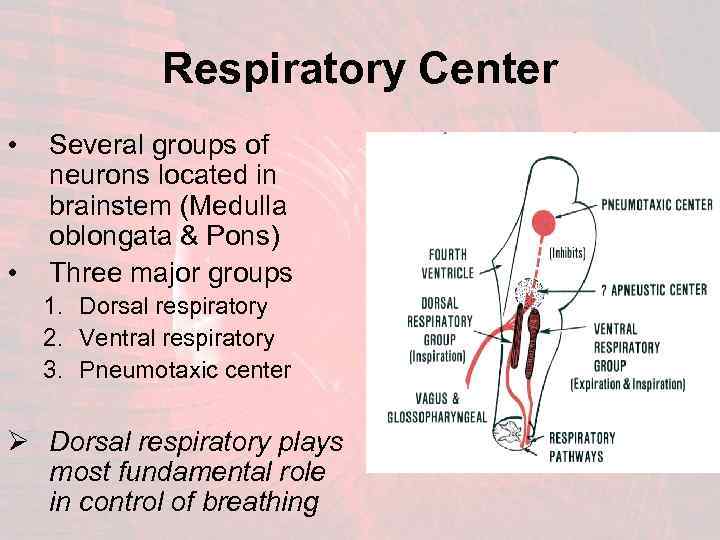 Respiratory Center • • Several groups of neurons located in brainstem (Medulla oblongata & Pons) Three major groups 1. Dorsal respiratory 2. Ventral respiratory 3. Pneumotaxic center Ø Dorsal respiratory plays most fundamental role in control of breathing
Respiratory Center • • Several groups of neurons located in brainstem (Medulla oblongata & Pons) Three major groups 1. Dorsal respiratory 2. Ventral respiratory 3. Pneumotaxic center Ø Dorsal respiratory plays most fundamental role in control of breathing
 16. 02. 2018 17
16. 02. 2018 17
 16. 02. 2018 18
16. 02. 2018 18
 16. 02. 2018 19
16. 02. 2018 19
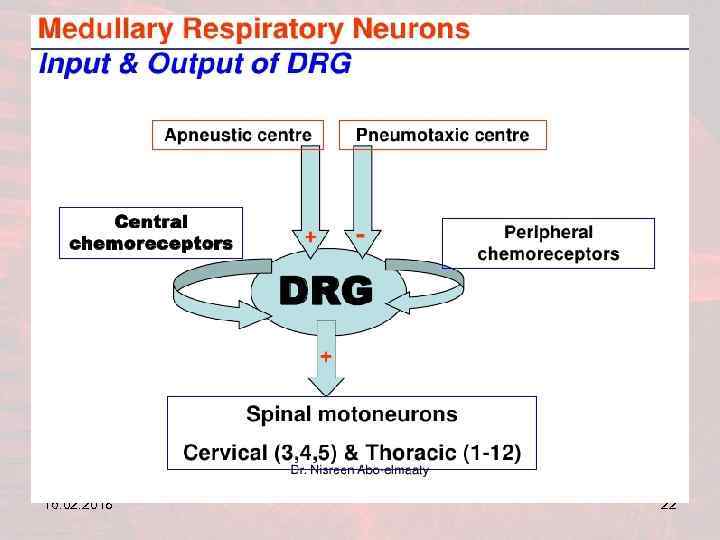
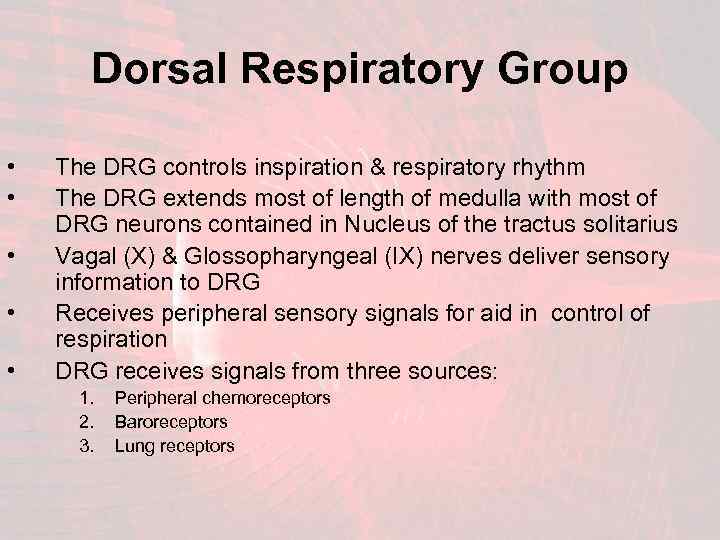 Dorsal Respiratory Group • • • The DRG controls inspiration & respiratory rhythm The DRG extends most of length of medulla with most of DRG neurons contained in Nucleus of the tractus solitarius Vagal (X) & Glossopharyngeal (IX) nerves deliver sensory information to DRG Receives peripheral sensory signals for aid in control of respiration DRG receives signals from three sources: 1. 2. 3. Peripheral chemoreceptors Baroreceptors Lung receptors
Dorsal Respiratory Group • • • The DRG controls inspiration & respiratory rhythm The DRG extends most of length of medulla with most of DRG neurons contained in Nucleus of the tractus solitarius Vagal (X) & Glossopharyngeal (IX) nerves deliver sensory information to DRG Receives peripheral sensory signals for aid in control of respiration DRG receives signals from three sources: 1. 2. 3. Peripheral chemoreceptors Baroreceptors Lung receptors
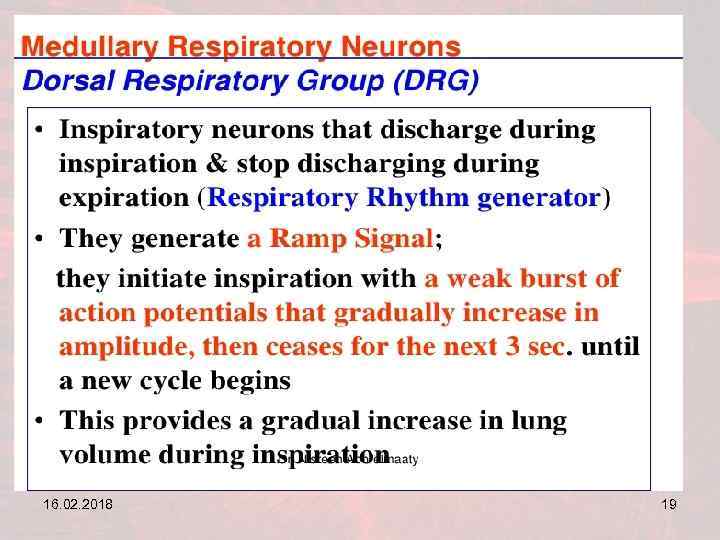
 Rhythmical Inspiratory Rhythm • The DRG generates the basic rhythm of respiration • Neurons emits repetitive bursts of inspiratory action potential • Cause of these rhythmic discharges has not been determined but believed to involve adjacent areas of medulla
Rhythmical Inspiratory Rhythm • The DRG generates the basic rhythm of respiration • Neurons emits repetitive bursts of inspiratory action potential • Cause of these rhythmic discharges has not been determined but believed to involve adjacent areas of medulla
 16. 02. 2018 22
16. 02. 2018 22
 16. 02. 2018 23
16. 02. 2018 23
 Inspiratory “RAMP” Signal • Motor signal transmitted from the DRG to the diaphragm is not an instantaneous action potential burst • Signal begins weakly and increases steadily in a ‘ramp -like’ manner for 2 seconds to cause contraction of diaphragm (Inspiration) • The excitatory signal abruptly stops for next 3 seconds to allow relaxation of diaphragm (Expiration) • The advantage of the ramp signal is that it causes a steady increase in inspiratory volume
Inspiratory “RAMP” Signal • Motor signal transmitted from the DRG to the diaphragm is not an instantaneous action potential burst • Signal begins weakly and increases steadily in a ‘ramp -like’ manner for 2 seconds to cause contraction of diaphragm (Inspiration) • The excitatory signal abruptly stops for next 3 seconds to allow relaxation of diaphragm (Expiration) • The advantage of the ramp signal is that it causes a steady increase in inspiratory volume
 Control of Inspiratory “RAMP” • Two ways the ‘Ramp’ is controlled: 1. Control of the rate of ramp signal increases • • Ramp signal increases more rapidly during activity Lungs fill more rapidly 2. Control of limiting point at which ramp ceases • • • Earlier the ramp ceases; the shorter the inspiration duration This also shortens the duration of expiration Frequency of respiration increases
Control of Inspiratory “RAMP” • Two ways the ‘Ramp’ is controlled: 1. Control of the rate of ramp signal increases • • Ramp signal increases more rapidly during activity Lungs fill more rapidly 2. Control of limiting point at which ramp ceases • • • Earlier the ramp ceases; the shorter the inspiration duration This also shortens the duration of expiration Frequency of respiration increases
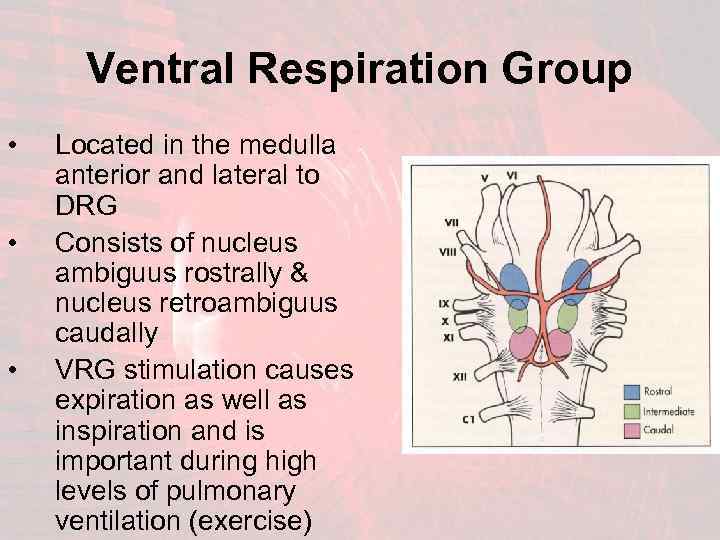 Ventral Respiration Group • • • Located in the medulla anterior and lateral to DRG Consists of nucleus ambiguus rostrally & nucleus retroambiguus caudally VRG stimulation causes expiration as well as inspiration and is important during high levels of pulmonary ventilation (exercise)
Ventral Respiration Group • • • Located in the medulla anterior and lateral to DRG Consists of nucleus ambiguus rostrally & nucleus retroambiguus caudally VRG stimulation causes expiration as well as inspiration and is important during high levels of pulmonary ventilation (exercise)
 VRG: Inspiration & Expiration The VRG functions differently from DRG Ø Ø VRG inactive during normal quiet respiration VRG does not appear to participate in basic rhythmic oscillation which controls respiration VRG contributes to respiratory drive to increase pulmonary ventilation VRG stimulates abdominal muscles to assist in forced exhalation
VRG: Inspiration & Expiration The VRG functions differently from DRG Ø Ø VRG inactive during normal quiet respiration VRG does not appear to participate in basic rhythmic oscillation which controls respiration VRG contributes to respiratory drive to increase pulmonary ventilation VRG stimulates abdominal muscles to assist in forced exhalation
 16. 02. 2018 28
16. 02. 2018 28
 16. 02. 2018 29
16. 02. 2018 29
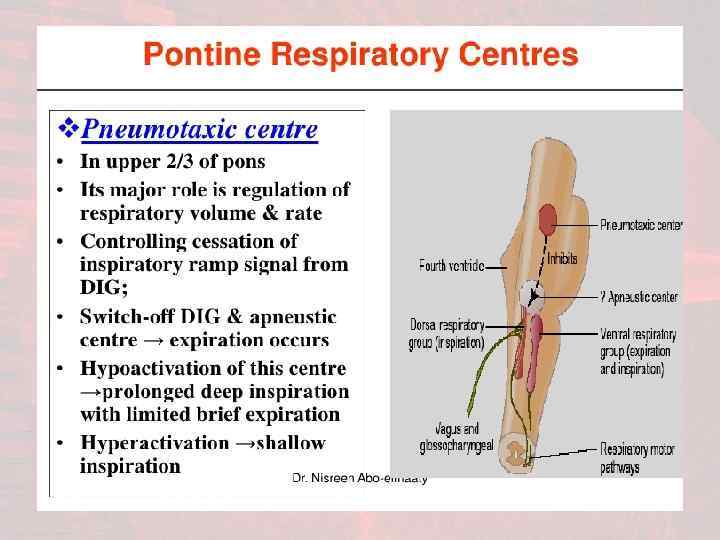
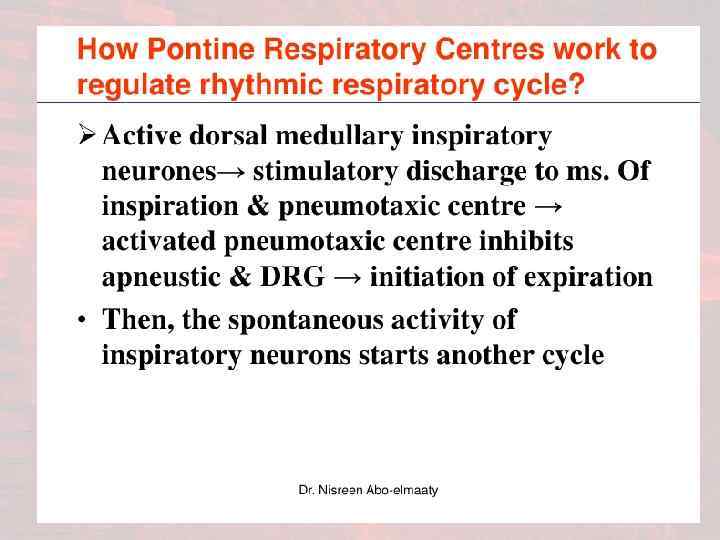
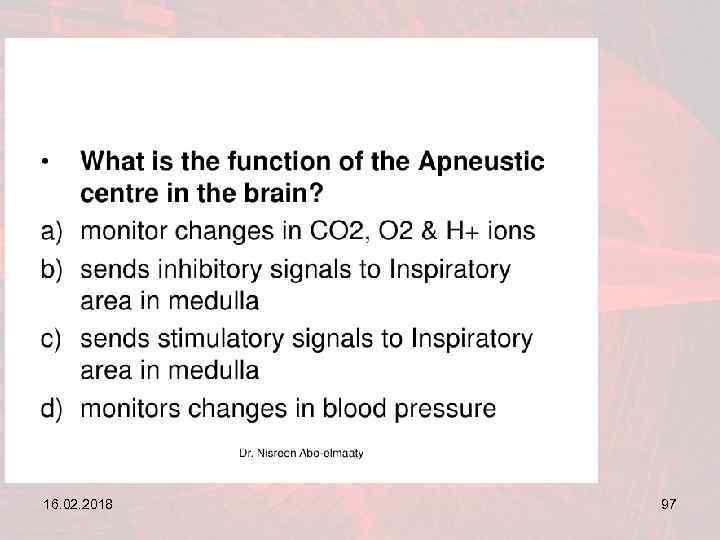
 ‘Apneustic’ Center • A center of neurons in lower pons with a poorly understood purpose or function – Signals the DRG to prevent or retard the ‘switch-off’ of inspiratory ramp stimuli – The lungs become almost completely filled with air with only occasional short expiratory gasps • The apneustic center operates in association with the pneumotaxic center to control the intensity of inspiration
‘Apneustic’ Center • A center of neurons in lower pons with a poorly understood purpose or function – Signals the DRG to prevent or retard the ‘switch-off’ of inspiratory ramp stimuli – The lungs become almost completely filled with air with only occasional short expiratory gasps • The apneustic center operates in association with the pneumotaxic center to control the intensity of inspiration
 16. 02. 2018 31
16. 02. 2018 31
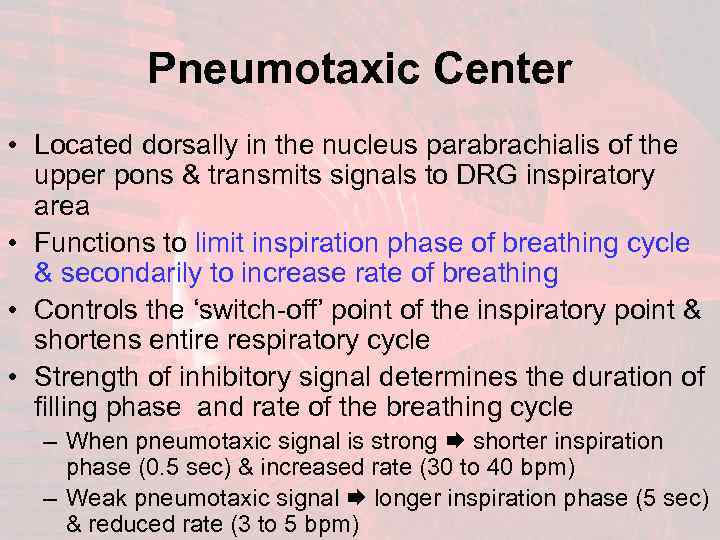 Pneumotaxic Center • Located dorsally in the nucleus parabrachialis of the upper pons & transmits signals to DRG inspiratory area • Functions to limit inspiration phase of breathing cycle & secondarily to increase rate of breathing • Controls the ‘switch-off’ point of the inspiratory point & shortens entire respiratory cycle • Strength of inhibitory signal determines the duration of filling phase and rate of the breathing cycle – When pneumotaxic signal is strong shorter inspiration phase (0. 5 sec) & increased rate (30 to 40 bpm) – Weak pneumotaxic signal longer inspiration phase (5 sec) & reduced rate (3 to 5 bpm)
Pneumotaxic Center • Located dorsally in the nucleus parabrachialis of the upper pons & transmits signals to DRG inspiratory area • Functions to limit inspiration phase of breathing cycle & secondarily to increase rate of breathing • Controls the ‘switch-off’ point of the inspiratory point & shortens entire respiratory cycle • Strength of inhibitory signal determines the duration of filling phase and rate of the breathing cycle – When pneumotaxic signal is strong shorter inspiration phase (0. 5 sec) & increased rate (30 to 40 bpm) – Weak pneumotaxic signal longer inspiration phase (5 sec) & reduced rate (3 to 5 bpm)
 16. 02. 2018 33
16. 02. 2018 33
 16. 02. 2018 34
16. 02. 2018 34
 • Chemical Control of Respiration 16. 02. 2018 35
• Chemical Control of Respiration 16. 02. 2018 35
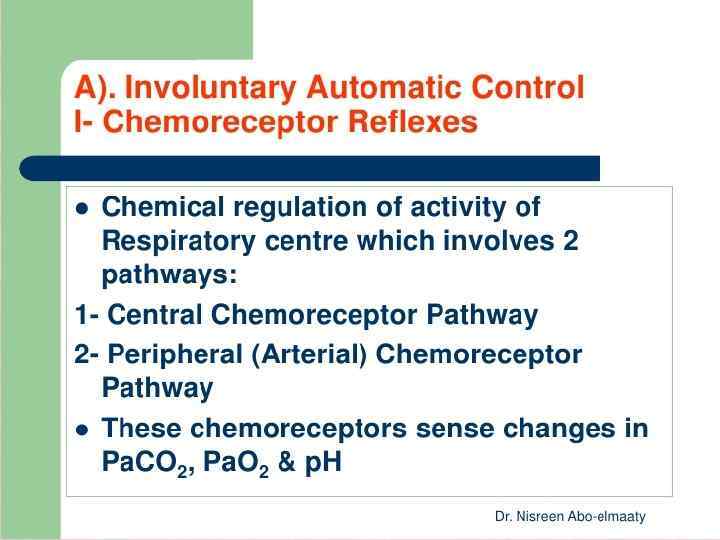
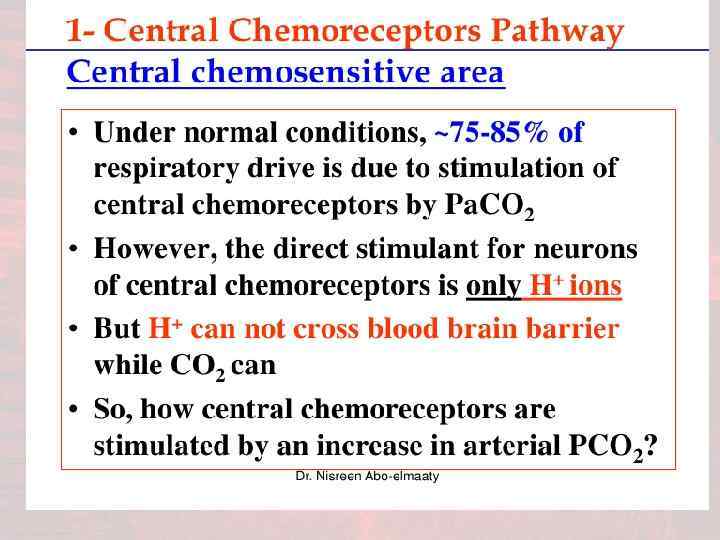
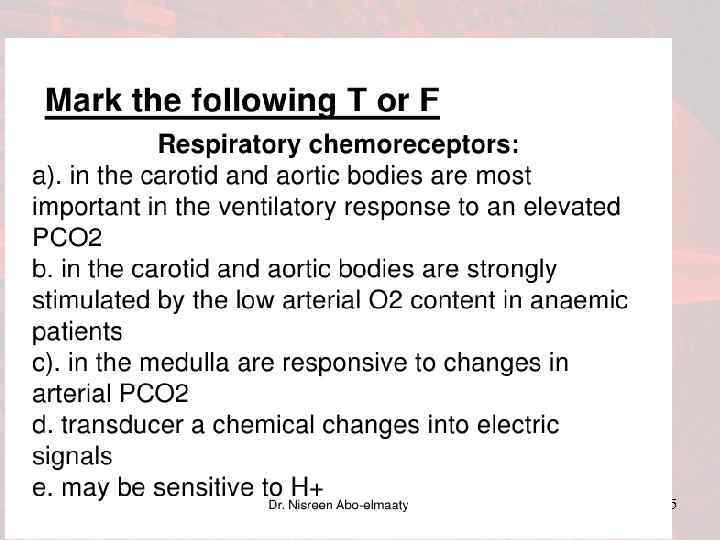
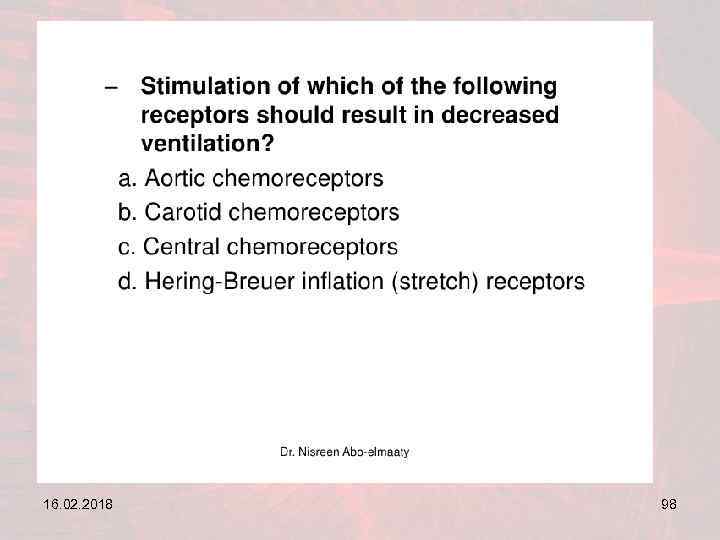
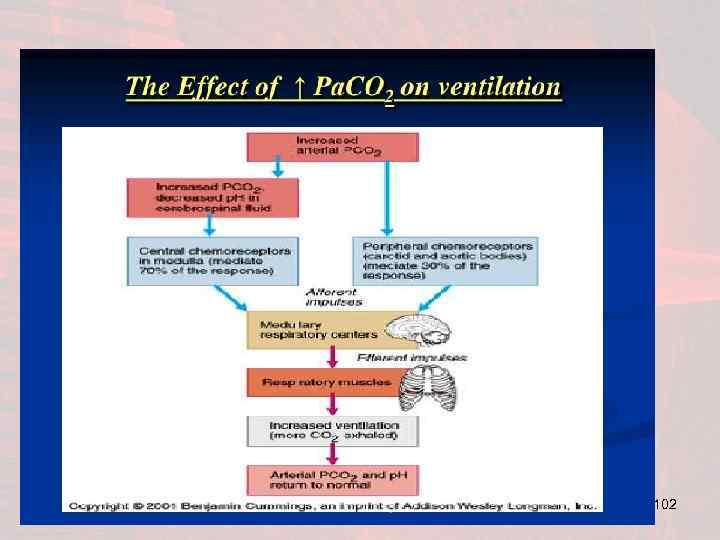
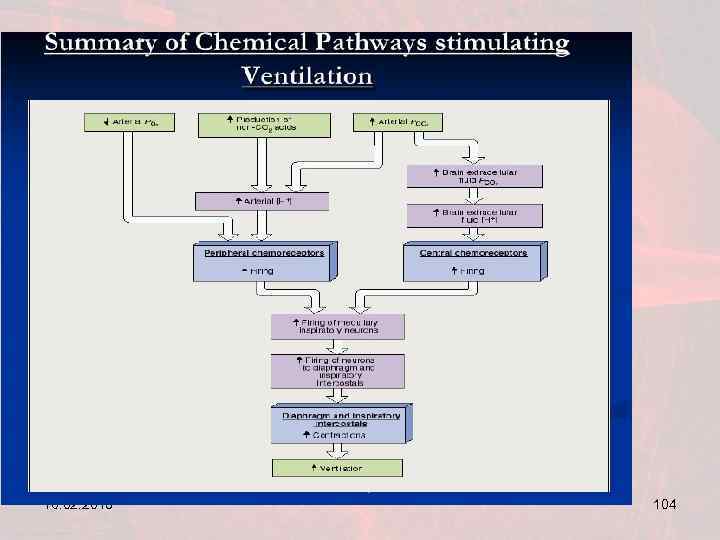
 Chemical Control of Respiration • Excess carbon dioxide or hydrogen ions in blood act directly on the respiratory center to increase strength of both inspiratory & expiratory motor signals • Oxygen does not have a direct effect on respiratory centers but acts on peripheral chemoreceptors in carotid & aortic bodies
Chemical Control of Respiration • Excess carbon dioxide or hydrogen ions in blood act directly on the respiratory center to increase strength of both inspiratory & expiratory motor signals • Oxygen does not have a direct effect on respiratory centers but acts on peripheral chemoreceptors in carotid & aortic bodies
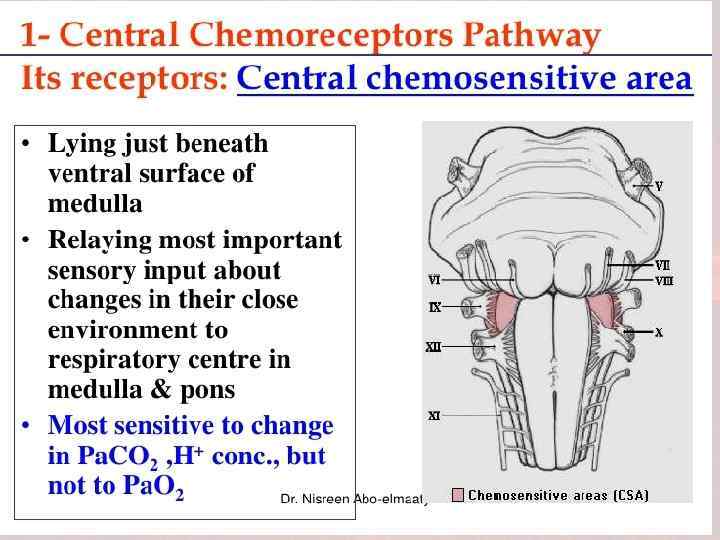
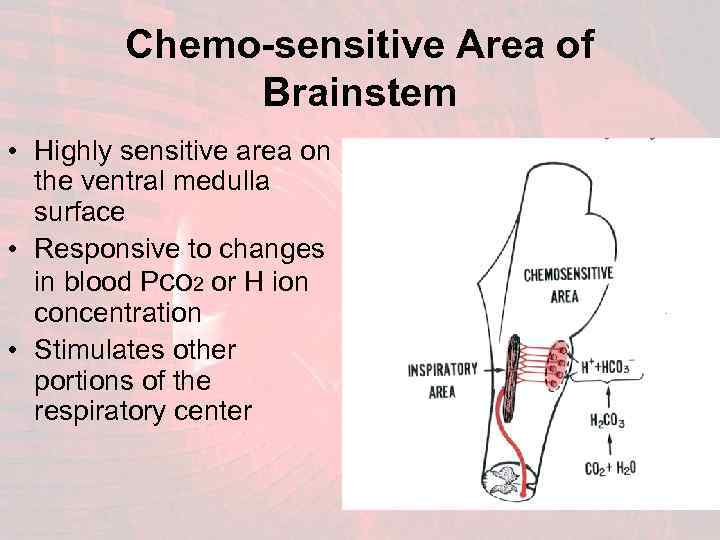 Chemo-sensitive Area of Brainstem • Highly sensitive area on the ventral medulla surface • Responsive to changes in blood Pco 2 or H ion concentration • Stimulates other portions of the respiratory center
Chemo-sensitive Area of Brainstem • Highly sensitive area on the ventral medulla surface • Responsive to changes in blood Pco 2 or H ion concentration • Stimulates other portions of the respiratory center
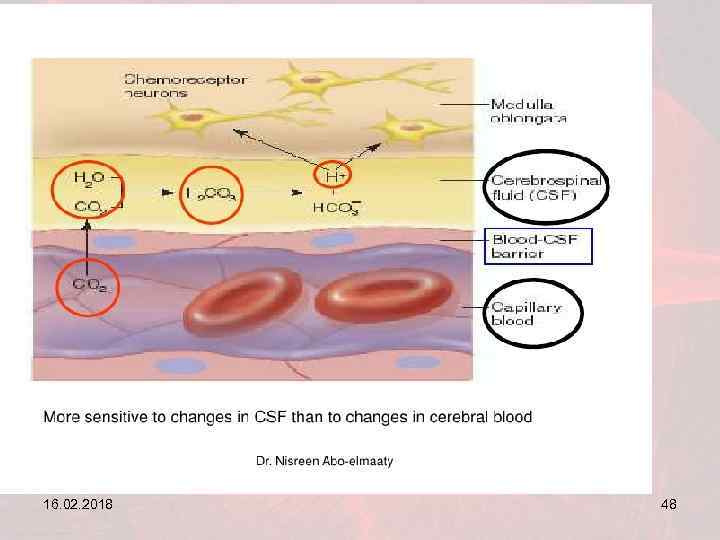
 Response to Hydrogen Ions • Hydrogen ions have an important direct stimulus to chemosensitive neurons • [H] ions do not easily cross the blood-brain barrier • Changes in the blood [H] concentration have less effect in stimulating the chemosensitive neurons than changes in blood carbon dioxide • CO 2 believed to cause stimulation of these neurons secondarily by changing the H ion concentration
Response to Hydrogen Ions • Hydrogen ions have an important direct stimulus to chemosensitive neurons • [H] ions do not easily cross the blood-brain barrier • Changes in the blood [H] concentration have less effect in stimulating the chemosensitive neurons than changes in blood carbon dioxide • CO 2 believed to cause stimulation of these neurons secondarily by changing the H ion concentration
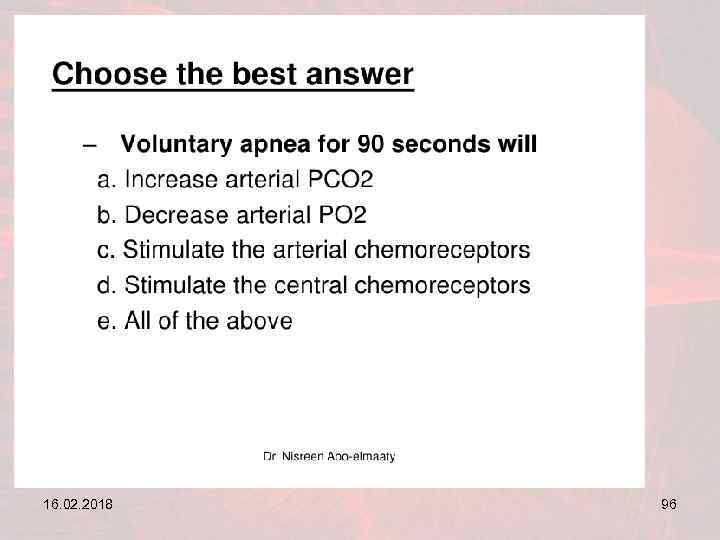
 Effects of Blood Carbon Dioxide • Respiratory center activity is increased very strongly by elevations in blood carbon dioxide levels • CO 2 has potent direct effect, via [H], on the chemosensitive area • CO 2 is highly permeable to blood-brain barrier so blood & brain concentrations are equal • CO 2 reacts with H 2 O to form carbonic acid which dissociates into hydrogen & bicarbonate ions in interstitial fluid of medulla or CSF • The released hydrogen ions in brain stimulate respiratory center activity
Effects of Blood Carbon Dioxide • Respiratory center activity is increased very strongly by elevations in blood carbon dioxide levels • CO 2 has potent direct effect, via [H], on the chemosensitive area • CO 2 is highly permeable to blood-brain barrier so blood & brain concentrations are equal • CO 2 reacts with H 2 O to form carbonic acid which dissociates into hydrogen & bicarbonate ions in interstitial fluid of medulla or CSF • The released hydrogen ions in brain stimulate respiratory center activity
 Decreased Stimulatory Effect • Excitation of respiratory center is great in the first hours of the carbon dioxide increase • After first 1 to 2 days of carbon dioxide exposure the stimulatory respiration response declines • The effect decreases to about a fifth the initial response • The decline results from renal adjustment of hydrogen concentration back to normal • Changes in blood CO 2 concentration has potent acute effect on controlling respiration drive but a weak chronic effect after a few days of adaptation • COPD pts have a blunted response to increased CO 2
Decreased Stimulatory Effect • Excitation of respiratory center is great in the first hours of the carbon dioxide increase • After first 1 to 2 days of carbon dioxide exposure the stimulatory respiration response declines • The effect decreases to about a fifth the initial response • The decline results from renal adjustment of hydrogen concentration back to normal • Changes in blood CO 2 concentration has potent acute effect on controlling respiration drive but a weak chronic effect after a few days of adaptation • COPD pts have a blunted response to increased CO 2
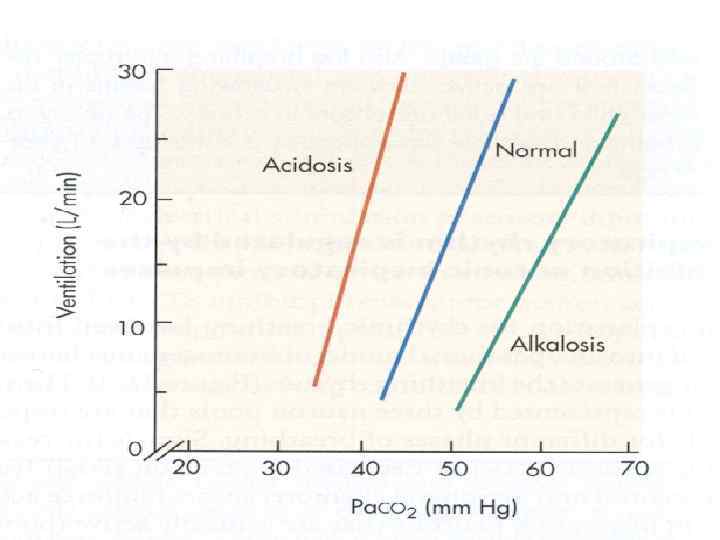
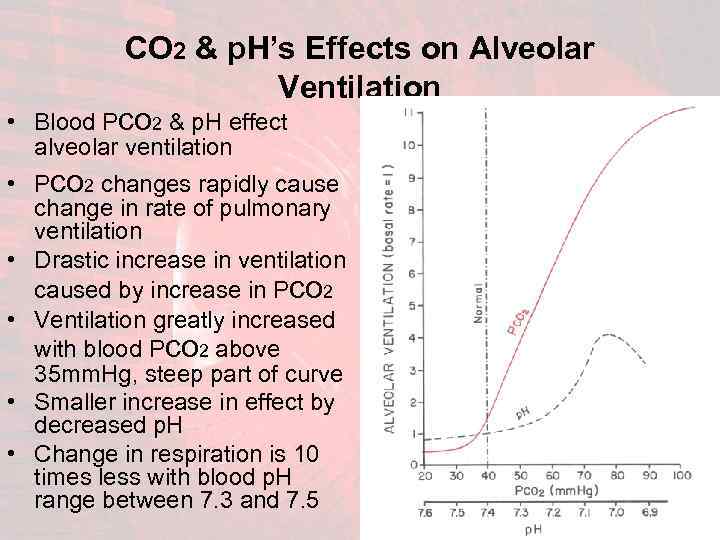 • CO 2 & p. H’s Effects on Alveolar Ventilation Blood Pco 2 & p. H effect alveolar ventilation • Pco 2 changes rapidly cause change in rate of pulmonary ventilation • Drastic increase in ventilation caused by increase in Pco 2 • Ventilation greatly increased with blood Pco 2 above 35 mm. Hg, steep part of curve • Smaller increase in effect by decreased p. H • Change in respiration is 10 times less with blood p. H range between 7. 3 and 7. 5
• CO 2 & p. H’s Effects on Alveolar Ventilation Blood Pco 2 & p. H effect alveolar ventilation • Pco 2 changes rapidly cause change in rate of pulmonary ventilation • Drastic increase in ventilation caused by increase in Pco 2 • Ventilation greatly increased with blood Pco 2 above 35 mm. Hg, steep part of curve • Smaller increase in effect by decreased p. H • Change in respiration is 10 times less with blood p. H range between 7. 3 and 7. 5
 Oxygen’s Effect on Respiration • Changes in oxygen have virtually no direct effect on respiratory center to alter respiratory drive • Changes in O 2 concentration acts indirectly by peripheral receptors to alter respiratory drive • Proper delivery of oxygen occurs despite significant changes in lung ventilation • Hemoglobin-oxygen buffer system delivers normal amounts of O 2 to tissues over wide range of pulmonary O 2 partial pressures (60 mm. Hg to 1000 mm. Hg) • Because of the large O 2 reserve created by this buffer system the respiratory center is not affected by oxygen changes as drastically as the respiratory center responds to Pco 2 changes • Blood oxygen levels below Po 2 of 70 mm. Hg are sensed by peripheral chemoreceptors
Oxygen’s Effect on Respiration • Changes in oxygen have virtually no direct effect on respiratory center to alter respiratory drive • Changes in O 2 concentration acts indirectly by peripheral receptors to alter respiratory drive • Proper delivery of oxygen occurs despite significant changes in lung ventilation • Hemoglobin-oxygen buffer system delivers normal amounts of O 2 to tissues over wide range of pulmonary O 2 partial pressures (60 mm. Hg to 1000 mm. Hg) • Because of the large O 2 reserve created by this buffer system the respiratory center is not affected by oxygen changes as drastically as the respiratory center responds to Pco 2 changes • Blood oxygen levels below Po 2 of 70 mm. Hg are sensed by peripheral chemoreceptors
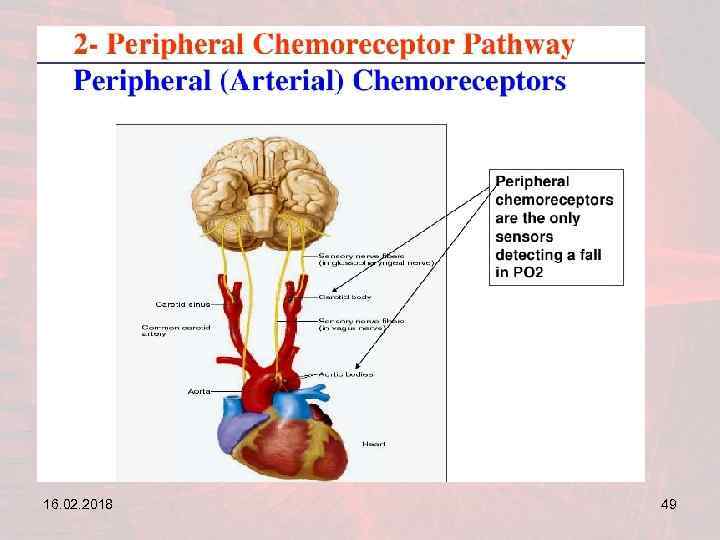
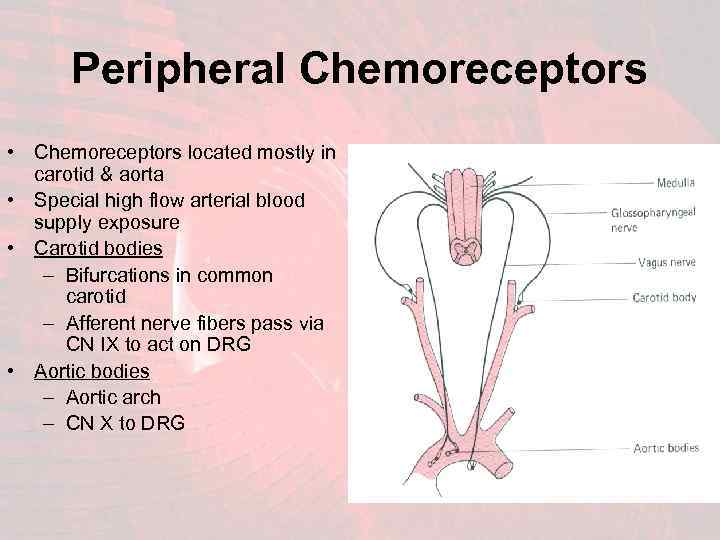 Peripheral Chemoreceptors • Chemoreceptors located mostly in carotid & aorta • Special high flow arterial blood supply exposure • Carotid bodies – Bifurcations in common carotid – Afferent nerve fibers pass via CN IX to act on DRG • Aortic bodies – Aortic arch – CN X to DRG (IX) (X)
Peripheral Chemoreceptors • Chemoreceptors located mostly in carotid & aorta • Special high flow arterial blood supply exposure • Carotid bodies – Bifurcations in common carotid – Afferent nerve fibers pass via CN IX to act on DRG • Aortic bodies – Aortic arch – CN X to DRG (IX) (X)
 16. 02. 2018 44
16. 02. 2018 44
 16. 02. 2018 45
16. 02. 2018 45
 16. 02. 2018 46
16. 02. 2018 46
 16. 02. 2018 47
16. 02. 2018 47
 16. 02. 2018 48
16. 02. 2018 48
 16. 02. 2018 49
16. 02. 2018 49
 16. 02. 2018 50
16. 02. 2018 50
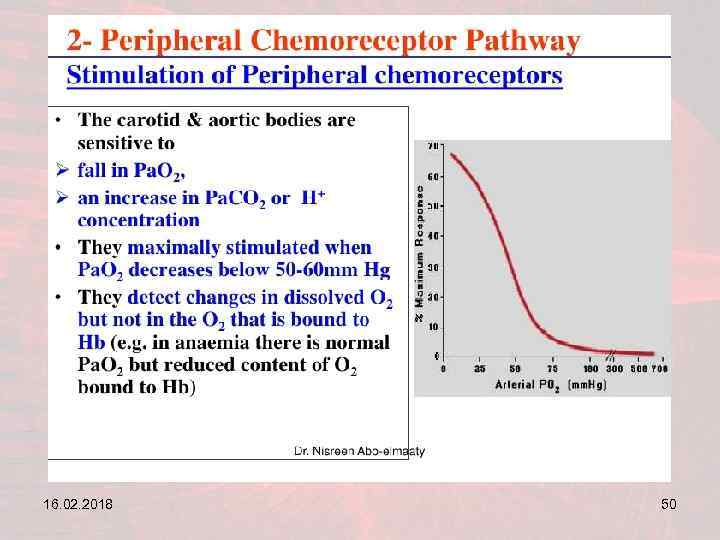
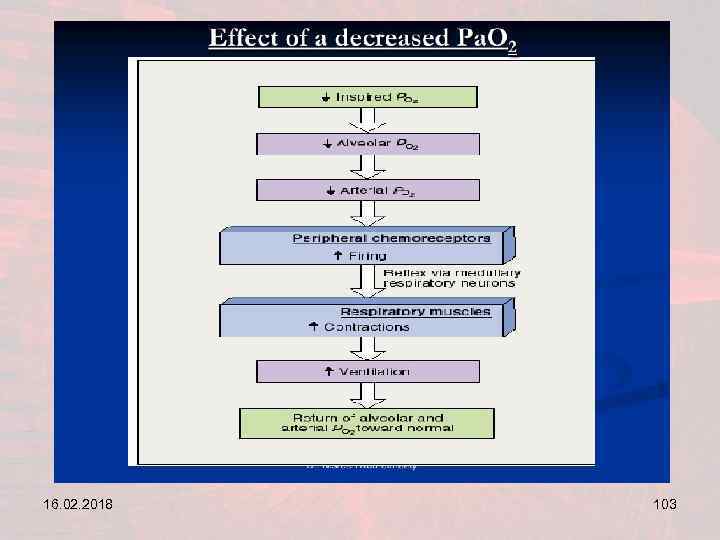
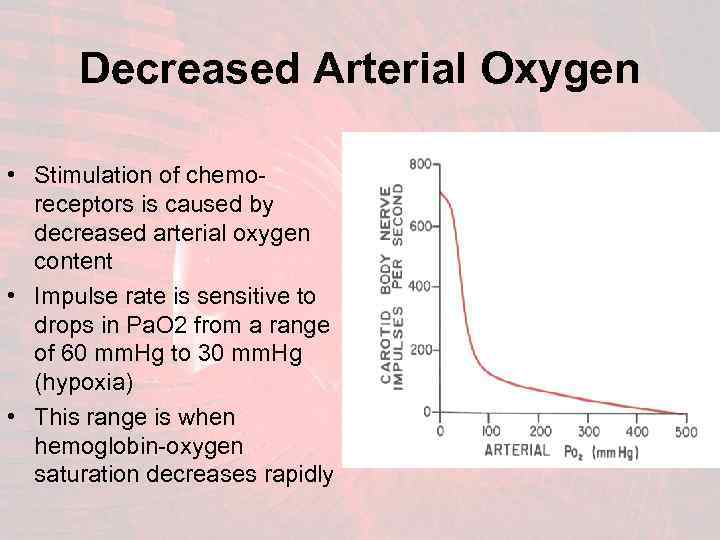 Decreased Arterial Oxygen • Stimulation of chemoreceptors is caused by decreased arterial oxygen content • Impulse rate is sensitive to drops in Pa. O 2 from a range of 60 mm. Hg to 30 mm. Hg (hypoxia) • This range is when hemoglobin-oxygen saturation decreases rapidly
Decreased Arterial Oxygen • Stimulation of chemoreceptors is caused by decreased arterial oxygen content • Impulse rate is sensitive to drops in Pa. O 2 from a range of 60 mm. Hg to 30 mm. Hg (hypoxia) • This range is when hemoglobin-oxygen saturation decreases rapidly
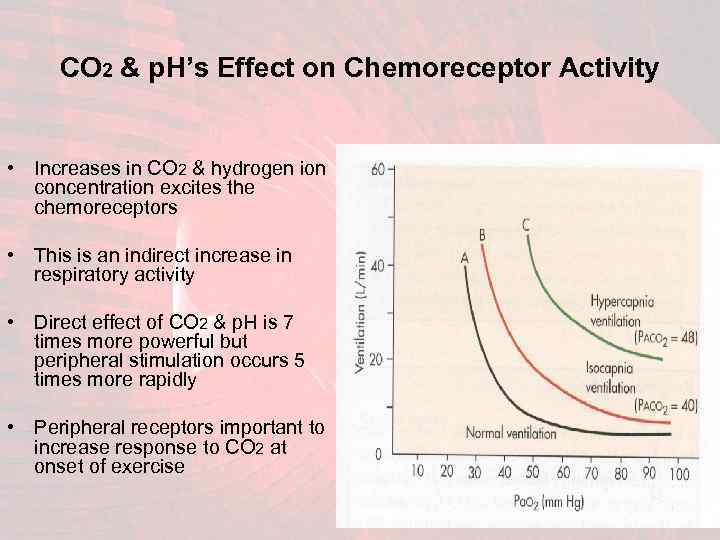 CO 2 & p. H’s Effect on Chemoreceptor Activity • Increases in CO 2 & hydrogen ion concentration excites the chemoreceptors • This is an indirect increase in respiratory activity • Direct effect of CO 2 & p. H is 7 times more powerful but peripheral stimulation occurs 5 times more rapidly • Peripheral receptors important to increase response to CO 2 at onset of exercise
CO 2 & p. H’s Effect on Chemoreceptor Activity • Increases in CO 2 & hydrogen ion concentration excites the chemoreceptors • This is an indirect increase in respiratory activity • Direct effect of CO 2 & p. H is 7 times more powerful but peripheral stimulation occurs 5 times more rapidly • Peripheral receptors important to increase response to CO 2 at onset of exercise
 Mechanism of Chemoreptor Stimulation • Exact means of low PO 2 stimulation of nerve endings in carotid & aortic bodies is unknown • Glomus cells are glandular-like cells synapsing with nerve endings in carotid & aortic bodies • Glomus cells may function as chemoreceptors which stimulate nerve endings • Other studies suggest nerve endings directly sensitive to low PO 2
Mechanism of Chemoreptor Stimulation • Exact means of low PO 2 stimulation of nerve endings in carotid & aortic bodies is unknown • Glomus cells are glandular-like cells synapsing with nerve endings in carotid & aortic bodies • Glomus cells may function as chemoreceptors which stimulate nerve endings • Other studies suggest nerve endings directly sensitive to low PO 2
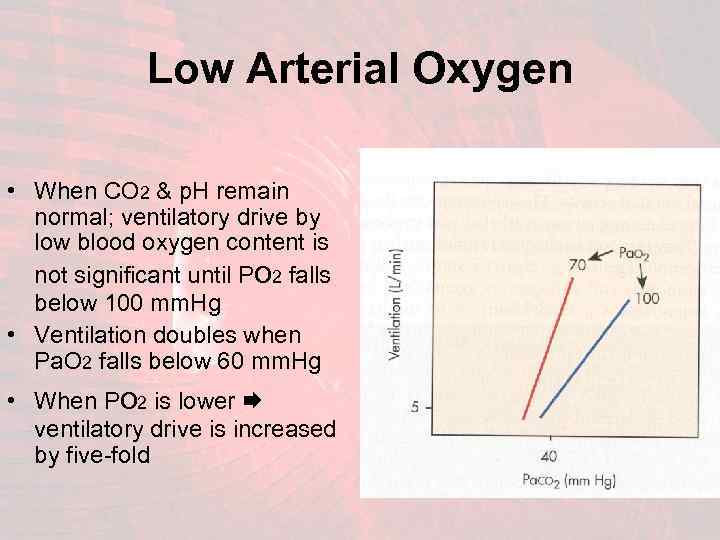 Low Arterial Oxygen • When CO 2 & p. H remain normal; ventilatory drive by low blood oxygen content is not significant until Po 2 falls below 100 mm. Hg • Ventilation doubles when Pa. O 2 falls below 60 mm. Hg • When Po 2 is lower ventilatory drive is increased by five-fold
Low Arterial Oxygen • When CO 2 & p. H remain normal; ventilatory drive by low blood oxygen content is not significant until Po 2 falls below 100 mm. Hg • Ventilation doubles when Pa. O 2 falls below 60 mm. Hg • When Po 2 is lower ventilatory drive is increased by five-fold
 Control of Respiratory Activity • The intensity of respiratory control signals is increased or decreased to match the ventilatory needs of the body • The ultimate goal of respiration is to maintain proper concentrations of oxygen, carbon dioxide & hydrogen ions in the tissue • Respiration activity is highly responsive to these changes
Control of Respiratory Activity • The intensity of respiratory control signals is increased or decreased to match the ventilatory needs of the body • The ultimate goal of respiration is to maintain proper concentrations of oxygen, carbon dioxide & hydrogen ions in the tissue • Respiration activity is highly responsive to these changes
 16. 02. 2018 56
16. 02. 2018 56
 16. 02. 2018 57
16. 02. 2018 57
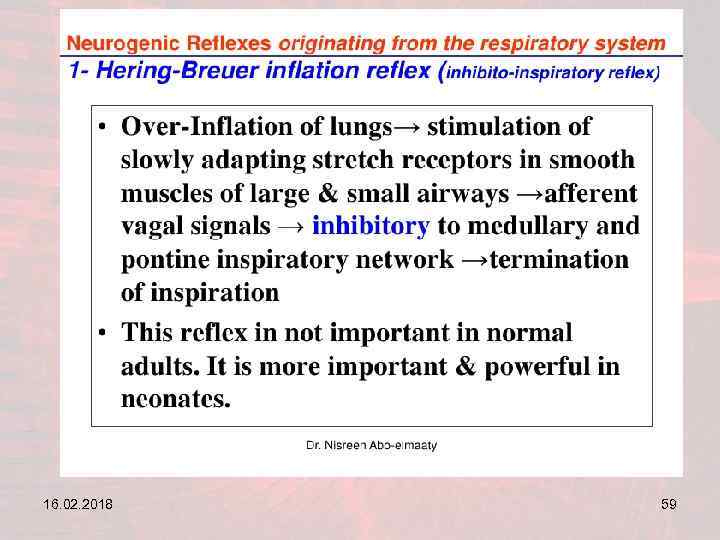
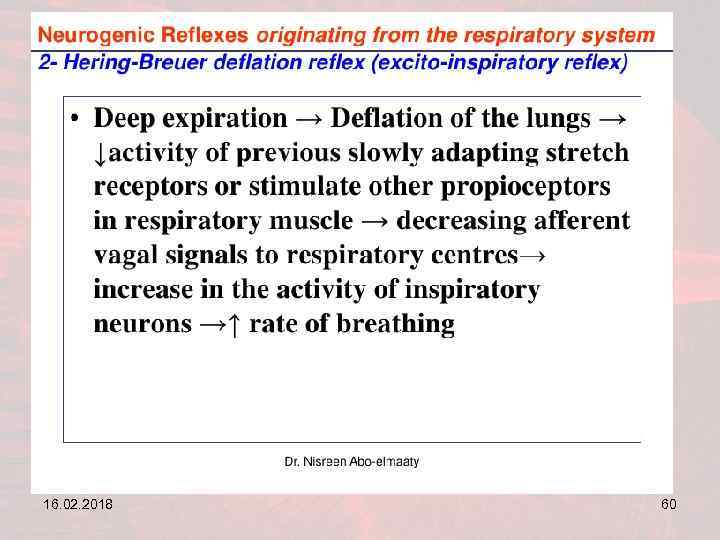
 The Hering-Breuer Reflex • A protective feed-back reflex which limits the over-inflation of lungs • Stretch receptors are located in muscular portions of bronchi & bronchioles • These receptors transmit signals via the vagus nerve (X) to the DRG when lung is overstretched (TV > 1. 5 L) • Feedback response switches off the inspiratory ramp & stops further inflation • This reflex also increases the rate of respiration
The Hering-Breuer Reflex • A protective feed-back reflex which limits the over-inflation of lungs • Stretch receptors are located in muscular portions of bronchi & bronchioles • These receptors transmit signals via the vagus nerve (X) to the DRG when lung is overstretched (TV > 1. 5 L) • Feedback response switches off the inspiratory ramp & stops further inflation • This reflex also increases the rate of respiration
 16. 02. 2018 59
16. 02. 2018 59
 16. 02. 2018 60
16. 02. 2018 60
 16. 02. 2018 61
16. 02. 2018 61
 16. 02. 2018 62
16. 02. 2018 62
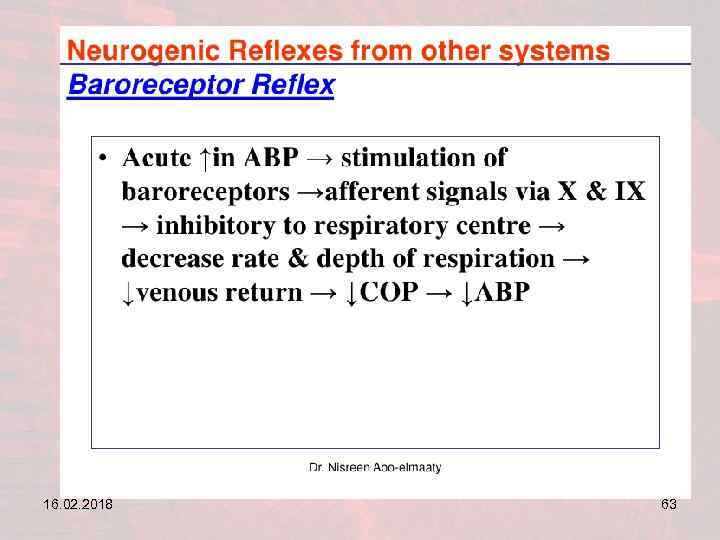 16. 02. 2018 63
16. 02. 2018 63
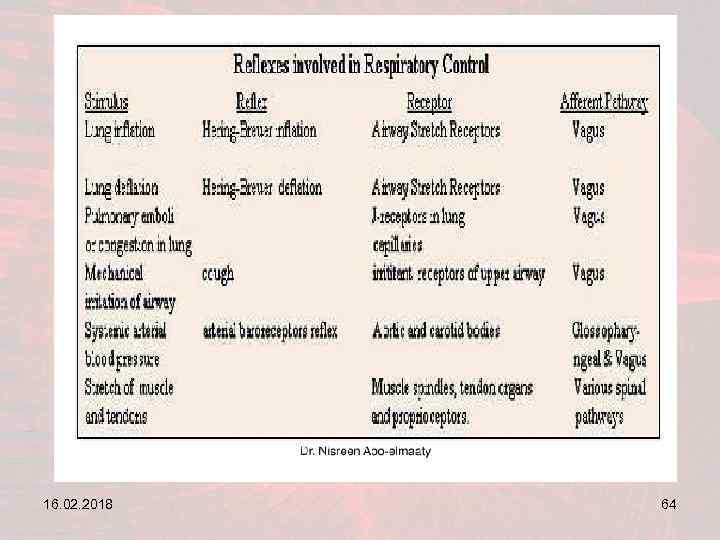 16. 02. 2018 64
16. 02. 2018 64
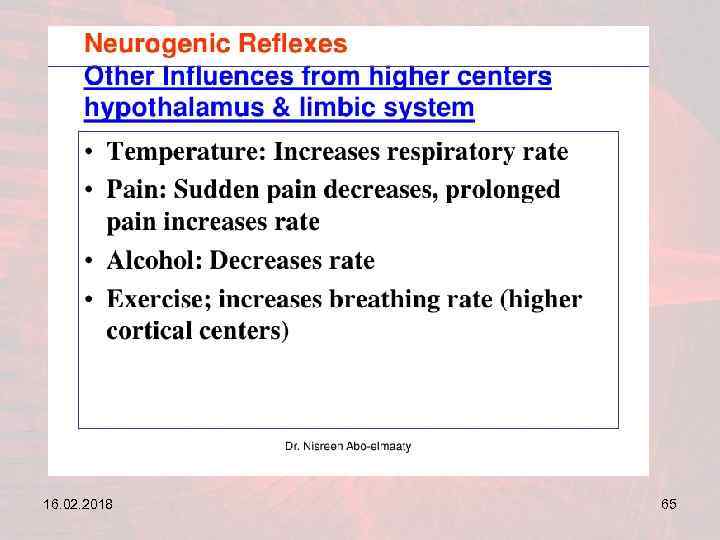 16. 02. 2018 65
16. 02. 2018 65
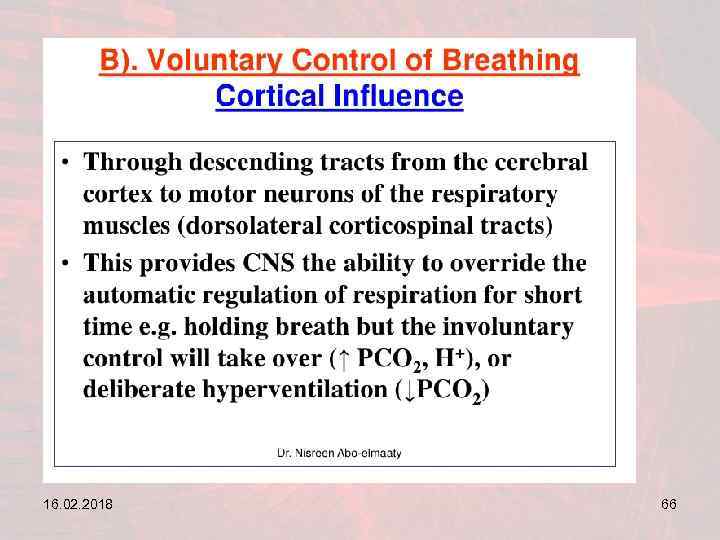 16. 02. 2018 66
16. 02. 2018 66
 16. 02. 2018 67
16. 02. 2018 67
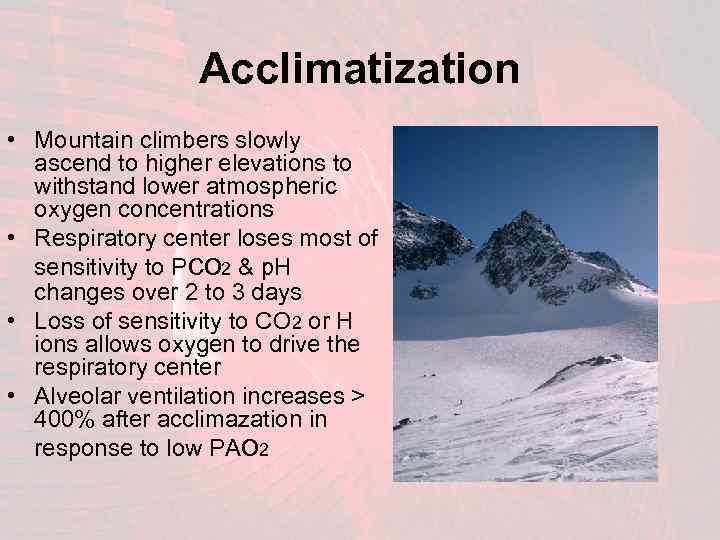 Acclimatization • Mountain climbers slowly ascend to higher elevations to withstand lower atmospheric oxygen concentrations • Respiratory center loses most of sensitivity to Pco 2 & p. H changes over 2 to 3 days • Loss of sensitivity to CO 2 or H ions allows oxygen to drive the respiratory center • Alveolar ventilation increases > 400% after acclimazation in response to low PAo 2
Acclimatization • Mountain climbers slowly ascend to higher elevations to withstand lower atmospheric oxygen concentrations • Respiratory center loses most of sensitivity to Pco 2 & p. H changes over 2 to 3 days • Loss of sensitivity to CO 2 or H ions allows oxygen to drive the respiratory center • Alveolar ventilation increases > 400% after acclimazation in response to low PAo 2
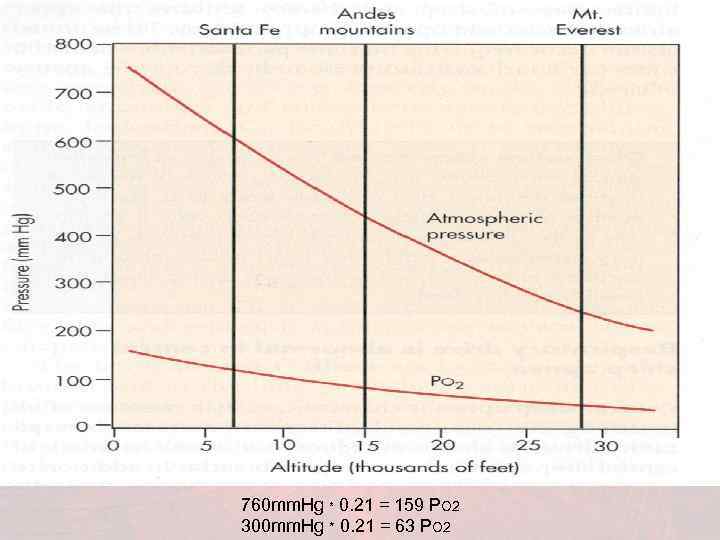 760 mm. Hg * 0. 21 = 159 PO 2 300 mm. Hg * 0. 21 = 63 PO 2
760 mm. Hg * 0. 21 = 159 PO 2 300 mm. Hg * 0. 21 = 63 PO 2
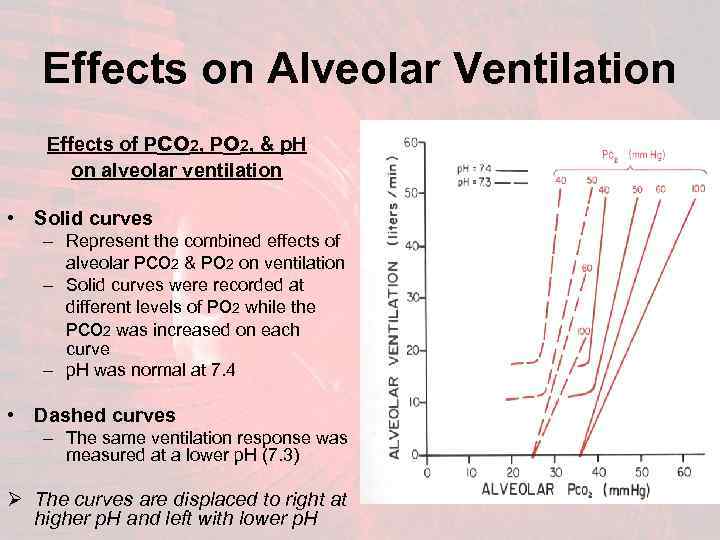 Effects on Alveolar Ventilation Effects of Pco 2, Po 2, & p. H on alveolar ventilation • Solid curves – Represent the combined effects of alveolar Pco 2 & Po 2 on ventilation – Solid curves were recorded at different levels of Po 2 while the Pco 2 was increased on each curve – p. H was normal at 7. 4 • Dashed curves – The same ventilation response was measured at a lower p. H (7. 3) Ø The curves are displaced to right at higher p. H and left with lower p. H
Effects on Alveolar Ventilation Effects of Pco 2, Po 2, & p. H on alveolar ventilation • Solid curves – Represent the combined effects of alveolar Pco 2 & Po 2 on ventilation – Solid curves were recorded at different levels of Po 2 while the Pco 2 was increased on each curve – p. H was normal at 7. 4 • Dashed curves – The same ventilation response was measured at a lower p. H (7. 3) Ø The curves are displaced to right at higher p. H and left with lower p. H
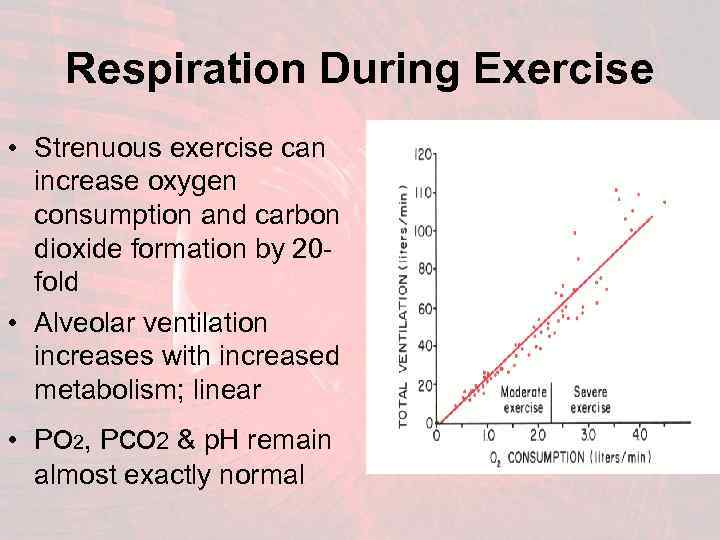 Respiration During Exercise • Strenuous exercise can increase oxygen consumption and carbon dioxide formation by 20 fold • Alveolar ventilation increases with increased metabolism; linear • Po 2, Pco 2 & p. H remain almost exactly normal
Respiration During Exercise • Strenuous exercise can increase oxygen consumption and carbon dioxide formation by 20 fold • Alveolar ventilation increases with increased metabolism; linear • Po 2, Pco 2 & p. H remain almost exactly normal
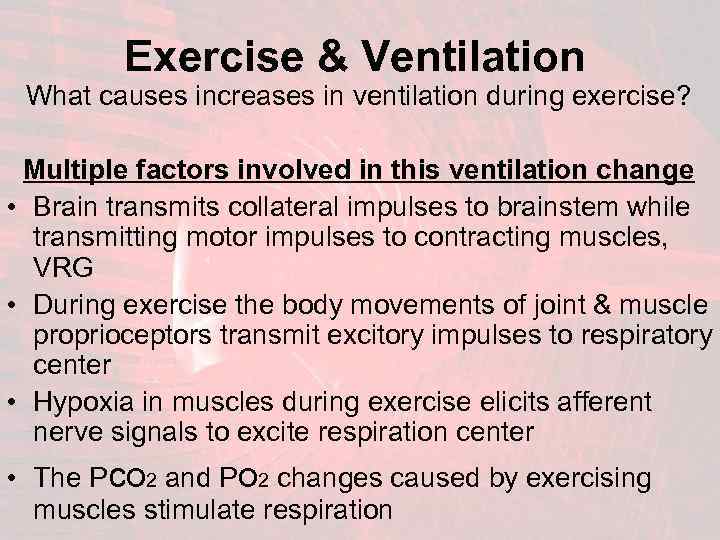 Exercise & Ventilation What causes increases in ventilation during exercise? Multiple factors involved in this ventilation change • Brain transmits collateral impulses to brainstem while transmitting motor impulses to contracting muscles, VRG • During exercise the body movements of joint & muscle proprioceptors transmit excitory impulses to respiratory center • Hypoxia in muscles during exercise elicits afferent nerve signals to excite respiration center • The Pco 2 and Po 2 changes caused by exercising muscles stimulate respiration
Exercise & Ventilation What causes increases in ventilation during exercise? Multiple factors involved in this ventilation change • Brain transmits collateral impulses to brainstem while transmitting motor impulses to contracting muscles, VRG • During exercise the body movements of joint & muscle proprioceptors transmit excitory impulses to respiratory center • Hypoxia in muscles during exercise elicits afferent nerve signals to excite respiration center • The Pco 2 and Po 2 changes caused by exercising muscles stimulate respiration
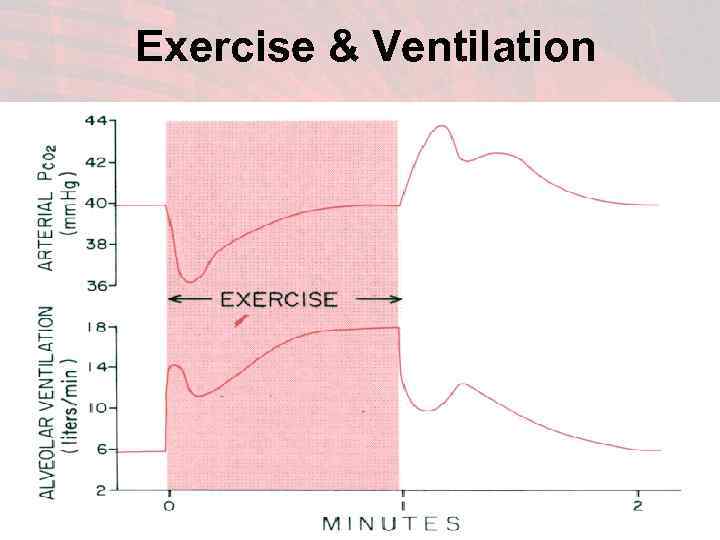 Exercise & Ventilation
Exercise & Ventilation
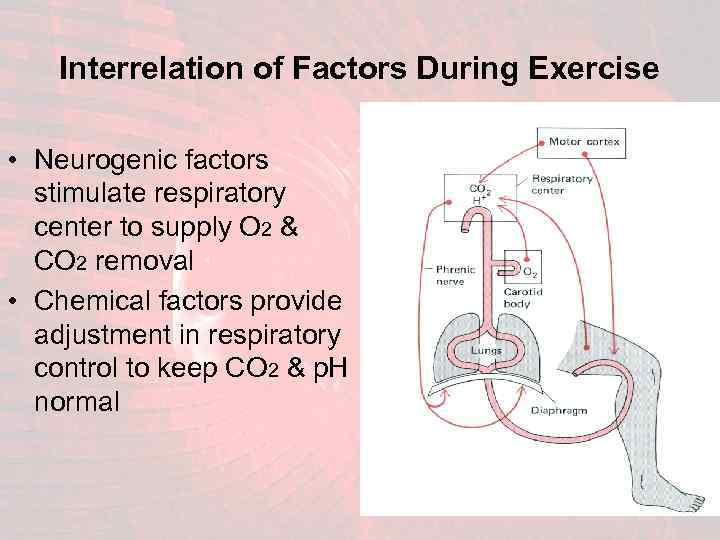 Interrelation of Factors During Exercise • Neurogenic factors stimulate respiratory center to supply O 2 & CO 2 removal • Chemical factors provide adjustment in respiratory control to keep CO 2 & p. H normal
Interrelation of Factors During Exercise • Neurogenic factors stimulate respiratory center to supply O 2 & CO 2 removal • Chemical factors provide adjustment in respiratory control to keep CO 2 & p. H normal
 Voluntary Control of Respiration • Respiration can controlled voluntarily • Hyper or hypoventilation to extent of serious derangement in Pco 2, p. H, Po 2 • Voluntary control is not mediated through respiratory center • Pathway for voluntary control from cortex & higher centers downward through cortispinal tract to spinal neurons that drive respiratory muscles
Voluntary Control of Respiration • Respiration can controlled voluntarily • Hyper or hypoventilation to extent of serious derangement in Pco 2, p. H, Po 2 • Voluntary control is not mediated through respiratory center • Pathway for voluntary control from cortex & higher centers downward through cortispinal tract to spinal neurons that drive respiratory muscles
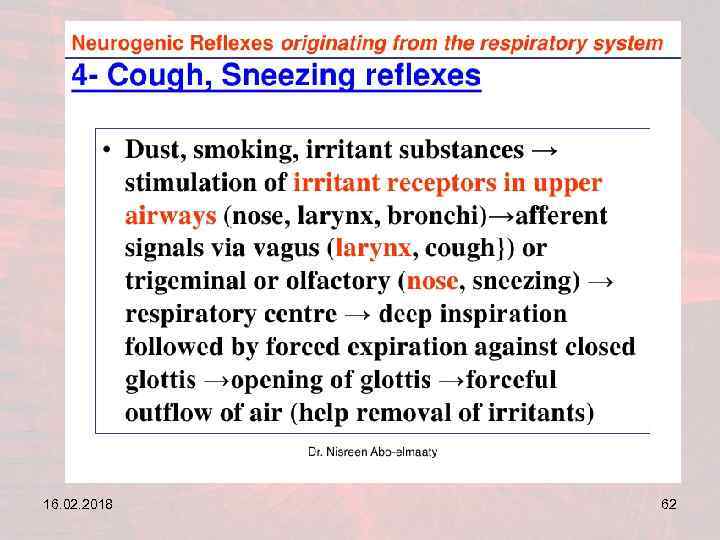
 Irritant Receptors In Airways • The epithelium of trachea, bronchi & bronchioles have sensitive nerve endings • Pulmonary irritant receptors are stimulated by different noxious environmental products • Coughing or sneezing results • These receptors may also cause bronchial constriction in diseases such as asthma & emphysema
Irritant Receptors In Airways • The epithelium of trachea, bronchi & bronchioles have sensitive nerve endings • Pulmonary irritant receptors are stimulated by different noxious environmental products • Coughing or sneezing results • These receptors may also cause bronchial constriction in diseases such as asthma & emphysema
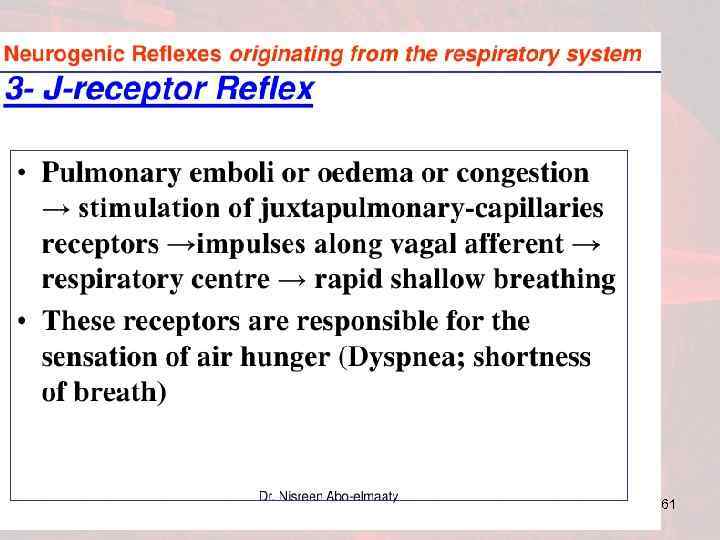
 Lung “J Receptors” • Sensory nerve endings in alveolar walls juxtapose the pulmonary capillaries • The ‘J receptors’ become stimulated when engorged by blood or when pulmonary edema occurs as in CHF • Functional role for ‘J receptors’ not well defined – their excitation may give the feeling of dyspnea
Lung “J Receptors” • Sensory nerve endings in alveolar walls juxtapose the pulmonary capillaries • The ‘J receptors’ become stimulated when engorged by blood or when pulmonary edema occurs as in CHF • Functional role for ‘J receptors’ not well defined – their excitation may give the feeling of dyspnea
 Brain Edema • Respiratory center activity depressed or inactivated by acute brain edema (ie: head trauma /concussion) • Blood flow reductions affects cellular metabolism & function • Treatment includes mechanical hyperventilation & hypertonic diuresis
Brain Edema • Respiratory center activity depressed or inactivated by acute brain edema (ie: head trauma /concussion) • Blood flow reductions affects cellular metabolism & function • Treatment includes mechanical hyperventilation & hypertonic diuresis
 • Types of Breathing 16. 02. 2018 80
• Types of Breathing 16. 02. 2018 80
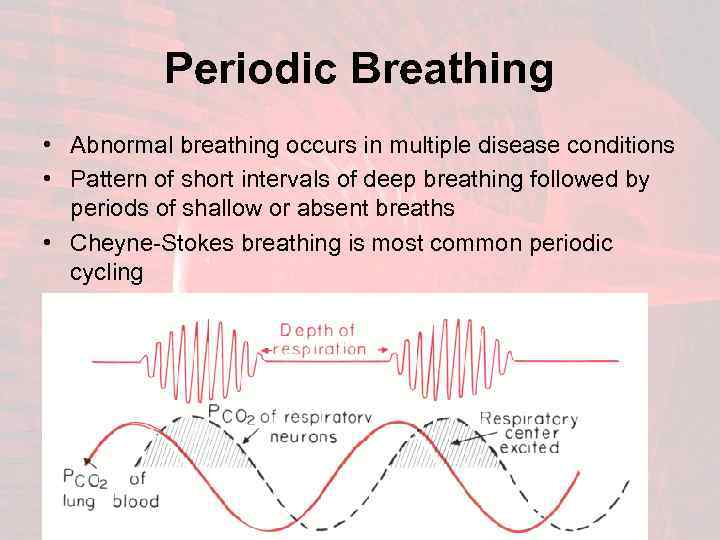 Periodic Breathing • Abnormal breathing occurs in multiple disease conditions • Pattern of short intervals of deep breathing followed by periods of shallow or absent breaths • Cheyne-Stokes breathing is most common periodic cycling
Periodic Breathing • Abnormal breathing occurs in multiple disease conditions • Pattern of short intervals of deep breathing followed by periods of shallow or absent breaths • Cheyne-Stokes breathing is most common periodic cycling
 Cheyne-Stokes Breathing • The basic cause of Cheyne-Stokes breathing: – Over-breathing causes a decrease of CO 2 & increases blood oxygen in pulmonay blood – The altered pulmonary blood is transported to brain to inhibits excess ventilation – The response is delayed in depressing respiratory center because of it takes a few seconds for brain to respond – After a pause in breathing, the cycle resumes with rapid deep breaths again
Cheyne-Stokes Breathing • The basic cause of Cheyne-Stokes breathing: – Over-breathing causes a decrease of CO 2 & increases blood oxygen in pulmonay blood – The altered pulmonary blood is transported to brain to inhibits excess ventilation – The response is delayed in depressing respiratory center because of it takes a few seconds for brain to respond – After a pause in breathing, the cycle resumes with rapid deep breaths again
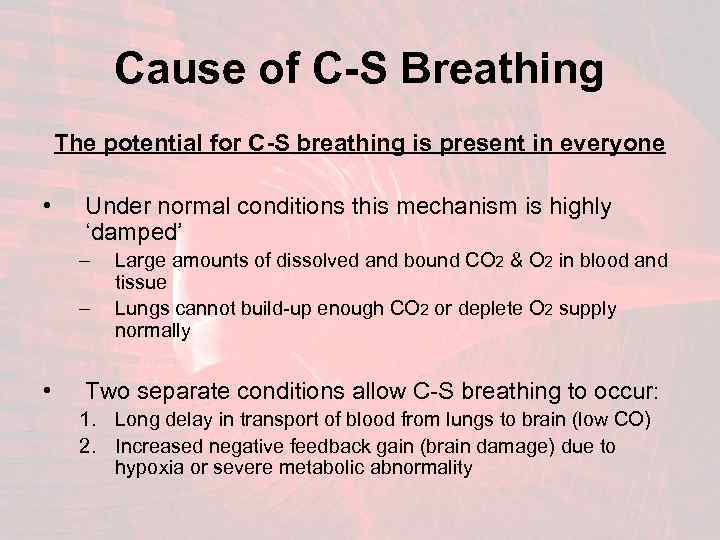 Cause of C-S Breathing The potential for C-S breathing is present in everyone • Under normal conditions this mechanism is highly ‘damped’ – – • Large amounts of dissolved and bound CO 2 & O 2 in blood and tissue Lungs cannot build-up enough CO 2 or deplete O 2 supply normally Two separate conditions allow C-S breathing to occur: 1. Long delay in transport of blood from lungs to brain (low CO) 2. Increased negative feedback gain (brain damage) due to hypoxia or severe metabolic abnormality
Cause of C-S Breathing The potential for C-S breathing is present in everyone • Under normal conditions this mechanism is highly ‘damped’ – – • Large amounts of dissolved and bound CO 2 & O 2 in blood and tissue Lungs cannot build-up enough CO 2 or deplete O 2 supply normally Two separate conditions allow C-S breathing to occur: 1. Long delay in transport of blood from lungs to brain (low CO) 2. Increased negative feedback gain (brain damage) due to hypoxia or severe metabolic abnormality
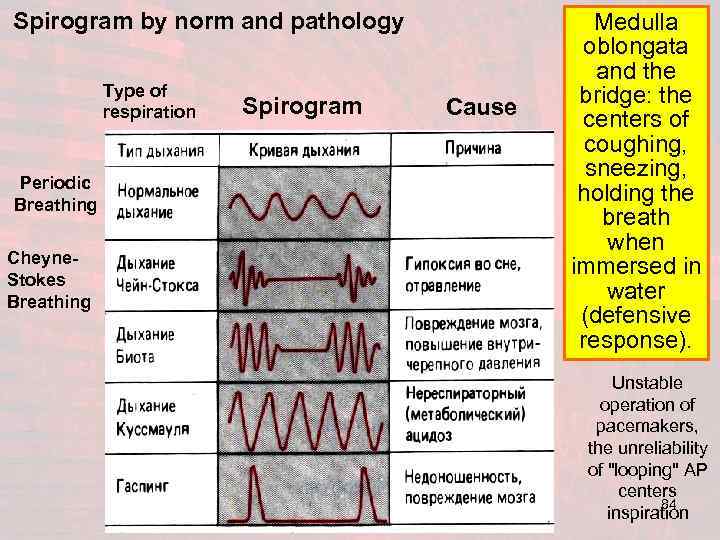 Spirogram by norm and pathology Type of respiration Periodic Breathing Cheyne. Stokes Breathing Spirogram Cause Medulla oblongata and the bridge: the centers of coughing, sneezing, holding the breath when immersed in water (defensive response). Unstable operation of pacemakers, the unreliability of "looping" AP centers 84 inspiration
Spirogram by norm and pathology Type of respiration Periodic Breathing Cheyne. Stokes Breathing Spirogram Cause Medulla oblongata and the bridge: the centers of coughing, sneezing, holding the breath when immersed in water (defensive response). Unstable operation of pacemakers, the unreliability of "looping" AP centers 84 inspiration
 Features of breath in children 16. 02. 2018 85
Features of breath in children 16. 02. 2018 85
 What is the Normal Breathing Rate of Children? • Children breathe faster than adults. • Body size, weight and activity level influence normal breathing rates. But age is the factor most commonly used to determine normal values. • Normal breathing rate ranges from as high as 30 to 60 breaths per minute at birth to as low as 12 to 16 breaths per minute at age 18. • Breathing maintains the child's critical balance of oxygen and carbon dioxide. 16. 02. 2018 86
What is the Normal Breathing Rate of Children? • Children breathe faster than adults. • Body size, weight and activity level influence normal breathing rates. But age is the factor most commonly used to determine normal values. • Normal breathing rate ranges from as high as 30 to 60 breaths per minute at birth to as low as 12 to 16 breaths per minute at age 18. • Breathing maintains the child's critical balance of oxygen and carbon dioxide. 16. 02. 2018 86
 Breaths by Age • According to the New York State Department of Health, infants, from birth to 1 year, should have 30 to 60 breaths per minute. • Toddlers, ages 1 to 3, breathe 24 to 40 times per minute. • Pre-schoolers, ages 3 to 6 years, average 22 to 34 breaths per minute. • Six- to 12 -year-olds have 18 to 30 breaths per minute. • Adolescents, ages 12 to 18, have 12 to 16 breaths per minute. • Summary • In a normal breath for a minute the baby should be as follows: 50 breaths - in neonates; 25 breaths - the child up to a year; 27 -30 breaths - a child of up to 3 years; 25 breaths - in children from 4 to 6 years.
Breaths by Age • According to the New York State Department of Health, infants, from birth to 1 year, should have 30 to 60 breaths per minute. • Toddlers, ages 1 to 3, breathe 24 to 40 times per minute. • Pre-schoolers, ages 3 to 6 years, average 22 to 34 breaths per minute. • Six- to 12 -year-olds have 18 to 30 breaths per minute. • Adolescents, ages 12 to 18, have 12 to 16 breaths per minute. • Summary • In a normal breath for a minute the baby should be as follows: 50 breaths - in neonates; 25 breaths - the child up to a year; 27 -30 breaths - a child of up to 3 years; 25 breaths - in children from 4 to 6 years.
 Things to Consider • Children are not all alike, and various authorities report slightly different normal breathing ranges, though most vary by only a few percent. • But the trend of decreasing normal rate with increasing age remains unchanged in all cases. • Normal rates vary according to weight, activity levels and growth-related 16. 02. 2018 88 developmental milestones.
Things to Consider • Children are not all alike, and various authorities report slightly different normal breathing ranges, though most vary by only a few percent. • But the trend of decreasing normal rate with increasing age remains unchanged in all cases. • Normal rates vary according to weight, activity levels and growth-related 16. 02. 2018 88 developmental milestones.
 Breathing for Equilibrium • Normal breathing rate is important because breathing delivers oxygen to a developing child's heart, brain, liver and all the other organ systems. • A child not only needs oxygen for ongoing metabolism, like an adult, but for creation of new and growing tissues, bones and nerves. • Breathing also eliminates carbon dioxide, the normal waste product of metabolism and growth. • A child's biochemistry is carefully balanced between too much and too little carbon dioxide. • A normal breathing rate is one of the most important regulators of that balance 16. 02. 2018 89
Breathing for Equilibrium • Normal breathing rate is important because breathing delivers oxygen to a developing child's heart, brain, liver and all the other organ systems. • A child not only needs oxygen for ongoing metabolism, like an adult, but for creation of new and growing tissues, bones and nerves. • Breathing also eliminates carbon dioxide, the normal waste product of metabolism and growth. • A child's biochemistry is carefully balanced between too much and too little carbon dioxide. • A normal breathing rate is one of the most important regulators of that balance 16. 02. 2018 89
 Dangers • According to Dr. A. T. Rotta, in the March 2003 issue of "Respiratory Care, " many of the most important childhood respiratory emergencies are related to breathing rates. • Slow breathing causes oxygen starvation and damage to the most active, growing systems. A buildup of too much carbon dioxide can cause unconsciousness, seizures and coma. This can be caused by an airway obstruction, inflammation, or accidental ingestion of depressant medications like pain killers, tranquilizers and intoxicants. • Breathing too fast will cause the elimination of too much carbon dioxide. This causes irregular heart beats, changes in blood flow to vital organs and neurological changes. High fever and accidental ingestion of stimulants can cause this imbalance 16. 02. 2018 90
Dangers • According to Dr. A. T. Rotta, in the March 2003 issue of "Respiratory Care, " many of the most important childhood respiratory emergencies are related to breathing rates. • Slow breathing causes oxygen starvation and damage to the most active, growing systems. A buildup of too much carbon dioxide can cause unconsciousness, seizures and coma. This can be caused by an airway obstruction, inflammation, or accidental ingestion of depressant medications like pain killers, tranquilizers and intoxicants. • Breathing too fast will cause the elimination of too much carbon dioxide. This causes irregular heart beats, changes in blood flow to vital organs and neurological changes. High fever and accidental ingestion of stimulants can cause this imbalance 16. 02. 2018 90
 Counting Breaths • Normal breathing rate in children is easy to measure. Simply count the breathing cycles -- an inhalation and an exhalation is one breath -- in a complete minute. • Do not count part of a minute and multiply. • A child's breathing rate can be irregular due to pain, crying or restlessness. • Also check the depth of each breath. If breathing is unusually shallow or deep, oxygen and carbon dioxide disturbances can also result. • All abnormal signs and symptoms accompanying an abnormal breathing rate should receive immediate medical attention. 16. 02. 2018 91
Counting Breaths • Normal breathing rate in children is easy to measure. Simply count the breathing cycles -- an inhalation and an exhalation is one breath -- in a complete minute. • Do not count part of a minute and multiply. • A child's breathing rate can be irregular due to pain, crying or restlessness. • Also check the depth of each breath. If breathing is unusually shallow or deep, oxygen and carbon dioxide disturbances can also result. • All abnormal signs and symptoms accompanying an abnormal breathing rate should receive immediate medical attention. 16. 02. 2018 91
 That’s All For Today
That’s All For Today
 16. 02. 2018 93
16. 02. 2018 93
 16. 02. 2018 94
16. 02. 2018 94
 16. 02. 2018 95
16. 02. 2018 95
 16. 02. 2018 96
16. 02. 2018 96
 16. 02. 2018 97
16. 02. 2018 97
 16. 02. 2018 98
16. 02. 2018 98
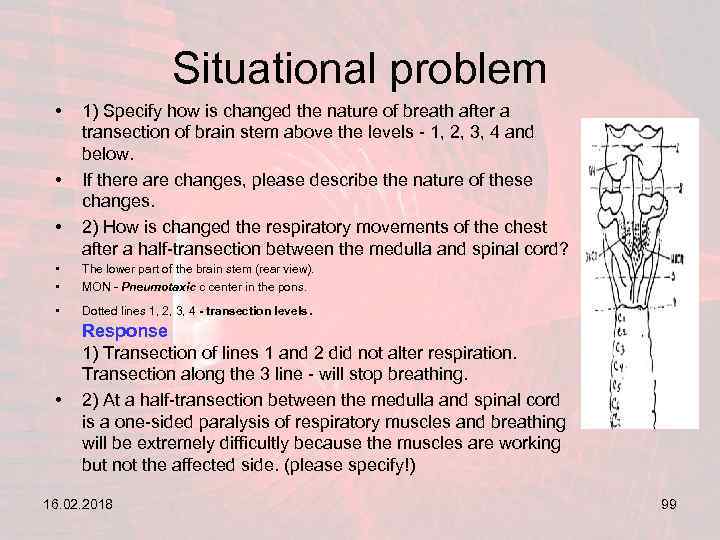 Situational problem • • • 1) Specify how is changed the nature of breath after a transection of brain stem above the levels - 1, 2, 3, 4 and below. If there are changes, please describe the nature of these changes. 2) How is changed the respiratory movements of the chest after a half-transection between the medulla and spinal cord? • • The lower part of the brain stem (rear view). MON - Pneumotaxic c center in the pons. • Dotted lines 1, 2, 3, 4 - transection levels. • Response 1) Transection of lines 1 and 2 did not alter respiration. Transection along the 3 line - will stop breathing. 2) At a half-transection between the medulla and spinal cord is a one-sided paralysis of respiratory muscles and breathing will be extremely difficultly because the muscles are working but not the affected side. (please specify!) 16. 02. 2018 99
Situational problem • • • 1) Specify how is changed the nature of breath after a transection of brain stem above the levels - 1, 2, 3, 4 and below. If there are changes, please describe the nature of these changes. 2) How is changed the respiratory movements of the chest after a half-transection between the medulla and spinal cord? • • The lower part of the brain stem (rear view). MON - Pneumotaxic c center in the pons. • Dotted lines 1, 2, 3, 4 - transection levels. • Response 1) Transection of lines 1 and 2 did not alter respiration. Transection along the 3 line - will stop breathing. 2) At a half-transection between the medulla and spinal cord is a one-sided paralysis of respiratory muscles and breathing will be extremely difficultly because the muscles are working but not the affected side. (please specify!) 16. 02. 2018 99
 Control questions (feedback) • 1. The mechanism of the first breath of the child. • 2. With what it is connected low size elastic draughts of lungs at an exhalation at the newborn? • 3. Value of reflexes of Goering and Brayer at newborns. • 4. As frequency of breath of the child changes at sucking movements. • 5. What is irritant receptors and their value in the breath mechanism? 16. 02. 2018 100
Control questions (feedback) • 1. The mechanism of the first breath of the child. • 2. With what it is connected low size elastic draughts of lungs at an exhalation at the newborn? • 3. Value of reflexes of Goering and Brayer at newborns. • 4. As frequency of breath of the child changes at sucking movements. • 5. What is irritant receptors and their value in the breath mechanism? 16. 02. 2018 100
 16. 02. 2018 101
16. 02. 2018 101
 16. 02. 2018 102
16. 02. 2018 102
 16. 02. 2018 103
16. 02. 2018 103
 16. 02. 2018 104
16. 02. 2018 104
 16. 02. 2018 105
16. 02. 2018 105
 Experience Frederick.
Experience Frederick.
 16. 02. 2018 110
16. 02. 2018 110


