8f6a0e717d805befb0be683f5c107060.ppt
- Количество слайдов: 31
 Tissue Fluorescence Spectroscopy Lecture 16
Tissue Fluorescence Spectroscopy Lecture 16
 Outline • Steady-state fluorescence – Instrumentation and Data Analysis Methods • Statistical methods: Principal components analysis • Empirical methods: Ratio imaging • Modeling: Quantitative extraction of biochemical info – Fluorescence in disease diagnostics – Fluorescence in disease therapeutics
Outline • Steady-state fluorescence – Instrumentation and Data Analysis Methods • Statistical methods: Principal components analysis • Empirical methods: Ratio imaging • Modeling: Quantitative extraction of biochemical info – Fluorescence in disease diagnostics – Fluorescence in disease therapeutics

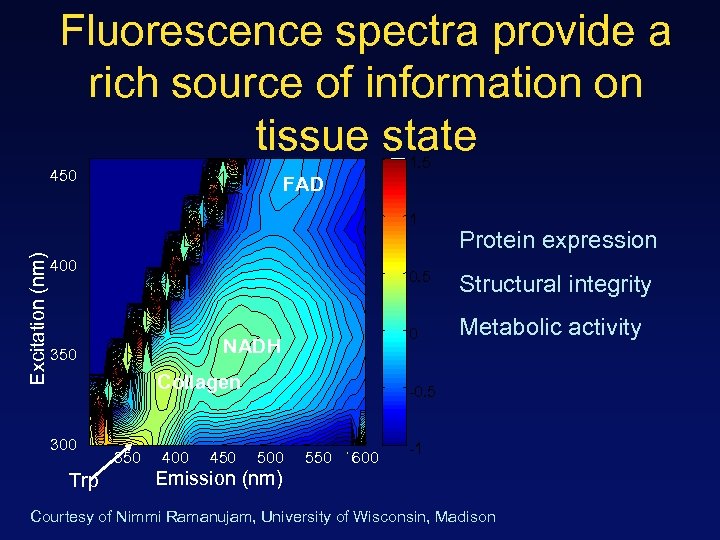 Fluorescence spectra provide a rich source of information on tissue state 1. 5 450 FAD Excitation (nm) 1 400 0. 5 Collagen Trp 350 400 450 Structural integrity 0 NADH 350 300 Protein expression Metabolic activity -0. 5 500 550 600 -1 Emission (nm) Courtesy of Nimmi Ramanujam, University of Wisconsin, Madison
Fluorescence spectra provide a rich source of information on tissue state 1. 5 450 FAD Excitation (nm) 1 400 0. 5 Collagen Trp 350 400 450 Structural integrity 0 NADH 350 300 Protein expression Metabolic activity -0. 5 500 550 600 -1 Emission (nm) Courtesy of Nimmi Ramanujam, University of Wisconsin, Madison
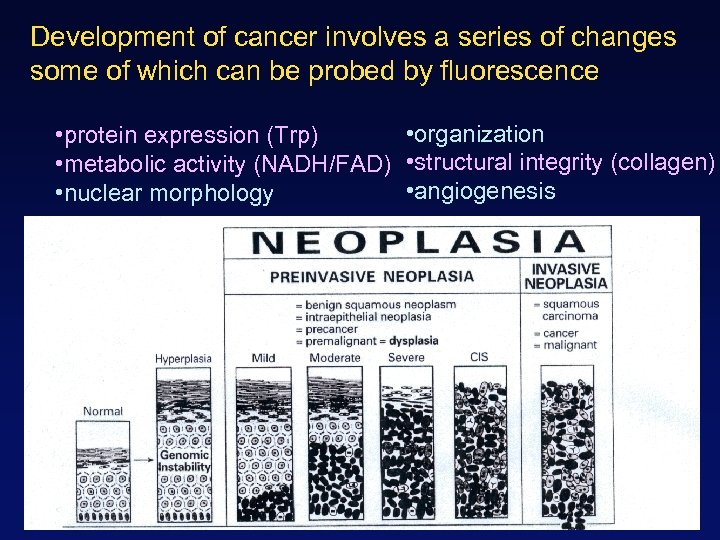 Development of cancer involves a series of changes some of which can be probed by fluorescence • organization • protein expression (Trp) • metabolic activity (NADH/FAD) • structural integrity (collagen) • angiogenesis • nuclear morphology
Development of cancer involves a series of changes some of which can be probed by fluorescence • organization • protein expression (Trp) • metabolic activity (NADH/FAD) • structural integrity (collagen) • angiogenesis • nuclear morphology
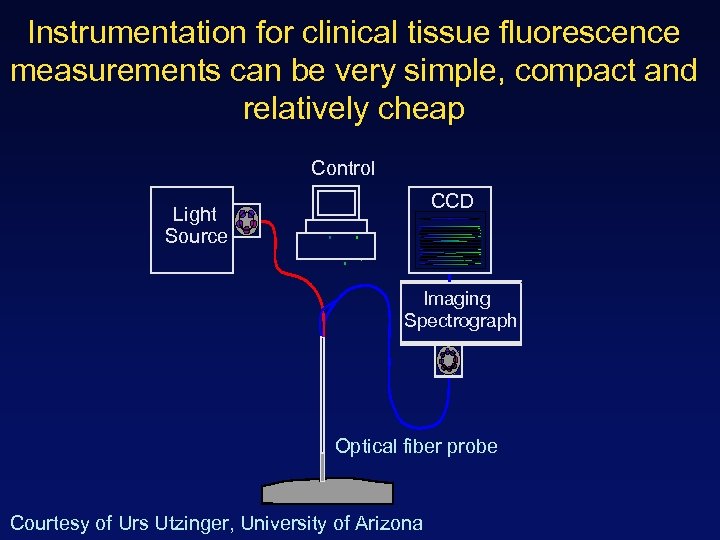 Instrumentation for clinical tissue fluorescence measurements can be very simple, compact and relatively cheap Control CCD Light Source Imaging Spectrograph Optical fiber probe Courtesy of Urs Utzinger, University of Arizona
Instrumentation for clinical tissue fluorescence measurements can be very simple, compact and relatively cheap Control CCD Light Source Imaging Spectrograph Optical fiber probe Courtesy of Urs Utzinger, University of Arizona
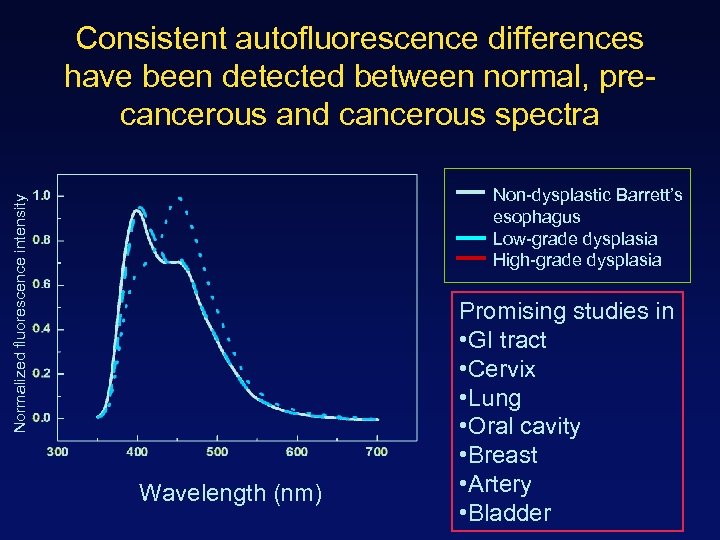 Consistent autofluorescence differences have been detected between normal, precancerous and cancerous spectra Normalized fluorescence intensity Non-dysplastic Barrett’s esophagus Low-grade dysplasia High-grade dysplasia Wavelength (nm) Promising studies in • GI tract • Cervix • Lung • Oral cavity • Breast • Artery • Bladder
Consistent autofluorescence differences have been detected between normal, precancerous and cancerous spectra Normalized fluorescence intensity Non-dysplastic Barrett’s esophagus Low-grade dysplasia High-grade dysplasia Wavelength (nm) Promising studies in • GI tract • Cervix • Lung • Oral cavity • Breast • Artery • Bladder
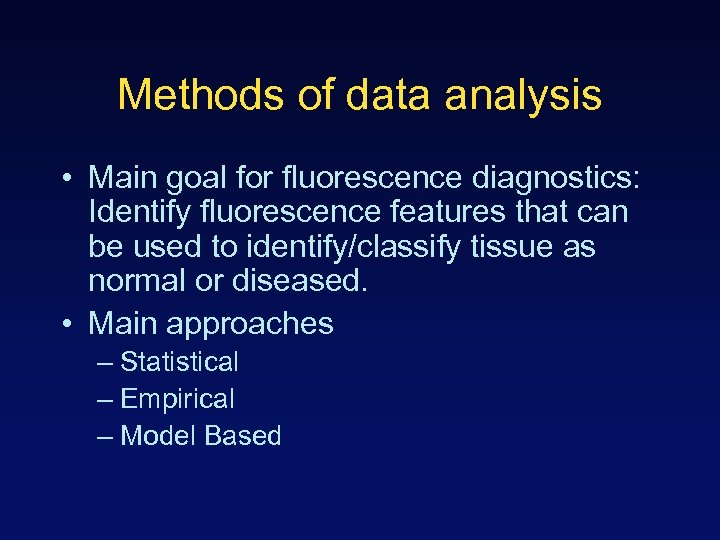 Methods of data analysis • Main goal for fluorescence diagnostics: Identify fluorescence features that can be used to identify/classify tissue as normal or diseased. • Main approaches – Statistical – Empirical – Model Based
Methods of data analysis • Main goal for fluorescence diagnostics: Identify fluorescence features that can be used to identify/classify tissue as normal or diseased. • Main approaches – Statistical – Empirical – Model Based
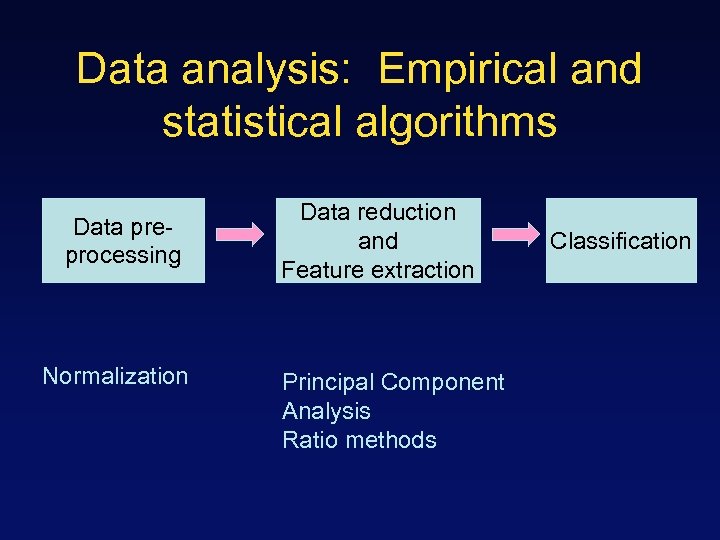 Data analysis: Empirical and statistical algorithms Data preprocessing Normalization Data reduction and Feature extraction Principal Component Analysis Ratio methods Classification
Data analysis: Empirical and statistical algorithms Data preprocessing Normalization Data reduction and Feature extraction Principal Component Analysis Ratio methods Classification
 Detection of cervical precancerous lesions using fluorescence spectroscopy: Principal components analysis Rebecca Richards Kortum group UT Austin
Detection of cervical precancerous lesions using fluorescence spectroscopy: Principal components analysis Rebecca Richards Kortum group UT Austin
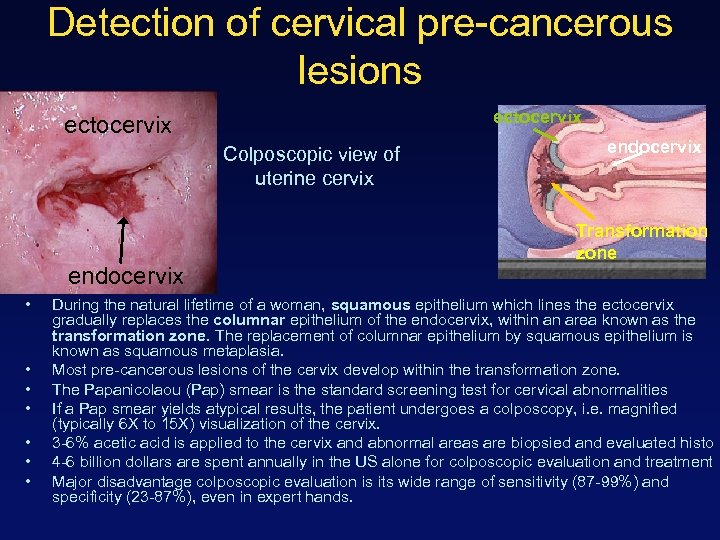 Detection of cervical pre-cancerous lesions ectocervix Colposcopic view of uterine cervix endocervix • • endocervix Transformation zone During the natural lifetime of a woman, squamous epithelium which lines the ectocervix gradually replaces the columnar epithelium of the endocervix, within an area known as the transformation zone. The replacement of columnar epithelium by squamous epithelium is known as squamous metaplasia. Most pre-cancerous lesions of the cervix develop within the transformation zone. The Papanicolaou (Pap) smear is the standard screening test for cervical abnormalities If a Pap smear yields atypical results, the patient undergoes a colposcopy, i. e. magnified (typically 6 X to 15 X) visualization of the cervix. 3 -6% acetic acid is applied to the cervix and abnormal areas are biopsied and evaluated histo 4 -6 billion dollars are spent annually in the US alone for colposcopic evaluation and treatment Major disadvantage colposcopic evaluation is its wide range of sensitivity (87 -99%) and specificity (23 -87%), even in expert hands.
Detection of cervical pre-cancerous lesions ectocervix Colposcopic view of uterine cervix endocervix • • endocervix Transformation zone During the natural lifetime of a woman, squamous epithelium which lines the ectocervix gradually replaces the columnar epithelium of the endocervix, within an area known as the transformation zone. The replacement of columnar epithelium by squamous epithelium is known as squamous metaplasia. Most pre-cancerous lesions of the cervix develop within the transformation zone. The Papanicolaou (Pap) smear is the standard screening test for cervical abnormalities If a Pap smear yields atypical results, the patient undergoes a colposcopy, i. e. magnified (typically 6 X to 15 X) visualization of the cervix. 3 -6% acetic acid is applied to the cervix and abnormal areas are biopsied and evaluated histo 4 -6 billion dollars are spent annually in the US alone for colposcopic evaluation and treatment Major disadvantage colposcopic evaluation is its wide range of sensitivity (87 -99%) and specificity (23 -87%), even in expert hands.
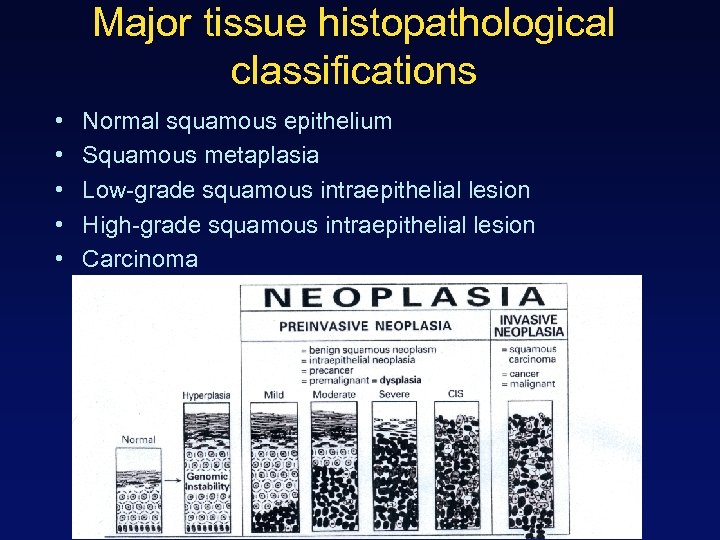 Major tissue histopathological classifications • • • Normal squamous epithelium Squamous metaplasia Low-grade squamous intraepithelial lesion High-grade squamous intraepithelial lesion Carcinoma
Major tissue histopathological classifications • • • Normal squamous epithelium Squamous metaplasia Low-grade squamous intraepithelial lesion High-grade squamous intraepithelial lesion Carcinoma
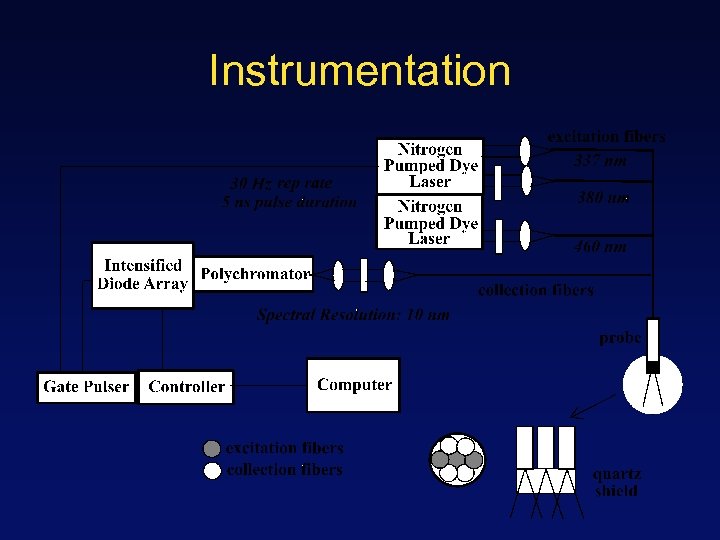 Instrumentation
Instrumentation
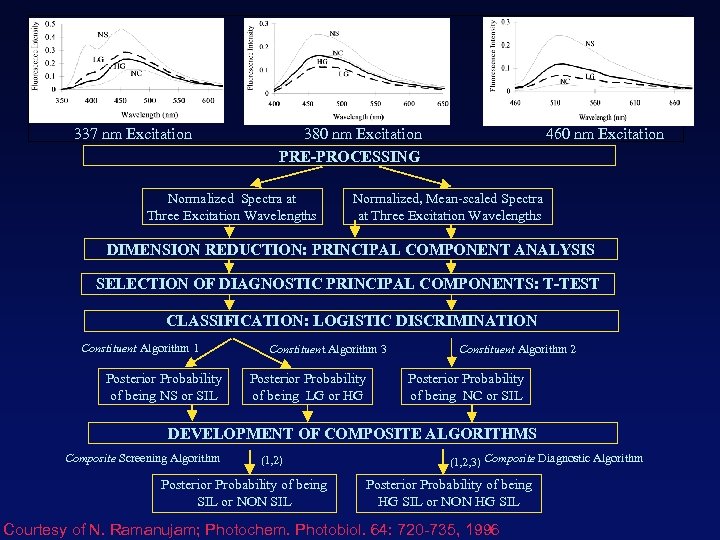 337 nm Excitation 380 nm Excitation 460 nm Excitation PRE-PROCESSING Normalized Spectra at Three Excitation Wavelengths Normalized, Mean-scaled Spectra at Three Excitation Wavelengths DIMENSION REDUCTION: PRINCIPAL COMPONENT ANALYSIS SELECTION OF DIAGNOSTIC PRINCIPAL COMPONENTS: T-TEST CLASSIFICATION: LOGISTIC DISCRIMINATION Constituent Algorithm 1 Posterior Probability of being NS or SIL Constituent Algorithm 3 Posterior Probability of being LG or HG Constituent Algorithm 2 Posterior Probability of being NC or SIL DEVELOPMENT OF COMPOSITE ALGORITHMS Composite Screening Algorithm (1, 2) Posterior Probability of being SIL or NON SIL (1, 2, 3) Composite Diagnostic Algorithm Posterior Probability of being HG SIL or NON HG SIL Courtesy of N. Ramanujam; Photochem. Photobiol. 64: 720 -735, 1996
337 nm Excitation 380 nm Excitation 460 nm Excitation PRE-PROCESSING Normalized Spectra at Three Excitation Wavelengths Normalized, Mean-scaled Spectra at Three Excitation Wavelengths DIMENSION REDUCTION: PRINCIPAL COMPONENT ANALYSIS SELECTION OF DIAGNOSTIC PRINCIPAL COMPONENTS: T-TEST CLASSIFICATION: LOGISTIC DISCRIMINATION Constituent Algorithm 1 Posterior Probability of being NS or SIL Constituent Algorithm 3 Posterior Probability of being LG or HG Constituent Algorithm 2 Posterior Probability of being NC or SIL DEVELOPMENT OF COMPOSITE ALGORITHMS Composite Screening Algorithm (1, 2) Posterior Probability of being SIL or NON SIL (1, 2, 3) Composite Diagnostic Algorithm Posterior Probability of being HG SIL or NON HG SIL Courtesy of N. Ramanujam; Photochem. Photobiol. 64: 720 -735, 1996
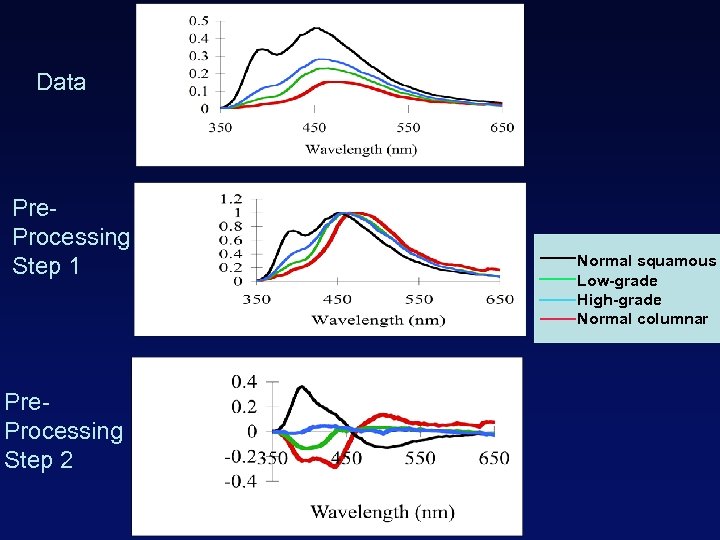 Data Pre. Processing Step 1 Pre. Processing Step 2 Normal squamous Low-grade High-grade Normal columnar
Data Pre. Processing Step 1 Pre. Processing Step 2 Normal squamous Low-grade High-grade Normal columnar
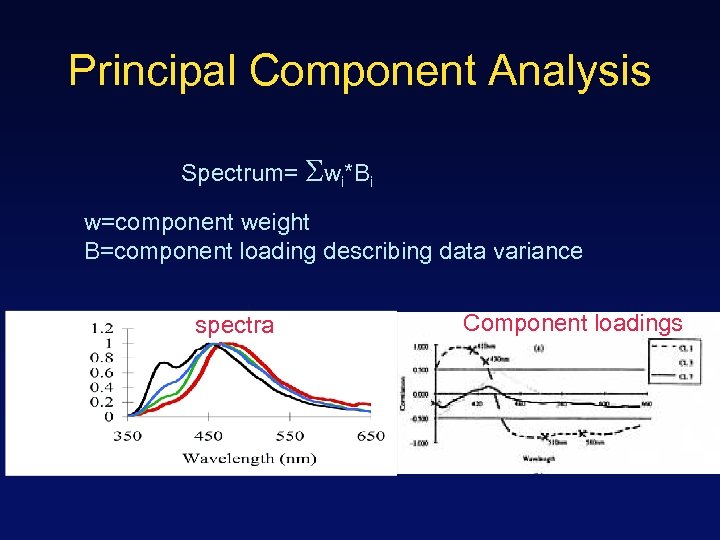 Principal Component Analysis Spectrum= wi*Bi w=component weight B=component loading describing data variance spectra Component loadings
Principal Component Analysis Spectrum= wi*Bi w=component weight B=component loading describing data variance spectra Component loadings
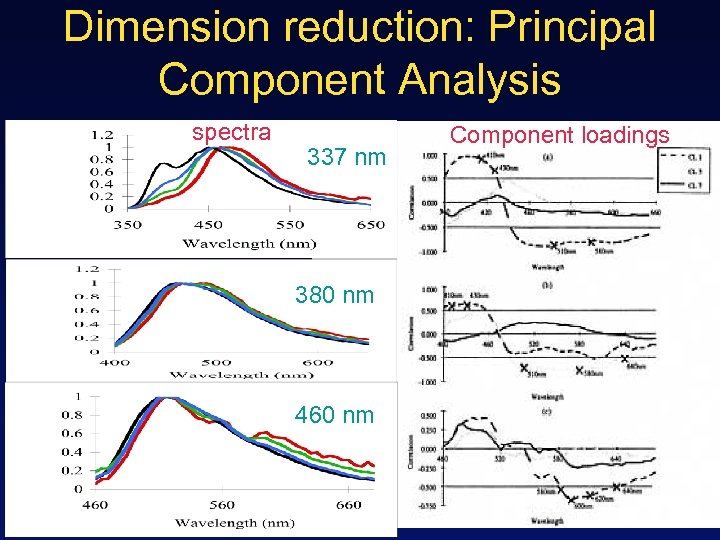 Dimension reduction: Principal Component Analysis spectra 337 nm 380 nm 460 nm Component loadings
Dimension reduction: Principal Component Analysis spectra 337 nm 380 nm 460 nm Component loadings
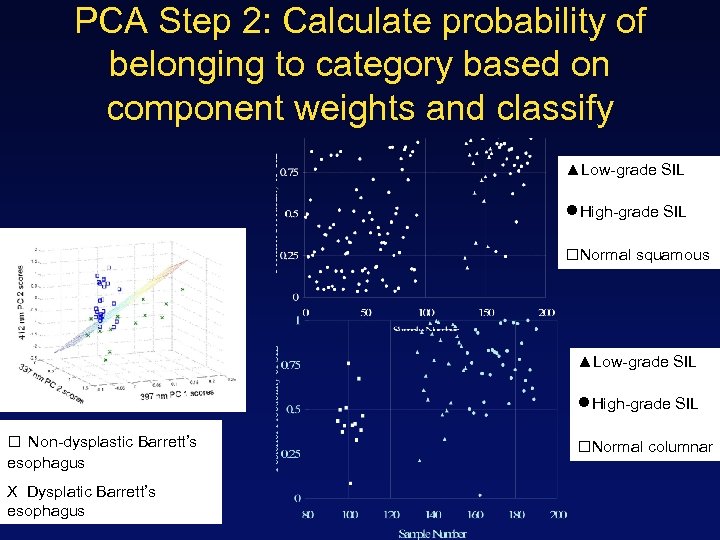 PCA Step 2: Calculate probability of belonging to category based on component weights and classify ▲Low-grade SIL ●High-grade SIL □Normal squamous ▲Low-grade SIL ●High-grade SIL □ Non-dysplastic Barrett’s esophagus X Dysplatic Barrett’s esophagus □Normal columnar
PCA Step 2: Calculate probability of belonging to category based on component weights and classify ▲Low-grade SIL ●High-grade SIL □Normal squamous ▲Low-grade SIL ●High-grade SIL □ Non-dysplastic Barrett’s esophagus X Dysplatic Barrett’s esophagus □Normal columnar
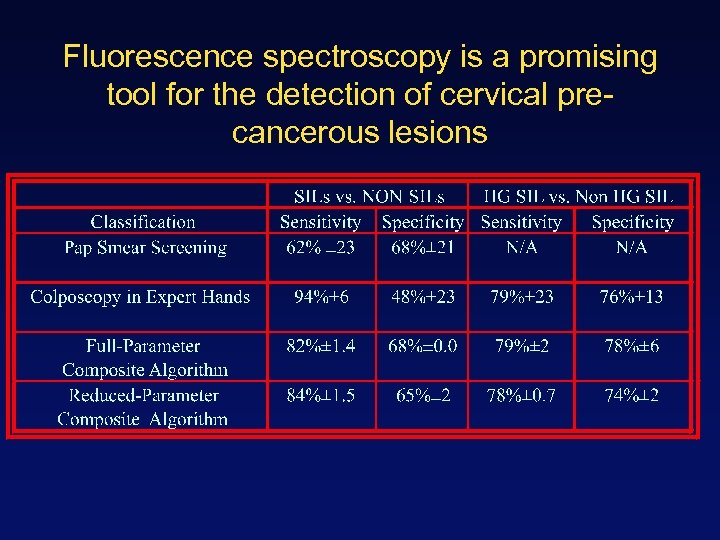 Fluorescence spectroscopy is a promising tool for the detection of cervical precancerous lesions
Fluorescence spectroscopy is a promising tool for the detection of cervical precancerous lesions
 Spectroscopic analysis using PCA • Uses full spectrum information to optimize sensitivity and specificity • Relatively easy to implement (automated software) • Provides no intuition with regards to the origin of spectral differences
Spectroscopic analysis using PCA • Uses full spectrum information to optimize sensitivity and specificity • Relatively easy to implement (automated software) • Provides no intuition with regards to the origin of spectral differences
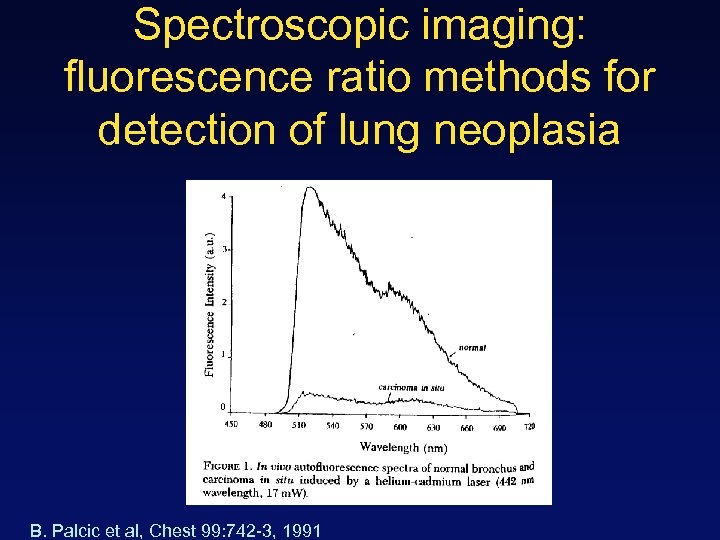 Spectroscopic imaging: fluorescence ratio methods for detection of lung neoplasia B. Palcic et al, Chest 99: 742 -3, 1991
Spectroscopic imaging: fluorescence ratio methods for detection of lung neoplasia B. Palcic et al, Chest 99: 742 -3, 1991
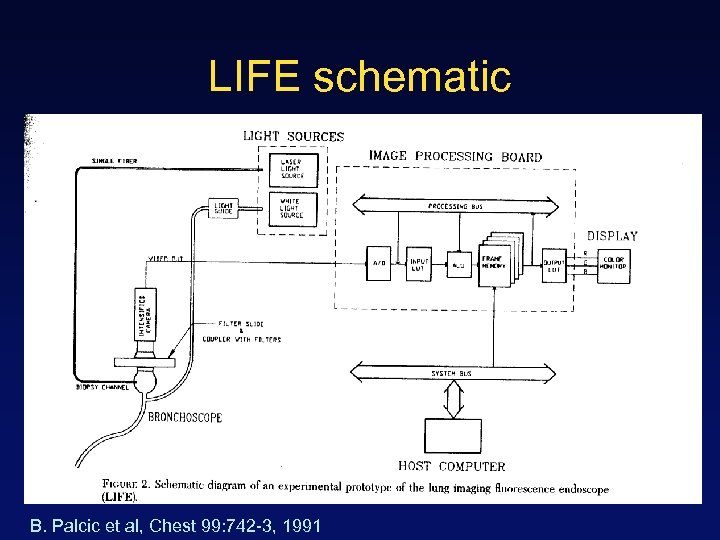 LIFE schematic B. Palcic et al, Chest 99: 742 -3, 1991
LIFE schematic B. Palcic et al, Chest 99: 742 -3, 1991
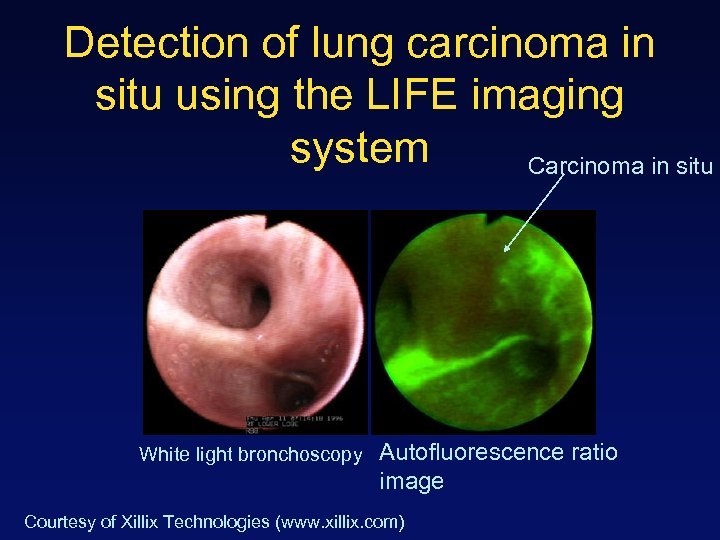 Detection of lung carcinoma in situ using the LIFE imaging system Carcinoma in situ White light bronchoscopy Autofluorescence ratio image Courtesy of Xillix Technologies (www. xillix. com)
Detection of lung carcinoma in situ using the LIFE imaging system Carcinoma in situ White light bronchoscopy Autofluorescence ratio image Courtesy of Xillix Technologies (www. xillix. com)
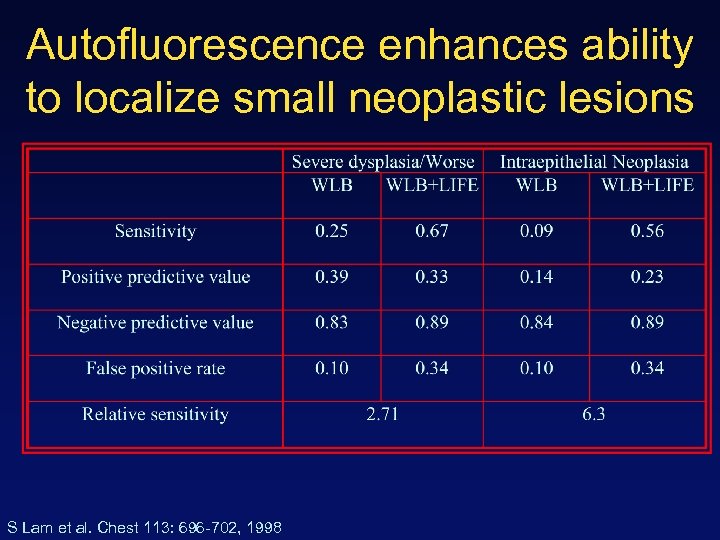 Autofluorescence enhances ability to localize small neoplastic lesions S Lam et al. Chest 113: 696 -702, 1998
Autofluorescence enhances ability to localize small neoplastic lesions S Lam et al. Chest 113: 696 -702, 1998
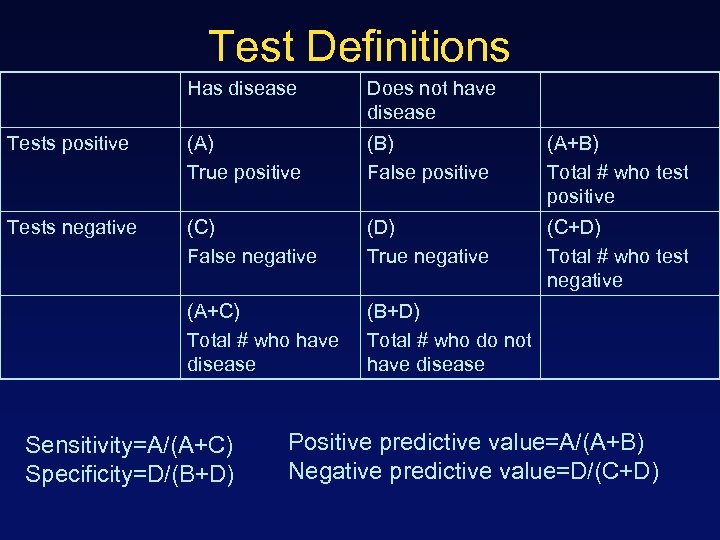 Test Definitions Has disease Does not have disease Tests positive (A) True positive (B) False positive (A+B) Total # who test positive Tests negative (C) False negative (D) True negative (C+D) Total # who test negative (A+C) Total # who have disease (B+D) Total # who do not have disease Sensitivity=A/(A+C) Specificity=D/(B+D) Positive predictive value=A/(A+B) Negative predictive value=D/(C+D)
Test Definitions Has disease Does not have disease Tests positive (A) True positive (B) False positive (A+B) Total # who test positive Tests negative (C) False negative (D) True negative (C+D) Total # who test negative (A+C) Total # who have disease (B+D) Total # who do not have disease Sensitivity=A/(A+C) Specificity=D/(B+D) Positive predictive value=A/(A+B) Negative predictive value=D/(C+D)
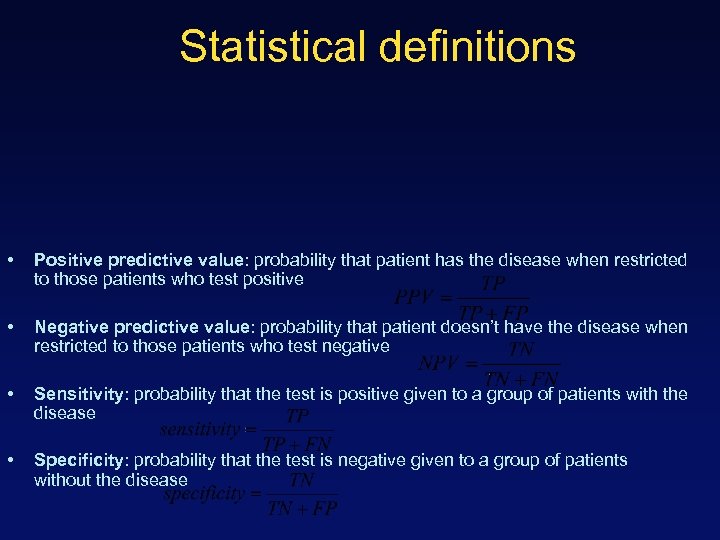 Statistical definitions • Positive predictive value: probability that patient has the disease when restricted to those patients who test positive • Negative predictive value: probability that patient doesn’t have the disease when restricted to those patients who test negative • Sensitivity: probability that the test is positive given to a group of patients with the disease • Specificity: probability that the test is negative given to a group of patients without the disease
Statistical definitions • Positive predictive value: probability that patient has the disease when restricted to those patients who test positive • Negative predictive value: probability that patient doesn’t have the disease when restricted to those patients who test negative • Sensitivity: probability that the test is positive given to a group of patients with the disease • Specificity: probability that the test is negative given to a group of patients without the disease
 Fluorescence imaging based on ratio methods • Wide field of view (probably a huge advantage for most clinical settings) • Eliminates effects of distance and angle of illumination • Easy to implement • Provides no intuition with regards to origins of spectral differences
Fluorescence imaging based on ratio methods • Wide field of view (probably a huge advantage for most clinical settings) • Eliminates effects of distance and angle of illumination • Easy to implement • Provides no intuition with regards to origins of spectral differences
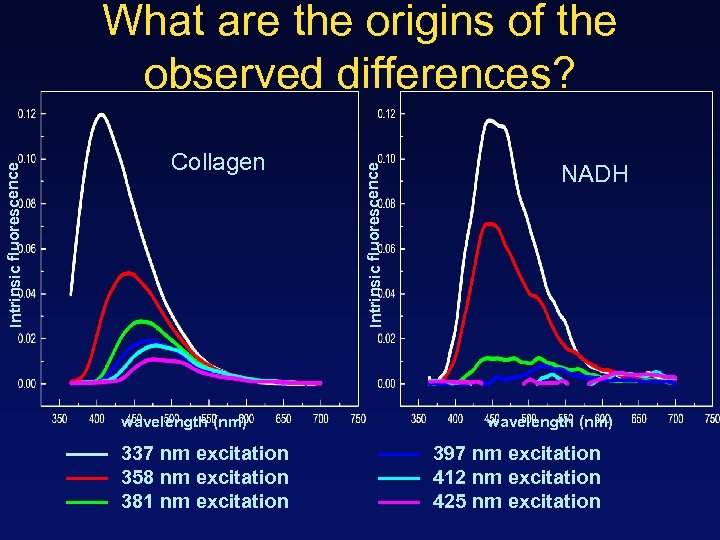 Collagen wavelength (nm) 337 nm excitation 358 nm excitation 381 nm excitation Intrinsic fluorescence What are the origins of the observed differences? NADH wavelength (nm) 397 nm excitation 412 nm excitation 425 nm excitation
Collagen wavelength (nm) 337 nm excitation 358 nm excitation 381 nm excitation Intrinsic fluorescence What are the origins of the observed differences? NADH wavelength (nm) 397 nm excitation 412 nm excitation 425 nm excitation
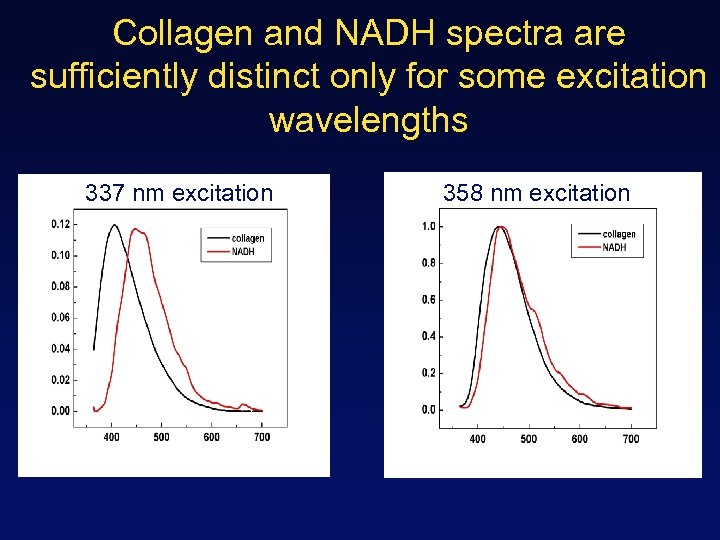 Collagen and NADH spectra are sufficiently distinct only for some excitation wavelengths 337 nm excitation 358 nm excitation
Collagen and NADH spectra are sufficiently distinct only for some excitation wavelengths 337 nm excitation 358 nm excitation
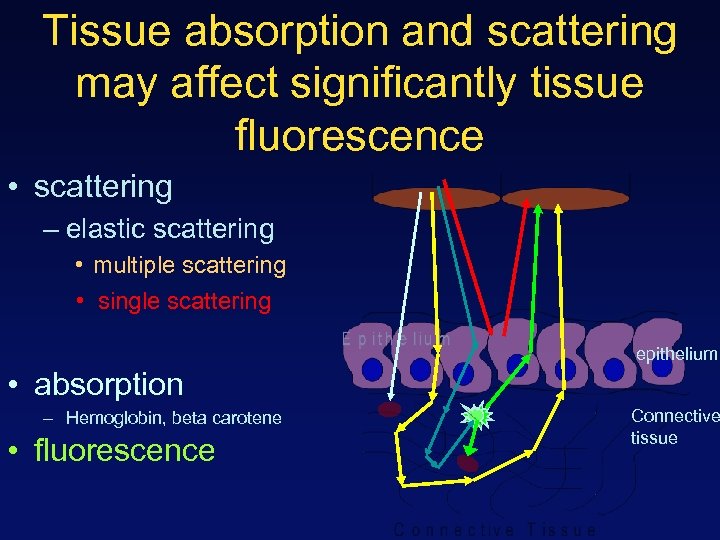 Tissue absorption and scattering may affect significantly tissue fluorescence • scattering – elastic scattering • multiple scattering • single scattering epithelium • absorption – Hemoglobin, beta carotene • fluorescence Connective tissue
Tissue absorption and scattering may affect significantly tissue fluorescence • scattering – elastic scattering • multiple scattering • single scattering epithelium • absorption – Hemoglobin, beta carotene • fluorescence Connective tissue
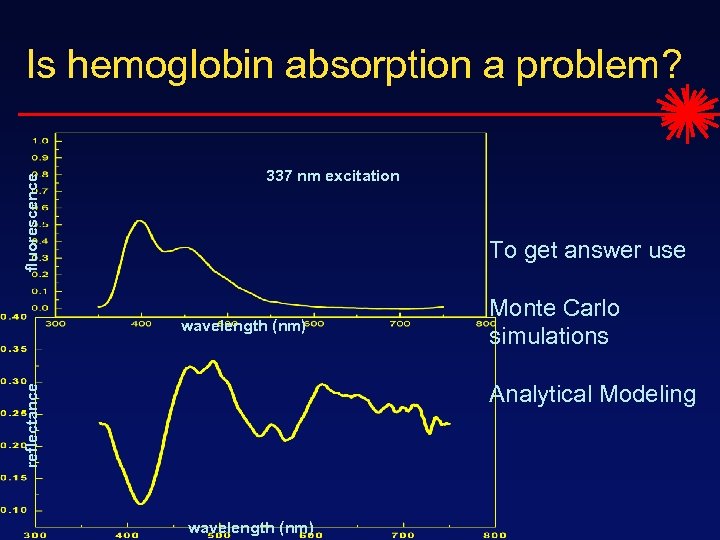 fluorescence Is hemoglobin absorption a problem? 337 nm excitation To get answer use wavelength (nm) Monte Carlo simulations reflectance Analytical Modeling wavelength (nm)
fluorescence Is hemoglobin absorption a problem? 337 nm excitation To get answer use wavelength (nm) Monte Carlo simulations reflectance Analytical Modeling wavelength (nm)


