8d6d271fea6b14c90d9ad78d2aeaa309.ppt
- Количество слайдов: 23
TIPS Made Easy: A Procedure Review Fabbricatore Aldo, Cea-Pereira Sonia Interventional Radiology Hospital Xeral Cies Vigo, Spain
Learning Objectives To present a review on TIPS (Transjugular Intrahepatic Portosystemic Shunt): Indications, contraindications, technique and complications
Transjugular Intrahepatic Portosystemic Shunt (TIPS) Definition It is an interventional radiologic procedure that creates a low-resistance channel between a normal branch of the portal vein and a main hepatic vein to decompress the splanchnic venous system in patient with portal hypertension 1
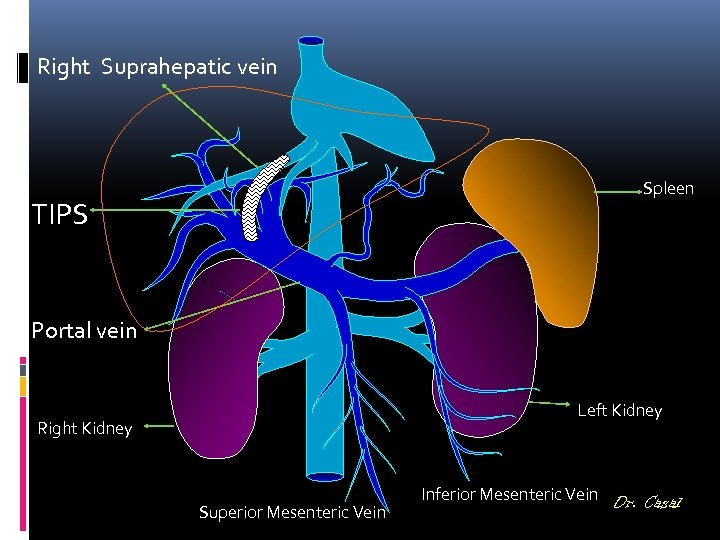
Right Suprahepatic vein Spleen TIPS Portal vein Left Kidney Right Kidney Superior Mesenteric Vein Inferior Mesenteric Vein Dr. Casal
The decision to perform a TIPS, should be reached by a team: Gastroenterologist / hepatologist, interventional radiologist and transplant physician where appropriate. TIPS should only be place by experience interventional radiologist or specially trained physicians. Success and complication rates should be monitored. Boyer TD, Haskal ZJ. . Hepatology 2005 Feb; 41 (2): 386 -400
TIPS Advantage: Inferior morbi-mortality compare to surgery. Transplant: It respects the hepatic hilium It is extracted with the liver (does not requires a surgery) Technical success rate around 95% Control of bleeding achieved in 91 -97% of cases Ascites control improved in 60 -85% of cases Preprocedure survival should be estimated MELD, CHILD-PUGH, APACHE II or bilirrubin
GOAL Variceal bleeding: Reduction in venous portal gradient to less than 12 mm. Hg Refractory Ascites: Reduction in venous portal gradient to at less 8 mm. Hg
Indications Acute variceal bleeding that cannot be successfully controlled with medical treatment (including sclerothepapy). Recurrent or refractory variceal bleeding in patients who cannot tolerate conventional medical treatment. Refractory ascites. Control of hepatic hydrothorax. Budd-Chiari syndrome (moderate disease).
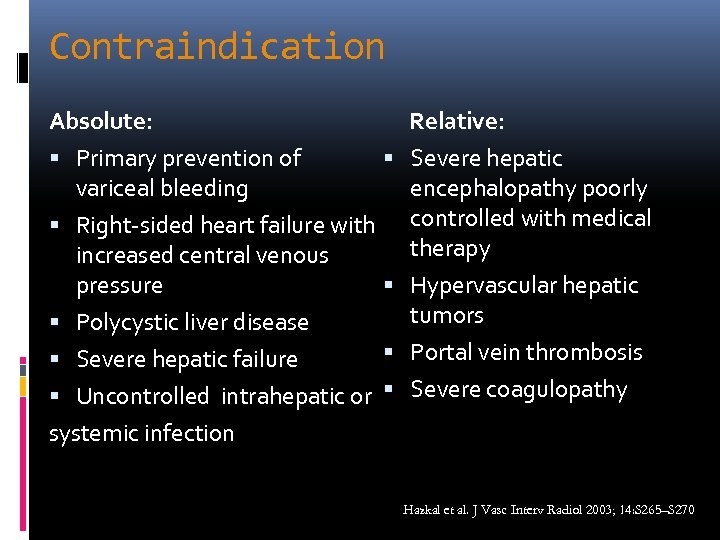
Contraindication Absolute: Primary prevention of variceal bleeding Right-sided heart failure with increased central venous pressure Polycystic liver disease Severe hepatic failure Uncontrolled intrahepatic or systemic infection Relative: Severe hepatic encephalopathy poorly controlled with medical therapy Hypervascular hepatic tumors Portal vein thrombosis Severe coagulopathy Hazkal et al. J Vasc Interv Radiol 2003; 14: S 265–S 270
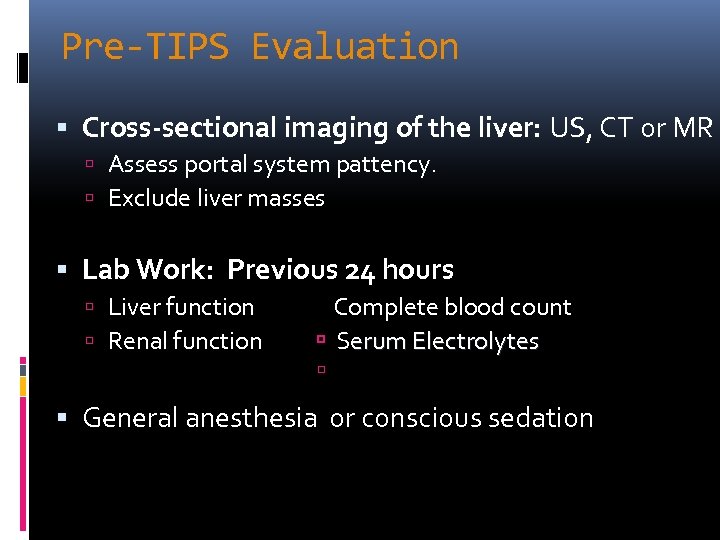
Pre-TIPS Evaluation Cross-sectional imaging of the liver: US, CT or MR Assess portal system pattency. Exclude liver masses Lab Work: Previous 24 hours Liver function Renal function Complete blood count Serum Electrolytes General anesthesia or conscious sedation
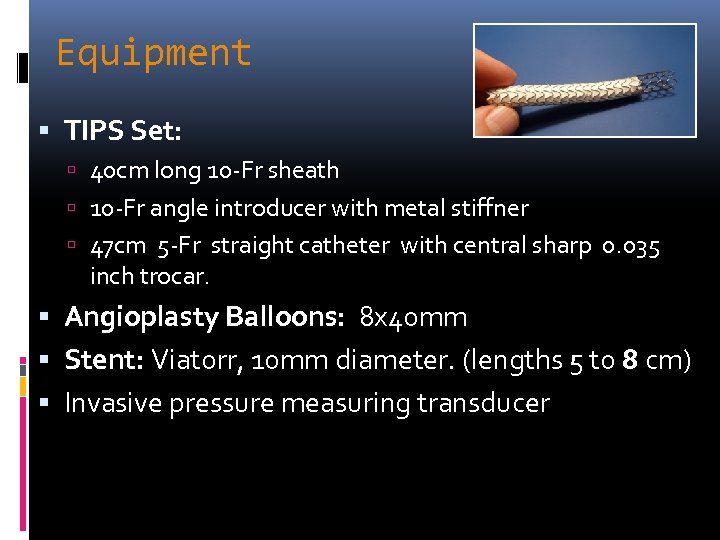
Equipment TIPS Set: 40 cm long 10 -Fr sheath 10 -Fr angle introducer with metal stiffner 47 cm 5 -Fr straight catheter with central sharp 0. 035 inch trocar. Angioplasty Balloons: 8 x 40 mm Stent: Viatorr, 10 mm diameter. (lengths 5 to 8 cm) Invasive pressure measuring transducer
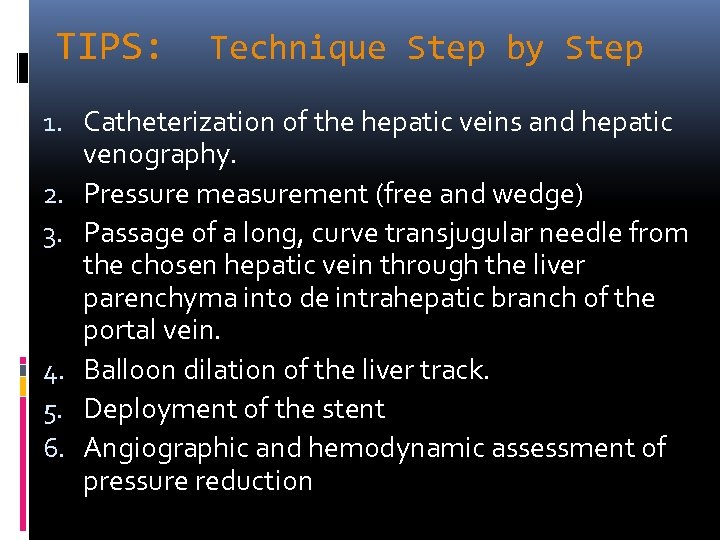
TIPS: Technique Step by Step 1. Catheterization of the hepatic veins and hepatic venography. 2. Pressure measurement (free and wedge) 3. Passage of a long, curve transjugular needle from the chosen hepatic vein through the liver parenchyma into de intrahepatic branch of the portal vein. 4. Balloon dilation of the liver track. 5. Deployment of the stent 6. Angiographic and hemodynamic assessment of pressure reduction
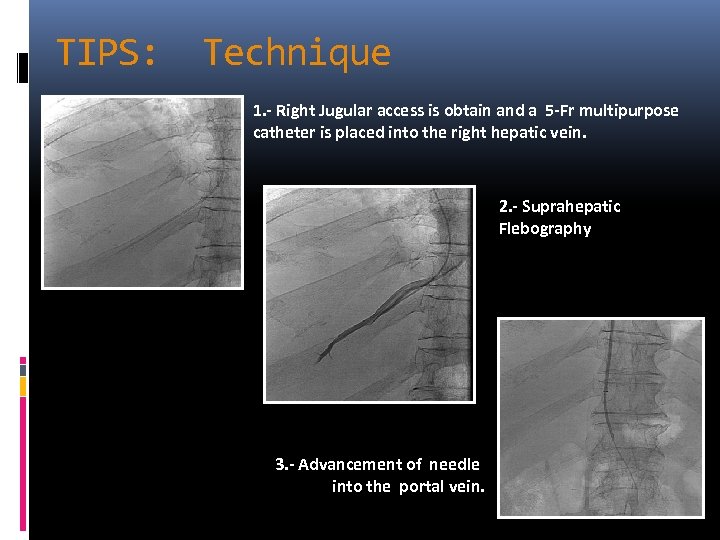
TIPS: Technique 1. - Right Jugular access is obtain and a 5 -Fr multipurpose catheter is placed into the right hepatic vein. 2. - Suprahepatic Flebography 3. - Advancement of needle into the portal vein.
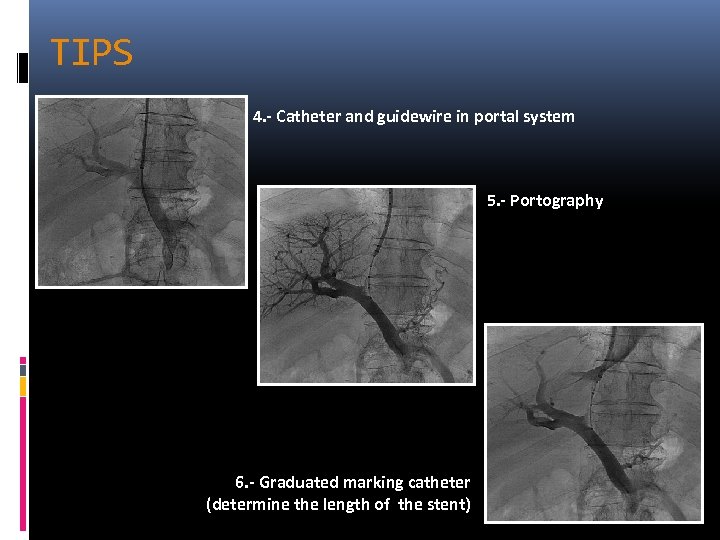
TIPS 4. - Catheter and guidewire in portal system 5. - Portography 6. - Graduated marking catheter (determine the length of the stent)
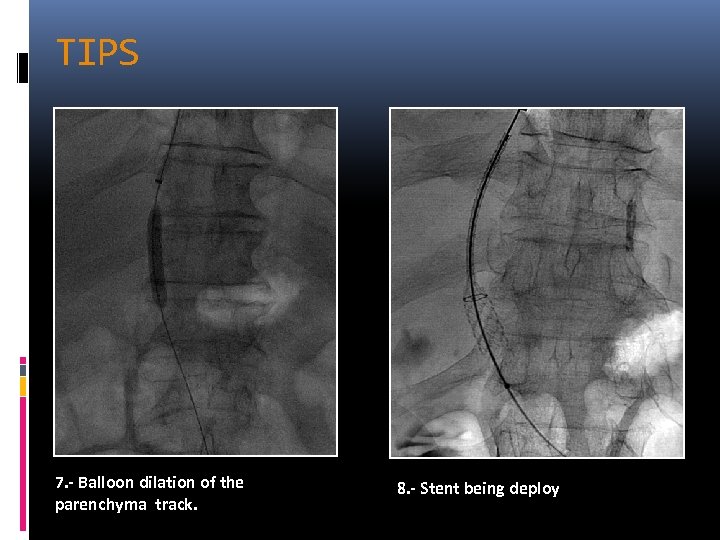
TIPS 7. - Balloon dilation of the parenchyma track. 8. - Stent being deploy
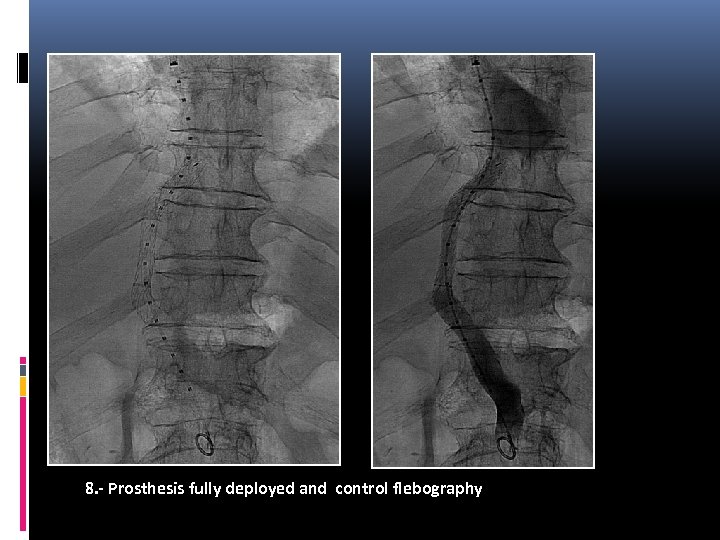
8. - Prosthesis fully deployed and control flebography
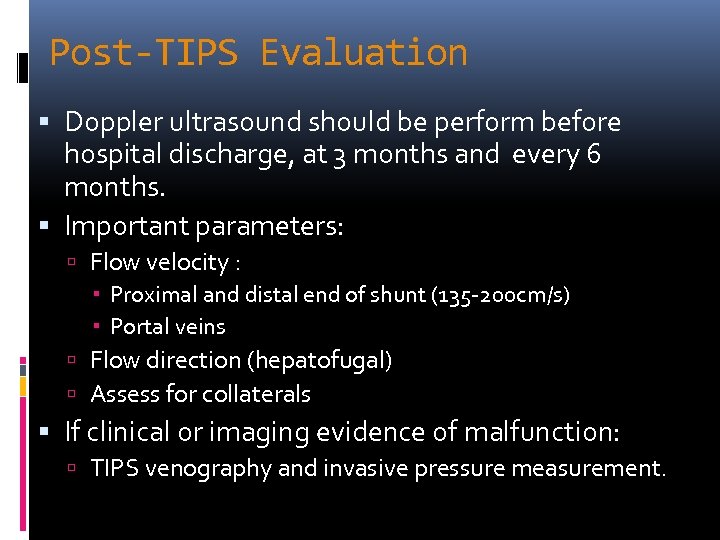
Post-TIPS Evaluation Doppler ultrasound should be perform before hospital discharge, at 3 months and every 6 months. Important parameters: Flow velocity : Proximal and distal end of shunt (135 -200 cm/s) Portal veins Flow direction (hepatofugal) Assess for collaterals If clinical or imaging evidence of malfunction: TIPS venography and invasive pressure measurement.
Complications Intraprocedure Complication around 7% Major Complication 3% Minor Complication 4% Periprocedural complication 10 -15% Intraprocedure Mortality 0 -2% Depends on severity of liver disease Childs-Pugh C 30 days mortality of 90%
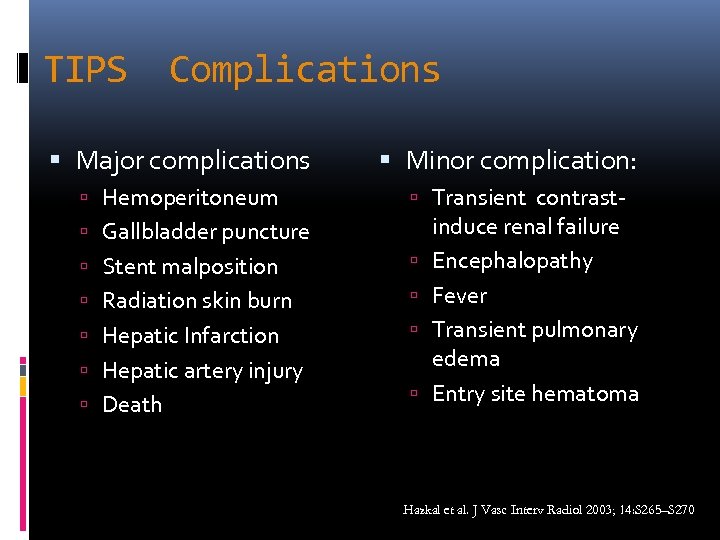
TIPS Complications Major complications Hemoperitoneum Minor complication: Transient contrast- Gallbladder puncture Stent malposition Radiation skin burn Hepatic Infarction Hepatic artery injury Death induce renal failure Encephalopathy Fever Transient pulmonary edema Entry site hematoma Hazkal et al. J Vasc Interv Radiol 2003; 14: S 265–S 270
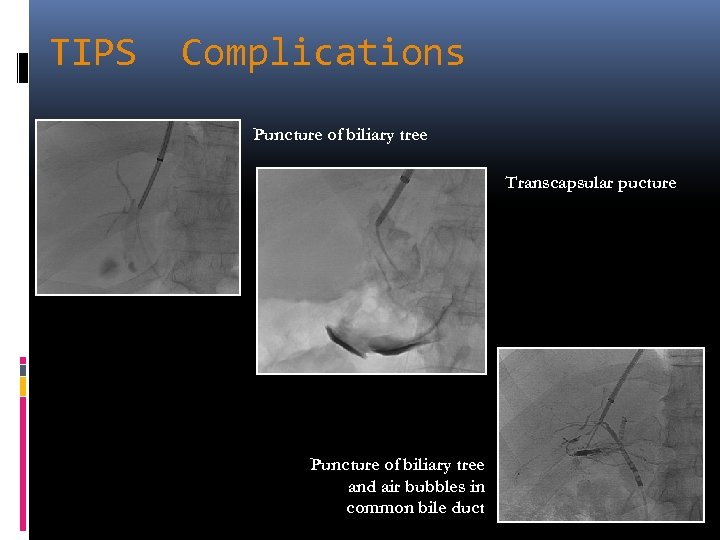
TIPS Complications Puncture of biliary tree Transcapsular pucture Puncture of biliary tree and air bubbles in common bile duct
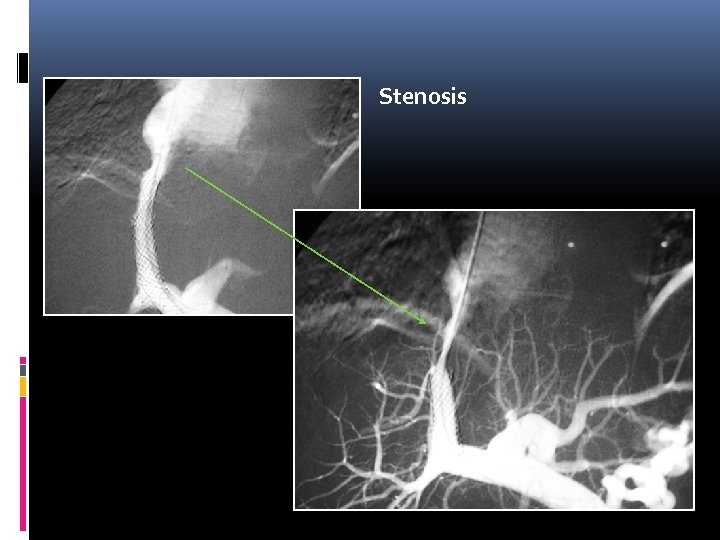
Stenosis
Conclusions TIPS is a safe and successful technique developed to treat complications of portal hypertension with a low incidence of major complications in which patient selection and timing to perform the procedure are critical to obtain a good clinical outcome. TIPS should not be considered as primary therapy for any complication of portal hypertension
Reference 1. Luca et al. TIPS for prevention of recurrent bleeding in patients with cirrhosis: Meta-analysis of randomized clinical trial. Radiology 1999 August; 212 (2): 411 -421. 2. Boyer TD, Haskal ZJ. The role of transjugular intrahepatic portosystemic shunt in the management of portal hypertension. Hepatology 2005 Feb; 41 (2): 386 -400 3. Mauro et al. Image-Guided Interventions. Expert Radiology. 1 st Edition. Saunders. Pennsylvania, USA. 2008. 1777 p 4. Hazkal et al. Quality Improvement Guidelines for Transjugular Intrahepatic Portosystemic Shunt. J Vasc Interv Radiol 2003; 14: S 265– S 270 5. Waldman D, Patel N and Saad W. Interventional Radiology Secrets. 1 st Edition. Hanley&Belfus. USA. 2004. 349 p
8d6d271fea6b14c90d9ad78d2aeaa309.ppt