033ad6b765b39f7ce4225907d55a83ec.ppt
- Количество слайдов: 33
 Timing of Orchidopexy Keeping General Paediatric Surgery in DGH Su-Anna Boddy, FRCS Chair, Children’s Surgical Forum, RCS Consultant Paediatric Urologist, St George’s Hospital 19 Nov 2014
Timing of Orchidopexy Keeping General Paediatric Surgery in DGH Su-Anna Boddy, FRCS Chair, Children’s Surgical Forum, RCS Consultant Paediatric Urologist, St George’s Hospital 19 Nov 2014
 Timing for Orchidopexy • National Screening Committee • East Midlands Specialised Commissioning Group • British Association of Paediatric Urologists Consensus Document • APA + RCPCH • Clinical & Training Standards Manager RCS 2
Timing for Orchidopexy • National Screening Committee • East Midlands Specialised Commissioning Group • British Association of Paediatric Urologists Consensus Document • APA + RCPCH • Clinical & Training Standards Manager RCS 2
 National Screening Committee • Bilateral UDT on NNU refer to Paediatrician • Single UDT examined by GP at 6 weeks, 3 months and 5 -6 months of age • If still UDT then refer to paediatric/adult urologist/surgeon around 1 yr of age • Operation currently planned to be done around 2 yrs of age 3
National Screening Committee • Bilateral UDT on NNU refer to Paediatrician • Single UDT examined by GP at 6 weeks, 3 months and 5 -6 months of age • If still UDT then refer to paediatric/adult urologist/surgeon around 1 yr of age • Operation currently planned to be done around 2 yrs of age 3
 East Midlands Specialist Commissioning Group • The work of the review group resulted in regionally agreed model of care and clinical standards for GPS in the East Midlands • Managed Clinical Networks • One outcome measure was age at orchidopexy – questioning the National Screening Committee current standard 4
East Midlands Specialist Commissioning Group • The work of the review group resulted in regionally agreed model of care and clinical standards for GPS in the East Midlands • Managed Clinical Networks • One outcome measure was age at orchidopexy – questioning the National Screening Committee current standard 4
 BAPU Consensus Document PROMOTING EXCELLENCE IN PAEDIATRIC UROLOGY Germ cells differentiation into adult dark spermatogonia occurs at 3 -6 months. Due to morphology, biopsy and ultrasound changes at 3 to 6 months, early operation may optimise potential fertility outcome and may reduce malignancy • Orchidopexy can occur within 3 -6 months though surgery occurring between 6 and 12 months is acceptable.
BAPU Consensus Document PROMOTING EXCELLENCE IN PAEDIATRIC UROLOGY Germ cells differentiation into adult dark spermatogonia occurs at 3 -6 months. Due to morphology, biopsy and ultrasound changes at 3 to 6 months, early operation may optimise potential fertility outcome and may reduce malignancy • Orchidopexy can occur within 3 -6 months though surgery occurring between 6 and 12 months is acceptable.
 Association of Paediatric Anaesthetists - APA • General anaesthetics and the developing brain – rat studies 2 years ago suggesting anaesthetic agents themselves cause harm to neurodevelopement under 1 yr of age but artificially high doses in rats ( Flack and Soriano ) not supported by FDA • If surgery to under 1 yr olds ? Higher mortality and morbidity and ? In tertiary centre 6
Association of Paediatric Anaesthetists - APA • General anaesthetics and the developing brain – rat studies 2 years ago suggesting anaesthetic agents themselves cause harm to neurodevelopement under 1 yr of age but artificially high doses in rats ( Flack and Soriano ) not supported by FDA • If surgery to under 1 yr olds ? Higher mortality and morbidity and ? In tertiary centre 6
 Commissioning Guide for orchidopexy for UDT needs to be aligned to UK National Screening Standards • • • Richard Stewart , & Sharon Verne, East Midlands SCN Bob Bingham, President APA Feilim Murphy, Secretary BAPU Jane Howdon, RCPCH Su-Anna Boddy, Chair CSF at RCS David Elliman, National Screening Committee Hugh Davies and John Marshall, Public Health England Emma Fernandez, Commissioning guides RCS Apologies Rick Turnock Past President BAPS 7
Commissioning Guide for orchidopexy for UDT needs to be aligned to UK National Screening Standards • • • Richard Stewart , & Sharon Verne, East Midlands SCN Bob Bingham, President APA Feilim Murphy, Secretary BAPU Jane Howdon, RCPCH Su-Anna Boddy, Chair CSF at RCS David Elliman, National Screening Committee Hugh Davies and John Marshall, Public Health England Emma Fernandez, Commissioning guides RCS Apologies Rick Turnock Past President BAPS 7
 Teleconference – History of UDT • 1970 - operation 4 -6 yrs morphology showed testicular atrophy • 1990 – operation 2 yrs before germ cell depletion • 2000 – operation under 1 yr - the sooner the testis located outside the body greater reduction in changes that could impact on sperm cell production 8
Teleconference – History of UDT • 1970 - operation 4 -6 yrs morphology showed testicular atrophy • 1990 – operation 2 yrs before germ cell depletion • 2000 – operation under 1 yr - the sooner the testis located outside the body greater reduction in changes that could impact on sperm cell production 8
 Hadziselimovic and John Hutson • Germ cell differentiation into adult spermatagonia occurs at 3 -6 months • 3 -6 months temperature affects testis development (children undergo a mini puberty) this causes failure of transformation of the cells leading to abnormal cell developement • UDT at 3 months will remain UDT in 98% 9
Hadziselimovic and John Hutson • Germ cell differentiation into adult spermatagonia occurs at 3 -6 months • 3 -6 months temperature affects testis development (children undergo a mini puberty) this causes failure of transformation of the cells leading to abnormal cell developement • UDT at 3 months will remain UDT in 98% 9
 Morphology and later functional change • Data not currently available • Evidence is available from 1970’s shows this is the case but surgery too late • Proxy measures of fertility ie sperm analysis flawed do not predict long term likelihood of parent hood • 2 papers show earlier surgery reduces malignancy 10
Morphology and later functional change • Data not currently available • Evidence is available from 1970’s shows this is the case but surgery too late • Proxy measures of fertility ie sperm analysis flawed do not predict long term likelihood of parent hood • 2 papers show earlier surgery reduces malignancy 10
 Questions from National Screening Committee • Evidence would preferably be by controlled trial and the link between morphological changes and the ability to father children need to be firmly linked. • Are children being operated on within the current time frame? • Large number of boys referred later than current guidelines 11
Questions from National Screening Committee • Evidence would preferably be by controlled trial and the link between morphological changes and the ability to father children need to be firmly linked. • Are children being operated on within the current time frame? • Large number of boys referred later than current guidelines 11
 Recommendation from National Screening Committee after review of ‘evidence’ • GP review at 3 months • If still UDT refer to surgeon • Operation recommended on or around one year of age • This can be incorporated into National Screening committee Guidance without a major change 12
Recommendation from National Screening Committee after review of ‘evidence’ • GP review at 3 months • If still UDT refer to surgeon • Operation recommended on or around one year of age • This can be incorporated into National Screening committee Guidance without a major change 12
 Problems for keeping General Paediatric Surgery in DGHs • How does an agreed age for orchidopexy of around 1 yr of age help this? ! • SAC in General Surgery currently only has an optional module for elective General Surgery of Childhood • Trusts do not advertise jobs for General Surgeons with an commitment in General Paediatric Surgery 13
Problems for keeping General Paediatric Surgery in DGHs • How does an agreed age for orchidopexy of around 1 yr of age help this? ! • SAC in General Surgery currently only has an optional module for elective General Surgery of Childhood • Trusts do not advertise jobs for General Surgeons with an commitment in General Paediatric Surgery 13
 Must keep GPS in DGH • Trusts must advertise General/Urological Surgery + commitment to GPS • Surgeon/anaesthetist to do UDT around 1 yr • BAUS obligatory module/25% of exam in Paediatric Urology good succession planning • Shape of Training? • ASGBI, BAUS, BAPS, + SAC Gen Surg 14
Must keep GPS in DGH • Trusts must advertise General/Urological Surgery + commitment to GPS • Surgeon/anaesthetist to do UDT around 1 yr • BAUS obligatory module/25% of exam in Paediatric Urology good succession planning • Shape of Training? • ASGBI, BAUS, BAPS, + SAC Gen Surg 14
 CSF Guidance to Commissioners and Service Planners • Provides guidance for the development of managed clinical networks • CSF - July 2010 Endorsed by: RCS, RCPCH, RCo. A, APS, APA, ASGBI, BAUS 15
CSF Guidance to Commissioners and Service Planners • Provides guidance for the development of managed clinical networks • CSF - July 2010 Endorsed by: RCS, RCPCH, RCo. A, APS, APA, ASGBI, BAUS 15
 Survey on GPS Service Provision • Published in December 2010 • Delivered by CSF – Funded by DH England • A map of GPS service across all hospitals in England • Numbers of ENT, plastic, Orthopaed, Dental, across all hospitals in England • Available online at: www. rcseng. ac. uk • Planned update 2015
Survey on GPS Service Provision • Published in December 2010 • Delivered by CSF – Funded by DH England • A map of GPS service across all hospitals in England • Numbers of ENT, plastic, Orthopaed, Dental, across all hospitals in England • Available online at: www. rcseng. ac. uk • Planned update 2015
 Children’s Surgical Forum (CSF) • Advisory Multidisciplinary Panel • Setting and monitoring standards • Collaborating with external bodies 17
Children’s Surgical Forum (CSF) • Advisory Multidisciplinary Panel • Setting and monitoring standards • Collaborating with external bodies 17
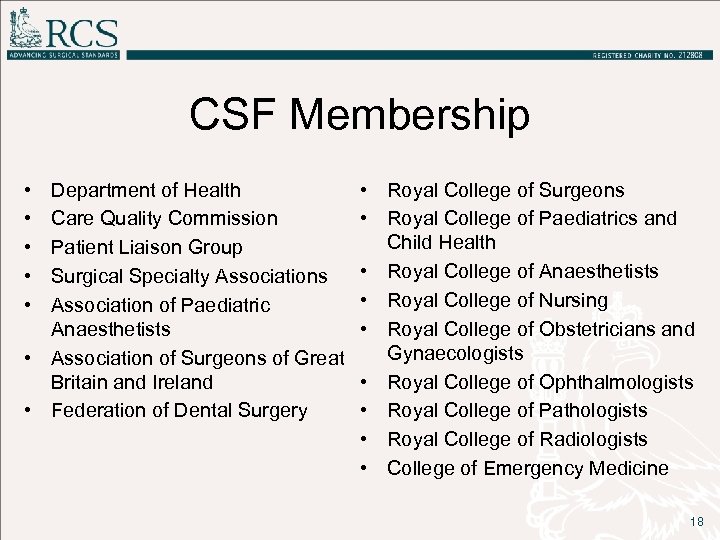 CSF Membership • • • Department of Health Care Quality Commission Patient Liaison Group Surgical Specialty Associations Association of Paediatric Anaesthetists • Association of Surgeons of Great Britain and Ireland • Federation of Dental Surgery • Royal College of Surgeons • Royal College of Paediatrics and Child Health • Royal College of Anaesthetists • Royal College of Nursing • Royal College of Obstetricians and Gynaecologists • Royal College of Ophthalmologists • Royal College of Pathologists • Royal College of Radiologists • College of Emergency Medicine 18
CSF Membership • • • Department of Health Care Quality Commission Patient Liaison Group Surgical Specialty Associations Association of Paediatric Anaesthetists • Association of Surgeons of Great Britain and Ireland • Federation of Dental Surgery • Royal College of Surgeons • Royal College of Paediatrics and Child Health • Royal College of Anaesthetists • Royal College of Nursing • Royal College of Obstetricians and Gynaecologists • Royal College of Ophthalmologists • Royal College of Pathologists • Royal College of Radiologists • College of Emergency Medicine 18
 Managed Clinical Networks • • Interconnected system of providers Not limited by boundaries Multidirectional flow (not hub & spoke) Contractual agreements specifying service requirements and outcomes Benefits: • Common standards • Integrated service • Service planning • Workforce planning • Training • Audit 19
Managed Clinical Networks • • Interconnected system of providers Not limited by boundaries Multidirectional flow (not hub & spoke) Contractual agreements specifying service requirements and outcomes Benefits: • Common standards • Integrated service • Service planning • Workforce planning • Training • Audit 19
 What are the barriers to Managed Paediatric Surgical Networks? • Competitive environment • Lack of financial support • Rigid contractual arrangements 20
What are the barriers to Managed Paediatric Surgical Networks? • Competitive environment • Lack of financial support • Rigid contractual arrangements 20
 NHS Passport – Facilitating Cross-site work • Flexible movement between hospitals • Confirmation that all necessary requirements for safe practice have been carried out in home Trust • Delivery through Appraisal and Revalidation – ‘Certificate’ • Administered via Academy of Royal Colleges – Alastair Henderson
NHS Passport – Facilitating Cross-site work • Flexible movement between hospitals • Confirmation that all necessary requirements for safe practice have been carried out in home Trust • Delivery through Appraisal and Revalidation – ‘Certificate’ • Administered via Academy of Royal Colleges – Alastair Henderson
 NHS Passport – Facilitating Cross-site work Certificate of Fitness for Honorary Practice • Flexible movement of Consultants between hospitals for short-term work and support of colleagues • Cover for emergencies and absences in short notice • Support for clinicians to extend and reinforce their skills Ø Provide and receive short-term specialist training Ø Take advantage of CPD opportunities in innovative techniques and technology
NHS Passport – Facilitating Cross-site work Certificate of Fitness for Honorary Practice • Flexible movement of Consultants between hospitals for short-term work and support of colleagues • Cover for emergencies and absences in short notice • Support for clinicians to extend and reinforce their skills Ø Provide and receive short-term specialist training Ø Take advantage of CPD opportunities in innovative techniques and technology
 Certificate of Fitness for Honorary Practice – Content and Delivery • Information currently included in the Honorary Contract • Confirmation that all necessary requirements for safe practice have been carried out in the home Trust. • No additional paperwork • Delivery through Appraisal and Revalidation 23
Certificate of Fitness for Honorary Practice – Content and Delivery • Information currently included in the Honorary Contract • Confirmation that all necessary requirements for safe practice have been carried out in the home Trust. • No additional paperwork • Delivery through Appraisal and Revalidation 23
 Managed local provider Paediatric Surgical Networks • Support surgeons, anaesthetists, nurses, and whole MDT to ensure children can receive surgical care, in a safe and appropriate environment, which is as close to their home as possible. 24
Managed local provider Paediatric Surgical Networks • Support surgeons, anaesthetists, nurses, and whole MDT to ensure children can receive surgical care, in a safe and appropriate environment, which is as close to their home as possible. 24
 Configuration of Services • Agreed guidelines and protocols for managing the service in place covering the full patient pathway • Regular assessment of performance • Forum for sharing best practice including all contributors 25
Configuration of Services • Agreed guidelines and protocols for managing the service in place covering the full patient pathway • Regular assessment of performance • Forum for sharing best practice including all contributors 25
 Governance and leadership • Written policy regarding age range of children anaesthetised and operated upon within the hospital (and for out-of-hours period if level of paediatric anaesthetic competences is different) • Evaluated with audit of outcomes, transfers and untoward incidents 26
Governance and leadership • Written policy regarding age range of children anaesthetised and operated upon within the hospital (and for out-of-hours period if level of paediatric anaesthetic competences is different) • Evaluated with audit of outcomes, transfers and untoward incidents 26
 Education and training • Consultants work within limits of their professional competence • All surgeons and anaesthetists operating on and anaesthetising children, regularly undertake paediatric life support training and safe guarding. 27
Education and training • Consultants work within limits of their professional competence • All surgeons and anaesthetists operating on and anaesthetising children, regularly undertake paediatric life support training and safe guarding. 27
 Delivery and environment • Care is delivered in a child and family-friendly environment with registered children’s nurses • At any time the emergency department includes sufficient cover for emergencies in children • Surgeons and anaesthetists providing this cover have appropriate training, competence and CPD 28
Delivery and environment • Care is delivered in a child and family-friendly environment with registered children’s nurses • At any time the emergency department includes sufficient cover for emergencies in children • Surgeons and anaesthetists providing this cover have appropriate training, competence and CPD 28
 Keeping GPS in DGH • Managed Clinical Networks • Trusts to appropriately advertise • Shape of Training? A General Surgeon who can deliver elective and emergency surgery in children ( and adults? ) • Paediatric surgeons from Tertiary centre? • Anaesthetists keeping appropriate skills for young children 29
Keeping GPS in DGH • Managed Clinical Networks • Trusts to appropriately advertise • Shape of Training? A General Surgeon who can deliver elective and emergency surgery in children ( and adults? ) • Paediatric surgeons from Tertiary centre? • Anaesthetists keeping appropriate skills for young children 29
 Commissioning Guidance by all 10 Specialty Associations at RCS, badged by NICE 30
Commissioning Guidance by all 10 Specialty Associations at RCS, badged by NICE 30
 SCNs need to establish Managed Paediatric Surgical Networks for all of Children’s Surgery 31
SCNs need to establish Managed Paediatric Surgical Networks for all of Children’s Surgery 31
 32
32
 Let’s Network! CSForum@rcseng. ac. uk
Let’s Network! CSForum@rcseng. ac. uk


