beda266d7818894193e9d500069df2af.ppt
- Количество слайдов: 38
 Tightly integrated internal solutions: Care management UMR Care Management provides integrated, member-centric services that can be tailored to your overall strategy. We help employers develop multi-year strategies to adapt their health culture to value healthy lifestyles, emphasize personal accountability and, ultimately, mitigate their medical claim trend. We focus on educating and motivating members, moving them from incentives for participation to incentives based on achievement of empirical, clinical health markers, such as BMI, LDL, fasting glucose and blood pressure. We equip your plan members with the knowledge and resources to take a more active role in their health care decisions and to think like consumers when choosing the right options for them. UMR recognizes that when it comes to member care, one size does not fit all – a service of utmost value to one plan member may be of little or no value to another. Incentives, such as reduced co-pays or premiums, reward members for appropriate use of high-value services or adopting a healthy lifestyle. Government estimates show as much as 75 percent of health care costs can be attributed to a preventable disease, so offering 100 percent coverage for preventive care may be a sound investment. Preventive care, such as age- and gender-specific screenings, can detect these diseases early, when they are most treatable, and help at-risk members make healthy lifestyle changes to avoid developing a chronic and costly condition. We can also offer value-based benefit solutions that combine the strength of our care management programs with the benefits of consumer-driven health plans. The result is a plan that uses incentives to steer plan members to the highest-value care at the most affordable rates. 1 © 2012 United Health. Care Services, Inc.
Tightly integrated internal solutions: Care management UMR Care Management provides integrated, member-centric services that can be tailored to your overall strategy. We help employers develop multi-year strategies to adapt their health culture to value healthy lifestyles, emphasize personal accountability and, ultimately, mitigate their medical claim trend. We focus on educating and motivating members, moving them from incentives for participation to incentives based on achievement of empirical, clinical health markers, such as BMI, LDL, fasting glucose and blood pressure. We equip your plan members with the knowledge and resources to take a more active role in their health care decisions and to think like consumers when choosing the right options for them. UMR recognizes that when it comes to member care, one size does not fit all – a service of utmost value to one plan member may be of little or no value to another. Incentives, such as reduced co-pays or premiums, reward members for appropriate use of high-value services or adopting a healthy lifestyle. Government estimates show as much as 75 percent of health care costs can be attributed to a preventable disease, so offering 100 percent coverage for preventive care may be a sound investment. Preventive care, such as age- and gender-specific screenings, can detect these diseases early, when they are most treatable, and help at-risk members make healthy lifestyle changes to avoid developing a chronic and costly condition. We can also offer value-based benefit solutions that combine the strength of our care management programs with the benefits of consumer-driven health plans. The result is a plan that uses incentives to steer plan members to the highest-value care at the most affordable rates. 1 © 2012 United Health. Care Services, Inc.
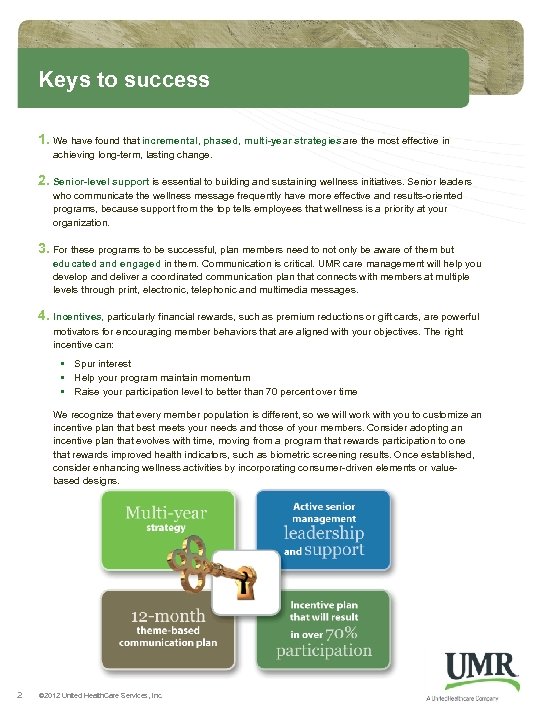 Keys to success 1. We have found that incremental, phased, multi-year strategies are the most effective in achieving long-term, lasting change. 2. Senior-level support is essential to building and sustaining wellness initiatives. Senior leaders who communicate the wellness message frequently have more effective and results-oriented programs, because support from the top tells employees that wellness is a priority at your organization. 3. For these programs to be successful, plan members need to not only be aware of them but educated and engaged in them. Communication is critical. UMR care management will help you develop and deliver a coordinated communication plan that connects with members at multiple levels through print, electronic, telephonic and multimedia messages. 4. Incentives, particularly financial rewards, such as premium reductions or gift cards, are powerful motivators for encouraging member behaviors that are aligned with your objectives. The right incentive can: • Spur interest • Help your program maintain momentum • Raise your participation level to better than 70 percent over time We recognize that every member population is different, so we will work with you to customize an incentive plan that best meets your needs and those of your members. Consider adopting an incentive plan that evolves with time, moving from a program that rewards participation to one that rewards improved health indicators, such as biometric screening results. Once established, consider enhancing wellness activities by incorporating consumer-driven elements or valuebased designs. 2 © 2012 United Health. Care Services, Inc.
Keys to success 1. We have found that incremental, phased, multi-year strategies are the most effective in achieving long-term, lasting change. 2. Senior-level support is essential to building and sustaining wellness initiatives. Senior leaders who communicate the wellness message frequently have more effective and results-oriented programs, because support from the top tells employees that wellness is a priority at your organization. 3. For these programs to be successful, plan members need to not only be aware of them but educated and engaged in them. Communication is critical. UMR care management will help you develop and deliver a coordinated communication plan that connects with members at multiple levels through print, electronic, telephonic and multimedia messages. 4. Incentives, particularly financial rewards, such as premium reductions or gift cards, are powerful motivators for encouraging member behaviors that are aligned with your objectives. The right incentive can: • Spur interest • Help your program maintain momentum • Raise your participation level to better than 70 percent over time We recognize that every member population is different, so we will work with you to customize an incentive plan that best meets your needs and those of your members. Consider adopting an incentive plan that evolves with time, moving from a program that rewards participation to one that rewards improved health indicators, such as biometric screening results. Once established, consider enhancing wellness activities by incorporating consumer-driven elements or valuebased designs. 2 © 2012 United Health. Care Services, Inc.
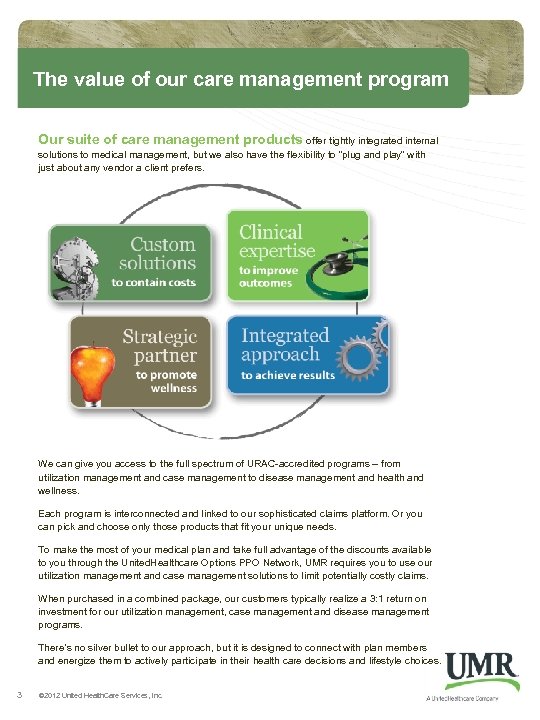 The value of our care management program Our suite of care management products offer tightly integrated internal solutions to medical management, but we also have the flexibility to “plug and play” with just about any vendor a client prefers. We can give you access to the full spectrum of URAC-accredited programs – from utilization management and case management to disease management and health and wellness. Each program is interconnected and linked to our sophisticated claims platform. Or you can pick and choose only those products that fit your unique needs. To make the most of your medical plan and take full advantage of the discounts available to you through the United. Healthcare Options PPO Network, UMR requires you to use our utilization management and case management solutions to limit potentially costly claims. When purchased in a combined package, our customers typically realize a 3: 1 return on investment for our utilization management, case management and disease management programs. There’s no silver bullet to our approach, but it is designed to connect with plan members and energize them to actively participate in their health care decisions and lifestyle choices. 3 © 2012 United Health. Care Services, Inc.
The value of our care management program Our suite of care management products offer tightly integrated internal solutions to medical management, but we also have the flexibility to “plug and play” with just about any vendor a client prefers. We can give you access to the full spectrum of URAC-accredited programs – from utilization management and case management to disease management and health and wellness. Each program is interconnected and linked to our sophisticated claims platform. Or you can pick and choose only those products that fit your unique needs. To make the most of your medical plan and take full advantage of the discounts available to you through the United. Healthcare Options PPO Network, UMR requires you to use our utilization management and case management solutions to limit potentially costly claims. When purchased in a combined package, our customers typically realize a 3: 1 return on investment for our utilization management, case management and disease management programs. There’s no silver bullet to our approach, but it is designed to connect with plan members and energize them to actively participate in their health care decisions and lifestyle choices. 3 © 2012 United Health. Care Services, Inc.
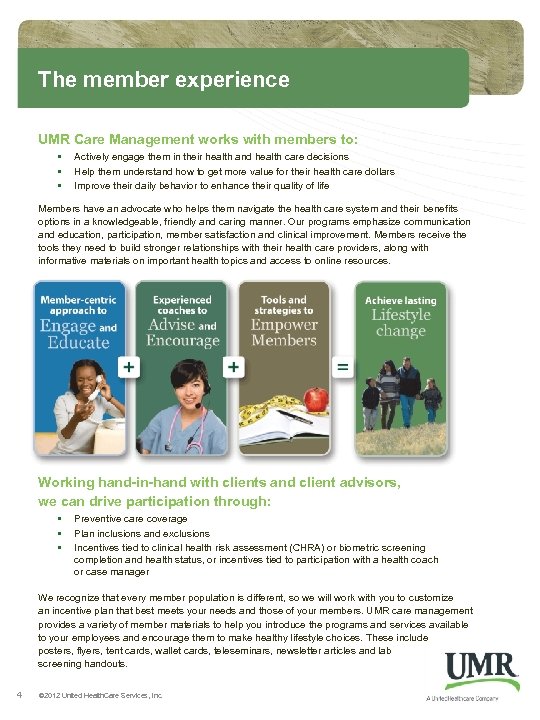 The member experience UMR Care Management works with members to: • • • Actively engage them in their health and health care decisions Help them understand how to get more value for their health care dollars Improve their daily behavior to enhance their quality of life Members have an advocate who helps them navigate the health care system and their benefits options in a knowledgeable, friendly and caring manner. Our programs emphasize communication and education, participation, member satisfaction and clinical improvement. Members receive the tools they need to build stronger relationships with their health care providers, along with informative materials on important health topics and access to online resources. Working hand-in-hand with clients and client advisors, we can drive participation through: • • • Preventive care coverage Plan inclusions and exclusions Incentives tied to clinical health risk assessment (CHRA) or biometric screening completion and health status, or incentives tied to participation with a health coach or case manager We recognize that every member population is different, so we will work with you to customize an incentive plan that best meets your needs and those of your members. UMR care management provides a variety of member materials to help you introduce the programs and services available to your employees and encourage them to make healthy lifestyle choices. These include posters, flyers, tent cards, wallet cards, teleseminars, newsletter articles and lab screening handouts. 4 © 2012 United Health. Care Services, Inc.
The member experience UMR Care Management works with members to: • • • Actively engage them in their health and health care decisions Help them understand how to get more value for their health care dollars Improve their daily behavior to enhance their quality of life Members have an advocate who helps them navigate the health care system and their benefits options in a knowledgeable, friendly and caring manner. Our programs emphasize communication and education, participation, member satisfaction and clinical improvement. Members receive the tools they need to build stronger relationships with their health care providers, along with informative materials on important health topics and access to online resources. Working hand-in-hand with clients and client advisors, we can drive participation through: • • • Preventive care coverage Plan inclusions and exclusions Incentives tied to clinical health risk assessment (CHRA) or biometric screening completion and health status, or incentives tied to participation with a health coach or case manager We recognize that every member population is different, so we will work with you to customize an incentive plan that best meets your needs and those of your members. UMR care management provides a variety of member materials to help you introduce the programs and services available to your employees and encourage them to make healthy lifestyle choices. These include posters, flyers, tent cards, wallet cards, teleseminars, newsletter articles and lab screening handouts. 4 © 2012 United Health. Care Services, Inc.
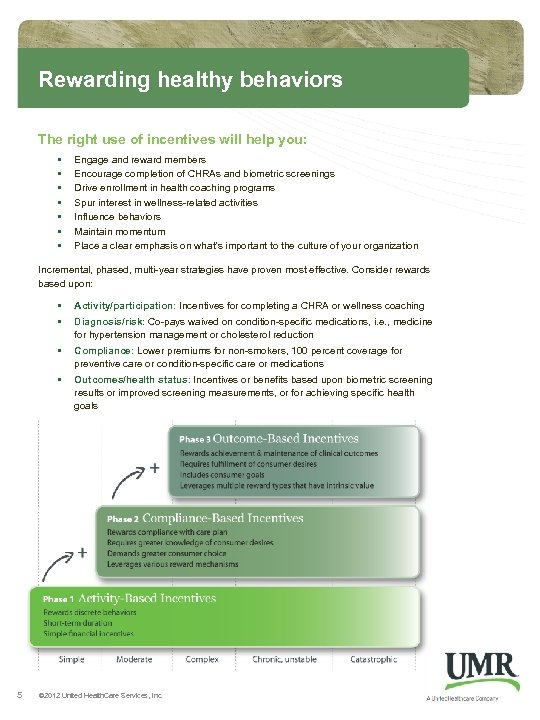 Rewarding healthy behaviors The right use of incentives will help you: • • Engage and reward members Encourage completion of CHRAs and biometric screenings Drive enrollment in health coaching programs Spur interest in wellness-related activities Influence behaviors Maintain momentum Place a clear emphasis on what’s important to the culture of your organization Incremental, phased, multi-year strategies have proven most effective. Consider rewards based upon: • • • Compliance: Lower premiums for non-smokers, 100 percent coverage for preventive care or condition-specific care or medications • 5 Activity/participation: Incentives for completing a CHRA or wellness coaching Outcomes/health status: Incentives or benefits based upon biometric screening results or improved screening measurements, or for achieving specific health goals Diagnosis/risk: Co-pays waived on condition-specific medications, i. e. , medicine for hypertension management or cholesterol reduction © 2012 United Health. Care Services, Inc.
Rewarding healthy behaviors The right use of incentives will help you: • • Engage and reward members Encourage completion of CHRAs and biometric screenings Drive enrollment in health coaching programs Spur interest in wellness-related activities Influence behaviors Maintain momentum Place a clear emphasis on what’s important to the culture of your organization Incremental, phased, multi-year strategies have proven most effective. Consider rewards based upon: • • • Compliance: Lower premiums for non-smokers, 100 percent coverage for preventive care or condition-specific care or medications • 5 Activity/participation: Incentives for completing a CHRA or wellness coaching Outcomes/health status: Incentives or benefits based upon biometric screening results or improved screening measurements, or for achieving specific health goals Diagnosis/risk: Co-pays waived on condition-specific medications, i. e. , medicine for hypertension management or cholesterol reduction © 2012 United Health. Care Services, Inc.
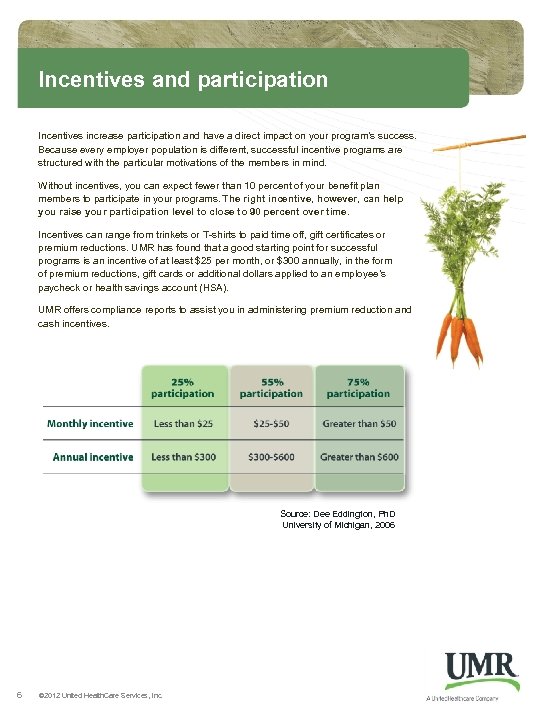 Incentives and participation Incentives increase participation and have a direct impact on your program’s success. Because every employer population is different, successful incentive programs are structured with the particular motivations of the members in mind. Without incentives, you can expect fewer than 10 percent of your benefit plan members to participate in your programs. The right incentive, however, can help you raise your participation level to close to 90 percent over time. Incentives can range from trinkets or T-shirts to paid time off, gift certificates or premium reductions. UMR has found that a good starting point for successful programs is an incentive of at least $25 per month, or $300 annually, in the form of premium reductions, gift cards or additional dollars applied to an employee’s paycheck or health savings account (HSA). UMR offers compliance reports to assist you in administering premium reduction and cash incentives. Source: Dee Eddington, Ph. D University of Michigan, 2006 6 © 2012 United Health. Care Services, Inc.
Incentives and participation Incentives increase participation and have a direct impact on your program’s success. Because every employer population is different, successful incentive programs are structured with the particular motivations of the members in mind. Without incentives, you can expect fewer than 10 percent of your benefit plan members to participate in your programs. The right incentive, however, can help you raise your participation level to close to 90 percent over time. Incentives can range from trinkets or T-shirts to paid time off, gift certificates or premium reductions. UMR has found that a good starting point for successful programs is an incentive of at least $25 per month, or $300 annually, in the form of premium reductions, gift cards or additional dollars applied to an employee’s paycheck or health savings account (HSA). UMR offers compliance reports to assist you in administering premium reduction and cash incentives. Source: Dee Eddington, Ph. D University of Michigan, 2006 6 © 2012 United Health. Care Services, Inc.
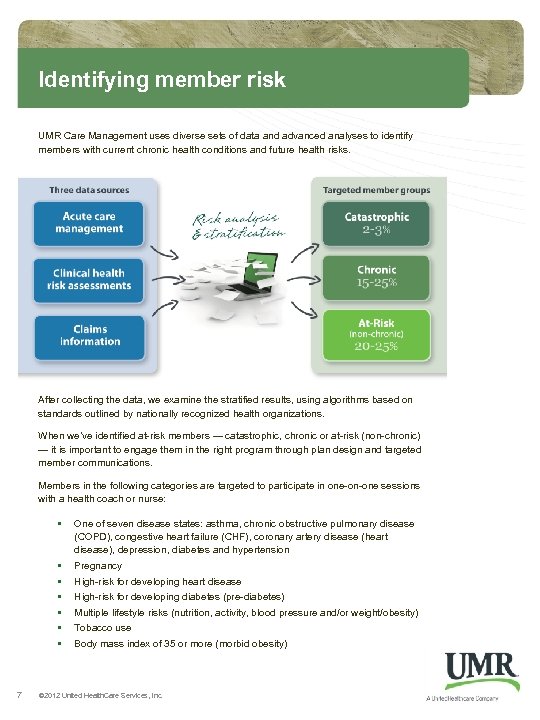 Identifying member risk UMR Care Management uses diverse sets of data and advanced analyses to identify members with current chronic health conditions and future health risks. After collecting the data, we examine the stratified results, using algorithms based on standards outlined by nationally recognized health organizations. When we’ve identified at-risk members — catastrophic, chronic or at-risk (non-chronic) — it is important to engage them in the right program through plan design and targeted member communications. Members in the following categories are targeted to participate in one-on-one sessions with a health coach or nurse: • • 7 One of seven disease states: asthma, chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), coronary artery disease (heart disease), depression, diabetes and hypertension Pregnancy High-risk for developing heart disease High-risk for developing diabetes (pre-diabetes) Multiple lifestyle risks (nutrition, activity, blood pressure and/or weight/obesity) Tobacco use Body mass index of 35 or more (morbid obesity) © 2012 United Health. Care Services, Inc.
Identifying member risk UMR Care Management uses diverse sets of data and advanced analyses to identify members with current chronic health conditions and future health risks. After collecting the data, we examine the stratified results, using algorithms based on standards outlined by nationally recognized health organizations. When we’ve identified at-risk members — catastrophic, chronic or at-risk (non-chronic) — it is important to engage them in the right program through plan design and targeted member communications. Members in the following categories are targeted to participate in one-on-one sessions with a health coach or nurse: • • 7 One of seven disease states: asthma, chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), coronary artery disease (heart disease), depression, diabetes and hypertension Pregnancy High-risk for developing heart disease High-risk for developing diabetes (pre-diabetes) Multiple lifestyle risks (nutrition, activity, blood pressure and/or weight/obesity) Tobacco use Body mass index of 35 or more (morbid obesity) © 2012 United Health. Care Services, Inc.
 Nurse. Line® and maternity management Nurse. Line connects members with highly trained registered nurses any time of day, seven days a week. Nurses help callers make more informed choices about when and where to seek the appropriate care, providing information on specific conditions and treatment options. This can result in fewer emergency room visits and hospital stays, leading to lower overall health expenses. Through Nurse. Line, members also can access an audio health information library, with more than 1, 100 recorded topics, such as aging, common illnesses, fitness and surgical procedures. Our maternity management program offers assessments and information for women considering having a baby and prenatal education and guidance to those expecting. The result is an increased number of healthy, full-term deliveries and a decrease in costly, extended hospital stays. We identify participants using claim edits, triggers and utilization review. Our nurse coaches then provide education, follow-up calls and support based on the woman’s individual risks. Those identified as high-risk are placed into our case management program, to monitor their conditions and keep customers informed of high-cost situations. All members who join the maternity management program during the first or second trimester receive an incentive gift. Once enrolled in the program, expectant mothers are contacted by nurse case managers who have extensive clinical backgrounds in obstetrics/ gynecology. Members also can choose from a selection of highquality books and other materials containing helpful information about pregnancy, pre-term labor, childbirth, breast feeding and infant care. 8 © 2012 United Health. Care Services, Inc.
Nurse. Line® and maternity management Nurse. Line connects members with highly trained registered nurses any time of day, seven days a week. Nurses help callers make more informed choices about when and where to seek the appropriate care, providing information on specific conditions and treatment options. This can result in fewer emergency room visits and hospital stays, leading to lower overall health expenses. Through Nurse. Line, members also can access an audio health information library, with more than 1, 100 recorded topics, such as aging, common illnesses, fitness and surgical procedures. Our maternity management program offers assessments and information for women considering having a baby and prenatal education and guidance to those expecting. The result is an increased number of healthy, full-term deliveries and a decrease in costly, extended hospital stays. We identify participants using claim edits, triggers and utilization review. Our nurse coaches then provide education, follow-up calls and support based on the woman’s individual risks. Those identified as high-risk are placed into our case management program, to monitor their conditions and keep customers informed of high-cost situations. All members who join the maternity management program during the first or second trimester receive an incentive gift. Once enrolled in the program, expectant mothers are contacted by nurse case managers who have extensive clinical backgrounds in obstetrics/ gynecology. Members also can choose from a selection of highquality books and other materials containing helpful information about pregnancy, pre-term labor, childbirth, breast feeding and infant care. 8 © 2012 United Health. Care Services, Inc.
 Health and wellness UMR’s health and wellness program provides a proactive approach to improving the health of employees. We identify members’ current and future health risks and then help them understand those risks and how they are linked to conditions such as diabetes and heart disease. We give them the tools and support to make healthier lifestyle choices that reduce their likelihood of developing a chronic disease. Completing a clinical health risk assessment (CHRA) is the first step for members. Our CHRA asks questions about members’ medical history and lifestyle habits such as food choices, physical activity level, tobacco use and readiness to change. We combine the CHRA reports with biometric screening results for blood pressure, glucose levels and cholesterol to gain a more complete picture of the overall health of a group. Members identified as high risk for future health problems are invited to work with a personal health coach in a series of one-on-one phone conversations. Our coaches are trained in behavior-change techniques and provide information and encouragement to help participants set goals and follow through with their plan to live healthier. UMR can assist you in establishing a workplace culture that supports healthy behaviors to improve the well-being of your employees. We provide strategies and support in crafting customized wellness plans, along with employee challenges that encourage participation in physical activity, weight loss or healthy eating programs. We encourage customers to attach incentives to their wellness programs. Incentives increase participation and have a direct impact on your program’s success. Because every employer population is different, successful incentive programs are structured with the particular motivations of the members in mind. The program includes: Clinical health risk assessments Onsite biometric health screenings Personal health coaching Quarterly newsletters Educational information Worksite wellness strategies and support Incentive administration 9 © 2012 United Health. Care Services, Inc.
Health and wellness UMR’s health and wellness program provides a proactive approach to improving the health of employees. We identify members’ current and future health risks and then help them understand those risks and how they are linked to conditions such as diabetes and heart disease. We give them the tools and support to make healthier lifestyle choices that reduce their likelihood of developing a chronic disease. Completing a clinical health risk assessment (CHRA) is the first step for members. Our CHRA asks questions about members’ medical history and lifestyle habits such as food choices, physical activity level, tobacco use and readiness to change. We combine the CHRA reports with biometric screening results for blood pressure, glucose levels and cholesterol to gain a more complete picture of the overall health of a group. Members identified as high risk for future health problems are invited to work with a personal health coach in a series of one-on-one phone conversations. Our coaches are trained in behavior-change techniques and provide information and encouragement to help participants set goals and follow through with their plan to live healthier. UMR can assist you in establishing a workplace culture that supports healthy behaviors to improve the well-being of your employees. We provide strategies and support in crafting customized wellness plans, along with employee challenges that encourage participation in physical activity, weight loss or healthy eating programs. We encourage customers to attach incentives to their wellness programs. Incentives increase participation and have a direct impact on your program’s success. Because every employer population is different, successful incentive programs are structured with the particular motivations of the members in mind. The program includes: Clinical health risk assessments Onsite biometric health screenings Personal health coaching Quarterly newsletters Educational information Worksite wellness strategies and support Incentive administration 9 © 2012 United Health. Care Services, Inc.
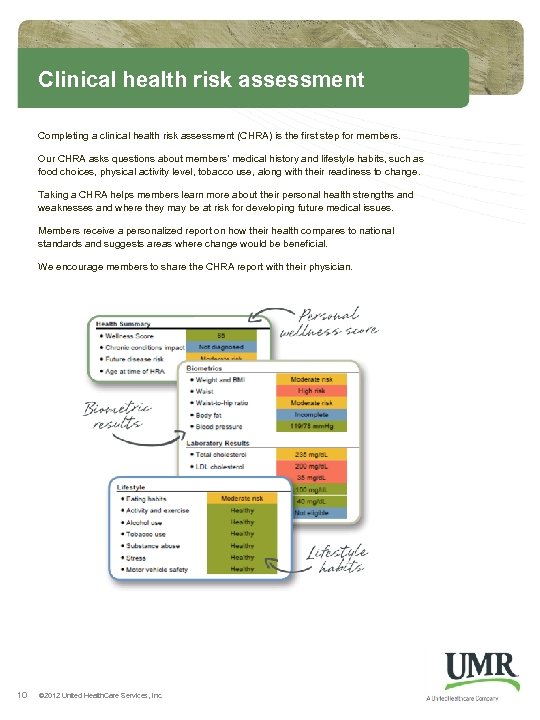 Clinical health risk assessment Completing a clinical health risk assessment (CHRA) is the first step for members. Our CHRA asks questions about members’ medical history and lifestyle habits, such as food choices, physical activity level, tobacco use, along with their readiness to change. Taking a CHRA helps members learn more about their personal health strengths and weaknesses and where they may be at risk for developing future medical issues. Members receive a personalized report on how their health compares to national standards and suggests areas where change would be beneficial. We encourage members to share the CHRA report with their physician. 10 © 2012 United Health. Care Services, Inc.
Clinical health risk assessment Completing a clinical health risk assessment (CHRA) is the first step for members. Our CHRA asks questions about members’ medical history and lifestyle habits, such as food choices, physical activity level, tobacco use, along with their readiness to change. Taking a CHRA helps members learn more about their personal health strengths and weaknesses and where they may be at risk for developing future medical issues. Members receive a personalized report on how their health compares to national standards and suggests areas where change would be beneficial. We encourage members to share the CHRA report with their physician. 10 © 2012 United Health. Care Services, Inc.
 Onsite biometric screenings We combine the CHRA reports with biometric screening results, such as blood pressure, glucose levels and cholesterol, to gain a more complete picture of the overall health of a group. Screening results also help us to determine which individuals would benefit most from working with a health and wellness coach in making lifestyle changes to reduce their risks of developing a chronic medical condition, such as heart disease or diabetes. Our biometric screening partner, Wellness Inc. , will guide each customer through the program implementation process, including the selection of onsite screening dates, customization of promotional materials, registration and identification of staffing needs. Wellness Inc. will mail the test results to each participant’s home within two weeks, and all results from the biometric screening will be securely transferred and populated to the participant’s online CHRA. Members who cannot receive their biometric tests during a scheduled onsite date have access to a national network of labs, where they can go to complete their screenings. This network is available through a partnership with Lab. Corp, a nationally recognized business with more than 2, 500 labs nationwide. Screenings include: Blood pressure Height and weight Waist circumference Body-mass index (BMI) Basic blood panel (lipids, fasting glucose) Venipuncture or finger stick Critical call outreach Convenient process for remote employees Flu vaccinations 11 © 2012 United Health. Care Services, Inc.
Onsite biometric screenings We combine the CHRA reports with biometric screening results, such as blood pressure, glucose levels and cholesterol, to gain a more complete picture of the overall health of a group. Screening results also help us to determine which individuals would benefit most from working with a health and wellness coach in making lifestyle changes to reduce their risks of developing a chronic medical condition, such as heart disease or diabetes. Our biometric screening partner, Wellness Inc. , will guide each customer through the program implementation process, including the selection of onsite screening dates, customization of promotional materials, registration and identification of staffing needs. Wellness Inc. will mail the test results to each participant’s home within two weeks, and all results from the biometric screening will be securely transferred and populated to the participant’s online CHRA. Members who cannot receive their biometric tests during a scheduled onsite date have access to a national network of labs, where they can go to complete their screenings. This network is available through a partnership with Lab. Corp, a nationally recognized business with more than 2, 500 labs nationwide. Screenings include: Blood pressure Height and weight Waist circumference Body-mass index (BMI) Basic blood panel (lipids, fasting glucose) Venipuncture or finger stick Critical call outreach Convenient process for remote employees Flu vaccinations 11 © 2012 United Health. Care Services, Inc.
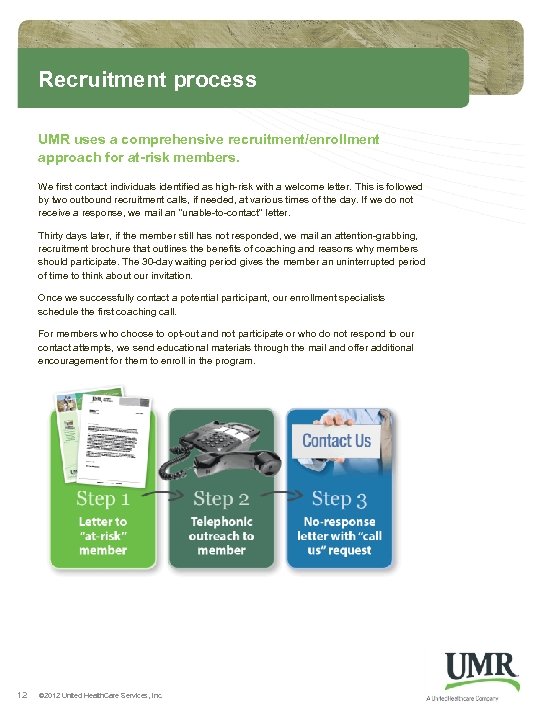 Recruitment process UMR uses a comprehensive recruitment/enrollment approach for at-risk members. We first contact individuals identified as high-risk with a welcome letter. This is followed by two outbound recruitment calls, if needed, at various times of the day. If we do not receive a response, we mail an “unable-to-contact” letter. Thirty days later, if the member still has not responded, we mail an attention-grabbing, recruitment brochure that outlines the benefits of coaching and reasons why members should participate. The 30 -day waiting period gives the member an uninterrupted period of time to think about our invitation. Once we successfully contact a potential participant, our enrollment specialists schedule the first coaching call. For members who choose to opt-out and not participate or who do not respond to our contact attempts, we send educational materials through the mail and offer additional encouragement for them to enroll in the program. 12 © 2012 United Health. Care Services, Inc.
Recruitment process UMR uses a comprehensive recruitment/enrollment approach for at-risk members. We first contact individuals identified as high-risk with a welcome letter. This is followed by two outbound recruitment calls, if needed, at various times of the day. If we do not receive a response, we mail an “unable-to-contact” letter. Thirty days later, if the member still has not responded, we mail an attention-grabbing, recruitment brochure that outlines the benefits of coaching and reasons why members should participate. The 30 -day waiting period gives the member an uninterrupted period of time to think about our invitation. Once we successfully contact a potential participant, our enrollment specialists schedule the first coaching call. For members who choose to opt-out and not participate or who do not respond to our contact attempts, we send educational materials through the mail and offer additional encouragement for them to enroll in the program. 12 © 2012 United Health. Care Services, Inc.
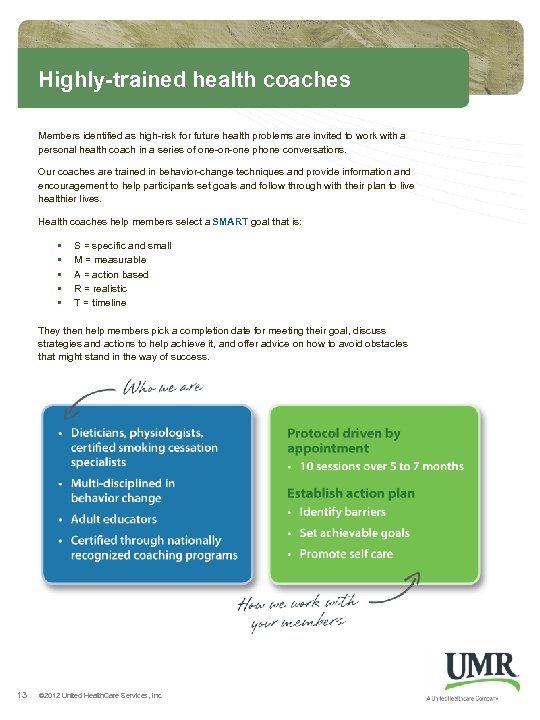 Highly-trained health coaches Members identified as high-risk for future health problems are invited to work with a personal health coach in a series of one-on-one phone conversations. Our coaches are trained in behavior-change techniques and provide information and encouragement to help participants set goals and follow through with their plan to live healthier lives. Health coaches help members select a SMART goal that is: • • • S = specific and small M = measurable A = action based R = realistic T = timeline They then help members pick a completion date for meeting their goal, discuss strategies and actions to help achieve it, and offer advice on how to avoid obstacles that might stand in the way of success. 13 © 2012 United Health. Care Services, Inc.
Highly-trained health coaches Members identified as high-risk for future health problems are invited to work with a personal health coach in a series of one-on-one phone conversations. Our coaches are trained in behavior-change techniques and provide information and encouragement to help participants set goals and follow through with their plan to live healthier lives. Health coaches help members select a SMART goal that is: • • • S = specific and small M = measurable A = action based R = realistic T = timeline They then help members pick a completion date for meeting their goal, discuss strategies and actions to help achieve it, and offer advice on how to avoid obstacles that might stand in the way of success. 13 © 2012 United Health. Care Services, Inc.
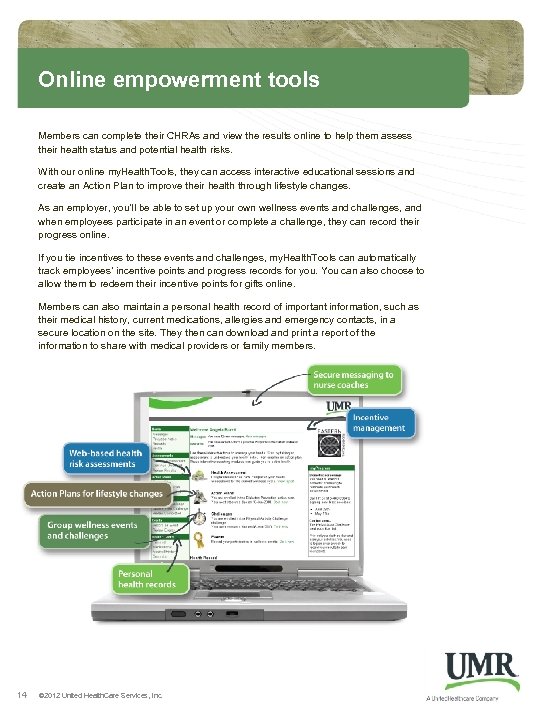 Online empowerment tools Members can complete their CHRAs and view the results online to help them assess their health status and potential health risks. With our online my. Health. Tools, they can access interactive educational sessions and create an Action Plan to improve their health through lifestyle changes. As an employer, you’ll be able to set up your own wellness events and challenges, and when employees participate in an event or complete a challenge, they can record their progress online. If you tie incentives to these events and challenges, my. Health. Tools can automatically track employees’ incentive points and progress records for you. You can also choose to allow them to redeem their incentive points for gifts online. Members can also maintain a personal health record of important information, such as their medical history, current medications, allergies and emergency contacts, in a secure location on the site. They then can download and print a report of the information to share with medical providers or family members. 14 © 2012 United Health. Care Services, Inc.
Online empowerment tools Members can complete their CHRAs and view the results online to help them assess their health status and potential health risks. With our online my. Health. Tools, they can access interactive educational sessions and create an Action Plan to improve their health through lifestyle changes. As an employer, you’ll be able to set up your own wellness events and challenges, and when employees participate in an event or complete a challenge, they can record their progress online. If you tie incentives to these events and challenges, my. Health. Tools can automatically track employees’ incentive points and progress records for you. You can also choose to allow them to redeem their incentive points for gifts online. Members can also maintain a personal health record of important information, such as their medical history, current medications, allergies and emergency contacts, in a secure location on the site. They then can download and print a report of the information to share with medical providers or family members. 14 © 2012 United Health. Care Services, Inc.
 Online action plans UMR’s my. Health. Tools include action plans that help members make healthy lifestyle choices and changes to their behavior. The interactive, online tutorials offer plans for a variety of lifestyle behaviors: • • • Healthy eating Stress management Exercise and activity Weight management Smoking cessation Diabetes prevention Heart disease prevention Depression Risky drinking Each action plan includes: • An assessment to help participants better understand the impact of their current lifestyle behaviors on their overall health • An interactive educational video • Weekly lessons to keep participants moving forward • Health Trackers – record-keeping logs for members to download and record their actions and see their progress from week to week 15 © 2012 United Health. Care Services, Inc.
Online action plans UMR’s my. Health. Tools include action plans that help members make healthy lifestyle choices and changes to their behavior. The interactive, online tutorials offer plans for a variety of lifestyle behaviors: • • • Healthy eating Stress management Exercise and activity Weight management Smoking cessation Diabetes prevention Heart disease prevention Depression Risky drinking Each action plan includes: • An assessment to help participants better understand the impact of their current lifestyle behaviors on their overall health • An interactive educational video • Weekly lessons to keep participants moving forward • Health Trackers – record-keeping logs for members to download and record their actions and see their progress from week to week 15 © 2012 United Health. Care Services, Inc.
 Worksite wellness If you are ready to engage and lead your employees in the pursuit of better health, UMR can help you establish a culture of wellness. Our worksite wellness program is designed to guide employers in making your work environment more supportive of behaviors such as healthy eating, physical activity, stress management and tobacco cessation. The goal is to improve the physical, mental, emotional and occupational well-being of your employees. UMR assigns worksite wellness consultants to help customers initiate and maintain results-oriented programming, starting with an evaluation of the steps they already have taken toward wellness. We then assist with identifying appropriate interventions, establishing desired objectives and measuring the results of these efforts. We also provide a worksite wellness toolkit with templates, sample documents and suggestions for crafting a customized wellness operating plan. UMR has developed several wellness programs for you to deliver to your employees. The ready-toimplement challenges encourage participants to begin or maintain physical activity, weight loss or healthy eating programs. A well workplace contributes to: Reduced absenteeism Lower disease risk Increased productivity Improved morale and retention Better cost control Enhanced quality of life Fewer injuries 16 © 2012 United Health. Care Services, Inc.
Worksite wellness If you are ready to engage and lead your employees in the pursuit of better health, UMR can help you establish a culture of wellness. Our worksite wellness program is designed to guide employers in making your work environment more supportive of behaviors such as healthy eating, physical activity, stress management and tobacco cessation. The goal is to improve the physical, mental, emotional and occupational well-being of your employees. UMR assigns worksite wellness consultants to help customers initiate and maintain results-oriented programming, starting with an evaluation of the steps they already have taken toward wellness. We then assist with identifying appropriate interventions, establishing desired objectives and measuring the results of these efforts. We also provide a worksite wellness toolkit with templates, sample documents and suggestions for crafting a customized wellness operating plan. UMR has developed several wellness programs for you to deliver to your employees. The ready-toimplement challenges encourage participants to begin or maintain physical activity, weight loss or healthy eating programs. A well workplace contributes to: Reduced absenteeism Lower disease risk Increased productivity Improved morale and retention Better cost control Enhanced quality of life Fewer injuries 16 © 2012 United Health. Care Services, Inc.
 Disease management UMR has found that these seven health conditions drive medical claims costs for employers: • • Asthma Chronic obstructive pulmonary disease (COPD) Congestive heart failure Coronary artery disease Depression (co-morbid condition) Diabetes Hypertension (high blood pressure) Identifying plan members and helping them manage their conditions provides the maximum value to you, while helping participants improve their well-being. The program also can mitigate indirect costs to you, such as absenteeism and reduced productivity. Our program uses the leading behavior change model to determine an individual’s current stage of readiness to change and how we can best guide the participant toward improved health. To maximize your short-term return on investment, we focus on those who are currently most ready to make a healthy change. Members with a chronic condition are automatically enrolled in the program, and those identified for one-on-one coaching are invited to participate through a combination of letters and phone calls. To help drive participation in the program, UMR offers customers new to disease management a $100 gift card incentive. It is given to eligible members who enroll in one-on-one coaching during an introductory time period. Lower-risk participants receive a free subscription to our quarterly newsletter and periodic communications about their condition and making healthy changes. All members can access Nurse. Line to talk with a nurse about any health-related questions, 24 hours a day, seven days a week. 17 © 2012 United Health. Care Services, Inc.
Disease management UMR has found that these seven health conditions drive medical claims costs for employers: • • Asthma Chronic obstructive pulmonary disease (COPD) Congestive heart failure Coronary artery disease Depression (co-morbid condition) Diabetes Hypertension (high blood pressure) Identifying plan members and helping them manage their conditions provides the maximum value to you, while helping participants improve their well-being. The program also can mitigate indirect costs to you, such as absenteeism and reduced productivity. Our program uses the leading behavior change model to determine an individual’s current stage of readiness to change and how we can best guide the participant toward improved health. To maximize your short-term return on investment, we focus on those who are currently most ready to make a healthy change. Members with a chronic condition are automatically enrolled in the program, and those identified for one-on-one coaching are invited to participate through a combination of letters and phone calls. To help drive participation in the program, UMR offers customers new to disease management a $100 gift card incentive. It is given to eligible members who enroll in one-on-one coaching during an introductory time period. Lower-risk participants receive a free subscription to our quarterly newsletter and periodic communications about their condition and making healthy changes. All members can access Nurse. Line to talk with a nurse about any health-related questions, 24 hours a day, seven days a week. 17 © 2012 United Health. Care Services, Inc.
 Targeted member messaging UMR believes that members — especially those with a chronic condition — can make improvements to their health with help from timely, personalized, health care recommendations. Our targeted member messages, called Healthe. Notes, offer members advice for improving their health while making the most of their health care dollars. Healthe. Notes alert members to gaps in care, or health opportunities, identified through analysis of medical and pharmacy claims information. Health opportunities are developed from widely accepted medical guidelines and serve to: • Remind members to schedule recommended health screenings, schedule doctor visits and refill medications • Provide members a starting point for conversations with their doctor, who might recommend following the suggested opportunities • Offer members suggestions on how to save money on prescription medications Improve health Lower costs Engage members in health discussions Encourage prescribed Rx use 18 © 2012 United Health. Care Services, Inc.
Targeted member messaging UMR believes that members — especially those with a chronic condition — can make improvements to their health with help from timely, personalized, health care recommendations. Our targeted member messages, called Healthe. Notes, offer members advice for improving their health while making the most of their health care dollars. Healthe. Notes alert members to gaps in care, or health opportunities, identified through analysis of medical and pharmacy claims information. Health opportunities are developed from widely accepted medical guidelines and serve to: • Remind members to schedule recommended health screenings, schedule doctor visits and refill medications • Provide members a starting point for conversations with their doctor, who might recommend following the suggested opportunities • Offer members suggestions on how to save money on prescription medications Improve health Lower costs Engage members in health discussions Encourage prescribed Rx use 18 © 2012 United Health. Care Services, Inc.
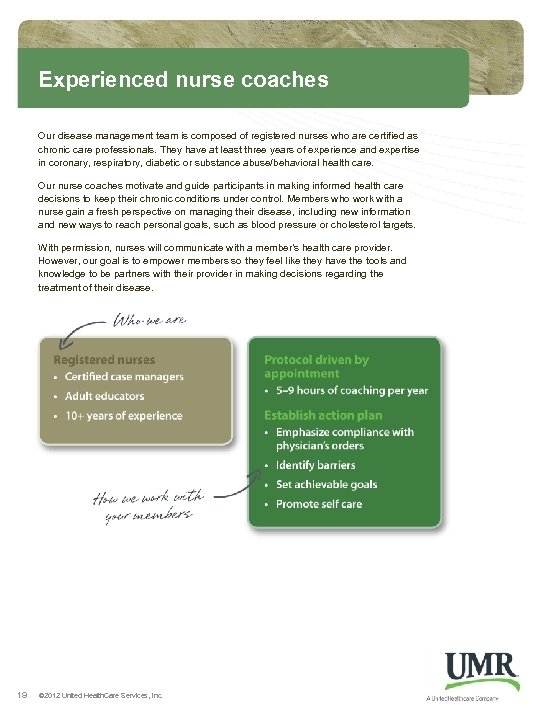 Experienced nurse coaches Our disease management team is composed of registered nurses who are certified as chronic care professionals. They have at least three years of experience and expertise in coronary, respiratory, diabetic or substance abuse/behavioral health care. Our nurse coaches motivate and guide participants in making informed health care decisions to keep their chronic conditions under control. Members who work with a nurse gain a fresh perspective on managing their disease, including new information and new ways to reach personal goals, such as blood pressure or cholesterol targets. With permission, nurses will communicate with a member’s health care provider. However, our goal is to empower members so they feel like they have the tools and knowledge to be partners with their provider in making decisions regarding the treatment of their disease. 19 © 2012 United Health. Care Services, Inc.
Experienced nurse coaches Our disease management team is composed of registered nurses who are certified as chronic care professionals. They have at least three years of experience and expertise in coronary, respiratory, diabetic or substance abuse/behavioral health care. Our nurse coaches motivate and guide participants in making informed health care decisions to keep their chronic conditions under control. Members who work with a nurse gain a fresh perspective on managing their disease, including new information and new ways to reach personal goals, such as blood pressure or cholesterol targets. With permission, nurses will communicate with a member’s health care provider. However, our goal is to empower members so they feel like they have the tools and knowledge to be partners with their provider in making decisions regarding the treatment of their disease. 19 © 2012 United Health. Care Services, Inc.
 Tiers of participation Coaching strategies, intervention and contact with members are based on the participant’s risk rating. The highest-risk candidates receive the most personalized and intensive outreach, while lower-risk individuals are supported by their CHRA reports, access to online tools and quarterly newsletters mailed to all participants. We divide participants into five categories: • • TIER 1 Accepted: These are high-risk members who have been successfully contacted and enrolled in the disease management program and have agreed to engage in one-on-one counseling. • TIER 2 Non-engaged: This group is composed of high-risk members who decline participation in one-on-one counseling with a nurse case manager. They remain eligible for one-on-one counseling and can enroll in the counseling process at any time. They are invited to enroll annually. • TIER 3 Maintenance: These members have finished their coaching program in Tier 1 and have graduated to a lower level of risk where they demonstrate increased awareness of their condition and continue to manage it, avoiding relapse. • 20 Recruitment: This group is made up of at-risk members who have not yet been assigned a tier. They receive an initial invitation letter, followed by recruitment calls, and are eligible for newsletters and online information. TIER 4 Self-directed: Members in this group have a chronic condition but are considered lower risk, successfully managing their condition day-to-day. They have access to program benefits such as educational materials, quarterly newsletters and Web-based support tools, but they are not targeted for one-onone coaching with a registered nurse case manager. © 2012 United Health. Care Services, Inc.
Tiers of participation Coaching strategies, intervention and contact with members are based on the participant’s risk rating. The highest-risk candidates receive the most personalized and intensive outreach, while lower-risk individuals are supported by their CHRA reports, access to online tools and quarterly newsletters mailed to all participants. We divide participants into five categories: • • TIER 1 Accepted: These are high-risk members who have been successfully contacted and enrolled in the disease management program and have agreed to engage in one-on-one counseling. • TIER 2 Non-engaged: This group is composed of high-risk members who decline participation in one-on-one counseling with a nurse case manager. They remain eligible for one-on-one counseling and can enroll in the counseling process at any time. They are invited to enroll annually. • TIER 3 Maintenance: These members have finished their coaching program in Tier 1 and have graduated to a lower level of risk where they demonstrate increased awareness of their condition and continue to manage it, avoiding relapse. • 20 Recruitment: This group is made up of at-risk members who have not yet been assigned a tier. They receive an initial invitation letter, followed by recruitment calls, and are eligible for newsletters and online information. TIER 4 Self-directed: Members in this group have a chronic condition but are considered lower risk, successfully managing their condition day-to-day. They have access to program benefits such as educational materials, quarterly newsletters and Web-based support tools, but they are not targeted for one-onone coaching with a registered nurse case manager. © 2012 United Health. Care Services, Inc.
 Utilization management and case management UMR monitors all cases from initial notification through discharge. Our goal is to intervene as early as possible to ensure cases don’t deviate from the expected treatment plan and become complicated and costly for your employees. Cases that might be deemed “high-risk” are forwarded to our case management or disease management programs for further review. We maintain an up-to-date list of inpatient and outpatient procedures that require notification, and we can customize our list based on your specific requests. We measure utilization management savings by comparing the estimated cost of the care requested to the cost of care authorized. In most instances, our utilization management program customers see a 2 to 1 return on investment (ROI) approximately one year after the completion of program implementation. UMR case management targets complicated cases to achieve better medical outcomes for plan members and greater cost savings to you. The key to our success is the case manager’s ability to identify, coordinate and negotiate alternative treatment plans and related costs. • • • Our case management team is made up of licensed, registered nurses 95 percent of our nurses have certified case manager (CCM) credentials All must have three years of acute care clinical experience and expertise in at least one specialized field Our system identifies case management opportunities using an automated trigger list that can be customized at your request. The list is based on ICD, CPT and dollar threshold criteria or when a member’s inpatient length of stay reaches five days. Each case is unique and handled according to the specific needs of the member. On average, cases remain open for four months. UMR measures the success of its case management program by the following criteria: • • 21 Improved clinical efficacy Reasonable medical action plan Coordination with providers and family Clinically eligible for coverage Customer satisfaction correspondence Coordination with stop loss vendors Return on investment © 2012 United Health. Care Services, Inc.
Utilization management and case management UMR monitors all cases from initial notification through discharge. Our goal is to intervene as early as possible to ensure cases don’t deviate from the expected treatment plan and become complicated and costly for your employees. Cases that might be deemed “high-risk” are forwarded to our case management or disease management programs for further review. We maintain an up-to-date list of inpatient and outpatient procedures that require notification, and we can customize our list based on your specific requests. We measure utilization management savings by comparing the estimated cost of the care requested to the cost of care authorized. In most instances, our utilization management program customers see a 2 to 1 return on investment (ROI) approximately one year after the completion of program implementation. UMR case management targets complicated cases to achieve better medical outcomes for plan members and greater cost savings to you. The key to our success is the case manager’s ability to identify, coordinate and negotiate alternative treatment plans and related costs. • • • Our case management team is made up of licensed, registered nurses 95 percent of our nurses have certified case manager (CCM) credentials All must have three years of acute care clinical experience and expertise in at least one specialized field Our system identifies case management opportunities using an automated trigger list that can be customized at your request. The list is based on ICD, CPT and dollar threshold criteria or when a member’s inpatient length of stay reaches five days. Each case is unique and handled according to the specific needs of the member. On average, cases remain open for four months. UMR measures the success of its case management program by the following criteria: • • 21 Improved clinical efficacy Reasonable medical action plan Coordination with providers and family Clinically eligible for coverage Customer satisfaction correspondence Coordination with stop loss vendors Return on investment © 2012 United Health. Care Services, Inc.
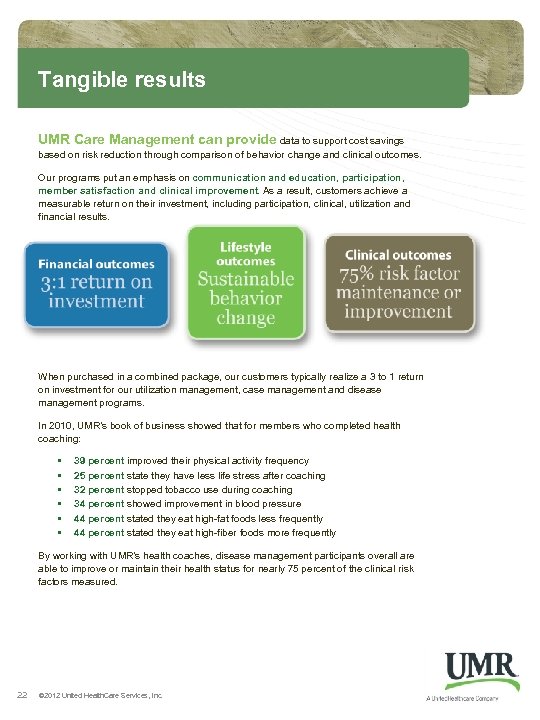 Tangible results UMR Care Management can provide data to support cost savings based on risk reduction through comparison of behavior change and clinical outcomes. Our programs put an emphasis on communication and education, participation, member satisfaction and clinical improvement. As a result, customers achieve a measurable return on their investment, including participation, clinical, utilization and financial results. When purchased in a combined package, our customers typically realize a 3 to 1 return on investment for our utilization management, case management and disease management programs. In 2010, UMR’s book of business showed that for members who completed health coaching: • • • 39 percent improved their physical activity frequency 25 percent state they have less life stress after coaching 32 percent stopped tobacco use during coaching 34 percent showed improvement in blood pressure 44 percent stated they eat high-fat foods less frequently 44 percent stated they eat high-fiber foods more frequently By working with UMR’s health coaches, disease management participants overall are able to improve or maintain their health status for nearly 75 percent of the clinical risk factors measured. 22 © 2012 United Health. Care Services, Inc.
Tangible results UMR Care Management can provide data to support cost savings based on risk reduction through comparison of behavior change and clinical outcomes. Our programs put an emphasis on communication and education, participation, member satisfaction and clinical improvement. As a result, customers achieve a measurable return on their investment, including participation, clinical, utilization and financial results. When purchased in a combined package, our customers typically realize a 3 to 1 return on investment for our utilization management, case management and disease management programs. In 2010, UMR’s book of business showed that for members who completed health coaching: • • • 39 percent improved their physical activity frequency 25 percent state they have less life stress after coaching 32 percent stopped tobacco use during coaching 34 percent showed improvement in blood pressure 44 percent stated they eat high-fat foods less frequently 44 percent stated they eat high-fiber foods more frequently By working with UMR’s health coaches, disease management participants overall are able to improve or maintain their health status for nearly 75 percent of the clinical risk factors measured. 22 © 2012 United Health. Care Services, Inc.
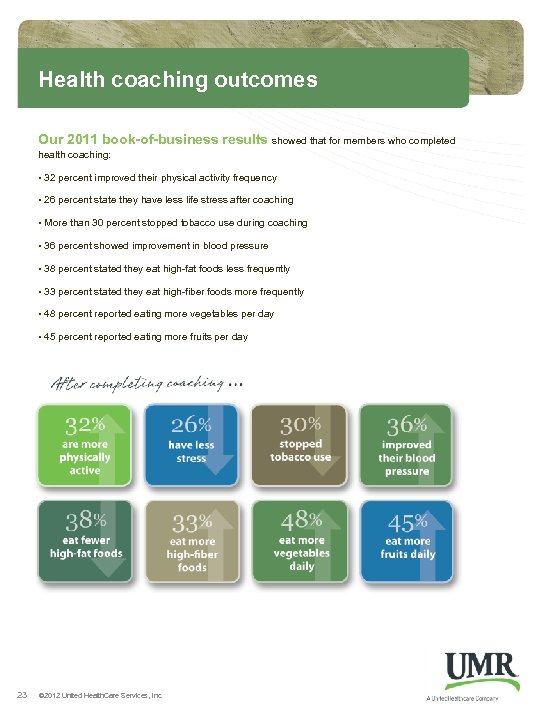 Health coaching outcomes Our 2011 book-of-business results showed that for members who completed health coaching: • 32 percent improved their physical activity frequency • 26 percent state they have less life stress after coaching • More than 30 percent stopped tobacco use during coaching • 36 percent showed improvement in blood pressure • 38 percent stated they eat high-fat foods less frequently • 33 percent stated they eat high-fiber foods more frequently • 48 percent reported eating more vegetables per day • 45 percent reported eating more fruits per day 23 © 2012 United Health. Care Services, Inc.
Health coaching outcomes Our 2011 book-of-business results showed that for members who completed health coaching: • 32 percent improved their physical activity frequency • 26 percent state they have less life stress after coaching • More than 30 percent stopped tobacco use during coaching • 36 percent showed improvement in blood pressure • 38 percent stated they eat high-fat foods less frequently • 33 percent stated they eat high-fiber foods more frequently • 48 percent reported eating more vegetables per day • 45 percent reported eating more fruits per day 23 © 2012 United Health. Care Services, Inc.
 Wellness improvement targets UMR can help you implement an incentive strategy that rewards year-to-year improvements to achieve long-term results. Our wellness improvement targets show members which of their health indicators place them at risk for a chronic disease and give members both financial and healthdriven motivations to improve their well-being. We can assist you in determining the type and level of incentive that best fits your employee population. To qualify for the incentive, a participant must maintain or improve his or her wellness score and meet a specific number of improvement targets based upon risk level. The higher the risk level, the more measures the participant is required to improve: As you consider whether this program is right for you, remember that this strategy must be an ongoing, long-term commitment with meaningful incentives to be successful. 24 © 2012 United Health. Care Services, Inc.
Wellness improvement targets UMR can help you implement an incentive strategy that rewards year-to-year improvements to achieve long-term results. Our wellness improvement targets show members which of their health indicators place them at risk for a chronic disease and give members both financial and healthdriven motivations to improve their well-being. We can assist you in determining the type and level of incentive that best fits your employee population. To qualify for the incentive, a participant must maintain or improve his or her wellness score and meet a specific number of improvement targets based upon risk level. The higher the risk level, the more measures the participant is required to improve: As you consider whether this program is right for you, remember that this strategy must be an ongoing, long-term commitment with meaningful incentives to be successful. 24 © 2012 United Health. Care Services, Inc.
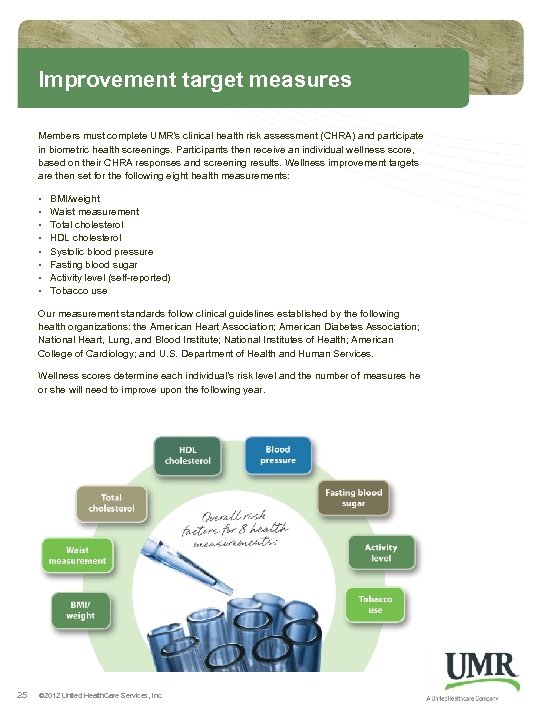 Improvement target measures Members must complete UMR’s clinical health risk assessment (CHRA) and participate in biometric health screenings. Participants then receive an individual wellness score, based on their CHRA responses and screening results. Wellness improvement targets are then set for the following eight health measurements: • • BMI/weight Waist measurement Total cholesterol HDL cholesterol Systolic blood pressure Fasting blood sugar Activity level (self-reported) Tobacco use Our measurement standards follow clinical guidelines established by the following health organizations: the American Heart Association; American Diabetes Association; National Heart, Lung, and Blood Institute; National Institutes of Health; American College of Cardiology; and U. S. Department of Health and Human Services. Wellness scores determine each individual’s risk level and the number of measures he or she will need to improve upon the following year. 25 © 2012 United Health. Care Services, Inc.
Improvement target measures Members must complete UMR’s clinical health risk assessment (CHRA) and participate in biometric health screenings. Participants then receive an individual wellness score, based on their CHRA responses and screening results. Wellness improvement targets are then set for the following eight health measurements: • • BMI/weight Waist measurement Total cholesterol HDL cholesterol Systolic blood pressure Fasting blood sugar Activity level (self-reported) Tobacco use Our measurement standards follow clinical guidelines established by the following health organizations: the American Heart Association; American Diabetes Association; National Heart, Lung, and Blood Institute; National Institutes of Health; American College of Cardiology; and U. S. Department of Health and Human Services. Wellness scores determine each individual’s risk level and the number of measures he or she will need to improve upon the following year. 25 © 2012 United Health. Care Services, Inc.
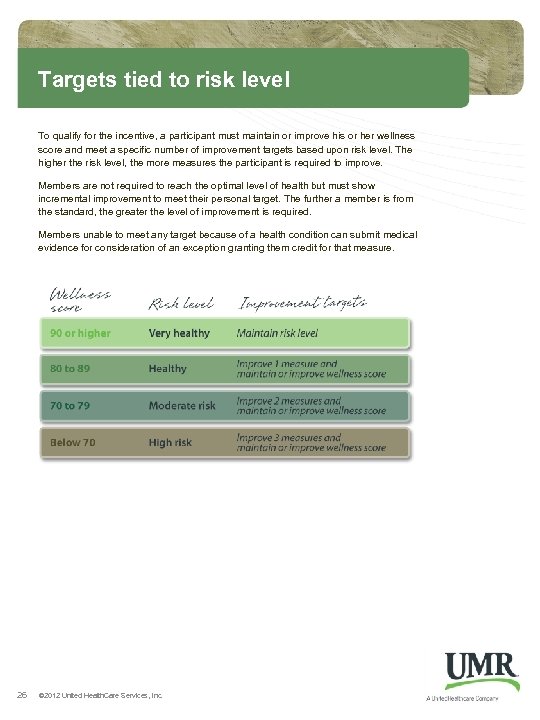 Targets tied to risk level To qualify for the incentive, a participant must maintain or improve his or her wellness score and meet a specific number of improvement targets based upon risk level. The higher the risk level, the more measures the participant is required to improve. Members are not required to reach the optimal level of health but must show incremental improvement to meet their personal target. The further a member is from the standard, the greater the level of improvement is required. Members unable to meet any target because of a health condition can submit medical evidence for consideration of an exception granting them credit for that measure. 26 © 2012 United Health. Care Services, Inc.
Targets tied to risk level To qualify for the incentive, a participant must maintain or improve his or her wellness score and meet a specific number of improvement targets based upon risk level. The higher the risk level, the more measures the participant is required to improve. Members are not required to reach the optimal level of health but must show incremental improvement to meet their personal target. The further a member is from the standard, the greater the level of improvement is required. Members unable to meet any target because of a health condition can submit medical evidence for consideration of an exception granting them credit for that measure. 26 © 2012 United Health. Care Services, Inc.
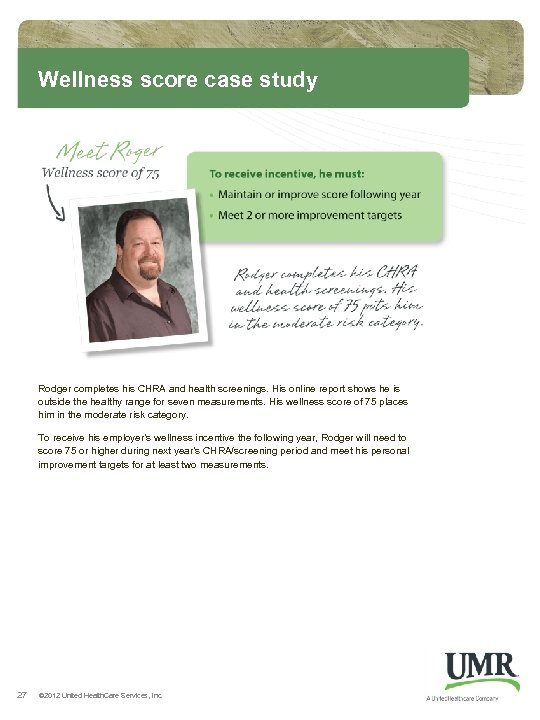 Wellness score case study Rodger completes his CHRA and health screenings. His online report shows he is outside the healthy range for seven measurements. His wellness score of 75 places him in the moderate risk category. To receive his employer’s wellness incentive the following year, Rodger will need to score 75 or higher during next year’s CHRA/screening period and meet his personal improvement targets for at least two measurements. 27 © 2012 United Health. Care Services, Inc.
Wellness score case study Rodger completes his CHRA and health screenings. His online report shows he is outside the healthy range for seven measurements. His wellness score of 75 places him in the moderate risk category. To receive his employer’s wellness incentive the following year, Rodger will need to score 75 or higher during next year’s CHRA/screening period and meet his personal improvement targets for at least two measurements. 27 © 2012 United Health. Care Services, Inc.
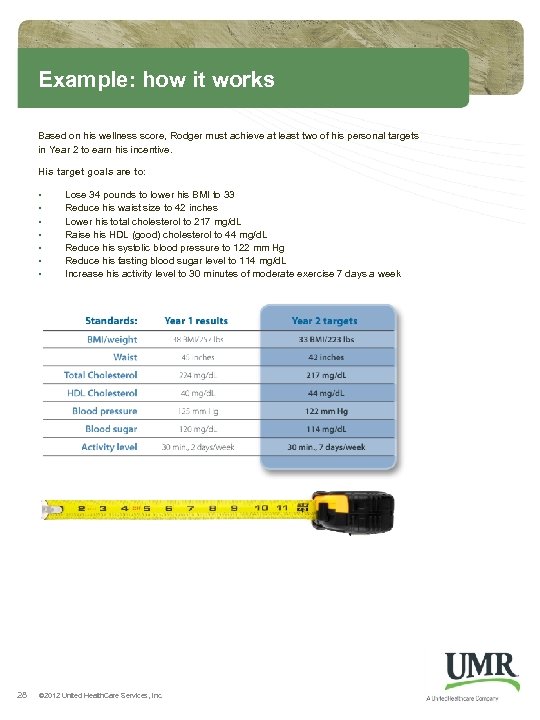 Example: how it works Based on his wellness score, Rodger must achieve at least two of his personal targets in Year 2 to earn his incentive. His target goals are to: • • 28 Lose 34 pounds to lower his BMI to 33 Reduce his waist size to 42 inches Lower his total cholesterol to 217 mg/d. L Raise his HDL (good) cholesterol to 44 mg/d. L Reduce his systolic blood pressure to 122 mm Hg Reduce his fasting blood sugar level to 114 mg/d. L Increase his activity level to 30 minutes of moderate exercise 7 days a week © 2012 United Health. Care Services, Inc.
Example: how it works Based on his wellness score, Rodger must achieve at least two of his personal targets in Year 2 to earn his incentive. His target goals are to: • • 28 Lose 34 pounds to lower his BMI to 33 Reduce his waist size to 42 inches Lower his total cholesterol to 217 mg/d. L Raise his HDL (good) cholesterol to 44 mg/d. L Reduce his systolic blood pressure to 122 mm Hg Reduce his fasting blood sugar level to 114 mg/d. L Increase his activity level to 30 minutes of moderate exercise 7 days a week © 2012 United Health. Care Services, Inc.
 Coaching success: hypertension Frank found out he had hypertension when he was 40 years old but lacked the knowledge and motivation to improve his condition. That changes after Frank completes his online clinical health risk assessment and participates in a biometric screening at work. His blood pressure of 178/94 puts him at risk for heart disease and stroke, and his body mass index of 28 tells him he is overweight. He receives a recruitment call from UMR Disease Management and learns that working with a personal health coach could help. 29 © 2012 United Health. Care Services, Inc.
Coaching success: hypertension Frank found out he had hypertension when he was 40 years old but lacked the knowledge and motivation to improve his condition. That changes after Frank completes his online clinical health risk assessment and participates in a biometric screening at work. His blood pressure of 178/94 puts him at risk for heart disease and stroke, and his body mass index of 28 tells him he is overweight. He receives a recruitment call from UMR Disease Management and learns that working with a personal health coach could help. 29 © 2012 United Health. Care Services, Inc.
 Coaching success: hypertension Frank’s doctor recommends he take a second blood pressure medicine and adopt a low-sodium diet. Frank tells his health coach that he know he should watch less television and be more active. He completes a sodium self-screening tool and finds he is eating too much salt. Frank’s coach helps him set realistic goals. He agrees to eat fresh vegetables instead of potato chips at lunch and to begin walking more and ride his bike with his grandson several times a week. With his coach’s support, Frank has lost 10 pounds in six months and lowered his blood pressure to 132/74. 30 © 2012 United Health. Care Services, Inc.
Coaching success: hypertension Frank’s doctor recommends he take a second blood pressure medicine and adopt a low-sodium diet. Frank tells his health coach that he know he should watch less television and be more active. He completes a sodium self-screening tool and finds he is eating too much salt. Frank’s coach helps him set realistic goals. He agrees to eat fresh vegetables instead of potato chips at lunch and to begin walking more and ride his bike with his grandson several times a week. With his coach’s support, Frank has lost 10 pounds in six months and lowered his blood pressure to 132/74. 30 © 2012 United Health. Care Services, Inc.
 Coaching success: diabetes Preventive care is covered 100 percent by Betty’s employer. She receives her annual physical and learns she has type 2 diabetes. Betty weighs 200 pounds and is considered obese. Her blood-sugar level of 8. 2 is high, so her doctor prescribes diabetes medicine. After filling her prescription, Betty receives a recruitment call from UMR Disease Management. She learns that a personal health coach could help her manage her condition through medication, weight loss and increased physical activity. 31 © 2012 United Health. Care Services, Inc.
Coaching success: diabetes Preventive care is covered 100 percent by Betty’s employer. She receives her annual physical and learns she has type 2 diabetes. Betty weighs 200 pounds and is considered obese. Her blood-sugar level of 8. 2 is high, so her doctor prescribes diabetes medicine. After filling her prescription, Betty receives a recruitment call from UMR Disease Management. She learns that a personal health coach could help her manage her condition through medication, weight loss and increased physical activity. 31 © 2012 United Health. Care Services, Inc.
 Coaching success: diabetes Betty talks to her coach online and by phone, and they discuss the barriers and benefits of making healthy changes. Her nurse tells her about recommended diabetes care and how to plan healthy meals. Betty learns the importance of preventive care, including annual eye exams and dental check-ups. She begins to read food labels when grocery shopping and starts a journal to track her food intake. This helps her make healthier choices and reduce her portion sizes. She then adds walking to her routine. Betty continues to discuss her challenges and celebrate her accomplishments with her coach. She has lost 12 pounds in three months and lowered her blood-sugar level to 6. 2 – well within recommended guidelines. 32 © 2012 United Health. Care Services, Inc.
Coaching success: diabetes Betty talks to her coach online and by phone, and they discuss the barriers and benefits of making healthy changes. Her nurse tells her about recommended diabetes care and how to plan healthy meals. Betty learns the importance of preventive care, including annual eye exams and dental check-ups. She begins to read food labels when grocery shopping and starts a journal to track her food intake. This helps her make healthier choices and reduce her portion sizes. She then adds walking to her routine. Betty continues to discuss her challenges and celebrate her accomplishments with her coach. She has lost 12 pounds in three months and lowered her blood-sugar level to 6. 2 – well within recommended guidelines. 32 © 2012 United Health. Care Services, Inc.
 Coaching success: child asthma Andrea has received treatment for asthma for several years and went to the emergency room twice recently because of her asthma. Andrea’s mom, Cathy, receives a recruitment call from UMR Disease Management and learns that a personal health coach can work with her to help manage Andrea’s condition. Cathy agrees to enroll her daughter in the program. Coaching is available at no cost to the family. 33 © 2012 United Health. Care Services, Inc.
Coaching success: child asthma Andrea has received treatment for asthma for several years and went to the emergency room twice recently because of her asthma. Andrea’s mom, Cathy, receives a recruitment call from UMR Disease Management and learns that a personal health coach can work with her to help manage Andrea’s condition. Cathy agrees to enroll her daughter in the program. Coaching is available at no cost to the family. 33 © 2012 United Health. Care Services, Inc.
 Coaching success: child asthma Cathy speaks to a health coach and says her goal is to bring Andrea’s symptoms under control so that she doesn’t miss school and can participate in sports. Andrea’s asthma has interfered with playing soccer and singing in the choir. She also often has symptoms such as coughing at night. Cathy tells her coach that Andrea has not taken her asthma medicine as directed. The coach helps Cathy understand Andrea’s condition. Cathy agrees to follow the doctor’s treatment plan and to share Andrea’s asthma action plan with her school. Cathy gives her daughter her preventive medication as directed. Andrea has fewer symptoms at night and is able to play soccer without needing her rescue inhaler. She goes an entire semester without missing school and makes no trips to the ER. 34 © 2012 United Health. Care Services, Inc.
Coaching success: child asthma Cathy speaks to a health coach and says her goal is to bring Andrea’s symptoms under control so that she doesn’t miss school and can participate in sports. Andrea’s asthma has interfered with playing soccer and singing in the choir. She also often has symptoms such as coughing at night. Cathy tells her coach that Andrea has not taken her asthma medicine as directed. The coach helps Cathy understand Andrea’s condition. Cathy agrees to follow the doctor’s treatment plan and to share Andrea’s asthma action plan with her school. Cathy gives her daughter her preventive medication as directed. Andrea has fewer symptoms at night and is able to play soccer without needing her rescue inhaler. She goes an entire semester without missing school and makes no trips to the ER. 34 © 2012 United Health. Care Services, Inc.
 Case management success story Helen has a history of chronic obstructive pulmonary disease (COPD), high blood pressure, high cholesterol and depression. She enters UMR’s case management program after being admitted to the intensive care unit with shortness of breath, weakness and dizziness. After her admission, she becomes unresponsive, receives a blood transfusion and is placed on a ventilator to help her breathe. 35 © 2012 United Health. Care Services, Inc.
Case management success story Helen has a history of chronic obstructive pulmonary disease (COPD), high blood pressure, high cholesterol and depression. She enters UMR’s case management program after being admitted to the intensive care unit with shortness of breath, weakness and dizziness. After her admission, she becomes unresponsive, receives a blood transfusion and is placed on a ventilator to help her breathe. 35 © 2012 United Health. Care Services, Inc.
 Case management success story Helen’s husband, Steve, works with a case management nurse to coordinate his wife’s care. The registered nurse explains Helen’s plan of treatment and answers Steve’s questions about the family’s health care benefits. When her condition is stable, Helen is transferred to a long-term, acute care facility. Doctors there discover a part of Helen’s bowel is not working properly and give her intravenous fluids to provide the nutrition she needs. After her discharge, Helen continues to receive oxygen treatment to help her breathe and has home care visits from occupational, physical and skilled nurses. The UMR care management nurse helps Steve understand his wife’s day-to-day care, and he ensures Helen keeps her doctor appointments and sticks to her treatment plan. 36 © 2012 United Health. Care Services, Inc.
Case management success story Helen’s husband, Steve, works with a case management nurse to coordinate his wife’s care. The registered nurse explains Helen’s plan of treatment and answers Steve’s questions about the family’s health care benefits. When her condition is stable, Helen is transferred to a long-term, acute care facility. Doctors there discover a part of Helen’s bowel is not working properly and give her intravenous fluids to provide the nutrition she needs. After her discharge, Helen continues to receive oxygen treatment to help her breathe and has home care visits from occupational, physical and skilled nurses. The UMR care management nurse helps Steve understand his wife’s day-to-day care, and he ensures Helen keeps her doctor appointments and sticks to her treatment plan. 36 © 2012 United Health. Care Services, Inc.
 Tobacco cessation success story Tom started smoking about 35 years ago and now smokes about 15 cigarettes a day. He has tried to quit 15 to 20 times before but always took up smoking again. Tom decides to try again and learns working with a UMR tobacco cessation specialist could help. He enrolls in the coaching program and chooses to try nicotine replacement patches to overcome his cravings. He tells his personal coach he is motivated to quit because he knows people who have developed chronic lung disease, the price of cigarettes is becoming too expensive, and his workplace is going tobacco-free. 37 © 2012 United Health. Care Services, Inc.
Tobacco cessation success story Tom started smoking about 35 years ago and now smokes about 15 cigarettes a day. He has tried to quit 15 to 20 times before but always took up smoking again. Tom decides to try again and learns working with a UMR tobacco cessation specialist could help. He enrolls in the coaching program and chooses to try nicotine replacement patches to overcome his cravings. He tells his personal coach he is motivated to quit because he knows people who have developed chronic lung disease, the price of cigarettes is becoming too expensive, and his workplace is going tobacco-free. 37 © 2012 United Health. Care Services, Inc.
 Tobacco cessation success story Tom’s coach suggests strategies for achieving his goal, including evening walks to take his mind off smoking and talking to himself while driving to work. Tom also talks to a co-worker who recently quit about how much more money they have now that they no longer buy cigarettes. Tom has remained tobacco-free for six months and now walks about two miles a day. He says coaching helped him recognize his triggers, and the nicotine patches helped control his cravings. He feels healthier than ever and is proud to have quit after so many failed attempts. 38 © 2012 United Health. Care Services, Inc. UM 0901 1012
Tobacco cessation success story Tom’s coach suggests strategies for achieving his goal, including evening walks to take his mind off smoking and talking to himself while driving to work. Tom also talks to a co-worker who recently quit about how much more money they have now that they no longer buy cigarettes. Tom has remained tobacco-free for six months and now walks about two miles a day. He says coaching helped him recognize his triggers, and the nicotine patches helped control his cravings. He feels healthier than ever and is proud to have quit after so many failed attempts. 38 © 2012 United Health. Care Services, Inc. UM 0901 1012


