75448a7fe987d1eacfc8c6013125de92.ppt
- Количество слайдов: 68
Tick-Borne Diseases Stephen J. Gluckman, M. D.
Tick-Borne Diseases n n Lyme Disease Babesiosis Ehrlichiosis “Tick Typhus” n n Rocky Mountain Spotted Fever African Tick Typhus n n n Tularemia Relapsing fever Powassan Tick Paralysis STARI
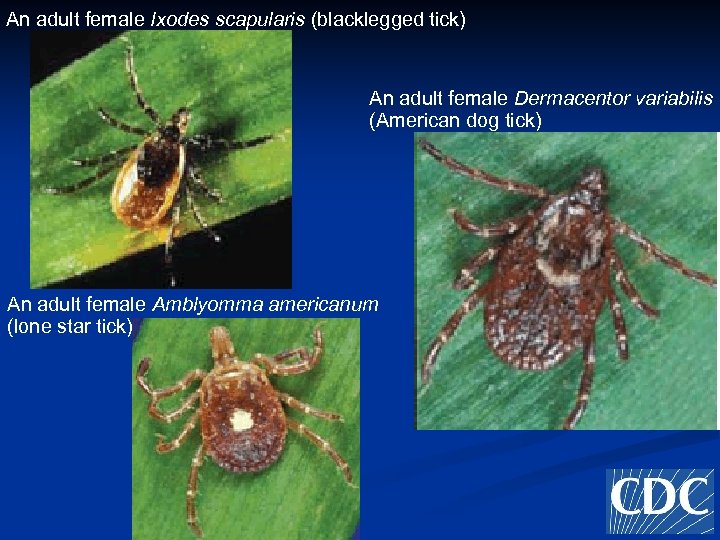
An adult female Ixodes scapularis (blacklegged tick) An adult female Dermacentor variabilis (American dog tick) An adult female Amblyomma americanum (lone star tick)

Lyme Disease Clinical Presentations A few things to clarify n n Erythema migrans Carditis n n n Neurological n n n Transient heart block Myocarditis VII CN palsy Aseptic meningitis Radiculoneuritis Lyme Encephalopathy Rheumatologic n Acute pauci-articular arthritis
Where Do You See Lyme Disease? Throughout the world
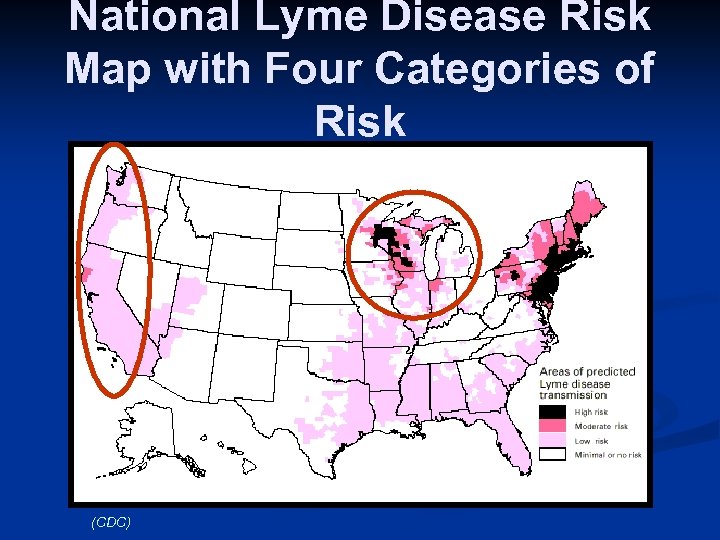
National Lyme Disease Risk Map with Four Categories of Risk (CDC)
Borrelia Burgdorferi B. burgdorferi is not from Mars B. Burgdorferi is not from another dimension B. Burgdorferi is just another bug
How Big is the Ixodes Tick? 1 -2 mm

Ixodes Ticks
Diagnosing Erythema Migrans ANY LARGE RED PATCH WITHOUT ANOTHER EXPLANATION IS ERYTHEMA MIGRANS


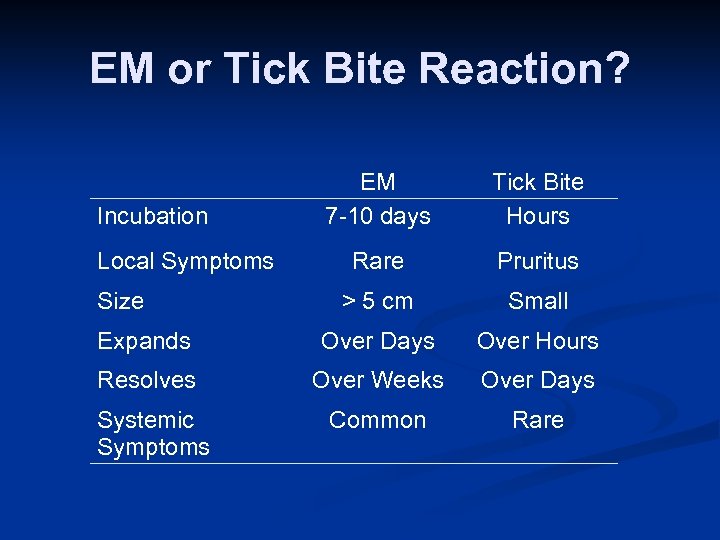
EM or Tick Bite Reaction? EM 7 -10 days Tick Bite Hours Rare Pruritus > 5 cm Small Expands Over Days Over Hours Resolves Over Weeks Over Days Common Rare Incubation Local Symptoms Size Systemic Symptoms
Erythema Migrans n Things to remember It is a clinical diagnosis, not a laboratory diagnosis n It is NEVER an emergency n “Target” lesion only occurs in 30% n Any big red patch is EM unless you have another explanation
Lyme Disease and VII CN Palsy n Differential Diagnosis HSV (was idiopathic) n HIV n Herpes Zoster n Local Infection/Trauma/Tumor n Sarcoidosis n Lyme n More likely with: preceding or present erythema migrans n
Lyme Disease and VII CN Palsy n Should you treat empirically? Tick time of year n Potential tick exposure n Bilateral n n “Diagnosis” n n Lyme Serology Lumbar Puncture?
Lyme Radiculoneuropathy n Differential Diagnosis Diabetes n Herpes zoster (sine herpete) n Herniated disc n Collapsed Vertebral body n Syphilis n
Case n n n 45 year old who has had several years of “low grade” fevers, painful lymph nodes, scratchy throat, and mental cloudiness He has been treated with oral doxycycline, azithromycin, and paromomycin. He has also been treated with three courses of IV ceftriaxone totaling 5 months n n He has had line related of Staphylococcus aureus bacteremia and ceftriaxone induced acute cholecystitis Is this resistant neuroborreliosis?
LYME ENECEPHALOPATHY n TO DIAGNOSE NEED BOTH Objective evidence of neurological disease n Objective evidence of B. burgdorferi in the CNS n n Lack of response related to: Incorrect diagnosis n Impatience n Permanent damage n
When Should One Think of Lyme Arthritis? n n n Monoarticular or pauciarticular Typically knee Differential Diagnosis: septic, crystal, rheumatoid, Reiter’s Class II fluid Arthralgias can be part of early Lyme Disease, but they are usually associated with EM and do not become chronic
Major Clinical Error n Chronic fatigue, chronic diffuse aching, recurrent sore throats, lymphadynia, and “low grade” fevers are not symptoms of active Lyme disease.
Lyme Serology n Misunderstandings about the use of serological testing for Lyme disease is the primary reason for the misunderstanding of this relatively uncomplicated infectious disease. “Real” Lyme disease is generally easy to diagnose and treat n Diseases misdiagnosed as Lyme disease are not n
There is NO TEST for Lyme Disease
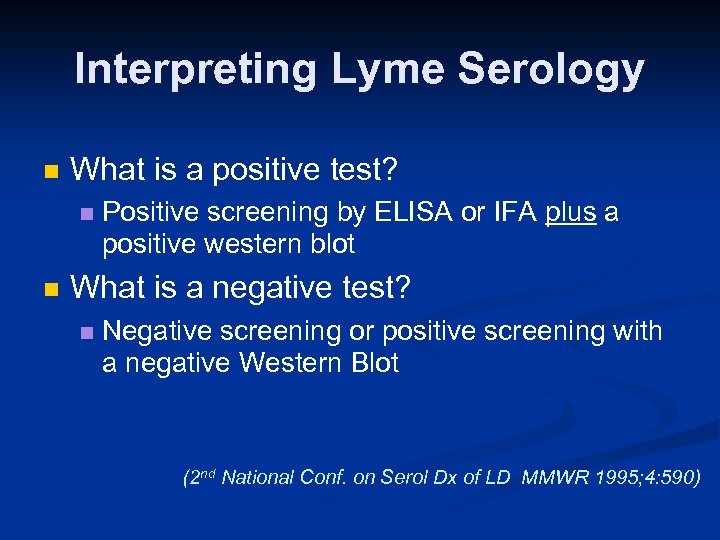
Interpreting Lyme Serology n What is a positive test? n n Positive screening by ELISA or IFA plus a positive western blot What is a negative test? n Negative screening or positive screening with a negative Western Blot (2 nd National Conf. on Serol Dx of LD MMWR 1995; 4: 590)
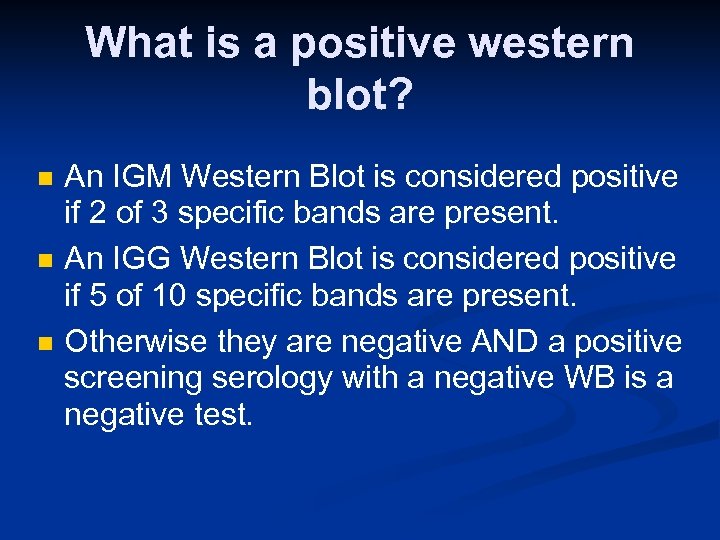
What is a positive western blot? n n n An IGM Western Blot is considered positive if 2 of 3 specific bands are present. An IGG Western Blot is considered positive if 5 of 10 specific bands are present. Otherwise they are negative AND a positive screening serology with a negative WB is a negative test.
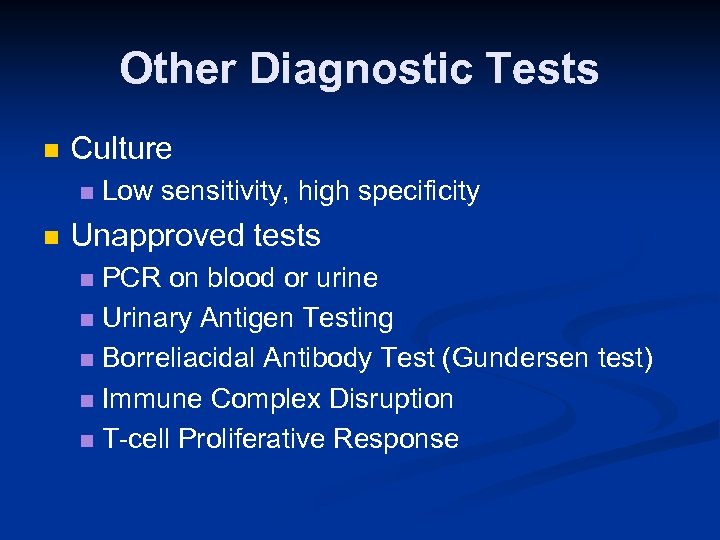
Other Diagnostic Tests n Culture n n Low sensitivity, high specificity Unapproved tests PCR on blood or urine n Urinary Antigen Testing n Borreliacidal Antibody Test (Gundersen test) n Immune Complex Disruption n T-cell Proliferative Response n
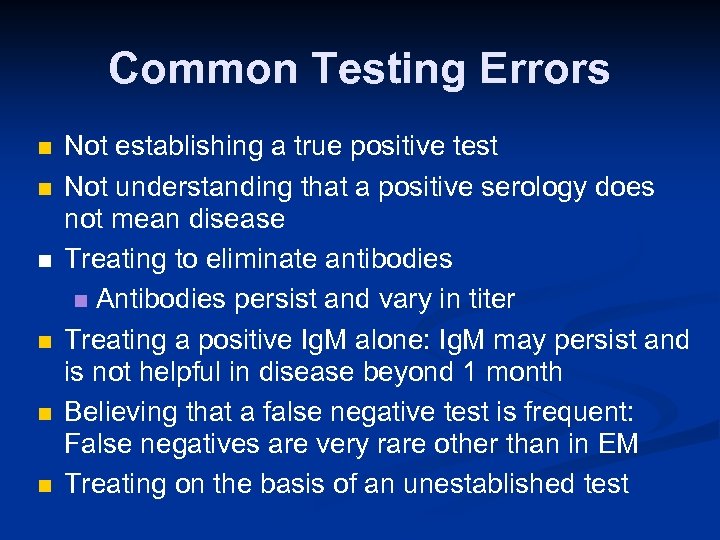
Common Testing Errors n n n Not establishing a true positive test Not understanding that a positive serology does not mean disease Treating to eliminate antibodies n Antibodies persist and vary in titer Treating a positive Ig. M alone: Ig. M may persist and is not helpful in disease beyond 1 month Believing that a false negative test is frequent: False negatives are very rare other than in EM Treating on the basis of an unestablished test
So, what is the consequence of misunderstanding the serology? THE CREATION OF MYTHS Ø An entire syndrome (disease? ) has been created that does not exist Ø A belief that the serology is not good. Ø A belief that Lyme disease is difficult to treat.
How Good is the Treatment of Lyme Disease? VERY GOOD There Rarely is a Reason to Retreat a Patient
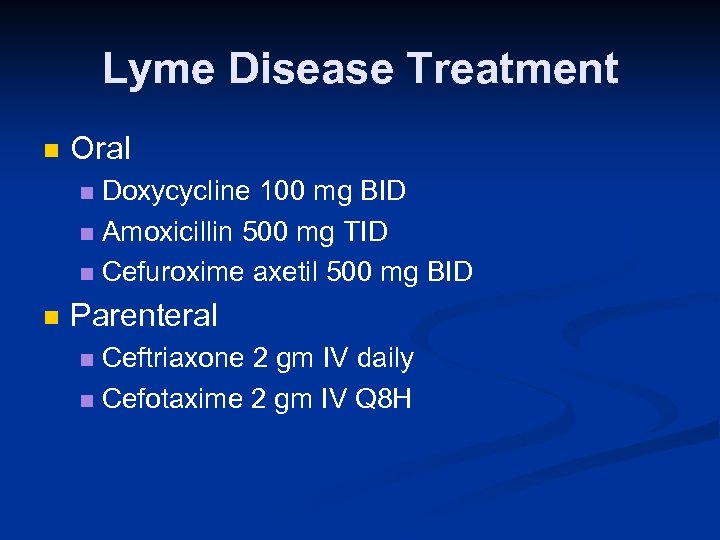
Lyme Disease Treatment n Oral Doxycycline 100 mg BID n Amoxicillin 500 mg TID n Cefuroxime axetil 500 mg BID n n Parenteral Ceftriaxone 2 gm IV daily n Cefotaxime 2 gm IV Q 8 H n
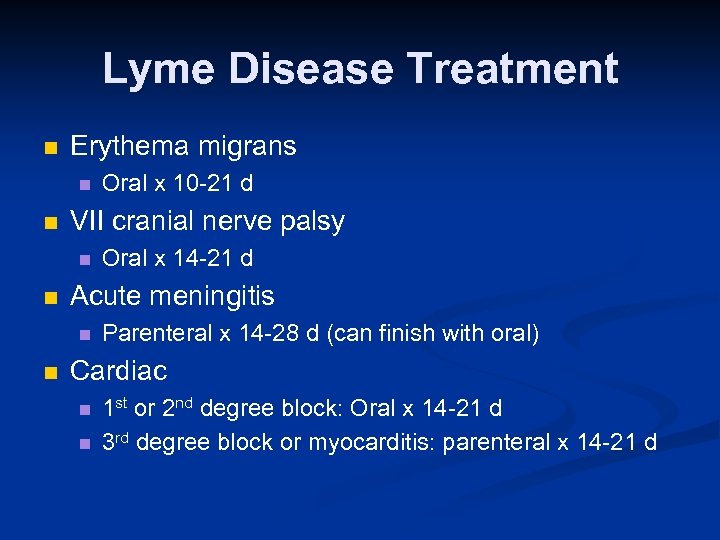
Lyme Disease Treatment n Erythema migrans n n VII cranial nerve palsy n n Oral x 14 -21 d Acute meningitis n n Oral x 10 -21 d Parenteral x 14 -28 d (can finish with oral) Cardiac n n 1 st or 2 nd degree block: Oral x 14 -21 d 3 rd degree block or myocarditis: parenteral x 14 -21 d
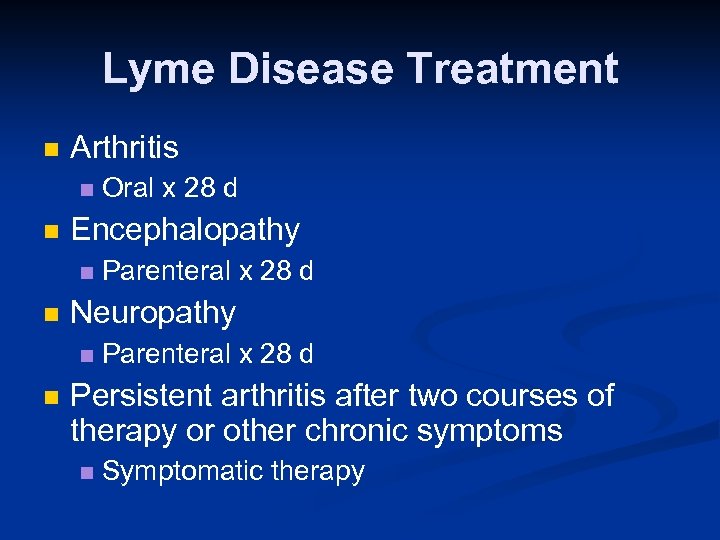
Lyme Disease Treatment n Arthritis n n Encephalopathy n n Parenteral x 28 d Neuropathy n n Oral x 28 d Parenteral x 28 d Persistent arthritis after two courses of therapy or other chronic symptoms n Symptomatic therapy
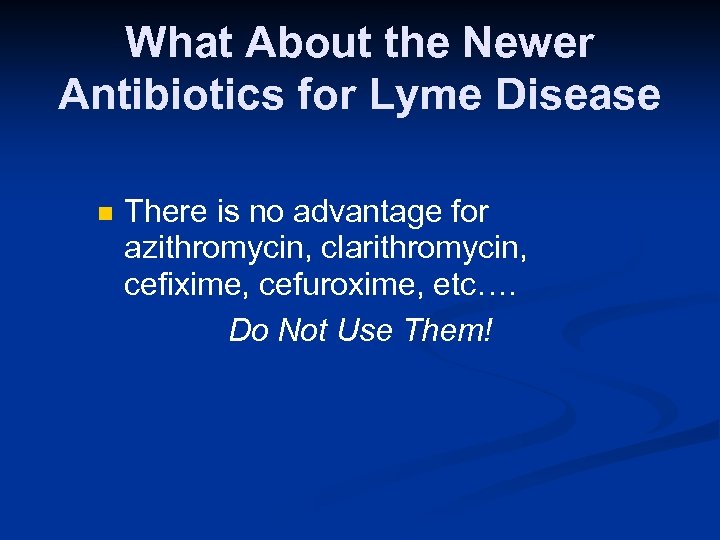
What About the Newer Antibiotics for Lyme Disease n There is no advantage for azithromycin, clarithromycin, cefixime, cefuroxime, etc…. Do Not Use Them!
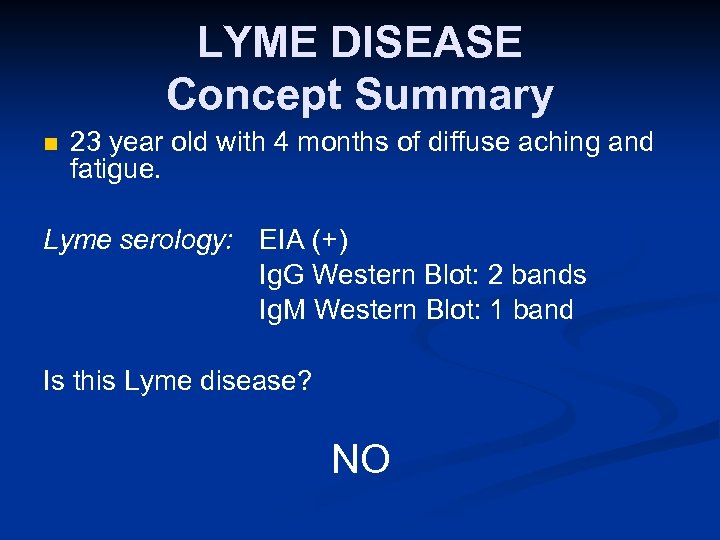
LYME DISEASE Concept Summary n 23 year old with 4 months of diffuse aching and fatigue. Lyme serology: EIA (+) Ig. G Western Blot: 2 bands Ig. M Western Blot: 1 band Is this Lyme disease? NO
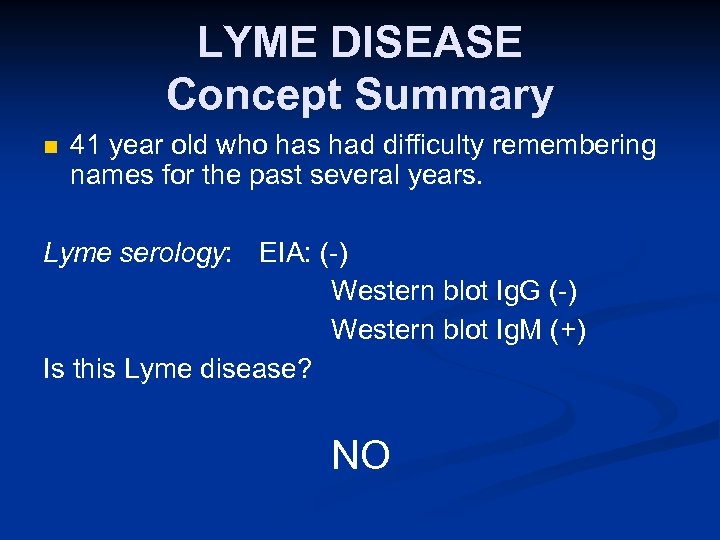
LYME DISEASE Concept Summary n 41 year old who has had difficulty remembering names for the past several years. Lyme serology: EIA: (-) Western blot Ig. G (-) Western blot Ig. M (+) Is this Lyme disease? NO
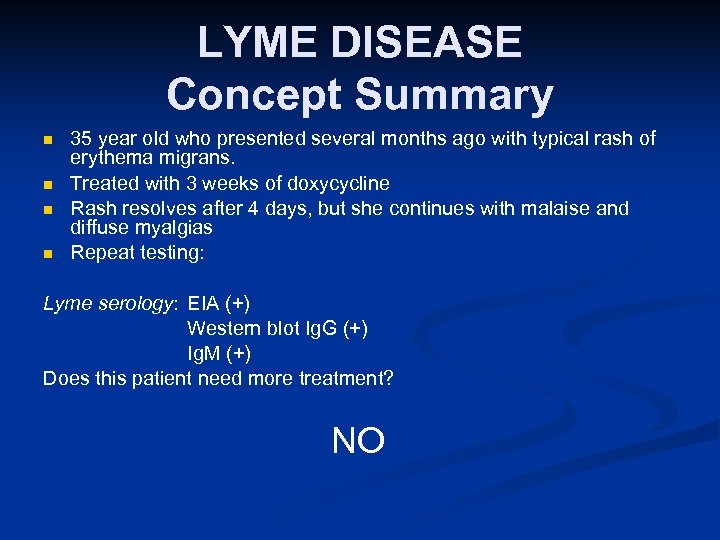
LYME DISEASE Concept Summary n n 35 year old who presented several months ago with typical rash of erythema migrans. Treated with 3 weeks of doxycycline Rash resolves after 4 days, but she continues with malaise and diffuse myalgias Repeat testing: Lyme serology: EIA (+) Western blot Ig. G (+) Ig. M (+) Does this patient need more treatment? NO
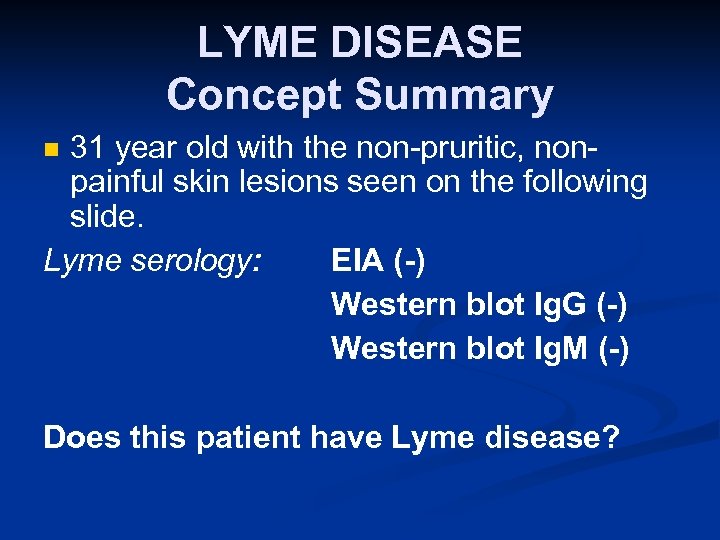
LYME DISEASE Concept Summary 31 year old with the non-pruritic, nonpainful skin lesions seen on the following slide. Lyme serology: EIA (-) Western blot Ig. G (-) Western blot Ig. M (-) n Does this patient have Lyme disease?

YOU BETCHA
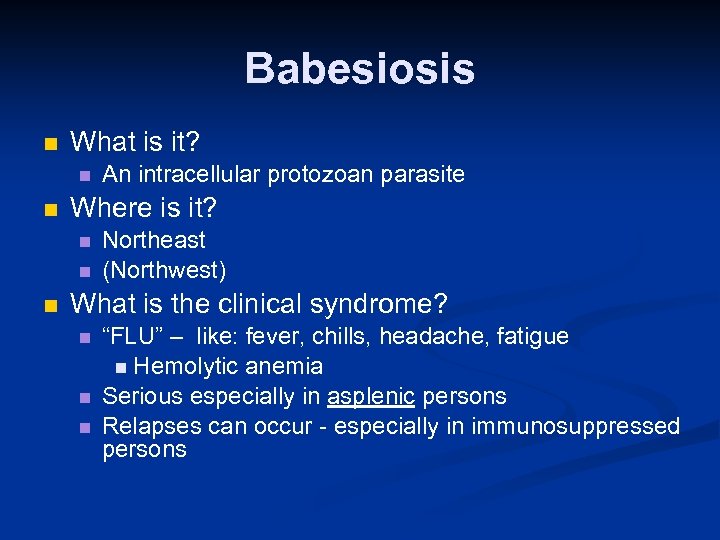
Babesiosis n What is it? n n Where is it? n n n An intracellular protozoan parasite Northeast (Northwest) What is the clinical syndrome? n n n “FLU” – like: fever, chills, headache, fatigue n Hemolytic anemia Serious especially in asplenic persons Relapses can occur - especially in immunosuppressed persons
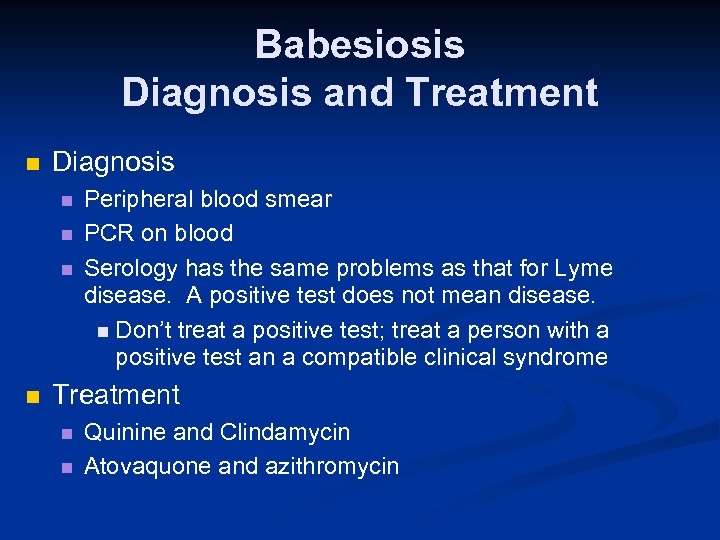
Babesiosis Diagnosis and Treatment n Diagnosis n n Peripheral blood smear PCR on blood Serology has the same problems as that for Lyme disease. A positive test does not mean disease. n Don’t treat a positive test; treat a person with a positive test an a compatible clinical syndrome Treatment n n Quinine and Clindamycin Atovaquone and azithromycin

Babesiosis
Ehrlichiosis and Anaplasmosis n What are they? n Rickettsiaceae family n Human Monocytic Ehrlichiosis (HME) n Lone n Human star tick Granulocytic Anaplasmosis (HGA) n Ixodes n ticks Where is it? n Everywhere
Human Monocytic Ehrlichiosis n n n E. chaffeensis First described in 1987 Primarily infects mononuclear cells Reservoir: deer, dogs, goats Vector: Lone star tick (Amblyomma americanum)
Human Granulocytic Anaplasmosis n n First described in 1994 Organism recently named Anaplasma phagocytophilum. Reservoir: deer, rodents, elk Vector: Ixodes ticks
Ehrlichiosis and Anaplasmosis SIGNS AND SYMPTOMS n Incubation period: 5 - 10 days n Early symptoms are non-specific (“flu-like”) n n Fever, headache, myalgias GI symptoms can occur Rash variable Laboratory n Leucopenia, thrombocytopenia, abnormal liver enzymes
Ehrlichiosis and Anaplasmosis n COMPLICATIONS Can be very severe n n n n Renal failure ARDS DIC Encephalitis 3% mortality Worse in patients with impaired host defenses Watch out for dual or triple infections with n Borrelia burgdorferi and Babesia
Ehrlichiosis and Anaplasmosis n n n DIAGNOSIS Peripheral smear looking for morulae Serology PCR (state laboratories) Culture Treat based on epidemiologic and clinical clues. Do not delay while waiting for confirmation.
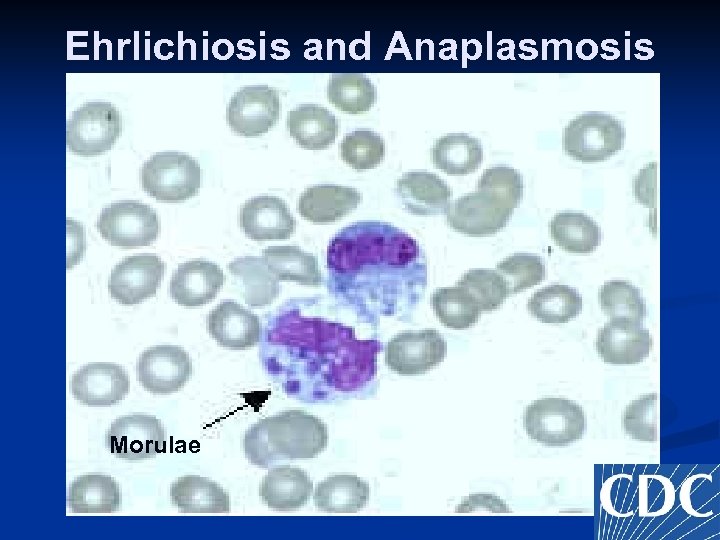
Ehrlichiosis and Anaplasmosis Morulae
Ehrlichiosis and Anaplasmosis n n TREATMENT Treatment should not be delayed until laboratory confirmation is obtained Doxycycline: 100 mg PO/IV Until 3 days after fever abates n Expect response in 24 - 72 hours n n Pregnancy and children ? ? ? n Rifampin 600 mg IV/PO has been used
Rocky Mountain Spotted Fever n n n Clinical Spectrum from mild to fulminant Throughout the Western Hemisphere Vector: Dermacentor n Dog or Wood Ticks
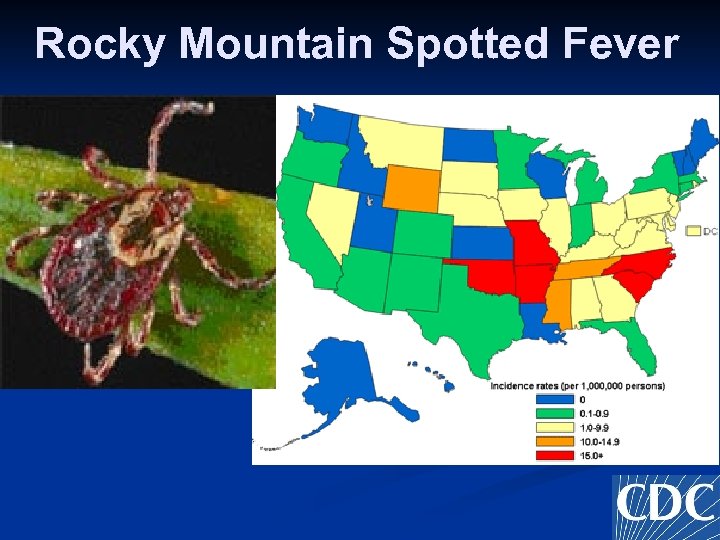
Rocky Mountain Spotted Fever
Rocky Mountain Spotted Fever Clinical Manifestations n n Incubation Period: 3 - 14 days (ave 5 - 7) Non-specific Fever n Headache n Myalgias n GI n n n Rash Mortality about 25% if treatment delayed
Rocky Mountain Spotted Fever Rash n Begins on day 3 - 5 Only 15% have a rash on the first day n 10% never get a rash n n Do not wait for a rash to initiate therapy Starts on ankles and wrists Spreads centrally and to palms/soles

Rocky Mountain Spotted Fever Diagnosis n n Initially made clinically on suspicion and epidemiology Serology Used to confirm diagnosis n Takes at least 10 -14 days to seroconvert n n Skin biopsy Rapid, if available (requires special stains) n 70% sensitive n
Rocky Mountain Spotted Fever Treatment n Can not overstress the importance of early therapy n n n Mortality related to when treatment initiated n < 5 days 6. 5% n > 5 days 22. 9% (most saw a physician within the first five days) Doxycycline for adults and children Chloramphenicol is the alternative
Tick Typhus n n Throughout the world All have rashes Typically on trunk n Most with tick bite site eschar n n All diagnosed serologically All treated with doxycycline Consider the diagnosis in a febrile returning traveler
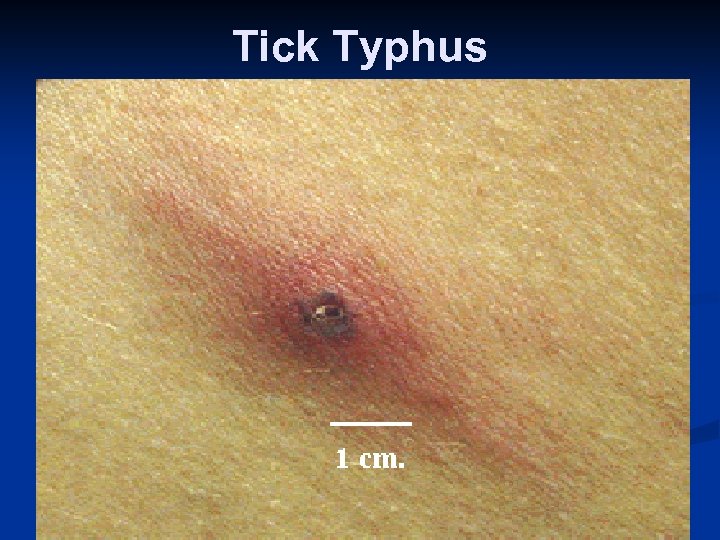
Tick Typhus
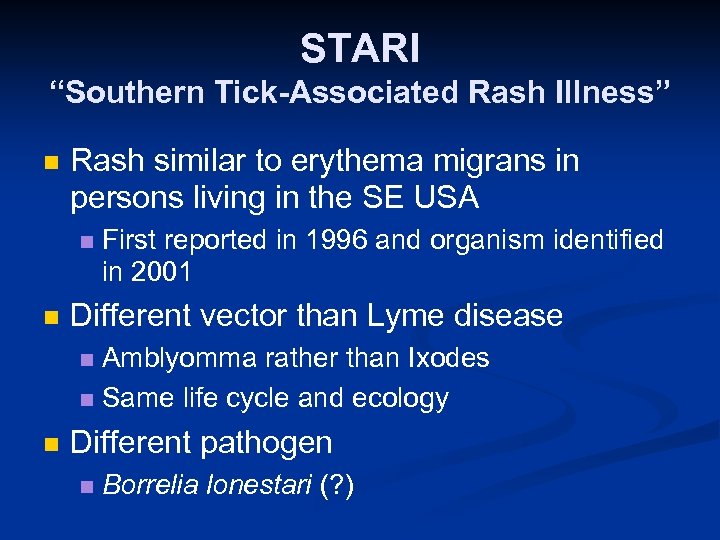
STARI “Southern Tick-Associated Rash Illness” n Rash similar to erythema migrans in persons living in the SE USA n n First reported in 1996 and organism identified in 2001 Different vector than Lyme disease Amblyomma rather than Ixodes n Same life cycle and ecology n n Different pathogen n Borrelia lonestari (? )

Amblyomma americanum “Lone Star” Tick
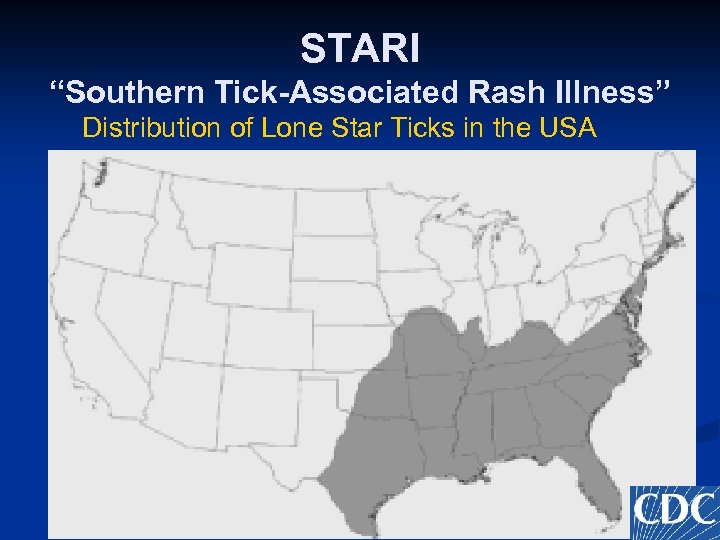
STARI “Southern Tick-Associated Rash Illness” Distribution of Lone Star Ticks in the USA
STARI “Southern Tick-Associated Rash Illness” n Diagnosis Unable to culture at this time n PCR on biopsy of rash n Lyme disease serology is negative n n Treatment n n ? Doxycycline Sequellae n None known to date
Managing a Tick Bite n You get a phone call at 5: 30 on a Friday evening from a patient who says that he just found a tick behind the ear of his wife. They ask: How should they remove it? n Should she get antibiotics? n
Removing a Tick n n n Do not use Vaseline, kerosene, matches, gasoline Use a hemostat or forceps and grasp tick as close to the skin as possible Pull back gently and firmly perpendicular to the skin Don’t squeeze or crush Don’t worry about residual mouth parts
Antibiotic ? n Need to address three questions Type of tick? n Attached or engorged? n Duration of attachment? n n Prophylactic antibiotics generally not indicated
SINGLE DOSE DOXYCYCLINE? n If: > 8 years old n Attached tick was nymph or adult Ixodes scapularis n Attached for at least 36 hours n Prophylaxis can be started within 72 hours of tick removal n Local prevalence of Lyme disease is > 20% n No contraindication to doxy n n Otherwise observation alone is recommended
Questions?
75448a7fe987d1eacfc8c6013125de92.ppt