2ecda09d25bb53a3d7a46a53cecfc318.ppt
- Количество слайдов: 86
 Tianjin Medical University General Hospital
Tianjin Medical University General Hospital
 l INTRADUCTION l N-1 RELATED ANATOMY AND PHYSIOLOGY l N-2 CONGENITAL DEVELOPMENTAL ANOMALY OF THE OPTIC DISC l N-3 DISIASES OF OPTIC NERVE l N-4 THE OPTIC PATHWAY AND VISUAL CORTEX DISIASES
l INTRADUCTION l N-1 RELATED ANATOMY AND PHYSIOLOGY l N-2 CONGENITAL DEVELOPMENTAL ANOMALY OF THE OPTIC DISC l N-3 DISIASES OF OPTIC NERVE l N-4 THE OPTIC PATHWAY AND VISUAL CORTEX DISIASES
 INTRADUCTION l Neuro-ophthalmology is a crossing clinical science related with neurology and ophthalmology. l The source of the eye and the brain in some gene expression is identical l Modern molecuology and Human genome project provide more theory basic for neuroophthalmology l modern image technic : CT, MRI, f. MRI
INTRADUCTION l Neuro-ophthalmology is a crossing clinical science related with neurology and ophthalmology. l The source of the eye and the brain in some gene expression is identical l Modern molecuology and Human genome project provide more theory basic for neuroophthalmology l modern image technic : CT, MRI, f. MRI
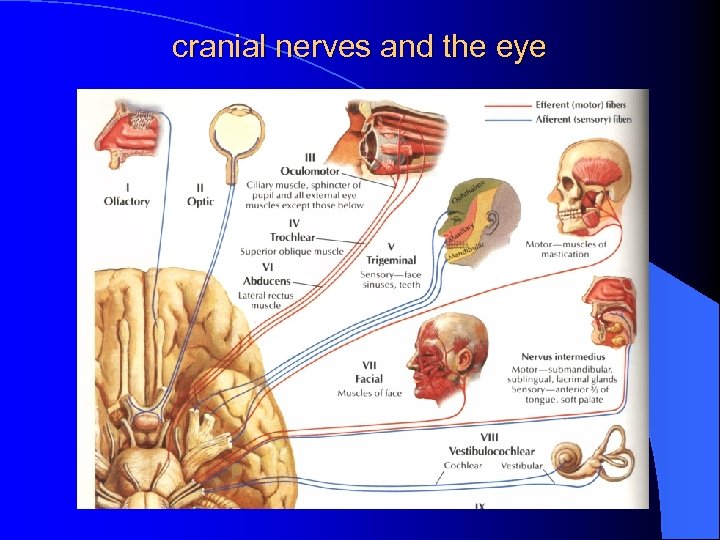 cranial nerves and the eye
cranial nerves and the eye
 INTRADUCTION cranial nerves and the eye l l l 6/12 pairs of the cranial nerve are linked with the eye II optic nerve, a part of the brain III, IV and VI is oculomotor, trochlear and abduces nerves respectively ( motor ) V is trigeminal nerve ( sense ) VII is facial nerve ( motor ) 38% of nerve fibers in the central system are related with the eye; 65% petients with brain diseases may have some features on the eye
INTRADUCTION cranial nerves and the eye l l l 6/12 pairs of the cranial nerve are linked with the eye II optic nerve, a part of the brain III, IV and VI is oculomotor, trochlear and abduces nerves respectively ( motor ) V is trigeminal nerve ( sense ) VII is facial nerve ( motor ) 38% of nerve fibers in the central system are related with the eye; 65% petients with brain diseases may have some features on the eye
 N-1 RELATED BASIC STUDY N-1 -1 optic nerve and brain l The optic nerve consists of 1. 0 million axons that oringinate in the ganglio cell layer of the retina and extend toward the occipital cortex. l It has a similar organization to the white matter of the brain, it is a part of the brain. l It segregated into 500 pathways by lamina cribrosa.
N-1 RELATED BASIC STUDY N-1 -1 optic nerve and brain l The optic nerve consists of 1. 0 million axons that oringinate in the ganglio cell layer of the retina and extend toward the occipital cortex. l It has a similar organization to the white matter of the brain, it is a part of the brain. l It segregated into 500 pathways by lamina cribrosa.
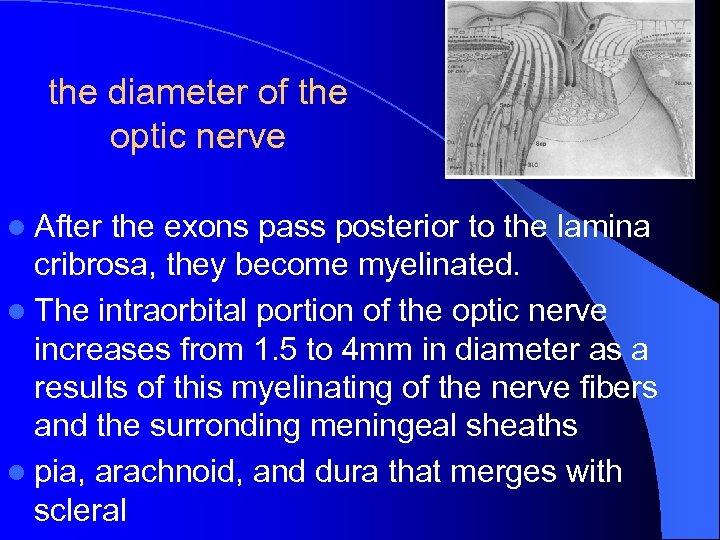 the diameter of the optic nerve l After the exons pass posterior to the lamina cribrosa, they become myelinated. l The intraorbital portion of the optic nerve increases from 1. 5 to 4 mm in diameter as a results of this myelinating of the nerve fibers and the surronding meningeal sheaths l pia, arachnoid, and dura that merges with scleral
the diameter of the optic nerve l After the exons pass posterior to the lamina cribrosa, they become myelinated. l The intraorbital portion of the optic nerve increases from 1. 5 to 4 mm in diameter as a results of this myelinating of the nerve fibers and the surronding meningeal sheaths l pia, arachnoid, and dura that merges with scleral
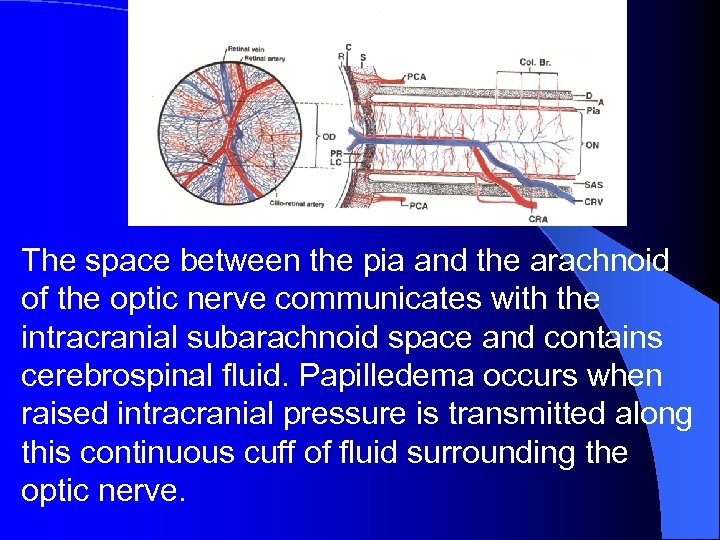 The space between the pia and the arachnoid of the optic nerve communicates with the intracranial subarachnoid space and contains cerebrospinal fluid. Papilledema occurs when raised intracranial pressure is transmitted along this continuous cuff of fluid surrounding the optic nerve.
The space between the pia and the arachnoid of the optic nerve communicates with the intracranial subarachnoid space and contains cerebrospinal fluid. Papilledema occurs when raised intracranial pressure is transmitted along this continuous cuff of fluid surrounding the optic nerve.
 N-1 RELATED BASIC STUDY N 1 -2 axoplasmic transport (A. T) in axons of G. C. : l (1)Orthograde transport ( axoplasmic flow ) from the somata of retinal G. C. to their terminals in the lateral geniculate body ( LGB ). l (2)Retrograde transport occurs from the LGB terminals back to the somata in the retina. l (3)Transplant The A. T. depends upon the different pressure between intraocular and intra-optic nerve. The obstruction of A. T. contributes to swelling of the optic disc.
N-1 RELATED BASIC STUDY N 1 -2 axoplasmic transport (A. T) in axons of G. C. : l (1)Orthograde transport ( axoplasmic flow ) from the somata of retinal G. C. to their terminals in the lateral geniculate body ( LGB ). l (2)Retrograde transport occurs from the LGB terminals back to the somata in the retina. l (3)Transplant The A. T. depends upon the different pressure between intraocular and intra-optic nerve. The obstruction of A. T. contributes to swelling of the optic disc.
 N-1 -3 visual pathway and cortex N-1 -3 -1 The optic nerve l Intraocular- ( 1 mm) can be seen with ophthalmoscope l Intraorbital- (length 25 mm) is relatively free to move, the eye rotation is facility l Intracanalicular- ( 9 mm) becomes anchored firmly. As a result, a small mass lesion in the optic canal can produce a compressive optic neuropathy. l Intracrainal (length 16 mm ) till to chiasm
N-1 -3 visual pathway and cortex N-1 -3 -1 The optic nerve l Intraocular- ( 1 mm) can be seen with ophthalmoscope l Intraorbital- (length 25 mm) is relatively free to move, the eye rotation is facility l Intracanalicular- ( 9 mm) becomes anchored firmly. As a result, a small mass lesion in the optic canal can produce a compressive optic neuropathy. l Intracrainal (length 16 mm ) till to chiasm
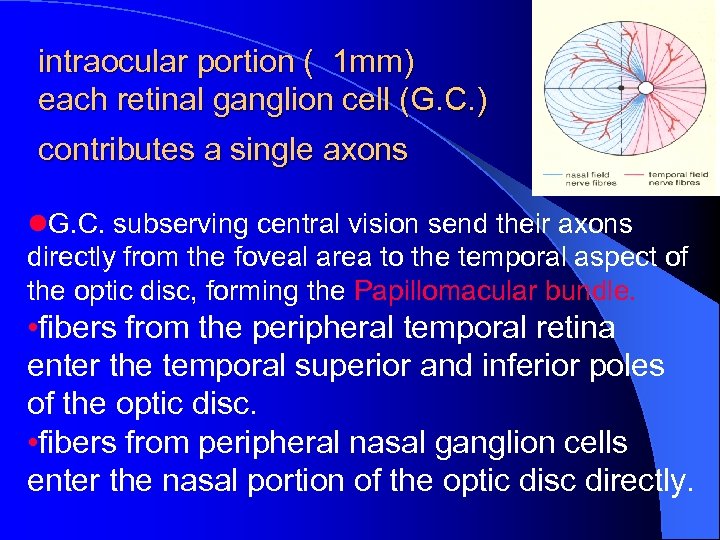 intraocular portion ( 1 mm) each retinal ganglion cell (G. C. ) contributes a single axons l. G. C. subserving central vision send their axons directly from the foveal area to the temporal aspect of the optic disc, forming the Papillomacular bundle. • fibers from the peripheral temporal retina enter the temporal superior and inferior poles of the optic disc. • fibers from peripheral nasal ganglion cells enter the nasal portion of the optic disc directly.
intraocular portion ( 1 mm) each retinal ganglion cell (G. C. ) contributes a single axons l. G. C. subserving central vision send their axons directly from the foveal area to the temporal aspect of the optic disc, forming the Papillomacular bundle. • fibers from the peripheral temporal retina enter the temporal superior and inferior poles of the optic disc. • fibers from peripheral nasal ganglion cells enter the nasal portion of the optic disc directly.
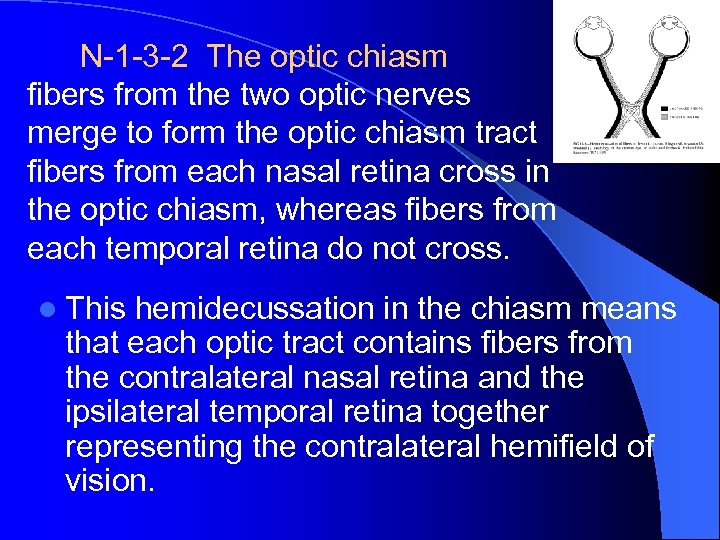 N-1 -3 -2 The optic chiasm fibers from the two optic nerves merge to form the optic chiasm tract fibers from each nasal retina cross in the optic chiasm, whereas fibers from each temporal retina do not cross. l This hemidecussation in the chiasm means that each optic tract contains fibers from the contralateral nasal retina and the ipsilateral temporal retina together representing the contralateral hemifield of vision.
N-1 -3 -2 The optic chiasm fibers from the two optic nerves merge to form the optic chiasm tract fibers from each nasal retina cross in the optic chiasm, whereas fibers from each temporal retina do not cross. l This hemidecussation in the chiasm means that each optic tract contains fibers from the contralateral nasal retina and the ipsilateral temporal retina together representing the contralateral hemifield of vision.
 N-1 -3 -3 The optic tracts l The optic tracts begin at the posterior aspect of the optic chiasm continue posteriorly to the colliculus, than to l ①the lateral geniculate nucleus cortical(90%) l ②a special fibers into the superior colliculus pulvinar (丘脑枕) cortical. l This structures are thought to provide visual input to neuroendocrine systems controlling diurnal rhythms and visual analysis.
N-1 -3 -3 The optic tracts l The optic tracts begin at the posterior aspect of the optic chiasm continue posteriorly to the colliculus, than to l ①the lateral geniculate nucleus cortical(90%) l ②a special fibers into the superior colliculus pulvinar (丘脑枕) cortical. l This structures are thought to provide visual input to neuroendocrine systems controlling diurnal rhythms and visual analysis.
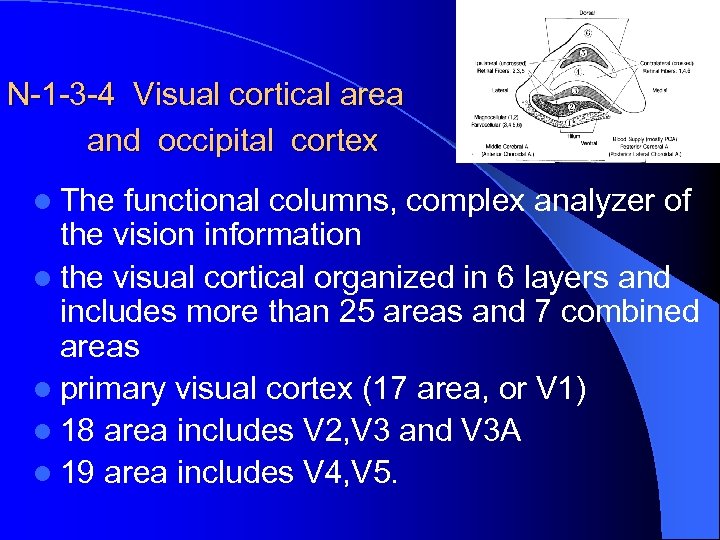 N-1 -3 -4 Visual cortical area and occipital cortex l The functional columns, complex analyzer of the vision information l the visual cortical organized in 6 layers and includes more than 25 areas and 7 combined areas l primary visual cortex (17 area, or V 1) l 18 area includes V 2, V 3 and V 3 A l 19 area includes V 4, V 5.
N-1 -3 -4 Visual cortical area and occipital cortex l The functional columns, complex analyzer of the vision information l the visual cortical organized in 6 layers and includes more than 25 areas and 7 combined areas l primary visual cortex (17 area, or V 1) l 18 area includes V 2, V 3 and V 3 A l 19 area includes V 4, V 5.
 N-1 -3 -5 Visual cortical cells N-1 -3 -6 The optic radiation l the visual cortical cells may be divided into l the magnocellular (M cell), the large ones, that is thought to subserve motion detection, stereopsis, and low spatial frequency contrast sensitivity l The parvocellular (P cell), or smallest, that probably serve fine spacial resolution and color vision. l ①simple ②complex ③ hyper complex cells
N-1 -3 -5 Visual cortical cells N-1 -3 -6 The optic radiation l the visual cortical cells may be divided into l the magnocellular (M cell), the large ones, that is thought to subserve motion detection, stereopsis, and low spatial frequency contrast sensitivity l The parvocellular (P cell), or smallest, that probably serve fine spacial resolution and color vision. l ①simple ②complex ③ hyper complex cells
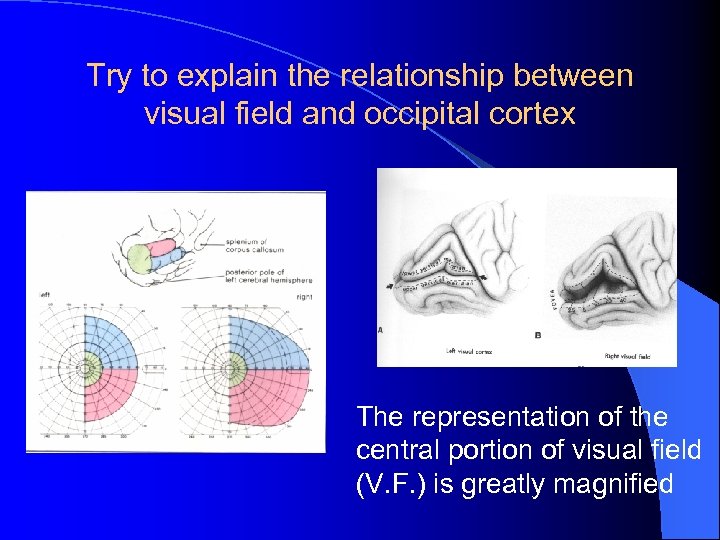 Try to explain the relationship between visual field and occipital cortex The representation of the central portion of visual field (V. F. ) is greatly magnified
Try to explain the relationship between visual field and occipital cortex The representation of the central portion of visual field (V. F. ) is greatly magnified
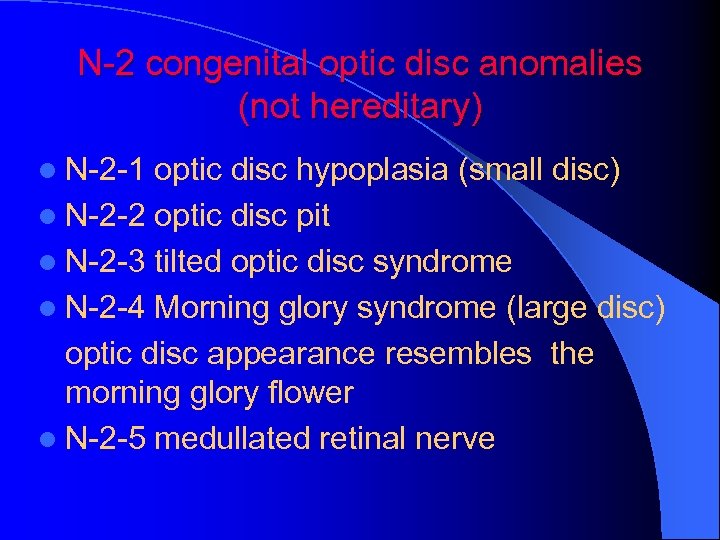 N-2 congenital optic disc anomalies (not hereditary) l N-2 -1 optic disc hypoplasia (small disc) l N-2 -2 optic disc pit l N-2 -3 tilted optic disc syndrome l N-2 -4 Morning glory syndrome (large disc) optic disc appearance resembles the morning glory flower l N-2 -5 medullated retinal nerve
N-2 congenital optic disc anomalies (not hereditary) l N-2 -1 optic disc hypoplasia (small disc) l N-2 -2 optic disc pit l N-2 -3 tilted optic disc syndrome l N-2 -4 Morning glory syndrome (large disc) optic disc appearance resembles the morning glory flower l N-2 -5 medullated retinal nerve
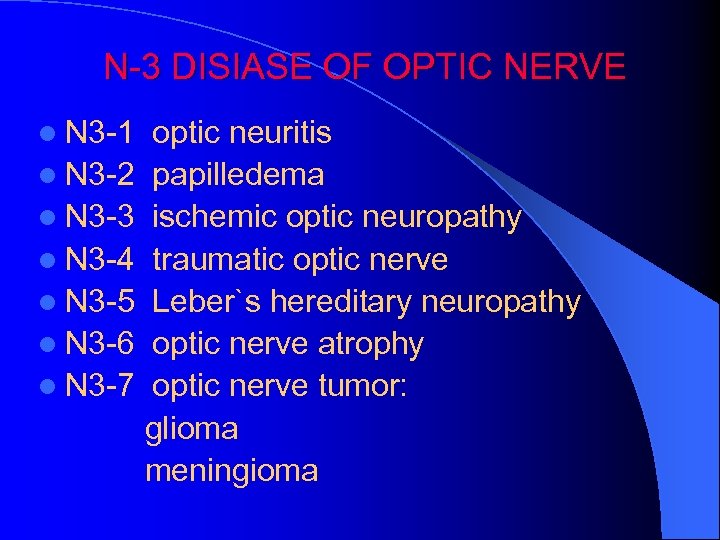 N-3 DISIASE OF OPTIC NERVE l N 3 -1 l N 3 -2 l N 3 -3 l N 3 -4 l N 3 -5 l N 3 -6 l N 3 -7 optic neuritis papilledema ischemic optic neuropathy traumatic optic nerve Leber`s hereditary neuropathy optic nerve atrophy optic nerve tumor: glioma meningioma
N-3 DISIASE OF OPTIC NERVE l N 3 -1 l N 3 -2 l N 3 -3 l N 3 -4 l N 3 -5 l N 3 -6 l N 3 -7 optic neuritis papilledema ischemic optic neuropathy traumatic optic nerve Leber`s hereditary neuropathy optic nerve atrophy optic nerve tumor: glioma meningioma
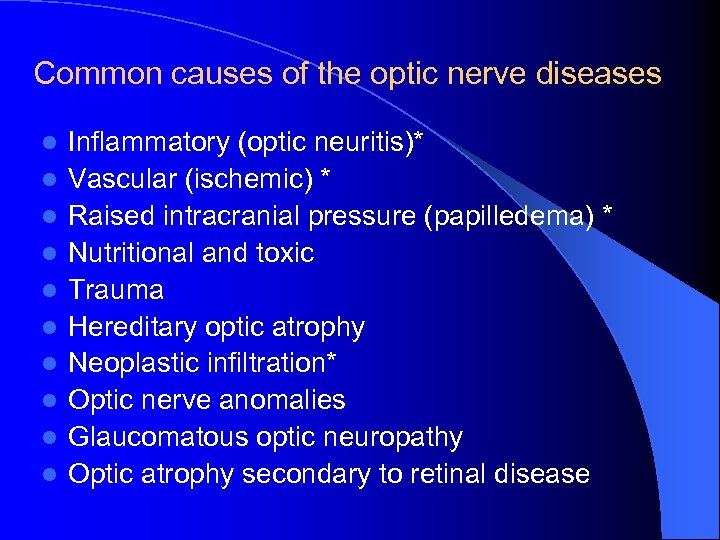 Common causes of the optic nerve diseases l l l l l Inflammatory (optic neuritis)* Vascular (ischemic) * Raised intracranial pressure (papilledema) * Nutritional and toxic Trauma Hereditary optic atrophy Neoplastic infiltration* Optic nerve anomalies Glaucomatous optic neuropathy Optic atrophy secondary to retinal disease
Common causes of the optic nerve diseases l l l l l Inflammatory (optic neuritis)* Vascular (ischemic) * Raised intracranial pressure (papilledema) * Nutritional and toxic Trauma Hereditary optic atrophy Neoplastic infiltration* Optic nerve anomalies Glaucomatous optic neuropathy Optic atrophy secondary to retinal disease
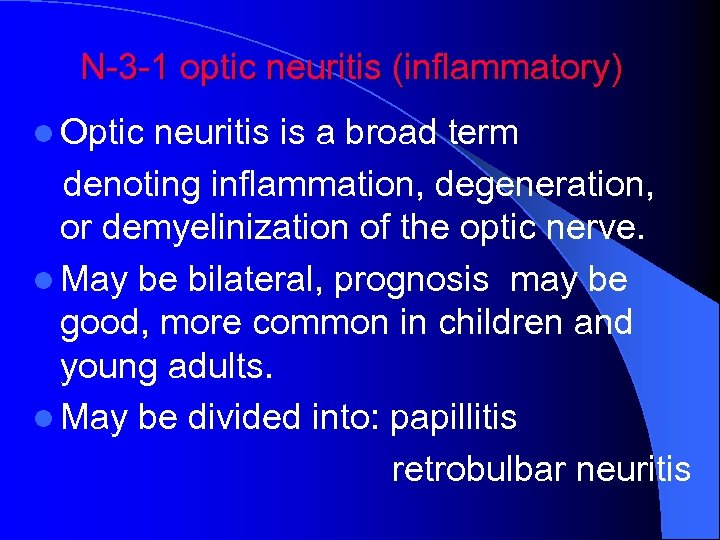 N-3 -1 optic neuritis (inflammatory) l Optic neuritis is a broad term denoting inflammation, degeneration, or demyelinization of the optic nerve. l May be bilateral, prognosis may be good, more common in children and young adults. l May be divided into: papillitis retrobulbar neuritis
N-3 -1 optic neuritis (inflammatory) l Optic neuritis is a broad term denoting inflammation, degeneration, or demyelinization of the optic nerve. l May be bilateral, prognosis may be good, more common in children and young adults. l May be divided into: papillitis retrobulbar neuritis
 N-3 -1 the papillitis N-3 -1 -1 etiology 1. idiopathic neuritis: 15%--75% 2. local extension of inflammatory disease 3. viral infection 4. systemic infectious and inflammation 5. nutrational and metabolic 6. toxic 7. demyelinating disease
N-3 -1 the papillitis N-3 -1 -1 etiology 1. idiopathic neuritis: 15%--75% 2. local extension of inflammatory disease 3. viral infection 4. systemic infectious and inflammation 5. nutrational and metabolic 6. toxic 7. demyelinating disease
 8. genetically determined optic atrophy 9. vascular disease 10. neoplastic 11. trama 12. radiation neuropathy 13. hemorrhage 14. psychological disease
8. genetically determined optic atrophy 9. vascular disease 10. neoplastic 11. trama 12. radiation neuropathy 13. hemorrhage 14. psychological disease
 N-3 -1 -1 -2 pathology of the papillitis l In early stage, is an outpouring of white blood cell, predominantly neutrophils. l The nerve fibers are swollen and fragmented. Fat-bearing macrophages soon appear, carrying away degenerated myelin material. l As the process becomes more chronic, lymphocytes and plasma cells predominate.
N-3 -1 -1 -2 pathology of the papillitis l In early stage, is an outpouring of white blood cell, predominantly neutrophils. l The nerve fibers are swollen and fragmented. Fat-bearing macrophages soon appear, carrying away degenerated myelin material. l As the process becomes more chronic, lymphocytes and plasma cells predominate.
 l In mild cases the nerve fibers may be preserved with a minimum amount of scar tissue formation. l When nerve tissue is permanently destroyed, fibrous gliosis replaces the nerve elements. l Due to increased pressure of intra-optic nerve, the axoplasmic transport may be influenced, the nerve fiber lesion may be continue, may lead to atrophy.
l In mild cases the nerve fibers may be preserved with a minimum amount of scar tissue formation. l When nerve tissue is permanently destroyed, fibrous gliosis replaces the nerve elements. l Due to increased pressure of intra-optic nerve, the axoplasmic transport may be influenced, the nerve fiber lesion may be continue, may lead to atrophy.
 N-3 -1 -1 -3 Clinic findings l Severe loss of vision in more cases, even to no light perception and may improve dramatically within 2 -3 weeks. l Eye pain may be present especially upon movement of the globe. l Central scotomas or ceco-central scotoma are the most common V. F. defect. l The pupil is dilated and the direct pupillary light reflex is sluggish ( relative afferent pupillary defect , RAPD)
N-3 -1 -1 -3 Clinic findings l Severe loss of vision in more cases, even to no light perception and may improve dramatically within 2 -3 weeks. l Eye pain may be present especially upon movement of the globe. l Central scotomas or ceco-central scotoma are the most common V. F. defect. l The pupil is dilated and the direct pupillary light reflex is sluggish ( relative afferent pupillary defect , RAPD)
 l In early stage, hyperemia of the optic disk and distention of large veins. blurred disk margins and filling of the physiologic cup. l The process may advance to marked edema of the nerve head, but elevation of more than 3 diopters (1 mm) are unusual. Extensive surrounding retinal edema may be present. l Flame-shaped hemorrhages may occur in the nerve fiber layer near the optic disk. l Retina: edema, exudate, and macular may be affected, It is called “neuroritinitis”.
l In early stage, hyperemia of the optic disk and distention of large veins. blurred disk margins and filling of the physiologic cup. l The process may advance to marked edema of the nerve head, but elevation of more than 3 diopters (1 mm) are unusual. Extensive surrounding retinal edema may be present. l Flame-shaped hemorrhages may occur in the nerve fiber layer near the optic disk. l Retina: edema, exudate, and macular may be affected, It is called “neuroritinitis”.
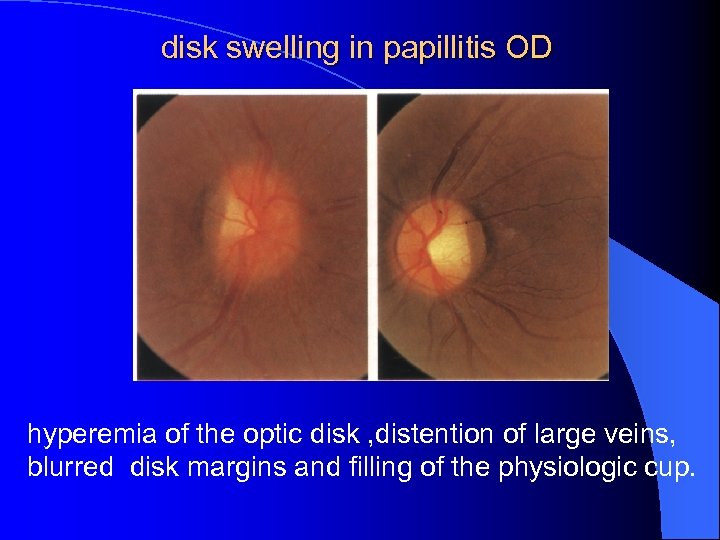 disk swelling in papillitis OD hyperemia of the optic disk , distention of large veins, blurred disk margins and filling of the physiologic cup.
disk swelling in papillitis OD hyperemia of the optic disk , distention of large veins, blurred disk margins and filling of the physiologic cup.
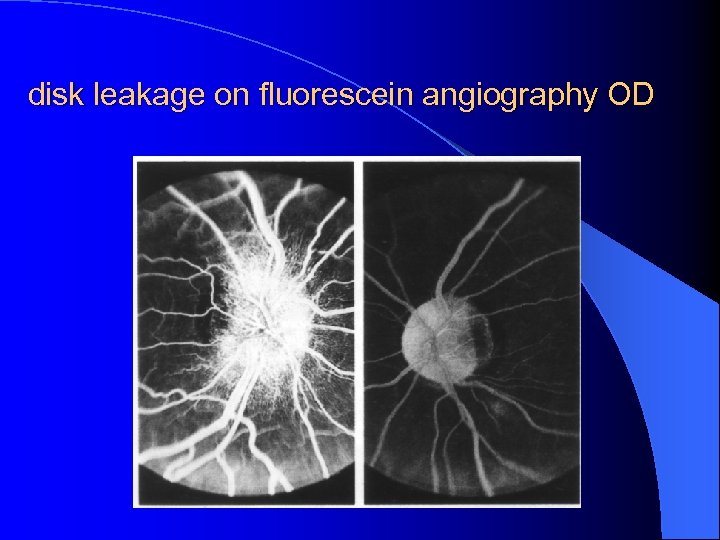 disk leakage on fluorescein angiography OD
disk leakage on fluorescein angiography OD
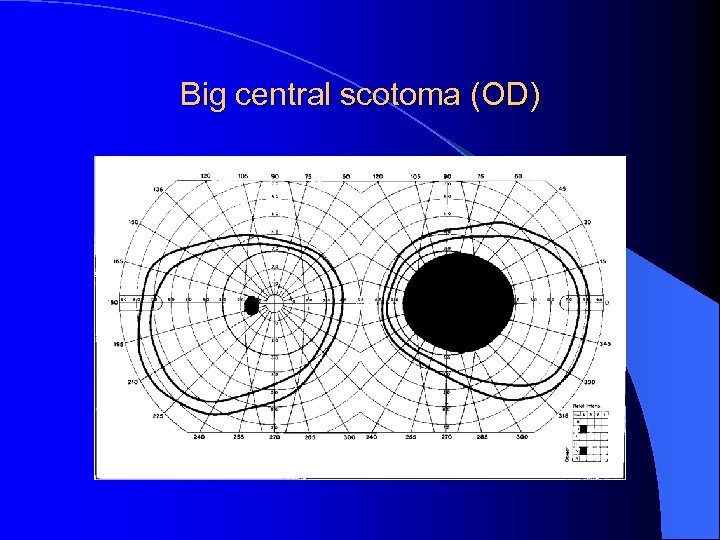 Big central scotoma (OD)
Big central scotoma (OD)
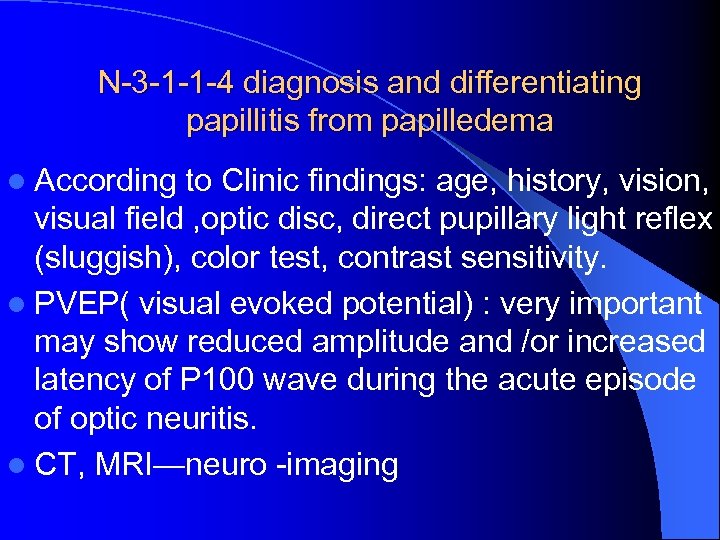 N-3 -1 -1 -4 diagnosis and differentiating papillitis from papilledema l According to Clinic findings: age, history, vision, visual field , optic disc, direct pupillary light reflex (sluggish), color test, contrast sensitivity. l PVEP( visual evoked potential) : very important may show reduced amplitude and /or increased latency of P 100 wave during the acute episode of optic neuritis. l CT, MRI—neuro -imaging
N-3 -1 -1 -4 diagnosis and differentiating papillitis from papilledema l According to Clinic findings: age, history, vision, visual field , optic disc, direct pupillary light reflex (sluggish), color test, contrast sensitivity. l PVEP( visual evoked potential) : very important may show reduced amplitude and /or increased latency of P 100 wave during the acute episode of optic neuritis. l CT, MRI—neuro -imaging
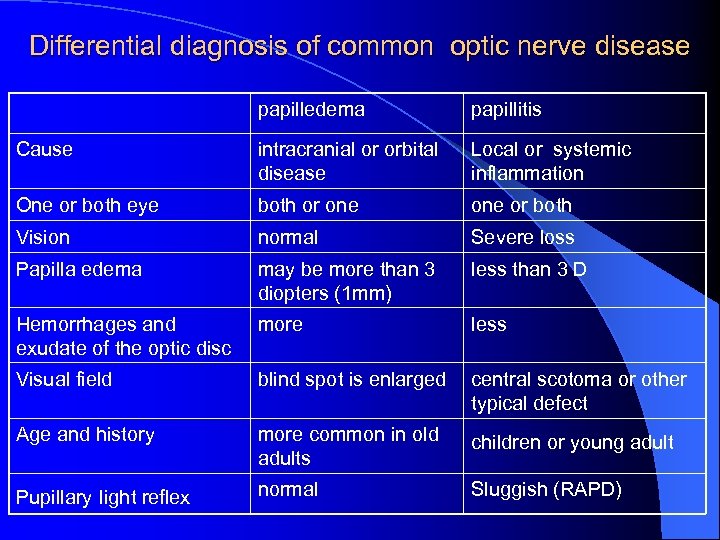 Differential diagnosis of common optic nerve disease papilledema papillitis Cause intracranial or orbital disease Local or systemic inflammation One or both eye both or one or both Vision normal Severe loss Papilla edema may be more than 3 diopters (1 mm) less than 3 D Hemorrhages and exudate of the optic disc more less Visual field blind spot is enlarged central scotoma or other typical defect Age and history more common in old adults children or young adult Pupillary light reflex normal Sluggish (RAPD)
Differential diagnosis of common optic nerve disease papilledema papillitis Cause intracranial or orbital disease Local or systemic inflammation One or both eye both or one or both Vision normal Severe loss Papilla edema may be more than 3 diopters (1 mm) less than 3 D Hemorrhages and exudate of the optic disc more less Visual field blind spot is enlarged central scotoma or other typical defect Age and history more common in old adults children or young adult Pupillary light reflex normal Sluggish (RAPD)
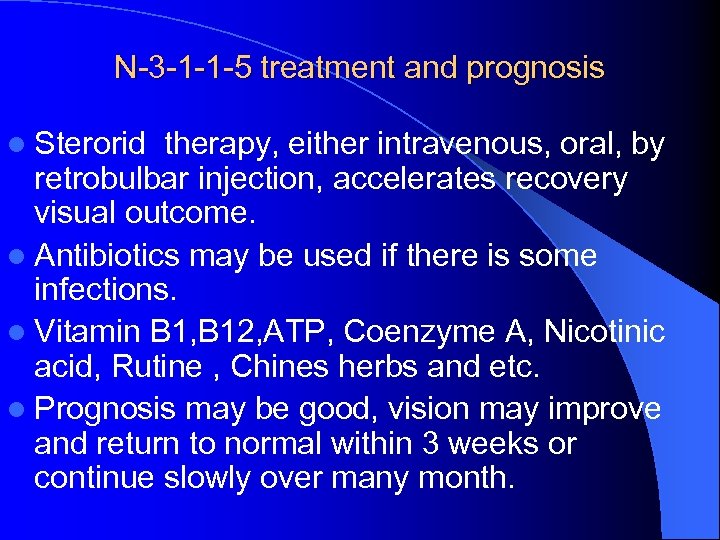 N-3 -1 -1 -5 treatment and prognosis l Sterorid therapy, either intravenous, oral, by retrobulbar injection, accelerates recovery visual outcome. l Antibiotics may be used if there is some infections. l Vitamin B 1, B 12, ATP, Coenzyme A, Nicotinic acid, Rutine , Chines herbs and etc. l Prognosis may be good, vision may improve and return to normal within 3 weeks or continue slowly over many month.
N-3 -1 -1 -5 treatment and prognosis l Sterorid therapy, either intravenous, oral, by retrobulbar injection, accelerates recovery visual outcome. l Antibiotics may be used if there is some infections. l Vitamin B 1, B 12, ATP, Coenzyme A, Nicotinic acid, Rutine , Chines herbs and etc. l Prognosis may be good, vision may improve and return to normal within 3 weeks or continue slowly over many month.
 N-3 -1 -2 retrobulbar neuritis inflammation occurs far enough behind the optic disk, so may be “the patient sees nothing and the doctor sees nothing”. l type : acute and chronic ( more common ) l ① axial retrobulbar neuritis: l ② retrobulbar perineuritis: syphilitic? l ③ transverse optic neuritis: severe type l
N-3 -1 -2 retrobulbar neuritis inflammation occurs far enough behind the optic disk, so may be “the patient sees nothing and the doctor sees nothing”. l type : acute and chronic ( more common ) l ① axial retrobulbar neuritis: l ② retrobulbar perineuritis: syphilitic? l ③ transverse optic neuritis: severe type l
 N-3 -1 -2 -1 etiology l Multiple sclerosis ( in west counties) : it is typically a chronic relapsing and demyelinating disorder of the central nervous system. HLA – A 3, B 7? the cause is unknown. l “lesions are dissimilated in time and space” ( systemic symptoms may appear late) l Neuromyelitis optica ( in Asian ) l Other causes may be considered: nutritional and toxic, vitamin deficiency, tobaco -alcohol amblyopia, methanol, ethylene glycol
N-3 -1 -2 -1 etiology l Multiple sclerosis ( in west counties) : it is typically a chronic relapsing and demyelinating disorder of the central nervous system. HLA – A 3, B 7? the cause is unknown. l “lesions are dissimilated in time and space” ( systemic symptoms may appear late) l Neuromyelitis optica ( in Asian ) l Other causes may be considered: nutritional and toxic, vitamin deficiency, tobaco -alcohol amblyopia, methanol, ethylene glycol
 N-3 -1 -2 -2 Clinic findings and diagnosis l Severe loss of vision may be suddenly or gradually, one eye in more cases, or bilateral. vision may be no light perception. l Vision may be influenced due to “temperature” l Fundus examination may be normal in early stage. l But vision, V. F. , the pupil and pupillary light reflex, especially VEP are very important. l Neuro- imaging examinations are needed, for example CT, MRI of brain and orbit.
N-3 -1 -2 -2 Clinic findings and diagnosis l Severe loss of vision may be suddenly or gradually, one eye in more cases, or bilateral. vision may be no light perception. l Vision may be influenced due to “temperature” l Fundus examination may be normal in early stage. l But vision, V. F. , the pupil and pupillary light reflex, especially VEP are very important. l Neuro- imaging examinations are needed, for example CT, MRI of brain and orbit.
 N-3 -1 -2 -3 treatment l Need not treatment? l A large, multicenter prospective study conducted from 1988 to 1991 with yearly follow-up. l Patients treated with oral prednisone did not have a better outcome than those treated with a placibo. l the patient sees nothing, the doctor sees nothing, and the treatment seems nothing too?
N-3 -1 -2 -3 treatment l Need not treatment? l A large, multicenter prospective study conducted from 1988 to 1991 with yearly follow-up. l Patients treated with oral prednisone did not have a better outcome than those treated with a placibo. l the patient sees nothing, the doctor sees nothing, and the treatment seems nothing too?
 N 3 -2 Papilledema l The term papilledema should be used only when referring to disk swelling produced by intracranial pressure , and it may be used to evaluate that if there is a disease with raised intracranial pressure. l There may not be any primary inflammation and any functional damage in early stage l A common sign in neuroophthalmology
N 3 -2 Papilledema l The term papilledema should be used only when referring to disk swelling produced by intracranial pressure , and it may be used to evaluate that if there is a disease with raised intracranial pressure. l There may not be any primary inflammation and any functional damage in early stage l A common sign in neuroophthalmology
 N 3 -2 -1 Etiology of the Papilledema ①Raised intracranial pressure l Intracranial mass( cerebral tumor, hydrocephalus) l Pseudotumor cerebri l Inflammation: meningitis or encephalitis, abscess, Guillain-Barre syndrome l Arteriovenous malformation l Uremia l Craniosynostoses l Respiratory failure l Severe allarrgic brain disease l Spinal tumor
N 3 -2 -1 Etiology of the Papilledema ①Raised intracranial pressure l Intracranial mass( cerebral tumor, hydrocephalus) l Pseudotumor cerebri l Inflammation: meningitis or encephalitis, abscess, Guillain-Barre syndrome l Arteriovenous malformation l Uremia l Craniosynostoses l Respiratory failure l Severe allarrgic brain disease l Spinal tumor
 ②Normal intracranial pressure l Congenital optic disk abnormality l Lebers disease l Inflammatory optic neuropathy l Ischemic optic neuropathy l Toxic neuropathy l Compressive optic neuropathy in the orbit ( dysthyroid ) l Infiltration disease: glioma, leukaemia, lymphoma, l Local vascular optic neuropathy: malignant hypertension, retinal central venous obstruction, optic disk vasculitis, ocular hypotony , uveitis l Mucopolysaccharidosis
②Normal intracranial pressure l Congenital optic disk abnormality l Lebers disease l Inflammatory optic neuropathy l Ischemic optic neuropathy l Toxic neuropathy l Compressive optic neuropathy in the orbit ( dysthyroid ) l Infiltration disease: glioma, leukaemia, lymphoma, l Local vascular optic neuropathy: malignant hypertension, retinal central venous obstruction, optic disk vasculitis, ocular hypotony , uveitis l Mucopolysaccharidosis
 N 3 -2 -2 Mechanism of the papilledema ( axonal transport blocking ) l. If there was not any normal optic nerve fibers and / or not expedite subarachnoid space along all visual pathway, the papilledema duo to intraorbit, intracanalicular and intracranial compressive diseases will not be occur. l. Because the papilledema is caused by axonal distension of the normal optic nerve fibers, and the transmitting of the pressure is through the subarachnoid space.
N 3 -2 -2 Mechanism of the papilledema ( axonal transport blocking ) l. If there was not any normal optic nerve fibers and / or not expedite subarachnoid space along all visual pathway, the papilledema duo to intraorbit, intracanalicular and intracranial compressive diseases will not be occur. l. Because the papilledema is caused by axonal distension of the normal optic nerve fibers, and the transmitting of the pressure is through the subarachnoid space.
 N 3 -2 -3 Clinical findings l 1 Early type l 2 Decompensated ( Metaphase advanced) type l 3 Late atrophy type
N 3 -2 -3 Clinical findings l 1 Early type l 2 Decompensated ( Metaphase advanced) type l 3 Late atrophy type
 l l l Mechanical signs: Elevation of the optic disk (3 diopters =1 mm) Blurring of the optic disc margins Filling in the physiological cup Edema of the peripapillary nerve fiber layer Retinal and/or choroidal folds l l l Vascular signs: Hyperemia of the optic disc Venous dilation and tortuosity Peripapillary hemorrhages Exudates in the disc or peripapillary area Nerve fiber layer infarctions
l l l Mechanical signs: Elevation of the optic disk (3 diopters =1 mm) Blurring of the optic disc margins Filling in the physiological cup Edema of the peripapillary nerve fiber layer Retinal and/or choroidal folds l l l Vascular signs: Hyperemia of the optic disc Venous dilation and tortuosity Peripapillary hemorrhages Exudates in the disc or peripapillary area Nerve fiber layer infarctions
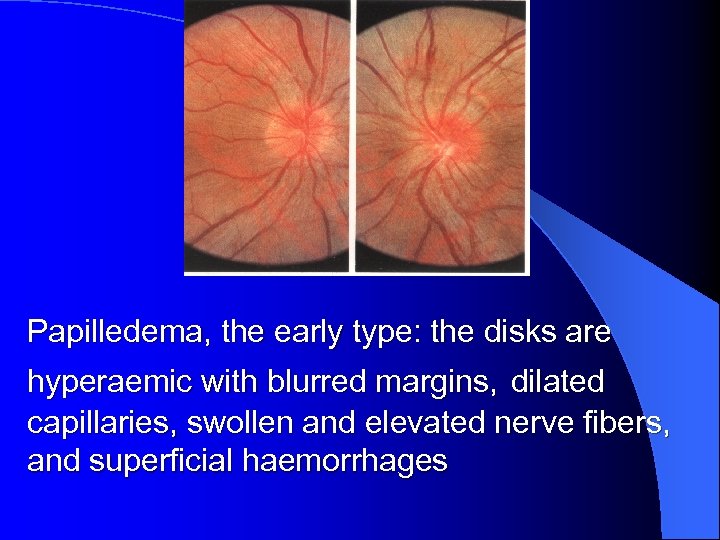 Papilledema, the early type: the disks are hyperaemic with blurred margins, dilated capillaries, swollen and elevated nerve fibers, and superficial haemorrhages
Papilledema, the early type: the disks are hyperaemic with blurred margins, dilated capillaries, swollen and elevated nerve fibers, and superficial haemorrhages
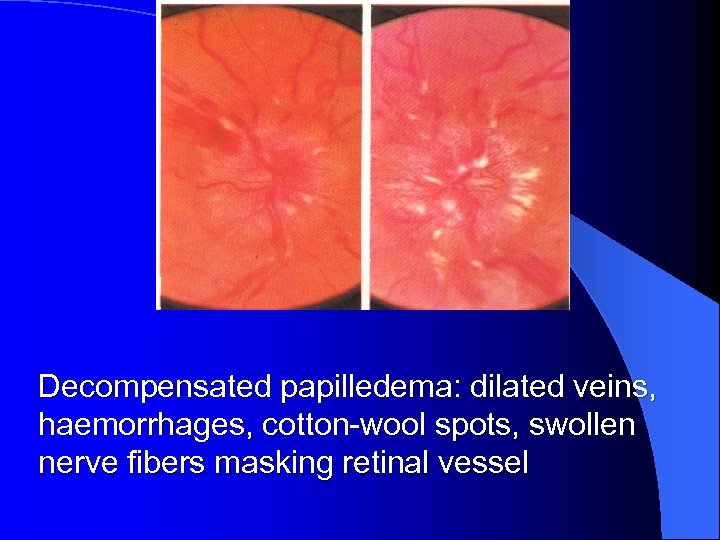 Decompensated papilledema: dilated veins, haemorrhages, cotton-wool spots, swollen nerve fibers masking retinal vessel
Decompensated papilledema: dilated veins, haemorrhages, cotton-wool spots, swollen nerve fibers masking retinal vessel
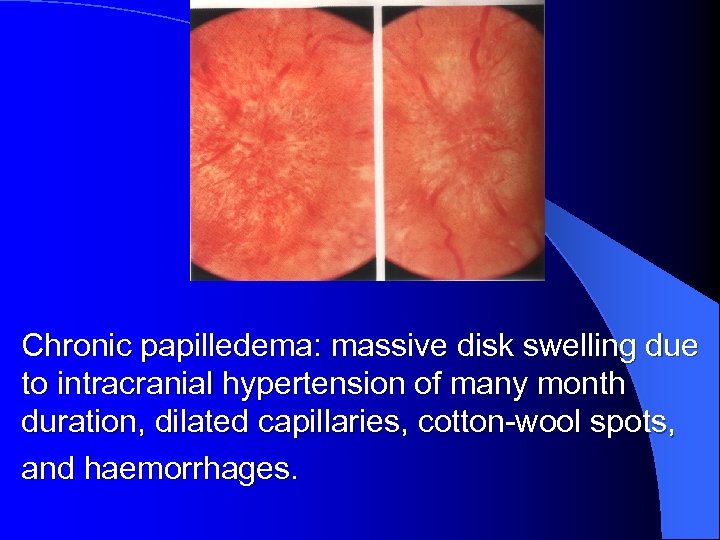 Chronic papilledema: massive disk swelling due to intracranial hypertension of many month duration, dilated capillaries, cotton-wool spots, and haemorrhages.
Chronic papilledema: massive disk swelling due to intracranial hypertension of many month duration, dilated capillaries, cotton-wool spots, and haemorrhages.
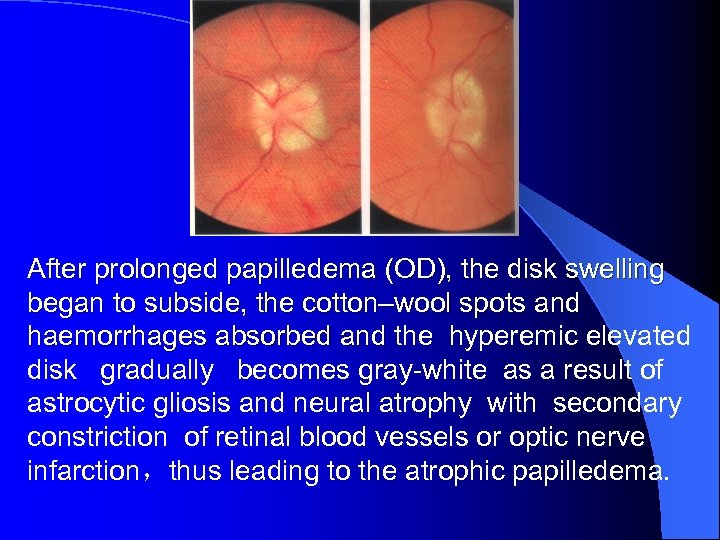 After prolonged papilledema (OD), the disk swelling began to subside, the cotton–wool spots and haemorrhages absorbed and the hyperemic elevated disk gradually becomes gray-white as a result of astrocytic gliosis and neural atrophy with secondary constriction of retinal blood vessels or optic nerve infarction,thus leading to the atrophic papilledema.
After prolonged papilledema (OD), the disk swelling began to subside, the cotton–wool spots and haemorrhages absorbed and the hyperemic elevated disk gradually becomes gray-white as a result of astrocytic gliosis and neural atrophy with secondary constriction of retinal blood vessels or optic nerve infarction,thus leading to the atrophic papilledema.
 N 3 -2 -4 diagnosis and treatment l according to age, history, fundus and l X-radio, CT, MRI, —neuro- imaging l Intracranial mass, l benign cerebral tumor may be appear in early type; l malignant tumor -- decompensated papilledema l Treatment, protection of the optic nerve
N 3 -2 -4 diagnosis and treatment l according to age, history, fundus and l X-radio, CT, MRI, —neuro- imaging l Intracranial mass, l benign cerebral tumor may be appear in early type; l malignant tumor -- decompensated papilledema l Treatment, protection of the optic nerve
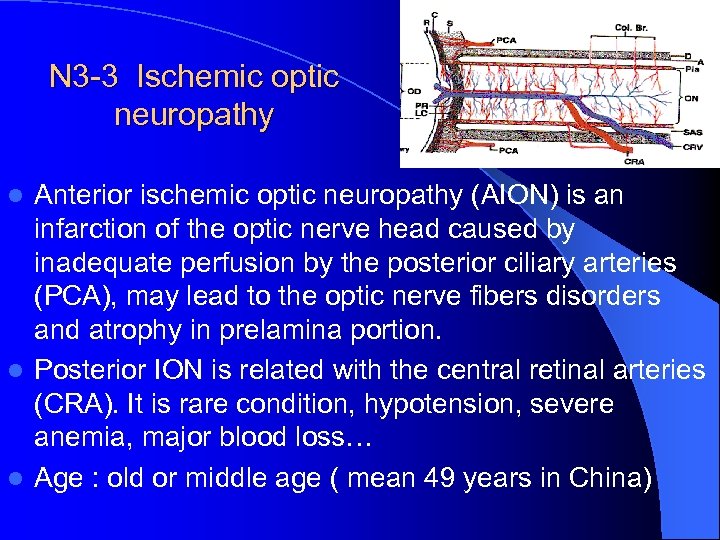 N 3 -3 Ischemic optic neuropathy Anterior ischemic optic neuropathy (AION) is an infarction of the optic nerve head caused by inadequate perfusion by the posterior ciliary arteries (PCA), may lead to the optic nerve fibers disorders and atrophy in prelamina portion. l Posterior ION is related with the central retinal arteries (CRA). It is rare condition, hypotension, severe anemia, major blood loss… l Age : old or middle age ( mean 49 years in China) l
N 3 -3 Ischemic optic neuropathy Anterior ischemic optic neuropathy (AION) is an infarction of the optic nerve head caused by inadequate perfusion by the posterior ciliary arteries (PCA), may lead to the optic nerve fibers disorders and atrophy in prelamina portion. l Posterior ION is related with the central retinal arteries (CRA). It is rare condition, hypotension, severe anemia, major blood loss… l Age : old or middle age ( mean 49 years in China) l
 N 3 -3 -1 ethiology l Arteritic AION, temporal arteritis (occult giant cell arteritis ) is more common in west countries. l Nonarteritic AION is common in China. l The etiology of nonarteritic AION remains unclear. Although vascular risk factors are important, crowding of the optic disc may also be a significant factor.
N 3 -3 -1 ethiology l Arteritic AION, temporal arteritis (occult giant cell arteritis ) is more common in west countries. l Nonarteritic AION is common in China. l The etiology of nonarteritic AION remains unclear. Although vascular risk factors are important, crowding of the optic disc may also be a significant factor.
 N 3 -3 -1 ethiology l An infarction or straitness of the posterior ciliary arteries (PCA) due to hypertension, cardiac disease, arteriosclerosis and diabetes, etc. l Inadequate perfusion of the PCA, the relationship between IOP and perfusion of the PCA that is related with systemic blood pressure. For example systemic hypotony. l The quality of the blood, for example anemia
N 3 -3 -1 ethiology l An infarction or straitness of the posterior ciliary arteries (PCA) due to hypertension, cardiac disease, arteriosclerosis and diabetes, etc. l Inadequate perfusion of the PCA, the relationship between IOP and perfusion of the PCA that is related with systemic blood pressure. For example systemic hypotony. l The quality of the blood, for example anemia
 N 3 -3 -2 pathology l Optic nerve fibers necrosis at anterior or posterior portion of the lamina cribrosa. l In the late, the optic nerve fibers may be disappeared and replaced by astroid fibers. l In arteritic AION, vessels of many organ system including the PCA may be involved, histological examination shows a granulomatous inflammation with epithelioid cells, lymphocytes, giant cell and disruption of the elastic lamina.
N 3 -3 -2 pathology l Optic nerve fibers necrosis at anterior or posterior portion of the lamina cribrosa. l In the late, the optic nerve fibers may be disappeared and replaced by astroid fibers. l In arteritic AION, vessels of many organ system including the PCA may be involved, histological examination shows a granulomatous inflammation with epithelioid cells, lymphocytes, giant cell and disruption of the elastic lamina.
 N 3 -3 -3 Clinical findings l Onset of AION is sudden and usually with both eyes, deterioration may progress over several days or weeks. V. A. is varies from normal to no light perception especially in arteritic AION. l Examination shows an optic disc that is swollen, often with nerve fiber layer hemorrhage. Exudates can occur but are uncommon, it may be shown in FFA that is infarction area of the optic disc.
N 3 -3 -3 Clinical findings l Onset of AION is sudden and usually with both eyes, deterioration may progress over several days or weeks. V. A. is varies from normal to no light perception especially in arteritic AION. l Examination shows an optic disc that is swollen, often with nerve fiber layer hemorrhage. Exudates can occur but are uncommon, it may be shown in FFA that is infarction area of the optic disc.
 l Perimetry: arcuate, nerve fiber bundle defects are typical that occur more common in low part of the V. F. corresponding to infarction area of the optic disc. l In the later stage, the optic nerve atrophy may occur like as glaucomatous damage. l Differentiate from Forster Kennedy syndrome that is papilledema on one side with optic atrophy on the other optic nerve compressed by neoplasm. This is commonly due to maningiomas of olfactory groove
l Perimetry: arcuate, nerve fiber bundle defects are typical that occur more common in low part of the V. F. corresponding to infarction area of the optic disc. l In the later stage, the optic nerve atrophy may occur like as glaucomatous damage. l Differentiate from Forster Kennedy syndrome that is papilledema on one side with optic atrophy on the other optic nerve compressed by neoplasm. This is commonly due to maningiomas of olfactory groove
 N 3 -3 -4 diagnosis (8 -2=6 4? 7? ) ① V. A decreased suddenly, usually with both eyes. ② typical V. F. defect ③ headache, eye pain, temporal artery biopsy in the arteritic AION. ④ FFA in the acute stage shows decreased perfusion of the optic disk often segmental or diffuse in the arteritic form, and disk leakage in the late phase. ⑤ papilledema, but no hyperaemia ⑥ other causes must be eliminated
N 3 -3 -4 diagnosis (8 -2=6 4? 7? ) ① V. A decreased suddenly, usually with both eyes. ② typical V. F. defect ③ headache, eye pain, temporal artery biopsy in the arteritic AION. ④ FFA in the acute stage shows decreased perfusion of the optic disk often segmental or diffuse in the arteritic form, and disk leakage in the late phase. ⑤ papilledema, but no hyperaemia ⑥ other causes must be eliminated
 N 3 -3 -5 treatment l High-dose systemic steroids should be started as soon as a clinical diagnosis of AION. l Lowering IOP may be effect to enhance the blood supply of the posterior ciliary artery l vitamin B 1, B 12, and Chinese herbers. l ethiological treatment: hypertension, arteriorsclerosis, diabetes, etc.
N 3 -3 -5 treatment l High-dose systemic steroids should be started as soon as a clinical diagnosis of AION. l Lowering IOP may be effect to enhance the blood supply of the posterior ciliary artery l vitamin B 1, B 12, and Chinese herbers. l ethiological treatment: hypertension, arteriorsclerosis, diabetes, etc.
 N 3 -4 traumatic optical neuropathy l strong power blunt trauma to the orbit l may lead to severe injury of the optic nerve l vision may be no light perception l Because the intracanalicular optic nerve anchored firmly, as a result, a small mass lesion in the optic canal can produce a compressive optic neuropathy, or due to l fracture of the optic canal and or orbit wall
N 3 -4 traumatic optical neuropathy l strong power blunt trauma to the orbit l may lead to severe injury of the optic nerve l vision may be no light perception l Because the intracanalicular optic nerve anchored firmly, as a result, a small mass lesion in the optic canal can produce a compressive optic neuropathy, or due to l fracture of the optic canal and or orbit wall
 N-3 -5 Lebers hereditary optic neuropathy l N-3 -5 -1 ethiology l Mitochondrial genome (mt DNA ) in 11778 l Nucleotides, mutation of the gene: l guanin (G) becomes adenine (A) guanine (G); adenine (A); thymine (T); cytosine (C) l 340 amino acid: asparagine histidine
N-3 -5 Lebers hereditary optic neuropathy l N-3 -5 -1 ethiology l Mitochondrial genome (mt DNA ) in 11778 l Nucleotides, mutation of the gene: l guanin (G) becomes adenine (A) guanine (G); adenine (A); thymine (T); cytosine (C) l 340 amino acid: asparagine histidine
 N-3 -5 -2 clinical features and treatment l Juvenile (boy or girl), gene transfer by female l Vision blurred, like as “retrobulbar neuritis”, optic nerve may be atrophy or not. l It`s prognosis depends upon novel locus l of the mutation l 11778 ---worst; 11484 best l Treatment : Idebenone 艾地苯锟
N-3 -5 -2 clinical features and treatment l Juvenile (boy or girl), gene transfer by female l Vision blurred, like as “retrobulbar neuritis”, optic nerve may be atrophy or not. l It`s prognosis depends upon novel locus l of the mutation l 11778 ---worst; 11484 best l Treatment : Idebenone 艾地苯锟
 N 3 -6 Optic atrophy l Optic atrophy is a general term used to describe the appearance of an optic disc that has lost its normal complement of healthy fibers. l It is not a clinical diagnosis but a physical finding. l It results from injury to any portion of the primary visual pathway: the retinal ganglion cell, nerve fiber layer, optic nerve, optic chiasm, optic tract, or lateral geniculate nucleus.
N 3 -6 Optic atrophy l Optic atrophy is a general term used to describe the appearance of an optic disc that has lost its normal complement of healthy fibers. l It is not a clinical diagnosis but a physical finding. l It results from injury to any portion of the primary visual pathway: the retinal ganglion cell, nerve fiber layer, optic nerve, optic chiasm, optic tract, or lateral geniculate nucleus.
 N 3 -6 -1 ethiology l It can be produced by inflammation, degeneration, ischemic, compressive, trauma, toxic, demyelinating disorder, and hereditary optic neuropathy. N 3 -6 -2 pathology Optic nerve fibers are degeneration, necrosis and may be disappeared and replaced by astroid fibers.
N 3 -6 -1 ethiology l It can be produced by inflammation, degeneration, ischemic, compressive, trauma, toxic, demyelinating disorder, and hereditary optic neuropathy. N 3 -6 -2 pathology Optic nerve fibers are degeneration, necrosis and may be disappeared and replaced by astroid fibers.
 N 3 -6 -3 clinical findings Visual loss and optic disk pale. l Primary ( descending ) optic atrophy: the fibers lesions occur at the posterior portion of the lamina cribrosa until the lateral geniculate body. l Secondary ( ascending ) optic atrophy: the fibers lesions occur at the anterior portion of the lamina cribrosa, or at the surface layer of the optic disc. l N 3 -6 -4 Diagnosis and treatment
N 3 -6 -3 clinical findings Visual loss and optic disk pale. l Primary ( descending ) optic atrophy: the fibers lesions occur at the posterior portion of the lamina cribrosa until the lateral geniculate body. l Secondary ( ascending ) optic atrophy: the fibers lesions occur at the anterior portion of the lamina cribrosa, or at the surface layer of the optic disc. l N 3 -6 -4 Diagnosis and treatment
 N 3 -7 OPTIC NERVE TUMOR l N 3 -7 -1 glioma of optic nerve l It is a pilocytic astrocytoma with a benign cytologic appearance, or mixed gliomas. l Most cases of optic nerve glioma present in the first decade of life. l About 20% of all childhood orbital tumors are gliomas of the optic nerve. l About 15% of patients with neurofibromatosis have optic nerve glioma.
N 3 -7 OPTIC NERVE TUMOR l N 3 -7 -1 glioma of optic nerve l It is a pilocytic astrocytoma with a benign cytologic appearance, or mixed gliomas. l Most cases of optic nerve glioma present in the first decade of life. l About 20% of all childhood orbital tumors are gliomas of the optic nerve. l About 15% of patients with neurofibromatosis have optic nerve glioma.
 N 3 -7 -1 -1 Clinic findings l Visual loss is the most common initial symptom. It may lead to strabismus and nystagmus. l It may combine with neurofibromatousis l intracranial (50%) and intraorbital (50%). l Proptosis is common symptom of intraorbital tumor. l Fundus: swollen or pale of the optic disk.
N 3 -7 -1 -1 Clinic findings l Visual loss is the most common initial symptom. It may lead to strabismus and nystagmus. l It may combine with neurofibromatousis l intracranial (50%) and intraorbital (50%). l Proptosis is common symptom of intraorbital tumor. l Fundus: swollen or pale of the optic disk.
 Intracranial glioma l Chiasmal gliomas sometimes produce endocrine dysfunction from hypothalamic involvement. l Systemic symptom results from increased intracranial pressure: headache, nausea, vomiting l Neuroimaging shows a characteristic fusiform thickening and kinking of the optic nerve.
Intracranial glioma l Chiasmal gliomas sometimes produce endocrine dysfunction from hypothalamic involvement. l Systemic symptom results from increased intracranial pressure: headache, nausea, vomiting l Neuroimaging shows a characteristic fusiform thickening and kinking of the optic nerve.
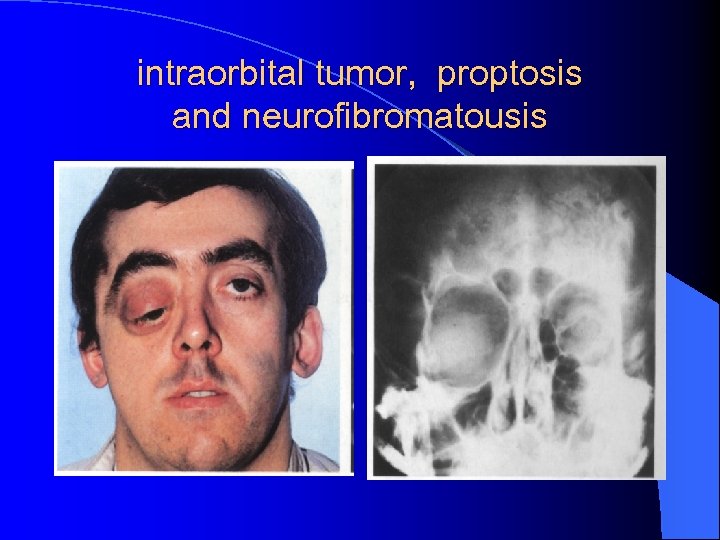 intraorbital tumor, proptosis and neurofibromatousis
intraorbital tumor, proptosis and neurofibromatousis
 N 3 -7 -1 -2 l Most treatment gliomas grow very slowly or cease growing after childhood. So the treatment is controversial. l Surgical therapy is not indicated for orbital optic gliomas unless a cosmetically unacceptable proptosis appears in a blind eye. l when the globe is involved and it is blind eye, the enucleation may be considered. l When the chiasm is involved, the surgical resection is necessary.
N 3 -7 -1 -2 l Most treatment gliomas grow very slowly or cease growing after childhood. So the treatment is controversial. l Surgical therapy is not indicated for orbital optic gliomas unless a cosmetically unacceptable proptosis appears in a blind eye. l when the globe is involved and it is blind eye, the enucleation may be considered. l When the chiasm is involved, the surgical resection is necessary.
 N 3 -7 -2 optic nerve meningioma l Of all meningiomas only about 1% invole the optic nerve. Optic nerve meningiomas make up about 5% of orbital tumors. l It derives from the outer arachnoid or dura, l is benign tumor, but may be malignent in children. l Orbital meningiomas may arise from ectopic nests of meningial cells that then compress the optic nerve from one side.
N 3 -7 -2 optic nerve meningioma l Of all meningiomas only about 1% invole the optic nerve. Optic nerve meningiomas make up about 5% of orbital tumors. l It derives from the outer arachnoid or dura, l is benign tumor, but may be malignent in children. l Orbital meningiomas may arise from ectopic nests of meningial cells that then compress the optic nerve from one side.
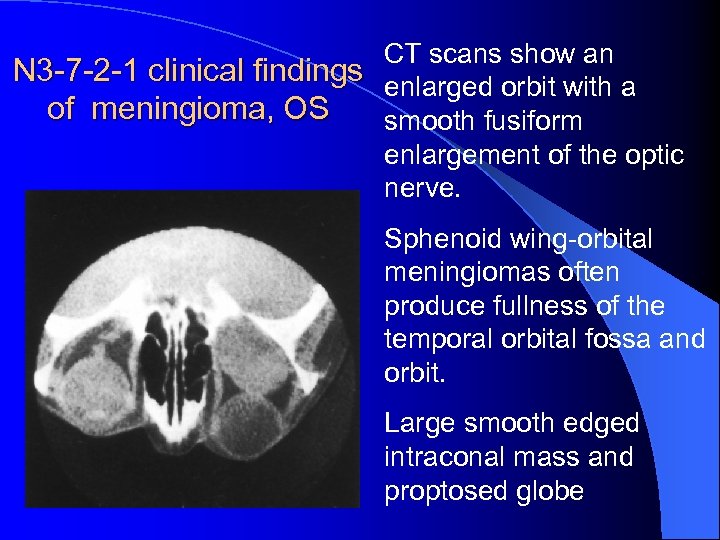 CT scans show an N 3 -7 -2 -1 clinical findings enlarged orbit with a of meningioma, OS smooth fusiform enlargement of the optic nerve. Sphenoid wing-orbital meningiomas often produce fullness of the temporal orbital fossa and orbit. Large smooth edged intraconal mass and proptosed globe
CT scans show an N 3 -7 -2 -1 clinical findings enlarged orbit with a of meningioma, OS smooth fusiform enlargement of the optic nerve. Sphenoid wing-orbital meningiomas often produce fullness of the temporal orbital fossa and orbit. Large smooth edged intraconal mass and proptosed globe
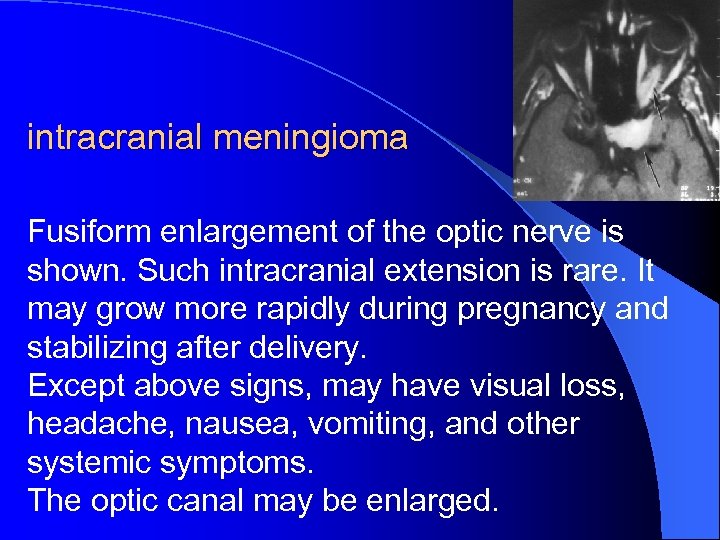 intracranial meningioma Fusiform enlargement of the optic nerve is shown. Such intracranial extension is rare. It may grow more rapidly during pregnancy and stabilizing after delivery. Except above signs, may have visual loss, headache, nausea, vomiting, and other systemic symptoms. The optic canal may be enlarged.
intracranial meningioma Fusiform enlargement of the optic nerve is shown. Such intracranial extension is rare. It may grow more rapidly during pregnancy and stabilizing after delivery. Except above signs, may have visual loss, headache, nausea, vomiting, and other systemic symptoms. The optic canal may be enlarged.
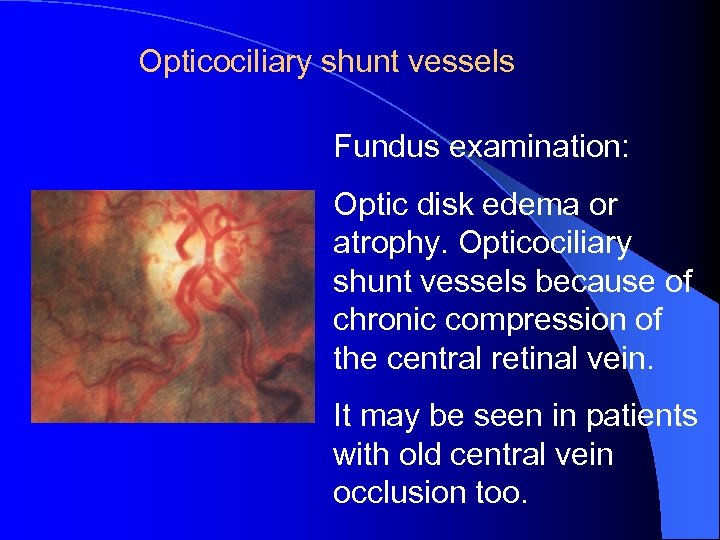 Opticociliary shunt vessels Fundus examination: Optic disk edema or atrophy. Opticociliary shunt vessels because of chronic compression of the central retinal vein. It may be seen in patients with old central vein occlusion too.
Opticociliary shunt vessels Fundus examination: Optic disk edema or atrophy. Opticociliary shunt vessels because of chronic compression of the central retinal vein. It may be seen in patients with old central vein occlusion too.
 N 3 -7 -2 -2 diagnosis l Proptosis, visual loss, chronic papilledema, and opticociliary shunt vessels. l Neuro -imaging: l Fusiform enlargement of the optic nerve, l the orbital enlargement, l and /or the optic canal may be enlarged depends upon the location of the tumor.
N 3 -7 -2 -2 diagnosis l Proptosis, visual loss, chronic papilledema, and opticociliary shunt vessels. l Neuro -imaging: l Fusiform enlargement of the optic nerve, l the orbital enlargement, l and /or the optic canal may be enlarged depends upon the location of the tumor.
 N 3 -7 -2 -3 treatment l Optic nerve meningiomas grow very slowly, but inexorably, and they sometimes lead to blindness. Since it cannot be removed without sacrificing visual acuity, many clinicians think that the lesions should merely be followed unless radiological evidence shows intracranial involvement. l Radiation therapy may be considered.
N 3 -7 -2 -3 treatment l Optic nerve meningiomas grow very slowly, but inexorably, and they sometimes lead to blindness. Since it cannot be removed without sacrificing visual acuity, many clinicians think that the lesions should merely be followed unless radiological evidence shows intracranial involvement. l Radiation therapy may be considered.
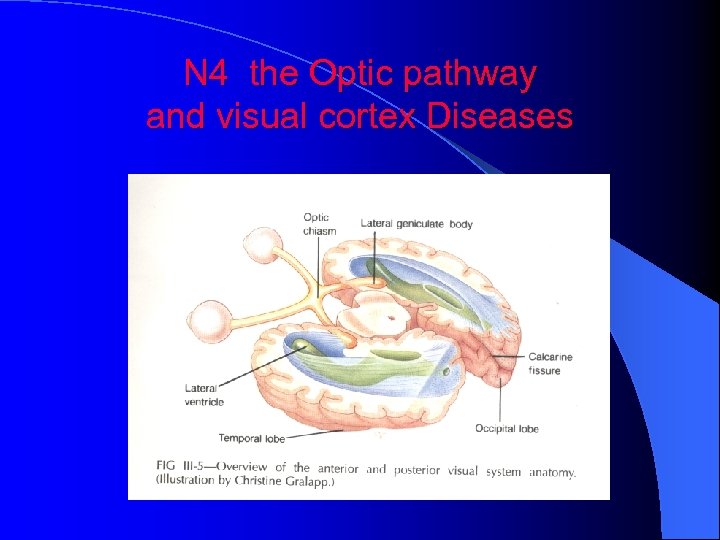 N 4 the Optic pathway and visual cortex Diseases
N 4 the Optic pathway and visual cortex Diseases
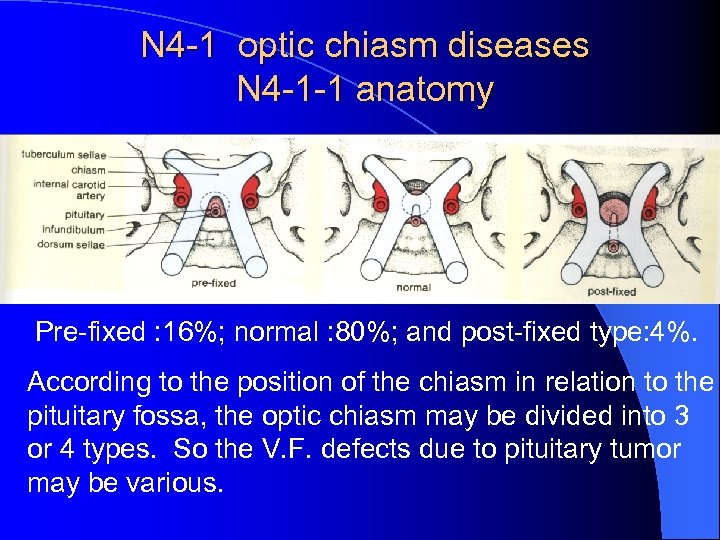 N 4 -1 optic chiasm diseases N 4 -1 -1 anatomy Pre-fixed : 16%; normal : 80%; and post-fixed type: 4%. According to the position of the chiasm in relation to the pituitary fossa, the optic chiasm may be divided into 3 or 4 types. So the V. F. defects due to pituitary tumor may be various.
N 4 -1 optic chiasm diseases N 4 -1 -1 anatomy Pre-fixed : 16%; normal : 80%; and post-fixed type: 4%. According to the position of the chiasm in relation to the pituitary fossa, the optic chiasm may be divided into 3 or 4 types. So the V. F. defects due to pituitary tumor may be various.
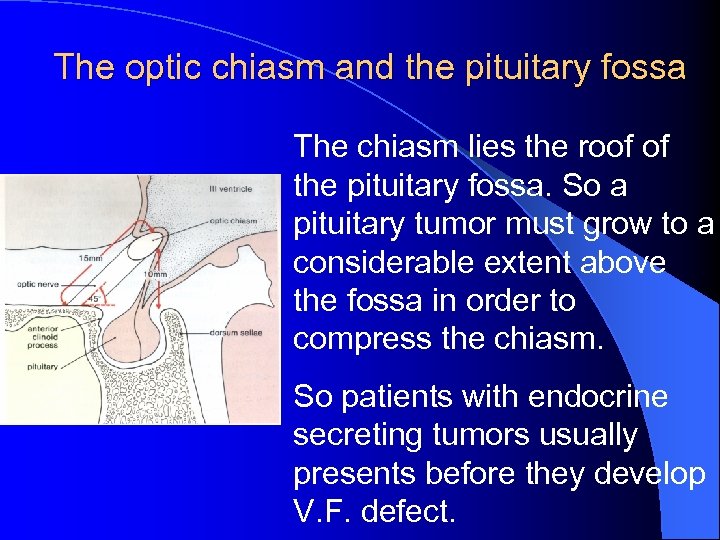 The optic chiasm and the pituitary fossa The chiasm lies the roof of the pituitary fossa. So a pituitary tumor must grow to a considerable extent above the fossa in order to compress the chiasm. So patients with endocrine secreting tumors usually presents before they develop V. F. defect.
The optic chiasm and the pituitary fossa The chiasm lies the roof of the pituitary fossa. So a pituitary tumor must grow to a considerable extent above the fossa in order to compress the chiasm. So patients with endocrine secreting tumors usually presents before they develop V. F. defect.
 Optic chiasm diseases l 1. pituitary adenoma: secreting and nonsecreting tumors that more often present visual loss. Homonymous visual field defects may be absolute or incomplete. l 2. craniopharyngioma, a congenital cyst, may be broken l 3. tuberculum sellae meningioma l 4. blood vessels diseases: aneurysm of the internal carotid or anterior cerebral arteries.
Optic chiasm diseases l 1. pituitary adenoma: secreting and nonsecreting tumors that more often present visual loss. Homonymous visual field defects may be absolute or incomplete. l 2. craniopharyngioma, a congenital cyst, may be broken l 3. tuberculum sellae meningioma l 4. blood vessels diseases: aneurysm of the internal carotid or anterior cerebral arteries.
 (1) Fiber damage at the anterior chiasm (anterior chiasmal syndrome) l Injure one optic nerve at its junction with the optic chiasm cause : l Diminished visual acuity and visual field loss in one eye l accompany a superior temporal defect in the opposite eye ( junctional scotoma )
(1) Fiber damage at the anterior chiasm (anterior chiasmal syndrome) l Injure one optic nerve at its junction with the optic chiasm cause : l Diminished visual acuity and visual field loss in one eye l accompany a superior temporal defect in the opposite eye ( junctional scotoma )
 l (2) Fiber damage in the body of the chiasm It may produce relative or absolute, congruous or incongruous bitemporal hemianopias, often without loss of V. A. l (3) Fiber damage in the posterior chiasm It may destroy primarily posterior, l macular-crossing fibers resulting in bitemporal hemianopic scotomata
l (2) Fiber damage in the body of the chiasm It may produce relative or absolute, congruous or incongruous bitemporal hemianopias, often without loss of V. A. l (3) Fiber damage in the posterior chiasm It may destroy primarily posterior, l macular-crossing fibers resulting in bitemporal hemianopic scotomata
 N 4 -2 Retrochiasmal pathway diseases l Optic Tract diseases l It may produce homonymous V. F. defects (overlapping visual field loss in the temporal field of one eye and the nasal field of the other) l and descending optic nerve atrophy. l V. F. defects from retrochiasmal lesions nearly always respect the vertical midline. l Sellar or suprasellar lesions that expand posteriorly may compress fibers of the optic tract, resulting in a homonymous hemianopia.
N 4 -2 Retrochiasmal pathway diseases l Optic Tract diseases l It may produce homonymous V. F. defects (overlapping visual field loss in the temporal field of one eye and the nasal field of the other) l and descending optic nerve atrophy. l V. F. defects from retrochiasmal lesions nearly always respect the vertical midline. l Sellar or suprasellar lesions that expand posteriorly may compress fibers of the optic tract, resulting in a homonymous hemianopia.
 N 4 -2 -1 Optic tract lesions N 4 -2 -2 Lesions of the LGB N 4 -2 -3 optic radiations diseases l Lesions of the optic radiations in the temporal lobe produce superior homonymous hemianopic visual field defects. l Lesions of the optic radiations in the parietal lobe cause inferior homonymous hemianopic visual field defects. l Internal capsular lesions may be associated with hemiparesis, visual and perceptual difficulty and etc.
N 4 -2 -1 Optic tract lesions N 4 -2 -2 Lesions of the LGB N 4 -2 -3 optic radiations diseases l Lesions of the optic radiations in the temporal lobe produce superior homonymous hemianopic visual field defects. l Lesions of the optic radiations in the parietal lobe cause inferior homonymous hemianopic visual field defects. l Internal capsular lesions may be associated with hemiparesis, visual and perceptual difficulty and etc.
 N 4 -2 -4 occipital cortex diseases l Bilateral homonymous hemianopia with bilateral macular sparing (keyhole field) l Cerebral blindness , also known as cortical blindness, results from bilateral occipital lobe destruction (due to severe toxic or trauma). Optic disk is normal. l Normal pupillary responses may distinguish it from total blindness caused by bilateral prechiasmal lesions.
N 4 -2 -4 occipital cortex diseases l Bilateral homonymous hemianopia with bilateral macular sparing (keyhole field) l Cerebral blindness , also known as cortical blindness, results from bilateral occipital lobe destruction (due to severe toxic or trauma). Optic disk is normal. l Normal pupillary responses may distinguish it from total blindness caused by bilateral prechiasmal lesions.
 Cerebral blindness l The primary optic pathway is defined as until the LGB. any lesion of the primary optic pathway will eventually produce opticatrophy visible upon fundus examination. l But the optic disk is normal in Cerebral blindness. l Macular sparing and macular splitting
Cerebral blindness l The primary optic pathway is defined as until the LGB. any lesion of the primary optic pathway will eventually produce opticatrophy visible upon fundus examination. l But the optic disk is normal in Cerebral blindness. l Macular sparing and macular splitting
 l Macula-sparing homonymous hemianopia: l The portion of the primary visual cortex supplied by the posterior cerebral artery (PCA). l The tip of the occipital lobe receives a dual blood supply from both the middle cerebral artery and the PCA. l After occlusion of the PCA, the primary visual cortex is destroyed, except for the region representing the macula at the posterior tip of the occipital lobe. This region remains perfused by the middle cerebral artery, thus sparing the macula.
l Macula-sparing homonymous hemianopia: l The portion of the primary visual cortex supplied by the posterior cerebral artery (PCA). l The tip of the occipital lobe receives a dual blood supply from both the middle cerebral artery and the PCA. l After occlusion of the PCA, the primary visual cortex is destroyed, except for the region representing the macula at the posterior tip of the occipital lobe. This region remains perfused by the middle cerebral artery, thus sparing the macula.
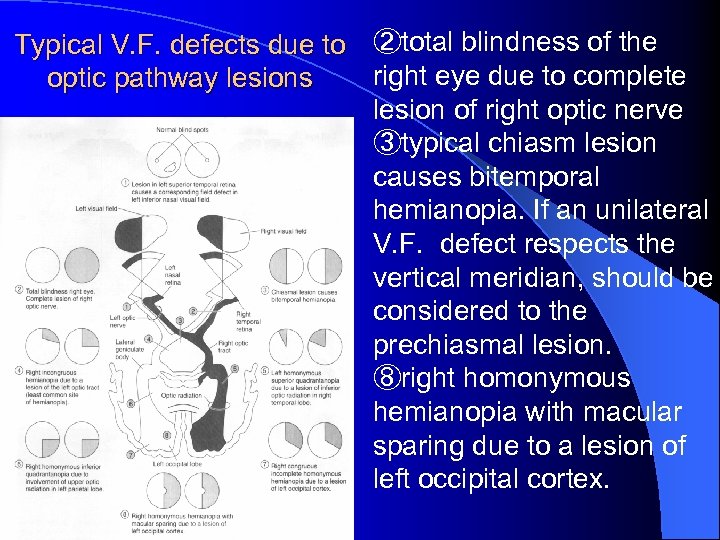 Typical V. F. defects due to ②total blindness of the right eye due to complete optic pathway lesions lesion of right optic nerve ③typical chiasm lesion causes bitemporal hemianopia. If an unilateral V. F. defect respects the vertical meridian, should be considered to the prechiasmal lesion. ⑧right homonymous hemianopia with macular sparing due to a lesion of left occipital cortex.
Typical V. F. defects due to ②total blindness of the right eye due to complete optic pathway lesions lesion of right optic nerve ③typical chiasm lesion causes bitemporal hemianopia. If an unilateral V. F. defect respects the vertical meridian, should be considered to the prechiasmal lesion. ⑧right homonymous hemianopia with macular sparing due to a lesion of left occipital cortex.
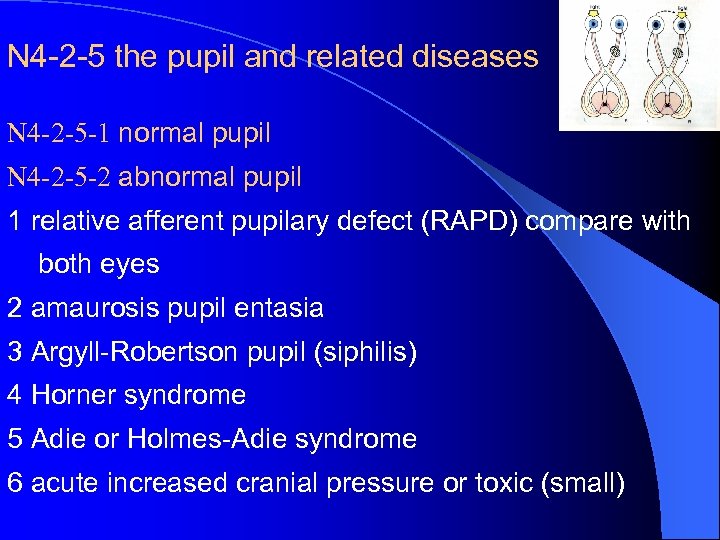 N 4 -2 -5 the pupil and related diseases N 4 -2 -5 -1 normal pupil N 4 -2 -5 -2 abnormal pupil 1 relative afferent pupilary defect (RAPD) compare with both eyes 2 amaurosis pupil entasia 3 Argyll-Robertson pupil (siphilis) 4 Horner syndrome 5 Adie or Holmes-Adie syndrome 6 acute increased cranial pressure or toxic (small)
N 4 -2 -5 the pupil and related diseases N 4 -2 -5 -1 normal pupil N 4 -2 -5 -2 abnormal pupil 1 relative afferent pupilary defect (RAPD) compare with both eyes 2 amaurosis pupil entasia 3 Argyll-Robertson pupil (siphilis) 4 Horner syndrome 5 Adie or Holmes-Adie syndrome 6 acute increased cranial pressure or toxic (small)
 Thank you!
Thank you!


