KappelleTIAdifferentialandmanagement29-3-2012.ppt
- Количество слайдов: 64
 TIA’s differential diagnosis and treatment L. J. Kappelle, University Medical Centre Utrecht, The Netherlands
TIA’s differential diagnosis and treatment L. J. Kappelle, University Medical Centre Utrecht, The Netherlands
 Transient Ischaemic Attack (TIA) clinical diagnosis
Transient Ischaemic Attack (TIA) clinical diagnosis
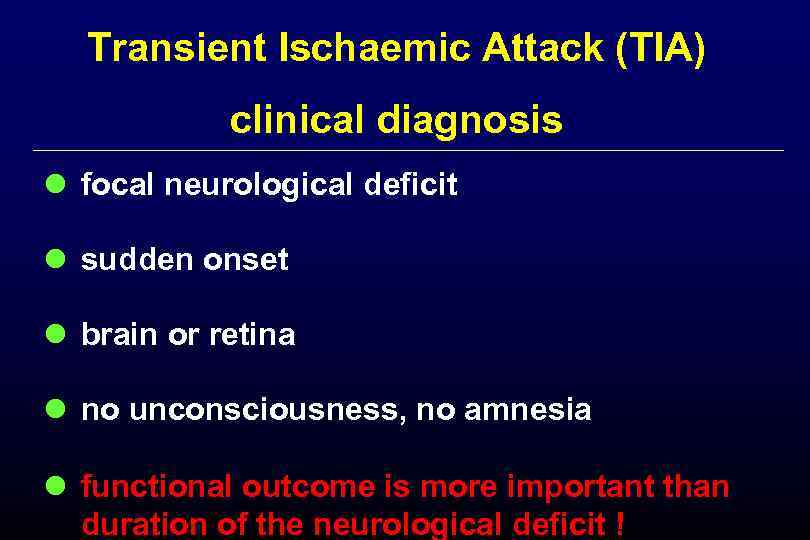 Transient Ischaemic Attack (TIA) clinical diagnosis l focal neurological deficit l sudden onset l brain or retina l no unconsciousness, no amnesia l functional outcome is more important than duration of the neurological deficit !
Transient Ischaemic Attack (TIA) clinical diagnosis l focal neurological deficit l sudden onset l brain or retina l no unconsciousness, no amnesia l functional outcome is more important than duration of the neurological deficit !
 TIA should be considered a serious warning TIA’s 2 1 3 ischaemic stroke
TIA should be considered a serious warning TIA’s 2 1 3 ischaemic stroke
 TIA – a difficult diagnosis l 29% referred by general practitioner did not have a TIA Harbison, Stroke 2003; 34: 71 -6. l 60% of patients, diagnosed at the emergency Prabhakaran, room, did not have a TIA Cerebrovas Dis 2008; 26: 630 -5. l in 11% of patients two neurologists disagreed Koudstaal, Stroke 1986; 17: 723 -8.
TIA – a difficult diagnosis l 29% referred by general practitioner did not have a TIA Harbison, Stroke 2003; 34: 71 -6. l 60% of patients, diagnosed at the emergency Prabhakaran, room, did not have a TIA Cerebrovas Dis 2008; 26: 630 -5. l in 11% of patients two neurologists disagreed Koudstaal, Stroke 1986; 17: 723 -8.

 Transient Ischaemic Attack (TIA) neurological deficit time
Transient Ischaemic Attack (TIA) neurological deficit time
 migraine aura or equivalent neurological deficit time
migraine aura or equivalent neurological deficit time
 epileptic seizure neurological deficit time
epileptic seizure neurological deficit time
 transient neurological deficits l TIA l migraine l epileptic seizure l anxiety, overbreathing l myasthenia gravis l transient global amnesia l. . .
transient neurological deficits l TIA l migraine l epileptic seizure l anxiety, overbreathing l myasthenia gravis l transient global amnesia l. . .
 man, 72 years; sudden onset of numbness in left arm and leg that disappeared after 30 minutes. Neurological exam: normal
man, 72 years; sudden onset of numbness in left arm and leg that disappeared after 30 minutes. Neurological exam: normal
 take home message 1 l the diagnosis of TIA may be difficult; take your time for the history l after the diagnosis of a TIA: make a CT-scan or MRI -scan
take home message 1 l the diagnosis of TIA may be difficult; take your time for the history l after the diagnosis of a TIA: make a CT-scan or MRI -scan
 TIA or minor ischaemic stroke: natural history 40 20
TIA or minor ischaemic stroke: natural history 40 20
 TIA or minor ischaemic stroke: natural history 40 20
TIA or minor ischaemic stroke: natural history 40 20
 early risk of stroke after TIA population base studies with face to face follow up study n/N % (95% CI) 2 days risk 7 days risk Giles, Lancet Neurol 2007; 6: 1063 -72.
early risk of stroke after TIA population base studies with face to face follow up study n/N % (95% CI) 2 days risk 7 days risk Giles, Lancet Neurol 2007; 6: 1063 -72.
 early risk of stroke after TIA population base studies with face to face follow up study n/N % (95% CI) 2 days risk 7 days risk Giles. Lancet Neurol 2007; 6: 1063 -72.
early risk of stroke after TIA population base studies with face to face follow up study n/N % (95% CI) 2 days risk 7 days risk Giles. Lancet Neurol 2007; 6: 1063 -72.
 early risk of stroke after TIA study n/N % (95% CI) 2 days risk 7 days risk Giles. Lancet Neurol 2007; 6: 1063 -72.
early risk of stroke after TIA study n/N % (95% CI) 2 days risk 7 days risk Giles. Lancet Neurol 2007; 6: 1063 -72.
 early risk of stroke after TIA study n/N % (95% CI) 2 days risk 7 days risk Giles, Lancet Neurol 2007; 6: 1063 -72.
early risk of stroke after TIA study n/N % (95% CI) 2 days risk 7 days risk Giles, Lancet Neurol 2007; 6: 1063 -72.
 prognosis after TIA: ABCD 2 score Johnston, Lancet 2007; 369: 283 -92.
prognosis after TIA: ABCD 2 score Johnston, Lancet 2007; 369: 283 -92.
 prognosis after TIA: ABCD 2 score l age ≥ 60 years 1 l blood pressure ≥ 140/90 mm Hg 1 l clinical features: weakness 2 speech l duration : ≥ 60 min 10 – 59 min l diabetes mellitus 1 2 1 1
prognosis after TIA: ABCD 2 score l age ≥ 60 years 1 l blood pressure ≥ 140/90 mm Hg 1 l clinical features: weakness 2 speech l duration : ≥ 60 min 10 – 59 min l diabetes mellitus 1 2 1 1
 prognosis after TIA: ABCD 2 score Johnston, Lancet 2007; 369: 283 -92.
prognosis after TIA: ABCD 2 score Johnston, Lancet 2007; 369: 283 -92.
 take home message 2 l the risk of recurrent stroke after TIA or minor ischaemic stroke is highest during the first week
take home message 2 l the risk of recurrent stroke after TIA or minor ischaemic stroke is highest during the first week
 secondary prevention after TIA or non-disabling ischaemic stroke
secondary prevention after TIA or non-disabling ischaemic stroke
 secondary prevention after TIA or non-disabling ischaemic stroke l antiplatelet therapy l antihypertensive drugs l statin l diet l exercise
secondary prevention after TIA or non-disabling ischaemic stroke l antiplatelet therapy l antihypertensive drugs l statin l diet l exercise
 secondary prevention after TIA or non-disabling ischaemic stroke l antiplatelet therapy Ø reduce the long-term l antihypertensive drugs risk of future stroke l statin with 80% l diet l exercise Hackam, Stroke 2007; 38: 1881 -5.
secondary prevention after TIA or non-disabling ischaemic stroke l antiplatelet therapy Ø reduce the long-term l antihypertensive drugs risk of future stroke l statin with 80% l diet l exercise Hackam, Stroke 2007; 38: 1881 -5.
 antiplatelet regimens that have been tested in patients with TIA and sinus rhythm Hankey, Lancet Neurol 2010; 9: 273 -84.
antiplatelet regimens that have been tested in patients with TIA and sinus rhythm Hankey, Lancet Neurol 2010; 9: 273 -84.
 antiplatelet regimens that have been tested in patients with TIA and sinus rhythm Hankey, Lancet Neurol 2010; 9: 273 -84.
antiplatelet regimens that have been tested in patients with TIA and sinus rhythm Hankey, Lancet Neurol 2010; 9: 273 -84.
 antiplatelet regimen after TIA
antiplatelet regimen after TIA
 risk of early recurrent stroke after TIA or minor stroke according to treatment
risk of early recurrent stroke after TIA or minor stroke according to treatment
 risk of early recurrent stroke after TIA or minor stroke according to treatment Oxvasc : median delay of treatment: 20 days 2004 -2007 : median delay of treatment: 1 day 2002 -2004 Rothwell. Lancet 2007; 370: 1432 -42.
risk of early recurrent stroke after TIA or minor stroke according to treatment Oxvasc : median delay of treatment: 20 days 2004 -2007 : median delay of treatment: 1 day 2002 -2004 Rothwell. Lancet 2007; 370: 1432 -42.
 risk of early recurrent stroke after TIA or minor stroke according to treatment Oxvasc : median delay of treatment: 20 days 2004 -2007 : median delay of treatment: 1 day 2002 -2004 Rothwell. Lancet 2007; 370: 1432 -42.
risk of early recurrent stroke after TIA or minor stroke according to treatment Oxvasc : median delay of treatment: 20 days 2004 -2007 : median delay of treatment: 1 day 2002 -2004 Rothwell. Lancet 2007; 370: 1432 -42.
 early treatment after TIA or minor stroke : median delay of treatment: 20 days 2004 -2007 : median delay of treatment: 8% absolute risk reduction: 1 day 2002 -2004 20 days 1 day Rothwell. Lancet 2007; 370: 1432 -42.
early treatment after TIA or minor stroke : median delay of treatment: 20 days 2004 -2007 : median delay of treatment: 8% absolute risk reduction: 1 day 2002 -2004 20 days 1 day Rothwell. Lancet 2007; 370: 1432 -42.
 take home message 3 l antiplatelet therapy should be started as soon as possible after the diagnosis of TIA
take home message 3 l antiplatelet therapy should be started as soon as possible after the diagnosis of TIA

 modifiable risk factors and relative risk of stroke
modifiable risk factors and relative risk of stroke
 modifiable risk factors and relative risk of stroke Hypertension Cardiac disease* Diabetes mellitus Smoking Elevated cholesterol 0 1 2 3 4 5 6 7 8 9 10 Relative Risk Sacco Stroke 1997; 28: 1507 -17.
modifiable risk factors and relative risk of stroke Hypertension Cardiac disease* Diabetes mellitus Smoking Elevated cholesterol 0 1 2 3 4 5 6 7 8 9 10 Relative Risk Sacco Stroke 1997; 28: 1507 -17.
 hypertension and risk of stroke
hypertension and risk of stroke
 hypertension and risk of stroke
hypertension and risk of stroke
 take home message 4 l management of vascular riskfactors is the most important aspect of secondary prevention after TIA or minor ischaemic stroke
take home message 4 l management of vascular riskfactors is the most important aspect of secondary prevention after TIA or minor ischaemic stroke
 15% of ischaemic stroke occurs in patients with atrial fibrillation
15% of ischaemic stroke occurs in patients with atrial fibrillation


 statine
statine
 Heart Protection Study simvastatine vs. placebo in high-risk individuals Lancet 2002; 360: 7 -22.
Heart Protection Study simvastatine vs. placebo in high-risk individuals Lancet 2002; 360: 7 -22.
 take home message 5 l patients who suffered from a TIA and have atrial fibrillation should be treated with warfarin l patients who suffered from a TIA should be treated with statines, unless cholesterol is < 3. 5 mmol/l
take home message 5 l patients who suffered from a TIA and have atrial fibrillation should be treated with warfarin l patients who suffered from a TIA should be treated with statines, unless cholesterol is < 3. 5 mmol/l
 duplex MR- angiography CT- angiography
duplex MR- angiography CT- angiography

 risk reduction of ipsilateral stroke and peri-operative death as a result of carotid surgery, according to the degree of stenosis % % Rothwell Lancet 2003; 361: 107 -16.
risk reduction of ipsilateral stroke and peri-operative death as a result of carotid surgery, according to the degree of stenosis % % Rothwell Lancet 2003; 361: 107 -16.
 risk reduction of ipsilateral stroke and peri-operative death as a result of carotid surgery, according to the degree of stenosis % % Rothwell Lancet 2003; 361: 107 -16.
risk reduction of ipsilateral stroke and peri-operative death as a result of carotid surgery, according to the degree of stenosis % % Rothwell Lancet 2003; 361: 107 -16.
 risk reduction of carotid surgery versus medical treatment in symptomatic patients with 70 - 99% ICA stenosis 70 -99% stenosis 40 50 -69% stenosis 30 ARR % 20 10 0 - 10 0 -2 2 -4 4 -12 > 12 time from event to randomisation (weeks)
risk reduction of carotid surgery versus medical treatment in symptomatic patients with 70 - 99% ICA stenosis 70 -99% stenosis 40 50 -69% stenosis 30 ARR % 20 10 0 - 10 0 -2 2 -4 4 -12 > 12 time from event to randomisation (weeks)
 risk reduction of carotid surgery versus medical treatment in symptomatic patients with 70 - 99% ICA stenosis 70 -99% stenosis 40 50 -69% stenosis 30 ARR % 20 10 0 - 10 0 -2 2 -4 4 -12 > 12 time from event to randomisation (weeks) Rothwell. Lancet 2004; 363: 915 -24.
risk reduction of carotid surgery versus medical treatment in symptomatic patients with 70 - 99% ICA stenosis 70 -99% stenosis 40 50 -69% stenosis 30 ARR % 20 10 0 - 10 0 -2 2 -4 4 -12 > 12 time from event to randomisation (weeks) Rothwell. Lancet 2004; 363: 915 -24.
 take home message 6 l carotid endarterectomy should be performed in patients with high grade stenosis and should be performed as soon as possible after a TIA or minor ischaemic stroke
take home message 6 l carotid endarterectomy should be performed in patients with high grade stenosis and should be performed as soon as possible after a TIA or minor ischaemic stroke
 management of TIA - conclusions
management of TIA - conclusions
 management of TIA - conclusions l take your time for the history l TIA is an emergency; secondary prevention should start as soon as possible! l management of vascular riskfactors is the most important aspect of secondary prevention l every patient with a TIA in the carotid territory needs to undergo duplex ultrasound examination
management of TIA - conclusions l take your time for the history l TIA is an emergency; secondary prevention should start as soon as possible! l management of vascular riskfactors is the most important aspect of secondary prevention l every patient with a TIA in the carotid territory needs to undergo duplex ultrasound examination

 short-term outcome after stenting versus carotid endarterectomy according to age CEA worse CAS worse Carotid Stenting Trialists’ Collaborators
short-term outcome after stenting versus carotid endarterectomy according to age CEA worse CAS worse Carotid Stenting Trialists’ Collaborators
 short-term outcome after stenting versus carotid endarterectomy according to age CEA worse CAS worse Carotid Stenting Trialists’ Collaborators
short-term outcome after stenting versus carotid endarterectomy according to age CEA worse CAS worse Carotid Stenting Trialists’ Collaborators
 Lancet 2002; 360: 7 -22.
Lancet 2002; 360: 7 -22.
 MRI FLAIR MRI diffusie 0831432
MRI FLAIR MRI diffusie 0831432


 6 -1 x 100% = 83% 6 6 mm. 1 mm.
6 -1 x 100% = 83% 6 6 mm. 1 mm.




