Thyroid Carcinoma Vic V. Vernenkar, D. O. St.

dr.berjis,thyroid_carcinoma.ppt
- Количество слайдов: 39
 Thyroid Carcinoma Vic V. Vernenkar, D.O. St. Barnabas Hospital Department of Surgery
Thyroid Carcinoma Vic V. Vernenkar, D.O. St. Barnabas Hospital Department of Surgery
 Introduction Infrequent cancer -1% of all cancers Benign diseases common 1200 pts die annually Requires multidisciplinary approach
Introduction Infrequent cancer -1% of all cancers Benign diseases common 1200 pts die annually Requires multidisciplinary approach
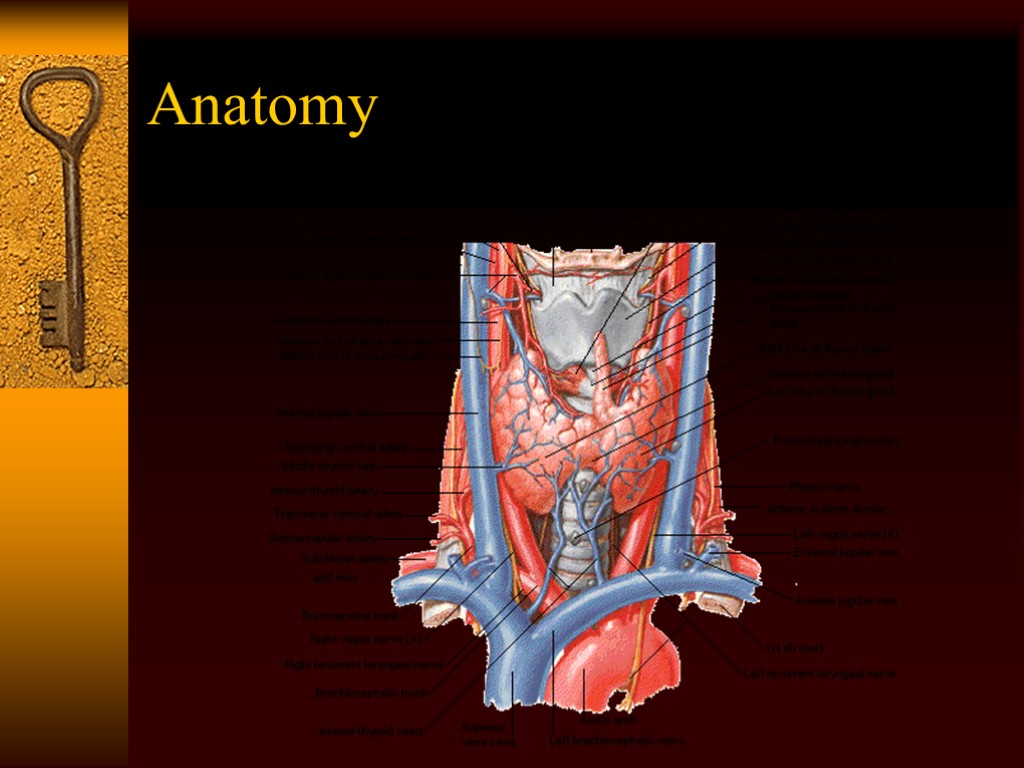
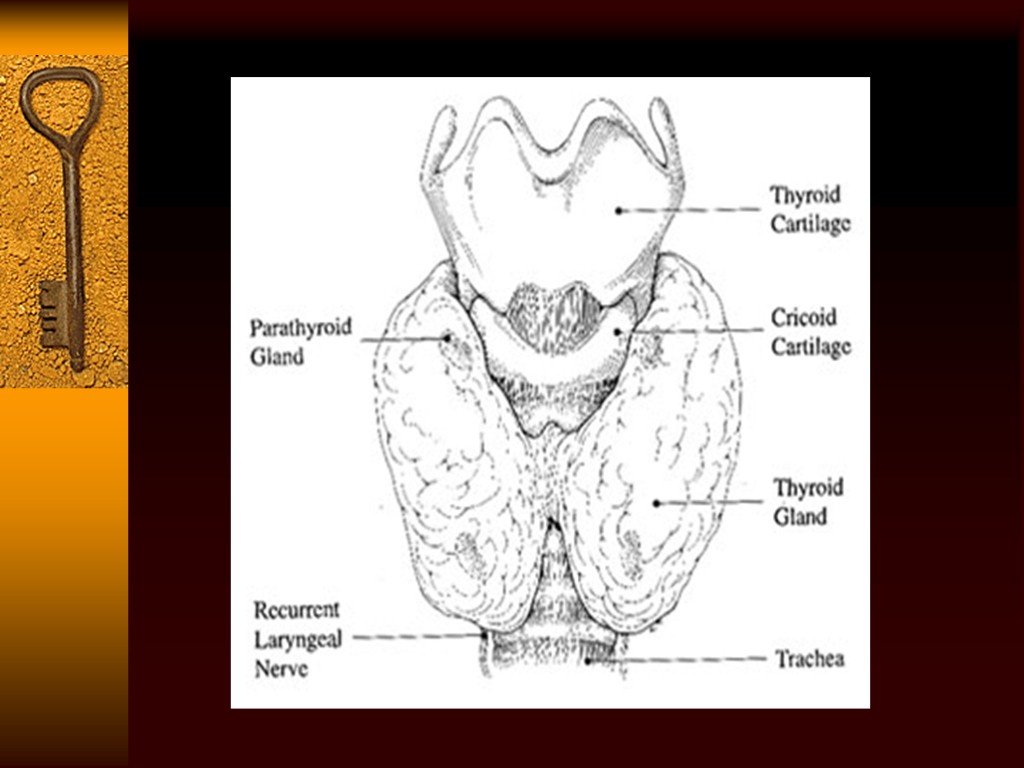
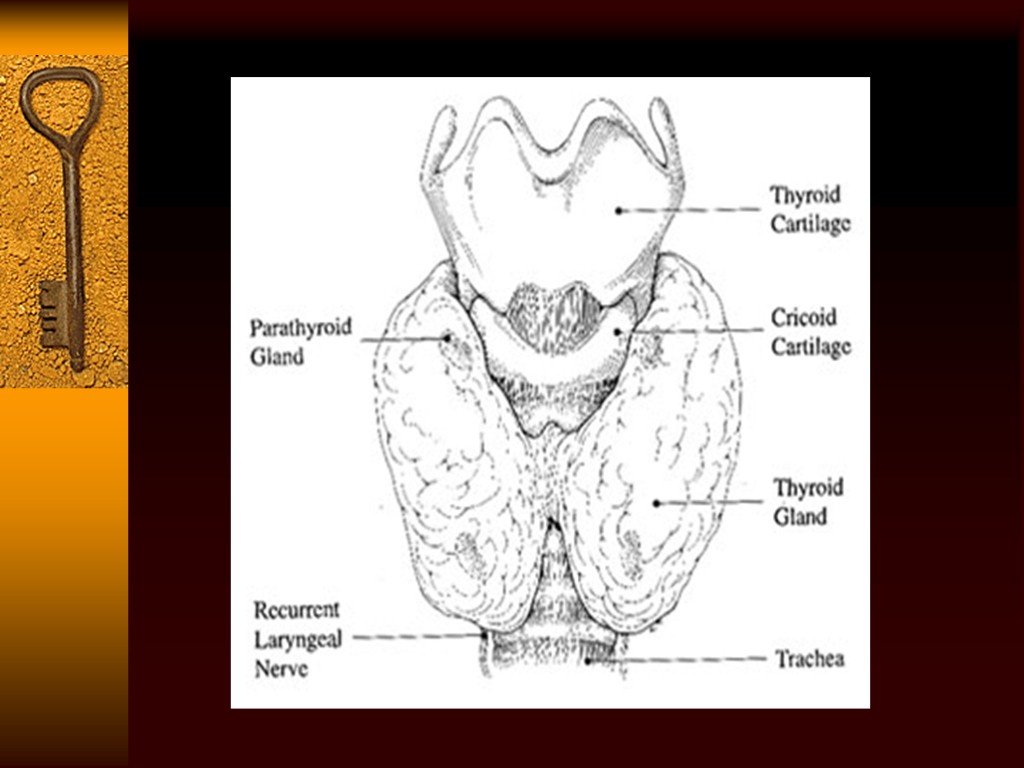
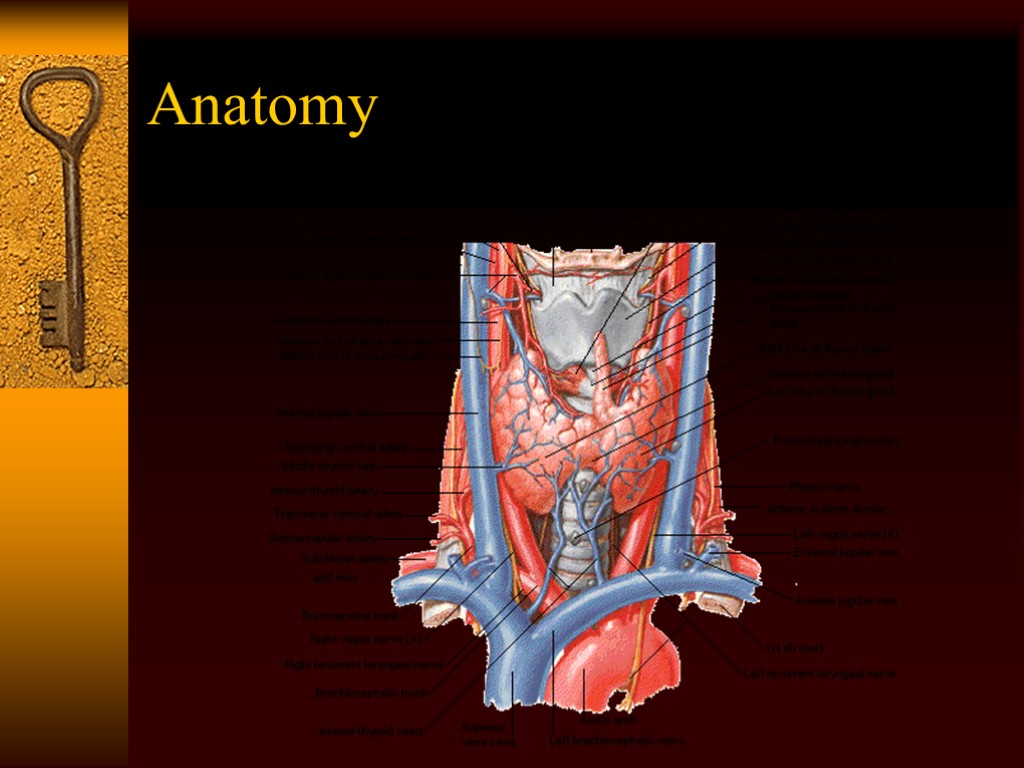 Anatomy
Anatomy
 Frequency 17,000 cases diagnosed annually. Women 3 times more than men. Peak incidence 30-40s. Papillary, follicular, medullary, anaplastic, lymphoma, and sarcoma. Papillary 80%, follicular 10%, medullary 5-10%, anaplastic 1-2%.
Frequency 17,000 cases diagnosed annually. Women 3 times more than men. Peak incidence 30-40s. Papillary, follicular, medullary, anaplastic, lymphoma, and sarcoma. Papillary 80%, follicular 10%, medullary 5-10%, anaplastic 1-2%.
 Etiology/Risk Factors Arise from the two cell types in the gland. Follicular cells make papillary, follicular, and anaplastic. C-cells produce medullary. Radiation exposure (papillary). Populations with low dietary iodine have a higher proportion of follicular and anaplastic cancers.
Etiology/Risk Factors Arise from the two cell types in the gland. Follicular cells make papillary, follicular, and anaplastic. C-cells produce medullary. Radiation exposure (papillary). Populations with low dietary iodine have a higher proportion of follicular and anaplastic cancers.
 History Painless, palpable solitary nodule. Nodules are present in 4-7% of population. Most are benign 5% are malignant Age at presentation (>60 and <30) Sex (males) Rapid growth
History Painless, palpable solitary nodule. Nodules are present in 4-7% of population. Most are benign 5% are malignant Age at presentation (>60 and <30) Sex (males) Rapid growth
 History Malignant nodules usually painless Sudden onset pain usually benign. Hoarseness suggests malignancy, nerve involvement. Dysphagia Heat intolerance, palpitations suggest autonomously functioning nodules. Family history (medullary).
History Malignant nodules usually painless Sudden onset pain usually benign. Hoarseness suggests malignancy, nerve involvement. Dysphagia Heat intolerance, palpitations suggest autonomously functioning nodules. Family history (medullary).
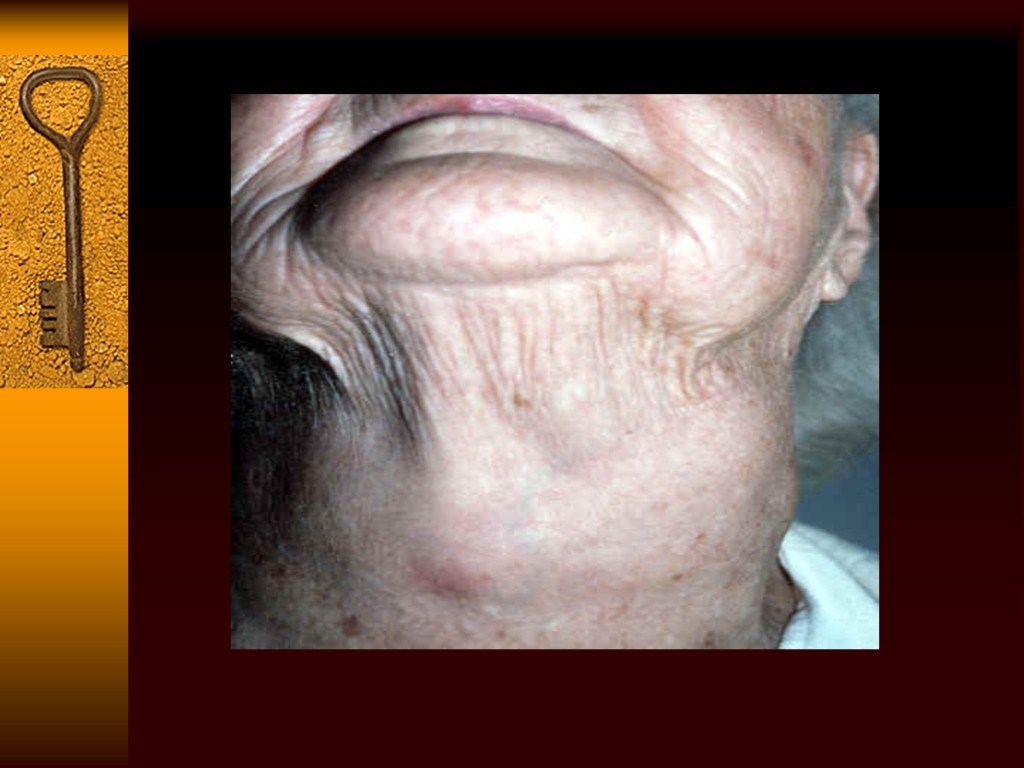
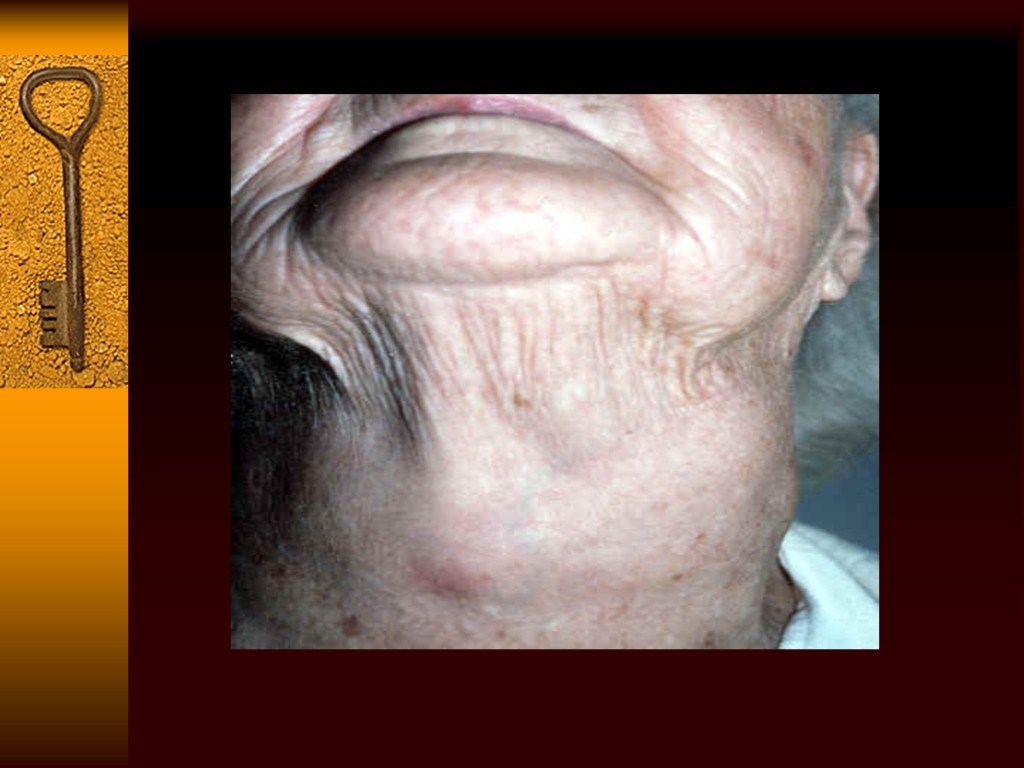
 Physical Exam Thorough HEENT exam includes: Thyroid gland Soft tissues of neck Solid, soft, mobile, or fixed? Tenderness? Laryngoscopy if hoarse preop!
Physical Exam Thorough HEENT exam includes: Thyroid gland Soft tissues of neck Solid, soft, mobile, or fixed? Tenderness? Laryngoscopy if hoarse preop!
 The Goal….. Differentiate malignant from benign. Determine which patients require intervention. Who can be monitored? Avoid unnecessary surgery.
The Goal….. Differentiate malignant from benign. Determine which patients require intervention. Who can be monitored? Avoid unnecessary surgery.
 Fine Needle Aspiration First intervention in evaluation of a nodule. Inexpensive, easy, few complications. Need a good cytopathologist. Four types of results; Benign, malignant,indeterminate, non-diagnostic. 69% benign, 4% malignant, 10% indeterminate, 17% non-diagnostic. Sensitivity 83%, specificity 92% False positive 2.9%, negative 5.2%
Fine Needle Aspiration First intervention in evaluation of a nodule. Inexpensive, easy, few complications. Need a good cytopathologist. Four types of results; Benign, malignant,indeterminate, non-diagnostic. 69% benign, 4% malignant, 10% indeterminate, 17% non-diagnostic. Sensitivity 83%, specificity 92% False positive 2.9%, negative 5.2%
 FNA If non-diagnostic, repeat If malignant go to OR If benign, stop and follow If indeterminate or suspicious OR OK, the path says it’s a “Follicular neoplasm.” FNA can diagnose papillary and medullary cancers Complications of FNA
FNA If non-diagnostic, repeat If malignant go to OR If benign, stop and follow If indeterminate or suspicious OR OK, the path says it’s a “Follicular neoplasm.” FNA can diagnose papillary and medullary cancers Complications of FNA
 Laboratory TSH sensitive for hypo and hyperthyroidism, but does not rule out malignancy. TFTs not indicated in work up initially. Serum thyroglobulin used as tumor marker post op. Calcitonin, for post op monitoring in Medullary cancers.
Laboratory TSH sensitive for hypo and hyperthyroidism, but does not rule out malignancy. TFTs not indicated in work up initially. Serum thyroglobulin used as tumor marker post op. Calcitonin, for post op monitoring in Medullary cancers.
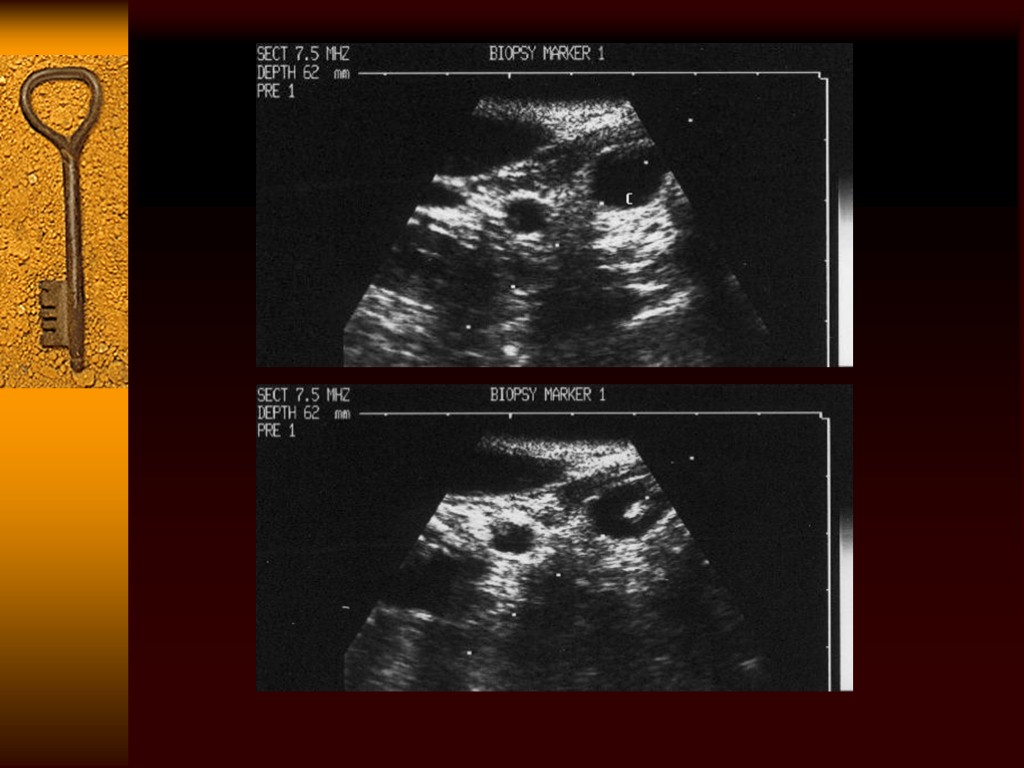
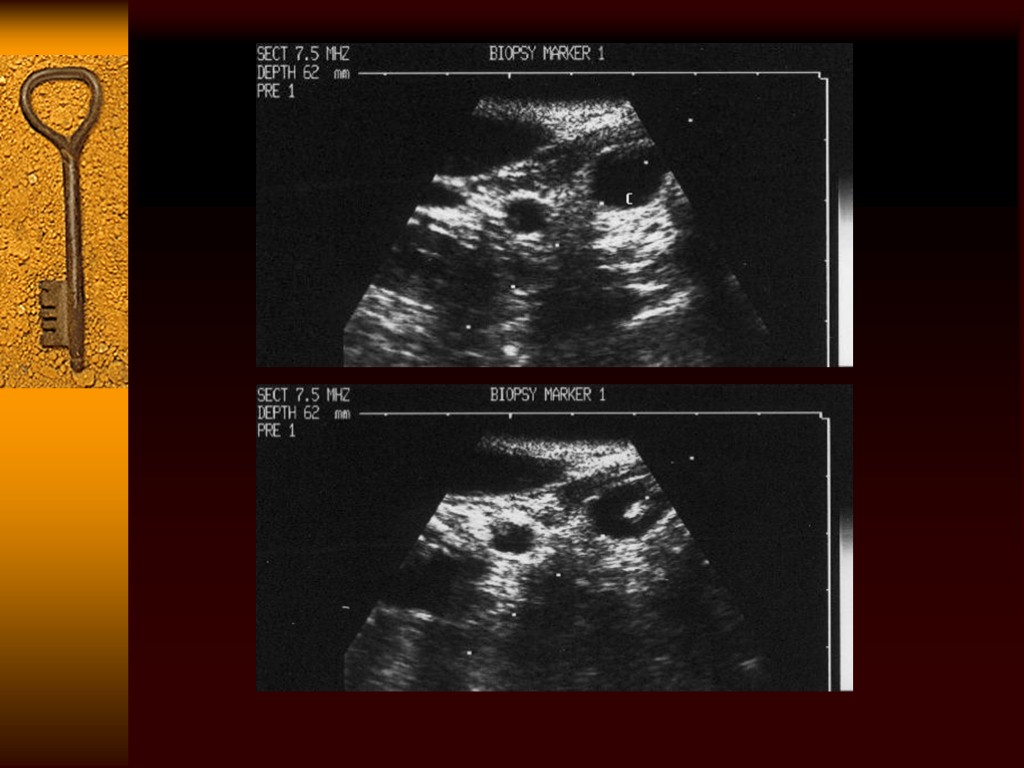
 Imaging Ultrasound: solid vs. Cystic, for FNA accuracy, for monitoring of benign lesions. Scans: determines function of the nodule. Cold nodules are those that don’t take up iodine123, hot ones are the opposite. Carcinoma cannot be ruled out based on scans, with 4% of hot nodules being malignant. May be useful with indeterminate however. CT and MRI not used routinely.
Imaging Ultrasound: solid vs. Cystic, for FNA accuracy, for monitoring of benign lesions. Scans: determines function of the nodule. Cold nodules are those that don’t take up iodine123, hot ones are the opposite. Carcinoma cannot be ruled out based on scans, with 4% of hot nodules being malignant. May be useful with indeterminate however. CT and MRI not used routinely.
 Papillary Carcinoma Most common (80%) Women 3 times more common 30-40 years of age Familial also (FAP) Radiation exposure as a child Patients with Hashimoto’s thyroiditis Slow growing, TSH sensitive, take up iodine, TSH stimulation produces thryroglobulin response.
Papillary Carcinoma Most common (80%) Women 3 times more common 30-40 years of age Familial also (FAP) Radiation exposure as a child Patients with Hashimoto’s thyroiditis Slow growing, TSH sensitive, take up iodine, TSH stimulation produces thryroglobulin response.
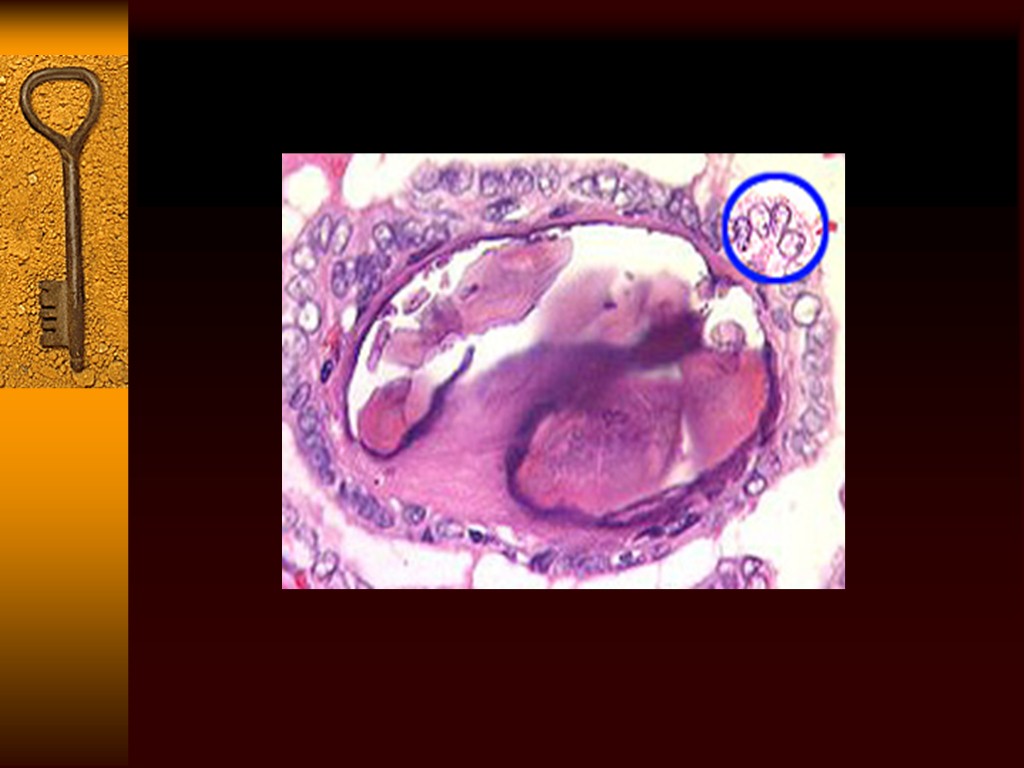
 Papillary Carcinoma Pathology:Unencapsulated, arborizing papillae. Well differentiated, rare mitoses. 50% have psammoma bodies (calcific concretions, circular laminations. Multicentric with tumor present in contralateral lobe as well.
Papillary Carcinoma Pathology:Unencapsulated, arborizing papillae. Well differentiated, rare mitoses. 50% have psammoma bodies (calcific concretions, circular laminations. Multicentric with tumor present in contralateral lobe as well.
 Papillary Carcinoma Local invasion through capsule, invading trachea, nerve, causing dyspnea, hoarseness. Propensity to spread to the cervical lymph nodes. Clinically evident in 1/3 patients. Most commonly central compartment, located medial to carotids, from hyoid to sternal notch. Distant spread to bone, lungs.
Papillary Carcinoma Local invasion through capsule, invading trachea, nerve, causing dyspnea, hoarseness. Propensity to spread to the cervical lymph nodes. Clinically evident in 1/3 patients. Most commonly central compartment, located medial to carotids, from hyoid to sternal notch. Distant spread to bone, lungs.
 Follicular Carcinoma Second most common (10%) Iodine deficient areas 3 times more in women Present more advanced in stage than papillary Late 40’s Also TSH sensitive, takes up iodine, produces thryroglobulin.
Follicular Carcinoma Second most common (10%) Iodine deficient areas 3 times more in women Present more advanced in stage than papillary Late 40’s Also TSH sensitive, takes up iodine, produces thryroglobulin.
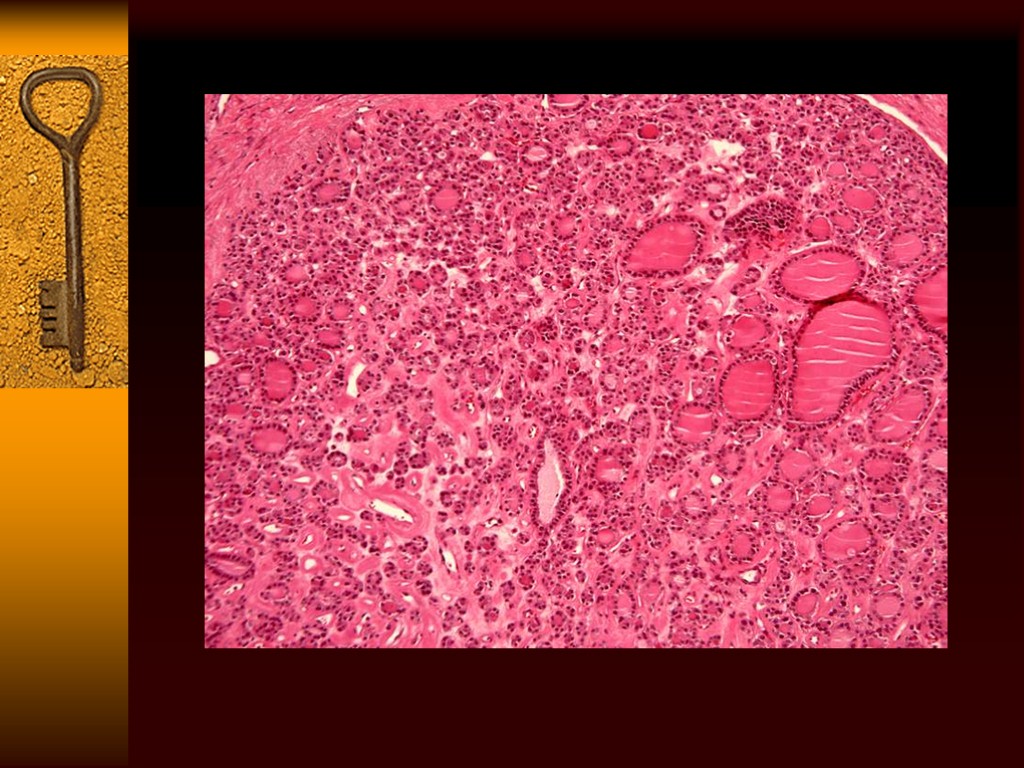
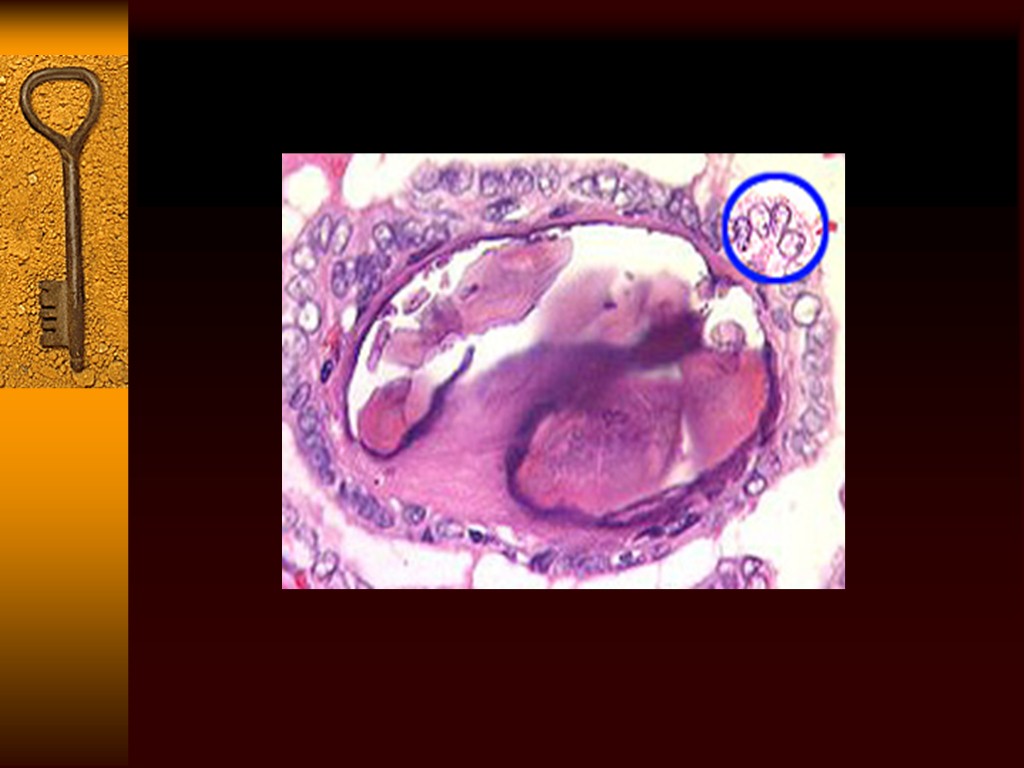
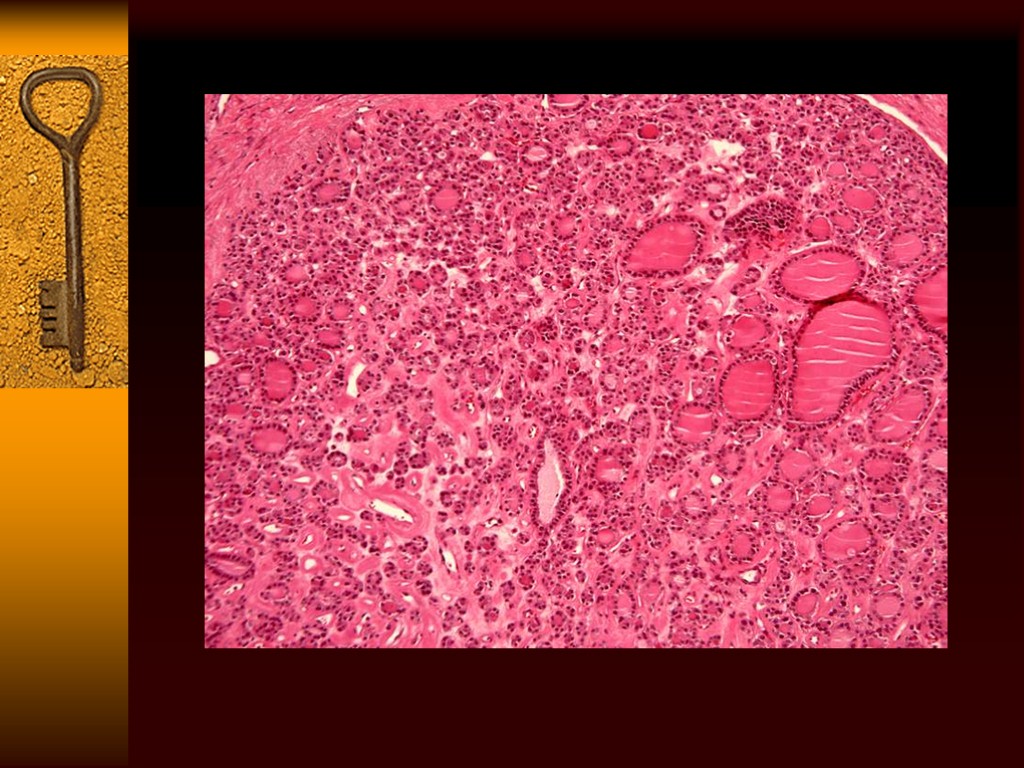
 Follicular Carcinoma Pathology: round, encapsulated, cystic changes, fibrosis, hemorrhages. Microscopically, neoplastic follicular cells. Differentiated from follicular adenomas by the presence of capsule invasion,vascular invasion. Cannot reliably diagnose based on FNA.
Follicular Carcinoma Pathology: round, encapsulated, cystic changes, fibrosis, hemorrhages. Microscopically, neoplastic follicular cells. Differentiated from follicular adenomas by the presence of capsule invasion,vascular invasion. Cannot reliably diagnose based on FNA.
 Follicular Carcinoma Local invasion is similar to papillary cancer with the same presentation. Cervical metastases are uncommon. Distant metastases is significantly higher (20%), with lung and bone most common sites.
Follicular Carcinoma Local invasion is similar to papillary cancer with the same presentation. Cervical metastases are uncommon. Distant metastases is significantly higher (20%), with lung and bone most common sites.
 Treatment and Prognosis Controversy regarding extent of therapy continues. Surgical excision whenever possible. Total thyroidectomy has been mainstay (all apparent thyroid tissue removed). Complications include nerve damage bilaterally, parathyroid injury bilaterally. After, get radioiodine scan, ablation if residual disease or recurrence.
Treatment and Prognosis Controversy regarding extent of therapy continues. Surgical excision whenever possible. Total thyroidectomy has been mainstay (all apparent thyroid tissue removed). Complications include nerve damage bilaterally, parathyroid injury bilaterally. After, get radioiodine scan, ablation if residual disease or recurrence.
 Treatment and Prognosis Over the years, modification to procedure to reduce the above complications. Subtotal thyroidectomy( small portion of thyroid tissue opposite the side of malignancy is left in place) and postop ablation. Thyroid lobectomy and isthmectomy also a viable option with small tumors
Treatment and Prognosis Over the years, modification to procedure to reduce the above complications. Subtotal thyroidectomy( small portion of thyroid tissue opposite the side of malignancy is left in place) and postop ablation. Thyroid lobectomy and isthmectomy also a viable option with small tumors
 Neck Examine the neck prior to surgery to detect lymph node spread. Gross cervical mets should be removed en bloc with a dissection in the compartment in which they reside. Excision of single nodes is not adequate. Elective lymph node dissection is not done, as radioactive iodine takes care of this.
Neck Examine the neck prior to surgery to detect lymph node spread. Gross cervical mets should be removed en bloc with a dissection in the compartment in which they reside. Excision of single nodes is not adequate. Elective lymph node dissection is not done, as radioactive iodine takes care of this.
 Postoperative Radioiodine and Ablation Radioiodine targets residual thyroid tissue and tumor after thyroidectomy. Given in diagnostic doses and therapeutic doses to ablate tissue.
Postoperative Radioiodine and Ablation Radioiodine targets residual thyroid tissue and tumor after thyroidectomy. Given in diagnostic doses and therapeutic doses to ablate tissue.
 Thyroid Suppression Therapy Maintained on thyroxine after surgery and ablation. Low TSH levels reduce tumor growth rates and reduce recurrence rates. Most recommend TSH levels of 0.1 mU/l. Follow-up q 6 months with thyroglobulin levels and repeat scans. Thyroglobulin is good because well differentiated tumors produce it.
Thyroid Suppression Therapy Maintained on thyroxine after surgery and ablation. Low TSH levels reduce tumor growth rates and reduce recurrence rates. Most recommend TSH levels of 0.1 mU/l. Follow-up q 6 months with thyroglobulin levels and repeat scans. Thyroglobulin is good because well differentiated tumors produce it.
 Prognosis Age: at diagnosis. Cancer relate death more common if patient is older than 40 years. Recurrences common in patients diagnosed when they were less than 20 years or older than 60 years. Men are twice more likely as women to die. Tumors greater than 4 cm have higher recurrence, death.
Prognosis Age: at diagnosis. Cancer relate death more common if patient is older than 40 years. Recurrences common in patients diagnosed when they were less than 20 years or older than 60 years. Men are twice more likely as women to die. Tumors greater than 4 cm have higher recurrence, death.
 Prognosis Histology:papillary has 30 year cancer related death rate of 6%. Follicular has a 30 year cancer related death rate of 15%. Local invasion portends poorer prognosis. After surgery, thyroxine is given. Do I scanning after stopping it for 6 weeks, TSH high now. Do scan, if some tissue remains on diagnostic dose, ablate it. Do it again if needed. LN metastases not important for prognosis. Distant metastases associated with a 68.1-fold increase in the rate of disease specific death.
Prognosis Histology:papillary has 30 year cancer related death rate of 6%. Follicular has a 30 year cancer related death rate of 15%. Local invasion portends poorer prognosis. After surgery, thyroxine is given. Do I scanning after stopping it for 6 weeks, TSH high now. Do scan, if some tissue remains on diagnostic dose, ablate it. Do it again if needed. LN metastases not important for prognosis. Distant metastases associated with a 68.1-fold increase in the rate of disease specific death.
 Hurthle Cell A variant of follicular, also known as oncocytic carcinoma. 5 year survival 50%. More common in women than men, presents in 5th decade of life. Same clinical presentation. Cannot diagnose on FNA Does not take up iodine, so treat aggressively. Thyroid suppression and radioiodine don’t work.
Hurthle Cell A variant of follicular, also known as oncocytic carcinoma. 5 year survival 50%. More common in women than men, presents in 5th decade of life. Same clinical presentation. Cannot diagnose on FNA Does not take up iodine, so treat aggressively. Thyroid suppression and radioiodine don’t work.
 Medullary Carcinoma 5%, female preponderance 75% sporadically, 25% familial. Familial cases are usually all over the gland, sporadic usually not multifocal. MEN 2A, MEN2B and FMTC syndromes.
Medullary Carcinoma 5%, female preponderance 75% sporadically, 25% familial. Familial cases are usually all over the gland, sporadic usually not multifocal. MEN 2A, MEN2B and FMTC syndromes.
 Men 2a, 2b, FMTC MEN 2a is Sipple syndrome,MTC, pheochromocytoma, hyperparathyroidism. MEN 2b is MTC, pheo, ganglionomas, marfan habitus. FMTC is just MTC Medullary cancer in these are most aggressive, younger age, rapid growth and metastases. In sporadic you get painless nodule, symptoms of invasion.
Men 2a, 2b, FMTC MEN 2a is Sipple syndrome,MTC, pheochromocytoma, hyperparathyroidism. MEN 2b is MTC, pheo, ganglionomas, marfan habitus. FMTC is just MTC Medullary cancer in these are most aggressive, younger age, rapid growth and metastases. In sporadic you get painless nodule, symptoms of invasion.
 Biochemical Testing Stimulating calcitonin release with IV pentagastrin increases sensitivity of test. First measure baseline calcitonin, then give pentagastrin. Measure calcitonin serially 1.5 and 5 min later. Used as tumor marker postop rather than screening now. Use genetic testing for screening. Histologically test for calcitonin and CEA.
Biochemical Testing Stimulating calcitonin release with IV pentagastrin increases sensitivity of test. First measure baseline calcitonin, then give pentagastrin. Measure calcitonin serially 1.5 and 5 min later. Used as tumor marker postop rather than screening now. Use genetic testing for screening. Histologically test for calcitonin and CEA.
 Treatment Total thyroidectomy Lymph node dissection of level VI. Parathyroid reimplantation if necessary. Lymph node mets are very common. Prophylactic thyroidectomy in children with MEN 2a,b. Surveillance with CEA, calcitonin. Does not take up iodine, so no radioiodine. Prognosis 10 y is 65%.
Treatment Total thyroidectomy Lymph node dissection of level VI. Parathyroid reimplantation if necessary. Lymph node mets are very common. Prophylactic thyroidectomy in children with MEN 2a,b. Surveillance with CEA, calcitonin. Does not take up iodine, so no radioiodine. Prognosis 10 y is 65%.
 Anaplastic Thyroid Carcinoma Bad.
Anaplastic Thyroid Carcinoma Bad.
 Indications for Thyroid Lobectomy Suspicion for malignancy Compressive symptoms Cosmetic issues Well-differentiated thyroid carcinoma in low risk patient (controversial)
Indications for Thyroid Lobectomy Suspicion for malignancy Compressive symptoms Cosmetic issues Well-differentiated thyroid carcinoma in low risk patient (controversial)
 Indications for Total Thyroidectomy Well-differentiated thyroid cancer Medullary thyroid cancer Sarcoma of thyroid Lymphoma of thyroid Obstructive goiter
Indications for Total Thyroidectomy Well-differentiated thyroid cancer Medullary thyroid cancer Sarcoma of thyroid Lymphoma of thyroid Obstructive goiter

