Dr.Berjis,Thyroid Carcinoma.ppt
- Количество слайдов: 39
 Thyroid Carcinoma Vic V. Vernenkar, D. O. St. Barnabas Hospital Department of Surgery
Thyroid Carcinoma Vic V. Vernenkar, D. O. St. Barnabas Hospital Department of Surgery
 Introduction ¨ Infrequent cancer -1% of all cancers ¨ Benign diseases common ¨ 1200 pts die annually ¨ Requires multidisciplinary approach
Introduction ¨ Infrequent cancer -1% of all cancers ¨ Benign diseases common ¨ 1200 pts die annually ¨ Requires multidisciplinary approach
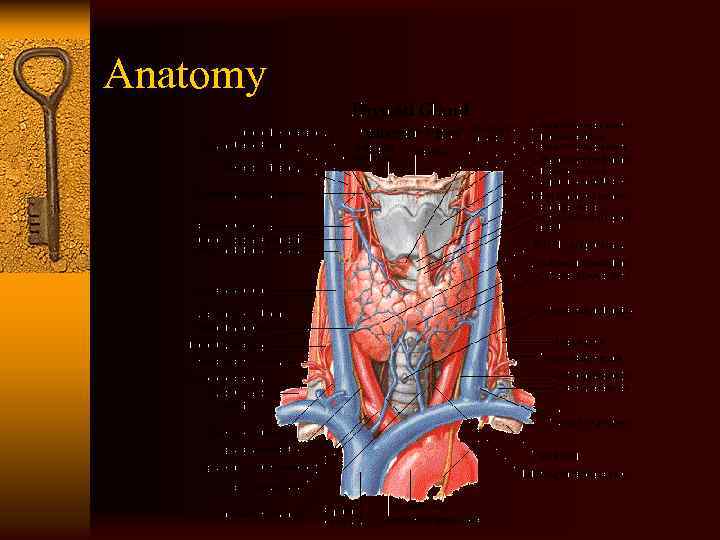 Anatomy
Anatomy

 Frequency ¨ 17, 000 cases diagnosed annually. ¨ Women 3 times more than men. ¨ Peak incidence 30 -40 s. ¨ Papillary, follicular, medullary, anaplastic, lymphoma, and sarcoma. ¨ Papillary 80%, follicular 10%, medullary 510%, anaplastic 1 -2%.
Frequency ¨ 17, 000 cases diagnosed annually. ¨ Women 3 times more than men. ¨ Peak incidence 30 -40 s. ¨ Papillary, follicular, medullary, anaplastic, lymphoma, and sarcoma. ¨ Papillary 80%, follicular 10%, medullary 510%, anaplastic 1 -2%.
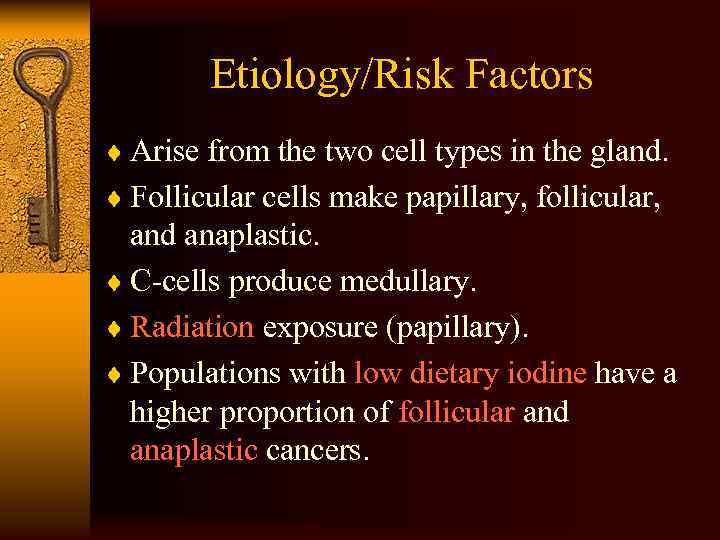 Etiology/Risk Factors ¨ Arise from the two cell types in the gland. ¨ Follicular cells make papillary, follicular, and anaplastic. ¨ C-cells produce medullary. ¨ Radiation exposure (papillary). ¨ Populations with low dietary iodine have a higher proportion of follicular and anaplastic cancers.
Etiology/Risk Factors ¨ Arise from the two cell types in the gland. ¨ Follicular cells make papillary, follicular, and anaplastic. ¨ C-cells produce medullary. ¨ Radiation exposure (papillary). ¨ Populations with low dietary iodine have a higher proportion of follicular and anaplastic cancers.
 History ¨ Painless, palpable solitary nodule. ¨ Nodules are present in 4 -7% of population. ¨ Most are benign ¨ 5% are malignant ¨ Age at presentation (>60 and <30) ¨ Sex (males) ¨ Rapid growth
History ¨ Painless, palpable solitary nodule. ¨ Nodules are present in 4 -7% of population. ¨ Most are benign ¨ 5% are malignant ¨ Age at presentation (>60 and <30) ¨ Sex (males) ¨ Rapid growth
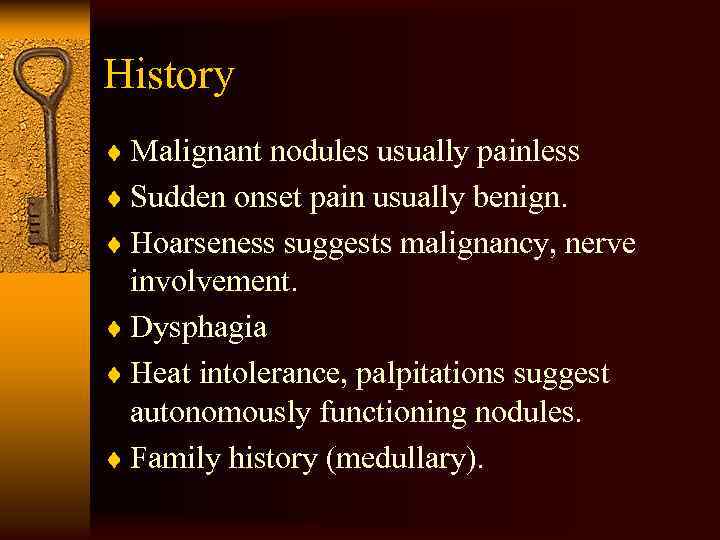 History ¨ Malignant nodules usually painless ¨ Sudden onset pain usually benign. ¨ Hoarseness suggests malignancy, nerve involvement. ¨ Dysphagia ¨ Heat intolerance, palpitations suggest autonomously functioning nodules. ¨ Family history (medullary).
History ¨ Malignant nodules usually painless ¨ Sudden onset pain usually benign. ¨ Hoarseness suggests malignancy, nerve involvement. ¨ Dysphagia ¨ Heat intolerance, palpitations suggest autonomously functioning nodules. ¨ Family history (medullary).
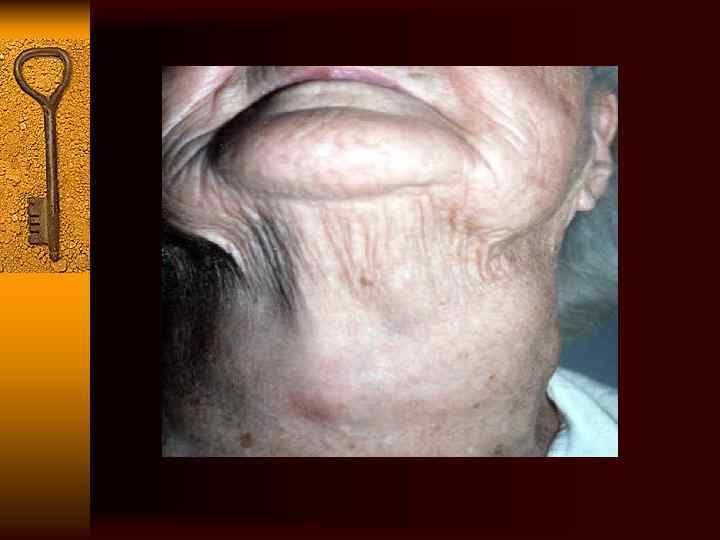
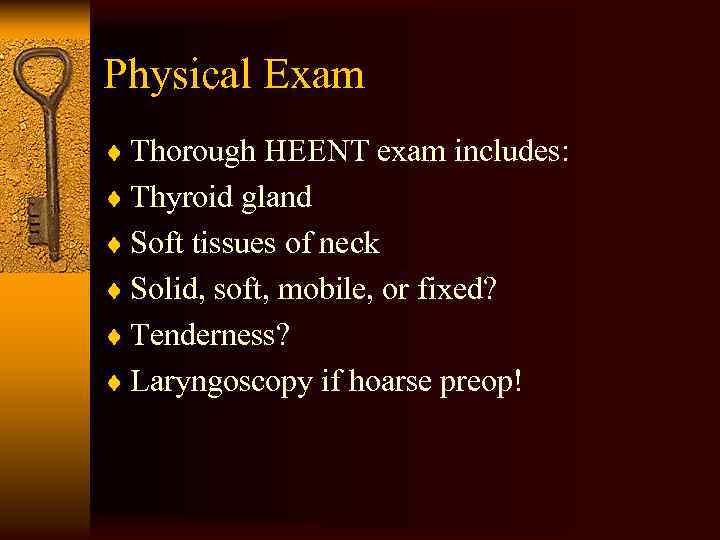 Physical Exam ¨ Thorough HEENT exam includes: ¨ Thyroid gland ¨ Soft tissues of neck ¨ Solid, soft, mobile, or fixed? ¨ Tenderness? ¨ Laryngoscopy if hoarse preop!
Physical Exam ¨ Thorough HEENT exam includes: ¨ Thyroid gland ¨ Soft tissues of neck ¨ Solid, soft, mobile, or fixed? ¨ Tenderness? ¨ Laryngoscopy if hoarse preop!
 The Goal…. . ¨ Differentiate malignant from benign. ¨ Determine which patients require intervention. ¨ Who can be monitored? ¨ Avoid unnecessary surgery.
The Goal…. . ¨ Differentiate malignant from benign. ¨ Determine which patients require intervention. ¨ Who can be monitored? ¨ Avoid unnecessary surgery.
 Fine Needle Aspiration ¨ First intervention in evaluation of a nodule. ¨ Inexpensive, easy, few complications. ¨ Need a good cytopathologist. ¨ Four types of results; Benign, malignant, indeterminate, non-diagnostic. ¨ 69% benign, 4% malignant, 10% indeterminate, 17% non-diagnostic. ¨ Sensitivity 83%, specificity 92% ¨ False positive 2. 9%, negative 5. 2%
Fine Needle Aspiration ¨ First intervention in evaluation of a nodule. ¨ Inexpensive, easy, few complications. ¨ Need a good cytopathologist. ¨ Four types of results; Benign, malignant, indeterminate, non-diagnostic. ¨ 69% benign, 4% malignant, 10% indeterminate, 17% non-diagnostic. ¨ Sensitivity 83%, specificity 92% ¨ False positive 2. 9%, negative 5. 2%
 FNA ¨ If non-diagnostic, repeat ¨ If malignant go to OR ¨ If benign, stop and follow ¨ If indeterminate or suspicious OR ¨ OK, the path says it’s a “Follicular neoplasm. ” ¨ FNA can diagnose papillary and medullary cancers ¨ Complications of FNA
FNA ¨ If non-diagnostic, repeat ¨ If malignant go to OR ¨ If benign, stop and follow ¨ If indeterminate or suspicious OR ¨ OK, the path says it’s a “Follicular neoplasm. ” ¨ FNA can diagnose papillary and medullary cancers ¨ Complications of FNA
 Laboratory ¨ TSH sensitive for hypo and hyperthyroidism, but does not rule out malignancy. ¨ TFTs not indicated in work up initially. ¨ Serum thyroglobulin used as tumor marker post op. ¨ Calcitonin, for post op monitoring in Medullary cancers.
Laboratory ¨ TSH sensitive for hypo and hyperthyroidism, but does not rule out malignancy. ¨ TFTs not indicated in work up initially. ¨ Serum thyroglobulin used as tumor marker post op. ¨ Calcitonin, for post op monitoring in Medullary cancers.
 Imaging ¨ Ultrasound: solid vs. Cystic, for FNA accuracy, for monitoring of benign lesions. ¨ Scans: determines function of the nodule. Cold nodules are those that don’t take up iodine 123, hot ones are the opposite. ¨ Carcinoma cannot be ruled out based on scans, with 4% of hot nodules being malignant. May be useful with indeterminate however. ¨ CT and MRI not used routinely.
Imaging ¨ Ultrasound: solid vs. Cystic, for FNA accuracy, for monitoring of benign lesions. ¨ Scans: determines function of the nodule. Cold nodules are those that don’t take up iodine 123, hot ones are the opposite. ¨ Carcinoma cannot be ruled out based on scans, with 4% of hot nodules being malignant. May be useful with indeterminate however. ¨ CT and MRI not used routinely.

 Papillary Carcinoma ¨ Most common (80%) ¨ Women 3 times more common ¨ 30 -40 years of age ¨ Familial also (FAP) ¨ Radiation exposure as a child ¨ Patients with Hashimoto’s thyroiditis ¨ Slow growing, TSH sensitive, take up iodine, TSH stimulation produces thryroglobulin response.
Papillary Carcinoma ¨ Most common (80%) ¨ Women 3 times more common ¨ 30 -40 years of age ¨ Familial also (FAP) ¨ Radiation exposure as a child ¨ Patients with Hashimoto’s thyroiditis ¨ Slow growing, TSH sensitive, take up iodine, TSH stimulation produces thryroglobulin response.
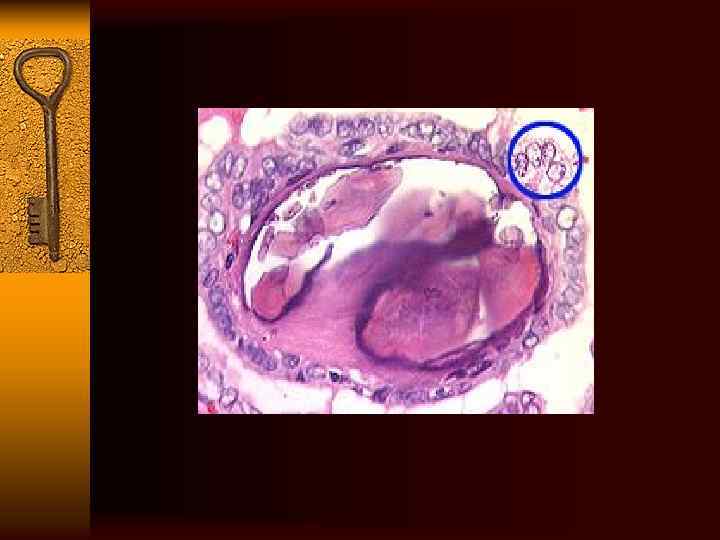
 Papillary Carcinoma ¨ Pathology: Unencapsulated, arborizing papillae. Well differentiated, rare mitoses. ¨ 50% have psammoma bodies (calcific concretions, circular laminations. ¨ Multicentric with tumor present in contralateral lobe as well.
Papillary Carcinoma ¨ Pathology: Unencapsulated, arborizing papillae. Well differentiated, rare mitoses. ¨ 50% have psammoma bodies (calcific concretions, circular laminations. ¨ Multicentric with tumor present in contralateral lobe as well.
 Papillary Carcinoma ¨ Local invasion through capsule, invading trachea, nerve, causing dyspnea, hoarseness. ¨ Propensity to spread to the cervical lymph nodes. Clinically evident in 1/3 patients. Most commonly central compartment, located medial to carotids, from hyoid to sternal notch. ¨ Distant spread to bone, lungs.
Papillary Carcinoma ¨ Local invasion through capsule, invading trachea, nerve, causing dyspnea, hoarseness. ¨ Propensity to spread to the cervical lymph nodes. Clinically evident in 1/3 patients. Most commonly central compartment, located medial to carotids, from hyoid to sternal notch. ¨ Distant spread to bone, lungs.
 Follicular Carcinoma ¨ Second most common (10%) ¨ Iodine deficient areas ¨ 3 times more in women ¨ Present more advanced in stage than papillary ¨ Late 40’s ¨ Also TSH sensitive, takes up iodine, produces thryroglobulin.
Follicular Carcinoma ¨ Second most common (10%) ¨ Iodine deficient areas ¨ 3 times more in women ¨ Present more advanced in stage than papillary ¨ Late 40’s ¨ Also TSH sensitive, takes up iodine, produces thryroglobulin.
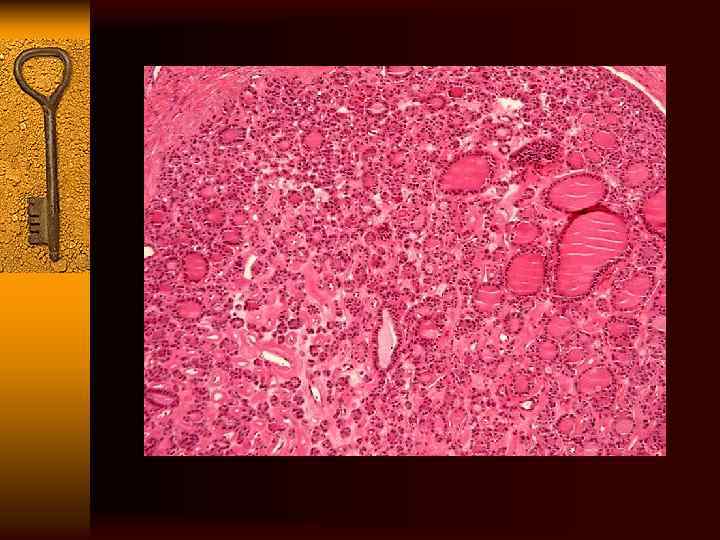
 Follicular Carcinoma ¨ Pathology: round, encapsulated, cystic changes, fibrosis, hemorrhages. Microscopically, neoplastic follicular cells. ¨ Differentiated from follicular adenomas by the presence of capsule invasion, vascular invasion. ¨ Cannot reliably diagnose based on FNA.
Follicular Carcinoma ¨ Pathology: round, encapsulated, cystic changes, fibrosis, hemorrhages. Microscopically, neoplastic follicular cells. ¨ Differentiated from follicular adenomas by the presence of capsule invasion, vascular invasion. ¨ Cannot reliably diagnose based on FNA.
 Follicular Carcinoma ¨ Local invasion is similar to papillary cancer with the same presentation. ¨ Cervical metastases are uncommon. ¨ Distant metastases is significantly higher (20%), with lung and bone most common sites.
Follicular Carcinoma ¨ Local invasion is similar to papillary cancer with the same presentation. ¨ Cervical metastases are uncommon. ¨ Distant metastases is significantly higher (20%), with lung and bone most common sites.
 Treatment and Prognosis ¨ Controversy regarding extent of therapy continues. ¨ Surgical excision whenever possible. ¨ Total thyroidectomy has been mainstay (all apparent thyroid tissue removed). Complications include nerve damage bilaterally, parathyroid injury bilaterally. ¨ After, get radioiodine scan, ablation if residual disease or recurrence.
Treatment and Prognosis ¨ Controversy regarding extent of therapy continues. ¨ Surgical excision whenever possible. ¨ Total thyroidectomy has been mainstay (all apparent thyroid tissue removed). Complications include nerve damage bilaterally, parathyroid injury bilaterally. ¨ After, get radioiodine scan, ablation if residual disease or recurrence.
 Treatment and Prognosis ¨ Over the years, modification to procedure to reduce the above complications. ¨ Subtotal thyroidectomy( small portion of thyroid tissue opposite the side of malignancy is left in place) and postop ablation. ¨ Thyroid lobectomy and isthmectomy also a viable option with small tumors
Treatment and Prognosis ¨ Over the years, modification to procedure to reduce the above complications. ¨ Subtotal thyroidectomy( small portion of thyroid tissue opposite the side of malignancy is left in place) and postop ablation. ¨ Thyroid lobectomy and isthmectomy also a viable option with small tumors
 Neck ¨ Examine the neck prior to surgery to detect lymph node spread. ¨ Gross cervical mets should be removed en bloc with a dissection in the compartment in which they reside. ¨ Excision of single nodes is not adequate. ¨ Elective lymph node dissection is not done, as radioactive iodine takes care of this.
Neck ¨ Examine the neck prior to surgery to detect lymph node spread. ¨ Gross cervical mets should be removed en bloc with a dissection in the compartment in which they reside. ¨ Excision of single nodes is not adequate. ¨ Elective lymph node dissection is not done, as radioactive iodine takes care of this.
 Postoperative Radioiodine and Ablation ¨ Radioiodine targets residual thyroid tissue and tumor after thyroidectomy. ¨ Given in diagnostic doses and therapeutic doses to ablate tissue.
Postoperative Radioiodine and Ablation ¨ Radioiodine targets residual thyroid tissue and tumor after thyroidectomy. ¨ Given in diagnostic doses and therapeutic doses to ablate tissue.
 Thyroid Suppression Therapy ¨ Maintained on thyroxine after surgery and ablation. Low TSH levels reduce tumor growth rates and reduce recurrence rates. ¨ Most recommend TSH levels of 0. 1 m. U/l. ¨ Follow-up q 6 months with thyroglobulin levels and repeat scans. ¨ Thyroglobulin is good because well differentiated tumors produce it.
Thyroid Suppression Therapy ¨ Maintained on thyroxine after surgery and ablation. Low TSH levels reduce tumor growth rates and reduce recurrence rates. ¨ Most recommend TSH levels of 0. 1 m. U/l. ¨ Follow-up q 6 months with thyroglobulin levels and repeat scans. ¨ Thyroglobulin is good because well differentiated tumors produce it.
 Prognosis ¨ Age: at diagnosis. Cancer relate death more common if patient is older than 40 years. ¨ Recurrences common in patients diagnosed when they were less than 20 years or older than 60 years. ¨ Men are twice more likely as women to die. ¨ Tumors greater than 4 cm have higher recurrence, death.
Prognosis ¨ Age: at diagnosis. Cancer relate death more common if patient is older than 40 years. ¨ Recurrences common in patients diagnosed when they were less than 20 years or older than 60 years. ¨ Men are twice more likely as women to die. ¨ Tumors greater than 4 cm have higher recurrence, death.
 Prognosis ¨ Histology: papillary has 30 year cancer related death rate of 6%. Follicular has a 30 year cancer related death rate of 15%. ¨ Local invasion portends poorer prognosis. ¨ After surgery, thyroxine is given. Do I scanning after stopping it for 6 weeks, TSH high now. Do scan, if some tissue remains on diagnostic dose, ablate it. Do it again if needed. ¨ LN metastases not important for prognosis. ¨ Distant metastases associated with a 68. 1 -fold increase in the rate of disease specific death.
Prognosis ¨ Histology: papillary has 30 year cancer related death rate of 6%. Follicular has a 30 year cancer related death rate of 15%. ¨ Local invasion portends poorer prognosis. ¨ After surgery, thyroxine is given. Do I scanning after stopping it for 6 weeks, TSH high now. Do scan, if some tissue remains on diagnostic dose, ablate it. Do it again if needed. ¨ LN metastases not important for prognosis. ¨ Distant metastases associated with a 68. 1 -fold increase in the rate of disease specific death.
 Hurthle Cell ¨ A variant of follicular, also known as oncocytic carcinoma. 5 year survival 50%. ¨ More common in women than men, presents in 5 th decade of life. ¨ Same clinical presentation. ¨ Cannot diagnose on FNA ¨ Does not take up iodine, so treat aggressively. ¨ Thyroid suppression and radioiodine don’t work.
Hurthle Cell ¨ A variant of follicular, also known as oncocytic carcinoma. 5 year survival 50%. ¨ More common in women than men, presents in 5 th decade of life. ¨ Same clinical presentation. ¨ Cannot diagnose on FNA ¨ Does not take up iodine, so treat aggressively. ¨ Thyroid suppression and radioiodine don’t work.
 Medullary Carcinoma ¨ 5%, female preponderance ¨ 75% sporadically, 25% familial. Familial cases are usually all over the gland, sporadic usually not multifocal. ¨ MEN 2 A, MEN 2 B and FMTC syndromes.
Medullary Carcinoma ¨ 5%, female preponderance ¨ 75% sporadically, 25% familial. Familial cases are usually all over the gland, sporadic usually not multifocal. ¨ MEN 2 A, MEN 2 B and FMTC syndromes.
 Men 2 a, 2 b, FMTC ¨ MEN 2 a is Sipple syndrome, MTC, pheochromocytoma, hyperparathyroidism. ¨ MEN 2 b is MTC, pheo, ganglionomas, marfan habitus. ¨ FMTC is just MTC ¨ Medullary cancer in these are most aggressive, younger age, rapid growth and metastases. ¨ In sporadic you get painless nodule, symptoms of invasion.
Men 2 a, 2 b, FMTC ¨ MEN 2 a is Sipple syndrome, MTC, pheochromocytoma, hyperparathyroidism. ¨ MEN 2 b is MTC, pheo, ganglionomas, marfan habitus. ¨ FMTC is just MTC ¨ Medullary cancer in these are most aggressive, younger age, rapid growth and metastases. ¨ In sporadic you get painless nodule, symptoms of invasion.
 Biochemical Testing ¨ Stimulating calcitonin release with IV pentagastrin increases sensitivity of test. ¨ First measure baseline calcitonin, then give pentagastrin. Measure calcitonin serially 1. 5 and 5 min later. ¨ Used as tumor marker postop rather than screening now. ¨ Use genetic testing for screening. ¨ Histologically test for calcitonin and CEA.
Biochemical Testing ¨ Stimulating calcitonin release with IV pentagastrin increases sensitivity of test. ¨ First measure baseline calcitonin, then give pentagastrin. Measure calcitonin serially 1. 5 and 5 min later. ¨ Used as tumor marker postop rather than screening now. ¨ Use genetic testing for screening. ¨ Histologically test for calcitonin and CEA.
 Treatment ¨ Total thyroidectomy ¨ Lymph node dissection of level VI. ¨ Parathyroid reimplantation if necessary. ¨ Lymph node mets are very common. ¨ Prophylactic thyroidectomy in children with MEN 2 a, b. ¨ Surveillance with CEA, calcitonin. ¨ Does not take up iodine, so no radioiodine. ¨ Prognosis 10 y is 65%.
Treatment ¨ Total thyroidectomy ¨ Lymph node dissection of level VI. ¨ Parathyroid reimplantation if necessary. ¨ Lymph node mets are very common. ¨ Prophylactic thyroidectomy in children with MEN 2 a, b. ¨ Surveillance with CEA, calcitonin. ¨ Does not take up iodine, so no radioiodine. ¨ Prognosis 10 y is 65%.
 Anaplastic Thyroid Carcinoma ¨ Bad.
Anaplastic Thyroid Carcinoma ¨ Bad.
 Indications for Thyroid Lobectomy ¨ Suspicion for malignancy ¨ Compressive symptoms ¨ Cosmetic issues ¨ Well-differentiated thyroid carcinoma in low risk patient (controversial)
Indications for Thyroid Lobectomy ¨ Suspicion for malignancy ¨ Compressive symptoms ¨ Cosmetic issues ¨ Well-differentiated thyroid carcinoma in low risk patient (controversial)
 Indications for Total Thyroidectomy ¨ Well-differentiated thyroid cancer ¨ Medullary thyroid cancer ¨ Sarcoma of thyroid ¨ Lymphoma of thyroid ¨ Obstructive goiter
Indications for Total Thyroidectomy ¨ Well-differentiated thyroid cancer ¨ Medullary thyroid cancer ¨ Sarcoma of thyroid ¨ Lymphoma of thyroid ¨ Obstructive goiter


