ff1fe5b6fa7f68ee657ad01ba4b59020.ppt
- Количество слайдов: 72
Thrombolytic Therapy in AMI Overview Dr. Vinod Sharma National Heart Institute New Delhi 1
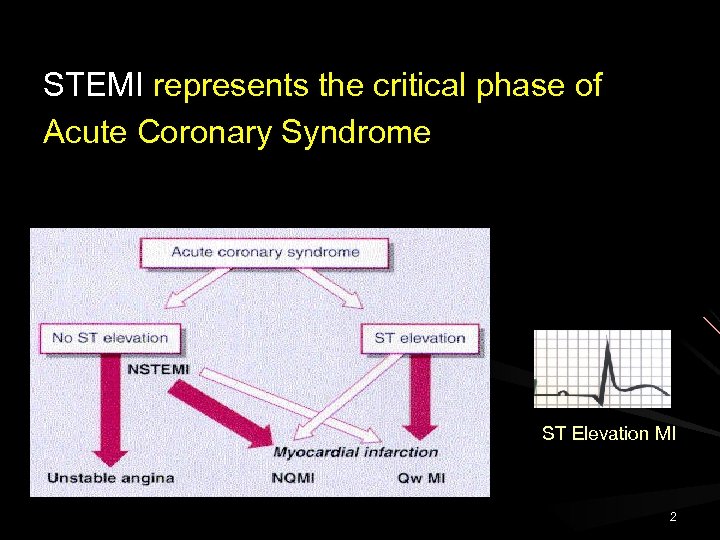
STEMI represents the critical phase of Acute Coronary Syndrome ST Elevation MI 2
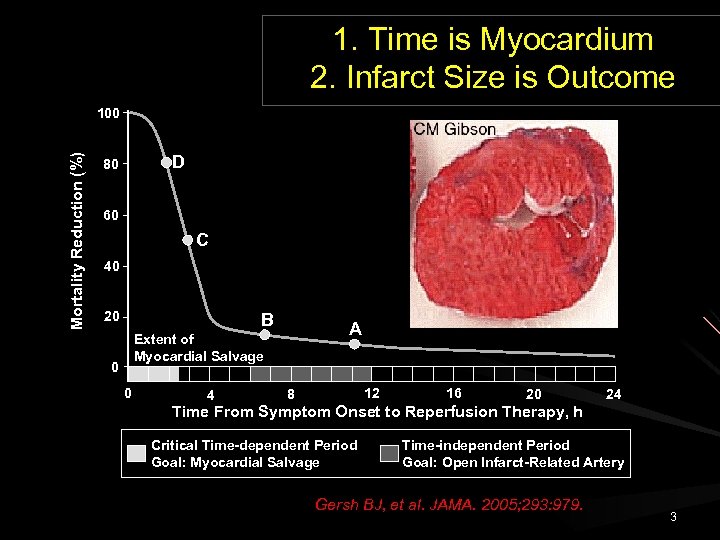
1. Time is Myocardium 2. Infarct Size is Outcome Mortality Reduction (%) 100 D 80 60 C 40 20 B A Extent of Myocardial Salvage 0 0 4 12 8 16 20 Time From Symptom Onset to Reperfusion Therapy, h Critical Time-dependent Period Goal: Myocardial Salvage 24 Time-independent Period Goal: Open Infarct-Related Artery Gersh BJ, et al. JAMA. 2005; 293: 979. 3
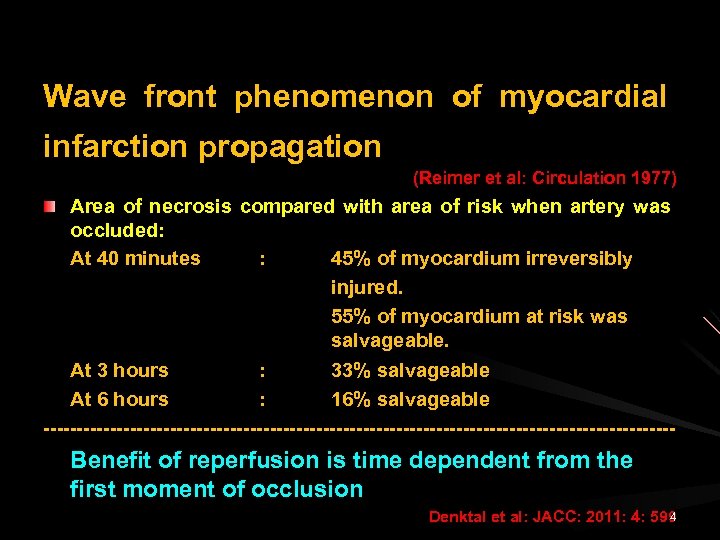
Wave front phenomenon of myocardial infarction propagation (Reimer et al: Circulation 1977) Area of necrosis compared with area of risk when artery was occluded: At 40 minutes : 45% of myocardium irreversibly injured. 55% of myocardium at risk was salvageable. t 3 hours At 3 hours : 33% salvageable A At 6 hours : 16% salvageable ------------------------------------------------ Benefit of reperfusion is time dependent from the first moment of occlusion 4 Denktal et al: JACC: 2011: 4: 599
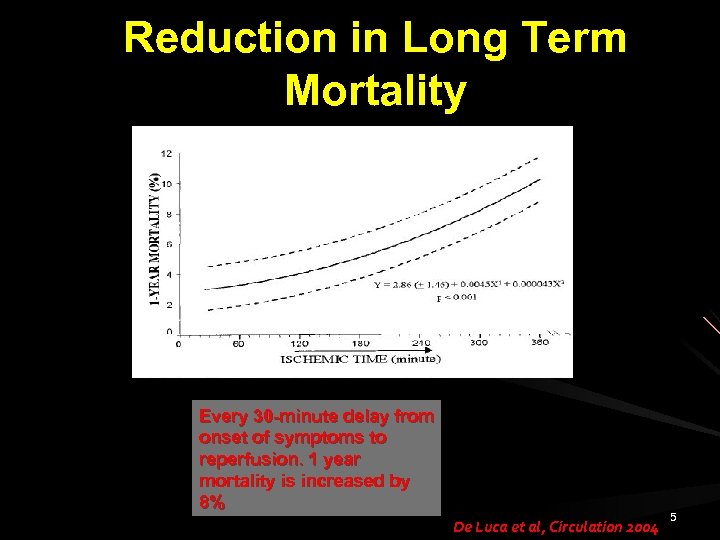
Reduction in Long Term Mortality Every 30 -minute delay from onset of symptoms to reperfusion. 1 year mortality is increased by 8% De Luca et al, Circulation 2004 5
Reperfusion is the key to save myocardium and life…. Aim is to open the blocked I. R. A. and Re -establish the coronary blood flow Rapid Early Complete Sustained 6
Reperfusion Strategy in Acute STEMI Thrombolysis Primary Angioplasty Pharmaco-invasive strategy 7

8
Thrombolytic Therapy in STEMI Streptokinase 1933 William Smith Tillett 1958 Sol Sherry Changed the focus from “palliation” to “cure” in AMI 9
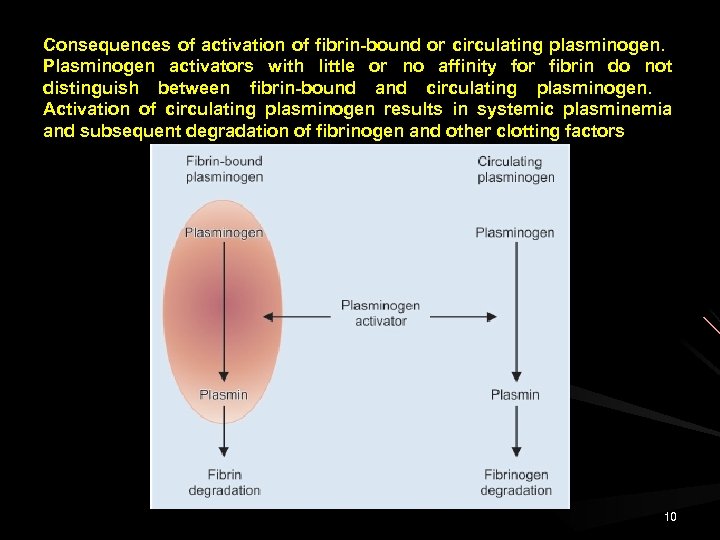
Consequences of activation of fibrin-bound or circulating plasminogen. Plasminogen activators with little or no affinity for fibrin do not distinguish between fibrin-bound and circulating plasminogen. Activation of circulating plasminogen results in systemic plasminemia and subsequent degradation of fibrinogen and other clotting factors 10
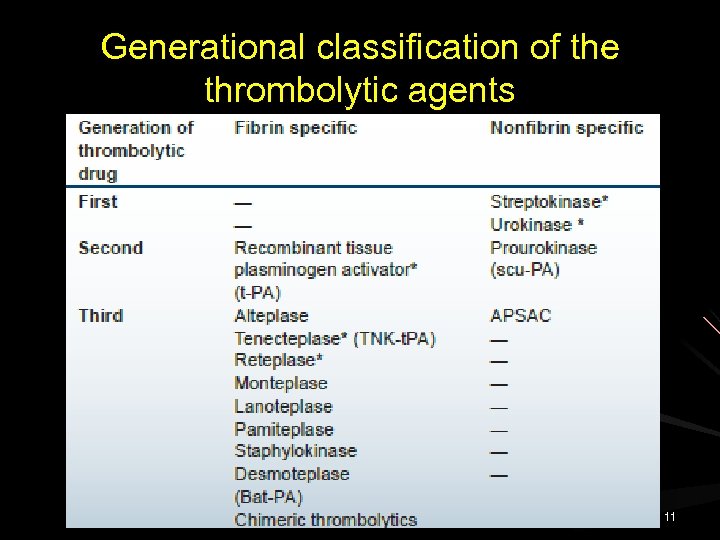
Generational classification of the thrombolytic agents 11
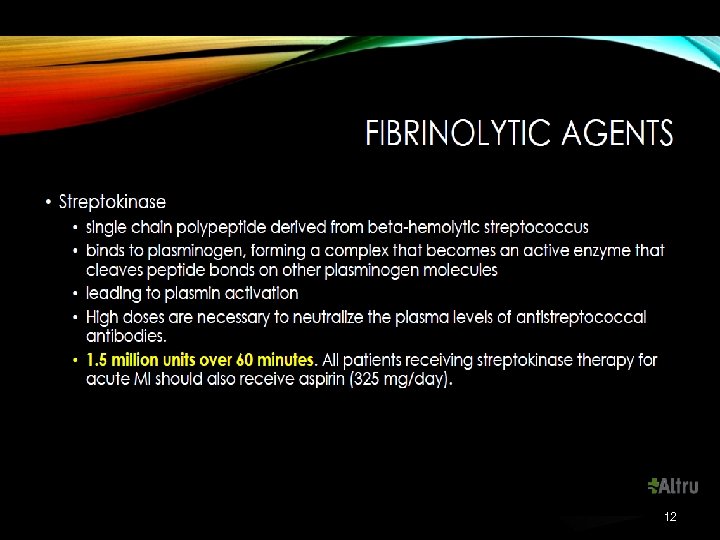
12
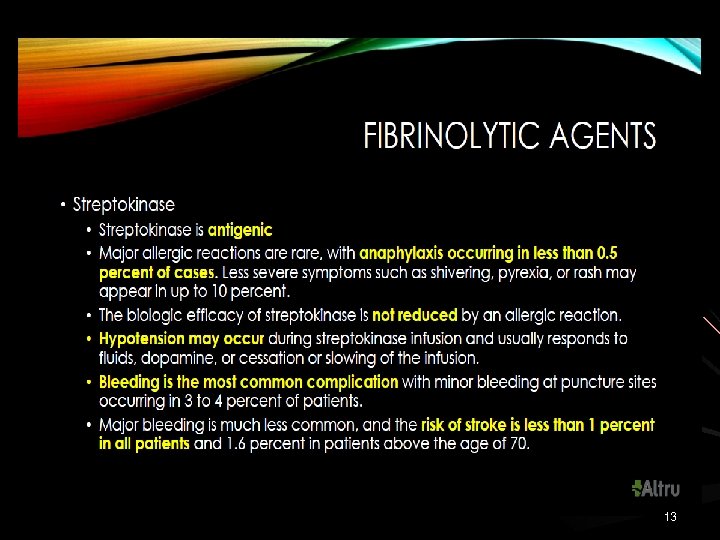
13
STEMI Care in India & the Real World: Challenges Ahead In a registry involving 50 cities, only 58. 5% of patients with STEMI were thrombolysed mostly with Streptokinase and a minority received percutaneous coronary intervention (PCI). 14
15
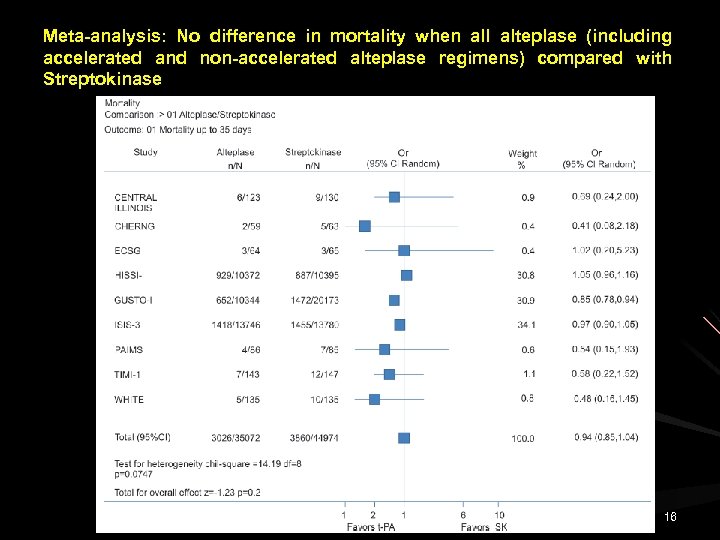
Meta-analysis: No difference in mortality when all alteplase (including accelerated and non-accelerated alteplase regimens) compared with Streptokinase 16
Reteplase A single chain, nonglycosylated peptide fibrin specific recombinant plasminogen activator derived from t-PA It is preferentially active fibrin bound plasminogen rather than fluid phase plasminogen indicating fibrin selectivity. __________________________ Bolus administration of Reteplase results in rapid reperfusion requiring significantly shorter time to reperfusion compared to Alteplase, Streptokinase & Urokinase. 17
(1995) International Joint Efficacy Comparison of Thrombolytics. Randomised, double-blind comparison of reteplase double bolus administration with streptokinase in acute myocardial infarction (INJECT): trial to investigate equivalence. Lancet 346: 329336. 18
INJECT Trial Reteplase double dose (10 U + 10 U n = 2695) was compared with standard dose of STK (1. 5 million over 60 months) Reteplase was as effective as STK in reducing mortality risk [Mortality at 35 days – 9% Vs 9. 5% (STK) (Reteplase)] 19
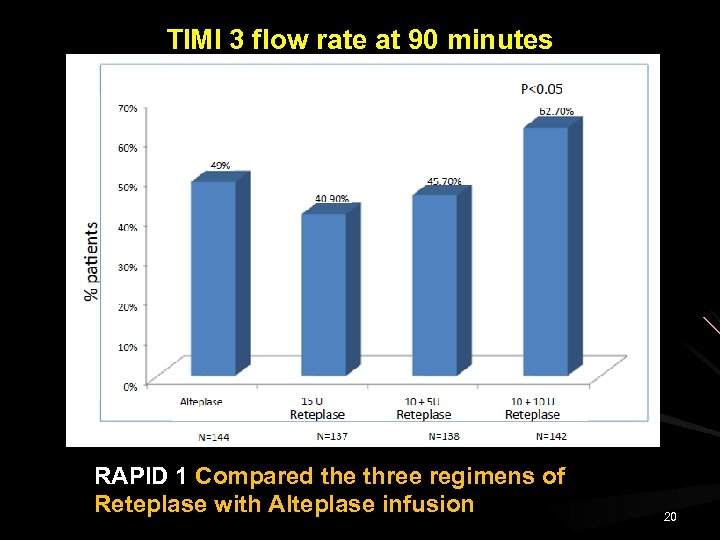
TIMI 3 flow rate at 90 minutes RAPID 1 Compared the three regimens of Reteplase with Alteplase infusion 20
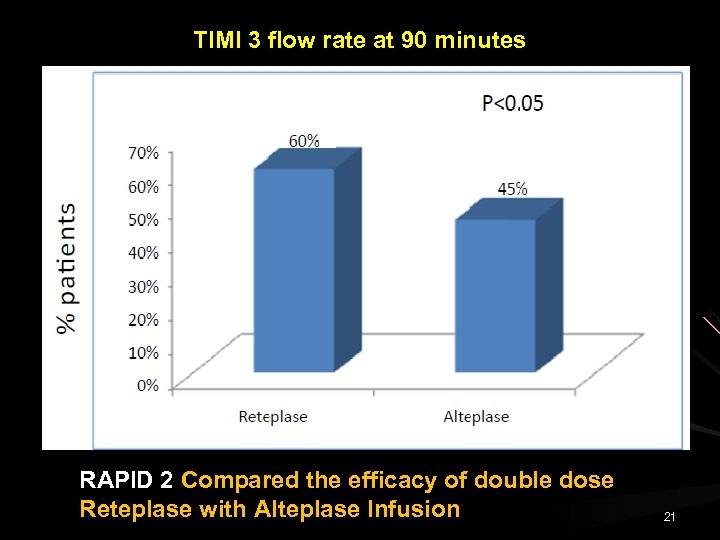
TIMI 3 flow rate at 90 minutes RAPID 2 Compared the efficacy of double dose Reteplase with Alteplase Infusion 21
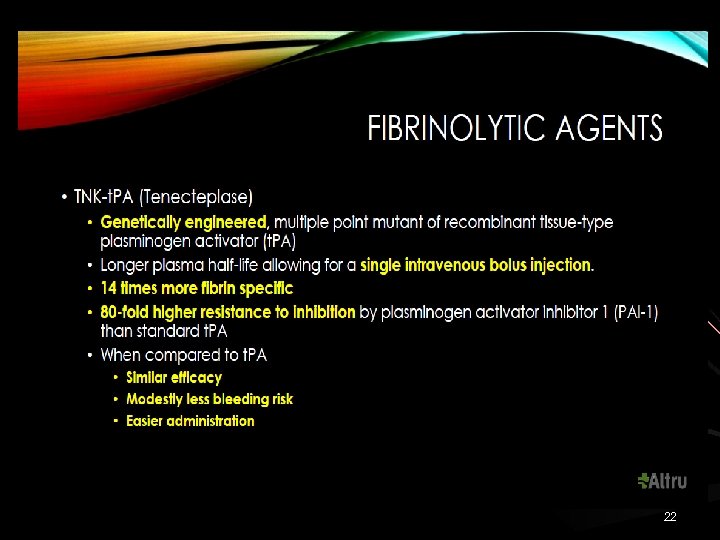
22
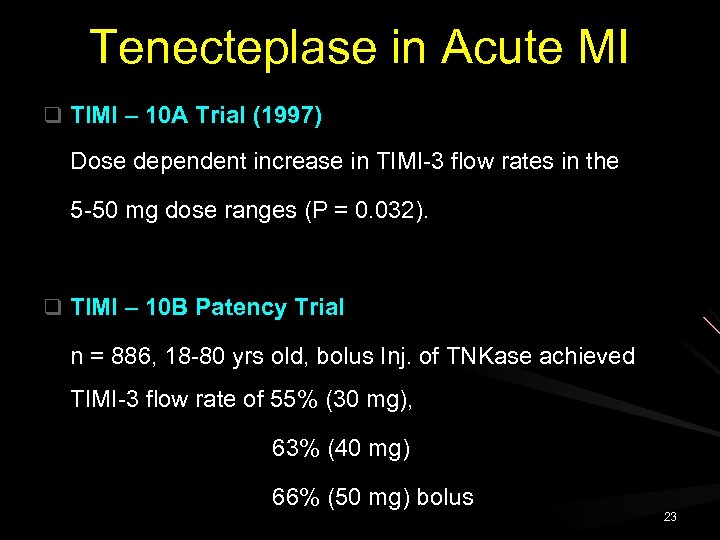
Tenecteplase in Acute MI q TIMI – 10 A Trial (1997) Dose dependent increase in TIMI-3 flow rates in the 5 -50 mg dose ranges (P = 0. 032). q TIMI – 10 B Patency Trial n = 886, 18 -80 yrs old, bolus Inj. of TNKase achieved TIMI-3 flow rate of 55% (30 mg), 63% (40 mg) 66% (50 mg) bolus 23
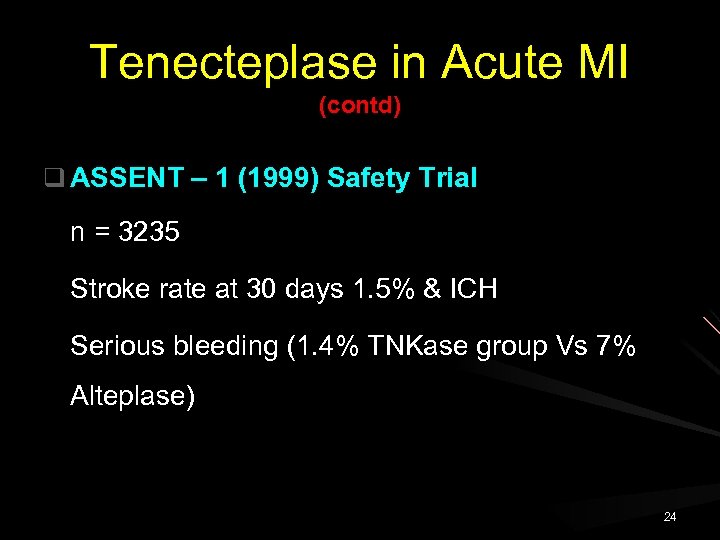
Tenecteplase in Acute MI (contd) q ASSENT – 1 (1999) Safety Trial n = 3235 Stroke rate at 30 days 1. 5% & ICH Serious bleeding (1. 4% TNKase group Vs 7% Alteplase) 24
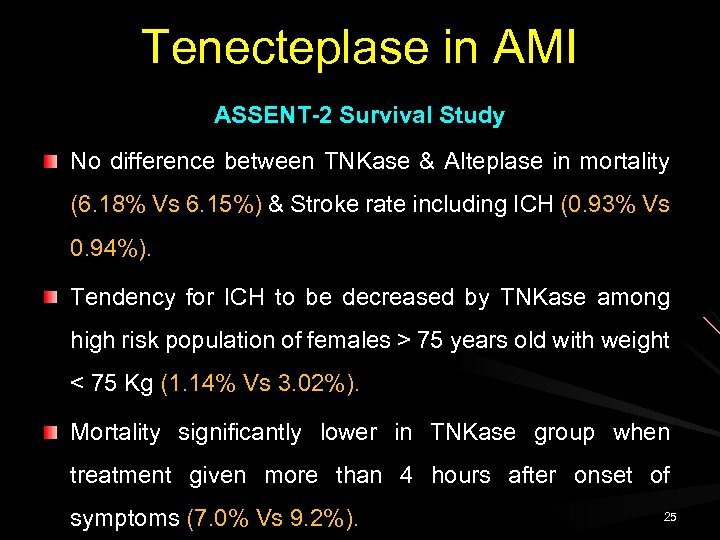
Tenecteplase in AMI ASSENT-2 Survival Study No difference between TNKase & Alteplase in mortality (6. 18% Vs 6. 15%) & Stroke rate including ICH (0. 93% Vs 0. 94%). Tendency for ICH to be decreased by TNKase among high risk population of females > 75 years old with weight < 75 Kg (1. 14% Vs 3. 02%). Mortality significantly lower in TNKase group when treatment given more than 4 hours after onset of symptoms (7. 0% Vs 9. 2%). 25
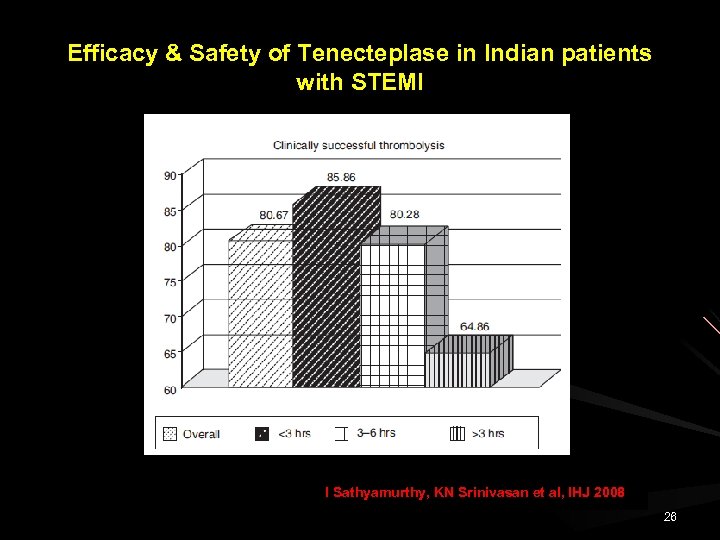
Efficacy & Safety of Tenecteplase in Indian patients with STEMI I Sathyamurthy, KN Srinivasan et al, IHJ 2008 26
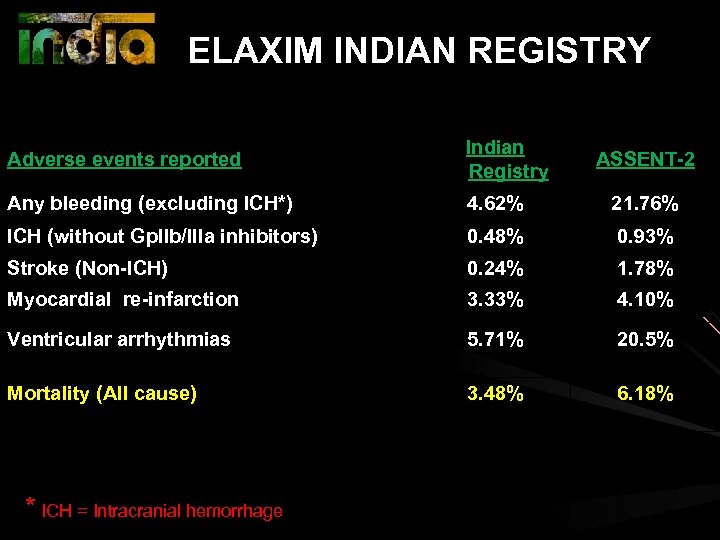
ELAXIM INDIAN REGISTRY Adverse events reported Indian Registry Any bleeding (excluding ICH*) 4. 62% 21. 76% ICH (without Gp. IIb/IIIa inhibitors) 0. 48% 0. 93% Stroke (Non-ICH) 0. 24% 1. 78% Myocardial re-infarction 3. 33% 4. 10% Ventricular arrhythmias 5. 71% 20. 5% Mortality (All cause) 3. 48% 6. 18% * ICH = Intracranial hemorrhage ASSENT-2
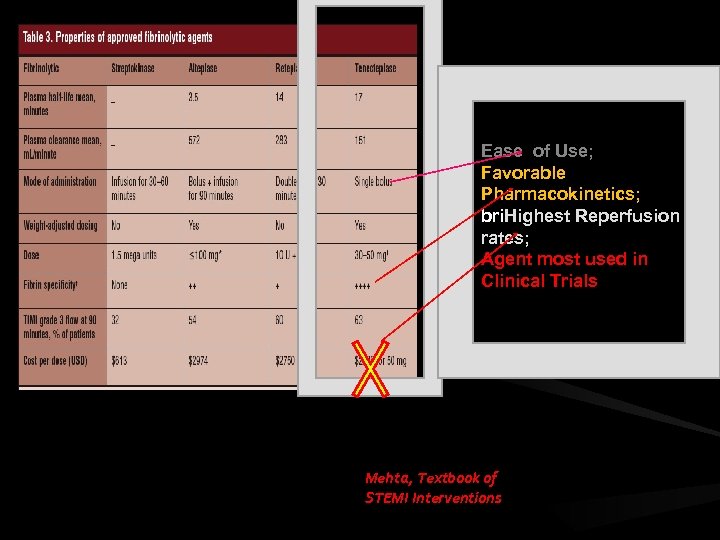
Ease of Use; Favorable Pharmacokinetics; bri. Highest Reperfusion rates; Agent most used in Clinical Trials Mehta, Textbook of STEMI Interventions
Pre-Hospital Thrombolysis 29
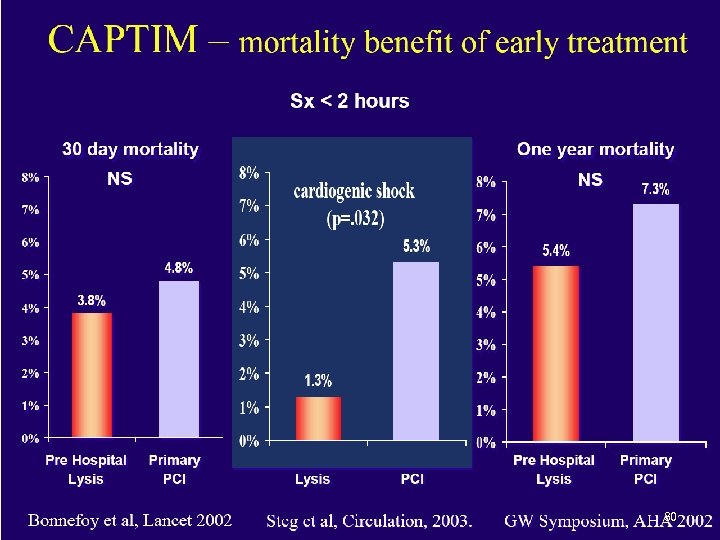
30
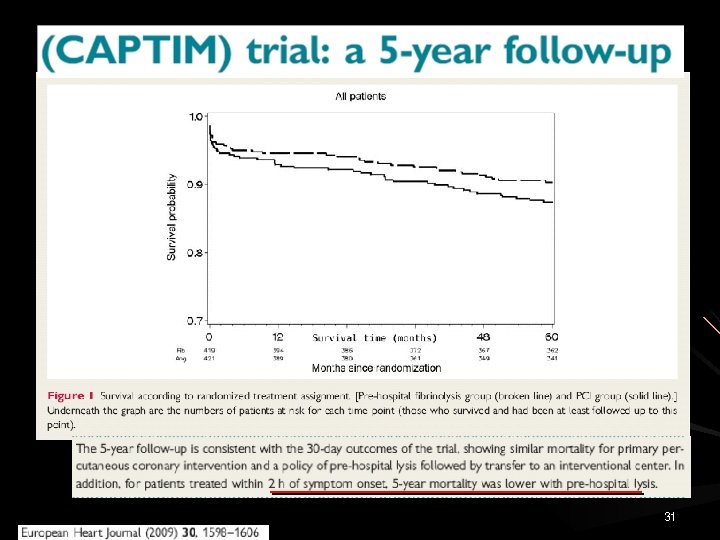
31
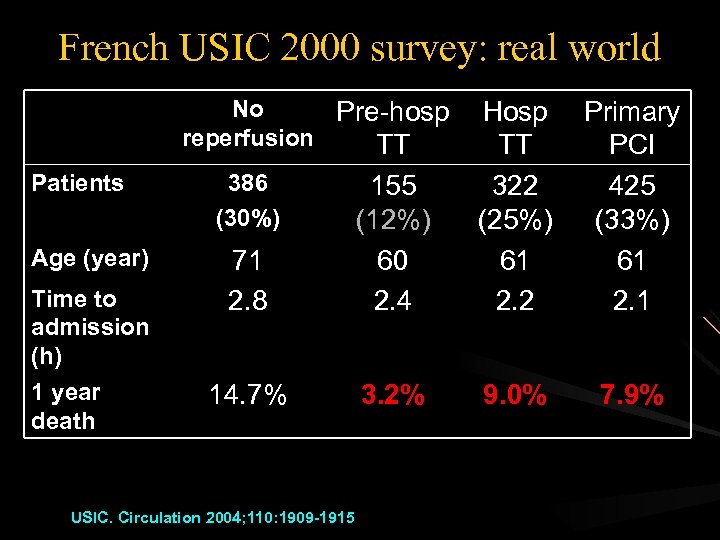
French USIC 2000 survey: real world No Pre-hosp reperfusion TT Patients Age (year) Time to admission (h) 1 year death 71 2. 8 155 (12%) 60 2. 4 Hosp TT 322 (25%) 61 2. 2 Primary PCI 425 (33%) 61 2. 1 14. 7% 3. 2% 9. 0% 7. 9% 386 (30%) USIC. Circulation 2004; 110: 1909 -1915
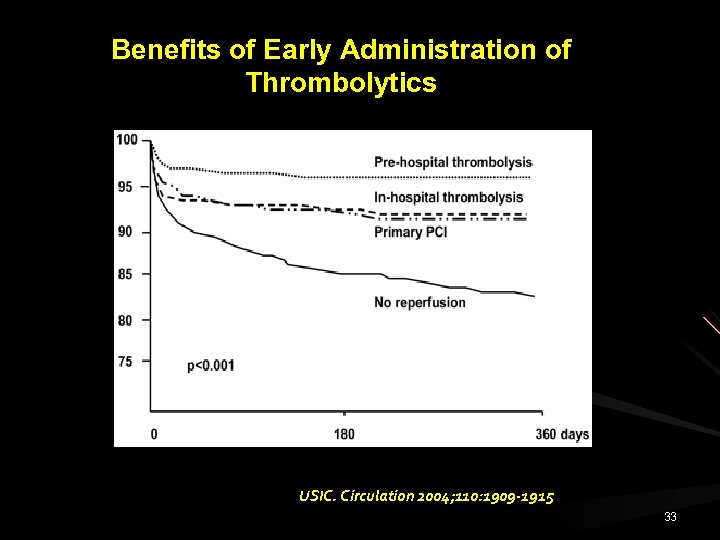
Benefits of Early Administration of Thrombolytics n = 1, 922 USIC. Circulation 2004; 110: 1909 -1915 33
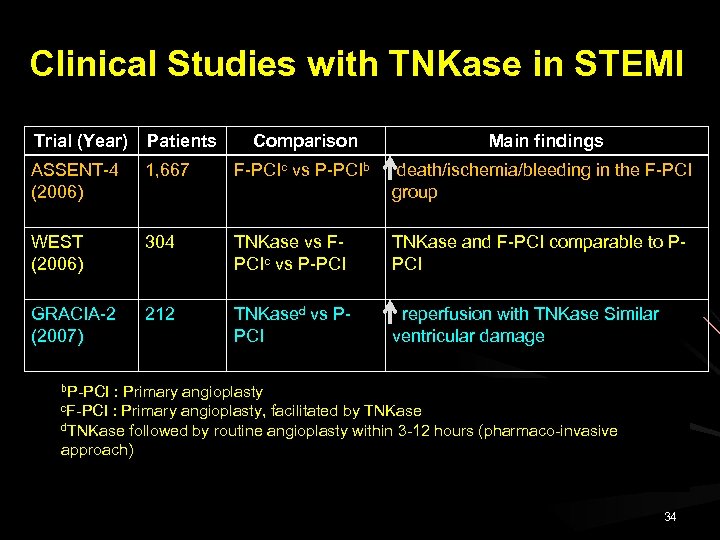
Clinical Studies with TNKase in STEMI Trial (Year) Patients Comparison Main findings ASSENT-4 (2006) 1, 667 F-PCIc vs P-PCIb death/ischemia/bleeding in the F-PCI group WEST (2006) 304 TNKase vs FPCIc vs P-PCI TNKase and F-PCI comparable to PPCI GRACIA-2 (2007) 212 TNKased vs PPCI reperfusion with TNKase Similar ventricular damage b. P-PCI : Primary angioplasty, facilitated by TNKase d. TNKase followed by routine angioplasty within 3 -12 hours (pharmaco-invasive approach) c. F-PCI 34
Dr. Lekha Adik Pathak 35
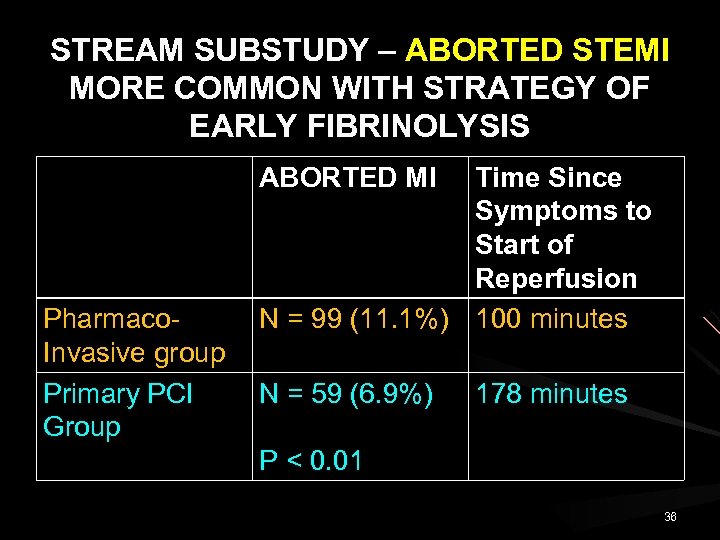
STREAM SUBSTUDY – ABORTED STEMI MORE COMMON WITH STRATEGY OF EARLY FIBRINOLYSIS ABORTED MI Pharmaco. Invasive group Primary PCI Group Time Since Symptoms to Start of Reperfusion N = 99 (11. 1%) 100 minutes N = 59 (6. 9%) 178 minutes P < 0. 01 36
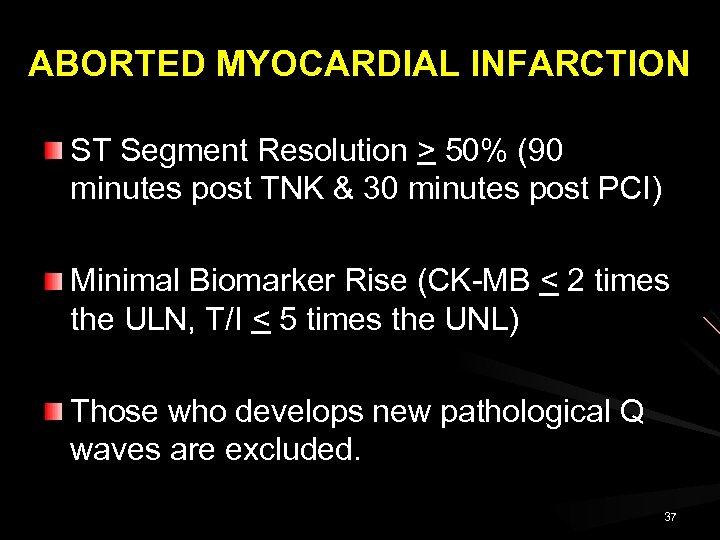
ABORTED MYOCARDIAL INFARCTION ST Segment Resolution > 50% (90 minutes post TNK & 30 minutes post PCI) Minimal Biomarker Rise (CK-MB < 2 times the ULN, T/I < 5 times the UNL) Those who develops new pathological Q waves are excluded. 37
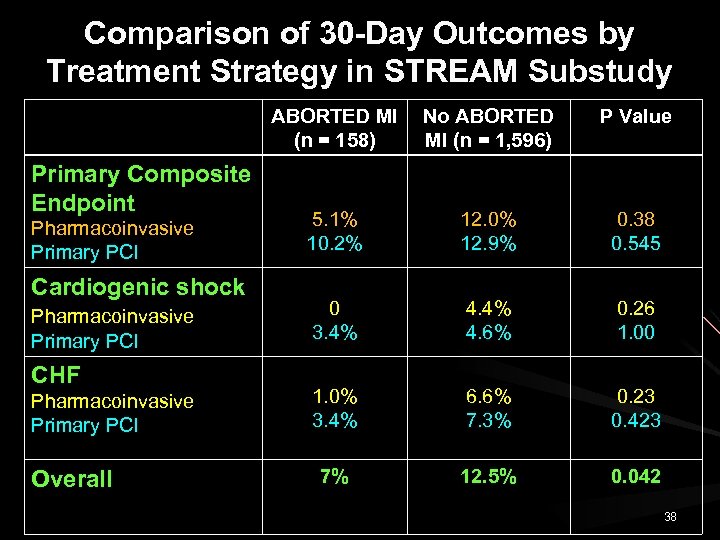
Comparison of 30 -Day Outcomes by Treatment Strategy in STREAM Substudy ABORTED MI No ABORTED (n = 158) MI (n = 1, 596) Primary Composite Endpoint Pharmacoinvasive Primary PCI Cardiogenic shock Pharmacoinvasive Primary PCI CHF Pharmacoinvasive Primary PCI Overall P Value 5. 1% 10. 2% 12. 0% 12. 9% 0. 38 0. 545 0 3. 4% 4. 6% 0. 26 1. 00 1. 0% 3. 4% 6. 6% 7. 3% 0. 23 0. 423 7% 12. 5% 0. 042 38
STREAM SUBSTUDY: ABORTION OF STEMI ONE YEAR FOLLOW UP All Cause Mortality Aborted MI Vs Non-aborted MI 3. 1% Vs 4. 5% (P =. 818) 39
STREAM TRIAL Coronary Flow Data > 70% of patients receiving early fibrinolysis had TIMI flow grade 2 or 3, compared with 20% of those arriving for primary PCI. Larger clinical benefit at longer term follow up. 40
Limitations of Thrombolysis 41
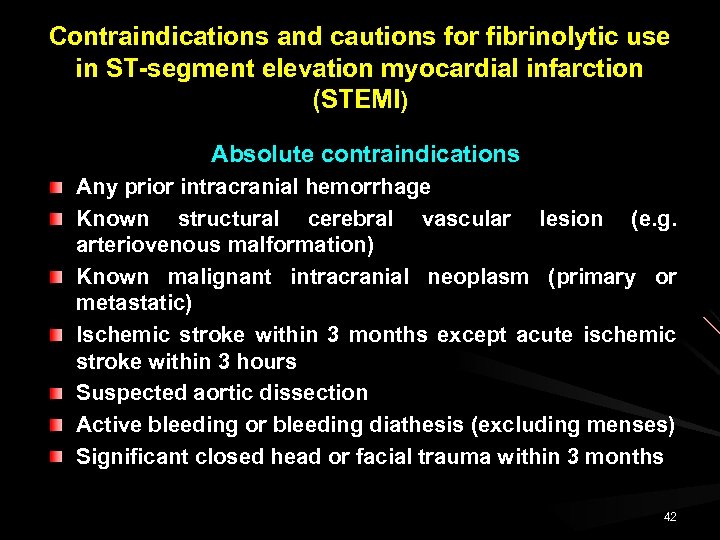
Contraindications and cautions for fibrinolytic use in ST-segment elevation myocardial infarction (STEMI) Absolute contraindications Any prior intracranial hemorrhage Known structural cerebral vascular lesion (e. g. arteriovenous malformation) Known malignant intracranial neoplasm (primary or metastatic) Ischemic stroke within 3 months except acute ischemic stroke within 3 hours Suspected aortic dissection Active bleeding or bleeding diathesis (excluding menses) Significant closed head or facial trauma within 3 months 42
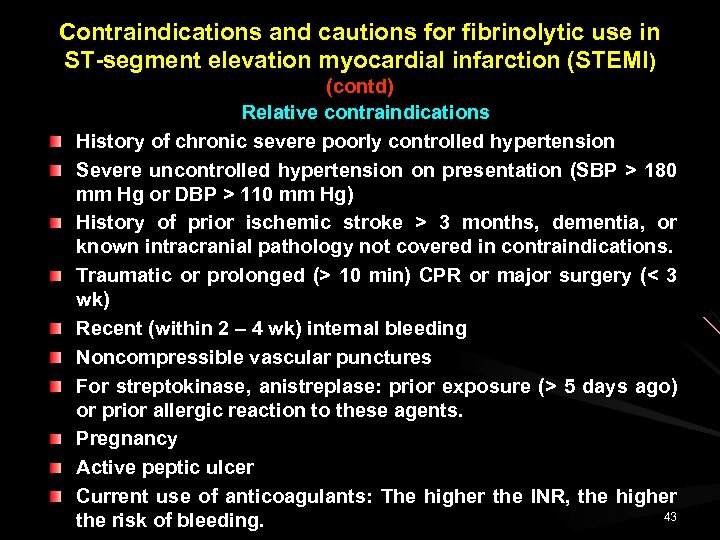
Contraindications and cautions for fibrinolytic use in ST-segment elevation myocardial infarction (STEMI) (contd) Relative contraindications History of chronic severe poorly controlled hypertension Severe uncontrolled hypertension on presentation (SBP > 180 mm Hg or DBP > 110 mm Hg) History of prior ischemic stroke > 3 months, dementia, or known intracranial pathology not covered in contraindications. Traumatic or prolonged (> 10 min) CPR or major surgery (< 3 wk) Recent (within 2 – 4 wk) internal bleeding Noncompressible vascular punctures For streptokinase, anistreplase: prior exposure (> 5 days ago) or prior allergic reaction to these agents. Pregnancy Active peptic ulcer Current use of anticoagulants: The higher the INR, the higher 43 the risk of bleeding.
Limitations of Thrombolytic therapy in STEMI Efficacy of thrombolysis declines rapidly with the increase in the time to treatment interval. 44
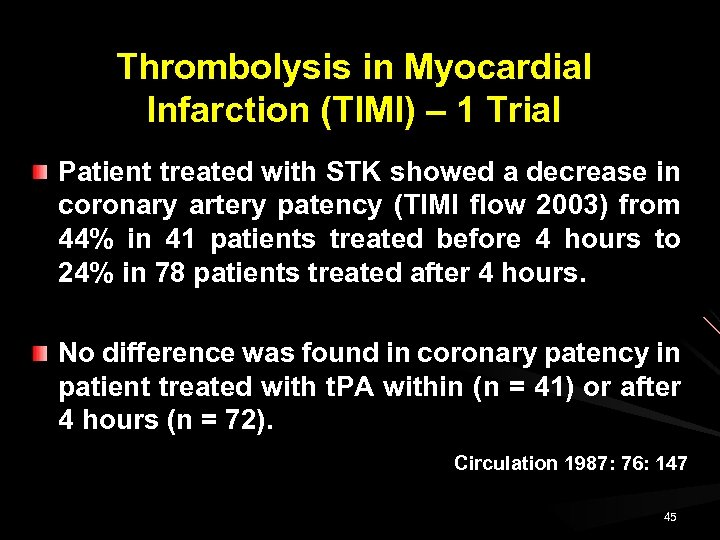
Thrombolysis in Myocardial Infarction (TIMI) – 1 Trial Patient treated with STK showed a decrease in coronary artery patency (TIMI flow 2003) from 44% in 41 patients treated before 4 hours to 24% in 78 patients treated after 4 hours. No difference was found in coronary patency in patient treated with t. PA within (n = 41) or after 4 hours (n = 72). Circulation 1987: 76: 147 45
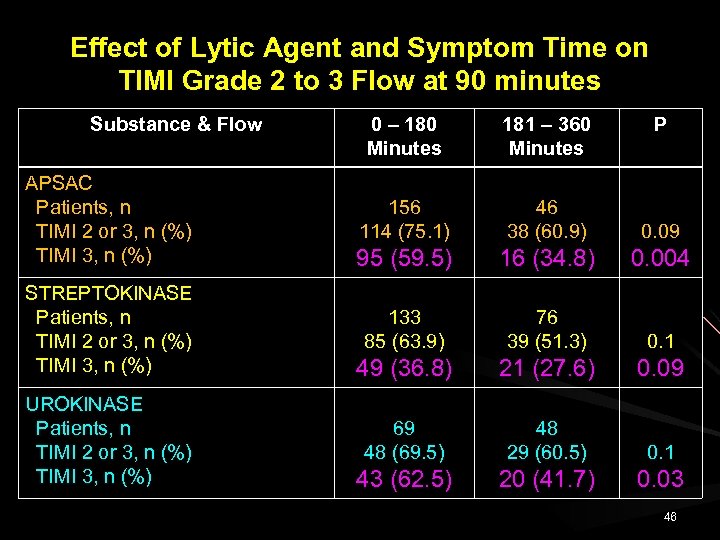
Effect of Lytic Agent and Symptom Time on TIMI Grade 2 to 3 Flow at 90 minutes Substance & Flow APSAC Patients, n TIMI 2 or 3, n (%) TIMI 3, n (%) STREPTOKINASE Patients, n TIMI 2 or 3, n (%) TIMI 3, n (%) UROKINASE Patients, n TIMI 2 or 3, n (%) TIMI 3, n (%) 0 – 180 Minutes 181 – 360 Minutes P 156 114 (75. 1) 46 38 (60. 9) 0. 09 95 (59. 5) 16 (34. 8) 0. 004 133 85 (63. 9) 76 39 (51. 3) 0. 1 49 (36. 8) 21 (27. 6) 0. 09 69 48 (69. 5) 48 29 (60. 5) 0. 1 43 (62. 5) 20 (41. 7) 0. 03 46
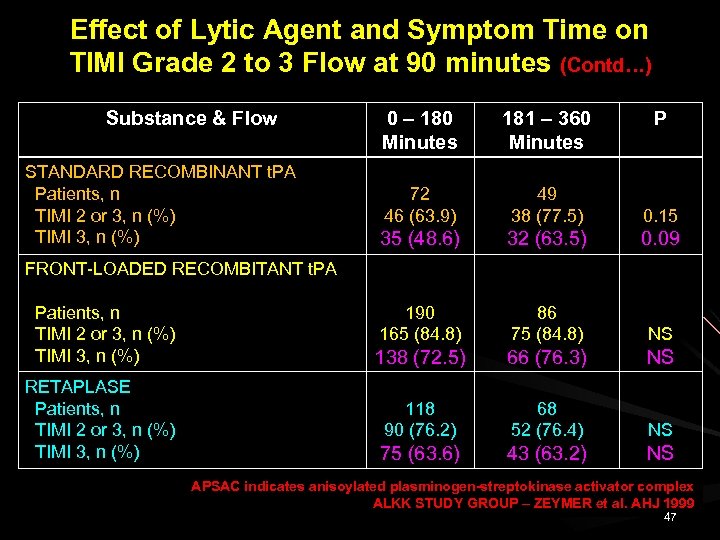
Effect of Lytic Agent and Symptom Time on TIMI Grade 2 to 3 Flow at 90 minutes (Contd…) Substance & Flow 181 – 360 Minutes 72 46 (63. 9) 49 38 (77. 5) 0. 15 35 (48. 6) 32 (63. 5) 0. 09 190 165 (84. 8) 86 75 (84. 8) NS 138 (72. 5) 66 (76. 3) NS 118 90 (76. 2) 68 52 (76. 4) NS 75 (63. 6) STANDARD RECOMBINANT t. PA Patients, n TIMI 2 or 3, n (%) TIMI 3, n (%) 0 – 180 Minutes P 43 (63. 2) NS FRONT-LOADED RECOMBITANT t. PA Patients, n TIMI 2 or 3, n (%) TIMI 3, n (%) RETAPLASE Patients, n TIMI 2 or 3, n (%) TIMI 3, n (%) APSAC indicates anisoylated plasminogen-streptokinase activator complex ALKK STUDY GROUP – ZEYMER et al. AHJ 1999 47
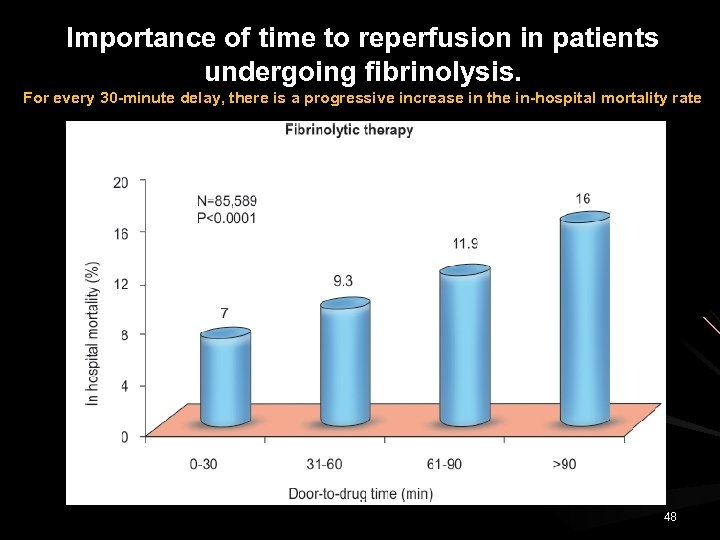
Importance of time to reperfusion in patients undergoing fibrinolysis. For every 30 -minute delay, there is a progressive increase in the in-hospital mortality rate 48
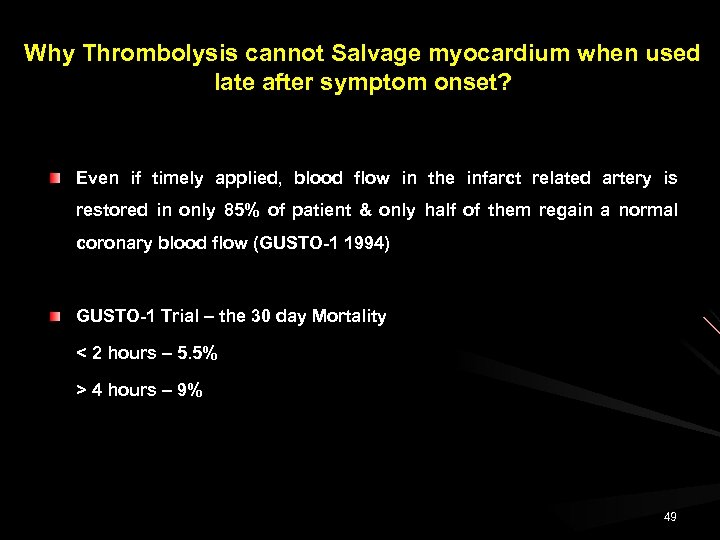
Why Thrombolysis cannot Salvage myocardium when used late after symptom onset? Even if timely applied, blood flow in the infarct related artery is restored in only 85% of patient & only half of them regain a normal coronary blood flow (GUSTO-1 1994) GUSTO-1 Trial – the 30 day Mortality < 2 hours – 5. 5% > 4 hours – 9% 49
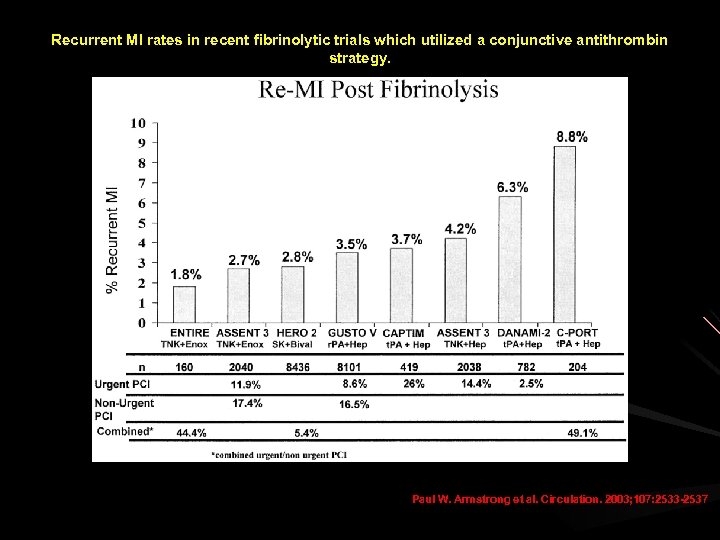
Recurrent MI rates in recent fibrinolytic trials which utilized a conjunctive antithrombin strategy. Paul W. Armstrong et al. Circulation. 2003; 107: 2533 -2537
Limitations of Thrombolytic Therapy Stroke Fibrinolytic Therapy Trialist Collaborators (FIT) - Thrombolysis is associated with an increase in stroke rate compared to control group (1. 2% vs 0. 8%) GUSTO-1 Study STK 1. 19% STK+ t. PA 1. 64% STREAM Trial 51
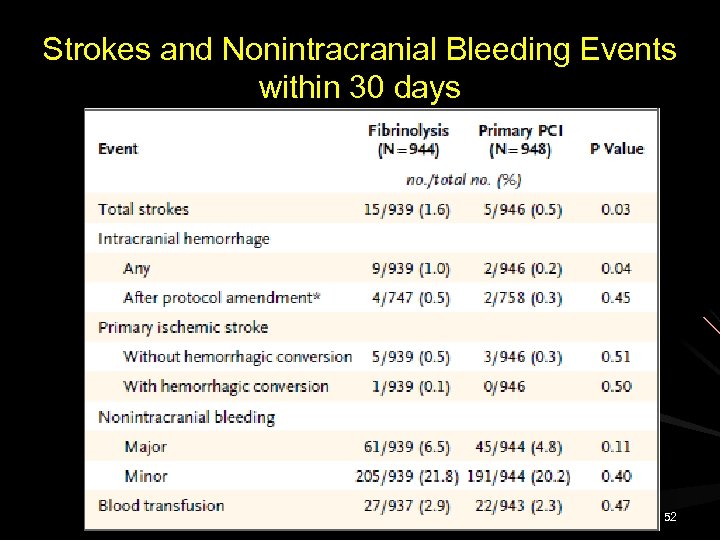
Strokes and Nonintracranial Bleeding Events within 30 days 52
Limitations of Thrombolytic Therapy AGE Short & long term mortality increases with age GUSTO-1 – 30 days Mortality - < 65 yrs – 3% - 65 – 74 yrs - 9. 5% - 75 – 85 yrs - 19. 6% - > 85 yrs - 30. 3% Increase in stroke, cardiogenic shock, bleeding & reinfarction Accelerated t-PA was associated with fewer combined death or disabling stroke in all but older patients 53
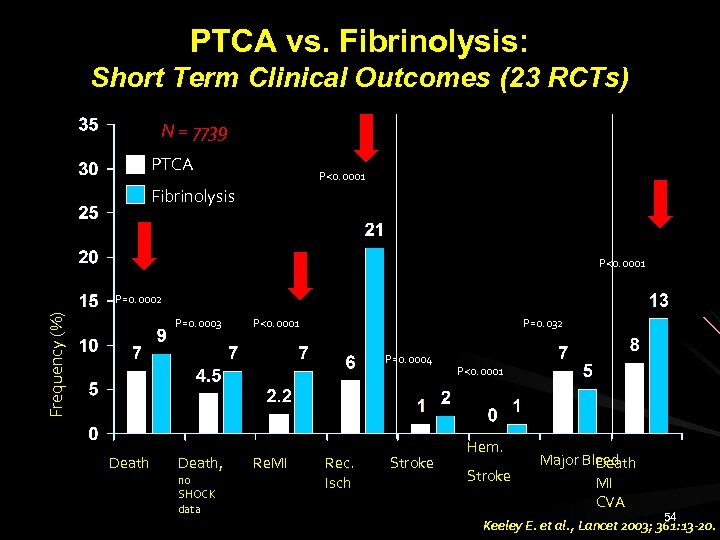
PTCA vs. Fibrinolysis: Short Term Clinical Outcomes (23 RCTs) N = 7739 PTCA P<0. 0001 Fibrinolysis P<0. 0001 Frequency (%) P=0. 0002 P=0. 0003 P<0. 0001 P=0. 032 P=0. 0004 Death, no SHOCK data Re. MI Rec. Isch Stroke P<0. 0001 Hem. Stroke Major Bleed Death MI CVA 54 Keeley E. et al. , Lancet 2003; 361: 13 -20.
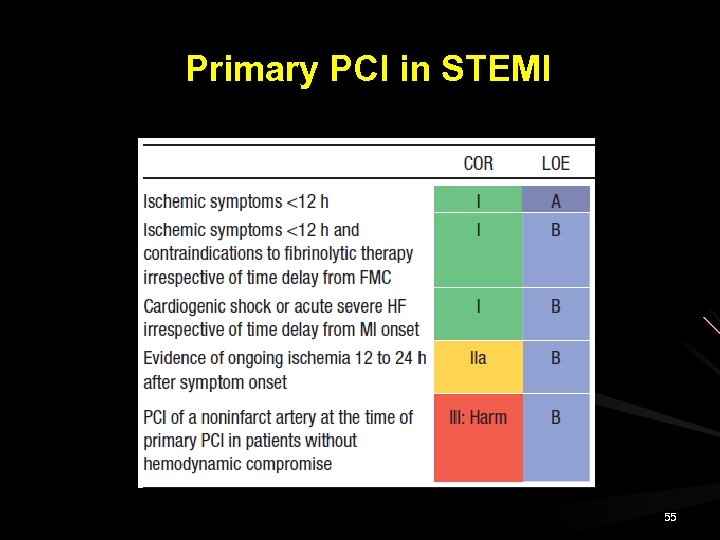
Primary PCI in STEMI 55
Is there still a Role for Fibrinolysis in era of primary percutaneous Intervention? 56
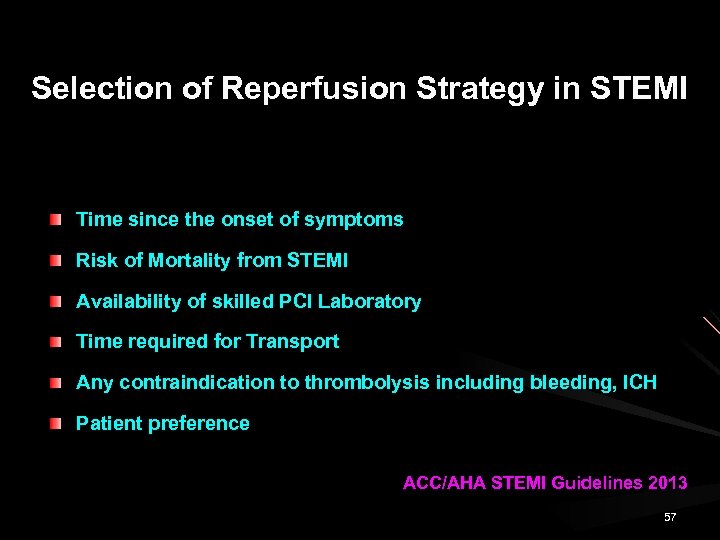
Selection of Reperfusion Strategy in STEMI Time since the onset of symptoms Risk of Mortality from STEMI Availability of skilled PCI Laboratory Time required for Transport Any contraindication to thrombolysis including bleeding, ICH Patient preference ACC/AHA STEMI Guidelines 2013 57
The degree of reversibility and extent of myocardial necrosis were both time dependent Reimer 1979 58
Fibrinolytics are needed because primary PCI cannot be delivered to all patients with STEMI within evidence based time frames needed for full effectiveness. 59
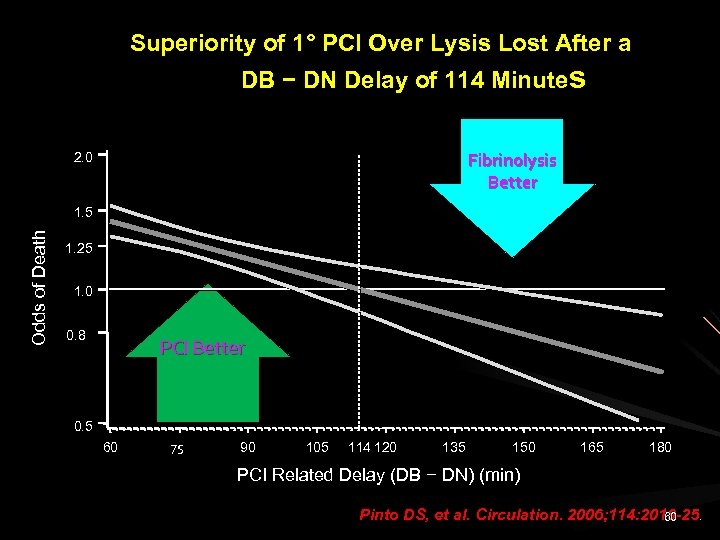
Superiority of 1° PCI Over Lysis Lost After a DB − DN Delay of 114 Minutes Fibrinolysis Better 2. 0 O dds of Deat h 1. 5 1. 25 1. 0 0. 8 PCI Better 0. 5 60 75 90 105 114 120 135 150 165 180 PCI Related Delay (DB − DN) (min) Pinto DS, et al. Circulation. 2006; 114: 2019 -25. 60
Survival benefit with PPCI in STEMI is attenuated if DB time is delayed by > 1 hour beyond the DN time for thrombolytic therapy. Longer DB-DN times would be associated with high mortality rates and reduced survival advantage. In addition to PPCI delays, patient risk factors viz. would significantly modulate the relative survival advantage of PPCI over fibrinolysis. 61
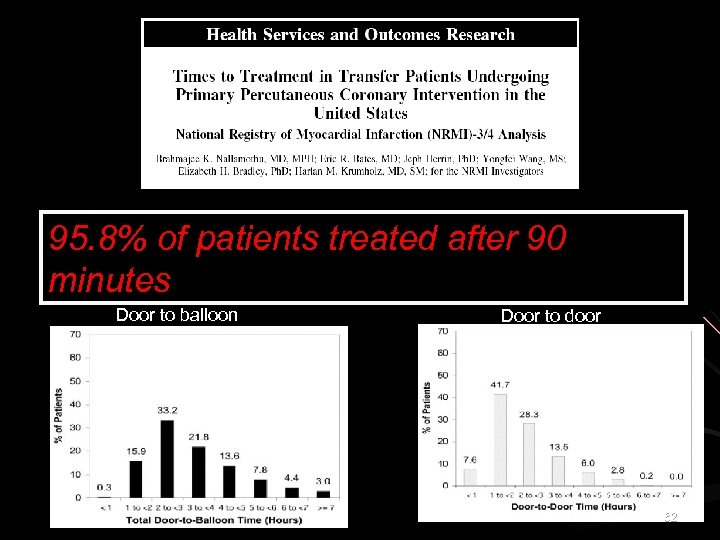
95. 8% of patients treated after 90 minutes Door to balloon Door to door 62
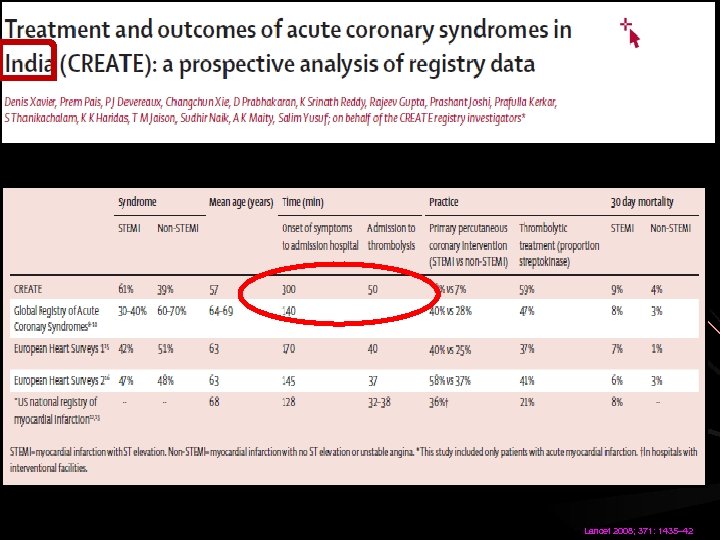
Lancet 2008; 371: 1435– 42
Despite the clinical superiority of PAMI, thrombolytic therapy is the default treatment in many countries due to the practical limitations of PAMI 64
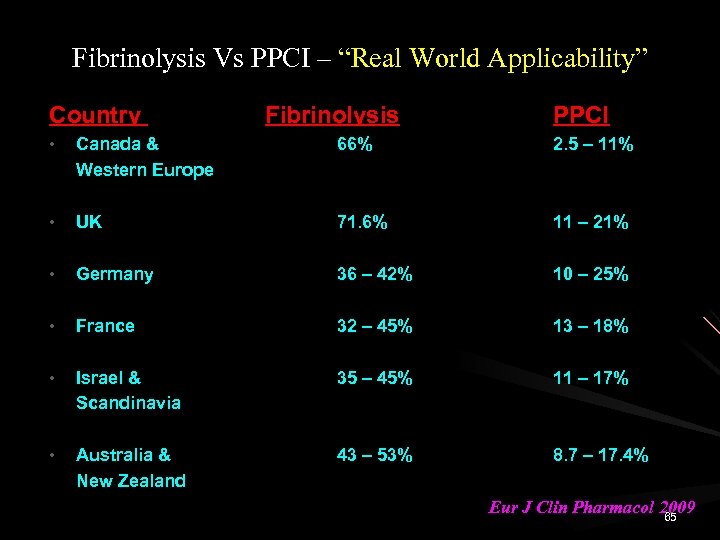
Fibrinolysis Vs PPCI – “Real World Applicability” Country Fibrinolysis PPCI • Canada & Western Europe 66% 2. 5 – 11% • UK 71. 6% 11 – 21% • Germany 36 – 42% 10 – 25% • France 32 – 45% 13 – 18% • Israel & Scandinavia 35 – 45% 11 – 17% • Australia & New Zealand 43 – 53% 8. 7 – 17. 4% Eur J Clin Pharmacol 2009 65
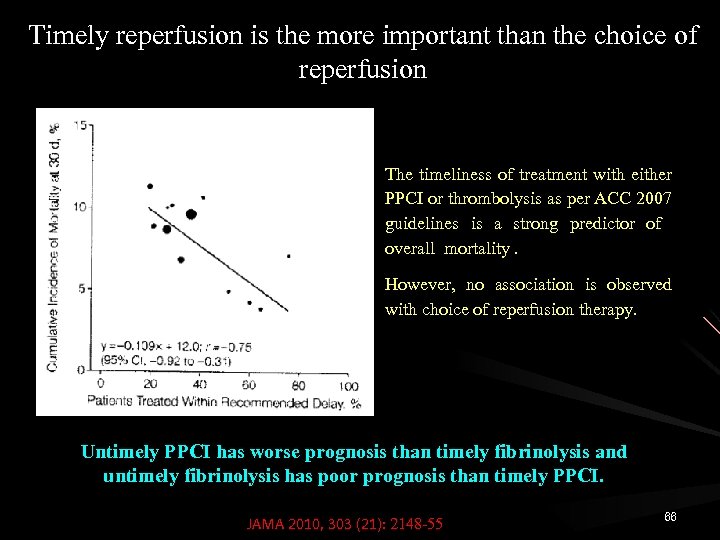
Timely reperfusion is the more important than the choice of reperfusion The timeliness of treatment with either PPCI or thrombolysis as per ACC 2007 guidelines is a strong predictor of overall mortality. However, no association is observed with choice of reperfusion therapy. Untimely PPCI has worse prognosis than timely fibrinolysis and untimely fibrinolysis has poor prognosis than timely PPCI. JAMA 2010, 303 (21): 2148 -55 66
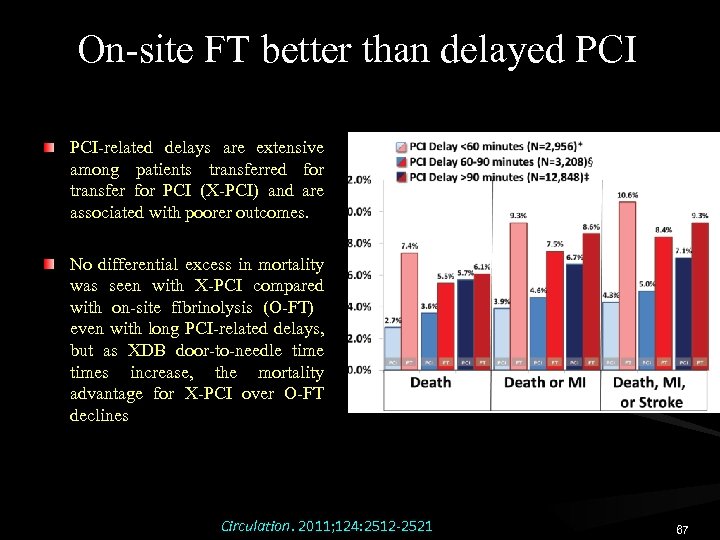
On-site FT better than delayed PCI-related delays are extensive among patients transferred for transfer for PCI (X-PCI) and are associated with poorer outcomes. No differential excess in mortality was seen with X-PCI compared with on-site fibrinolysis (O-FT) even with long PCI-related delays, but as XDB door-to-needle times increase, the mortality advantage for X-PCI over O-FT declines Circulation. 2011; 124: 2512 -2521 67
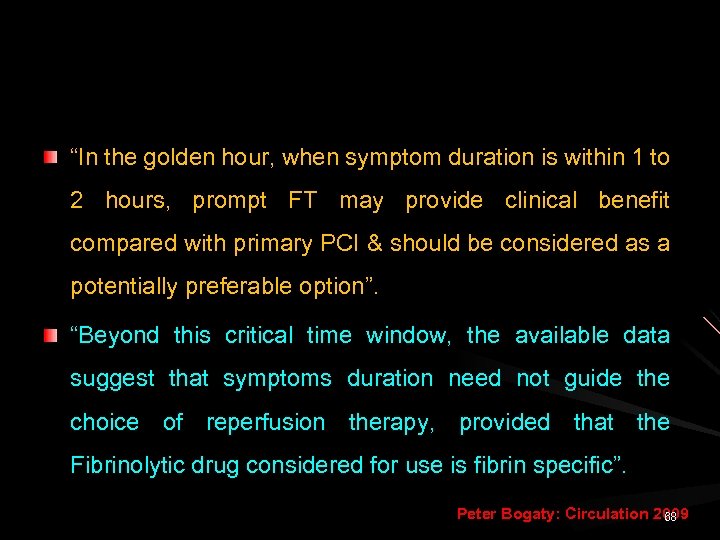
“In the golden hour, when symptom duration is within 1 to 2 hours, prompt FT may provide clinical benefit compared with primary PCI & should be considered as a potentially preferable option”. “Beyond this critical time window, the available data suggest that symptoms duration need not guide the choice of reperfusion therapy, provided that the Fibrinolytic drug considered for use is fibrin specific”. Peter Bogaty: Circulation 2009 68
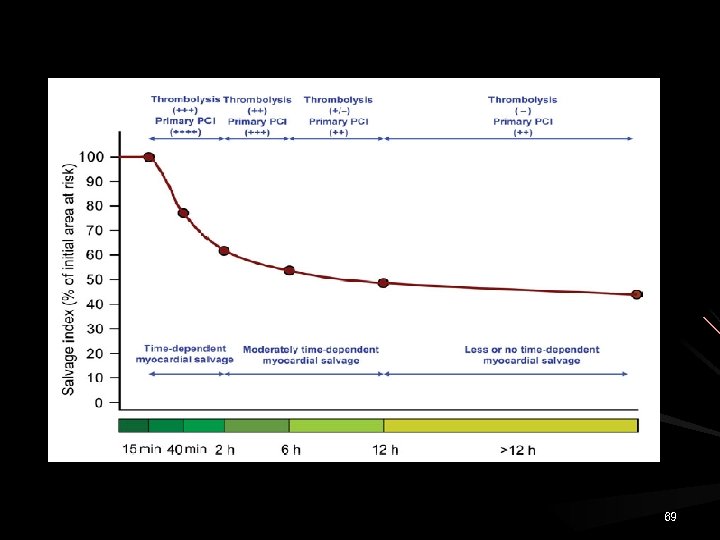
69
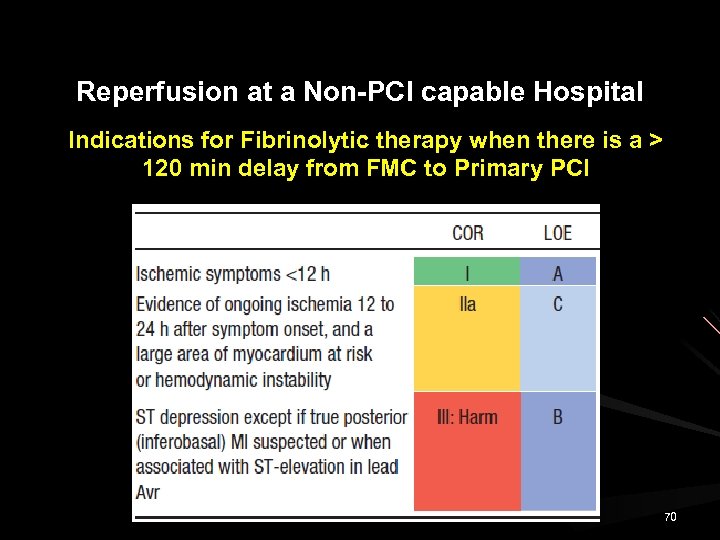
Reperfusion at a Non-PCI capable Hospital Indications for Fibrinolytic therapy when there is a > 120 min delay from FMC to Primary PCI 70
Reperfusion strategy in STEMI Where are we at the dawn of 2016? Thrombolysis or Primary Angioplasty Thrombolysis And Early Angioplasty Pharmaco-invasive stragey 71

THANK YOU 72
ff1fe5b6fa7f68ee657ad01ba4b59020.ppt