80c4ad496767431f78ab6691ba19fe83.ppt
- Количество слайдов: 57
Thrombolytic Therapy for Acute Ischemic Stroke: Should it be used in the Community? Moritz Haager PGY-5 Nov 17, 2005
Cases n STARS flight call – Case 1: 58 yo M in Lethbridge w/ large L MCA stroke onset 1. 5 hrs ago Stroke neurologist in Calgary wants t. PA given – Case 2: 65 yo M in Lethbridge w/ large R MCA stroke onset 2 hrs ago Stroke neurologist in Calgary wants t. PA given
Objectives n Review efficacy of t. PA in acute ischemic stroke (AIS): what is the current state of the evidence? n Review effectiveness of t. PA: Can we expand thrombolytic Tx to non-academic centers?
Bad Ideas Part I
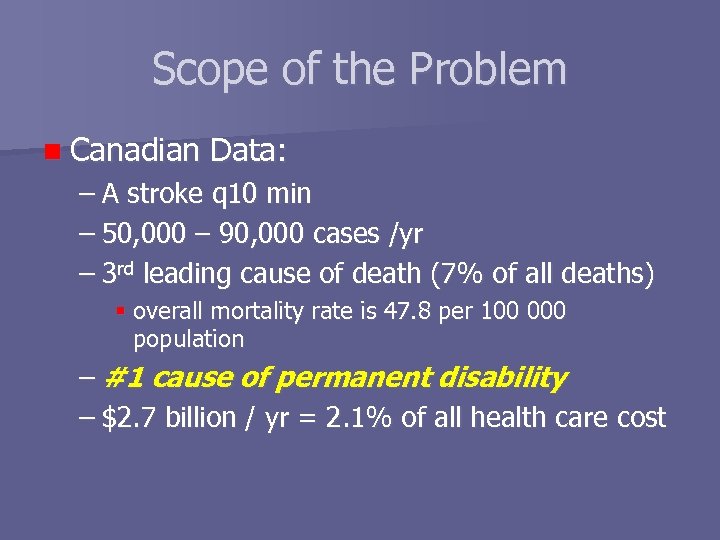
Scope of the Problem n Canadian Data: – A stroke q 10 min – 50, 000 – 90, 000 cases /yr – 3 rd leading cause of death (7% of all deaths) overall mortality rate is 47. 8 per 100 000 population – #1 cause of permanent disability – $2. 7 billion / yr = 2. 1% of all health care cost
Thrombolysis in Acute Ischemic Stroke: is it efficacious? How well does it work in RCT’s?
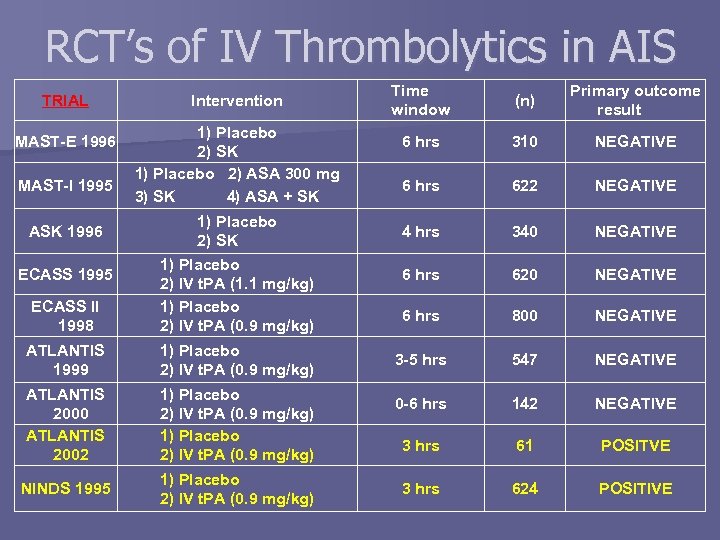
RCT’s of IV Thrombolytics in AIS TRIAL MAST-E 1996 MAST-I 1995 Intervention 1) Placebo 2) SK 1) Placebo 2) ASA 300 mg 3) SK 4) ASA + SK ECASS II 1998 1) Placebo 2) SK 1) Placebo 2) IV t. PA (1. 1 mg/kg) 1) Placebo 2) IV t. PA (0. 9 mg/kg) ATLANTIS 1999 1) Placebo 2) IV t. PA (0. 9 mg/kg) ATLANTIS 2000 ATLANTIS 2002 1) Placebo 2) IV t. PA (0. 9 mg/kg) NINDS 1995 1) Placebo 2) IV t. PA (0. 9 mg/kg) ASK 1996 ECASS 1995 Time window (n) Primary outcome result 6 hrs 310 NEGATIVE 6 hrs 622 NEGATIVE 4 hrs 340 NEGATIVE 6 hrs 620 NEGATIVE 6 hrs 800 NEGATIVE 3 -5 hrs 547 NEGATIVE 0 -6 hrs 142 NEGATIVE 3 hrs 61 POSITVE 3 hrs 624 POSITIVE
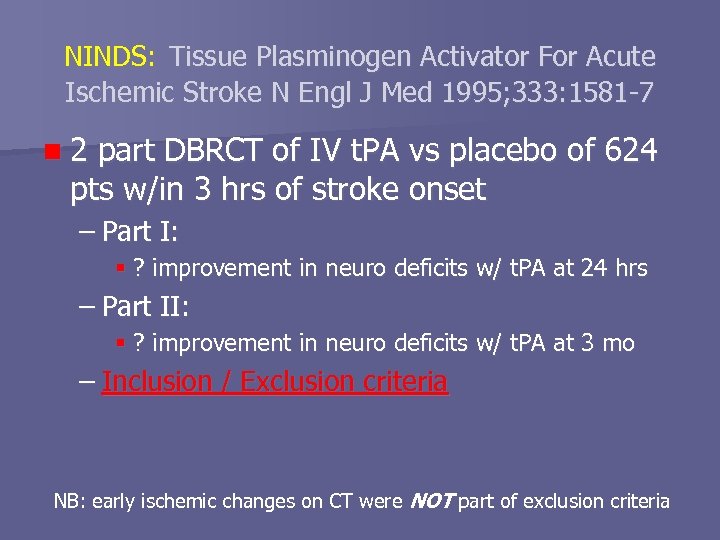
NINDS: Tissue Plasminogen Activator For Acute Ischemic Stroke N Engl J Med 1995; 333: 1581 -7 n 2 part DBRCT of IV t. PA vs placebo of 624 pts w/in 3 hrs of stroke onset – Part I: ? improvement in neuro deficits w/ t. PA at 24 hrs – Part II: ? improvement in neuro deficits w/ t. PA at 3 mo – Inclusion / Exclusion criteria NB: early ischemic changes on CT were NOT part of exclusion criteria
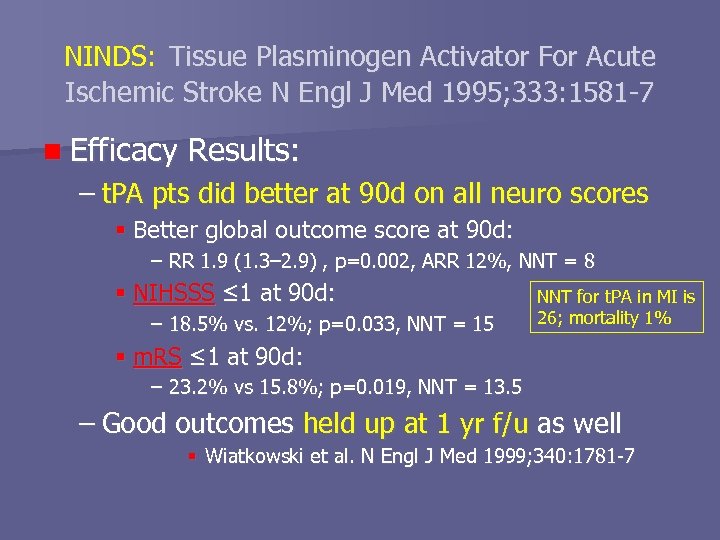
NINDS: Tissue Plasminogen Activator For Acute Ischemic Stroke N Engl J Med 1995; 333: 1581 -7 n Efficacy Results: – t. PA pts did better at 90 d on all neuro scores Better global outcome score at 90 d: – RR 1. 9 (1. 3– 2. 9) , p=0. 002, ARR 12%, NNT = 8 NIHSSS ≤ 1 at 90 d: – 18. 5% vs. 12%; p=0. 033, NNT = 15 NNT for t. PA in MI is 26; mortality 1% m. RS ≤ 1 at 90 d: – 23. 2% vs 15. 8%; p=0. 019, NNT = 13. 5 – Good outcomes held up at 1 yr f/u as well Wiatkowski et al. N Engl J Med 1999; 340: 1781 -7
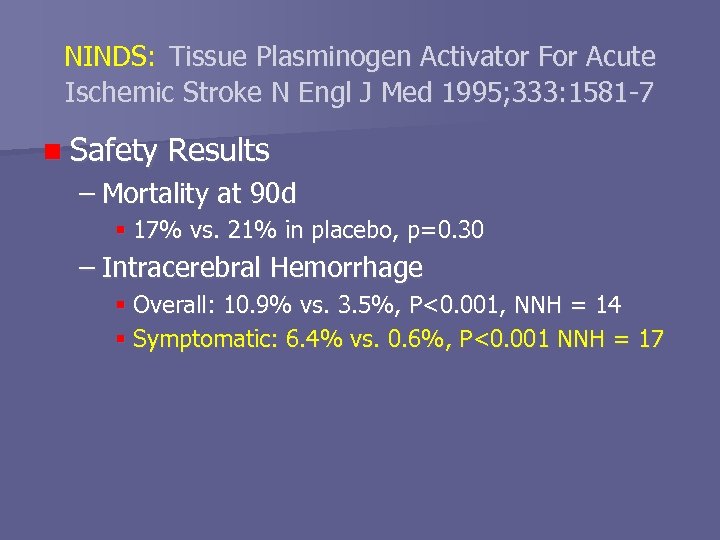
NINDS: Tissue Plasminogen Activator For Acute Ischemic Stroke N Engl J Med 1995; 333: 1581 -7 n Safety Results – Mortality at 90 d 17% vs. 21% in placebo, p=0. 30 – Intracerebral Hemorrhage Overall: 10. 9% vs. 3. 5%, P<0. 001, NNH = 14 Symptomatic: 6. 4% vs. 0. 6%, P<0. 001 NNH = 17
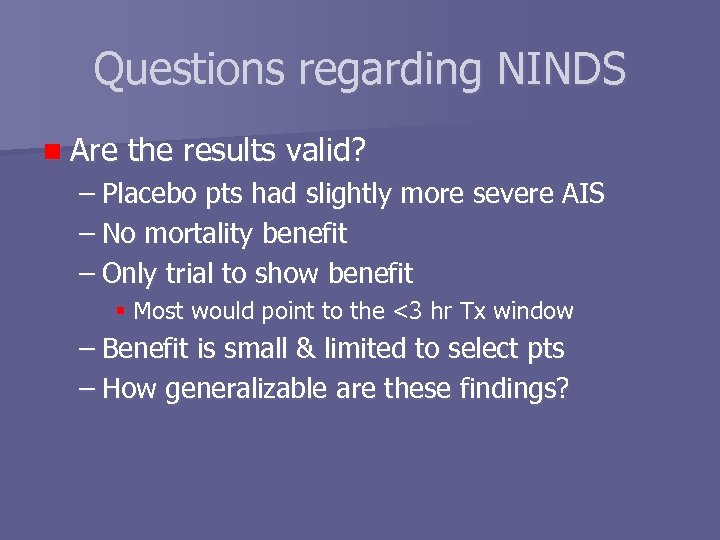
Questions regarding NINDS n Are the results valid? – Placebo pts had slightly more severe AIS – No mortality benefit – Only trial to show benefit Most would point to the <3 hr Tx window – Benefit is small & limited to select pts – How generalizable are these findings?
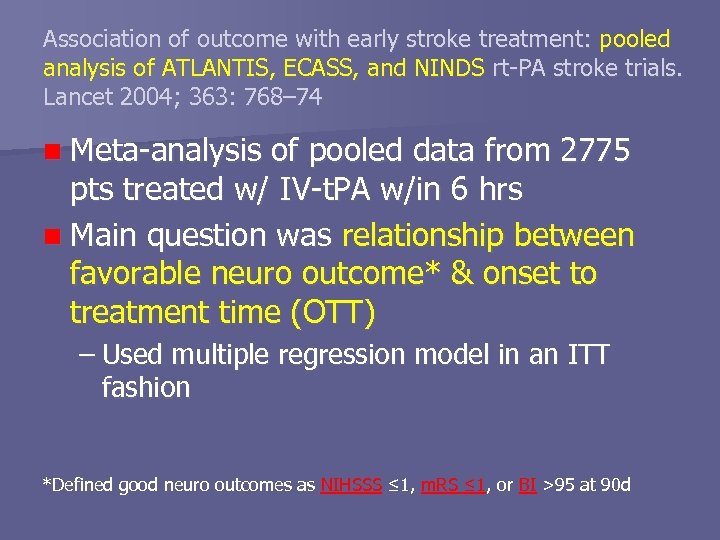
Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet 2004; 363: 768– 74 n Meta-analysis of pooled data from 2775 pts treated w/ IV-t. PA w/in 6 hrs n Main question was relationship between favorable neuro outcome* & onset to treatment time (OTT) – Used multiple regression model in an ITT fashion *Defined good neuro outcomes as NIHSSS ≤ 1, m. RS ≤ 1, or BI >95 at 90 d
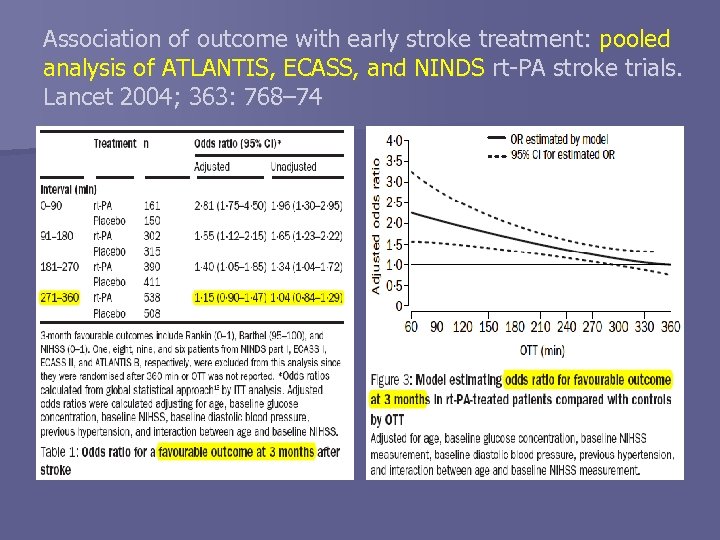
Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet 2004; 363: 768– 74
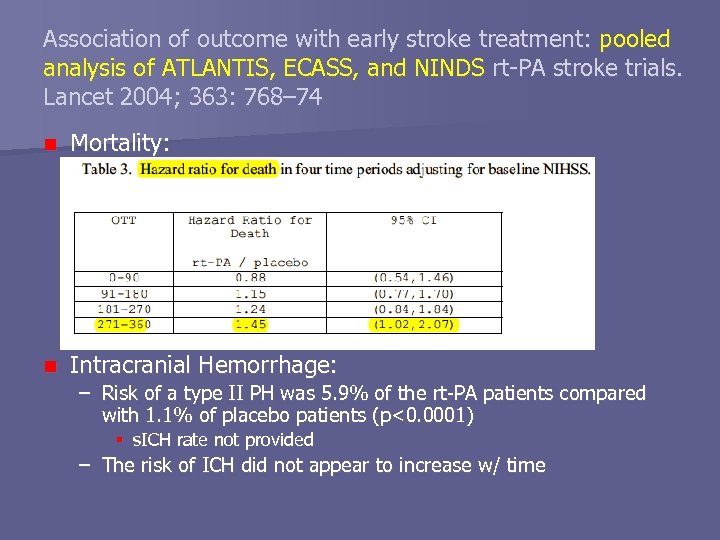
Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet 2004; 363: 768– 74 n Mortality: n Intracranial Hemorrhage: – Risk of a type II PH was 5. 9% of the rt-PA patients compared with 1. 1% of placebo patients (p<0. 0001) s. ICH rate not provided – The risk of ICH did not appear to increase w/ time
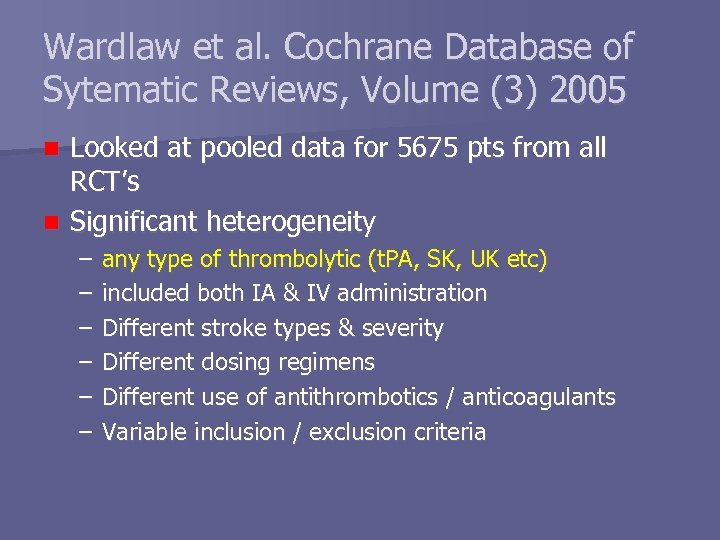
Wardlaw et al. Cochrane Database of Sytematic Reviews, Volume (3) 2005 Looked at pooled data for 5675 pts from all RCT’s n Significant heterogeneity n – – – any type of thrombolytic (t. PA, SK, UK etc) included both IA & IV administration Different stroke types & severity Different dosing regimens Different use of antithrombotics / anticoagulants Variable inclusion / exclusion criteria
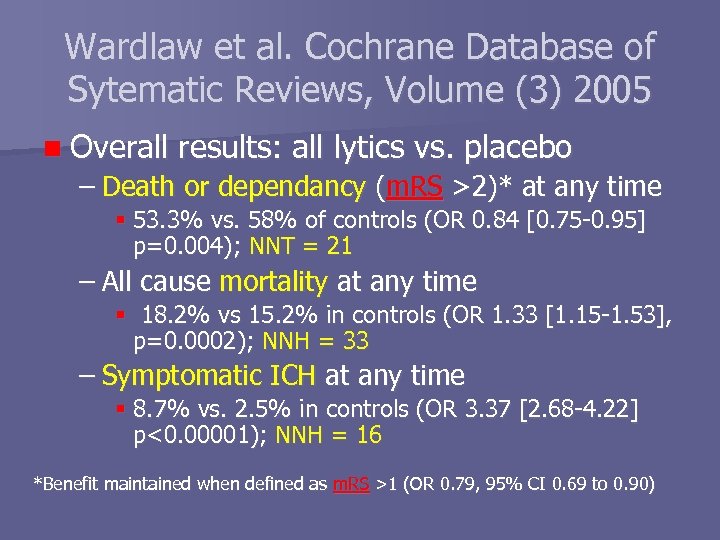
Wardlaw et al. Cochrane Database of Sytematic Reviews, Volume (3) 2005 n Overall results: all lytics vs. placebo – Death or dependancy (m. RS >2)* at any time 53. 3% vs. 58% of controls (OR 0. 84 [0. 75 -0. 95] p=0. 004); NNT = 21 – All cause mortality at any time 18. 2% vs 15. 2% in controls (OR 1. 33 [1. 15 -1. 53], p=0. 0002); NNH = 33 – Symptomatic ICH at any time 8. 7% vs. 2. 5% in controls (OR 3. 37 [2. 68 -4. 22] p<0. 00001); NNH = 16 *Benefit maintained when defined as m. RS >1 (OR 0. 79, 95% CI 0. 69 to 0. 90)
Bottomline Thrombolysis in AIS ASA in Acute Coronary Syndromes
Bad Ideas Part II
Thrombolysis in AIS: is it effective? Does t-PA work in the real world?
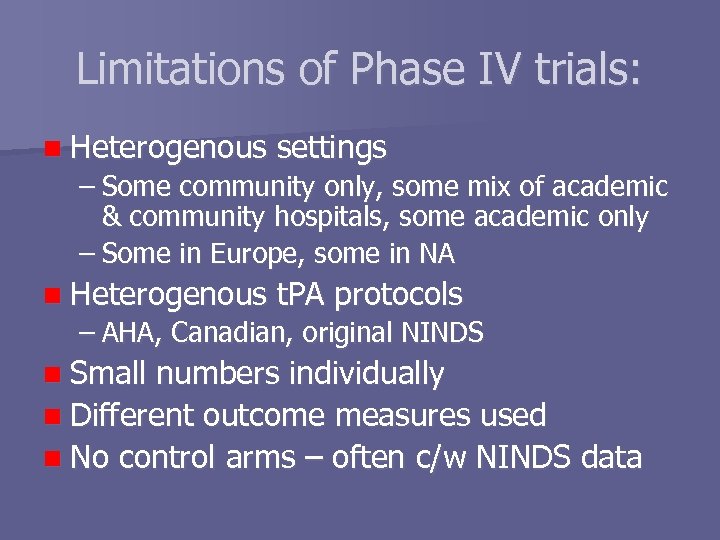
Limitations of Phase IV trials: n Heterogenous settings – Some community only, some mix of academic & community hospitals, some academic only – Some in Europe, some in NA n Heterogenous t. PA protocols – AHA, Canadian, original NINDS n Small numbers individually n Different outcome measures used n No control arms – often c/w NINDS data
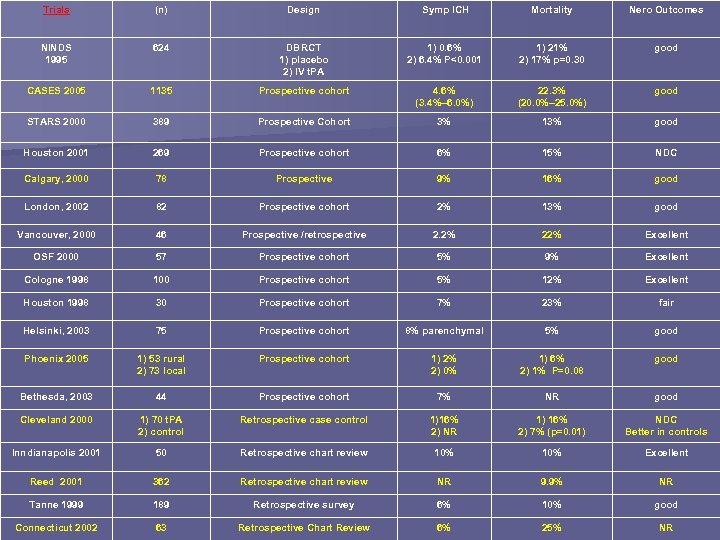
Trials (n) Design Symp ICH Mortality Nero Outcomes NINDS 1995 624 DBRCT 1) placebo 2) IV t. PA 1) 0. 6% 2) 6. 4% P<0. 001 1) 21% 2) 17% p=0. 30 good CASES 2005 1135 Prospective cohort 4. 6% (3. 4%– 6. 0%) 22. 3% (20. 0%– 25. 0%) good STARS 2000 389 Prospective Cohort 3% 13% good Houston 2001 269 Prospective cohort 6% 15% NDC Calgary, 2000 78 Prospective 9% 16% good London, 2002 82 Prospective cohort 2% 13% good Vancouver, 2000 46 Prospective /retrospective 2. 2% 22% Excellent OSF 2000 57 Prospective cohort 5% 9% Excellent Cologne 1998 100 Prospective cohort 5% 12% Excellent Houston 1998 30 Prospective cohort 7% 23% fair Helsinki, 2003 75 Prospective cohort 8% parenchymal 5% good Phoenix 2005 1) 53 rural 2) 73 local Prospective cohort 1) 2% 2) 0% 1) 6% 2) 1% P=0. 08 good Bethesda, 2003 44 Prospective cohort 7% NR good Cleveland 2000 1) 70 t. PA 2) control Retrospective case control 1)16% 2) NR 1) 16% 2) 7% (p=0. 01) NDC Better in controls Inndianapolis 2001 50 Retrospective chart review 10% Excellent Reed 2001 362 Retrospective chart review NR 9. 9% NR Tanne 1999 189 Retrospective survey 6% 10% good Connecticut 2002 63 Retrospective Chart Review 6% 25% NR
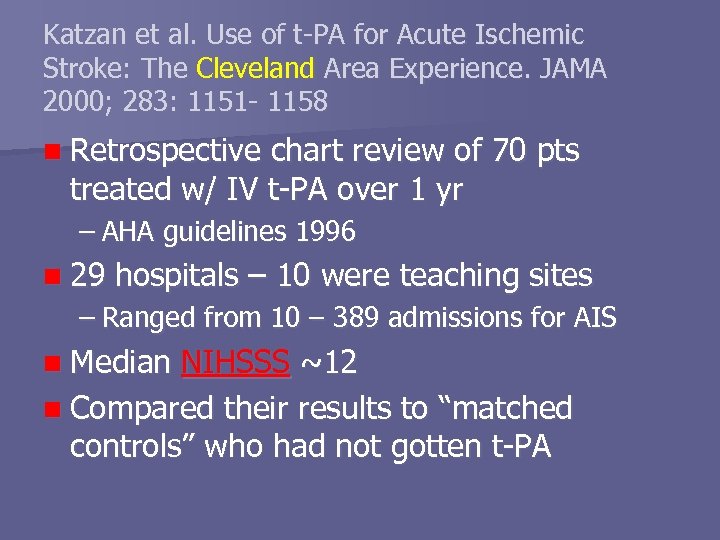
Katzan et al. Use of t-PA for Acute Ischemic Stroke: The Cleveland Area Experience. JAMA 2000; 283: 1151 - 1158 n Retrospective chart review of 70 pts treated w/ IV t-PA over 1 yr – AHA guidelines 1996 n 29 hospitals – 10 were teaching sites – Ranged from 10 – 389 admissions for AIS n Median NIHSSS ~12 n Compared their results to “matched controls” who had not gotten t-PA
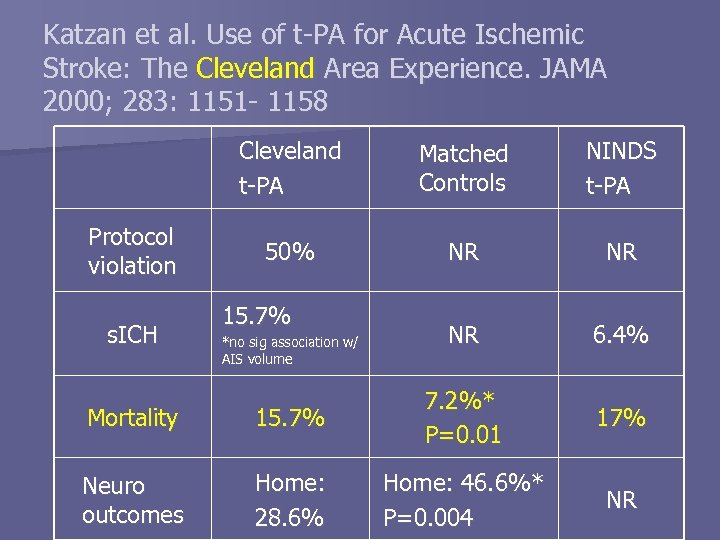
Katzan et al. Use of t-PA for Acute Ischemic Stroke: The Cleveland Area Experience. JAMA 2000; 283: 1151 - 1158 Cleveland t-PA Protocol violation s. ICH Matched Controls NINDS t-PA 50% NR NR NR 6. 4% 17% NR 15. 7% *no sig association w/ AIS volume Mortality 15. 7% 7. 2%* P=0. 01 Neuro outcomes Home: 28. 6% Home: 46. 6%* P=0. 004
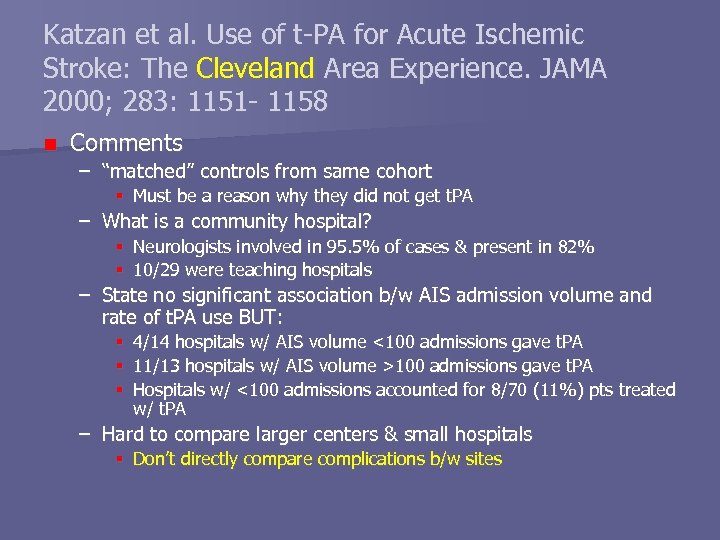
Katzan et al. Use of t-PA for Acute Ischemic Stroke: The Cleveland Area Experience. JAMA 2000; 283: 1151 - 1158 n Comments – “matched” controls from same cohort Must be a reason why they did not get t. PA – What is a community hospital? Neurologists involved in 95. 5% of cases & present in 82% 10/29 were teaching hospitals – State no significant association b/w AIS admission volume and rate of t. PA use BUT: 4/14 hospitals w/ AIS volume <100 admissions gave t. PA 11/13 hospitals w/ AIS volume >100 admissions gave t. PA Hospitals w/ <100 admissions accounted for 8/70 (11%) pts treated w/ t. PA – Hard to compare larger centers & small hospitals Don’t directly compare complications b/w sites
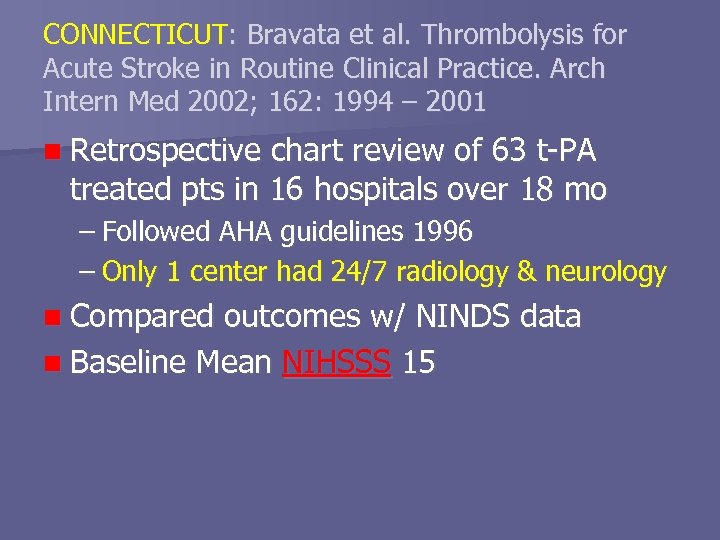
CONNECTICUT: Bravata et al. Thrombolysis for Acute Stroke in Routine Clinical Practice. Arch Intern Med 2002; 162: 1994 – 2001 n Retrospective chart review of 63 t-PA treated pts in 16 hospitals over 18 mo – Followed AHA guidelines 1996 – Only 1 center had 24/7 radiology & neurology n Compared outcomes w/ NINDS data n Baseline Mean NIHSSS 15
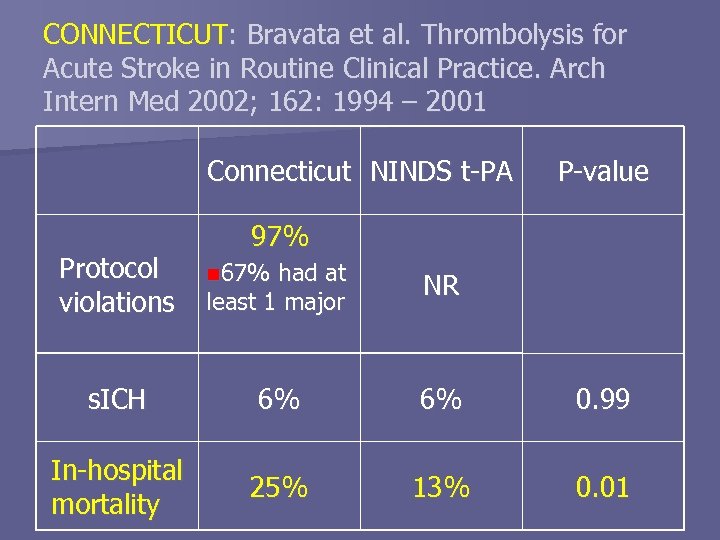
CONNECTICUT: Bravata et al. Thrombolysis for Acute Stroke in Routine Clinical Practice. Arch Intern Med 2002; 162: 1994 – 2001 Connecticut NINDS t-PA Protocol violations P-value 97% n 67% had at least 1 major NR s. ICH 6% 6% 0. 99 In-hospital mortality 25% 13% 0. 01
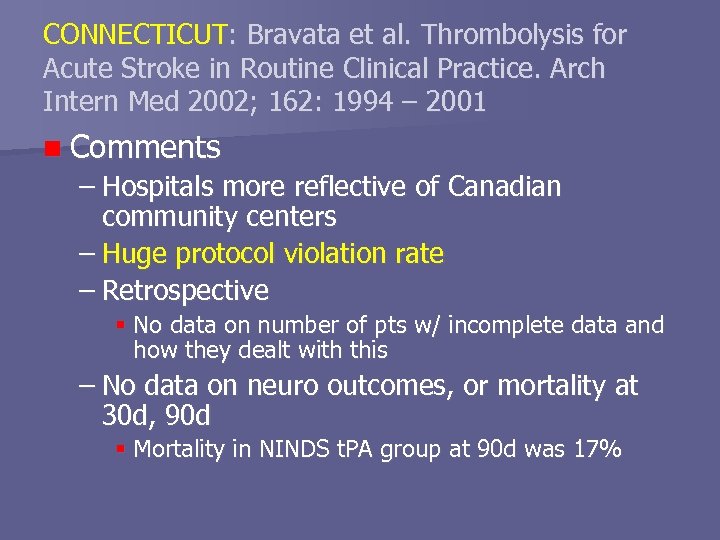
CONNECTICUT: Bravata et al. Thrombolysis for Acute Stroke in Routine Clinical Practice. Arch Intern Med 2002; 162: 1994 – 2001 n Comments – Hospitals more reflective of Canadian community centers – Huge protocol violation rate – Retrospective No data on number of pts w/ incomplete data and how they dealt with this – No data on neuro outcomes, or mortality at 30 d, 90 d Mortality in NINDS t. PA group at 90 d was 17%
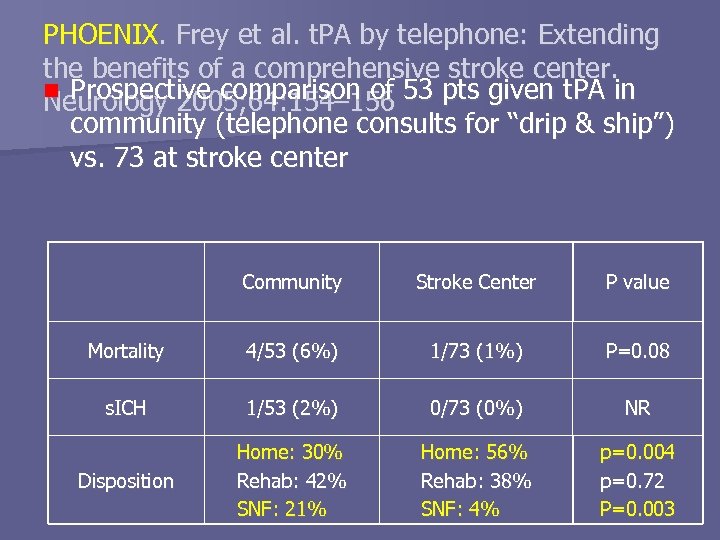
PHOENIX. Frey et al. t. PA by telephone: Extending the benefits of a comprehensive stroke center. n Prospective comparison of 53 pts given t. PA in Neurology 2005; 64: 154– 156 community (telephone consults for “drip & ship”) vs. 73 at stroke center Community Stroke Center P value Mortality 4/53 (6%) 1/73 (1%) P=0. 08 s. ICH 1/53 (2%) 0/73 (0%) NR Disposition Home: 30% Rehab: 42% SNF: 21% Home: 56% Rehab: 38% SNF: 4% p=0. 004 p=0. 72 P=0. 003
PHOENIX. Frey et al. t. PA by telephone: Extending the benefits of a comprehensive stroke center. Neurology 2005; 64: 154– 156 n Comments – Results suggest pts do better when treated in Stroke Center, but Community-treated pts were described as older, w/ more severe strokes Poor methods description – hard to assess The protocol violation rate is not provided Not sure if the difference in s. ICH is significant
Reed et al. Treatment With Tissue Plasminogen Activator and Inpatient Mortality Rates for Patients With Ischemic Stroke Treated in Community Hospitals. Stroke. 2001; 32: 1832 -1840 n Retrospective review of 362 pts treated w/ IV t. PA at 137 hospitals – 34% teaching centers, 78% had Neurosurgery n Results – – – In-hospital mortality 9. 9% (6. 9 – 13%) Final Disposition was home in 36% Multivariate analysis No significant interaction w/ teaching vs nonteaching hospital, or urban vs rural & likelihood of death
Reed et al. Treatment With Tissue Plasminogen Activator and Inpatient Mortality Rates for Patients With Ischemic Stroke Treated in Community Hospitals. Stroke. 2001; 32: 1832 -1840 n Comments: – Heterogenous collection of “community” hospitals – No baseline NIHSSS scores – No data on protocol violations – No data on symptomatic ICH – No neuro outcome data – Retrospective w/ poorly defined methods
CALGARY: Buchan et al. Effectiveness of t-PA in acute ischemic stroke: Outcome relates to appropriateness. Neurology 2000; 54(3): 679 n Prospective cohort of 68 consecutive pts treated w/ IV t-PA at FMC using NINDS protocol over 30 mo period n Baseline Mean NIHSS 15 n Compared outcomes to NINDS
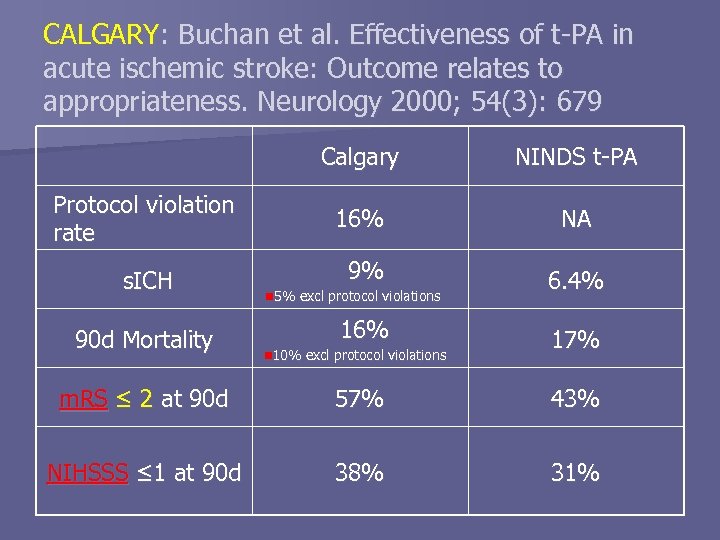
CALGARY: Buchan et al. Effectiveness of t-PA in acute ischemic stroke: Outcome relates to appropriateness. Neurology 2000; 54(3): 679 Calgary NINDS t-PA Protocol violation rate 16% NA s. ICH 9% 6. 4% 90 d Mortality n 5% excl protocol violations 16% n 10% excl protocol violations 17% m. RS ≤ 2 at 90 d 57% 43% NIHSSS ≤ 1 at 90 d 38% 31%
CALGARY: Buchan et al. Effectiveness of t-PA in acute ischemic stroke: Outcome relates to appropriateness. Neurology 2000; 54(3): 679 n Comment – Protocol violation associated w/ significantly higher risk of s. ICH, mortality, & worse neuro outcome 6/57 (10%) deaths in protocol pts vs 5/11 (46%) in violators (p < 0. 01) – Calculated NNT relative to the NINDS study placebo group NNT = 6 for good outcome (NIHSS score 0 to 1) NNT = 3 for independence (m. RS 0 -2)
CASES: Hill et al. Thrombolysis for acute ischemic stroke: results of the Canadian Alteplase for Stroke Effectiveness Study CMAJ 2005; 172(10): 1307 -12 n Prospective registry of 1135* t-PA treated AIS pts at 60 Canadian hospitals in 2. 5 yrs – 33 community, 27 academic 10 “high volume” centers = >1 pt treated/mo – Treated 61% of all pts n Median NIHSSS 14 at baseline n Looked at outcomes at 90 d * Estimate this accounts for 84% of all AIS pts treated w/ t. PA in Canada during study period
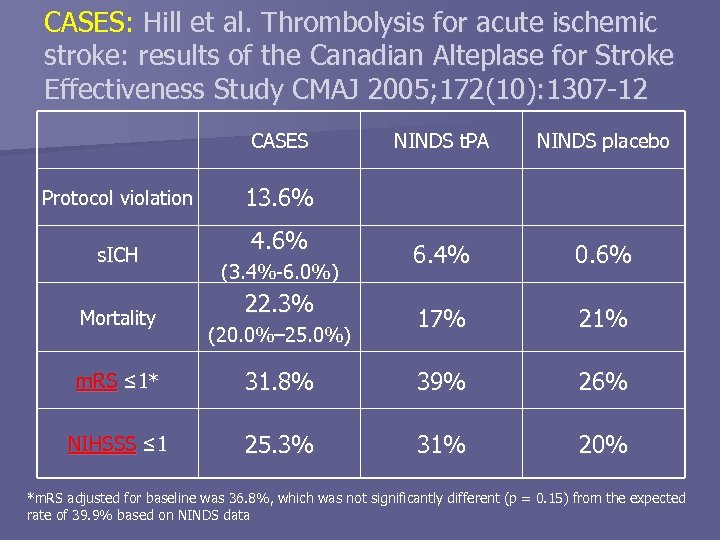
CASES: Hill et al. Thrombolysis for acute ischemic stroke: results of the Canadian Alteplase for Stroke Effectiveness Study CMAJ 2005; 172(10): 1307 -12 CASES Protocol violation s. ICH Mortality NINDS t. PA NINDS placebo 6. 4% 0. 6% 17% 21% 13. 6% 4. 6% (3. 4%-6. 0%) 22. 3% (20. 0%– 25. 0%) m. RS ≤ 1* 31. 8% 39% 26% NIHSSS ≤ 1 25. 3% 31% 20% *m. RS adjusted for baseline was 36. 8%, which was not significantly different (p = 0. 15) from the expected rate of 39. 9% based on NINDS data
CASES: Hill et al. Thrombolysis for acute ischemic stroke: results of the Canadian Alteplase for Stroke Effectiveness Study CMAJ 2005; 172(10): 1307 -12 n Multivariate Analysis – Found no significant difference in rate of neuro outcomes or s. ICH b/w pts treated at: High volume vs. low volume center Community vs. academic center – Found significant relationship b/w protocol violation & risk of s. ICH 7. 8% v. 3. 9%; RR 2. 0, 95%CI 1. 1– 3. 8 – Predictors of s. ICH: – Elevated glucose (OR 1. 6, 95% CI 1. 2– 2. 3 per 5 -mmol/L increase) – Increased time from stroke onset to Tx (OR 1. 2, 95% CI 1. 0– 1. 5 per 30 -minute increase)
Conclusions n IV t-PA improves neuro outcomes in select AIS pts in RCTs – Benefit diminishes rapidly with time n IV t-PA has a narrow therapeutic index – Need to select pts carefully & stick to protocol Multiple case series report results similar to NINDS in routine clinical use n The data to support or refute use of t-PA in community centers is limited & difficult to interpret n
Conclusions So should we give t-PA in Lethbridge? n Currently no n Tomorrow maybe yes, provided: n – – – Establishment of detailed protocol Telephone consult to stroke team at FMC Transmission of CT images to FMC Transfer for all t-PA pts to FMC Rigorous QI/QA process to track & address Protocol violation rate Outcomes of pts treated in periphery vs. at stroke center

Questions? Bad Ideas Part III
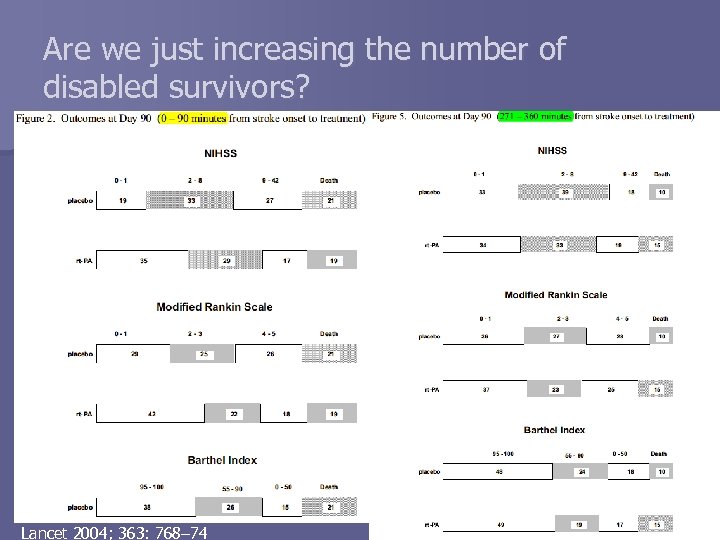
Are we just increasing the number of disabled survivors? Lancet 2004; 363: 768– 74
Barriers to t-PA Tx in CVA n Systematic review: – failure to recognise symptoms of stroke or seek urgent help – Failure to call for and ambulance first – Incorrect triage as non-urgent by paramedics or ED staff – delays in neuroimaging, – Inefficient stroke care pathways – Obtaining informed consent – Physician inexperience & uncertainty w/ giving thrombolytics in CVA Kwan et al. Age and Ageing 2004; 33: 116– 121
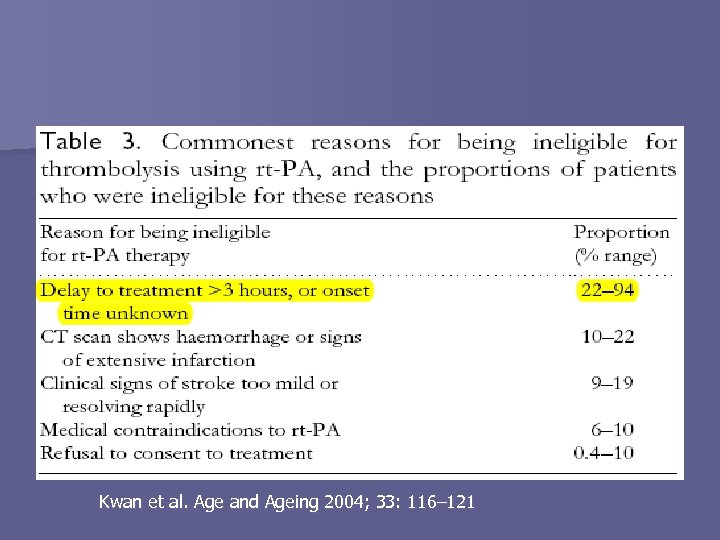
Kwan et al. Age and Ageing 2004; 33: 116– 121
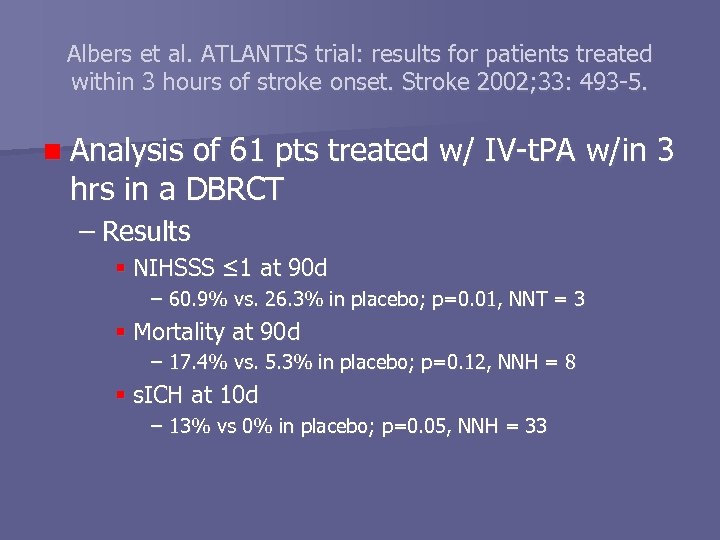
Albers et al. ATLANTIS trial: results for patients treated within 3 hours of stroke onset. Stroke 2002; 33: 493 -5. n Analysis of 61 pts treated w/ IV-t. PA w/in 3 hrs in a DBRCT – Results NIHSSS ≤ 1 at 90 d – 60. 9% vs. 26. 3% in placebo; p=0. 01, NNT = 3 Mortality at 90 d – 17. 4% vs. 5. 3% in placebo; p=0. 12, NNH = 8 s. ICH at 10 d – 13% vs 0% in placebo; p=0. 05, NNH = 33
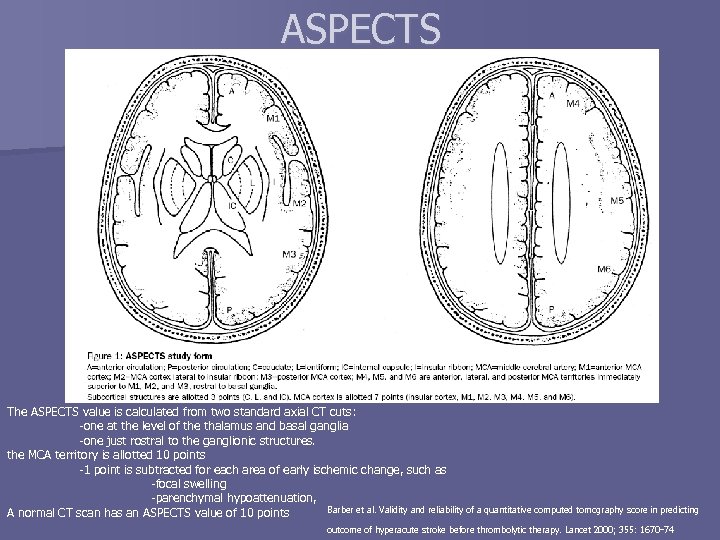
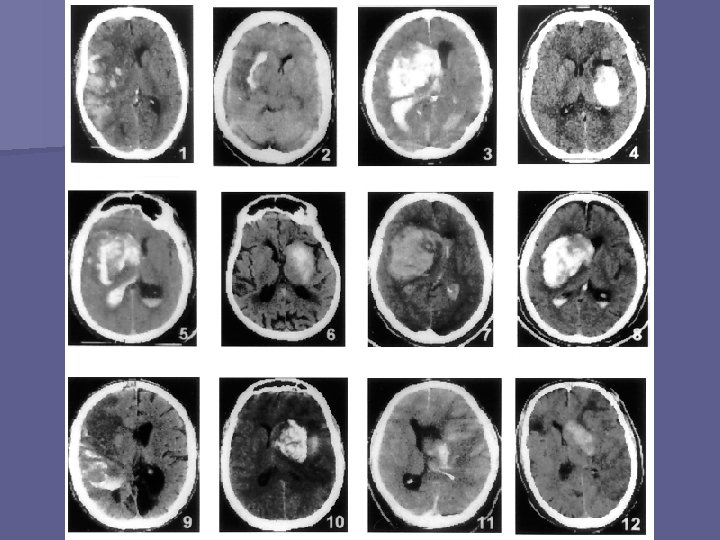
ASPECTS The ASPECTS value is calculated from two standard axial CT cuts: -one at the level of the thalamus and basal ganglia -one just rostral to the ganglionic structures. the MCA territory is allotted 10 points -1 point is subtracted for each area of early ischemic change, such as -focal swelling -parenchymal hypoattenuation, Barber et al. Validity and reliability of a quantitative computed tomography score in predicting A normal CT scan has an ASPECTS value of 10 points outcome of hyperacute stroke before thrombolytic therapy. Lancet 2000; 355: 1670– 74
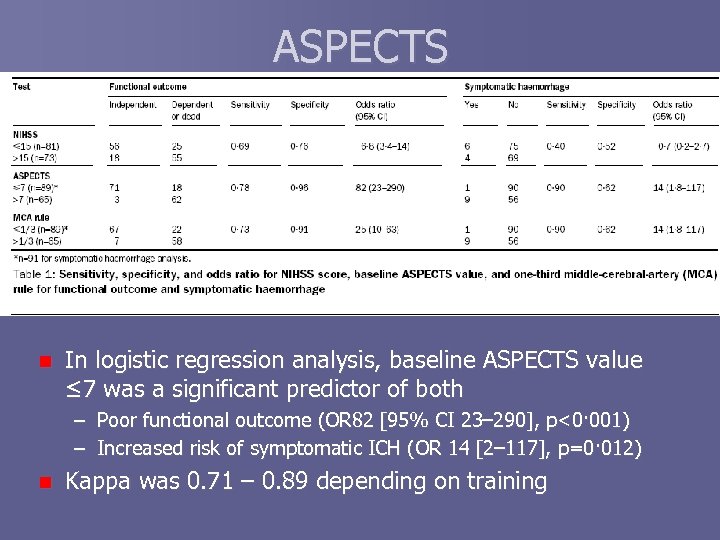
ASPECTS n In logistic regression analysis, baseline ASPECTS value ≤ 7 was a significant predictor of both – Poor functional outcome (OR 82 [95% CI 23– 290], p<0· 001) – Increased risk of symptomatic ICH (OR 14 [2– 117], p=0· 012) n Kappa was 0. 71 – 0. 89 depending on training
IV t-PA >3 hrs n Meta-analyses suggest modest benefit after 3 hrs – rapidly diminishes w/ time n New strategies to select pts w/ potentially reversible ischemia – DWI/PWI MRI Clinical – MRI mismatch – CT perfusion imaging (CTP) Estimates blood volume as ml /100 g brain tissue – Both need further study & validation
How does t-PA cause ICH? n Proposed mechanisms – interaction with NMDA receptors, promoting calcium influx into ischemic cells excitotoxicity – enhances degradative enzymatic activity in the intercellular matrix by up-regulating MMP-9, which leads to disruption of tissue integrity and may predispose to hemorrhage n giving inhibitors of these effects may minimize the side effects & this is under investigation: – – – caffeine & Et. OH in combo albumin Magnesium Hypothermia Oxygen Steroids Frey. Recombinant Tissue Plasminogen Activator (rt. PA) for Stroke: The perspective at 8 years. Neurologist 2005; 11: 123– 133
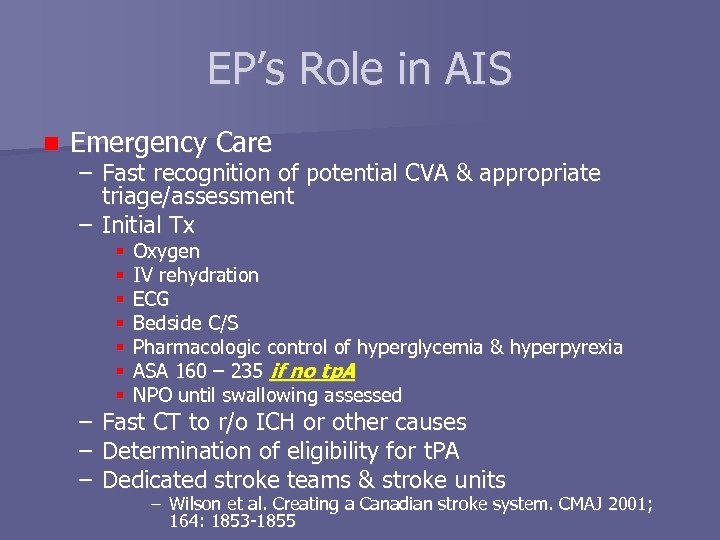
EP’s Role in AIS n Emergency Care – Fast recognition of potential CVA & appropriate triage/assessment – Initial Tx – – – Oxygen IV rehydration ECG Bedside C/S Pharmacologic control of hyperglycemia & hyperpyrexia ASA 160 – 235 if no tp. A NPO until swallowing assessed Fast CT to r/o ICH or other causes Determination of eligibility for t. PA Dedicated stroke teams & stroke units – Wilson et al. Creating a Canadian stroke system. CMAJ 2001; 164: 1853 -1855
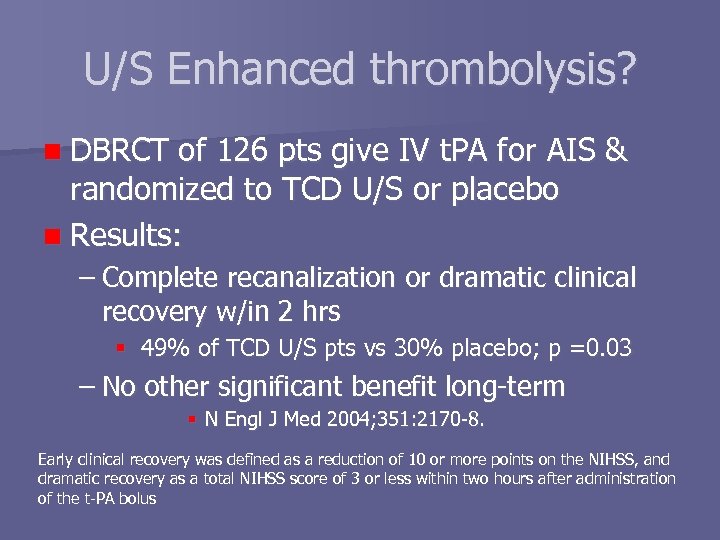
U/S Enhanced thrombolysis? n DBRCT of 126 pts give IV t. PA for AIS & randomized to TCD U/S or placebo n Results: – Complete recanalization or dramatic clinical recovery w/in 2 hrs 49% of TCD U/S pts vs 30% placebo; p =0. 03 – No other significant benefit long-term N Engl J Med 2004; 351: 2170 -8. Early clinical recovery was defined as a reduction of 10 or more points on the NIHSS, and dramatic recovery as a total NIHSS score of 3 or less within two hours after administration of the t-PA bolus
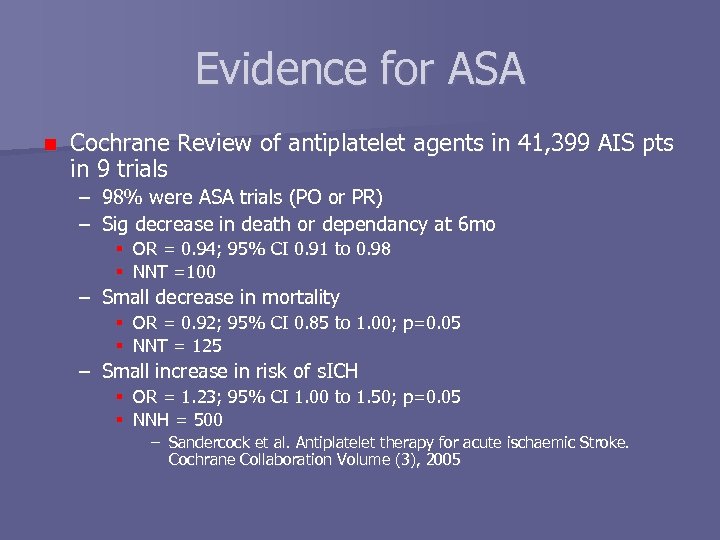
Evidence for ASA n Cochrane Review of antiplatelet agents in 41, 399 AIS pts in 9 trials – 98% were ASA trials (PO or PR) – Sig decrease in death or dependancy at 6 mo OR = 0. 94; 95% CI 0. 91 to 0. 98 NNT =100 – Small decrease in mortality OR = 0. 92; 95% CI 0. 85 to 1. 00; p=0. 05 NNT = 125 – Small increase in risk of s. ICH OR = 1. 23; 95% CI 1. 00 to 1. 50; p=0. 05 NNH = 500 – Sandercock et al. Antiplatelet therapy for acute ischaemic Stroke. Cochrane Collaboration Volume (3), 2005
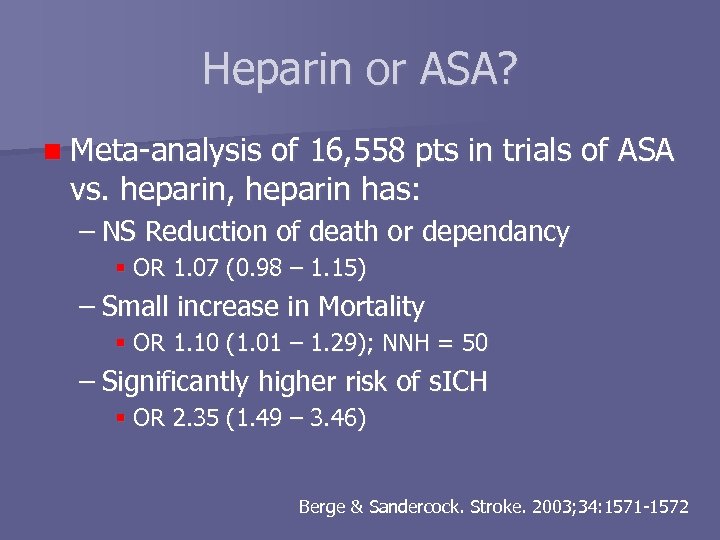
Heparin or ASA? n Meta-analysis of 16, 558 pts in trials of ASA vs. heparin, heparin has: – NS Reduction of death or dependancy OR 1. 07 (0. 98 – 1. 15) – Small increase in Mortality OR 1. 10 (1. 01 – 1. 29); NNH = 50 – Significantly higher risk of s. ICH OR 2. 35 (1. 49 – 3. 46) Berge & Sandercock. Stroke. 2003; 34: 1571 -1572
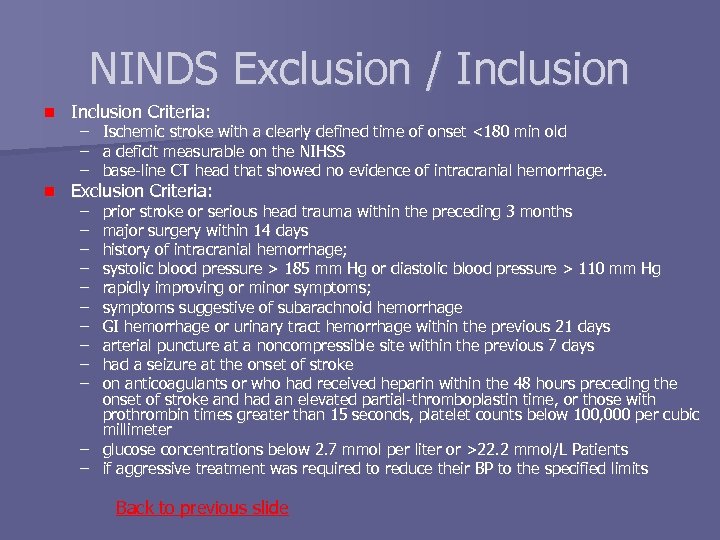
NINDS Exclusion / Inclusion n Inclusion Criteria: n Exclusion Criteria: – – – Ischemic stroke with a clearly defined time of onset <180 min old a deficit measurable on the NIHSS base-line CT head that showed no evidence of intracranial hemorrhage. – – – – – prior stroke or serious head trauma within the preceding 3 months major surgery within 14 days history of intracranial hemorrhage; systolic blood pressure > 185 mm Hg or diastolic blood pressure > 110 mm Hg rapidly improving or minor symptoms; symptoms suggestive of subarachnoid hemorrhage GI hemorrhage or urinary tract hemorrhage within the previous 21 days arterial puncture at a noncompressible site within the previous 7 days had a seizure at the onset of stroke on anticoagulants or who had received heparin within the 48 hours preceding the onset of stroke and had an elevated partial-thromboplastin time, or those with prothrombin times greater than 15 seconds, platelet counts below 100, 000 per cubic millimeter – glucose concentrations below 2. 7 mmol per liter or >22. 2 mmol/L Patients – if aggressive treatment was required to reduce their BP to the specified limits Back to previous slide
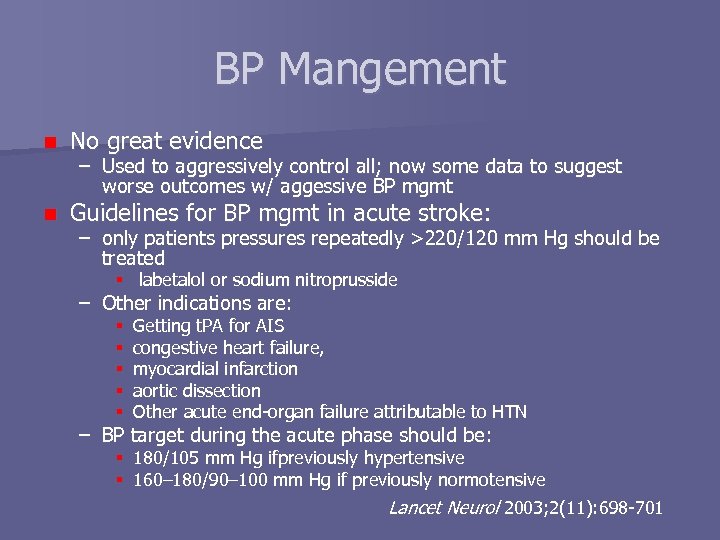
BP Mangement n No great evidence n Guidelines for BP mgmt in acute stroke: – Used to aggressively control all; now some data to suggest worse outcomes w/ aggessive BP mgmt – only patients pressures repeatedly >220/120 mm Hg should be treated labetalol or sodium nitroprusside – Other indications are: Getting t. PA for AIS congestive heart failure, myocardial infarction aortic dissection Other acute end-organ failure attributable to HTN – BP target during the acute phase should be: 180/105 mm Hg ifpreviously hypertensive 160– 180/90– 100 mm Hg if previously normotensive Lancet Neurol 2003; 2(11): 698 -701
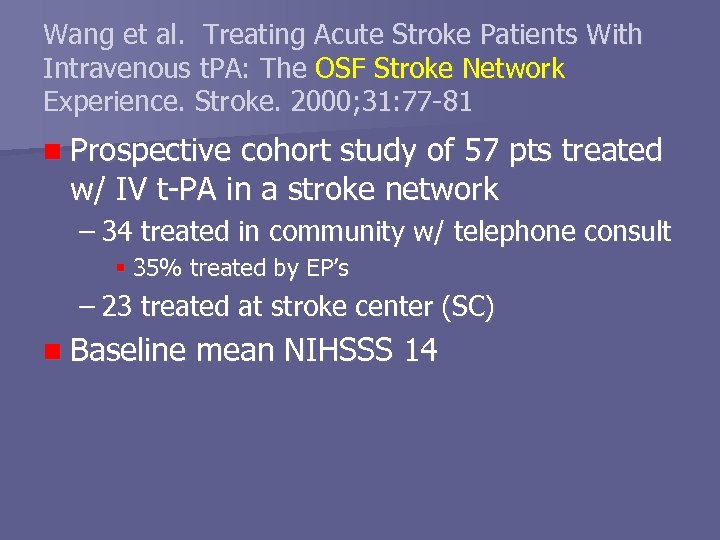
Wang et al. Treating Acute Stroke Patients With Intravenous t. PA: The OSF Stroke Network Experience. Stroke. 2000; 31: 77 -81 n Prospective cohort study of 57 pts treated w/ IV t-PA in a stroke network – 34 treated in community w/ telephone consult 35% treated by EP’s – 23 treated at stroke center (SC) n Baseline mean NIHSSS 14
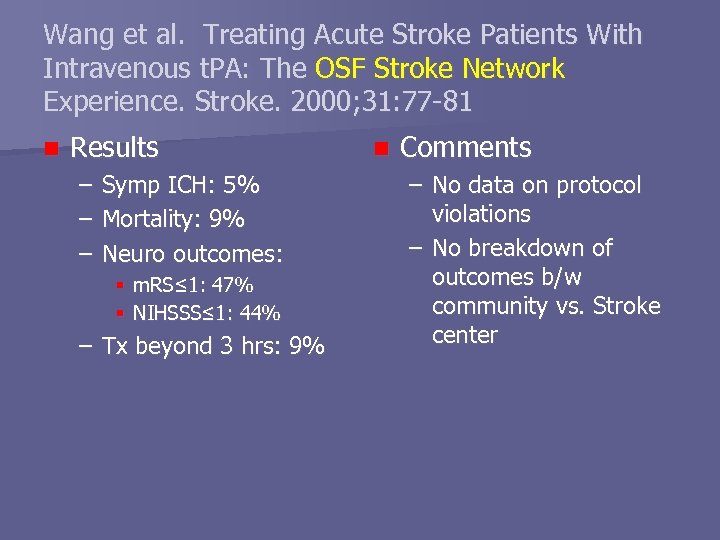
Wang et al. Treating Acute Stroke Patients With Intravenous t. PA: The OSF Stroke Network Experience. Stroke. 2000; 31: 77 -81 n Results – – – Symp ICH: 5% Mortality: 9% Neuro outcomes: m. RS≤ 1: 47% NIHSSS≤ 1: 44% – Tx beyond 3 hrs: 9% n Comments – No data on protocol violations – No breakdown of outcomes b/w community vs. Stroke center
80c4ad496767431f78ab6691ba19fe83.ppt