1934a97cb97e961dd081cc9384b0346f.ppt
- Количество слайдов: 59
Thought Disorder and Dissociative States Mark Y. Wahba Resident Rounds March 11/04
Some slides courtesy of § Dr. Moritz Haager, International man of mystery § Thought, Mood, and Personality Disorders in the ED

Outline § Psychosis § Thought Disorders § § § § § Schizophrenia Schizoaffective Disorder Delusional Disorder Brief Psychotic Episode Culture-Bound Syndromes Dissociative Disorders Medical Clearance Restraints Medications
Psychosis § “Psychosis is a disorder of thinking and perception in which information processing and reality testing are impaired, resulting in an inability to distinguish fantasy from reality” § www. emedicine. com/emerg/topic 520. htm § Many reasons for psychosis
Medical conditions associated with Psychosis § Substance abuse and drug toxicity § Central nervous system lesions— § § § tumor (especially limbic and pituitary), aneurysm, abscess Head trauma Infections—encephalitis, abscess, neurosyphilis Endocrine disease—thyroid, Cushing’s, Addison’s, pituitary, parathyroid Systemic lupus erythematosus and multiple sclerosis Cerebrovascular disease § Huntington’s disease § Parkinson’s disease § Migraine headache and temporal § § § arteritis Pellagra and pernicious anemia Porphyria Withdrawal states, including alcohol and benzodiazepines Delirium and dementia Sensory deprivation or over stimulation states can induce psychosis, such as psychosis induced in the intensive care unit
Schizophrenia § “Schizophrenia is a complex illness or group of disorders characterized by hallucinations, delusions, behavioral disturbances, disrupted social functioning, and associated symptoms in what is usually an otherwise clear sensorium” § Jacobson: Psychiatric Secrets, 2 nd ed. , Copyright © 2001 Hanley and Belfus § “Results in fluctuating, gradually deteriorating, or relatively stable disturbances in thinking, behavior, and perception” § www. emedicine. com/emerg/topic 520. htm

What are the symptoms of schizophrenia? § Schizophrenia involves at least a 6 -month period of continuous signs § § of the illness Delusions: false beliefs that (1) persist despite what most people would accept as evidence to the contrary and (2) are not shared by others in the same culture or subculture. Hallucinations: perceptions that appear to be real when no such stimulus is actually present. Grossly disorganized or catatonic behavior. Catatonia, a syndrome characterized by stupor with rigidity or flexibility of the musculature, may alternate with periods of overactivity Negative symptoms: (1) affective flattening or decreased emotional reactivity; (2) alogia or poverty of speech; (3) avolition or lack of goal directed activity
Schizophrenia: Facts § Etiology: Unknown § Incidence is 1% § Same across racial, cultural, and international lines § Approximately 40% of people with schizophrenia attempt suicide § 10– 20% succeed

Schizophrenia: Facts § Lost productivity in the United States costs an § § § estimated $20 billion per year 2. 5% of each healthcare dollar spent 1990, direct and indirect costs were estimated to be $33 billion Schizophrenic patients occupy as many as 25% of all hospital beds at any given time § Schizophrenia Gerstein PS http: //www. emedicine. com/emerg/topic 520. htm accessed Jan 27/04
How is schizophrenia differentiated from other psychiatric conditions? § Affective disorders: the duration of psychotic symptoms is § § relatively brief in relation to the affective symptoms Schizophreniform disorder, by definition, involves the symptoms of schizophrenia with a duration of less than 6 months Obsessive-compulsive disorder may have beliefs that border on delusions but generally recognize that their symptoms are at least somewhat irrational Brief reactive psychoses may be seen in patients with borderline or other personality disorders as well as dissociative disorders Posttraumatic stress disorder may involve visual, auditory, tactile, and olfactory hallucinations during flashbacks

Schizoaffective Disorder § Definition § “ an illness that combines symptoms of schizophrenia with a major affective disorder, i. e. , major depression or manic-depressive illness” § Jacobson: Psychiatric Secrets, 2 nd ed. , Copyright © 2001 Hanley and Belfus § “Pt must meet the diagnostic criteria for a major depressive episode or a manic episode concurrently with meeting the diagnostic criteria for the active phase of schizophrenia” § Kaplans and Sadock’s Synopsis of Psychiatry 8 th edition Williams and Wilkins Baltimore

How is schizoaffective disorder different from schizophrenia or bipolar affective disorder? § Psychotic symptoms are common during acute phases of bipolar affective disorder § In schizophrenia, the total duration of affective symptoms is brief relative to the total duration of the illness § In manic-depressive illness, delusions and hallucinations primarily occur during periods of mood instability
Delusional Disorder § “a condition of unknown cause whose chief feature is a nonbizarre delusion present for at least 1 month” § Jacobson: Psychiatric Secrets, 2 nd ed. , Copyright © 2001 Hanley and Belfus § Nonbizarre: involves situations that occur and are possible in real life § being followed, poisoned, infected, loved at a distance, being deceived by spouse or lover, having a disease
How do you differentiate it from Schizophrenia? 1. Nonbizzare delusions 2. minimal deterioration in personality or function 3. relative absence of other psychopathologic symptoms § No negative symptoms or catatonia § Don’t have hallucinations
Types of Delusions § Erotomania: a person, usually of higher status, is in love § § with the subject Grandiose: theme is one of inflated worth, power, knowledge, identity, or special relationship to a deity or important famous person Jealous: one’s sexual partner is unfaithful Persecutory: the person is being malevolently treated or conspired against in some way Somatic: the person has some physical defect, disorder, or disease
Brief Psychotic Disorder § Two concepts § symptoms may or may not meet criteria for schizophrenia 1. Short time § “less than one month but greater than one day” 2. May have developed in response to a severe psychosocial stressor or group of stressors
Brief Psychotic Disorder § Uncommon § Clinically: one major symptom of psychosis, abrupt onset

Culture Bound Psychotic Syndromes § Bulimia Nervosa - North America § Food binges, self induced vomiting, +/- depression, anorexia nervosa, substance abuse § Empacho - Mexico and Cuban. America § Inability to digest and excrete recently ingested food § Grisi siknis - Nicaragua § Headache, anxiety, anger, aimless running § Koro - Asia (my favorite) § Fear that penis will withdraw into abdomen causing death


Management § “Remain calm, empathetic and reassuring” § Ensure staff safety § Complete Hx and physical § Psychiatric interview § Assess pt’s complaint and understanding of current circumstances § Formal mental status examination

Mental Status Exam § A – appearance § S – speech § E – emotion (mood + affect) § P – perception § T – thought content + process § I – insight / judgment § C - cognition
Management § Assess potential for danger to themselves or others § Assess degree of dysfunction and ability to care for themselves in outpatient setting § Hospitalize § 1 st psychotic episode § Danger to themselves or others § Grossly debilitated
Management § “decision to hospitalize psychotic pts is complex and imprecise and often must be made in a short period with limited information” § Rosen’s 1547

Management § Form 1, Admission Certificate, Mental 1. 2. 3. Health Act, Section 2 Mental disorder Likely to present a danger to themself or others Unsuitable for admission to a facility other than a formal patient § Doesn’t want to come in voluntarily


Dissociative Disorders § Aka. “conversion disorders” § Essential feature: § “State of disrupted consciousness, memory, identity or perception of the environment” § Kaplans and Sadock’s Synopsis of Psychiatry 8 th edition Williams and Wilkins Baltimore

Dissociative Disorders § Pts have lost the sense of having one consciousness § Feel as though they have no identity, confused about who they are, or have multiple personalities § “everything that gives people their unique personalities-thoughts, feelings and actions- is abnormal in people with dissociative disorders” § Kaplans and Sadock’s Synopsis of Psychiatry 8 th edition Williams and Wilkins Baltimore

Dissociative Disorders § Dissociation arises as a self-defense against § trauma Two functions 1. helps people remove themselves from trauma at time of occurrence 2. delays the working through needed to place the trauma in perspective in their lives § Conflicting contradictory representations of the self are kept in separate mental compartments
Dissociative Disorders § Usually connected with trauma, personal conflicts, and poor relationships with others § “conversion” is used to indicate that the affects of the unsolvable problems are transformed into symptoms § Dissociative motor disorders, Dissociative anesthesia
Dissociative Disorders § DSM-IV has diagnostic criteria for 4 different Dissociative Disorders 1. Dissociative amnesia 2. Dissociative fugue 3. Dissociative identity disorder 4. Depersonalization disorder
Dissociative Amnesia § “Characterized by an inability to remember information, usually related to a stressful or traumatic event, that cannot be explained by ordinary forgetfulness, ingestion of substances or general medical condition” § Kaplans and Sadock’s Synopsis of Psychiatry 8 th edition Williams and Wilkins Baltimore

Dissociative Fugue § “Characterized by sudden and unexpected travel away from home or work, associated with an inability to recall the past and with confusion about a person’s personal identitiy or with the adoption of a new identity” § Kaplans and Sadock’s Synopsis of Psychiatry 8 th edition Williams and Wilkins Baltimore

Dissociative Identity Disorder § Most severe § “Characterized by the presence of two or more distinct personalities within a single person” § Kaplans and Sadock’s Synopsis of Psychiatry 8 th edition Williams and Wilkins Baltimore
Depersonalization Disorder § “Characterized by recurrent or persistent feelings of detachment from the body or mind” § Kaplans and Sadock’s Synopsis of Psychiatry 8 th edition Williams and Wilkins Baltimore

Dissociative Disorders § Management § Consult Psychiatry

Medical Clearance § What is medical clearance? § “Evaluation and treatment of organic causes of presenting psychiatric complaints, and any existing medical comorbidities prior to transfer of care to the psychiatric service. ”Emerg. Med. Clin. 18(2): 185 -198. 2000 § What constitutes a “medically clear” patient? § No physical illness identified § Known co morbid illness but not thought causative § Adequately treated medical condition
Medical Clearance § Are we doing a good job of “clearing” Pt’s? § Riba and Hale 1990: Psychosomatics 31(4): 400 -404 § Retrospective chart review of 137 pts in ED referred for psychiatric evaluation § 137 ED pts w/ psych sx § 68% had vitals done § HPI recorded in 33% § Cranial nerve exam in 20%

Medical Clearance § Functional (Psychiatric) vs. Organic § History “WHY NOW? ” § Precipitating events and chronology / acute stressors § baseline mental / physical status § prior psychiatric history / family psych hx § past medical history § Meds / Compliance thereof/ drugs of abuse § collateral hx (friends, family, EMS, old charts) § Is pt a potential danger to self or others? § MSE
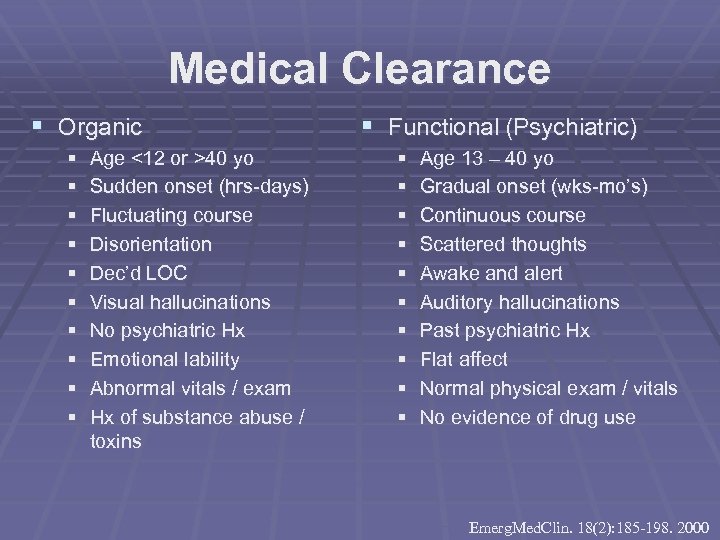
Medical Clearance § Organic § § § § § Age <12 or >40 yo Sudden onset (hrs-days) Fluctuating course Disorientation Dec’d LOC Visual hallucinations No psychiatric Hx Emotional lability Abnormal vitals / exam Hx of substance abuse / toxins § Functional (Psychiatric) § § § § § Age 13 – 40 yo Gradual onset (wks-mo’s) Continuous course Scattered thoughts Awake and alert Auditory hallucinations Past psychiatric Hx Flat affect Normal physical exam / vitals No evidence of drug use Emerg. Med. Clin. 18(2): 185 -198. 2000

Medical Clearance : Physical § Variety of presentations § agitated, combative, withdrawn, catatonic, cooperative with blunted affect § Examine all patients § attention to vital signs, pupillary findings, hydration status, and mental status. § Pay particular attention to fever and tachycardia § can be sign of neuroleptic malignant syndrome § Look for signs of dystonia, akathisia, tremor, muscle rigidity and Tardive dyskinesia § Mental status testing should typically reveal clear sensorium and orientation to person, place, and time. Assess attention, language, memory, constructions, and executive functions.
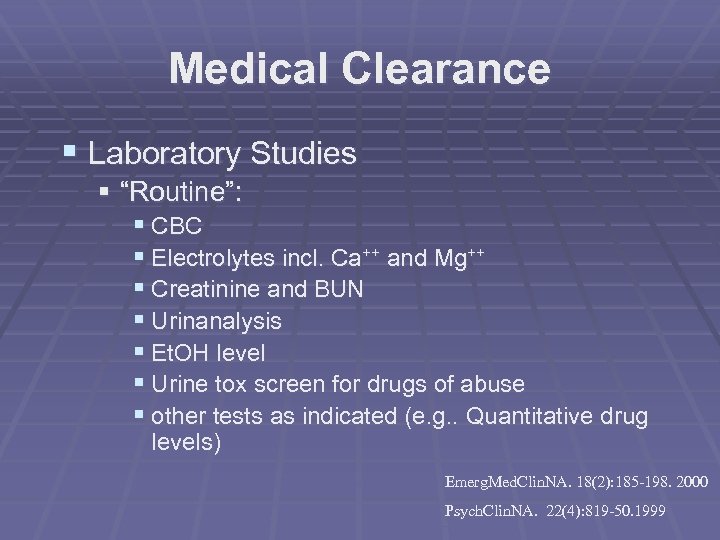
Medical Clearance § Laboratory Studies § “Routine”: § CBC § Electrolytes incl. Ca++ and Mg++ § Creatinine and BUN § Urinanalysis § Et. OH level § Urine tox screen for drugs of abuse § other tests as indicated (e. g. . Quantitative drug levels) Emerg. Med. Clin. NA. 18(2): 185 -198. 2000 Psych. Clin. NA. 22(4): 819 -50. 1999
Remember § psychiatric and organic illness can coexist and interact at the same time in the same patient § serious organic illness can be masked by acute psychiatric symptoms and difficulties obtaining a reliable Hx

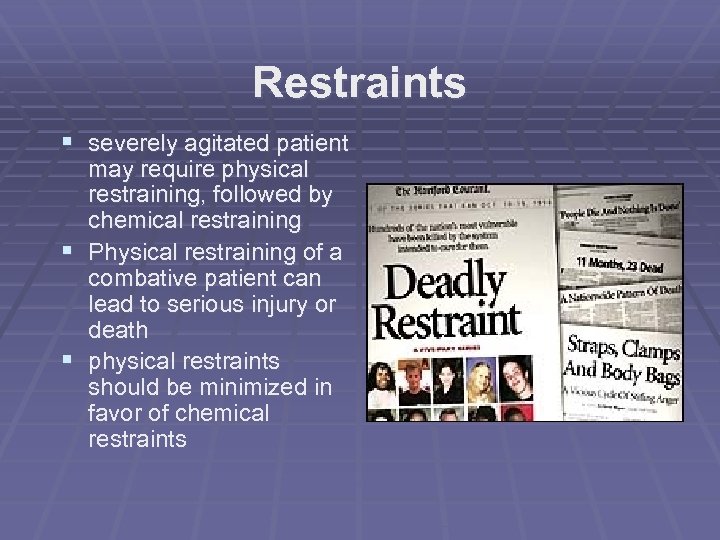
Restraints § severely agitated patient may require physical restraining, followed by chemical restraining § Physical restraining of a combative patient can lead to serious injury or death § physical restraints should be minimized in favor of chemical restraints
Restraints § Must document the reason, type and maximum duration of restraint § See CHR Guideline for Patients Requiring Mechanical/Chemical Restraint § Rosen’s 5 th ed. “The Combative Patient” P. 2591 § “The treating physician should not actively participate in applying restraints to preserve the physician-patient relationship and not be viewed as adversarial” p. 2595
Medications § All antipsychotics treat the positive symptoms § hallucinations, agitation, restructure disordered thinking § Atypical antipsychotic agents assist with the negative symptoms § flat affect, avolition, social withdrawal, poverty of speech and thought § less sedating, fewer movement disorders § Block dopamine receptors in several areas of the brain

Medications § Neuroleptic § old term used to describe antipsychotics due to their high degree of sedation § No longer appropriate b/c new agents cause little sedation

Medications in the ED § For sedation or rapid tranquilization § Haloperidol (Haldol) § § Butyrophenone derivative 5 mg IM/PO § Lorazepam (Ativan) § Benzodiazepine § 2 mg IM/PO/IV/SL § Combo of lorazepam 2 mg mixed in the same syringe with haloperidol 5 or 10 mg given IM or IV. Repeat q 2030 min § “The Haldol Hammer”
Atypical Antipsychotics § less likely to produce dystonia and tardive dyskinesia and more likely to improve negative symptoms § Quetiapine (Seroquel) § § Sedating in 15 min, give to “take the edge off” 25 to 50 mg po § Olanzapine (Zyprexa, Zydis wafer) § 5 mg or 10 mg po § Resperidone (Risperdal, M-tab) § 2 mg tab po § M-tab Coming soon to a hospital near you

“Big time” Medications § Zuclopenthixol deconate (Accuphase) § A thioxanthene § Depot antipsychotic given by IM injection § Dose 50 -150 mg IM § Sedates pt up to 72 hours
Medication Side effects Extrapyramidal syndromes § Acute dystonia § muscle rigidity and spasm § Laryngeal dystonia § Oculogyric crisis § bizarre upward gaze paralysis and contortion of facial and neck musculature § Akathisia § dysphoric sense of motor restlessness § Benztropine 2 mg po/IM or Diphenhydramine 50 mg IM/IV § Above +/or benzodiazepine
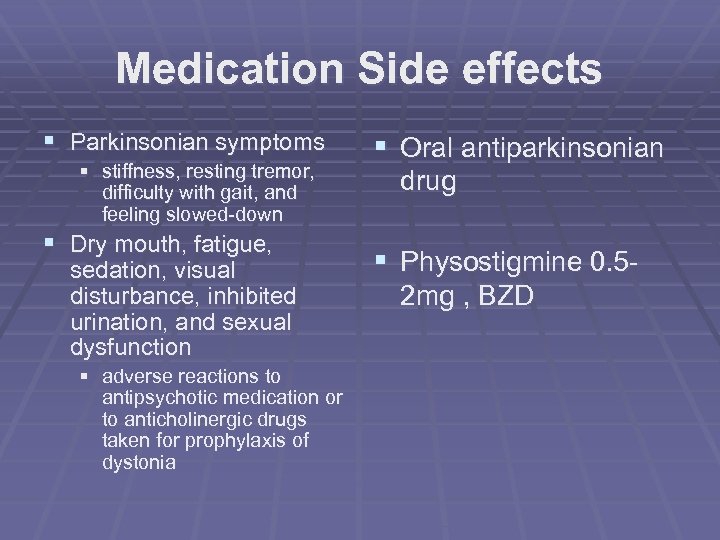
Medication Side effects § Parkinsonian symptoms § stiffness, resting tremor, difficulty with gait, and feeling slowed-down § Dry mouth, fatigue, sedation, visual disturbance, inhibited urination, and sexual dysfunction § adverse reactions to antipsychotic medication or to anticholinergic drugs taken for prophylaxis of dystonia § Oral antiparkinsonian drug § Physostigmine 0. 52 mg , BZD
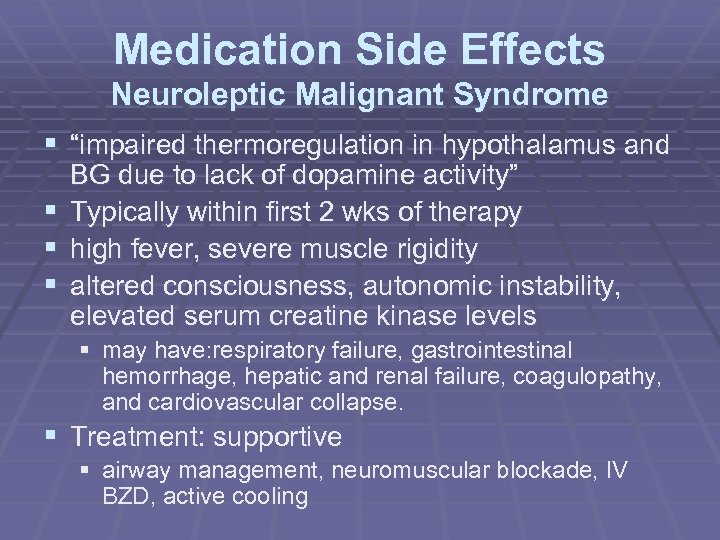
Medication Side Effects Neuroleptic Malignant Syndrome § “impaired thermoregulation in hypothalamus and § § § BG due to lack of dopamine activity” Typically within first 2 wks of therapy high fever, severe muscle rigidity altered consciousness, autonomic instability, elevated serum creatine kinase levels § may have: respiratory failure, gastrointestinal hemorrhage, hepatic and renal failure, coagulopathy, and cardiovascular collapse. § Treatment: supportive § airway management, neuromuscular blockade, IV BZD, active cooling

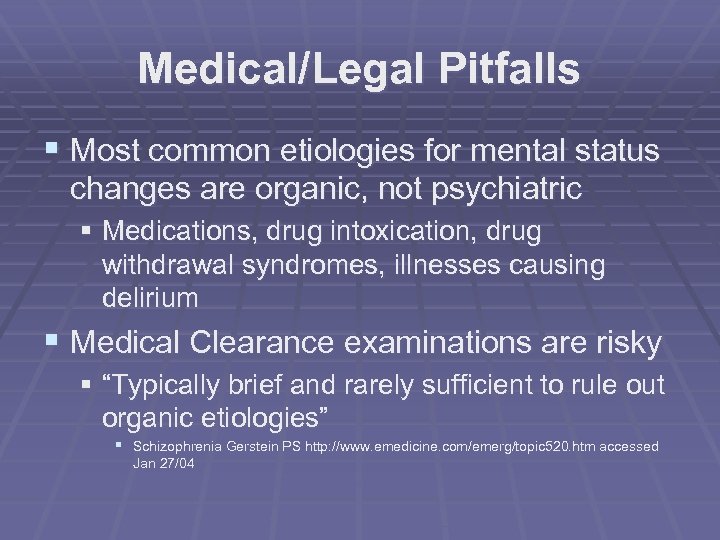
Medical/Legal Pitfalls § Most common etiologies for mental status changes are organic, not psychiatric § Medications, drug intoxication, drug withdrawal syndromes, illnesses causing delirium § Medical Clearance examinations are risky § “Typically brief and rarely sufficient to rule out organic etiologies” § Schizophrenia Gerstein PS http: //www. emedicine. com/emerg/topic 520. htm accessed Jan 27/04

Medical/Legal Pitfalls: Restraints § Document reasons for needing a restraint and involuntary commitment § Mention pt/staff safety and protection § Personally ensure restraints are applied safely, § do not order “restrain prn” § Chemical restraints are preferable to physical when prolonged behavioral control is necessary § Death can result from prolonged struggle against physical restraints
end
References § Stefan Brennan. R IV psychiatry U of A, member Bohemian FC, IRA § Jacobson: Psychiatric Secrets, 2 nd ed. , Copyright © 2001 Hanley and Belfus § Schizophrenia Gerstein PS http: //www. emedicine. com/emerg/topic 520. htm accessed Jan 27/04 § Kaplans and Sadock’s Synopsis of Psychiatry 8 th edition Williams and Wilkins Baltimore § Rosen’s 5 th edition
1934a97cb97e961dd081cc9384b0346f.ppt