862ddcb7c77ef5fe77115592791811a4.ppt
- Количество слайдов: 41
Third Stage Labor Management …. Plus (The Immediate Post-Birth Period) Authors: Marcia Gould Rohlik, MSN, RNC Janet Smith, BSN, RNC Evelyn M Hickson, RN, MSN, CNS
Objectives Discuss the nursing management of the third stage of labor. List potential complications associated with the third stage of labor and nursing management of each complication.
Definitions Third stage of labor Birth Delivery of the placenta Today’s scope – usually also includes the first hour into the 4 th Stage of labor (post partum)
Delivery of Placenta Decreases size of uterine cavity Decreased size reduces implantation site Uterine contractions of perpendicular muscle layers encourage separation Uterus contracts firmly after expulsion
Four Signs of Placental Separation Spherical uterus Uterus rises as placenta enters vagina Increased cord length protruding Gush of blood
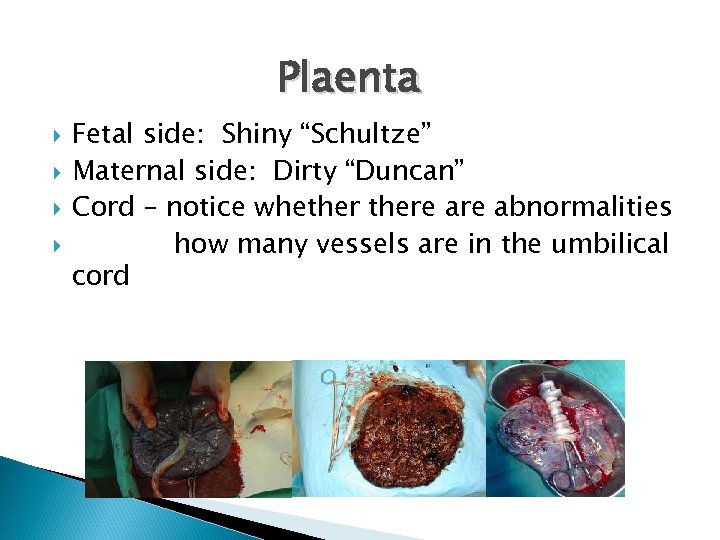
Plaenta Fetal side: Shiny “Schultze” Maternal side: Dirty “Duncan” Cord – notice whethere abnormalities how many vessels are in the umbilical cord

Immediate Post-Placental Delivery Care Fundus/Bleeding ◦ ◦ Palpation Massage Oxytocin-Uterine Tonic Baby to breast Assessment of Injury: ◦ Cervical ◦ Vaginal ◦ Perineum ◦ Labial Perineum ◦ Laceration or episiotomy ◦ Regional – block still functional if pt needs repair ◦ Is “Local” analgesia agent needed to provide comfort ? ◦ Sutures ◦ Packing – radio-opaque and documented
Normal Blood Loss at Delivery Vaginal Delivery ◦ < 500 m. L Cesarean Section ◦ < 1000 m. L
After Delivery of Placenta – Next hour Primary Goals: ü Assessment of Recovery – follow Standards of Care for assessment and documentation ü ü Newest national standards (as of Nov 2012) per Perinatal Guidelines – ACOG and AAP: Q 15 min Vital signs and OB check for 2 hours post delivery Comfort – get them off the wet stuff!! ü Bonding-baby and family ü Teaching – infant security, breast feeding, postpartum routine ü Documentation! ü
Physical Recovery & Comfort Hemostasis ◦ Fundus ◦ Lochia ◦ VS Recovery from epidural (regional) vs local and IV analgesia and anesthesia Ice Intake Sensitivity, modesty, Cultural Competence Topicals Medications for pain Modified Aldrete for analgesia recovery
Assessment Parameters – New This Year! Vaginal delivery Cesarean Section ◦ Maternal vital signs every 15 minutes x 8 (2 hours) ◦ Fundus, uterine tone and lochia every 15 minutes x 8 (2 hours)
Assessment Parameters Infant ◦ Vital signs every 30 minutes x 2 hours, then every 4 hours x 2, then every 8 hours
Pain Assessment Parameters Maternal ◦ Pain assessment every 15 minutes with maternal vital signs and after any intervention for pain management Infant ◦ Pain assessment once during the immediate transition period
Cardiovascular Ø Auto-transfusion of 500 -750 m. L of utero-placental blood flow into the mother’s circulating blood stream after the placenta is delivered Ø Increases patient’s risk for pulmonary edema if patient has: § Cardiac history – valve insufficiency or poor cardiac function § Preeclampsia § Receiving medications – Magnesium Sulfate § Fluid overloaded
Hemodynamic Changes Cardiac Output (the amount of blood a heart pumps out – Stroke Volume X HR) peaks immediately after birth and then slowly declines reaching pre-labor values 1 hour after delivery Labor Cardiac Output = 8 -11 liters/min ØDependent on: üAnalgesia üAmount of blood loss during and after delivery üMode of delivery üMaternal position
Hemodynamic Changes Heart Rate: remains stable or decreases slightly after birth depending on position ØDecrease in heart rate may be associated with rest/sleep or analgesia ØIncrease in heart rate may indicate: üPain üBlood loss üInfection
Hemodynamic Changes Blood Pressure – should remain stable or decrease slightly ◦ Increase in BP may indicate pain or preeclampsia Significant decrease in BP is a late sign of hypovolemia ◦ First sign will be maternal tachycardia Orthostatic hypotension may occur: ◦ Woman sits up from a reclining position ◦ Woman stands up to ambulate ◦ After emptying her bladder (due to a vaso-vagal stimulation)
Respiratory Issues Oxygen saturations should remain at or above 95% Increased respiratory rate may indicate pulmonary edema or pulmonary emboli Monitor and assess breath sounds in patients with risk factors for respiratory compromise or who are symptomatic (asthma, preexisting pneumonia/URI, preeclampsia)
Urine Output – Vaginal Delivery Postpartum patients with analgesia may not feel urge to urinate ◦ Assess bladder for distension ◦ Determine / Identify last void or if catheterization occurred prior to delivery ◦ Have 6 hours to demonstrate that they can spontaneously void after delivery (as long as bladder is not distended and lochia flow has not increased)
Urine Output – C-section Usually have indwelling catheter for up to 12 hours or until able to get up to void Urine Output is monitored during and after surgery Ensure that catheter is secured for patient comfort and integrity Catheter /perineum care Assess: Ø Patency of catheter Ø Volume (must be > 30 m. L / hr) Ø Color Ø Presence or absence of blood clots Ø Presence of bladder spasms / patient discomfort
Potential Complications
Third Stage Complications (Will be discussed in OB Emergencies) Postpartum hemorrhage Lacerations Hematomas Amniotic fluid emboli Other emboli – pulmonary, cerebral/stroke MI
Other Issues: Psycho-social issues ◦ ◦ ◦ Family Psychiatric CPS Family members Who is the baby daddy? ? ? Impact of other medical problems ◦ ◦ ◦ Diabetes Hypertension Cardiac Respiratory Auto-immune
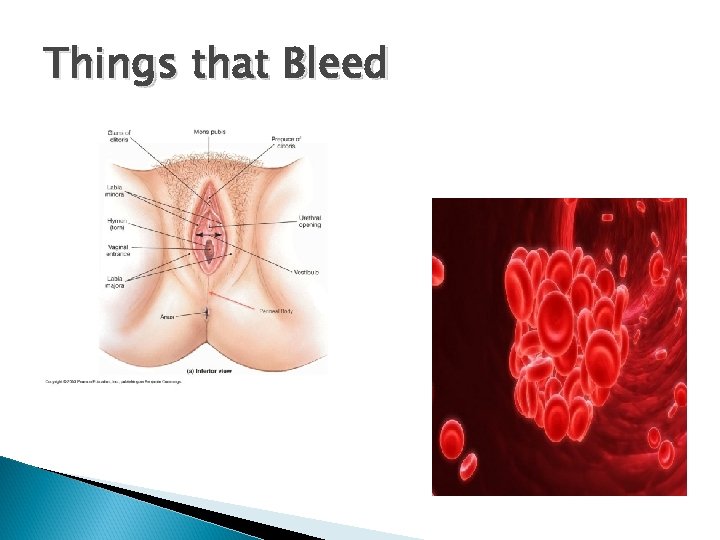
Things that Bleed
Laceration of cervix or vaginal wall ◦ ◦ Active bright red bleeding Steady stream or trickle of unclotted blood Firm uterus Call provider ◦ **Remember – a patient can bleed enough to become hypovolemic
Hematomas Vaginal Vulval Retroperitoneal
Pelvic Hematomas Definition: collection of blood in the subcutaneous layer of the pelvic tissue secondary to damage to a vessel wall without laceration of the tissue Three types: vagina, vulva, or sub-peritoneal areas
Vaginal Hematomas Results from trauma to the maternal soft tissues during delivery Frequently associated with Instrument (operative) forceps or vacuum delivery but many occur spontaneously Less common than vulvar hematomas Blood accumulates – in the perineum, vaginal walls, inguinal area
Vaginal Hematomas Symptoms: Severe rectal pressure Exam reveals a large mass protruding into the vagina Scant or no vaginal lochia As with vulvar hematomas, it is uncommon to find a single bleeding vessel as the source of bleeding
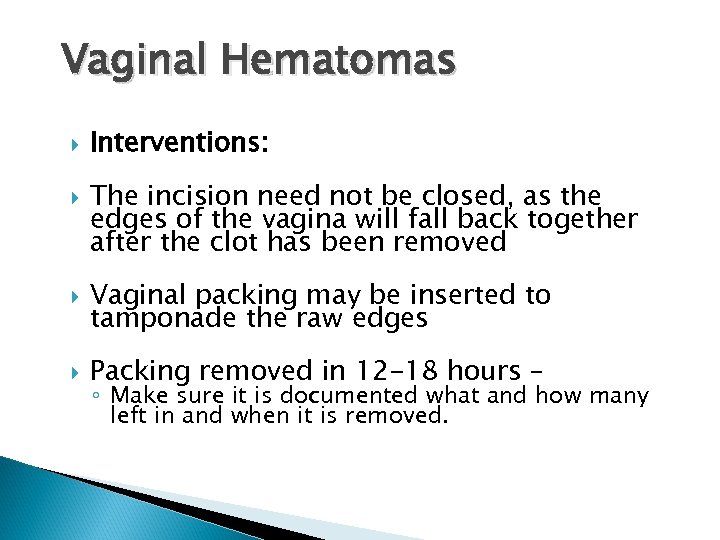
Vaginal Hematomas Interventions: The incision need not be closed, as the edges of the vagina will fall back together after the clot has been removed Vaginal packing may be inserted to tamponade the raw edges Packing removed in 12 -18 hours – ◦ Make sure it is documented what and how many left in and when it is removed.
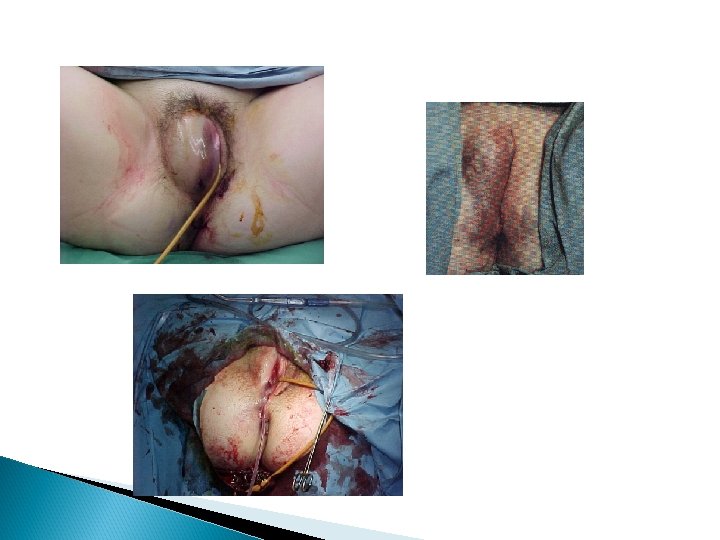
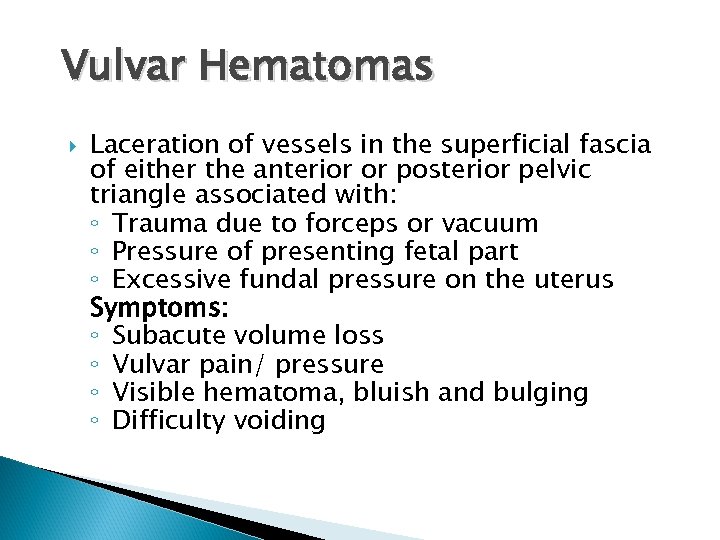
Vulvar Hematomas Laceration of vessels in the superficial fascia of either the anterior or posterior pelvic triangle associated with: ◦ Trauma due to forceps or vacuum ◦ Pressure of presenting fetal part ◦ Excessive fundal pressure on the uterus Symptoms: ◦ Subacute volume loss ◦ Vulvar pain/ pressure ◦ Visible hematoma, bluish and bulging ◦ Difficulty voiding
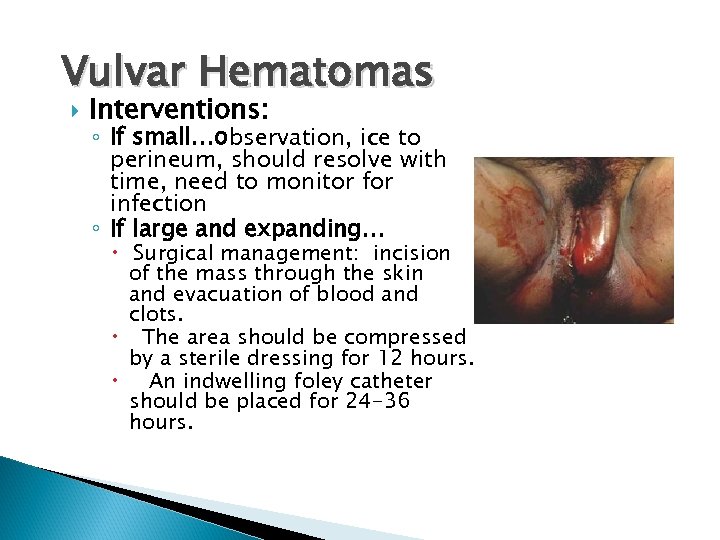
Vulvar Hematomas Interventions: ◦ If small…observation, ice to perineum, should resolve with time, need to monitor for infection ◦ If large and expanding… Surgical management: incision of the mass through the skin and evacuation of blood and clots. The area should be compressed by a sterile dressing for 12 hours. An indwelling foley catheter should be placed for 24 -36 hours.
Retroperitoneal Hematomas Least common of the pelvic hematomas Most dangerous - Life-threatening Symptoms: ◦ May not be impressive until mother becomes tachycardia followed by sudden onset of hypotension or shock Can result after C/S delivery with laceration of one of the vessels originating from the hypogastric artery or after rupture of a low transverse C/S delivery scar during VBAC. Intervention: Surgical exploration and ligation of the hypogastric vessels
Other areas of focus Psycho-Social Issues Pre-existing Medical Problems Bonding Teaching
Psycho-Social Issues Support Family dynamics Adoptions CPS alerts Substance abuse Depression/bipolar history Psychotic illness
Impact Other Medical Problems Cardiac disease Kidney disease Trauma Paralytic disorders Contagious illness
Bonding Physical contact and viewing Assessing quality of bonding and support First feedings Cultural awareness Reassurance, information Time pressures
Teaching Self care Baby care and feeding Newborn characteristics Physical expectations next few days Emotional expectations next few days Keep info short, targeted
Summary Time of dramatic changes Most physical care in background Need for supportive, compassionate, family -centered care

References Gorrie, T. , Mc. Kinney, E. , Murray, S. (1999). Foundations of maternal newborn nursing (2 nd ed. ). Philadelphia, PA: Saunders Davies, S. , (2001). Amniotic fluid embolus: a review of the literature. Canadian Journal of Anesthesiology 48(1), 88 -98. AWHONN’s Compendium of Postpartum Care. Johnson and Johnson Inc. ; 2006. Chin, MD, FACOG. On Call Obstetrics and gynecology. W. B. Saunders Co. Philadelphia; 1997. Jones, RNC, MSN, Marion W. Postpartum Complications. Health Education Innovations, Inc. ; 1996. Mattson, Ph. D, RNC, CTN, Susan and Smith, Ph. D, RNC, Judy E. Core Curriculum for Maternal-Newborn Nursing, AWHONN, 2 nd Ed. ; W. B. Saunders Co. Philadelphia; 2000. Rice-Simpson, RNC, MSN and Creehan, RNC, MS, MA, ACCE, Patricia A. Perinatal Nursing. AWHONN; Lippencott, Philadelphia; 2003.
862ddcb7c77ef5fe77115592791811a4.ppt