e30dd7a4ff0d4f4b404a5d274d6cbb96.ppt
- Количество слайдов: 38
Third Party Liability Presented by EDS Provider Field Consultants October 2009
Agenda • Session Objectives • TPL Responsibilities • Identifying TPL Resources • Health Management Systems • Cost Avoidance and TPL Resource Information • Updating TPL Information • Disallowance Project • TPL Policies • Medicare Buy-In • Casualty Cases • Common Denials • Submitting TPL Claims and • Helpful Tools Attachments • Managed Care and TPL • Questions • TPL Payments After IHCP Payments Third Party Liability 2 / October 2009
Session Objectives Following this session, providers will better understand the following: • IHCP is the payer of last resort • Coordination of benefits with other payors • Recovery of funds due the IHCP • The role of HMS Third Party Liability 3 / October 2009
Identifying TPL Resources What is TPL? • TPL stands for third-party liability. It is a term used to refer to insurance other than the IHCP, including: – A commercial group health or medical plan – An individually purchased health or medical plan – Casualty insurance, such as a homeowners or automobile liability policy, or compensation resulting from an accident or injury • This type of insurance is used only for casualty recovery, not cost avoidance Third Party Liability 4 / October 2009
TPL Responsibilities • Identify Medicaid member third-party insurance coverage; verify and update insurance information • Maintain TPL insurance information by accepting adds, updates, or deletes from various external entities • Maintain Medicare and other TPL insurance information by accepting adds, updates, or deletes from various external entities • File and pursue Medicaid liens in casualty cases • Provide Medicaid member birth expenditure information to county prosecutor’s office • Pay private health insurance premiums for Medicaid members when it is deemed cost-effective to do so • Meet federal and State TPL reporting requirements Third Party Liability 5 / October 2009
Identifying TPL Resources • Verify TPL member eligibility using one of the following verification options: – Automated Voice Response – Omni swipe card • BT 200711 includes download instructions for the Omni machine for expanded NPI information – Web inter. Change • What is the best option for TPL information? – Web inter. Change offers expanded TPL detail including: • Primary insurance name, address, and telephone number • Policy holder information Third Party Liability 6 / October 2009
Identifying TPL Resources Impact of QMB-Only Members • QMB (Qualified Medicare Beneficiary) – Medicare Premiums are paid by the state. This is referred to as Buy-in coverage. Discussed later in the presentation • If member eligibility reads QMB-Only, Medicaid is only liable for the Medicare coinsurance and deductible only • There is no Medicaid reimbursement when Medicare does not allow a service – Dental – Hearing Aids – Vision Refraction • Verify eligibility for Medicare at the following numbers: – Part A – 1 -866 -580 -5987 – Part B – 1 -866 -250 -5665 Third Party Liability 7 / October 2009
Updating TPL Information – Via Paper What is needed to update the member’s insurance information? • A copy of the member’s medical insurance card • A copy of the explanation of benefits (EOB) stating coverage is terminated • A letter on company letterhead from the insurance carrier or the employer stating what date the member’s coverage terminated • A copy of the Medicaid Third Party Liability Questionnaire form – Download this form from the Forms link at www. indianamedicaid. com Third Party Liability 8 / October 2009
Updating TPL Information – Electronically • Submit an electronic request to the EDS TPL Unit to update a member’s insurance information • The TPL Unit receives the request, researches, confirms the information, and updates the eligibility screen with corrected information – Updates are usually made within 20 days • Confirm that eligibility has been updated by reviewing the Eligibility Inquiry feature Third Party Liability 9 / October 2009
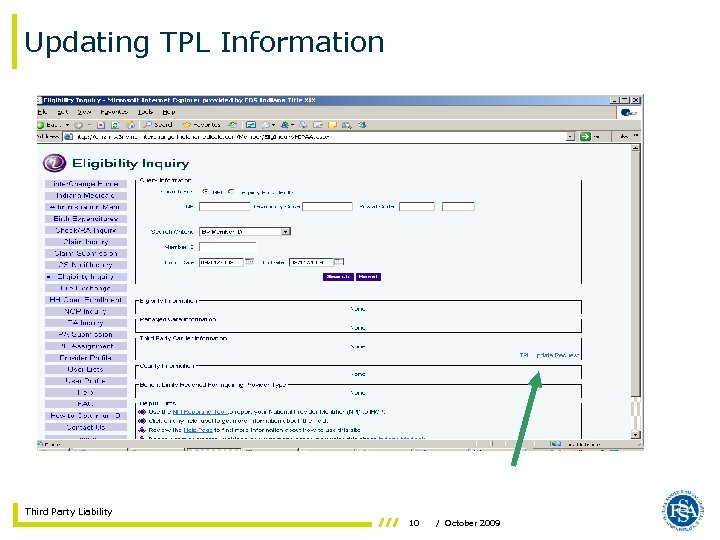
Updating TPL Information Third Party Liability 10 / October 2009
TPL Policies that Pay the Member What if a member has a health insurance policy that pays the member only? • Attempt to retrieve the funds from the payor via an assignment of benefits form – Providers should always ask members to sign an assignment of benefits form to submit to the other insurance with the claim – Providers create their own assignment forms • If carrier refuses to honor the assignment of benefits form, request that member forward TPL payment to the provider – If the member refuses to forward the TPL payment to the provider, submit the claim to EDS following the 90 -Day Provision procedure (discussed later in this presentation) • Indemnity policies are not loaded as a TPL resource. When providers or others notify EDS, the TPL unit will terminate the indemnity policy in Indiana. AIM Note: Reference Chapter 5, Section 3 of the IHCP Provider Manual for more information Third Party Liability 11 / October 2009
Reporting Casualty Cases to TPL • Providers should notify the Casualty Unit within the TPL Unit if they receive a request for a member’s medical records due to an accident or illness resulting from the negligent act of another person • Contact the Casualty Unit – By e-mail at INXIXTPLCasualty@eds. com – By telephone local (317) 488 -5046 or toll -free at 1 -800 -457 -4510 – By U. S. mail at: EDS TPL Casualty Unit P. O. Box 7262 Indianapolis, IN 46207 -7262 Third Party Liability 12 / October 2009
Submitting Claims with TPL Billing the IHCP for Insurer Copayments • Providers may not collect insurer copayments from the member • Providers must bill Medicaid for the usual and customary charges and report the TPL payment – The usual and customary charge includes the copay amount – Do not include write-off amounts on the claim Note: State-mandated copayments are not the same as TPL copayments, and may be collected from the member Third Party Liability 13 / October 2009
Submitting Claims with TPL Blanket Denial What is a blanket denial? • When a healthcare service is not a covered benefit for the insured, the IHCP accepts an EOB from the other insurer showing that the service is not covered What must the blanket denial EOB include? • Name of primary insurance carrier • Information sufficient to identify the member • Description of healthcare service • Statement of noncoverage of the service When does a blanket denial expire? • Blanket denial EOBs are valid until the end of the calendar year Third Party Liability 14 / October 2009
Submitting Claims with TPL 90 -Day Provision What if the third-party insurance does not respond? • When a third-party payer fails to respond within 90 days of the provider’s billing date, the claim may be submitted to the IHCP for payment consideration How to submit claims under the 90 -Day Provision: • Indicate 90 -Day Provision • Include attachments to support previous attempts to file with the primary carrier – Web inter. Change users may insert a claim note to invoke the 90 -Day Provision. Provider should write 90 -day rule no response, insurance carrier, and dates sent to carrier IHCP Provider Manual, Chapter 5, contains billing instructions Third Party Liability 15 / October 2009
Submitting Claims with TPL Helpful Hints When submitting TPL claims: • Include member identification (name and RID number) on the claim attachment • Clearly state the reason for noncoverage on the TPL attachment • Ensure that the primary insurance company name on the attachment matches the information in the member’s file • Hand write “Medicare Replacement Policy” on the claim form and EOB for Medicare HMO claims • Hand write the procedure code(s) on the EOB if not already indicated • Submit TPL claims to the appropriate claim P. O. Box – P. O. Box 7269 for CMS-1500 claims – P. O. Box 7271 for UB-04 claims Note: No attachments are required when TPL has made a payment Third Party Liability 16 / October 2009
Submitting Claims with TPL Member Receives Services outside the Commercial Network Did the member receive service outside a commercial network? • The member must follow the rules of his or her commercial plan first • If a provider is not in a member’s primary plan network, the provider should check with the primary plan before rendering service • The IHCP does not reimburse for services rendered out-of- network of another plan unless the policy reimburses for out-of-network services – If the plan makes payment, it is business as usual Third Party Liability 17 / October 2009
Submitting Claims without TPL Edits • If the IHCP has a TPL resource for a member on file and a claim is submitted for payment with zero dollars in the TPL field and no EOB is sent, the claim will deny for TPL • The TPL edits are: – 2500 – Recipient covered by Medicare A – no attachment – 2501 – Recipient covered by Medicare A – with attachment – 2502 – Recipient covered by Medicare B – no attachment – 2503 – Recipient covered by Medicare B – with attachment – 2504 – Recipient covered by Private insurance – no attachment – 2505 – Recipient covered by Private Insurance – with attachment – 2510 – Recipient covered by Medicare D Third Party Liability 18 / October 2009
Submitting Claims without TPL Edits Claims that bypass TPL edits: • Claims from a state psychiatric hospital • Claims with principal diagnosis code of: – Prenatal care – Pregnancy – Preventive pediatric – Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) • Services for dually eligible Medicare and Medicaid members, when the service is always noncovered by Medicare (program excluded) – Services sometimes covered by Medicare will not bypass TPL Third Party Liability 19 / October 2009
Submitting Claims without TPL Bypass Tables • Updating the TPL bypass tables: – EDS reviews the Medicare bypass tables annually – EDS uses the Medicare Covered and Non-Covered Manual to be sure the Medicare bypass tables are up-to-date with codes that are never covered by Medicare – EDS updates the commercial bypass tables based on information received from outside sources such as other carriers and providers Third Party Liability 20 / October 2009
Managed Care and TPL • Insurance questions concerning members who are enrolled in the risk-based managed care (RBMC) delivery system should be directed to the appropriate managed care organization (MCO) Third Party Liability 21 / October 2009
TPL Payments After IHCP Payments • What if a third party or the member makes payment after IHCP has paid the claim? – The provider should submit a replacement claim via Web inter. Change, or use the paper adjustment form or – The provider can use the credit balance reporting process administered by Health Management Systems (HMS) • Additional information was published in IHCP provider newsletter NL 200604 • For additional questions, call 1 -877 -2644854 Third Party Liability 22 / October 2009
Health Management Systems • HMS is contracted by EDS to perform retro-recovery (or “pay and chase”) of Medicaid claims from commercial insurance carriers and bills the carriers monthly • HMS performs data matches with commercial carriers to determine member TPL eligibility and provides Indiana. AIM with this insurance resource information • Beginning in May 2009, EDS and HMS have increased the frequency of TPL updates to the Indiana. AIM system from bimonthly to biweekly updates, in an effort to provide the most up to date TPL information Third Party Liability 23 / October 2009
Health Management Systems • HMS conducts disallowance projects where it looks for claims that should have been paid by Medicare or the Federal Employee Program (FEP) and notifies the provider to submit the claim to Medicare or FEP – Once the claim is paid by Medicare or FEP, the Medicaid claim is adjusted to show this payment and the funds recouped by Medicaid • HMS conducts provider self-audits for providers to report credit balances • Beginning in 2008, HMS conducts commercial insurance disallowance projects focused on hospital providers where it looks for claims covered by commercial carriers and notifies the provider to bill the carrier Third Party Liability 24 / October 2009
Cost Avoidance and TPL Resource Information Updates • When a member’s TPL insurance information is listed in Indiana. AIM, the member’s claim will be cost avoided (or denied) unless it was first submitted to the TPL carrier • EDS receives insurance information updates from the Indiana Client Eligibility System (ICES), HMS, claims data, members, providers, insurance carriers, and caseworkers • EDS verifies third-party insurance information and adds updates to Indiana. AIM within 20 business days of receipt • Update requirements are as follows: – Copy of the member’s medical insurance card – Copy of the EOB stating coverage is terminated – Letter on company letterhead from the insurance carrier or the employer stating what date the member’s coverage terminated – Copy of the Medicaid Third Party Liability Questionnaire form • This form can be downloaded from the IHCP Web site Third Party Liability 25 / October 2009
TPL: Disallowance Project Medicare • Effective May 23, 2007, Medicare carriers can only be billed by the provider of services – Because Medicaid can no longer bill TPL claims directly to Medicare carriers, the billing of TPL claims through the provider of service is the only viable method of recovery – Consequently, in addition to the Medicare Part A and FEP disallowance projects, HMS will also conduct a Medicare Part B disallowance project on a quarterly basis • How the disallowance projects work: – HMS identifies Medicaid paid claims that should have been billed to Medicare/FEP as primary – HMS will send listings of paid Medicaid claims to providers with instructions asking them to bill Medicare/FEP for the claims paid by Medicaid and respond within 60 days – Providers are to report back to HMS within 60 days by submitting a Credit Balance Worksheet and notify Medicaid as to which claims have been paid by Medicare/FEP and which have been denied Third Party Liability 26 / October 2009
TPL: Disallowance Project Commercial Insurance • How the Commercial Insurance disallowance projects work: – Focused on hospital providers – HMS identifies Medicaid paid claims that should have been billed to commercial carriers – HMS will send listings of paid Medicaid claims to providers with instructions asking them to bill the commercial carriers for the claims paid by Medicaid and respond within 60 days – Providers are to report back to HMS within 60 days and notify Medicaid as to which claims have been paid by the commercial carrier and which have been denied Third Party Liability 27 / October 2009
TPL: Disallowance Project Credit Balance Corrections • Credit Balance Worksheet – EDS will process adjustments to the claims – Instructions can be located at www. indianamedicaid. com Web site under Forms, TPL • Direct Refunds – Mail refunds to HMS at: Fifth Third Bank Indiana Medicaid/EDS P. O. Box 2303 Dept. 132 D Indianapolis, IN 46206 -2303 Third Party Liability 28 / October 2009
Medicare Buy-In Overview • Allows states to pay Part B Medicare premiums for dually eligible members (members eligible for both Medicaid and Medicare) • Automated data exchanges between EDS and the Centers for Medicare & Medicaid Services (CMS) are conducted monthly to identify, update, resolve differences, and monitor new and ongoing Medicare buy-in cases • The state is responsible for initiating Medicare buy-in for eligible members and EDS coordinates Medicare buy-in resolution with CMS • Medicare is generally the primary payer – Payment of Medicare premiums, coinsurance, and deductibles cost less than Medicaid benefits – States receive Federal Financial Participation (FFP) for premiums paid for members eligible as: • Qualified Medicare beneficiaries (QMB) • Qualified disabled working individual (QDWI) • Specified low-income Medicare beneficiaries (SLMB) • Money grant members Social Security Income (SSI) • Qualified individual (QI-1) Third Party Liability 29 / October 2009
Top Denials Third Party Liability 30 / October 2009
Edit 0558 Coinsurance and Deductible Amount Missing • Cause – Coinsurance and deductible amount is missing on the claim showing payment from Medicare • Resolution – Bill Medicare First for payment – CMS-1500 • Field 22 Left = The sum of Medicare Coinsurance, Deductible, and Psych Reduction Right – Medicare paid amount - UB-04 • • • Field 39 a-41 d Value code A 1 – Medicare Value code A 2 – Medicare Value code 06 – Medicare Field 54 A – Medicare paid deductible amount coinsurance amount blood deductible amount Third Party Liability 31 / October 2009
Edit 0593 Medicare Denied Detail • Cause – Occurs when Medicare denies a detail line and are included with the paid detail lines • Resolution – Refile new claim with Medicare Remittance Notice (MRN) electronically – Do not include paid detail lines on the new claim – These claims are processed as TPL claims Third Party Liability 32 / October 2009
Edit 2007 QMB-Recipient – Bill Medicare First • Cause – Claim was billed to Medicare Replacement or HMO policy but was never indicated on claim as a replacement or HMO policy • Resolution – Bill To Medicare Replacement or HMO Plan as primary – If payment was made from other plan, indicate payment on claim and write “Medicare Replacement” or “Medicare HMO” – If no payment from other plan write “Medicare Replacement” or “Medicare HMO” on claim and submit EOB from other plan with claim to noncrossover address Third Party Liability 33 / October 2009
Edit 2502 Recipient Covered by Medicare Part B (No Attachment) • Cause – If a physician or outpatient claim is submitted for a Medicare Part B covered service and recipient is covered by Medicare Part B – The claim will deny if no attachment indicating Part B has been billed • Resolution – Bill Medicare Part B first – Bill Medicaid with claim with Medicare Remittance Notice (MRN) or electronically using the attachment (ACN) process Third Party Liability 34 / October 2009
Edit 2505 Recipient Covered by Private Insurance • Cause – This member has private insurance, which must be billed prior to Medicaid • Resolution – Add the other insurance payment to the claim electronically – CMS-1500 • Add other insurance excluding Medicare payments to field 29 – UB-04 • Add other insurance excluding Medicare payments in field 54 B Third Party Liability 35 / October 2009
Helpful Tools Avenues of Resolution • IHCP Web site at www. indianamedicaid. com • IHCP Provider Manual (Web, CD-ROM, or paper) • HCBS Waiver Provider Manual (Web) • Customer Assistance – 1 -800 -577 -1278, or – (317) 655 -3240 in the Indianapolis local area • Written Correspondence – P. O. Box 7263 Indianapolis, IN 46207 -7263 • Provider Relations field consultant Third Party Liability 36 / October 2009
Questions Third Party Liability 37 / October 2009
Office of Medicaid Policy and Planning (OMPP) 402 W. Washington St, Room W 374 Indianapolis, IN 46204 EDS, an HP Company 950 N. Meridian St. , Suite 1150 Indianapolis, IN 46204 EDS and the EDS logo are registered trademarks of Hewlett-Packard Development Company, LP. HP is an equal opportunity employer and values the diversity of its people. © 2009 Hewlett-Packard Development Company, LP. October 2009
e30dd7a4ff0d4f4b404a5d274d6cbb96.ppt