Asthma.ppt
- Количество слайдов: 67
Theme: Bronchial asthma. Chronic obstructive diseases of lungs. Syndrome of lungs overfilling with air. Pulmonary emphysema
n n Aim: To learn the diagnostic, memorize the etiology, pathogenesis, clinical findings, differential diagnostic, complications, treatment, and prognosis of bronchial asthma. Professional motivation: Bronchial asthma is a chronic upper airway disease, very spread in a whole world. And the patients with asthma have a risk of heavy diseases as complications of it, such illness adjust well to the necessity for continued medical treatment throughout life. So necessary to know the clinical symptoms, laboratory investigation, xrays findings and treatment of this pathology. And that is why therapeutist must know this diseases to diagnose it in time and choose the right way of treatment.
Special attention should be paid to the following 1. Essentials of diagnosis. 2. General considerations. 3. Etiopathogenesis, clinical and laboratories findings of atopic asthma. 4. Etiology and pathogenesis of the infectiousallergic asthma. 5. The main symptoms of the infectious-allergic asthma. 6. Clinical and laboratories findings of the infectiousallergic asthma. 7. X-Rays findings. 8. Status asthmatics. 9. Immediately treatment of status asthmatics. 10 The treatment of the different forms of bronchial asthma. 11. Complications. 12. Prognosis for short and long term.

Key words and phrases: bronchial asthma; status asthmaticus; atopic or infeictious-allergic form; immediately treatment; Acute obstruction, bronchial hypersensitivity, wheezing, dyspnea associated with a stridorous cough, tenacious mucoid sputum, plugs and spirals, eosinophilia, acute bronchospasm, arterial hypoxemia, Epinephrine.

BRONCHIAL ASTHMA Essentials of Diagnosis: • Recurrent acute attacks of dyspnea, cough, and mucoid sputum, usually accompanied by wheezing. • Prolonged expiration with generalized wheezing and musical rales. • Bronchial obstruction reversible by drugs


General Considerations: Asthma is a bronchial hypersensitivity disorder characterized by reversible airway obstruction, produced by a combination of mucosal edema, constriction of the bronchial musculature, and excessivesecretion of viscid mucus, causing mucous plugs.

Atopic, or "extrinsic, " asthma has been thought to result from sensitization of the bronchial mucosa by tissue-specific antibodies. The antibodies produced are specific immunoglobulins of the Ig. E (type I) class, and the total serum Ig. E concentration is usually elevated. Exposure to the appropriate allergens by inhala-tion results in an antigen-antibody reaction, that releases vasoactive bronchoconstrictive chemical mediators, causing the characteristic tissue changes. More recent work suggests that immunoglobulin G (Ig. G) may play a role similar to that of Ig. E in some cases.








Approximately 50% of asthmatics are of the nonatopic ("intrinsic") type in which the bronchial reaction occurs in response to nonimmunologic stimuli such as infection, irritating inhalants, cold air, exercise, and emotional upset. These patients do not demonstrate elevated Ig. E antibodies in their serum, and the history does not suggest hypersensitivity to specific allergens, although there may be other immunologic mechanisms that have not yet been demon strated. Agrowing list of agents encountered in the work place have been shown to cause asthma. Some organic materials such as wood dust act through an immunologic mechanism, whereas certain chemicals and metal dusts apparently cause direct irritation or protein denaturation in low concentrations
Susceptible individuals may be affected by concentrations well below those allowed by US government standards. Occupational asthma should be suspected when symptoms occur repeatedly at work or within several hours there after and improve away from work. Improvement may require several days Beta-adrenergic blocking agents such as propranolol cause intense bronchial constriction in patients with asthma, apparently due to parasympathetic nerve stimulation. Aspirin and nonsteroidal antiinflammatory agents may cause severe asthma in some patients.
Clinical Findings Symptoms and Signs: Asthma is characterized by recurrent attacks of dyspnea, cough, and expectoration of tenacious mucoid sputum, and usually wheezing. Symptoms may be mild and may occur only in association with respiratory infection, or they may occur in various degrees of severity to the point of being life-threatening. Classic allergic (atopic) asthma usually begins in childhood and becomes progressively more severe throughout life, although spontaneous remissions may occur in adulthood. Hay fever often accompanies atopic asthma.






n n The acute attack is characterized by dyspnea usually associated with expiratory wheezing that may be heard without a stethoscope. Cough may be present but is usually not the predominant symptom. There is a small group of patients with asthma in whom paroxysmal cough may be the predominant symptom. When asthtna becomes prolonged, with severe intractable wheezing, it is known as status asthmaticus.


B. Laboratory Findings: The sputum is characteristically tenacious and mucoid, containing "plugs" and "spirals. " Eosinophils are seen microscopically. The differential blood count may show eosinophilia. In severe, acute bronchospasm, arterial hypoxemia may be present as a result of disturbed perfusion /ventilation relationships, alveolar hypoventilation, or functional right-to -left shunts.
Дослідження харкотиння
спірограма


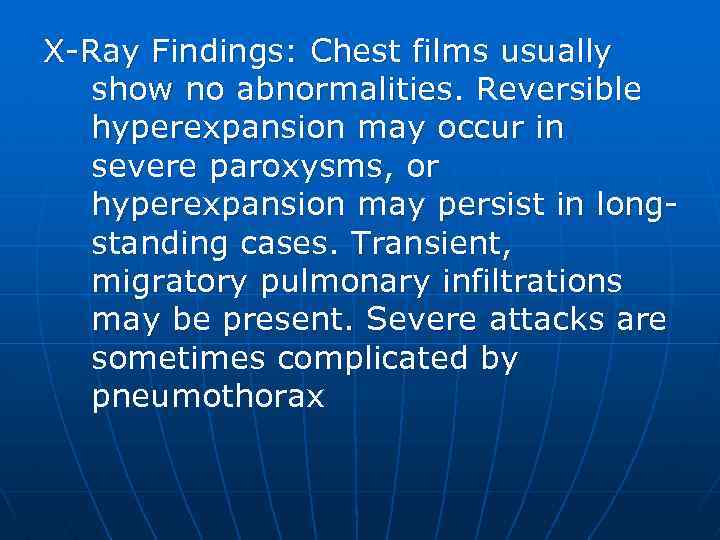
X-Ray Findings: Chest films usually show no abnormalities. Reversible hyperexpansion may occur in severe paroxysms, or hyperexpansion may persist in longstanding cases. Transient, migratory pulmonary infiltrations may be present. Severe attacks are sometimes complicated by pneumothorax
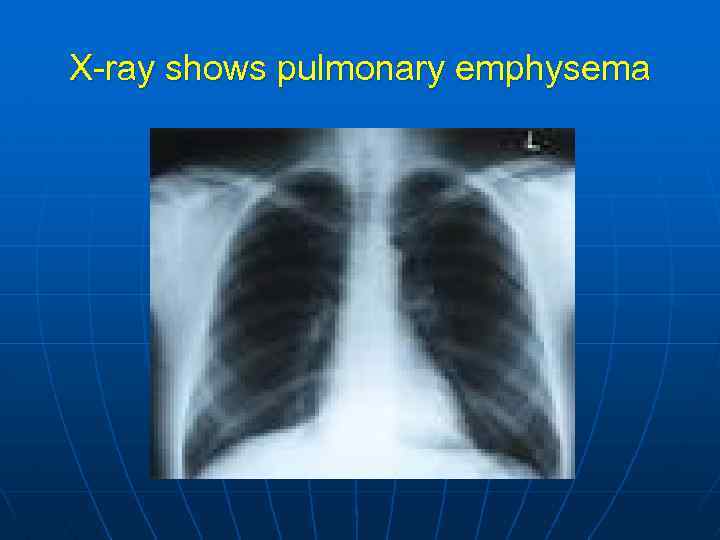
X-ray shows pulmonary emphysema

Endoscopic findings: hyperemia, edema of bronchial mucosa, hypersecretion

Allergic tests allow to determine allergens

Positive reaction

Differential Diagnosis Distinguish wheezing from that due to other disorders such as bronchitis, obstructive emphysema, and congestive heart failure.

Treatment The treatment may be divided into 2 phases: treatment of the acute attack and interim therapy, which is aimed at preventing further attacks. Epinephrine and intravenous aminophylline are the drugs of choice for the emergency management of acute asthma. However, for status asthmaticus or for acute attacks in epinephrine-resistant patients, the adrenal corticosteroids are usually necessary. Intravenous hydrocortisone and methylprednisolone are the preparations of choice. Note: Epinephrine should not be used in patients with hypertension or angina or in elderly patients.
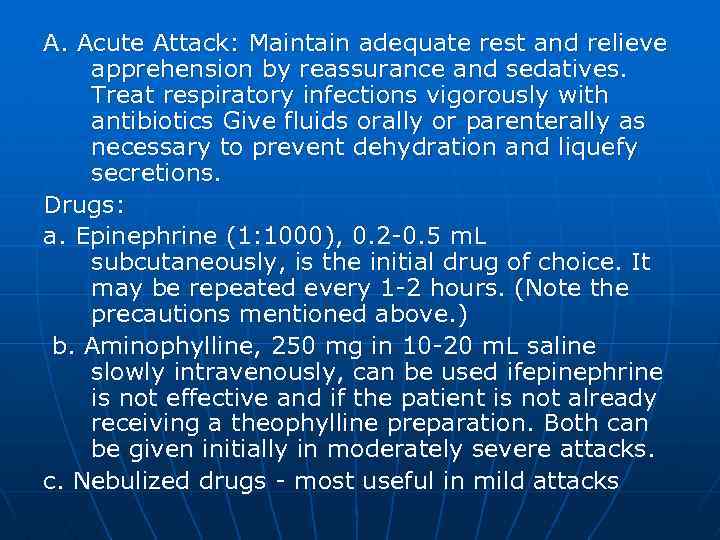
A. Acute Attack: Maintain adequate rest and relieve apprehension by reassurance and sedatives. Treat respiratory infections vigorously with antibiotics Give fluids orally or parenterally as necessary to prevent dehydration and liquefy secretions. Drugs: a. Epinephrine (1: 1000), 0. 2 -0. 5 m. L subcutaneously, is the initial drug of choice. It may be repeated every 1 -2 hours. (Note the precautions mentioned above. ) b. Aminophylline, 250 mg in 10 -20 m. L saline slowly intravenously, can be used ifepinephrine is not effective and if the patient is not already receiving a theophylline preparation. Both can be given initially in moderately severe attacks. c. Nebulized drugs - most useful in mild attacks

Usage of inhaler

Solotvino (salt caves)

Solotvino (salt caves)
Solotvino (salt caves)


Physiotherapy


Climatotherapy

Elimination of risk-factors

Bronchoscopy is used if it is necessary
(1) Isoproterenol, 1: 200, 1 -2 inhalations from a hand nebulizer every 30 -60 minutes, or 0. 5 m. L in 2. 5 -3 m. L saline by compressed air nebulizer or inter- mittent positive pressure breathing every 4 hours. (2) Isoetharine with phenylephrine (Bronkosol) may be used in the same dose as isoproterenol, 1: 200. (3) Epinephrine (1: 100) (for inhalation only), 1 -2 inhalations from hand nebulizer. Do not use for prolonged nebulization. d. Corticosteroid drugs : Most effective in severe attacks that do not respond satisfactorily to the above bronchodilators Give prednisone, 40— 60 mg/d orally in divided doses, and gradually reduce to nil over 7 -10 days. In moderate to severe attacks, hydrocortisone sodium succinate (Solu-Cortef), 100 -250 mg intravenously, may be given simultaneously with the first dose of oral corticosteroid.
e. Other drugs(1) The various bronchodilator agents given orally are of limited value in stopping an acute attack (see below). (2) Sedation should be avoided in severe asthma. In mild to moderate symptoms, hydroxyzine, 25 mg, or diazepam, 5 mg 3 -4 times daily, may be helpful in counteracting the central nervous system stimulant effects of sympathomimetic bronchodilator drugs f. Fluids-Patients with persistent symptoms who require hospitalization generally need supplement intravenous fluids to help liquefy secretions. g. Oxygen by nasal prongs or mask is indicated in the presence of moderate to severe symptoms.
Status asthmaticus. When severe wheezing persists after use of the measures listed above, hospitalization is required for hospitalization. The principal drugs for the treatment of the hospitalized patient are the following: a. Aminophylline 6 mg/kg intravenously in 100 m. L 5% dextrose in water over 20 minutes. Reduce or eliminate the loading dose (see below) for patients who have been taking theophylline preparations. (In overweight patients, calculation of the dose should be based on ideal rather than actual body weight, because theophylline does not penetrate into fatty tissue. )
The intravenous infusion should be continued according to the dosage schedule recommended by the PDA, which is lower than previously recommended by various authors: children and young adult smokers, 1 mg/kg/h for 12 hours, then reduce to 0. 8 mg/kg/h; healthy nonsmoking adults, 0 7 mg/kg/h, reduced to 0. 5 mg/kg/h after 12 hours; older patients and those with cor pulmonale, 0. 6 mg/kg/h, reduced to 0. 3 mg/kg/h after 12 hours, patients with congestive heart failure and liver failure, 0 5 mg/kg/h, reduced to 0. 1 - 0. 2 mg/kg/h after 12 hours. The subsequent dosage schedule should be determined by the serum concentration; 10 -20 Ju. g/ml is the recognized therapeutic range
For patients who have been taking theophylline drugs, determine (if possible) the amount and time of the last medication (1. 2 mg aminophylline is equivalent to 1 mg theophylline) and reduce the loading dose accordingly. When this information is not available, give a reduced loading dose of aminophylline of 2. 9 mg/kg, then continue with the maintenance schedule outlined above

b. Corticosteroids: The drugs of choice are either hydrocortisone sodium succinate (Solu. Cortef), 4 mg/kg, or methylprednisolone sodium succinate (Solu-Medrol), 2 mg/kg given intravenously every 4 hours until improvement is established In patients who have not had steroids, there is no evidence that more than 300 mg of Solu. Cortef per day is beneficial. Prednisone, 20 mg, or methylprednisolone (Medrol), 16 mg orally 4 times daily, can be started at the same time and continued in decreasing doses after the intravenous steroids are no longer needed.
B. Other Measures: Oxygen by nasal prongs or mask should be given in sufficient concentration to relieve hypoxemia. Dehydration is frequently present and must be corrected by intravenous replacement. Use up to 4 liters of 5% dextrose in water in 24 hours for an average-sized adult. Electrolytes should be monitored during continued intravenous replacement.

Nebulized isoproterenol or isoetharine with phenylephrine (Bronkosol), 0. 5 ml in 3 ml of 0. 5 N saline, may be added every 3 -4 hours. The use of intermittent positive pressure breathing has no clear advantage over a simple nebulizer driven by compressed air or oxygen. The addition of chest percussion and postural drainage every 2 -4 hours will usually aid in clearing tenacious secretions Arterial blood gases should be monitored every 30 -60 minutes initially. Unrelieved hypoxemia or a rising Pacoz blood gas measurements are not available, clinical deterioration of the patient is an indication for intubation and assisted or controlled respiration. After intubation, sedation with small doses of diazepam or morphine intravenously may be necessary to permit ventilatory control by the respirator. When control of wheezing or removal of secretions cannot be accomplished with the above measures, general anesthesia with halothane (Fluothane) together with bronchoscopy for aspiration and saline lavage of secretions may be lifesaving.

Interim Therapy: Attempt to identify the of fending allergens and protect the patient from further contact. Desensitization may be indicated occasionally. Emotional disturbances should be eliminated if possible. Patients with "intrinsic" asthma (usually associated with bronchitis) may be helped by antibiotic therapy Oral aminophylline (85% theophylline) in doses sufficient to produce therapeutic blood levels, usually 100 -400 mg 4 times daily, is the bronchodilator of choice. Various combinations of ephednne with aminophylline and a barbiturate or hydroxyzine have been used for many years with benefit in mild asthma. Side effects (tachycardia and central nervous system stimulation) are frequent and limit their usefulness.
The newer beta-adrenergic stimulators have a relatively greater degree of beta-2 specificity and longer action; accordingly, they are somewhat more effective and have fewer side effects. Terbutaline (Brethme, Bncanyl) may be given orally (2. 5 -5 mg 3 times daily) or subcutaneously (0. 25 mg). Albuterol (Proventil, Ventolm) may be given orally (2 -4 mg 3 or 4 times daily) or as a metered dose aerosol (1 -2 inhalations every 4— 6 hours) These agents cause an initial adrenergic response of anxiety and tremor, but this tends to decrease over a few days even while drug intake continues Patients should be advised against excessiveuse The older nebulized drugs, epinephnne, isoproterenol, metaproterenol (Alupent, Metaprel), and isoethanne (Bronkosol) are useful in relieving or preventing mild wheezing when used in a hand bulb or pressurized nebulizer.
Patients who are not helped by other measures may be treated on a long-term basis with a corticosteroid The dosage employed should be sufficient to keep the patient comfortable and relatively free of symptoms Begin with 10 mg 3 -4 times daily and reduce gradually to the lowest effective maintenance dose, preferably on an alternate-day schedule An aerosolized corticosteroid, beclomethasone dipropionate (Beclovent, Vanceni), has been found to be effective in many asthmatic patients who require corticosteroids It is virtually unabsorbable and thus has no systemic side effects Its action occurs in the bronchial mucosa It is not effective during an acute attack, since its action depends on deposition deep in the bronchial tree It is best introduced after wheezing has been controlled by a systemic corticosteroid, which can then be reduced or eliminated In patients who have been receiving long-term treatment with a systemic corticosteroid, joint pains and other symptoms may appear as that drug is reduced.

n n Prolonged gradual weamng may be necessary Some patients will continue to require systemic corticosteroid drugs in smaller dosage Some receive no benefit from the aerosolized form In a recent report, no adverse effects were found in mothers or infants when inhaled beclomethasone was used dur ing pregnancy in the recommended dosage Beclomethasone may be used after administration of a rapidly acting nebulized bronchodilator such as isoproterenol or isoethanne to achieve deeper deposition in the bronchial tree The initial dose is 2 mhalations 4 times daily, with subsequent adjustment to the lowest effective dose. Doses as frequent as 8 times daily are acceptable if significant improvement results Some patients are well maintained on twice daily treatments.
Pulmonary emphysema
Even patients who are well controlled with the nebulized drug may have occasional increased wheezing dunng colds or intense exposure to allergens. Short courses of prednisone may be required Cromolyn sodium (Intal) is useful mainly in atopic asthma to specifically inhibit the liberation of mediators initiated by the antigen antibody reaction. It is effective only during remissions to prevent recunent attacks and to reduce the requirement for corticosteroids. It is administered as a micronized powder by inhalation. Occasional phar yngeal and tracheal imtation has been noted, but no systemic side effects have been reported
n n Prognosis : Most patients with asthma adjust well to the necessity for continued medical treatment throughout life Inadequate control or persistent aggravation by unmodified environmental conditions favors the development of incapacitating or even life threatening complications

Thank you!
Asthma.ppt