2dd04d55347dffd337b63ebf7b8e77ed.ppt
- Количество слайдов: 43
 The wider strategic context – implications for HITs HIT Conference 17 June 2016 Becky Pollard - Director of Public Health, Bristol City Council Jo Copping - Public Health Consultant, Bristol City Council Paula Clarke - Director of Strategy and Transformation, United Hospital Bristol NHS Foundation Trust Justine Rawlings – Head of Strategic Planning, Bristol Clinical Commissioning Group Neighbourhoods Directorate Public Health Slide 1
The wider strategic context – implications for HITs HIT Conference 17 June 2016 Becky Pollard - Director of Public Health, Bristol City Council Jo Copping - Public Health Consultant, Bristol City Council Paula Clarke - Director of Strategy and Transformation, United Hospital Bristol NHS Foundation Trust Justine Rawlings – Head of Strategic Planning, Bristol Clinical Commissioning Group Neighbourhoods Directorate Public Health Slide 1
 Aim of session To give an overview of the wider strategic context in which Bristol Health Partners operates within To enable HITs prioritise and maximise their contribution towards improving the health and wellbeing of the local population Neighbourhoods Directorate Public Health Slide 2
Aim of session To give an overview of the wider strategic context in which Bristol Health Partners operates within To enable HITs prioritise and maximise their contribution towards improving the health and wellbeing of the local population Neighbourhoods Directorate Public Health Slide 2
 Key Strategic Programmes Our Bristol Plan – Mayor’s City Vision Health and wellbeing boards / strategies / public health priorities Joint strategic needs assessment Better Care programme NHS Commissioners vision NHS Five Year View / Bristol, North Somerset and South Gloucestershire Sustainability Transformation Plan Neighbourhoods Directorate Public Health Slide 3
Key Strategic Programmes Our Bristol Plan – Mayor’s City Vision Health and wellbeing boards / strategies / public health priorities Joint strategic needs assessment Better Care programme NHS Commissioners vision NHS Five Year View / Bristol, North Somerset and South Gloucestershire Sustainability Transformation Plan Neighbourhoods Directorate Public Health Slide 3
 Note of caution… Presentation largely focuses on strategies in Bristol, although similar strategies exist within each of the local authority and clinical commissioning group areas across greater Brsitol area (i. e. North Somerset and South Glocuestershire) Neighbourhoods Directorate Public Health Slide 4
Note of caution… Presentation largely focuses on strategies in Bristol, although similar strategies exist within each of the local authority and clinical commissioning group areas across greater Brsitol area (i. e. North Somerset and South Glocuestershire) Neighbourhoods Directorate Public Health Slide 4
 Our Bristol Plan – City health and wellbeing priorities (1) More new and affordable homes Reduce rough sleeping Better start in life - protect children’s centres – tackle child poverty, building resilience, safeguarding, family interventions for life Improve school results by working with educational providers to share best practice Safe, clean streets Infrastructure investment – public transport and digital inclusion Neighbourhoods Directorate Public Health Slide 5
Our Bristol Plan – City health and wellbeing priorities (1) More new and affordable homes Reduce rough sleeping Better start in life - protect children’s centres – tackle child poverty, building resilience, safeguarding, family interventions for life Improve school results by working with educational providers to share best practice Safe, clean streets Infrastructure investment – public transport and digital inclusion Neighbourhoods Directorate Public Health Slide 5
 Our Bristol Plan – City health and wellbeing priorities (2) Ethical Care Council - strong health and care workforce Support for carers Dementia friendly city Public Health - healthy lifestyles / tackle social isolation Mental health (prevention and care services) Control over health and care spending Protecting social services Tackling health inequalities Disability Equalities Forum - employment and support Neighbourhoods Directorate Public Health Slide 6
Our Bristol Plan – City health and wellbeing priorities (2) Ethical Care Council - strong health and care workforce Support for carers Dementia friendly city Public Health - healthy lifestyles / tackle social isolation Mental health (prevention and care services) Control over health and care spending Protecting social services Tackling health inequalities Disability Equalities Forum - employment and support Neighbourhoods Directorate Public Health Slide 6
 Our Bristol Plan – City health and wellbeing priorities (3) Tackle fuel poverty Protect green space Promote sustainable food networks Support/invest in cycling Improve air quality Make sports accessible to all Neighbourhoods Directorate Public Health Slide 7
Our Bristol Plan – City health and wellbeing priorities (3) Tackle fuel poverty Protect green space Promote sustainable food networks Support/invest in cycling Improve air quality Make sports accessible to all Neighbourhoods Directorate Public Health Slide 7
 Health and Wellbeing Boards Assess the needs of the local community through the Joint Strategic Needs Assessment (JSNA) and consider the need or likely need capable of being met or affected by Local Authority or CCG functions; Agree and produce a Health & Wellbeing Strategy, that addresses need, and which commissioners will need to take into account when they develop plans for health care, social care and public health; Promote Integration (across Health, Public Health and Social Care) Advise the Mayor in relation to the taking of executive decisions that concern health and well being functions of the local authority (this part is unique to Bristol) Neighbourhoods Directorate Public Health Slide 8
Health and Wellbeing Boards Assess the needs of the local community through the Joint Strategic Needs Assessment (JSNA) and consider the need or likely need capable of being met or affected by Local Authority or CCG functions; Agree and produce a Health & Wellbeing Strategy, that addresses need, and which commissioners will need to take into account when they develop plans for health care, social care and public health; Promote Integration (across Health, Public Health and Social Care) Advise the Mayor in relation to the taking of executive decisions that concern health and well being functions of the local authority (this part is unique to Bristol) Neighbourhoods Directorate Public Health Slide 8
 Health and Wellbeing Boards Key health challenges National challenges: Premature deaths – cancer, heart disease, stroke Dementia, Long term conditions Smoking, alcohol, unhealthy weight and mental health Local challenges: Growing and changing population – children and older people Health inequalities Neighbourhoods Directorate Public Health Slide 9
Health and Wellbeing Boards Key health challenges National challenges: Premature deaths – cancer, heart disease, stroke Dementia, Long term conditions Smoking, alcohol, unhealthy weight and mental health Local challenges: Growing and changing population – children and older people Health inequalities Neighbourhoods Directorate Public Health Slide 9
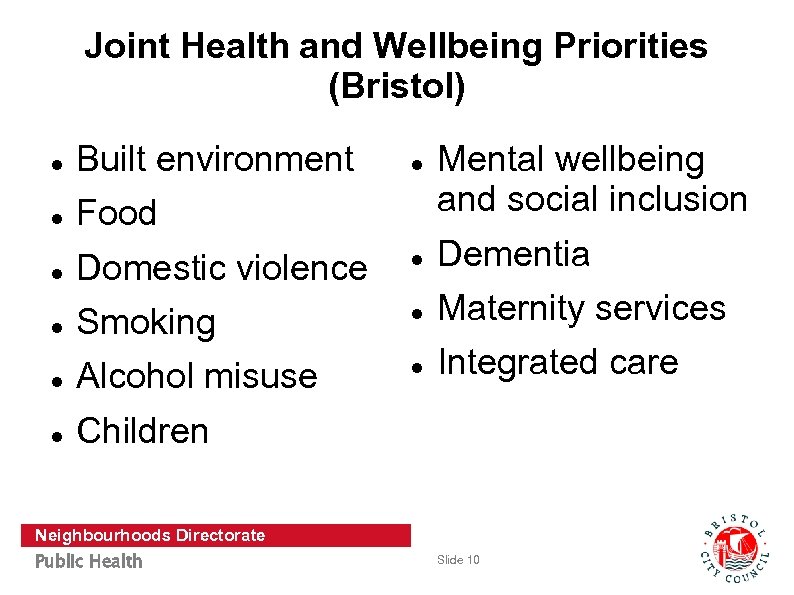 Joint Health and Wellbeing Priorities (Bristol) Built environment Food Mental wellbeing and social inclusion Domestic violence Dementia Smoking Maternity services Alcohol misuse Integrated care Children Neighbourhoods Directorate Public Health Slide 10
Joint Health and Wellbeing Priorities (Bristol) Built environment Food Mental wellbeing and social inclusion Domestic violence Dementia Smoking Maternity services Alcohol misuse Integrated care Children Neighbourhoods Directorate Public Health Slide 10
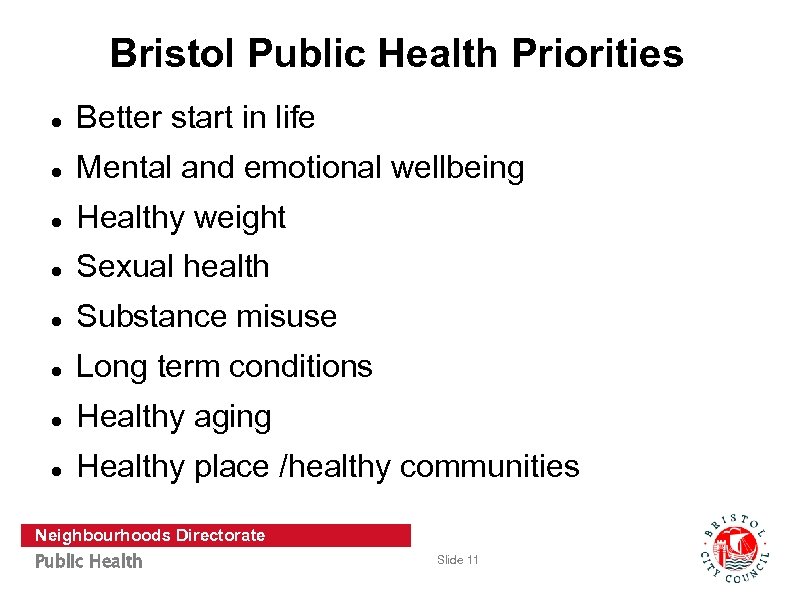 Bristol Public Health Priorities Better start in life Mental and emotional wellbeing Healthy weight Sexual health Substance misuse Long term conditions Healthy aging Healthy place /healthy communities Neighbourhoods Directorate Public Health Slide 11
Bristol Public Health Priorities Better start in life Mental and emotional wellbeing Healthy weight Sexual health Substance misuse Long term conditions Healthy aging Healthy place /healthy communities Neighbourhoods Directorate Public Health Slide 11
 Role of the Joint Strategic Needs Assessment Neighbourhoods Directorate Public Health Slide 12
Role of the Joint Strategic Needs Assessment Neighbourhoods Directorate Public Health Slide 12
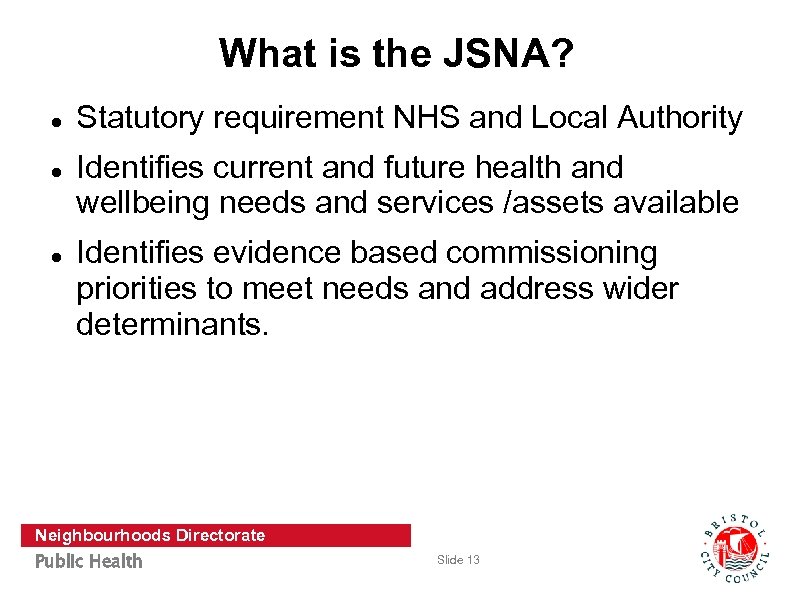 What is the JSNA? Statutory requirement NHS and Local Authority Identifies current and future health and wellbeing needs and services /assets available Identifies evidence based commissioning priorities to meet needs and address wider determinants. Neighbourhoods Directorate Public Health Slide 13
What is the JSNA? Statutory requirement NHS and Local Authority Identifies current and future health and wellbeing needs and services /assets available Identifies evidence based commissioning priorities to meet needs and address wider determinants. Neighbourhoods Directorate Public Health Slide 13
 JSNA should Influence strategic planning and commissioning Inform Joint Health and Wellbeing Strategy Be a tool to drive health improvement and reduce inequalities Promote the efficient use of resources Neighbourhoods Directorate Public Health Slide 14
JSNA should Influence strategic planning and commissioning Inform Joint Health and Wellbeing Strategy Be a tool to drive health improvement and reduce inequalities Promote the efficient use of resources Neighbourhoods Directorate Public Health Slide 14
 Current JSNA Overarching data profile Sections on: o Demographics o Life expectancy o Wider determinants o Lifestyles o Long term conditions National & local data Published Dec 2015 Ward boundaries changed May 2016 Neighbourhoods Directorate Public Health Slide 15
Current JSNA Overarching data profile Sections on: o Demographics o Life expectancy o Wider determinants o Lifestyles o Long term conditions National & local data Published Dec 2015 Ward boundaries changed May 2016 Neighbourhoods Directorate Public Health Slide 15
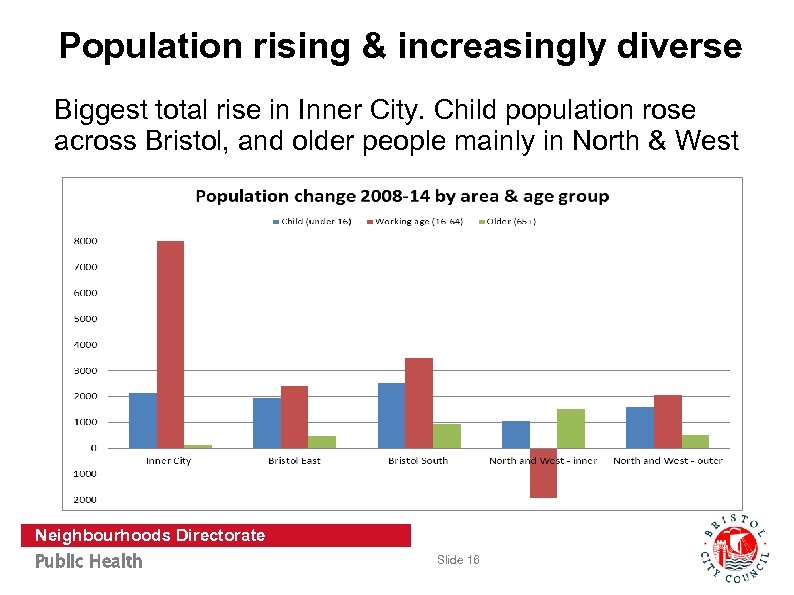 Population rising & increasingly diverse Biggest total rise in Inner City. Child population rose across Bristol, and older people mainly in North & West Neighbourhoods Directorate Public Health Slide 16
Population rising & increasingly diverse Biggest total rise in Inner City. Child population rose across Bristol, and older people mainly in North & West Neighbourhoods Directorate Public Health Slide 16
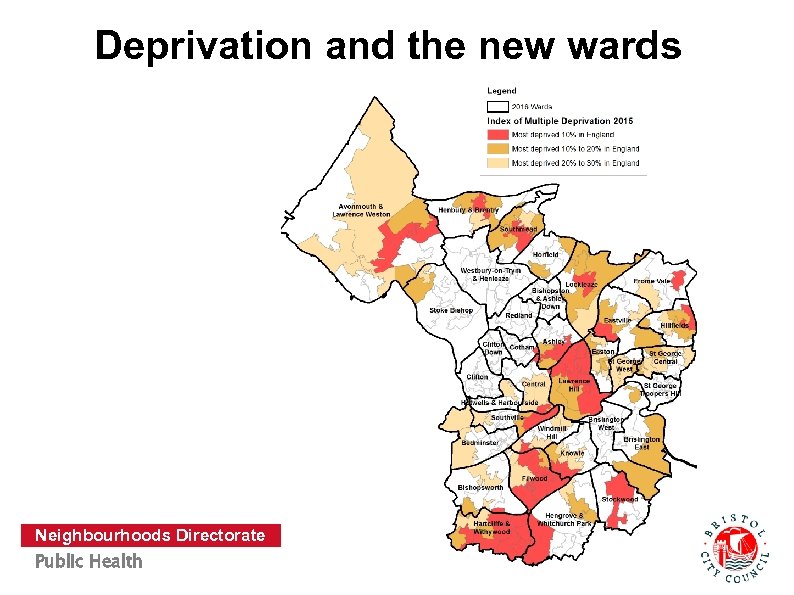 Deprivation and the new wards Neighbourhoods Directorate Public Health Slide 17
Deprivation and the new wards Neighbourhoods Directorate Public Health Slide 17
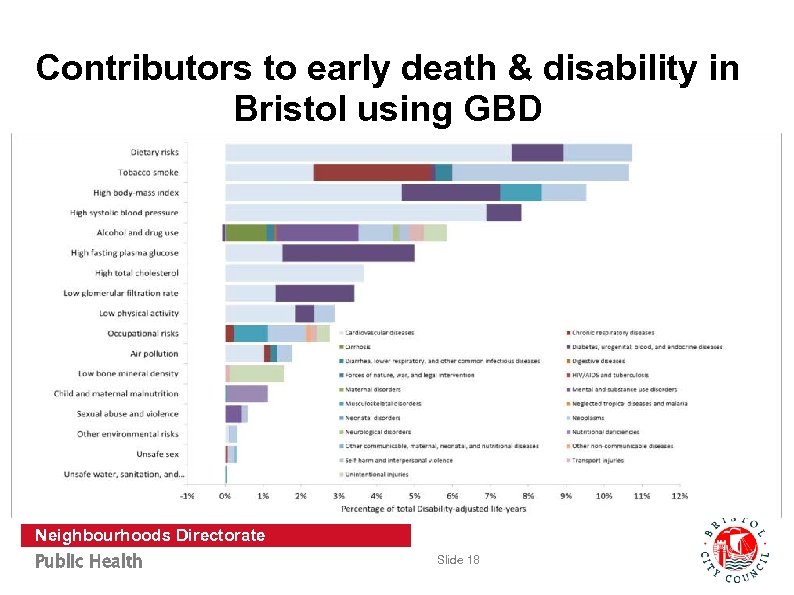 Contributors to early death & disability in Bristol using GBD Neighbourhoods Directorate Public Health Slide 18
Contributors to early death & disability in Bristol using GBD Neighbourhoods Directorate Public Health Slide 18
 Physical activity Local Quality of Life survey (2015) 2 in 3 Bristolians take enough weekly exercise Ward range 48% - 80% Note – detailed analysis of 40+ Qo. L variables to inform APPh. LE HIT Neighbourhoods Directorate Public Health Slide 19
Physical activity Local Quality of Life survey (2015) 2 in 3 Bristolians take enough weekly exercise Ward range 48% - 80% Note – detailed analysis of 40+ Qo. L variables to inform APPh. LE HIT Neighbourhoods Directorate Public Health Slide 19
 Overweight and obesity Children 4/5 yrs: 23% Children 10/11 yrs*: 35% Adults: 57% (national 65%) Inequalities across Bristol Neighbourhoods Directorate Public Health Slide 20
Overweight and obesity Children 4/5 yrs: 23% Children 10/11 yrs*: 35% Adults: 57% (national 65%) Inequalities across Bristol Neighbourhoods Directorate Public Health Slide 20
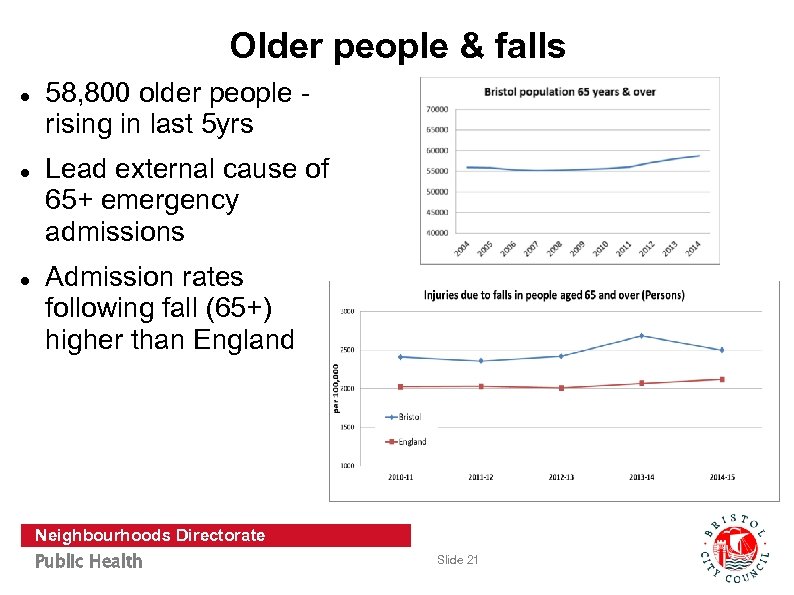 Older people & falls 58, 800 older people rising in last 5 yrs Lead external cause of 65+ emergency admissions Admission rates following fall (65+) higher than England Neighbourhoods Directorate Public Health Slide 21
Older people & falls 58, 800 older people rising in last 5 yrs Lead external cause of 65+ emergency admissions Admission rates following fall (65+) higher than England Neighbourhoods Directorate Public Health Slide 21
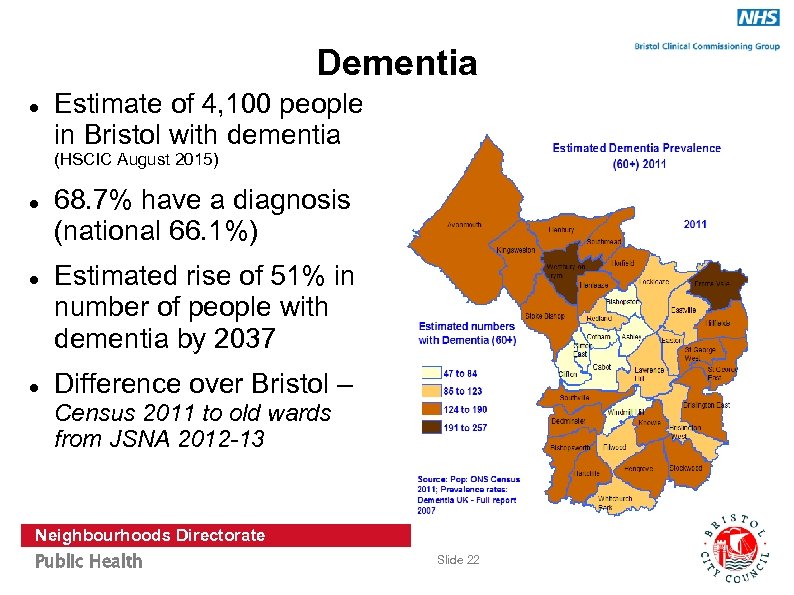 Dementia Estimate of 4, 100 people in Bristol with dementia (HSCIC August 2015) 68. 7% have a diagnosis (national 66. 1%) Estimated rise of 51% in number of people with dementia by 2037 Difference over Bristol – Census 2011 to old wards from JSNA 2012 -13 Neighbourhoods Directorate Public Health Slide 22
Dementia Estimate of 4, 100 people in Bristol with dementia (HSCIC August 2015) 68. 7% have a diagnosis (national 66. 1%) Estimated rise of 51% in number of people with dementia by 2037 Difference over Bristol – Census 2011 to old wards from JSNA 2012 -13 Neighbourhoods Directorate Public Health Slide 22
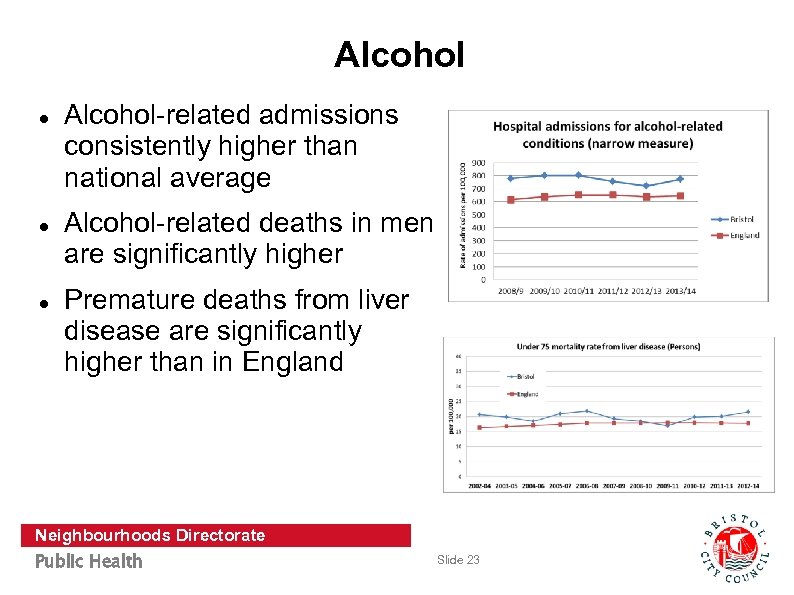 Alcohol Alcohol-related admissions consistently higher than national average Alcohol-related deaths in men are significantly higher Premature deaths from liver disease are significantly higher than in England Neighbourhoods Directorate Public Health Slide 23
Alcohol Alcohol-related admissions consistently higher than national average Alcohol-related deaths in men are significantly higher Premature deaths from liver disease are significantly higher than in England Neighbourhoods Directorate Public Health Slide 23
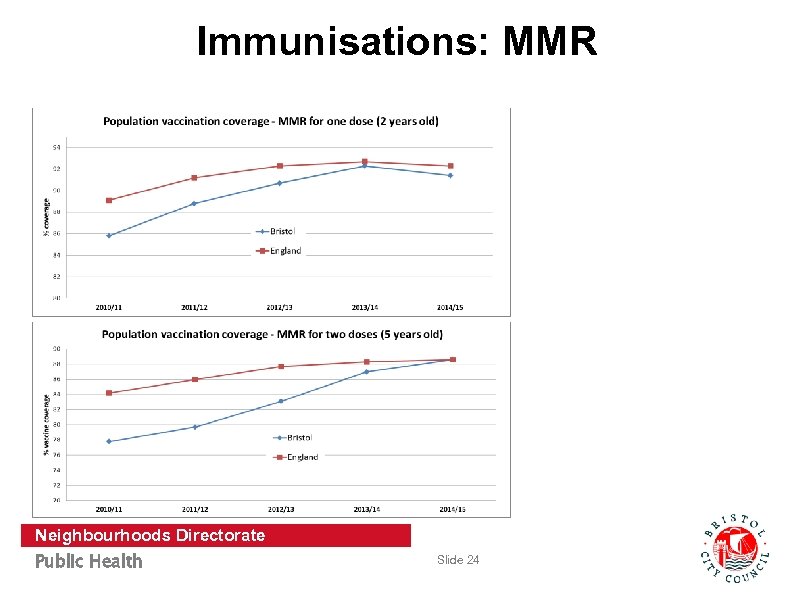 Immunisations: MMR Neighbourhoods Directorate Public Health Slide 24
Immunisations: MMR Neighbourhoods Directorate Public Health Slide 24
 What more do we need from JSNA? So what do we need to do about this data? How can we prevent these things? What are the inequalities? How do we make best use of limited resources what is the evidence? How can we make data access easier? Neighbourhoods Directorate Public Health Slide 25
What more do we need from JSNA? So what do we need to do about this data? How can we prevent these things? What are the inequalities? How do we make best use of limited resources what is the evidence? How can we make data access easier? Neighbourhoods Directorate Public Health Slide 25
 Plans for enhanced Bristol JSNA (1) Develop JSNA Chapters (needs assessments) Quantitative and qualitative data to give a comprehensive view of health (in priority areas) to include: - Current services and community assets - Evidence of effectiveness - Views of patients/public/staff/commissioners (2) Better access to data and JSNA products (such as JSNA chapters, new ward profiles, GP profiles etc. ) In order to determine gaps & recommendations for commissioners Neighbourhoods Directorate Public Health Slide 26
Plans for enhanced Bristol JSNA (1) Develop JSNA Chapters (needs assessments) Quantitative and qualitative data to give a comprehensive view of health (in priority areas) to include: - Current services and community assets - Evidence of effectiveness - Views of patients/public/staff/commissioners (2) Better access to data and JSNA products (such as JSNA chapters, new ward profiles, GP profiles etc. ) In order to determine gaps & recommendations for commissioners Neighbourhoods Directorate Public Health Slide 26
 JSNA and the role of HITs? Utilise JSNA profile to give overview of health and demographics www. bristol. gov. uk/jsna Use new JSNA chapters to understand key issues and recommendations for Bristol in relevant areas and Support the development of the JSNA chapters through reference groups Contribute to views of stakeholders Inform the ‘evidence of effectiveness’ section of the JSNA chapters Contribute local data Neighbourhoods Directorate Public Health Slide 27
JSNA and the role of HITs? Utilise JSNA profile to give overview of health and demographics www. bristol. gov. uk/jsna Use new JSNA chapters to understand key issues and recommendations for Bristol in relevant areas and Support the development of the JSNA chapters through reference groups Contribute to views of stakeholders Inform the ‘evidence of effectiveness’ section of the JSNA chapters Contribute local data Neighbourhoods Directorate Public Health Slide 27
 Better Care Bristol – Vision Integrated local services, bringing together health and social care resources in a locality model, targeting resources where need is greatest Prevention and self-care – focusing on key priority areas, help people to manage their lives well, stay healthy and avoid deterioration, promote independence and help people and their carers to manage conditions Integrated pathways that support people in managing conditions from the earliest indications through to severe and complex needs. Neighbourhoods Directorate Public Health Slide 28
Better Care Bristol – Vision Integrated local services, bringing together health and social care resources in a locality model, targeting resources where need is greatest Prevention and self-care – focusing on key priority areas, help people to manage their lives well, stay healthy and avoid deterioration, promote independence and help people and their carers to manage conditions Integrated pathways that support people in managing conditions from the earliest indications through to severe and complex needs. Neighbourhoods Directorate Public Health Slide 28
 Better Care Bristol - Enablers Integrating IT and sharing data, with IT development based on the needs of users and carers. Co-ordinating with workforce development and mobilise workforce initiatives to enable the integration agenda. Change management support – helping teams managing risk, supporting changes in behaviour, measuring progress, being open about change, making better use of voluntary sector and community assets, and empowering patients, service users and carers. Neighbourhoods Directorate Public Health Slide 29
Better Care Bristol - Enablers Integrating IT and sharing data, with IT development based on the needs of users and carers. Co-ordinating with workforce development and mobilise workforce initiatives to enable the integration agenda. Change management support – helping teams managing risk, supporting changes in behaviour, measuring progress, being open about change, making better use of voluntary sector and community assets, and empowering patients, service users and carers. Neighbourhoods Directorate Public Health Slide 29
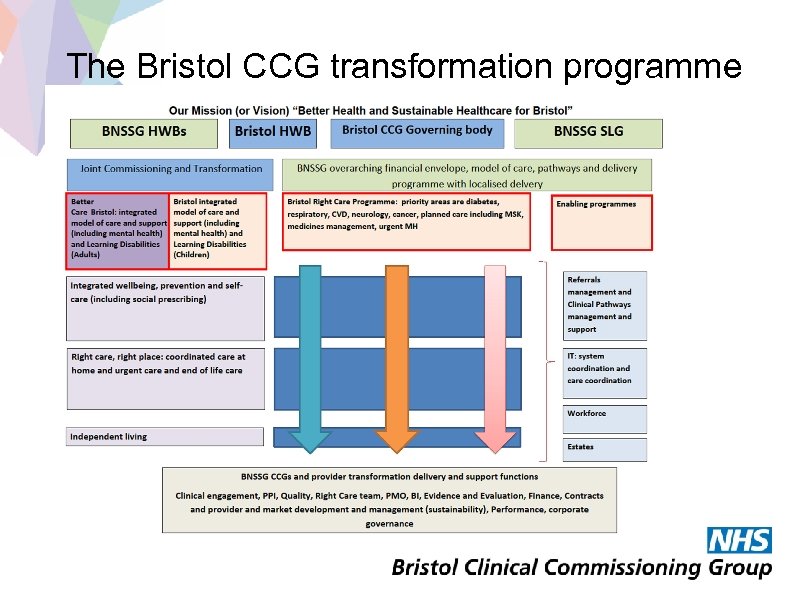 The Bristol CCG transformation programme
The Bristol CCG transformation programme
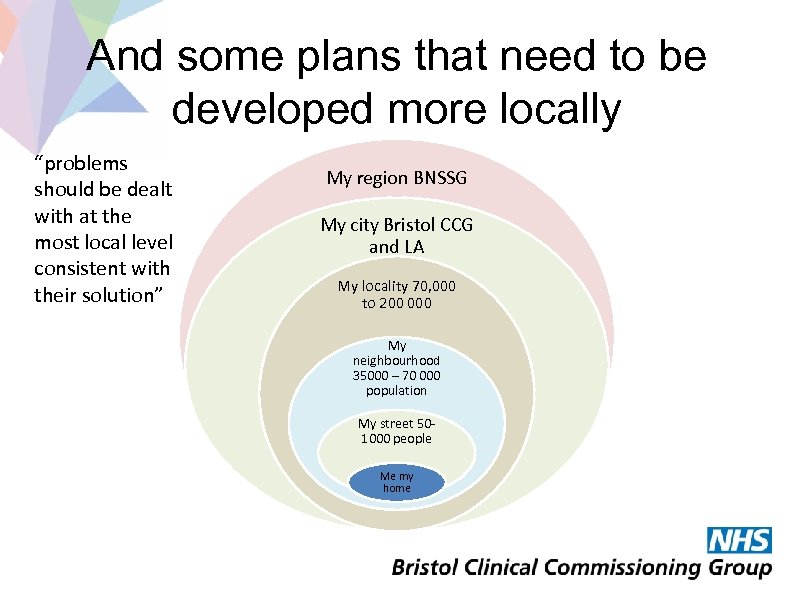 And some plans that need to be developed more locally “problems should be dealt with at the most local level consistent with their solution” My region BNSSG My city Bristol CCG and LA My locality 70, 000 to 200 000 My neighbourhood 35000 – 70 000 population My street 501000 people Me my home
And some plans that need to be developed more locally “problems should be dealt with at the most local level consistent with their solution” My region BNSSG My city Bristol CCG and LA My locality 70, 000 to 200 000 My neighbourhood 35000 – 70 000 population My street 501000 people Me my home
 BNSSG: Sustainability and Transformation Plan Paula Clarke Executive Director Strategy & Transformation University Hospitals Bristol NHS Foundation Trust
BNSSG: Sustainability and Transformation Plan Paula Clarke Executive Director Strategy & Transformation University Hospitals Bristol NHS Foundation Trust
 Background: The Five Year Forward View • The NHS Five Year Forward View, published in October 2014, considers the progress made in improving health and care services in recent years and the challenges that we face leading up to 2020/21. These challenges include: § § the quality of care that people receive can be variable the burden preventable illness constitutes growing demands on the NHS means that local health and care organisations are facing financial pressure the needs and expectations of the public are changing. New treatments options are emerging, and we rightly expect better care closer to home. • There is broad agreement that we must make changes to how we live, how we access care, and how care is delivered. • This means more preventative care; finding new ways to meet people’s needs; and identifying ways to do things more efficiently. • We need to close the gaps in health, finance and quality of care between where we are now and where we need to be in 2020/21.
Background: The Five Year Forward View • The NHS Five Year Forward View, published in October 2014, considers the progress made in improving health and care services in recent years and the challenges that we face leading up to 2020/21. These challenges include: § § the quality of care that people receive can be variable the burden preventable illness constitutes growing demands on the NHS means that local health and care organisations are facing financial pressure the needs and expectations of the public are changing. New treatments options are emerging, and we rightly expect better care closer to home. • There is broad agreement that we must make changes to how we live, how we access care, and how care is delivered. • This means more preventative care; finding new ways to meet people’s needs; and identifying ways to do things more efficiently. • We need to close the gaps in health, finance and quality of care between where we are now and where we need to be in 2020/21.
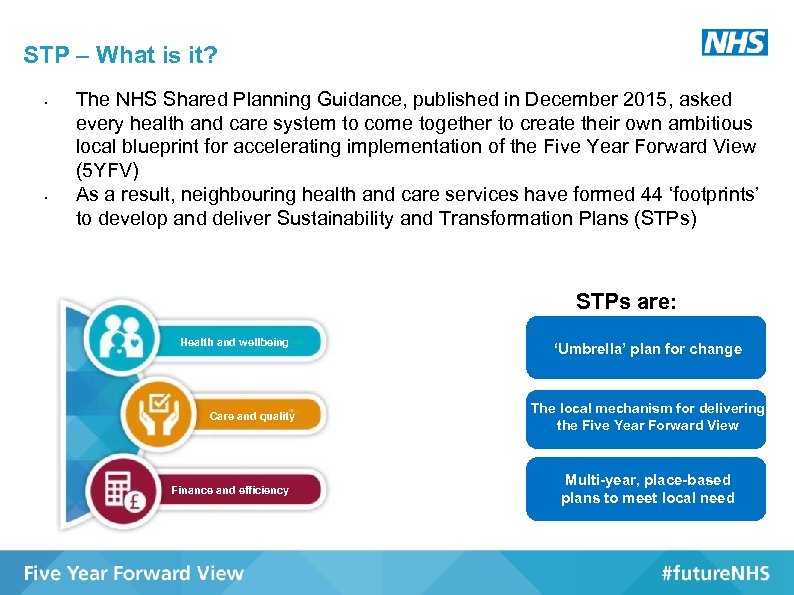 STP – What is it? • • The NHS Shared Planning Guidance, published in December 2015, asked every health and care system to come together to create their own ambitious local blueprint for accelerating implementation of the Five Year Forward View (5 YFV) As a result, neighbouring health and care services have formed 44 ‘footprints’ to develop and deliver Sustainability and Transformation Plans (STPs) STPs are: Health and wellbeing Care and quality Finance and efficiency ‘Umbrella’ plan for change The local mechanism for delivering the Five Year Forward View Multi-year, place-based plans to meet local need
STP – What is it? • • The NHS Shared Planning Guidance, published in December 2015, asked every health and care system to come together to create their own ambitious local blueprint for accelerating implementation of the Five Year Forward View (5 YFV) As a result, neighbouring health and care services have formed 44 ‘footprints’ to develop and deliver Sustainability and Transformation Plans (STPs) STPs are: Health and wellbeing Care and quality Finance and efficiency ‘Umbrella’ plan for change The local mechanism for delivering the Five Year Forward View Multi-year, place-based plans to meet local need
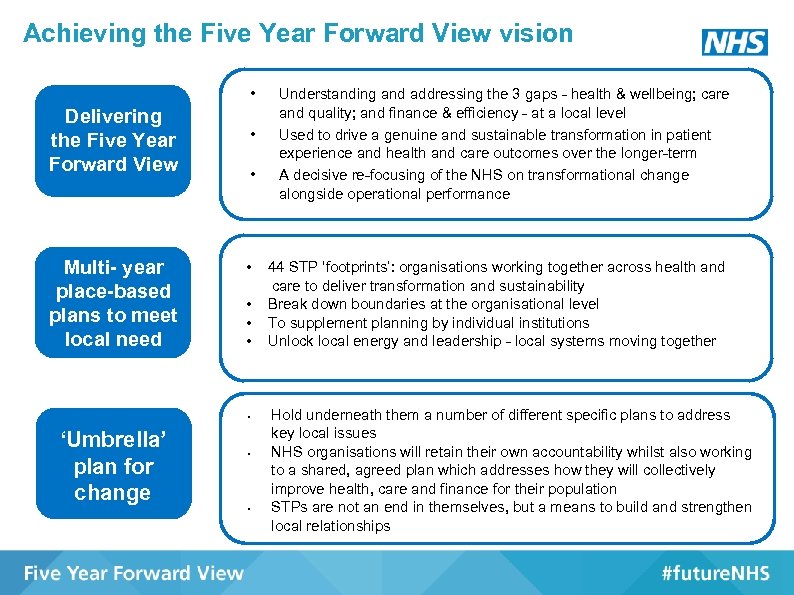 Achieving the Five Year Forward View vision • Delivering the Five Year Forward View Multi- year place-based plans to meet local need • • ‘Umbrella’ plan for change • • Understanding and addressing the 3 gaps - health & wellbeing; care and quality; and finance & efficiency - at a local level Used to drive a genuine and sustainable transformation in patient experience and health and care outcomes over the longer-term A decisive re-focusing of the NHS on transformational change alongside operational performance 44 STP ‘footprints’: organisations working together across health and care to deliver transformation and sustainability Break down boundaries at the organisational level To supplement planning by individual institutions Unlock local energy and leadership - local systems moving together Hold underneath them a number of different specific plans to address key local issues NHS organisations will retain their own accountability whilst also working to a shared, agreed plan which addresses how they will collectively improve health, care and finance for their population STPs are not an end in themselves, but a means to build and strengthen local relationships
Achieving the Five Year Forward View vision • Delivering the Five Year Forward View Multi- year place-based plans to meet local need • • ‘Umbrella’ plan for change • • Understanding and addressing the 3 gaps - health & wellbeing; care and quality; and finance & efficiency - at a local level Used to drive a genuine and sustainable transformation in patient experience and health and care outcomes over the longer-term A decisive re-focusing of the NHS on transformational change alongside operational performance 44 STP ‘footprints’: organisations working together across health and care to deliver transformation and sustainability Break down boundaries at the organisational level To supplement planning by individual institutions Unlock local energy and leadership - local systems moving together Hold underneath them a number of different specific plans to address key local issues NHS organisations will retain their own accountability whilst also working to a shared, agreed plan which addresses how they will collectively improve health, care and finance for their population STPs are not an end in themselves, but a means to build and strengthen local relationships
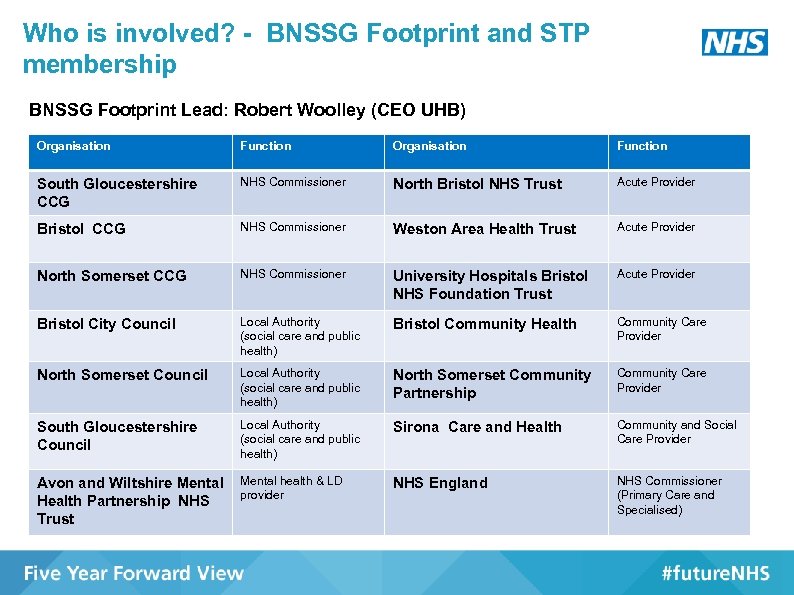 Who is involved? - BNSSG Footprint and STP membership BNSSG Footprint Lead: Robert Woolley (CEO UHB) Organisation Function South Gloucestershire CCG NHS Commissioner North Bristol NHS Trust Acute Provider Bristol CCG NHS Commissioner Weston Area Health Trust Acute Provider North Somerset CCG NHS Commissioner University Hospitals Bristol NHS Foundation Trust Acute Provider Bristol City Council Local Authority (social care and public health) Bristol Community Health Community Care Provider North Somerset Council Local Authority (social care and public health) North Somerset Community Partnership Community Care Provider South Gloucestershire Council Local Authority (social care and public health) Sirona Care and Health Community and Social Care Provider Avon and Wiltshire Mental Health Partnership NHS Trust Mental health & LD provider NHS England NHS Commissioner (Primary Care and Specialised)
Who is involved? - BNSSG Footprint and STP membership BNSSG Footprint Lead: Robert Woolley (CEO UHB) Organisation Function South Gloucestershire CCG NHS Commissioner North Bristol NHS Trust Acute Provider Bristol CCG NHS Commissioner Weston Area Health Trust Acute Provider North Somerset CCG NHS Commissioner University Hospitals Bristol NHS Foundation Trust Acute Provider Bristol City Council Local Authority (social care and public health) Bristol Community Health Community Care Provider North Somerset Council Local Authority (social care and public health) North Somerset Community Partnership Community Care Provider South Gloucestershire Council Local Authority (social care and public health) Sirona Care and Health Community and Social Care Provider Avon and Wiltshire Mental Health Partnership NHS Trust Mental health & LD provider NHS England NHS Commissioner (Primary Care and Specialised)
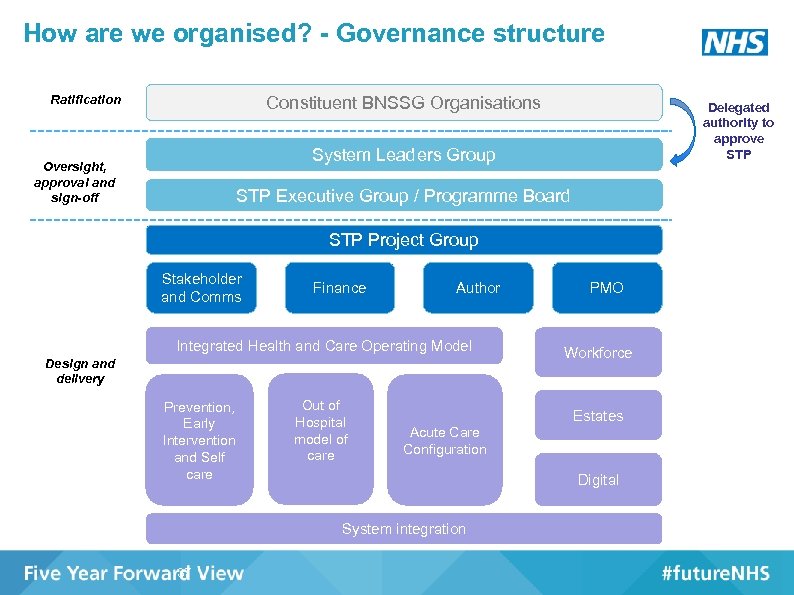 How are we organised? - Governance structure Ratification Constituent BNSSG Organisations Delegated authority to approve STP System Leaders Group Oversight, approval and sign-off STP Executive Group / Programme Board STP Project Group Stakeholder and Comms Finance Author Integrated Health and Care Operating Model Design and delivery Prevention, Early Intervention and Self care Out of Hospital model of care Workforce Estates Acute Care Configuration Digital System integration 37 PMO
How are we organised? - Governance structure Ratification Constituent BNSSG Organisations Delegated authority to approve STP System Leaders Group Oversight, approval and sign-off STP Executive Group / Programme Board STP Project Group Stakeholder and Comms Finance Author Integrated Health and Care Operating Model Design and delivery Prevention, Early Intervention and Self care Out of Hospital model of care Workforce Estates Acute Care Configuration Digital System integration 37 PMO
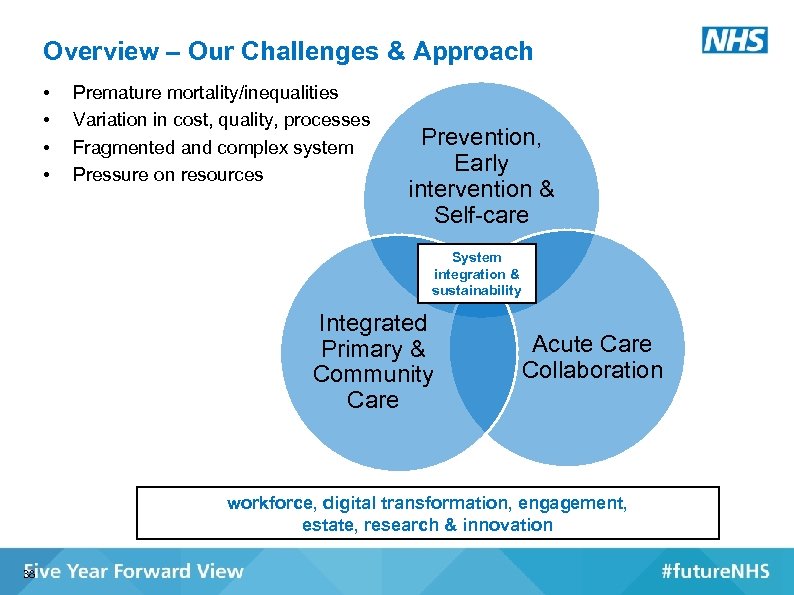 Overview – Our Challenges & Approach • • Premature mortality/inequalities Variation in cost, quality, processes Fragmented and complex system Pressure on resources Prevention, Early intervention & Self-care System integration & sustainability Integrated Primary & Community Care Acute Care Collaboration workforce, digital transformation, engagement, estate, research & innovation 38
Overview – Our Challenges & Approach • • Premature mortality/inequalities Variation in cost, quality, processes Fragmented and complex system Pressure on resources Prevention, Early intervention & Self-care System integration & sustainability Integrated Primary & Community Care Acute Care Collaboration workforce, digital transformation, engagement, estate, research & innovation 38
 So What's New? - Emerging themes & ideas • New relationship with the population – Shift to prevention, self-care, & early intervention in all services – Home as the locus of care delivery – Simplify points of access • New relationship between organisations / professionals – Workforce moving more easily across organisational boundaries – New roles, transferable training – Supporting the health & well-being of staff • Standardising and operating at the appropriate scale – Delivery around populations at different levels – Acute trust collaboration
So What's New? - Emerging themes & ideas • New relationship with the population – Shift to prevention, self-care, & early intervention in all services – Home as the locus of care delivery – Simplify points of access • New relationship between organisations / professionals – Workforce moving more easily across organisational boundaries – New roles, transferable training – Supporting the health & well-being of staff • Standardising and operating at the appropriate scale – Delivery around populations at different levels – Acute trust collaboration
 Emerging themes & ideas ctd. . • Pathways – Consistency in quality and access – Population approach, whole pathway review from prevention to acute – Eg. Diabetes, MSK, alcohol, falls, dementia • Digital enabled change - Connecting Care platform - Integrated personal health record and digital media
Emerging themes & ideas ctd. . • Pathways – Consistency in quality and access – Population approach, whole pathway review from prevention to acute – Eg. Diabetes, MSK, alcohol, falls, dementia • Digital enabled change - Connecting Care platform - Integrated personal health record and digital media
 What Next? Ø Submit next checkpoint report 30 th June Ø Feedback provided to each footprint Ø Progress planning and implementation by Autumn 2016 41
What Next? Ø Submit next checkpoint report 30 th June Ø Feedback provided to each footprint Ø Progress planning and implementation by Autumn 2016 41
 STP and the role of HITs Ø Supporting and accelerating the pace of change Ø Creating the evidence for impact Ø Demonstrating that translating the evidence into practice achieves the impact
STP and the role of HITs Ø Supporting and accelerating the pace of change Ø Creating the evidence for impact Ø Demonstrating that translating the evidence into practice achieves the impact
 Thank you
Thank you


