4098081a6287ffe3f28f23ba5840dba3.ppt
- Количество слайдов: 34
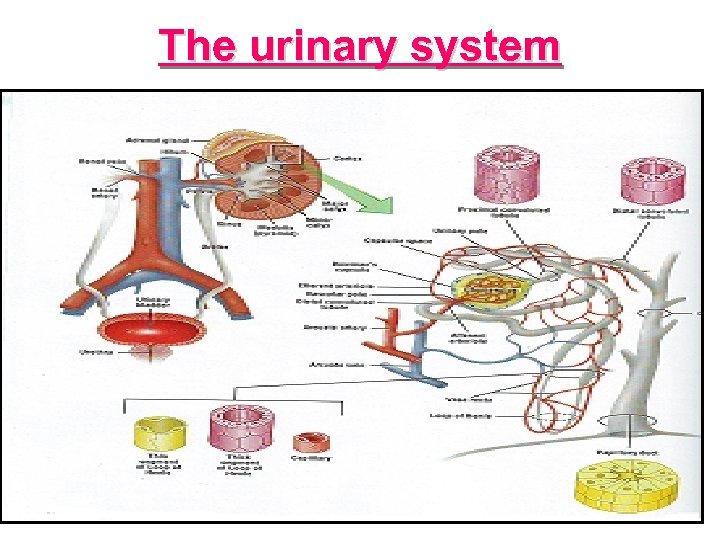 The urinary system
The urinary system
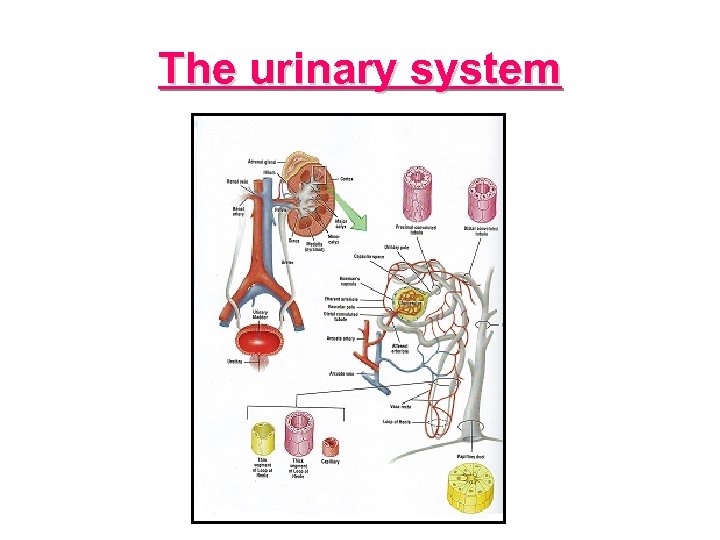
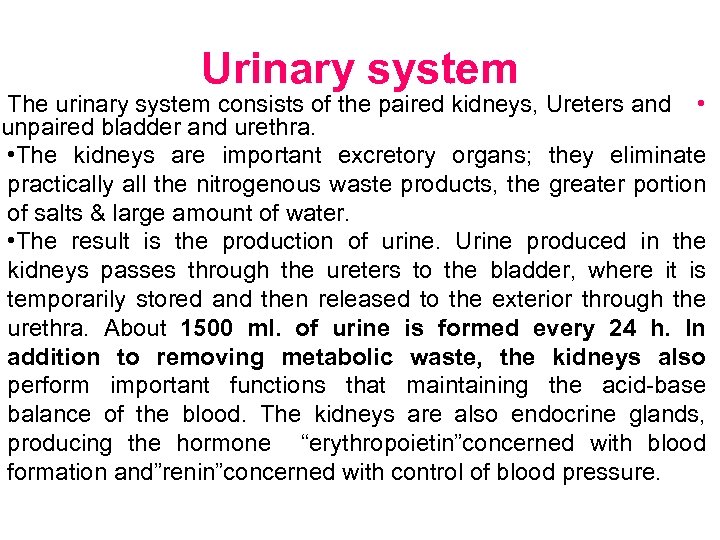 Urinary system The urinary system consists of the paired kidneys, Ureters and • unpaired bladder and urethra. • The kidneys are important excretory organs; they eliminate practically all the nitrogenous waste products, the greater portion of salts & large amount of water. • The result is the production of urine. Urine produced in the kidneys passes through the ureters to the bladder, where it is temporarily stored and then released to the exterior through the urethra. About 1500 ml. of urine is formed every 24 h. In addition to removing metabolic waste, the kidneys also perform important functions that maintaining the acid-base balance of the blood. The kidneys are also endocrine glands, producing the hormone “erythropoietin”concerned with blood formation and”renin”concerned with control of blood pressure.
Urinary system The urinary system consists of the paired kidneys, Ureters and • unpaired bladder and urethra. • The kidneys are important excretory organs; they eliminate practically all the nitrogenous waste products, the greater portion of salts & large amount of water. • The result is the production of urine. Urine produced in the kidneys passes through the ureters to the bladder, where it is temporarily stored and then released to the exterior through the urethra. About 1500 ml. of urine is formed every 24 h. In addition to removing metabolic waste, the kidneys also perform important functions that maintaining the acid-base balance of the blood. The kidneys are also endocrine glands, producing the hormone “erythropoietin”concerned with blood formation and”renin”concerned with control of blood pressure.
 Kidney Position: The kidneys located high on the posterior wall of the abdomen behind the peritoneum. The Right kidney is lowered than left due to the presence of liver. The kidneys occasionally congenitally located in the lower part of the abdomen called. Ectopia of the kidneys or Ectopic kidneys.
Kidney Position: The kidneys located high on the posterior wall of the abdomen behind the peritoneum. The Right kidney is lowered than left due to the presence of liver. The kidneys occasionally congenitally located in the lower part of the abdomen called. Ectopia of the kidneys or Ectopic kidneys.
 Structure : The kidneys are solid, bean shaped organs. The kidneys are surrounded by a “fibrous capsule” that is applied closely to its outer surface. Outside the capsule is a covering of fat known as the”perinephric fat”. The “perinephric fascia” surrounds the perinephric fat and enclose the kidneys and suprarenal glands. The perinephric fascia is a condensation of areolar tissue. It has a lateral convex border and a medial concave border which face the midline. The concave border show a depression called hilum through which the ureter descend, the renal vein leave, the renal artery, lymphatic vessel and nerve enter.
Structure : The kidneys are solid, bean shaped organs. The kidneys are surrounded by a “fibrous capsule” that is applied closely to its outer surface. Outside the capsule is a covering of fat known as the”perinephric fat”. The “perinephric fascia” surrounds the perinephric fat and enclose the kidneys and suprarenal glands. The perinephric fascia is a condensation of areolar tissue. It has a lateral convex border and a medial concave border which face the midline. The concave border show a depression called hilum through which the ureter descend, the renal vein leave, the renal artery, lymphatic vessel and nerve enter.
 Size : - • The size of the kidney is (5 inches) length, (3 inches) width, and (1 inch) thickness. The volume is (130 -150 c. c), & the average weight (170 gram).
Size : - • The size of the kidney is (5 inches) length, (3 inches) width, and (1 inch) thickness. The volume is (130 -150 c. c), & the average weight (170 gram).
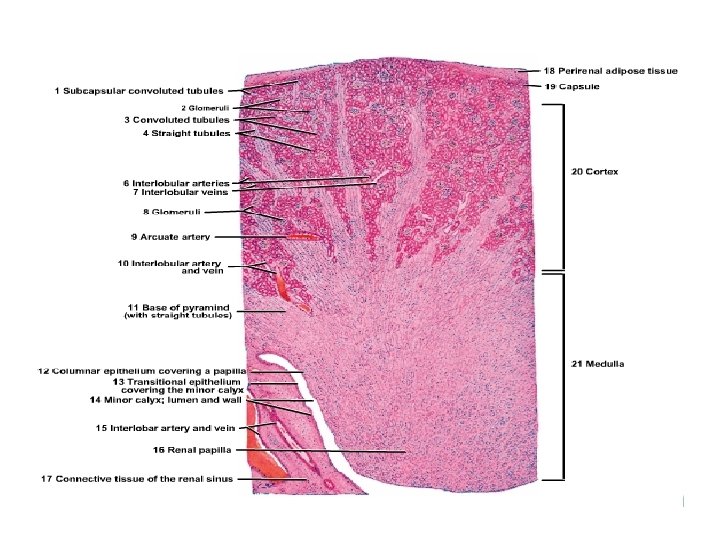
 On section: - » The kidneys show two areas an outer area called cortex and inner area called medulla which surround a cavity called renal sinus, which opens at the hilum.
On section: - » The kidneys show two areas an outer area called cortex and inner area called medulla which surround a cavity called renal sinus, which opens at the hilum.
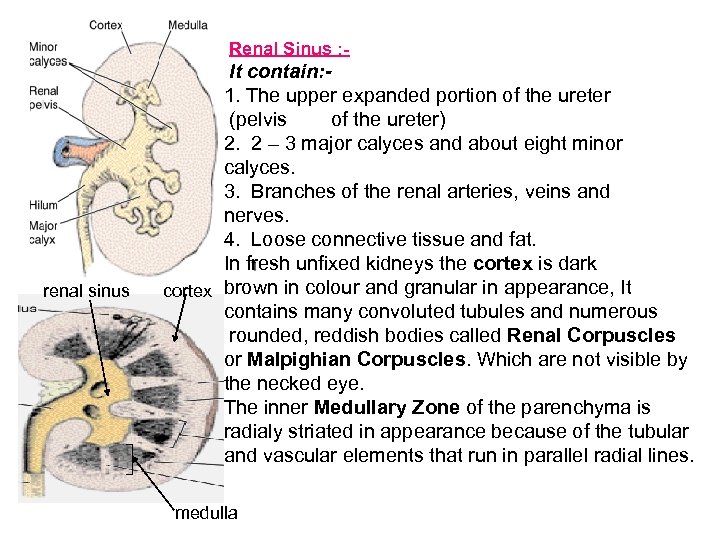 Renal Sinus : - renal sinus It contain: 1. The upper expanded portion of the ureter (pelvis of the ureter) 2. 2 – 3 major calyces and about eight minor calyces. 3. Branches of the renal arteries, veins and nerves. 4. Loose connective tissue and fat. In fresh unfixed kidneys the cortex is dark cortex brown in colour and granular in appearance, It contains many convoluted tubules and numerous rounded, reddish bodies called Renal Corpuscles or Malpighian Corpuscles. Which are not visible by the necked eye. The inner Medullary Zone of the parenchyma is radialy striated in appearance because of the tubular and vascular elements that run in parallel radial lines. medulla
Renal Sinus : - renal sinus It contain: 1. The upper expanded portion of the ureter (pelvis of the ureter) 2. 2 – 3 major calyces and about eight minor calyces. 3. Branches of the renal arteries, veins and nerves. 4. Loose connective tissue and fat. In fresh unfixed kidneys the cortex is dark cortex brown in colour and granular in appearance, It contains many convoluted tubules and numerous rounded, reddish bodies called Renal Corpuscles or Malpighian Corpuscles. Which are not visible by the necked eye. The inner Medullary Zone of the parenchyma is radialy striated in appearance because of the tubular and vascular elements that run in parallel radial lines. medulla
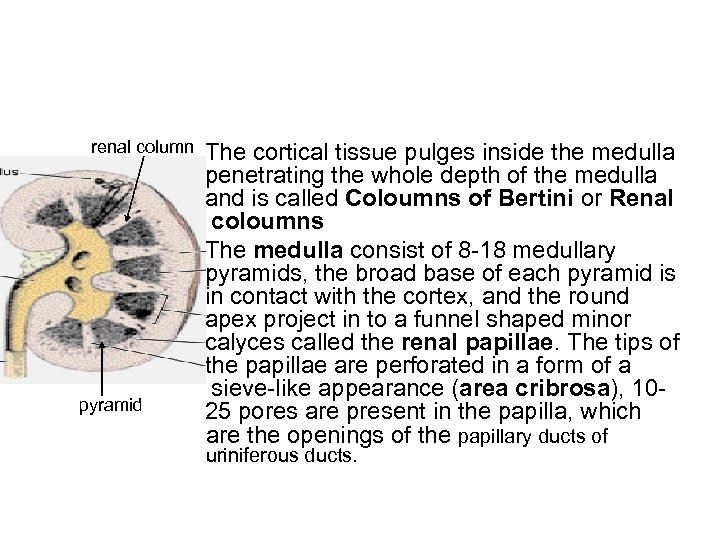 renal column pyramid The cortical tissue pulges inside the medulla penetrating the whole depth of the medulla and is called Coloumns of Bertini or Renal coloumns The medulla consist of 8 -18 medullary pyramids, the broad base of each pyramid is in contact with the cortex, and the round apex project in to a funnel shaped minor calyces called the renal papillae. The tips of the papillae are perforated in a form of a sieve-like appearance (area cribrosa), 1025 pores are present in the papilla, which are the openings of the papillary ducts of uriniferous ducts.
renal column pyramid The cortical tissue pulges inside the medulla penetrating the whole depth of the medulla and is called Coloumns of Bertini or Renal coloumns The medulla consist of 8 -18 medullary pyramids, the broad base of each pyramid is in contact with the cortex, and the round apex project in to a funnel shaped minor calyces called the renal papillae. The tips of the papillae are perforated in a form of a sieve-like appearance (area cribrosa), 1025 pores are present in the papilla, which are the openings of the papillary ducts of uriniferous ducts.
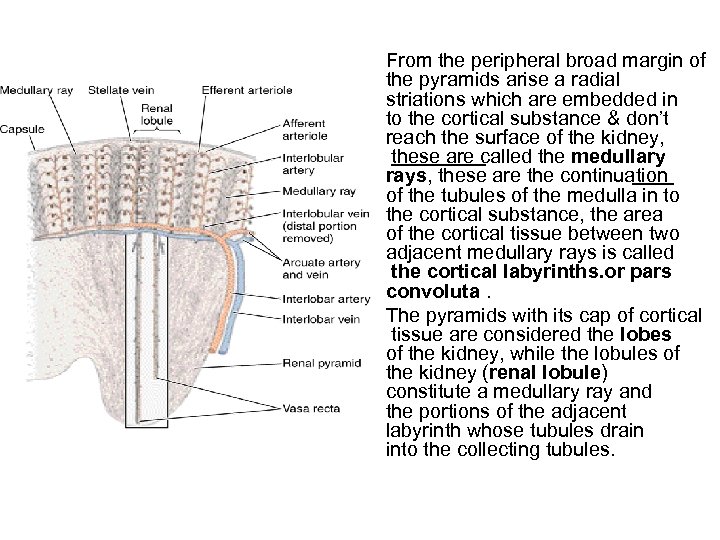 From the peripheral broad margin of the pyramids arise a radial striations which are embedded in to the cortical substance & don’t reach the surface of the kidney, these are called the medullary rays, these are the continuation of the tubules of the medulla in to the cortical substance, the area of the cortical tissue between two adjacent medullary rays is called the cortical labyrinths. or pars convoluta. The pyramids with its cap of cortical tissue are considered the lobes of the kidney, while the lobules of the kidney (renal lobule) constitute a medullary ray and the portions of the adjacent labyrinth whose tubules drain into the collecting tubules.
From the peripheral broad margin of the pyramids arise a radial striations which are embedded in to the cortical substance & don’t reach the surface of the kidney, these are called the medullary rays, these are the continuation of the tubules of the medulla in to the cortical substance, the area of the cortical tissue between two adjacent medullary rays is called the cortical labyrinths. or pars convoluta. The pyramids with its cap of cortical tissue are considered the lobes of the kidney, while the lobules of the kidney (renal lobule) constitute a medullary ray and the portions of the adjacent labyrinth whose tubules drain into the collecting tubules.
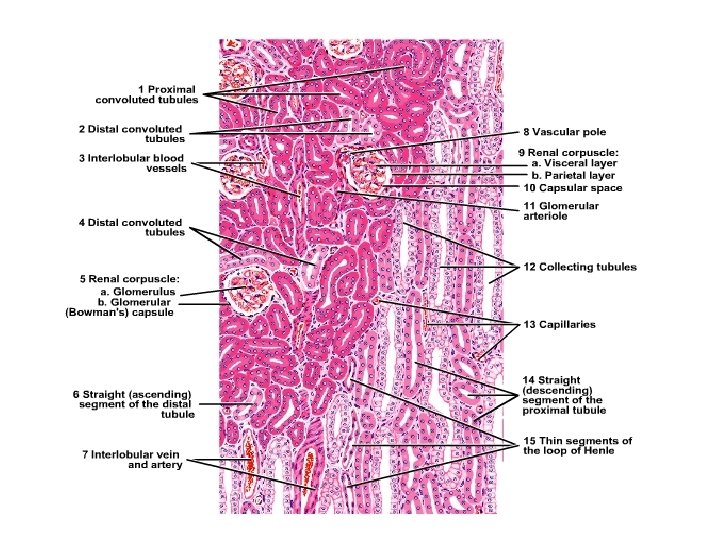
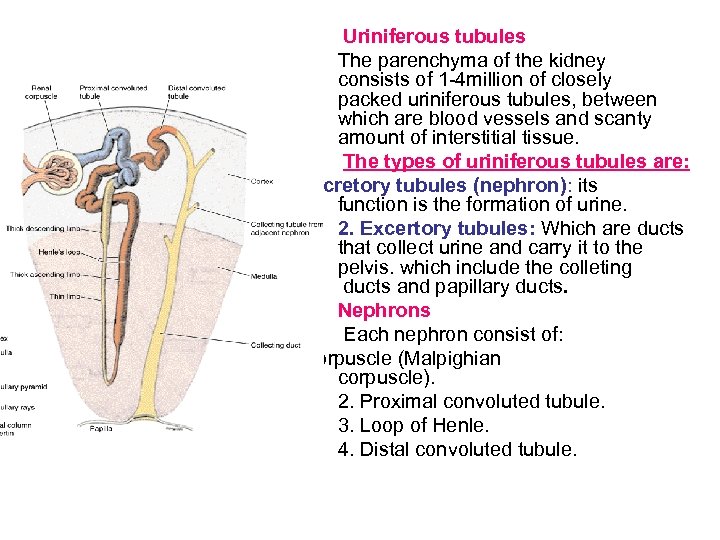 Uriniferous tubules The parenchyma of the kidney consists of 1 -4 million of closely packed uriniferous tubules, between which are blood vessels and scanty amount of interstitial tissue. The types of uriniferous tubules are: 1. Secretory tubules (nephron): its function is the formation of urine. 2. Excertory tubules: Which are ducts that collect urine and carry it to the pelvis. which include the colleting ducts and papillary ducts. Nephrons Each nephron consist of: 1. Renal corpuscle (Malpighian corpuscle). 2. Proximal convoluted tubule. 3. Loop of Henle. 4. Distal convoluted tubule.
Uriniferous tubules The parenchyma of the kidney consists of 1 -4 million of closely packed uriniferous tubules, between which are blood vessels and scanty amount of interstitial tissue. The types of uriniferous tubules are: 1. Secretory tubules (nephron): its function is the formation of urine. 2. Excertory tubules: Which are ducts that collect urine and carry it to the pelvis. which include the colleting ducts and papillary ducts. Nephrons Each nephron consist of: 1. Renal corpuscle (Malpighian corpuscle). 2. Proximal convoluted tubule. 3. Loop of Henle. 4. Distal convoluted tubule.
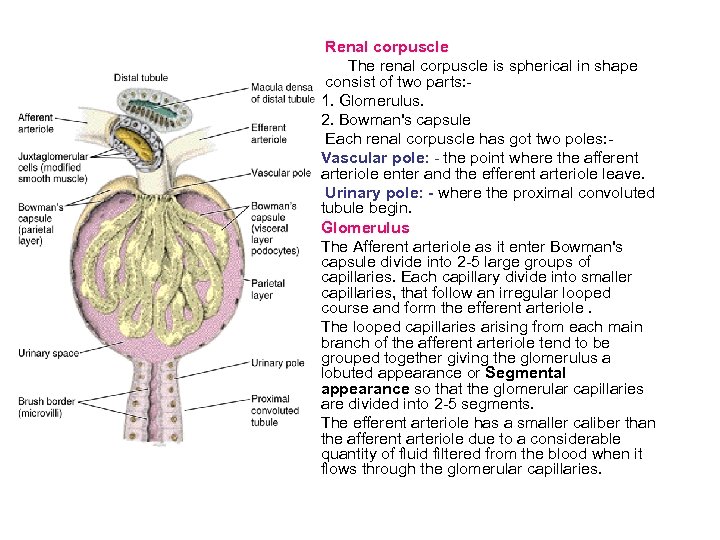 Renal corpuscle The renal corpuscle is spherical in shape consist of two parts: 1. Glomerulus. 2. Bowman's capsule Each renal corpuscle has got two poles: Vascular pole: - the point where the afferent arteriole enter and the efferent arteriole leave. Urinary pole: - where the proximal convoluted tubule begin. Glomerulus The Afferent arteriole as it enter Bowman's capsule divide into 2 -5 large groups of capillaries. Each capillary divide into smaller capillaries, that follow an irregular looped course and form the efferent arteriole. The looped capillaries arising from each main branch of the afferent arteriole tend to be grouped together giving the glomerulus a lobuted appearance or Segmental appearance so that the glomerular capillaries are divided into 2 -5 segments. The efferent arteriole has a smaller caliber than the afferent arteriole due to a considerable quantity of fluid filtered from the blood when it flows through the glomerular capillaries.
Renal corpuscle The renal corpuscle is spherical in shape consist of two parts: 1. Glomerulus. 2. Bowman's capsule Each renal corpuscle has got two poles: Vascular pole: - the point where the afferent arteriole enter and the efferent arteriole leave. Urinary pole: - where the proximal convoluted tubule begin. Glomerulus The Afferent arteriole as it enter Bowman's capsule divide into 2 -5 large groups of capillaries. Each capillary divide into smaller capillaries, that follow an irregular looped course and form the efferent arteriole. The looped capillaries arising from each main branch of the afferent arteriole tend to be grouped together giving the glomerulus a lobuted appearance or Segmental appearance so that the glomerular capillaries are divided into 2 -5 segments. The efferent arteriole has a smaller caliber than the afferent arteriole due to a considerable quantity of fluid filtered from the blood when it flows through the glomerular capillaries.
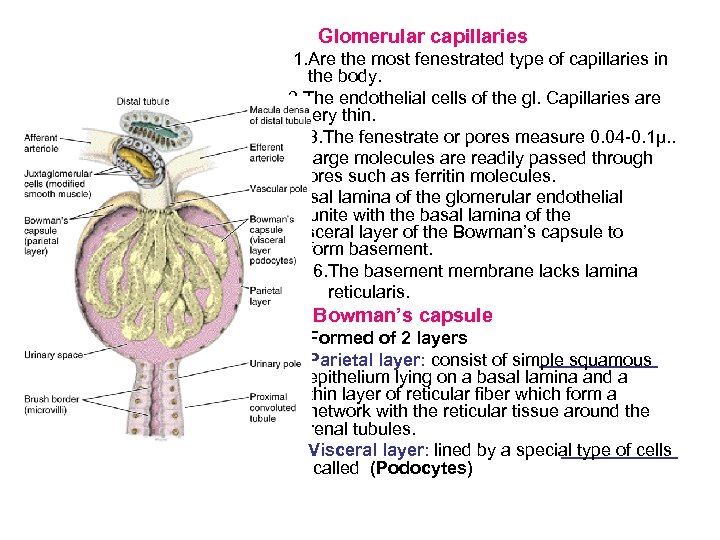 Glomerular capillaries 1. Are the most fenestrated type of capillaries in the body. 2. The endothelial cells of the gl. Capillaries are very thin. 3. The fenestrate or pores measure 0. 04 -0. 1μ. . 4. Large molecules are readily passed through the pores such as ferritin molecules. 5. Basal lamina of the glomerular endothelial cells unite with the basal lamina of the visceral layer of the Bowman’s capsule to form basement. 6. The basement membrane lacks lamina reticularis. Bowman’s capsule Formed of 2 layers Parietal layer: consist of simple squamous epithelium lying on a basal lamina and a thin layer of reticular fiber which form a network with the reticular tissue around the renal tubules. Visceral layer: lined by a special type of cells called (Podocytes)
Glomerular capillaries 1. Are the most fenestrated type of capillaries in the body. 2. The endothelial cells of the gl. Capillaries are very thin. 3. The fenestrate or pores measure 0. 04 -0. 1μ. . 4. Large molecules are readily passed through the pores such as ferritin molecules. 5. Basal lamina of the glomerular endothelial cells unite with the basal lamina of the visceral layer of the Bowman’s capsule to form basement. 6. The basement membrane lacks lamina reticularis. Bowman’s capsule Formed of 2 layers Parietal layer: consist of simple squamous epithelium lying on a basal lamina and a thin layer of reticular fiber which form a network with the reticular tissue around the renal tubules. Visceral layer: lined by a special type of cells called (Podocytes)
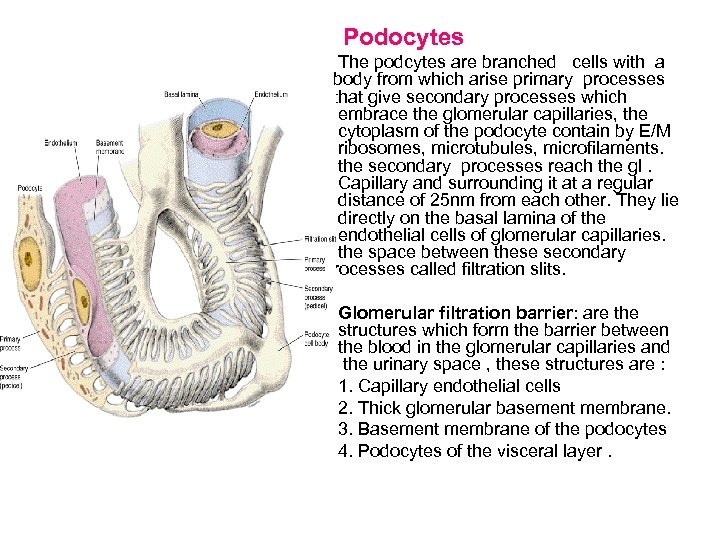 Podocytes The podcytes are branched cells with a body from which arise primary processes that give secondary processes which embrace the glomerular capillaries, the cytoplasm of the podocyte contain by E/M ribosomes, microtubules, microfilaments. the secondary processes reach the gl. Capillary and surrounding it at a regular distance of 25 nm from each other. They lie directly on the basal lamina of the endothelial cells of glomerular capillaries. the space between these secondary processes called filtration slits. Glomerular filtration barrier: are the structures which form the barrier between the blood in the glomerular capillaries and the urinary space , these structures are : 1. Capillary endothelial cells 2. Thick glomerular basement membrane. 3. Basement membrane of the podocytes 4. Podocytes of the visceral layer.
Podocytes The podcytes are branched cells with a body from which arise primary processes that give secondary processes which embrace the glomerular capillaries, the cytoplasm of the podocyte contain by E/M ribosomes, microtubules, microfilaments. the secondary processes reach the gl. Capillary and surrounding it at a regular distance of 25 nm from each other. They lie directly on the basal lamina of the endothelial cells of glomerular capillaries. the space between these secondary processes called filtration slits. Glomerular filtration barrier: are the structures which form the barrier between the blood in the glomerular capillaries and the urinary space , these structures are : 1. Capillary endothelial cells 2. Thick glomerular basement membrane. 3. Basement membrane of the podocytes 4. Podocytes of the visceral layer.
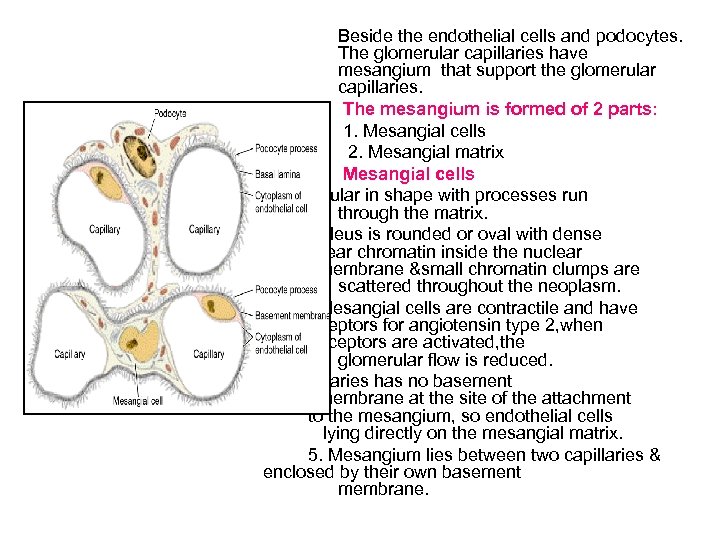 Beside the endothelial cells and podocytes. The glomerular capillaries have mesangium that support the glomerular capillaries. The mesangium is formed of 2 parts: 1. Mesangial cells 2. Mesangial matrix Mesangial cells 1. Irregular in shape with processes run through the matrix. 2. Nucleus is rounded or oval with dense nuclear chromatin inside the nuclear membrane &small chromatin clumps are scattered throughout the neoplasm. 3. Mesangial cells are contractile and have receptors for angiotensin type 2, when these receptors are activated, the glomerular flow is reduced. 4. The capillaries has no basement membrane at the site of the attachment to the mesangium, so endothelial cells lying directly on the mesangial matrix. 5. Mesangium lies between two capillaries & enclosed by their own basement membrane.
Beside the endothelial cells and podocytes. The glomerular capillaries have mesangium that support the glomerular capillaries. The mesangium is formed of 2 parts: 1. Mesangial cells 2. Mesangial matrix Mesangial cells 1. Irregular in shape with processes run through the matrix. 2. Nucleus is rounded or oval with dense nuclear chromatin inside the nuclear membrane &small chromatin clumps are scattered throughout the neoplasm. 3. Mesangial cells are contractile and have receptors for angiotensin type 2, when these receptors are activated, the glomerular flow is reduced. 4. The capillaries has no basement membrane at the site of the attachment to the mesangium, so endothelial cells lying directly on the mesangial matrix. 5. Mesangium lies between two capillaries & enclosed by their own basement membrane.
 Functions of the mesangium: 1. They give structural support of the glomerulus 2. Control blood flow through the glomerular loop. Phagocytosis, they are thought to remove any macromolecules that escape from capillaries to the tissue space. ntenance of the glomerular basement membrane 5. Synthesize extracellular matrix.
Functions of the mesangium: 1. They give structural support of the glomerulus 2. Control blood flow through the glomerular loop. Phagocytosis, they are thought to remove any macromolecules that escape from capillaries to the tissue space. ntenance of the glomerular basement membrane 5. Synthesize extracellular matrix.
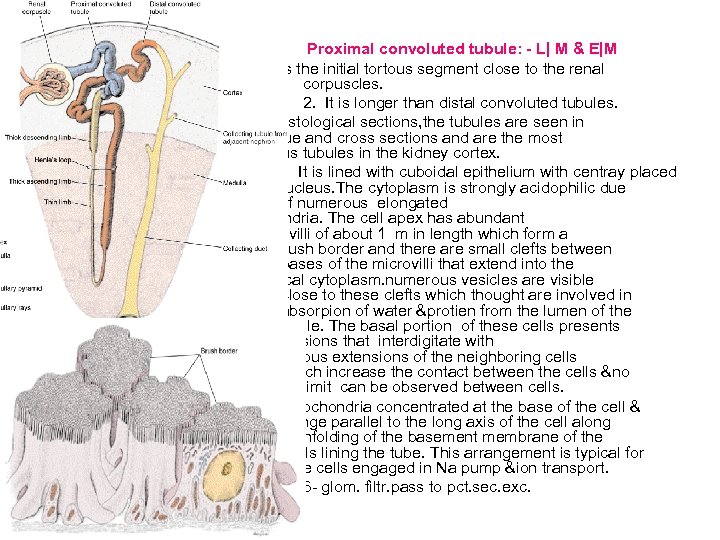 Proximal convoluted tubule: - L| M & E|M 1. It is the initial tortous segment close to the renal corpuscles. 2. It is longer than distal convoluted tubules. 3. In histological sections, the tubules are seen in oblique and cross sections and are the most numerous tubules in the kidney cortex. 4. It is lined with cuboidal epithelium with centray placed nucleus. The cytoplasm is strongly acidophilic due to presence of numerous elongated mitochondria. The cell apex has abundant microvilli of about 1 m in length which form a Brush border and there are small clefts between the bases of the microvilli that extend into the apical cytoplasm. numerous vesicles are visible close to these clefts which thought are involved in absorpion of water &protien from the lumen of the tubule. The basal portion of these cells presents lateral extensions that interdigitate with analogous extensions of the neighboring cells which increase the contact between the cells &no limit can be observed between cells. 5. Mitochondria concentrated at the base of the cell & arrange parallel to the long axis of the cell along the enfolding of the basement membrane of the cells lining the tube. This arrangement is typical for the cells engaged in Na pump &ion transport. 6 - glom. filtr. pass to pct. sec. exc.
Proximal convoluted tubule: - L| M & E|M 1. It is the initial tortous segment close to the renal corpuscles. 2. It is longer than distal convoluted tubules. 3. In histological sections, the tubules are seen in oblique and cross sections and are the most numerous tubules in the kidney cortex. 4. It is lined with cuboidal epithelium with centray placed nucleus. The cytoplasm is strongly acidophilic due to presence of numerous elongated mitochondria. The cell apex has abundant microvilli of about 1 m in length which form a Brush border and there are small clefts between the bases of the microvilli that extend into the apical cytoplasm. numerous vesicles are visible close to these clefts which thought are involved in absorpion of water &protien from the lumen of the tubule. The basal portion of these cells presents lateral extensions that interdigitate with analogous extensions of the neighboring cells which increase the contact between the cells &no limit can be observed between cells. 5. Mitochondria concentrated at the base of the cell & arrange parallel to the long axis of the cell along the enfolding of the basement membrane of the cells lining the tube. This arrangement is typical for the cells engaged in Na pump &ion transport. 6 - glom. filtr. pass to pct. sec. exc.
 Functions of proximal convoluted tubule Reabsorption of 85%of Na, Cl &water. Na is bsorbed by active process. Cl, & water reabsorbed by passive process. . Reabsorption of glucose. When the amount of glucose exceeds the absorbing capacity of the proximal tubule it appears in urine as in case of diabetes. 3. Reabsorption of protein & amino acid. 4. Excretion of foreign substances.
Functions of proximal convoluted tubule Reabsorption of 85%of Na, Cl &water. Na is bsorbed by active process. Cl, & water reabsorbed by passive process. . Reabsorption of glucose. When the amount of glucose exceeds the absorbing capacity of the proximal tubule it appears in urine as in case of diabetes. 3. Reabsorption of protein & amino acid. 4. Excretion of foreign substances.
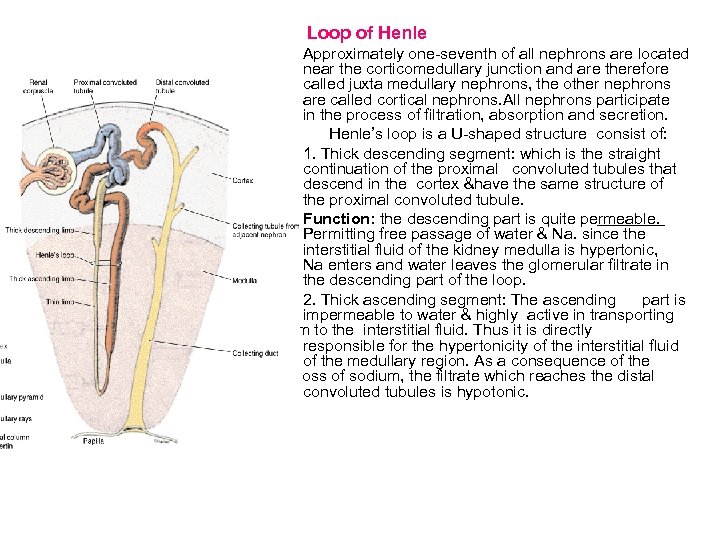 Loop of Henle Approximately one-seventh of all nephrons are located near the corticomedullary junction and are therefore called juxta medullary nephrons, the other nephrons are called cortical nephrons. All nephrons participate in the process of filtration, absorption and secretion. Henle’s loop is a U-shaped structure consist of: 1. Thick descending segment: which is the straight continuation of the proximal convoluted tubules that descend in the cortex &have the same structure of the proximal convoluted tubule. Function: the descending part is quite permeable. Permitting free passage of water & Na. since the interstitial fluid of the kidney medulla is hypertonic, Na enters and water leaves the glomerular filtrate in the descending part of the loop. 2. Thick ascending segment: The ascending part is impermeable to water & highly active in transporting sodium to the interstitial fluid. Thus it is directly responsible for the hypertonicity of the interstitial fluid of the medullary region. As a consequence of the loss of sodium, the filtrate which reaches the distal convoluted tubules is hypotonic.
Loop of Henle Approximately one-seventh of all nephrons are located near the corticomedullary junction and are therefore called juxta medullary nephrons, the other nephrons are called cortical nephrons. All nephrons participate in the process of filtration, absorption and secretion. Henle’s loop is a U-shaped structure consist of: 1. Thick descending segment: which is the straight continuation of the proximal convoluted tubules that descend in the cortex &have the same structure of the proximal convoluted tubule. Function: the descending part is quite permeable. Permitting free passage of water & Na. since the interstitial fluid of the kidney medulla is hypertonic, Na enters and water leaves the glomerular filtrate in the descending part of the loop. 2. Thick ascending segment: The ascending part is impermeable to water & highly active in transporting sodium to the interstitial fluid. Thus it is directly responsible for the hypertonicity of the interstitial fluid of the medullary region. As a consequence of the loss of sodium, the filtrate which reaches the distal convoluted tubules is hypotonic.
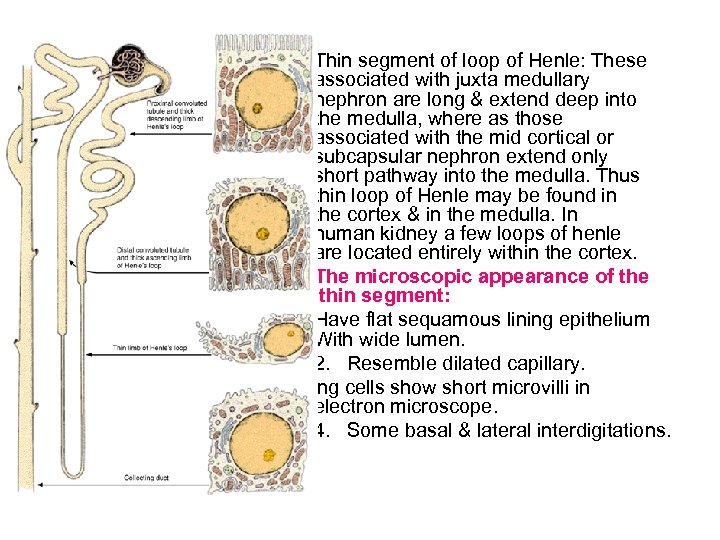 Thin segment of loop of Henle: These associated with juxta medullary nephron are long & extend deep into the medulla, where as those associated with the mid cortical or subcapsular nephron extend only short pathway into the medulla. Thus thin loop of Henle may be found in the cortex & in the medulla. In human kidney a few loops of henle are located entirely within the cortex. The microscopic appearance of the thin segment: 1. Have flat sequamous lining epithelium With wide lumen. 2. Resemble dilated capillary. 3. Lining cells show short microvilli in electron microscope. 4. Some basal & lateral interdigitations.
Thin segment of loop of Henle: These associated with juxta medullary nephron are long & extend deep into the medulla, where as those associated with the mid cortical or subcapsular nephron extend only short pathway into the medulla. Thus thin loop of Henle may be found in the cortex & in the medulla. In human kidney a few loops of henle are located entirely within the cortex. The microscopic appearance of the thin segment: 1. Have flat sequamous lining epithelium With wide lumen. 2. Resemble dilated capillary. 3. Lining cells show short microvilli in electron microscope. 4. Some basal & lateral interdigitations.
 Distal convoluted tubule: When the thick part of loop of Henle penetrate the cortex, it preserves its histological structure but become tortous & then called distal convoluted tubules which is the last segment of the nephron. The distal convoluted tubule found in the cortex. The distal convoluted tubules become contact with the vascular pole of the renal corpuscle of its parent nephron. The histology of the distal convoluted tubule: L|M &E|M. 1. It is lined by smaller cuboidal cells than proximal convoluted tubule 2. Number of lining cells of the distal convoluted tubules is more than that of the proximal convoluted tubules. 3. Cells are less acidophilic than the proximal convoluted tubules due to decreased number of mitochondria. 4. Lumen is wider than the proximal tubules. 5. They have no brush border. no apical clefts. 6. Mitochondria are present but less than that of proximal convoluted tubules, therefore the cells stains lighter than the cells of proximal convoluted tubules. 7. Extensive Basel & lateral extensions.
Distal convoluted tubule: When the thick part of loop of Henle penetrate the cortex, it preserves its histological structure but become tortous & then called distal convoluted tubules which is the last segment of the nephron. The distal convoluted tubule found in the cortex. The distal convoluted tubules become contact with the vascular pole of the renal corpuscle of its parent nephron. The histology of the distal convoluted tubule: L|M &E|M. 1. It is lined by smaller cuboidal cells than proximal convoluted tubule 2. Number of lining cells of the distal convoluted tubules is more than that of the proximal convoluted tubules. 3. Cells are less acidophilic than the proximal convoluted tubules due to decreased number of mitochondria. 4. Lumen is wider than the proximal tubules. 5. They have no brush border. no apical clefts. 6. Mitochondria are present but less than that of proximal convoluted tubules, therefore the cells stains lighter than the cells of proximal convoluted tubules. 7. Extensive Basel & lateral extensions.
 Functions: 1. Maintain acid - base balance. 2. Important in urine concentration. Reabsorption of Na ions from the lumen of the distal convoluted tubules to the blood while K is excreted in the urine. 4. Bicarbonate ions are reabsorbed back to the blood & hydrogen ions are excreted so the urine is acidic. function is under the effect of aldosterone secreted by the adrenal cortex. H (antidiuretic hormone) secreted by the posterior lobe of ary gland acts on the last part of the distal convoluted es & increases the permeability of the tubule to water dering the urine more concentrated. ADH also act on the collecting duct in a similar way.
Functions: 1. Maintain acid - base balance. 2. Important in urine concentration. Reabsorption of Na ions from the lumen of the distal convoluted tubules to the blood while K is excreted in the urine. 4. Bicarbonate ions are reabsorbed back to the blood & hydrogen ions are excreted so the urine is acidic. function is under the effect of aldosterone secreted by the adrenal cortex. H (antidiuretic hormone) secreted by the posterior lobe of ary gland acts on the last part of the distal convoluted es & increases the permeability of the tubule to water dering the urine more concentrated. ADH also act on the collecting duct in a similar way.
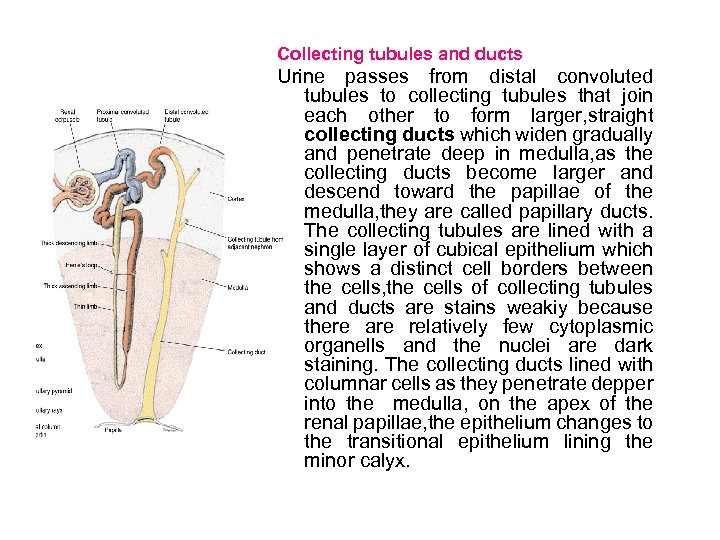 Collecting tubules and ducts Urine passes from distal convoluted tubules to collecting tubules that join each other to form larger, straight collecting ducts which widen gradually and penetrate deep in medulla, as the collecting ducts become larger and descend toward the papillae of the medulla, they are called papillary ducts. The collecting tubules are lined with a single layer of cubical epithelium which shows a distinct cell borders between the cells, the cells of collecting tubules and ducts are stains weakiy because there are relatively few cytoplasmic organells and the nuclei are dark staining. The collecting ducts lined with columnar cells as they penetrate depper into the medulla, on the apex of the renal papillae, the epithelium changes to the transitional epithelium lining the minor calyx.
Collecting tubules and ducts Urine passes from distal convoluted tubules to collecting tubules that join each other to form larger, straight collecting ducts which widen gradually and penetrate deep in medulla, as the collecting ducts become larger and descend toward the papillae of the medulla, they are called papillary ducts. The collecting tubules are lined with a single layer of cubical epithelium which shows a distinct cell borders between the cells, the cells of collecting tubules and ducts are stains weakiy because there are relatively few cytoplasmic organells and the nuclei are dark staining. The collecting ducts lined with columnar cells as they penetrate depper into the medulla, on the apex of the renal papillae, the epithelium changes to the transitional epithelium lining the minor calyx.
 Renal Interstitium The space between uriniferous tubules and blood and lymph vessels is called the renal interstitium. It occupies avery small volume in the cortex but increase in the medulla. The renal interstitium contains asmall amount of connective tissue with fibroblasts, some collagen fibers, and, mainly in the medulla , a highly hydrated ground subustance rich in proteoglycan. In the medulla the secreting cells called interstitial cells are found, they contain cytoplasmic lipid droplets and are implicated in the synthesis of prostaglandins and prostacyclin. The renal interstitium also responsible for salt and water homeostasis.
Renal Interstitium The space between uriniferous tubules and blood and lymph vessels is called the renal interstitium. It occupies avery small volume in the cortex but increase in the medulla. The renal interstitium contains asmall amount of connective tissue with fibroblasts, some collagen fibers, and, mainly in the medulla , a highly hydrated ground subustance rich in proteoglycan. In the medulla the secreting cells called interstitial cells are found, they contain cytoplasmic lipid droplets and are implicated in the synthesis of prostaglandins and prostacyclin. The renal interstitium also responsible for salt and water homeostasis.
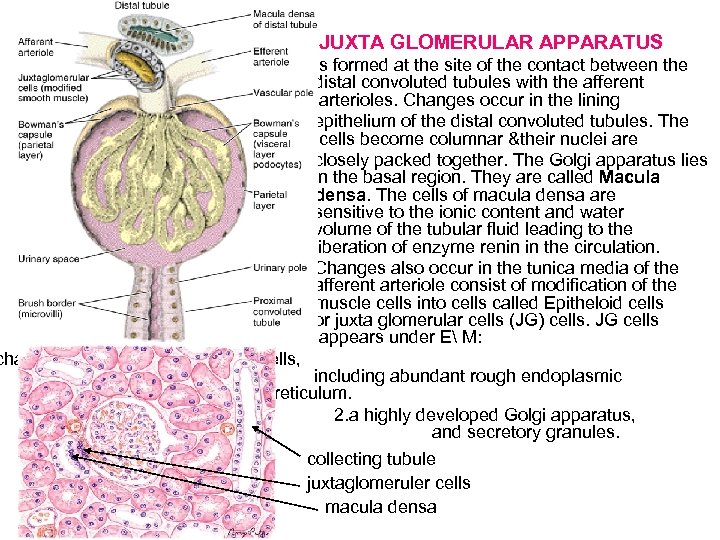 JUXTA GLOMERULAR APPARATUS Is formed at the site of the contact between the distal convoluted tubules with the afferent arterioles. Changes occur in the lining epithelium of the distal convoluted tubules. The cells become columnar &their nuclei are closely packed together. The Golgi apparatus lies in the basal region. They are called Macula densa. The cells of macula densa are sensitive to the ionic content and water volume of the tubular fluid leading to the liberation of enzyme renin in the circulation. Changes also occur in the tunica media of the afferent arteriole consist of modification of the muscle cells into cells called Epitheloid cells or juxta glomerular cells (JG) cells. JG cells appears under E M: characterstics of protein-secretin cells, including abundant rough endoplasmic reticulum. 2. a highly developed Golgi apparatus, and secretory granules. collecting tubule juxtaglomeruler cells macula densa
JUXTA GLOMERULAR APPARATUS Is formed at the site of the contact between the distal convoluted tubules with the afferent arterioles. Changes occur in the lining epithelium of the distal convoluted tubules. The cells become columnar &their nuclei are closely packed together. The Golgi apparatus lies in the basal region. They are called Macula densa. The cells of macula densa are sensitive to the ionic content and water volume of the tubular fluid leading to the liberation of enzyme renin in the circulation. Changes also occur in the tunica media of the afferent arteriole consist of modification of the muscle cells into cells called Epitheloid cells or juxta glomerular cells (JG) cells. JG cells appears under E M: characterstics of protein-secretin cells, including abundant rough endoplasmic reticulum. 2. a highly developed Golgi apparatus, and secretory granules. collecting tubule juxtaglomeruler cells macula densa
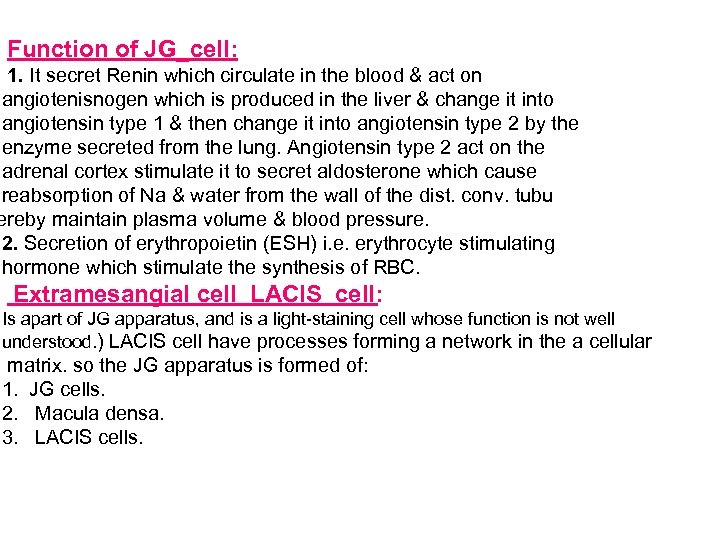 Function of JG_cell: 1. It secret Renin which circulate in the blood & act on angiotenisnogen which is produced in the liver & change it into angiotensin type 1 & then change it into angiotensin type 2 by the enzyme secreted from the lung. Angiotensin type 2 act on the adrenal cortex stimulate it to secret aldosterone which cause reabsorption of Na & water from the wall of the dist. conv. tubu ereby maintain plasma volume & blood pressure. 2. Secretion of erythropoietin (ESH) i. e. erythrocyte stimulating hormone which stimulate the synthesis of RBC. Extramesangial cell LACIS cell: Is apart of JG apparatus, and is a light-staining cell whose function is not well understood. ) LACIS cell have processes forming a network in the a cellular matrix. so the JG apparatus is formed of: 1. JG cells. 2. Macula densa. 3. LACIS cells.
Function of JG_cell: 1. It secret Renin which circulate in the blood & act on angiotenisnogen which is produced in the liver & change it into angiotensin type 1 & then change it into angiotensin type 2 by the enzyme secreted from the lung. Angiotensin type 2 act on the adrenal cortex stimulate it to secret aldosterone which cause reabsorption of Na & water from the wall of the dist. conv. tubu ereby maintain plasma volume & blood pressure. 2. Secretion of erythropoietin (ESH) i. e. erythrocyte stimulating hormone which stimulate the synthesis of RBC. Extramesangial cell LACIS cell: Is apart of JG apparatus, and is a light-staining cell whose function is not well understood. ) LACIS cell have processes forming a network in the a cellular matrix. so the JG apparatus is formed of: 1. JG cells. 2. Macula densa. 3. LACIS cells.
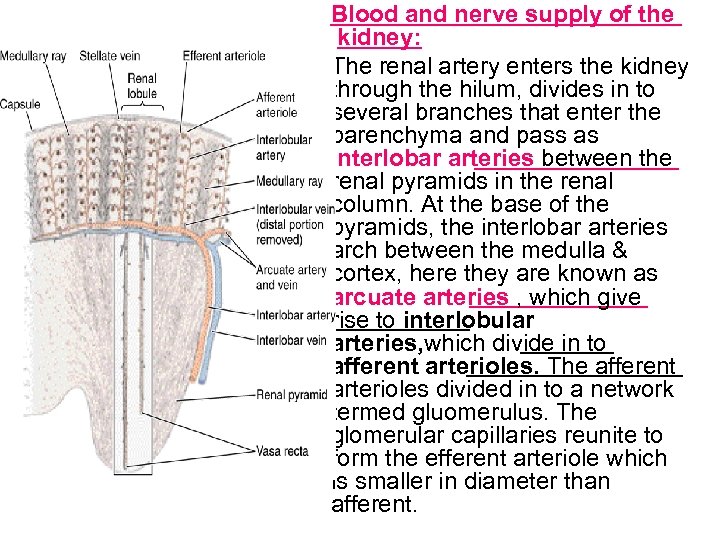 Blood and nerve supply of the kidney: The renal artery enters the kidney through the hilum, divides in to several branches that enter the parenchyma and pass as interlobar arteries between the renal pyramids in the renal column. At the base of the pyramids, the interlobar arteries arch between the medulla & cortex, here they are known as arcuate arteries , which give rise to interlobular arteries, which divide in to afferent arterioles. The afferent arterioles divided in to a network termed gluomerulus. The glomerular capillaries reunite to form the efferent arteriole which is smaller in diameter than afferent.
Blood and nerve supply of the kidney: The renal artery enters the kidney through the hilum, divides in to several branches that enter the parenchyma and pass as interlobar arteries between the renal pyramids in the renal column. At the base of the pyramids, the interlobar arteries arch between the medulla & cortex, here they are known as arcuate arteries , which give rise to interlobular arteries, which divide in to afferent arterioles. The afferent arterioles divided in to a network termed gluomerulus. The glomerular capillaries reunite to form the efferent arteriole which is smaller in diameter than afferent.
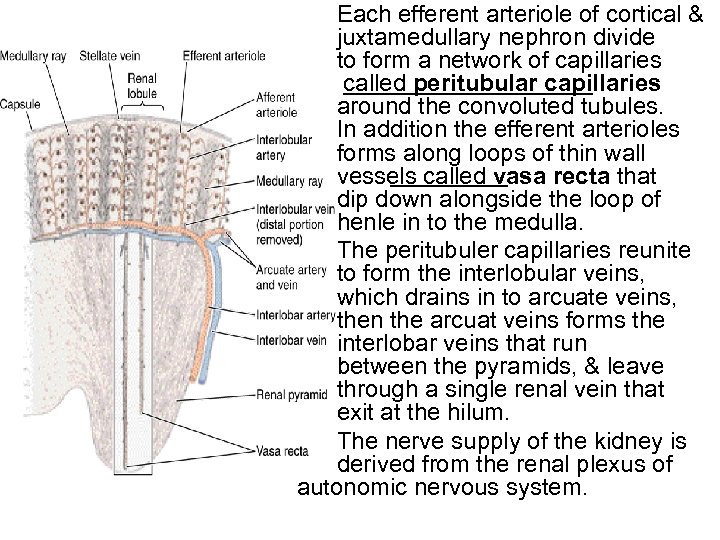 Each efferent arteriole of cortical & juxtamedullary nephron divide to form a network of capillaries called peritubular capillaries around the convoluted tubules. In addition the efferent arterioles forms along loops of thin wall vessels called vasa recta that dip down alongside the loop of henle in to the medulla. The peritubuler capillaries reunite to form the interlobular veins, which drains in to arcuate veins, then the arcuat veins forms the interlobar veins that run between the pyramids, & leave through a single renal vein that exit at the hilum. The nerve supply of the kidney is derived from the renal plexus of autonomic nervous system.
Each efferent arteriole of cortical & juxtamedullary nephron divide to form a network of capillaries called peritubular capillaries around the convoluted tubules. In addition the efferent arterioles forms along loops of thin wall vessels called vasa recta that dip down alongside the loop of henle in to the medulla. The peritubuler capillaries reunite to form the interlobular veins, which drains in to arcuate veins, then the arcuat veins forms the interlobar veins that run between the pyramids, & leave through a single renal vein that exit at the hilum. The nerve supply of the kidney is derived from the renal plexus of autonomic nervous system.
 The urinary system
The urinary system
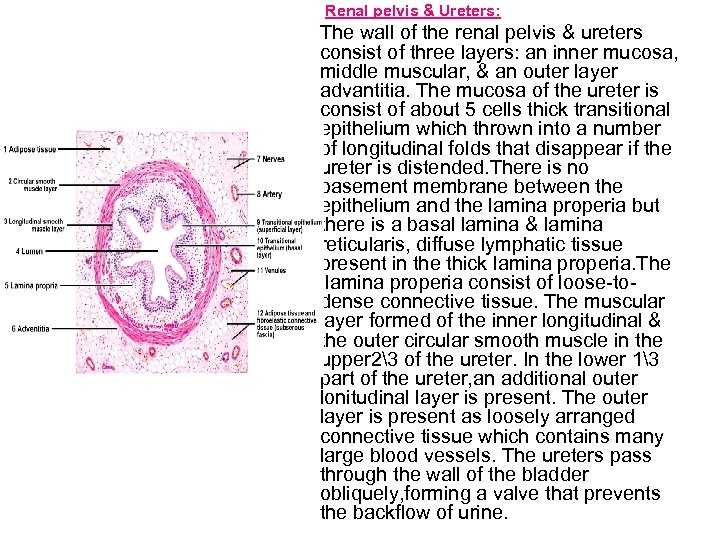 Renal pelvis & Ureters: The wall of the renal pelvis & ureters consist of three layers: an inner mucosa, middle muscular, & an outer layer advantitia. The mucosa of the ureter is consist of about 5 cells thick transitional epithelium which thrown into a number of longitudinal folds that disappear if the ureter is distended. There is no basement membrane between the epithelium and the lamina properia but there is a basal lamina & lamina reticularis, diffuse lymphatic tissue present in the thick lamina properia. The lamina properia consist of loose-todense connective tissue. The muscular layer formed of the inner longitudinal & the outer circular smooth muscle in the upper 23 of the ureter. In the lower 13 part of the ureter, an additional outer lonitudinal layer is present. The outer layer is present as loosely arranged connective tissue which contains many large blood vessels. The ureters pass through the wall of the bladder obliquely, forming a valve that prevents the backflow of urine.
Renal pelvis & Ureters: The wall of the renal pelvis & ureters consist of three layers: an inner mucosa, middle muscular, & an outer layer advantitia. The mucosa of the ureter is consist of about 5 cells thick transitional epithelium which thrown into a number of longitudinal folds that disappear if the ureter is distended. There is no basement membrane between the epithelium and the lamina properia but there is a basal lamina & lamina reticularis, diffuse lymphatic tissue present in the thick lamina properia. The lamina properia consist of loose-todense connective tissue. The muscular layer formed of the inner longitudinal & the outer circular smooth muscle in the upper 23 of the ureter. In the lower 13 part of the ureter, an additional outer lonitudinal layer is present. The outer layer is present as loosely arranged connective tissue which contains many large blood vessels. The ureters pass through the wall of the bladder obliquely, forming a valve that prevents the backflow of urine.
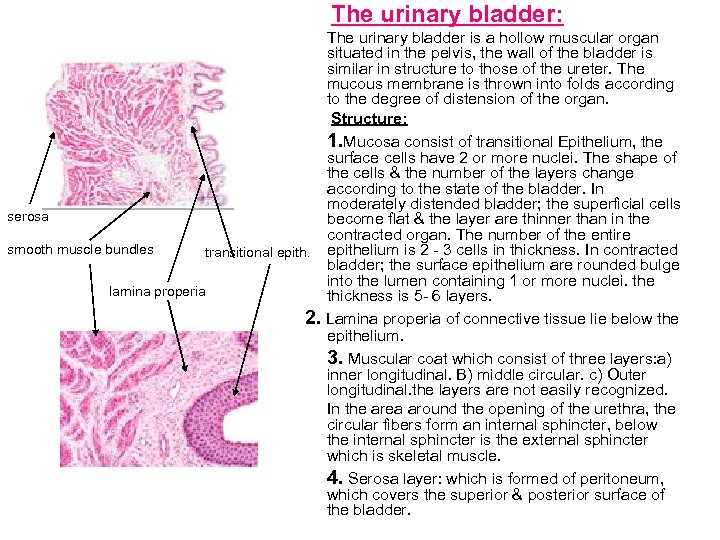 The urinary bladder: The urinary bladder is a hollow muscular organ situated in the pelvis, the wall of the bladder is similar in structure to those of the ureter. The mucous membrane is thrown into folds according to the degree of distension of the organ. Structure: 1. Mucosa consist of transitional Epithelium, the surface cells have 2 or more nuclei. The shape of the cells & the number of the layers change according to the state of the bladder. In moderately distended bladder; the superficial cells serosa become flat & the layer are thinner than in the contracted organ. The number of the entire smooth muscle bundles transitional epithelium is 2 - 3 cells in thickness. In contracted bladder; the surface epithelium are rounded bulge into the lumen containing 1 or more nuclei. the lamina properia thickness is 5 - 6 layers. 2. Lamina properia of connective tissue lie below the epithelium. 3. Muscular coat which consist of three layers: a) inner longitudinal. B) middle circular. c) Outer longitudinal. the layers are not easily recognized. In the area around the opening of the urethra, the circular fibers form an internal sphincter, below the internal sphincter is the external sphincter which is skeletal muscle. 4. Serosa layer: which is formed of peritoneum, which covers the superior & posterior surface of the bladder.
The urinary bladder: The urinary bladder is a hollow muscular organ situated in the pelvis, the wall of the bladder is similar in structure to those of the ureter. The mucous membrane is thrown into folds according to the degree of distension of the organ. Structure: 1. Mucosa consist of transitional Epithelium, the surface cells have 2 or more nuclei. The shape of the cells & the number of the layers change according to the state of the bladder. In moderately distended bladder; the superficial cells serosa become flat & the layer are thinner than in the contracted organ. The number of the entire smooth muscle bundles transitional epithelium is 2 - 3 cells in thickness. In contracted bladder; the surface epithelium are rounded bulge into the lumen containing 1 or more nuclei. the lamina properia thickness is 5 - 6 layers. 2. Lamina properia of connective tissue lie below the epithelium. 3. Muscular coat which consist of three layers: a) inner longitudinal. B) middle circular. c) Outer longitudinal. the layers are not easily recognized. In the area around the opening of the urethra, the circular fibers form an internal sphincter, below the internal sphincter is the external sphincter which is skeletal muscle. 4. Serosa layer: which is formed of peritoneum, which covers the superior & posterior surface of the bladder.
 Urethra: It is a tube which carries the urine from the bladder to the exterior. The male urethra is about 20 cm long & divided into three parts: 1. Prostatic part: 4 cm in length lined in its first part by the same epith. he bladder (transitional epith. ), however, in the part of the prostatic urethra nearest to the membranous urethra, the epith. change to pseudostratified columnar epith. anous part: 1 cm in length lined with stratified or pseudostratified columnar epith. penile part: 15 cm in length, lined by stratified columnar epith. or eudostratified columnar epith. The female urethra is a tube of 4 -5 cm, lined with stratified squamous epithelium with areas of pseudosratified columnar epithelium. The middle part of the female urethra is surrounded by external striated voluntary sphincter.
Urethra: It is a tube which carries the urine from the bladder to the exterior. The male urethra is about 20 cm long & divided into three parts: 1. Prostatic part: 4 cm in length lined in its first part by the same epith. he bladder (transitional epith. ), however, in the part of the prostatic urethra nearest to the membranous urethra, the epith. change to pseudostratified columnar epith. anous part: 1 cm in length lined with stratified or pseudostratified columnar epith. penile part: 15 cm in length, lined by stratified columnar epith. or eudostratified columnar epith. The female urethra is a tube of 4 -5 cm, lined with stratified squamous epithelium with areas of pseudosratified columnar epithelium. The middle part of the female urethra is surrounded by external striated voluntary sphincter.


