The Urinary System Chapter 18 9/9/10 Classroom ed.




9902-3__dmi_63_gu_system_classroom.ppt
- Количество слайдов: 70
 The Urinary System Chapter 18 9/9/10 Classroom ed.
The Urinary System Chapter 18 9/9/10 Classroom ed.
 Urinary System Often called the excretory system Two kidneys Two ureters One urinary bladder One urethra
Urinary System Often called the excretory system Two kidneys Two ureters One urinary bladder One urethra
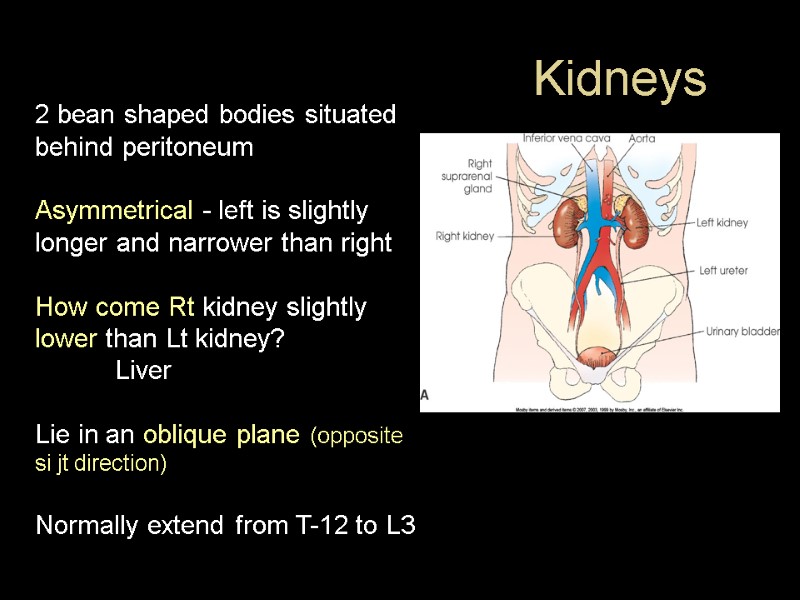
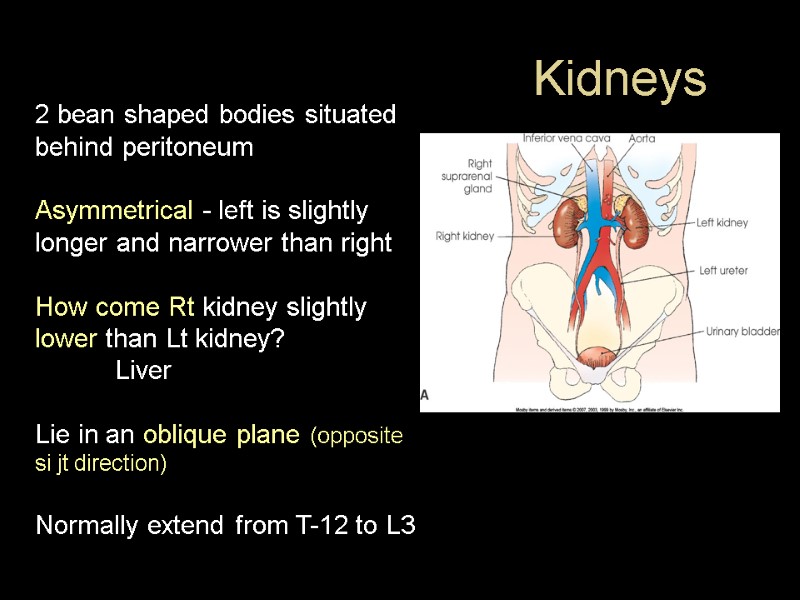 Kidneys 2 bean shaped bodies situated behind peritoneum Asymmetrical - left is slightly longer and narrower than right How come Rt kidney slightly lower than Lt kidney? Liver Lie in an oblique plane (opposite si jt direction) Normally extend from T-12 to L3
Kidneys 2 bean shaped bodies situated behind peritoneum Asymmetrical - left is slightly longer and narrower than right How come Rt kidney slightly lower than Lt kidney? Liver Lie in an oblique plane (opposite si jt direction) Normally extend from T-12 to L3
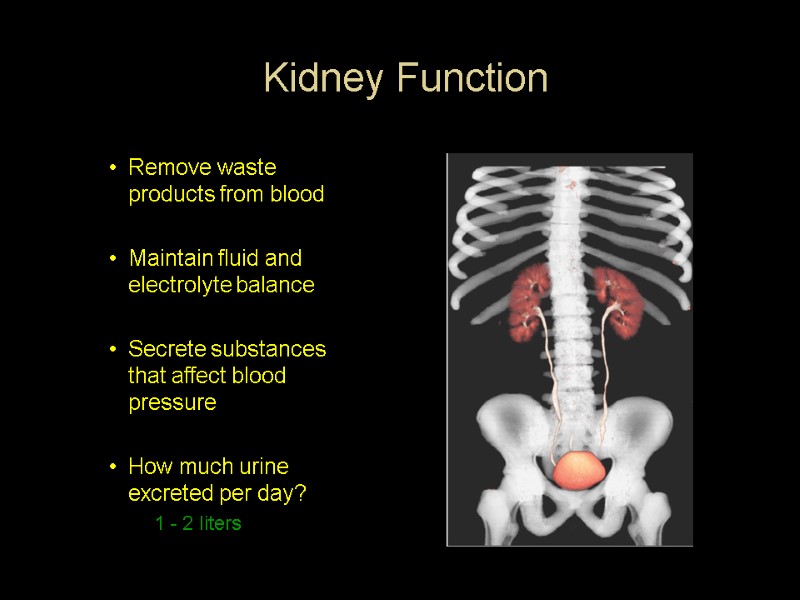
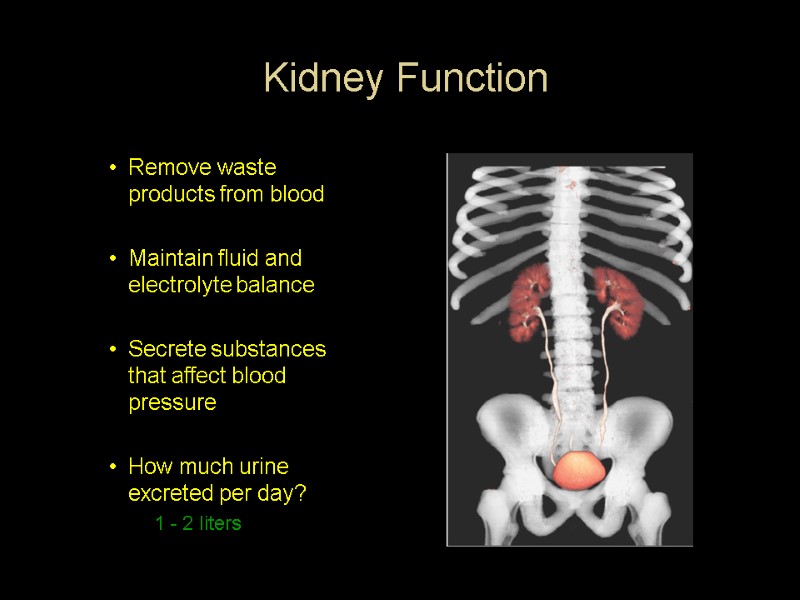 Kidney Function Remove waste products from blood Maintain fluid and electrolyte balance Secrete substances that affect blood pressure How much urine excreted per day? 1 - 2 liters
Kidney Function Remove waste products from blood Maintain fluid and electrolyte balance Secrete substances that affect blood pressure How much urine excreted per day? 1 - 2 liters
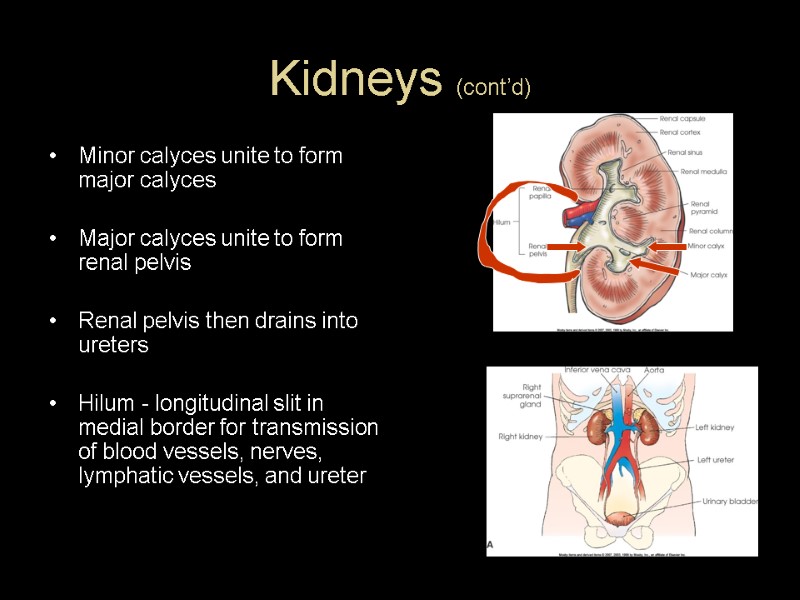
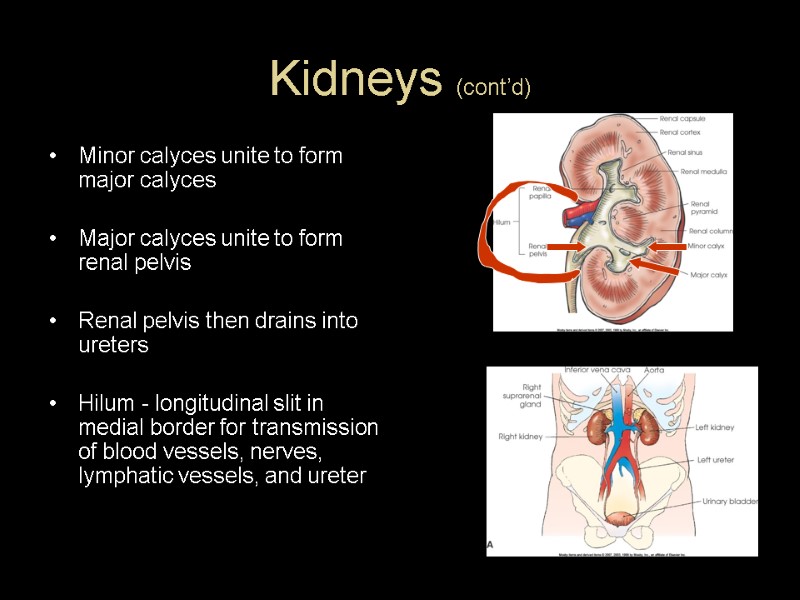 Kidneys (cont’d) Minor calyces unite to form major calyces Major calyces unite to form renal pelvis Renal pelvis then drains into ureters Hilum - longitudinal slit in medial border for transmission of blood vessels, nerves, lymphatic vessels, and ureter
Kidneys (cont’d) Minor calyces unite to form major calyces Major calyces unite to form renal pelvis Renal pelvis then drains into ureters Hilum - longitudinal slit in medial border for transmission of blood vessels, nerves, lymphatic vessels, and ureter
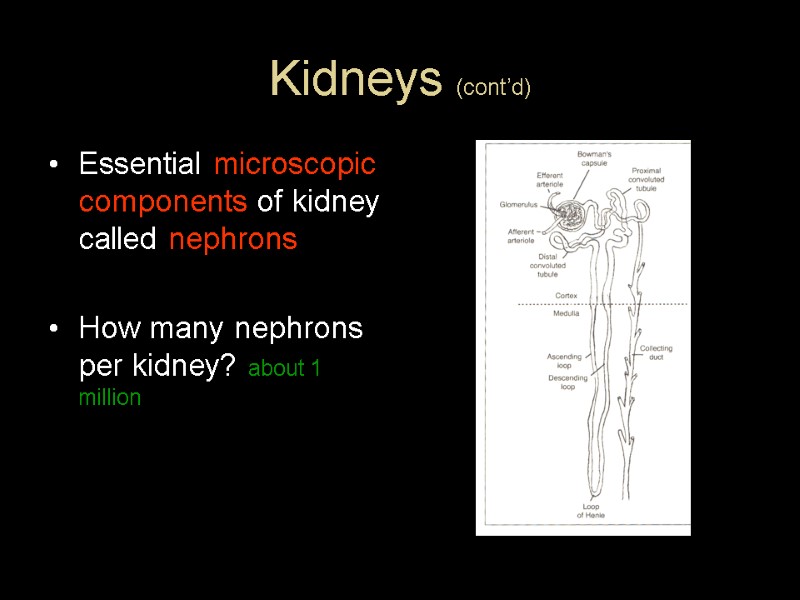
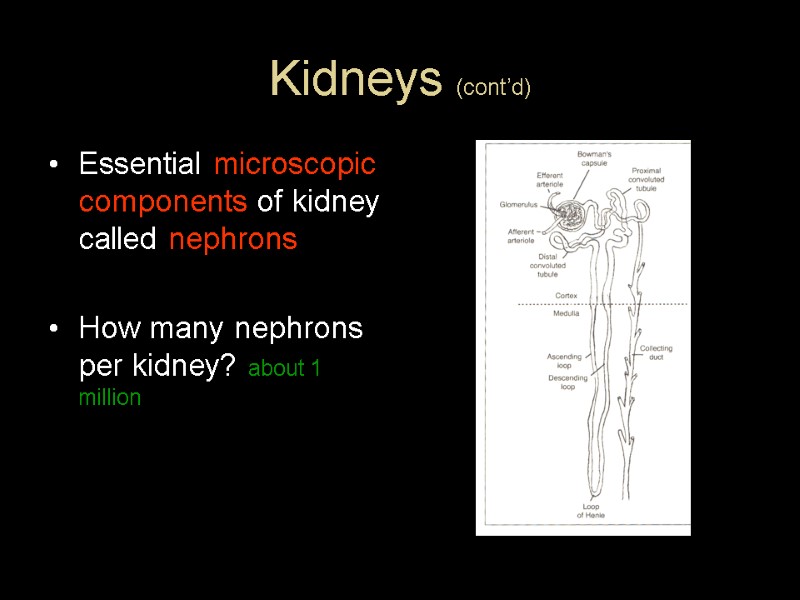 Kidneys (cont’d) Essential microscopic components of kidney called nephrons How many nephrons per kidney? about 1 million
Kidneys (cont’d) Essential microscopic components of kidney called nephrons How many nephrons per kidney? about 1 million
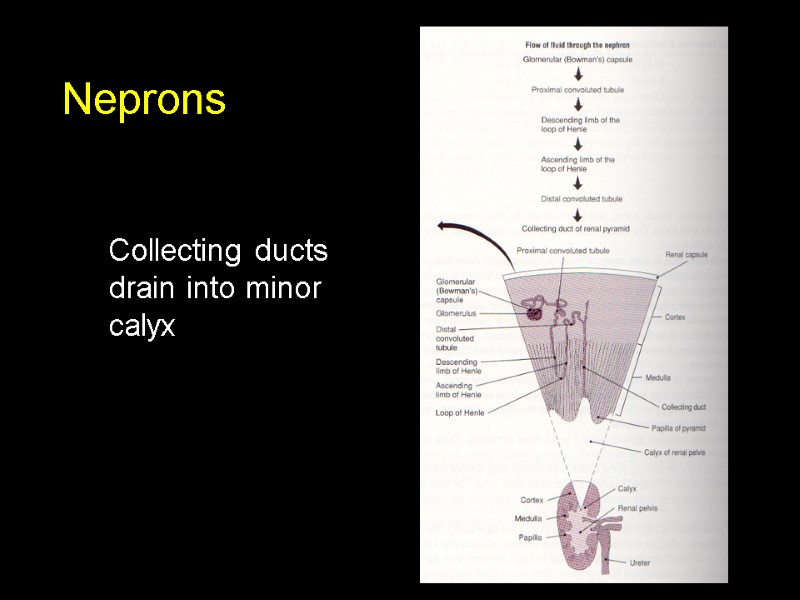
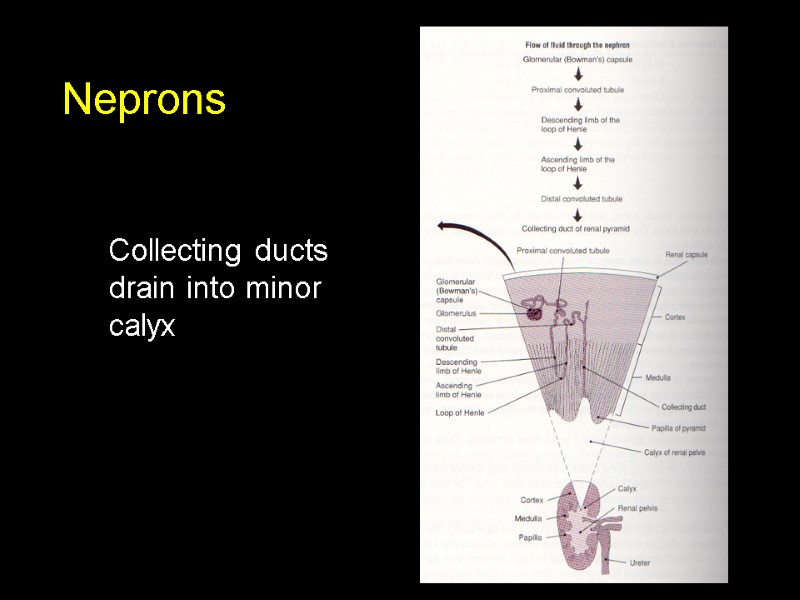 Neprons Collecting ducts drain into minor calyx
Neprons Collecting ducts drain into minor calyx
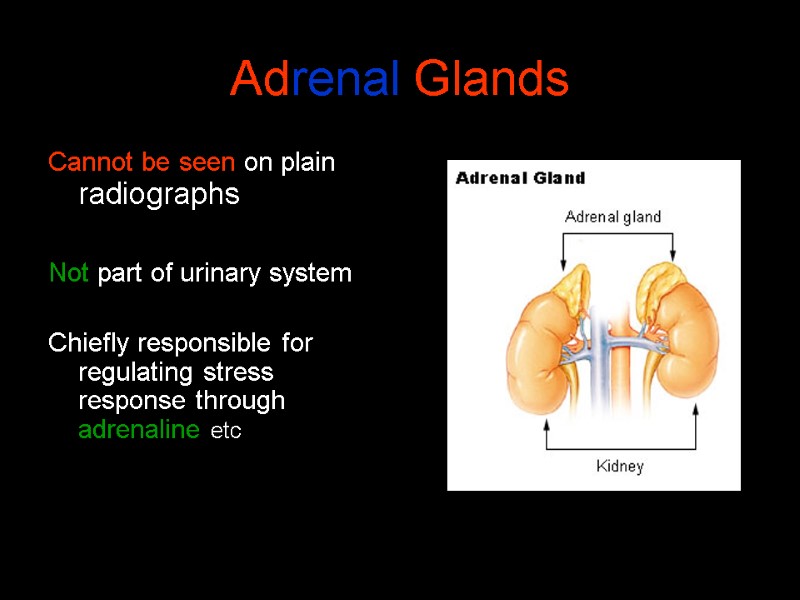
 Adrenal Glands Cannot be seen on plain radiographs Not part of urinary system Chiefly responsible for regulating stress response through adrenaline etc
Adrenal Glands Cannot be seen on plain radiographs Not part of urinary system Chiefly responsible for regulating stress response through adrenaline etc
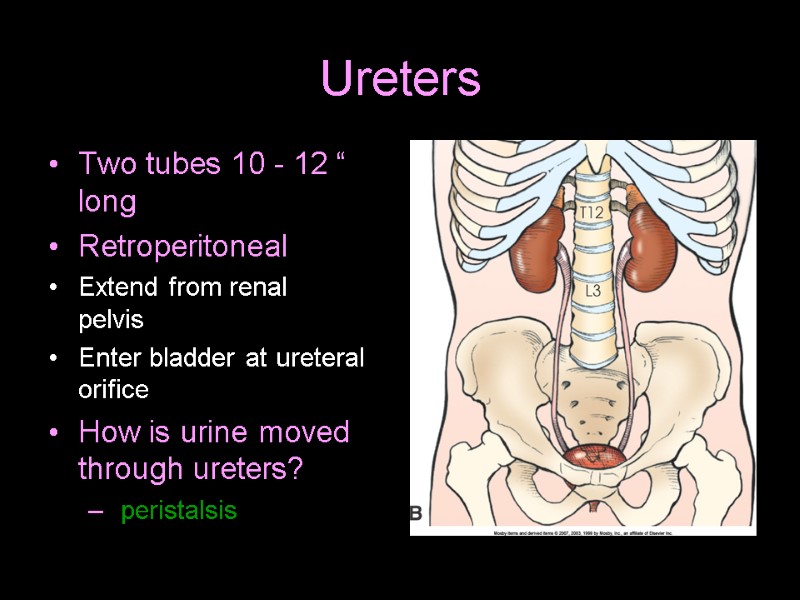
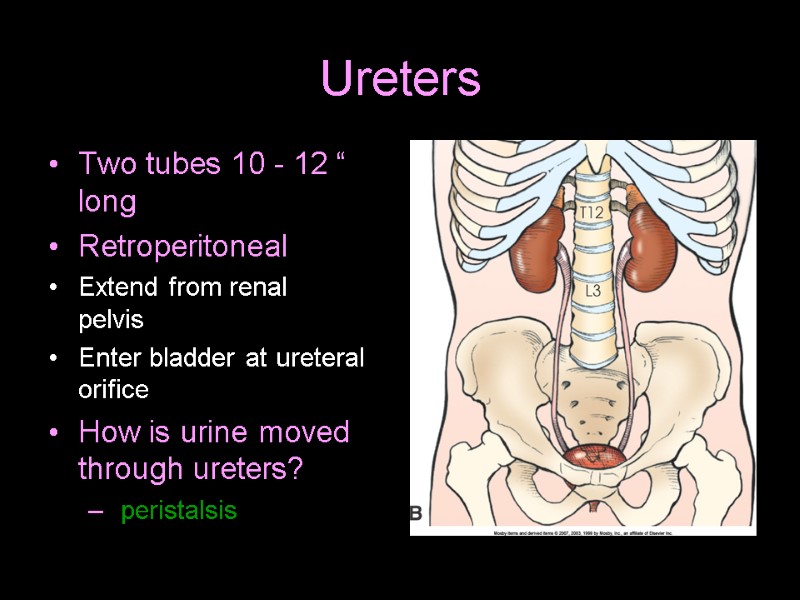 Ureters Two tubes 10 - 12 “ long Retroperitoneal Extend from renal pelvis Enter bladder at ureteral orifice How is urine moved through ureters? peristalsis
Ureters Two tubes 10 - 12 “ long Retroperitoneal Extend from renal pelvis Enter bladder at ureteral orifice How is urine moved through ureters? peristalsis
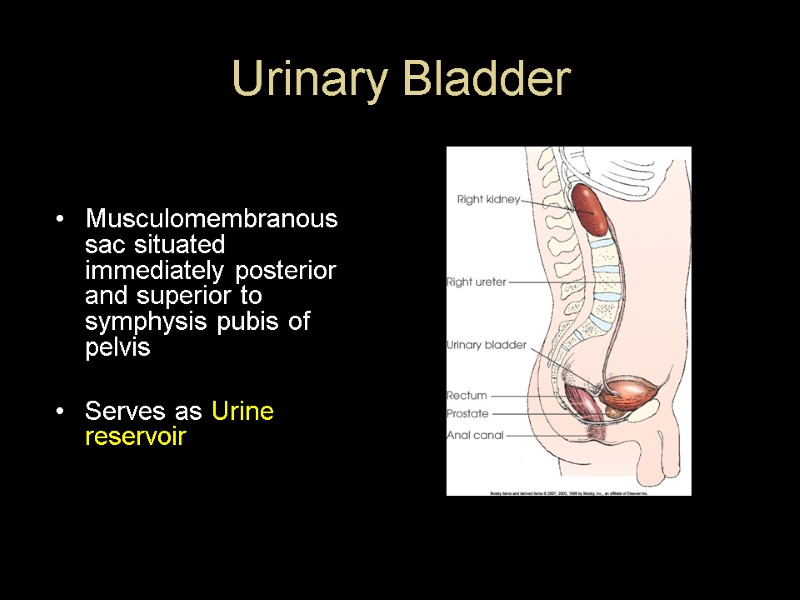
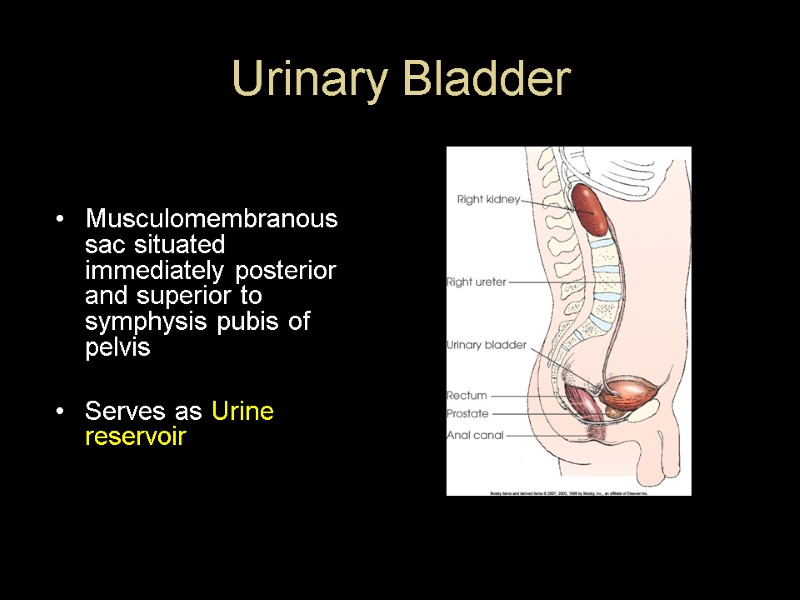 Urinary Bladder Musculomembranous sac situated immediately posterior and superior to symphysis pubis of pelvis Serves as Urine reservoir
Urinary Bladder Musculomembranous sac situated immediately posterior and superior to symphysis pubis of pelvis Serves as Urine reservoir
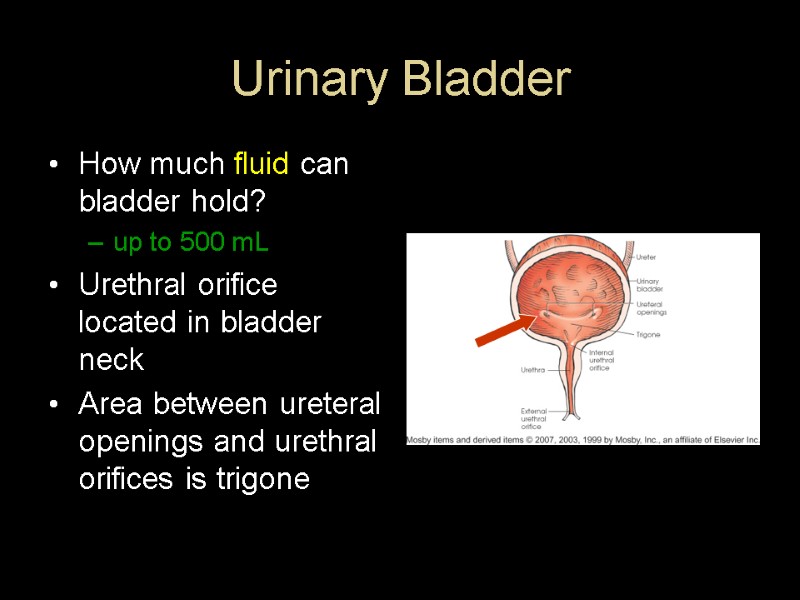
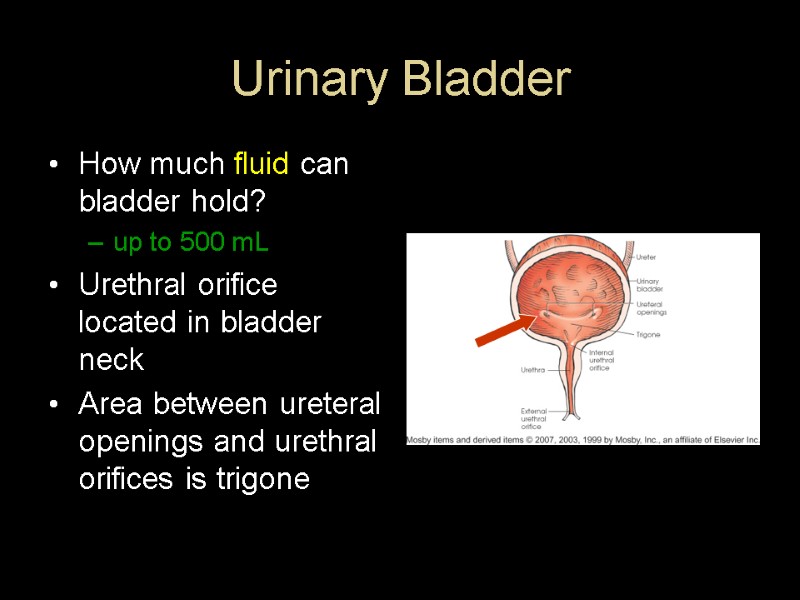 Urinary Bladder How much fluid can bladder hold? up to 500 mL Urethral orifice located in bladder neck Area between ureteral openings and urethral orifices is trigone
Urinary Bladder How much fluid can bladder hold? up to 500 mL Urethral orifice located in bladder neck Area between ureteral openings and urethral orifices is trigone
 Urethra Carries urine from bladder to? exterior of body How long is it in females? About 1.5 In males? About 7 to 8 Sphincter at neck of bladder controls flow Male urethra contains following parts: Prostate Membranous area Spongy area
Urethra Carries urine from bladder to? exterior of body How long is it in females? About 1.5 In males? About 7 to 8 Sphincter at neck of bladder controls flow Male urethra contains following parts: Prostate Membranous area Spongy area
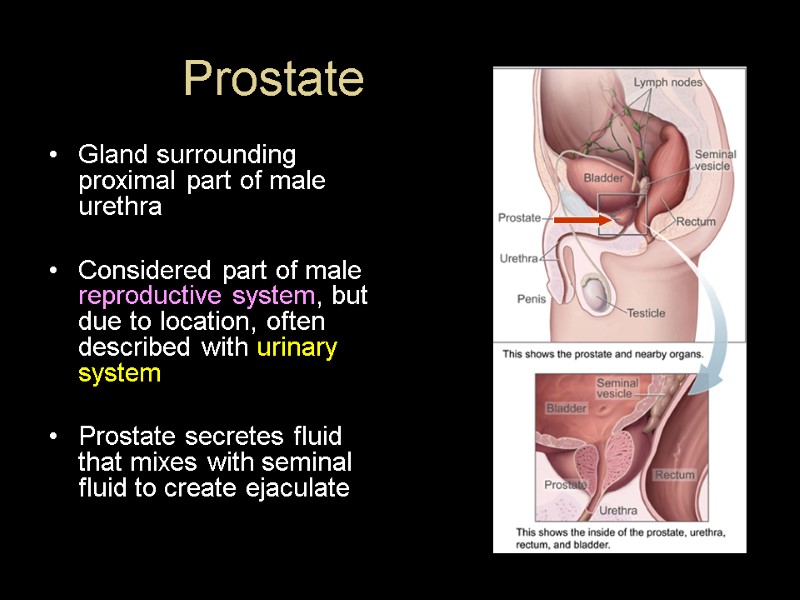
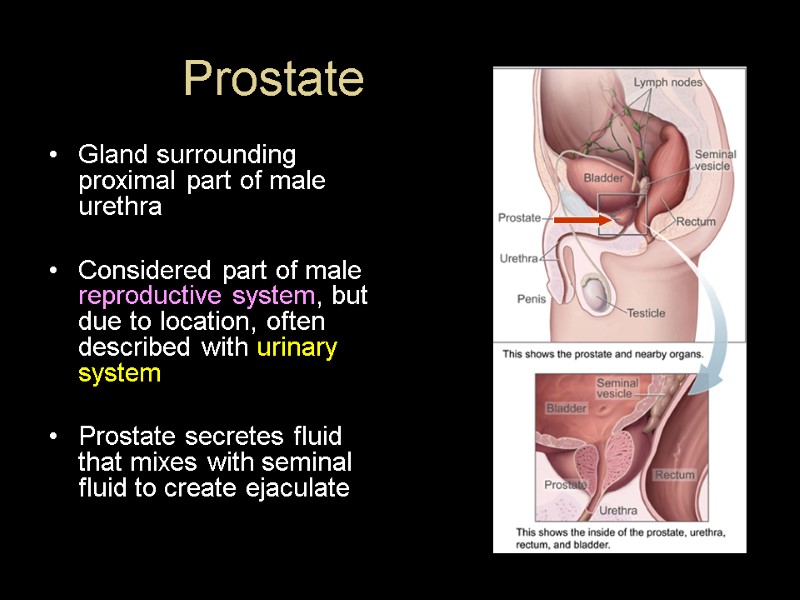 Prostate Gland surrounding proximal part of male urethra Considered part of male reproductive system, but due to location, often described with urinary system Prostate secretes fluid that mixes with seminal fluid to create ejaculate
Prostate Gland surrounding proximal part of male urethra Considered part of male reproductive system, but due to location, often described with urinary system Prostate secretes fluid that mixes with seminal fluid to create ejaculate
 Radiography of Urinary System aka Urography Radiographic investigation of renal drainage or collecting system
Radiography of Urinary System aka Urography Radiographic investigation of renal drainage or collecting system
 IVU- Intravenous Urogram ! Formerly erroneously known as IVP-Intravenous pyelogram! pyelo refers to renal pelvis and calyces only study also shows ureters, bladder, and sometimes urethra
IVU- Intravenous Urogram ! Formerly erroneously known as IVP-Intravenous pyelogram! pyelo refers to renal pelvis and calyces only study also shows ureters, bladder, and sometimes urethra
 Indications For Urography Demonstrate physiologic function and structure of urinary system Evaluate abd. Masses, renal cysts and tumors Urolithiasis (stones) Pyelonephritis (Inflammation of kidney) Hydronephrosis (distension of renal pelvis and calyces with urine) Effects of trauma Pre-op evaluation Renal hypertension
Indications For Urography Demonstrate physiologic function and structure of urinary system Evaluate abd. Masses, renal cysts and tumors Urolithiasis (stones) Pyelonephritis (Inflammation of kidney) Hydronephrosis (distension of renal pelvis and calyces with urine) Effects of trauma Pre-op evaluation Renal hypertension
 Contraindications Inability to filter contrast medium from blood Allergy to contrast Abnormal BUN and Creatinine levels
Contraindications Inability to filter contrast medium from blood Allergy to contrast Abnormal BUN and Creatinine levels
 Preparation Of Pt Pt should follow low residue diet for 1-2 days prior to exam laxative taken day before NPO after midnight Pts with multiple myeloma, high uric acid levels, or diabetes should be well hydrated before IVP exam Dehydration leads to increased risk of renal failure
Preparation Of Pt Pt should follow low residue diet for 1-2 days prior to exam laxative taken day before NPO after midnight Pts with multiple myeloma, high uric acid levels, or diabetes should be well hydrated before IVP exam Dehydration leads to increased risk of renal failure
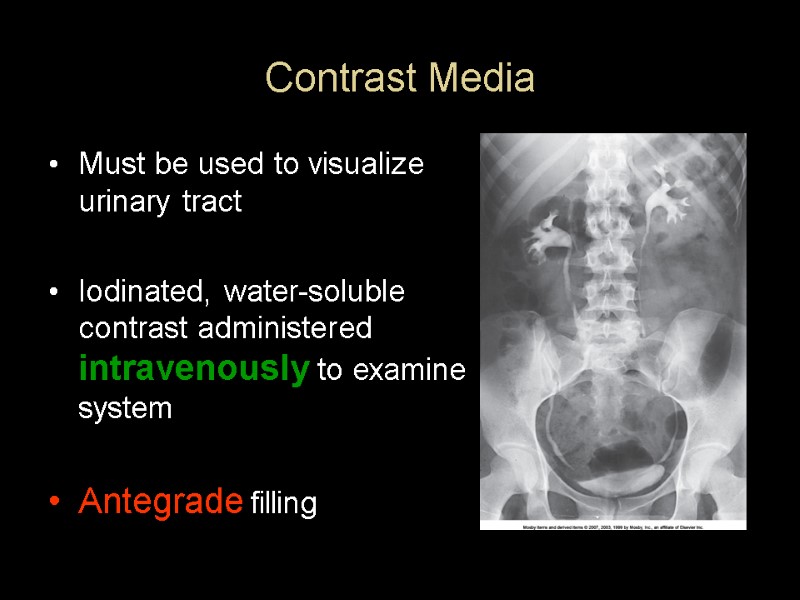
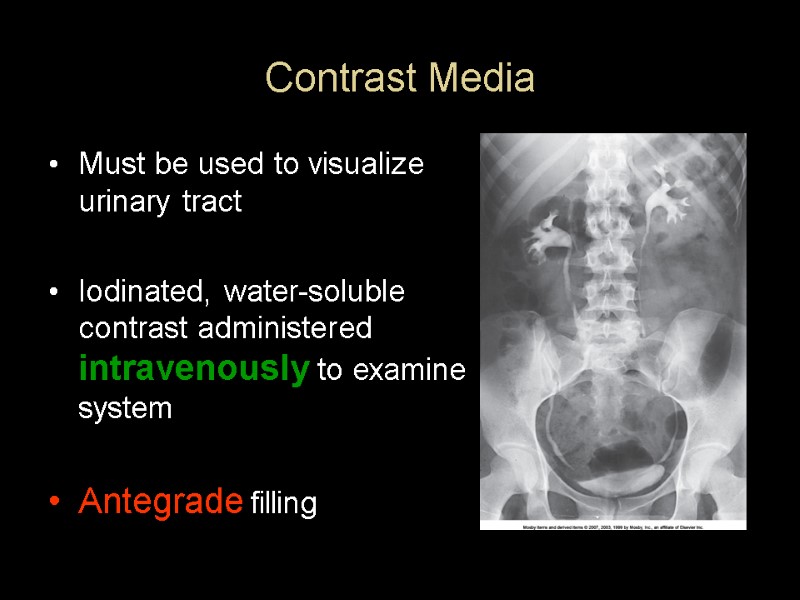 Contrast Media Must be used to visualize urinary tract Iodinated, water-soluble contrast administered intravenously to examine system Antegrade filling
Contrast Media Must be used to visualize urinary tract Iodinated, water-soluble contrast administered intravenously to examine system Antegrade filling
 Contrast Media Excretory urography (IVU) generally uses a 50 to 70% iodine solution Lower concentrations for bladder studies due to large amount required to fill bladder (30%) Non-ionic contrast is generally used More expensive, but- Patients less likely to have reactions with nonionic
Contrast Media Excretory urography (IVU) generally uses a 50 to 70% iodine solution Lower concentrations for bladder studies due to large amount required to fill bladder (30%) Non-ionic contrast is generally used More expensive, but- Patients less likely to have reactions with nonionic
 Contrast Media and Adverse Reactions Crucial not to leave pt alone for first 5 minutes after injection! Mild reactions warmth flushing hives, Nausea/Vomiting, respiratory edema (accumulation of fluid in lungs) Severe reactions Anaphylactic shock (sudden allergic response associated with a sudden drop in blood pressure and difficulty breathing). Can lead to death in a matter of minutes)
Contrast Media and Adverse Reactions Crucial not to leave pt alone for first 5 minutes after injection! Mild reactions warmth flushing hives, Nausea/Vomiting, respiratory edema (accumulation of fluid in lungs) Severe reactions Anaphylactic shock (sudden allergic response associated with a sudden drop in blood pressure and difficulty breathing). Can lead to death in a matter of minutes)
 Injection Procedure Obtain allergy history Explain exam to pt Prepare contrast and supplies (sterile tech.) Assist radiologist as necessary or Perform injection if IVcertified
Injection Procedure Obtain allergy history Explain exam to pt Prepare contrast and supplies (sterile tech.) Assist radiologist as necessary or Perform injection if IVcertified
 Injection Supplies (cont.d) Tourniquet IV arm board Towels Emergency kit Emesis basin Alcohol wipes, hibiclens, or povidone iodine wipes or swabs Contrast 19-22 G needle, butterfly or angiocath for infusion Extension tubing Tape or clear-type dressing
Injection Supplies (cont.d) Tourniquet IV arm board Towels Emergency kit Emesis basin Alcohol wipes, hibiclens, or povidone iodine wipes or swabs Contrast 19-22 G needle, butterfly or angiocath for infusion Extension tubing Tape or clear-type dressing
 IVU Procedure Scout – KUB Contrast is injected Timed sequence of films obtained until bladder begins to fill- Immediate image of kidneys 5 minute image of abd. or kidneys Compression applied
IVU Procedure Scout – KUB Contrast is injected Timed sequence of films obtained until bladder begins to fill- Immediate image of kidneys 5 minute image of abd. or kidneys Compression applied
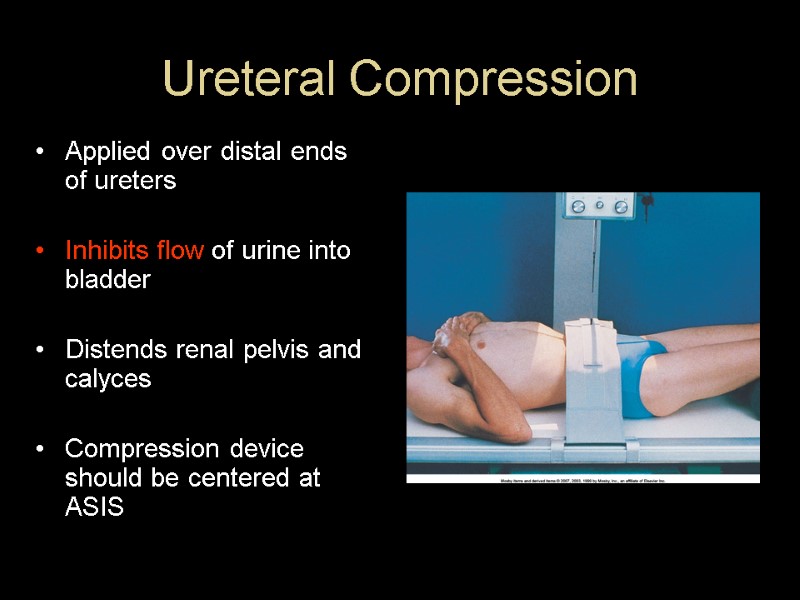
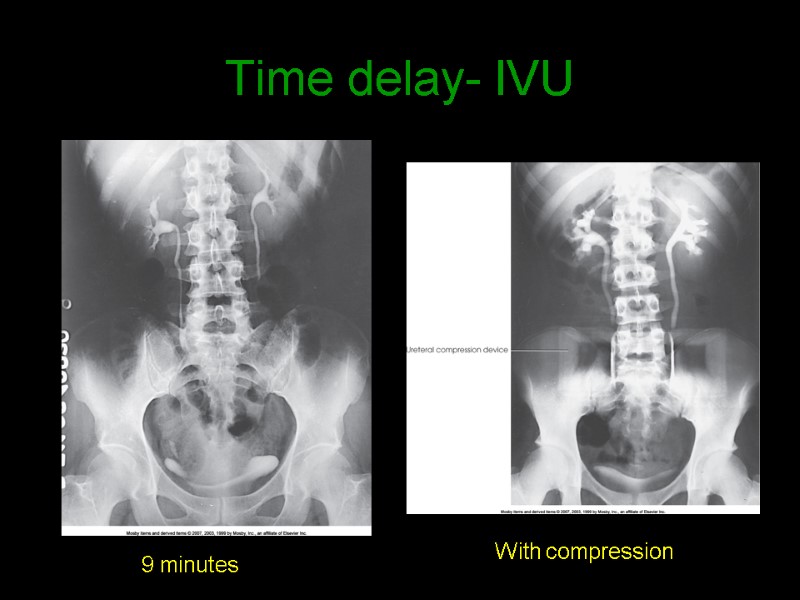
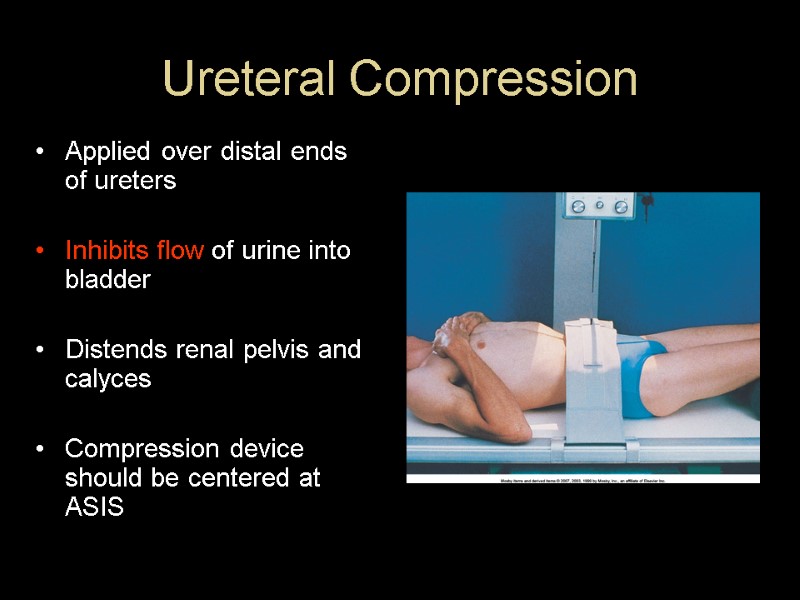 Ureteral Compression Applied over distal ends of ureters Inhibits flow of urine into bladder Distends renal pelvis and calyces Compression device should be centered at ASIS
Ureteral Compression Applied over distal ends of ureters Inhibits flow of urine into bladder Distends renal pelvis and calyces Compression device should be centered at ASIS
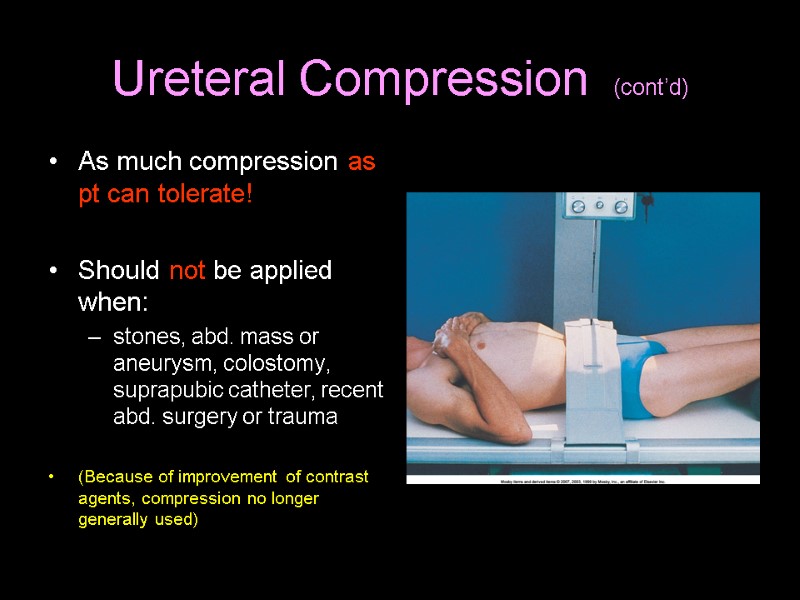 Ureteral Compression (cont’d) As much compression as pt can tolerate! Should not be applied when: stones, abd. mass or aneurysm, colostomy, suprapubic catheter, recent abd. surgery or trauma (Because of improvement of contrast agents, compression no longer generally used)
Ureteral Compression (cont’d) As much compression as pt can tolerate! Should not be applied when: stones, abd. mass or aneurysm, colostomy, suprapubic catheter, recent abd. surgery or trauma (Because of improvement of contrast agents, compression no longer generally used)
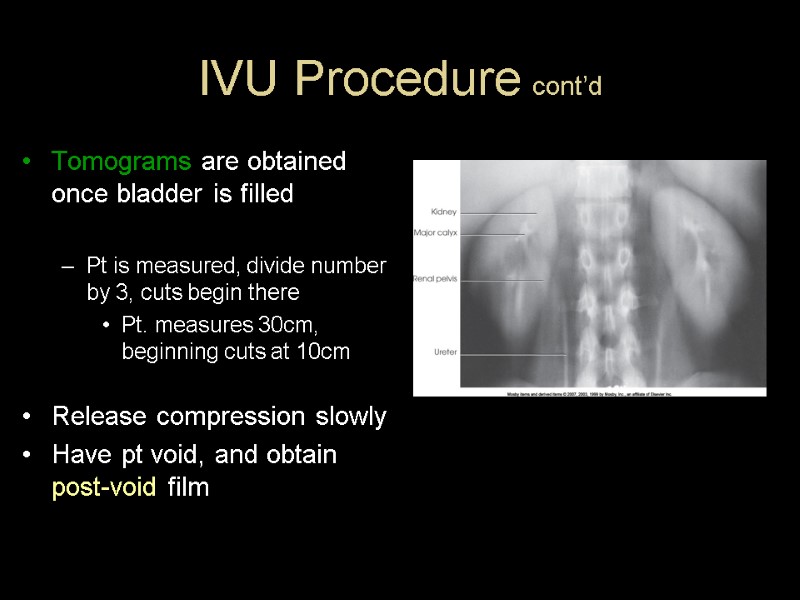
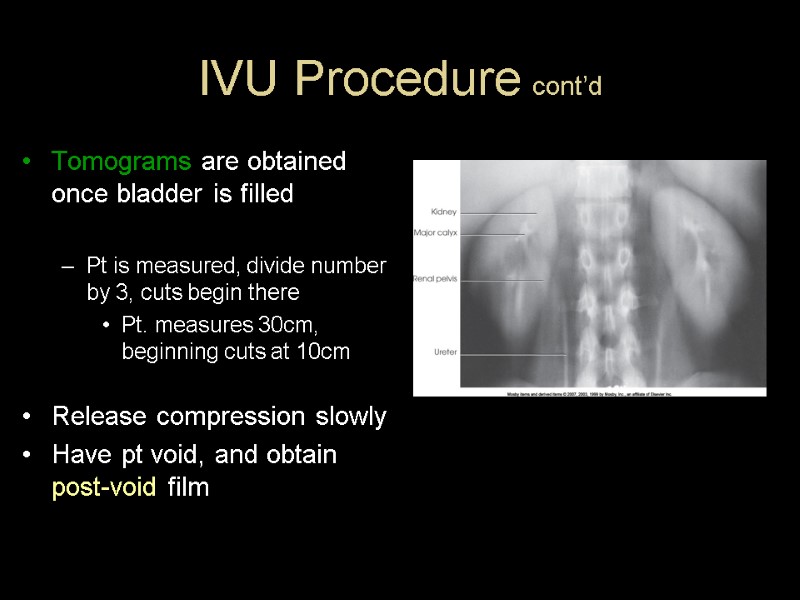 IVU Procedure cont’d Tomograms are obtained once bladder is filled Pt is measured, divide number by 3, cuts begin there Pt. measures 30cm, beginning cuts at 10cm Release compression slowly Have pt void, and obtain post-void film
IVU Procedure cont’d Tomograms are obtained once bladder is filled Pt is measured, divide number by 3, cuts begin there Pt. measures 30cm, beginning cuts at 10cm Release compression slowly Have pt void, and obtain post-void film
 Radiation Protection Radiographer is responsible! Gonadal shield - if it does not interfere with examination objective Close collimation Avoid repeat exposures Shield males for all urinary studies, except when urethra is of primary interest
Radiation Protection Radiographer is responsible! Gonadal shield - if it does not interfere with examination objective Close collimation Avoid repeat exposures Shield males for all urinary studies, except when urethra is of primary interest
 Radiation Protection Shield females when IR centered over kidneys Rule out chance of pregnancy before examination (Emergency cases may not allow time)
Radiation Protection Shield females when IR centered over kidneys Rule out chance of pregnancy before examination (Emergency cases may not allow time)
 Radiographic Positions IVU
Radiographic Positions IVU
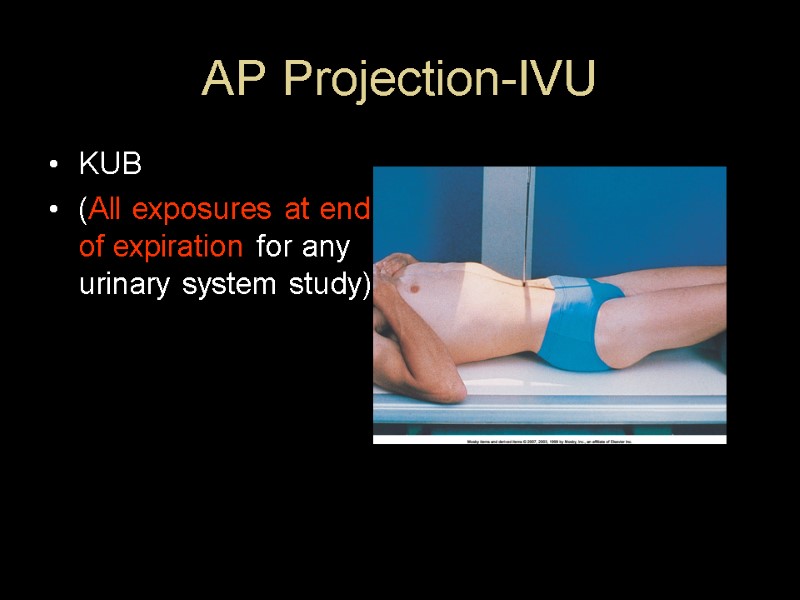
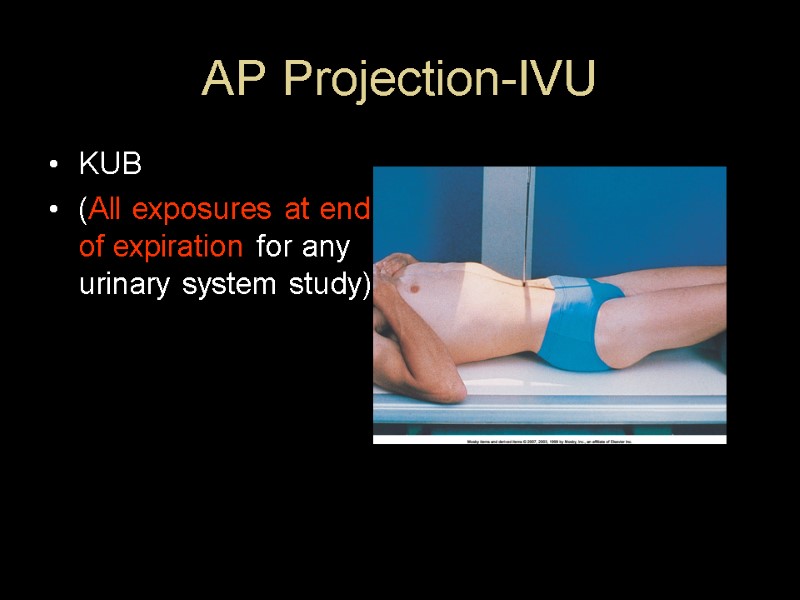 AP Projection-IVU KUB (All exposures at end of expiration for any urinary system study)
AP Projection-IVU KUB (All exposures at end of expiration for any urinary system study)
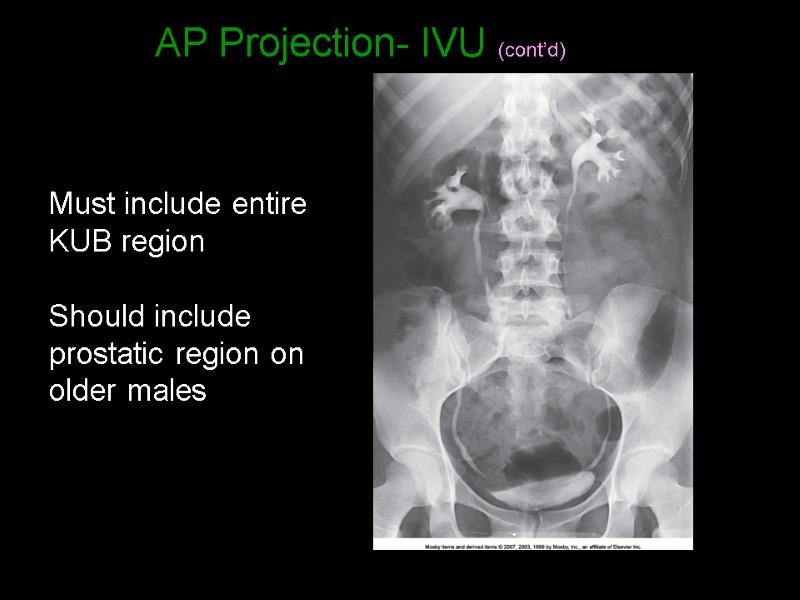
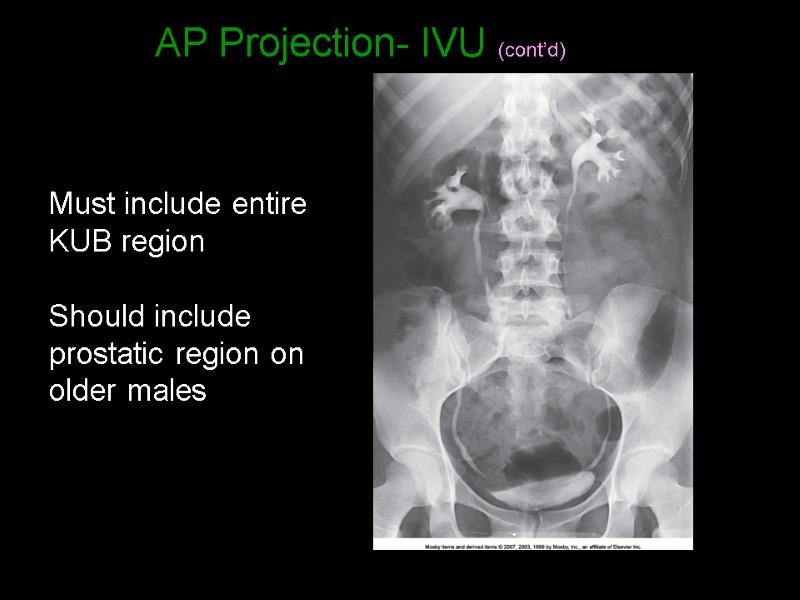 AP Projection- IVU (cont’d) Must include entire KUB region Should include prostatic region on older males
AP Projection- IVU (cont’d) Must include entire KUB region Should include prostatic region on older males
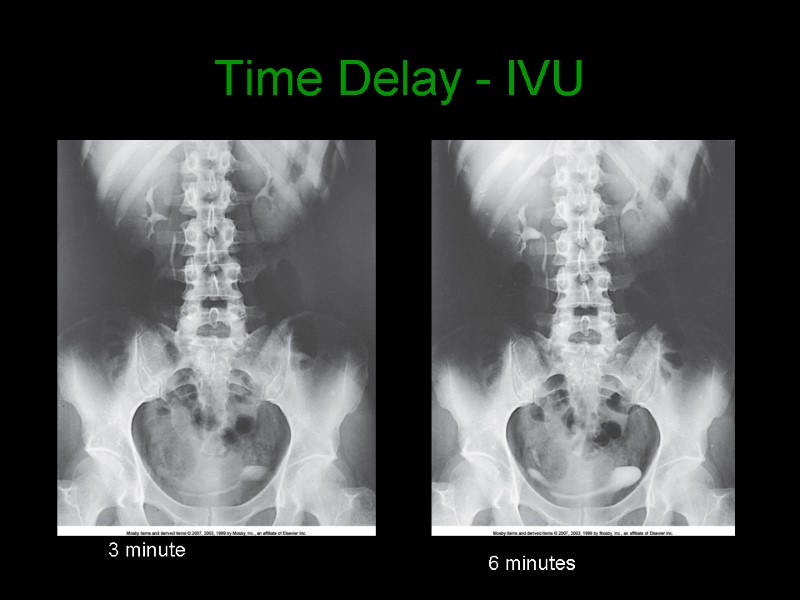
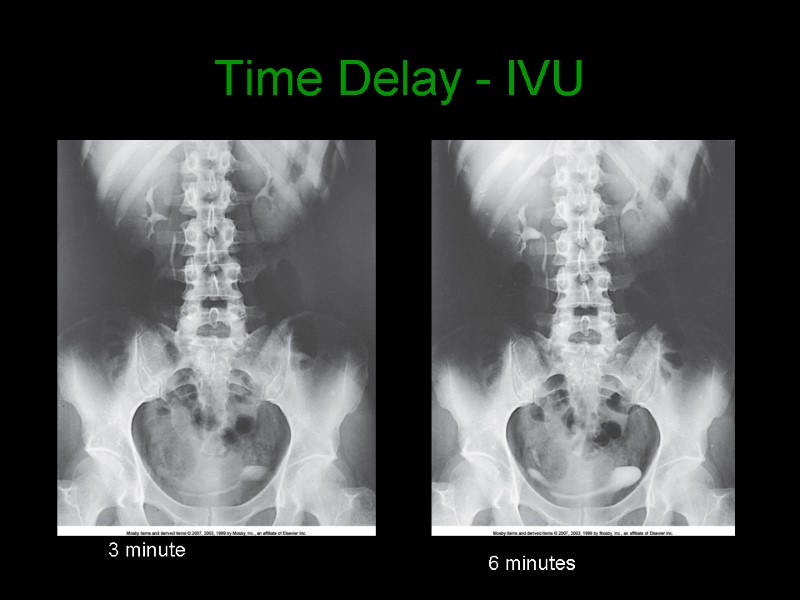 Time Delay - IVU 3 minute 6 minutes
Time Delay - IVU 3 minute 6 minutes
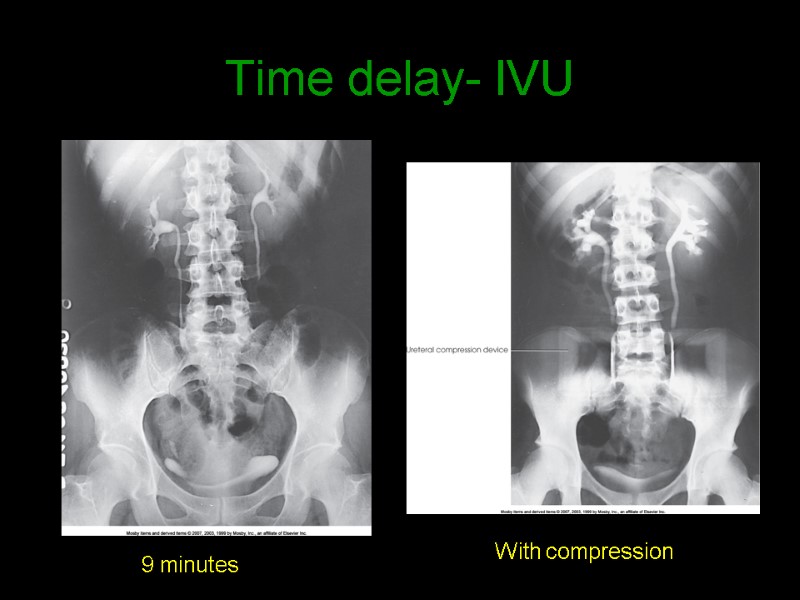 Time delay- IVU 9 minutes With compression
Time delay- IVU 9 minutes With compression
 AP Projection Variations Trendelenberg Lower head 15 - 20 degrees Helps demonstrate lower ureters Upright Center lower - organs change position Prone Demonstrates ureteropelvic region Fills obstructed ureter in cases of hydronephrosis (distension of renal pelvis and calyces with urine)
AP Projection Variations Trendelenberg Lower head 15 - 20 degrees Helps demonstrate lower ureters Upright Center lower - organs change position Prone Demonstrates ureteropelvic region Fills obstructed ureter in cases of hydronephrosis (distension of renal pelvis and calyces with urine)
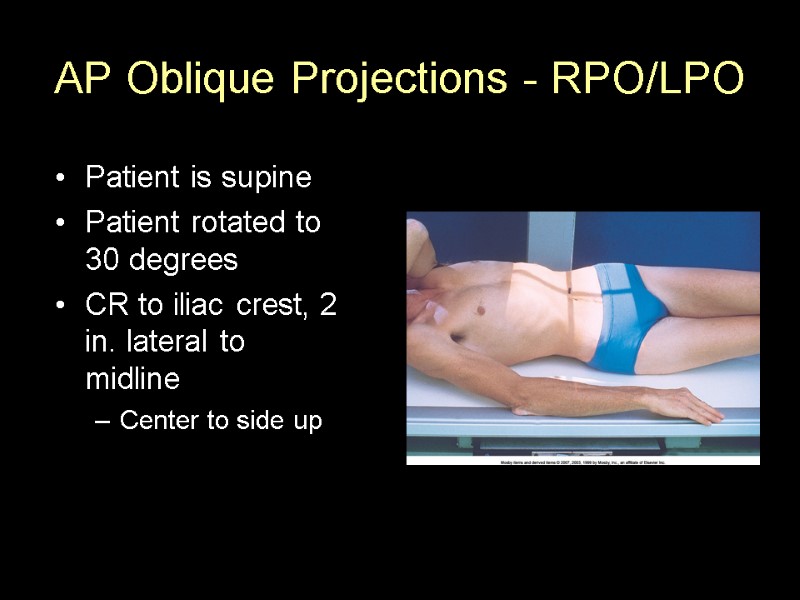
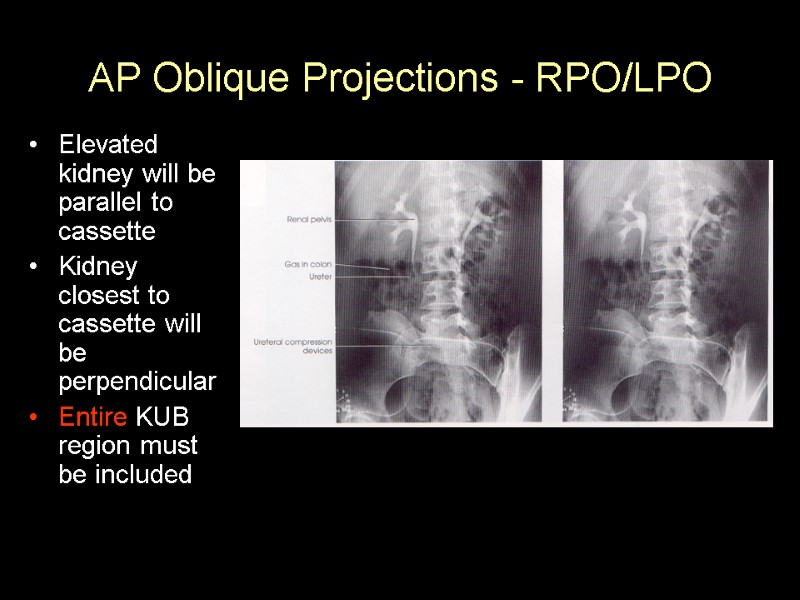
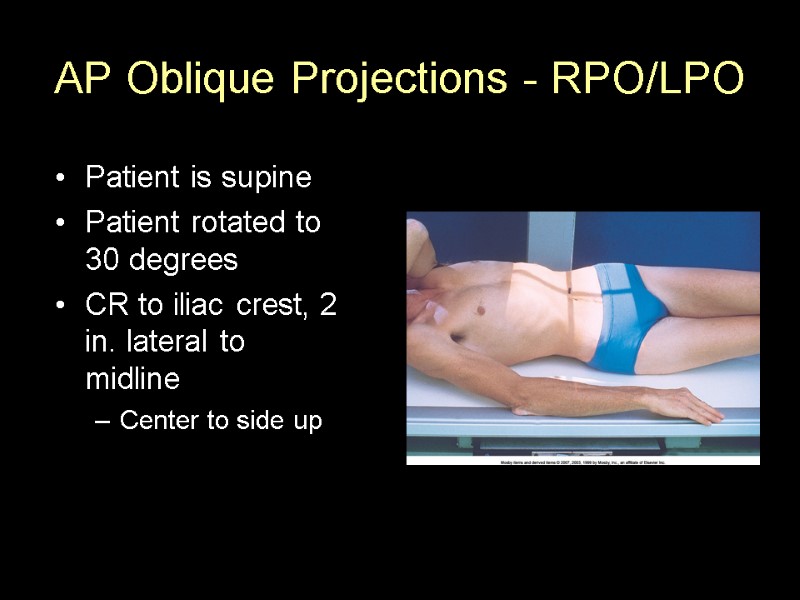 AP Oblique Projections - RPO/LPO Patient is supine Patient rotated to 30 degrees CR to iliac crest, 2 in. lateral to midline Center to side up
AP Oblique Projections - RPO/LPO Patient is supine Patient rotated to 30 degrees CR to iliac crest, 2 in. lateral to midline Center to side up
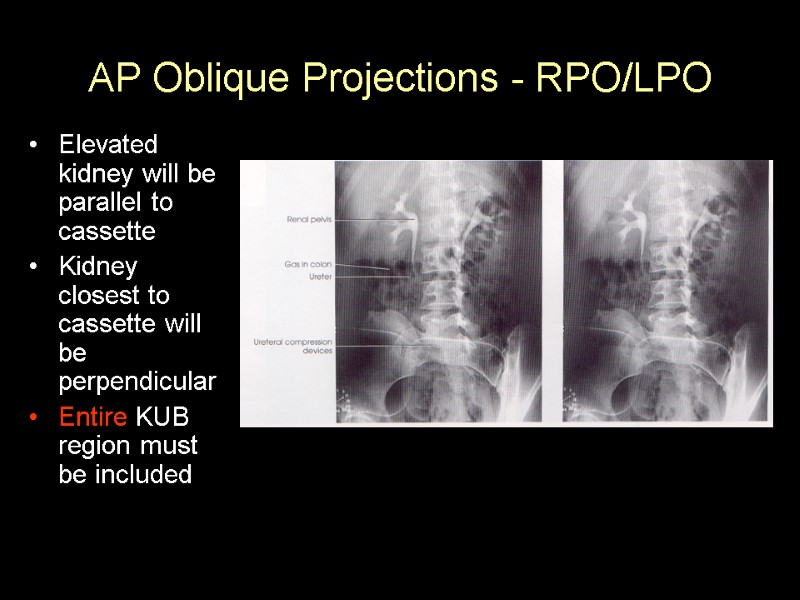 AP Oblique Projections - RPO/LPO Elevated kidney will be parallel to cassette Kidney closest to cassette will be perpendicular Entire KUB region must be included
AP Oblique Projections - RPO/LPO Elevated kidney will be parallel to cassette Kidney closest to cassette will be perpendicular Entire KUB region must be included
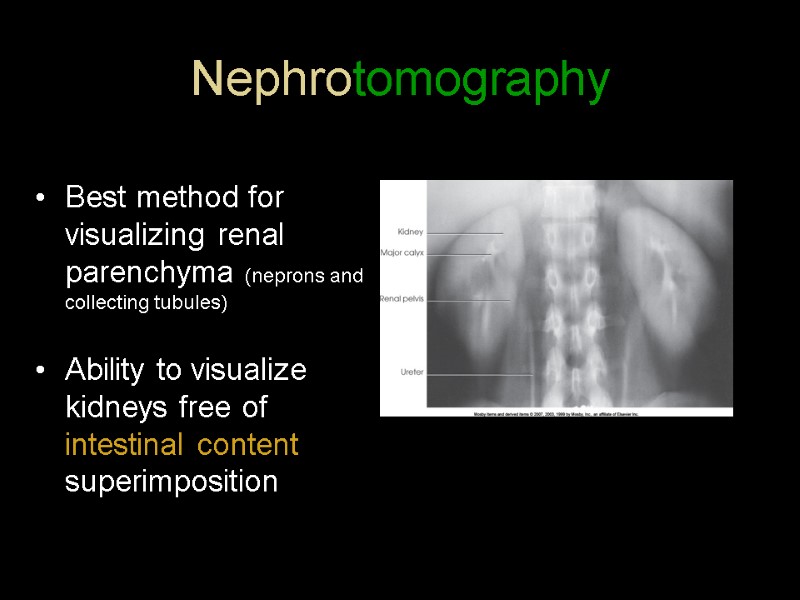
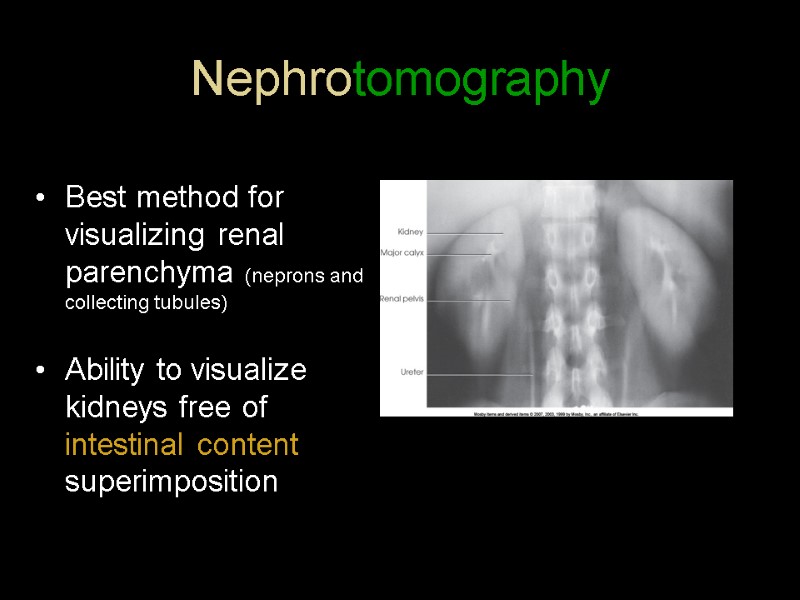 Nephrotomography Best method for visualizing renal parenchyma (neprons and collecting tubules) Ability to visualize kidneys free of intestinal content superimposition
Nephrotomography Best method for visualizing renal parenchyma (neprons and collecting tubules) Ability to visualize kidneys free of intestinal content superimposition

 Retrograde Urography What does retrograde mean? Opposite normal flow
Retrograde Urography What does retrograde mean? Opposite normal flow
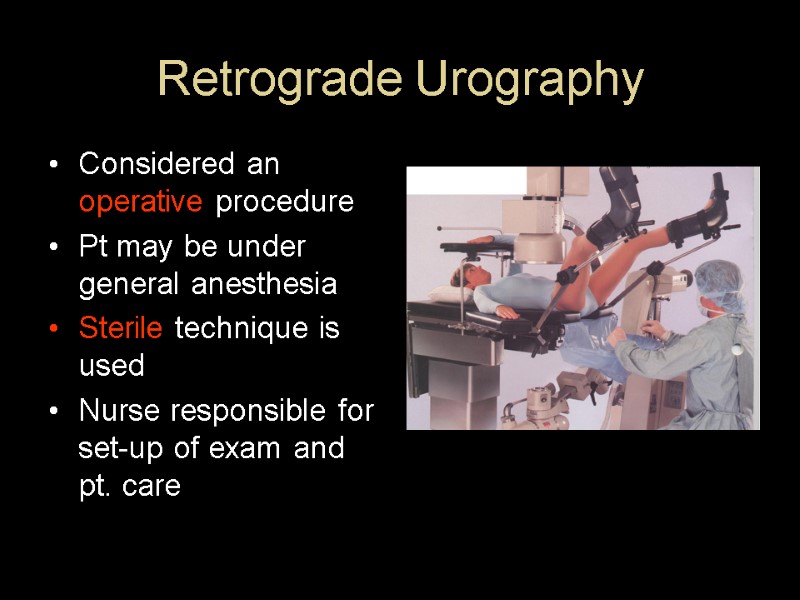
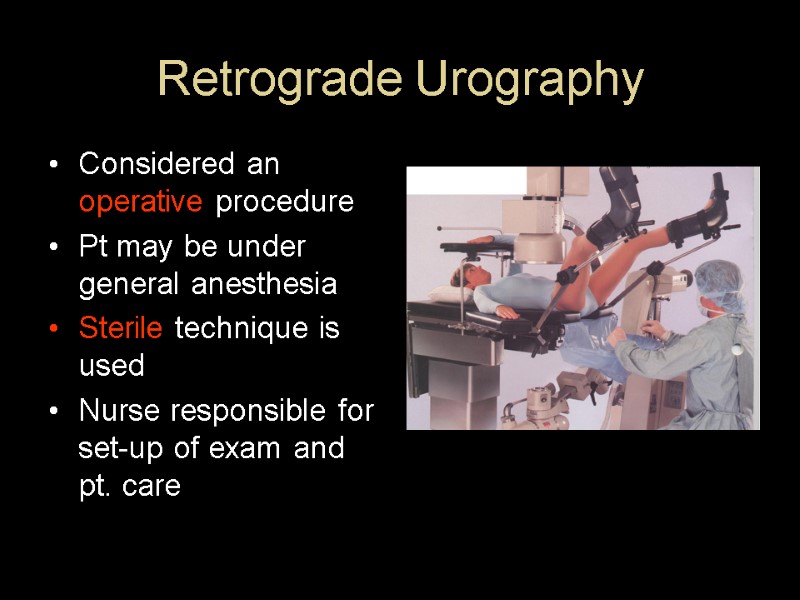 Retrograde Urography Considered an operative procedure Pt may be under general anesthesia Sterile technique is used Nurse responsible for set-up of exam and pt. care
Retrograde Urography Considered an operative procedure Pt may be under general anesthesia Sterile technique is used Nurse responsible for set-up of exam and pt. care
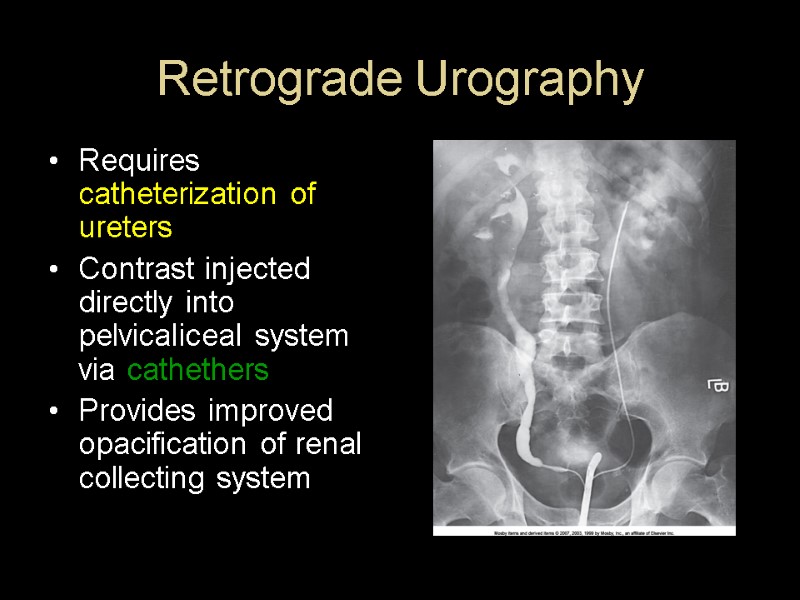
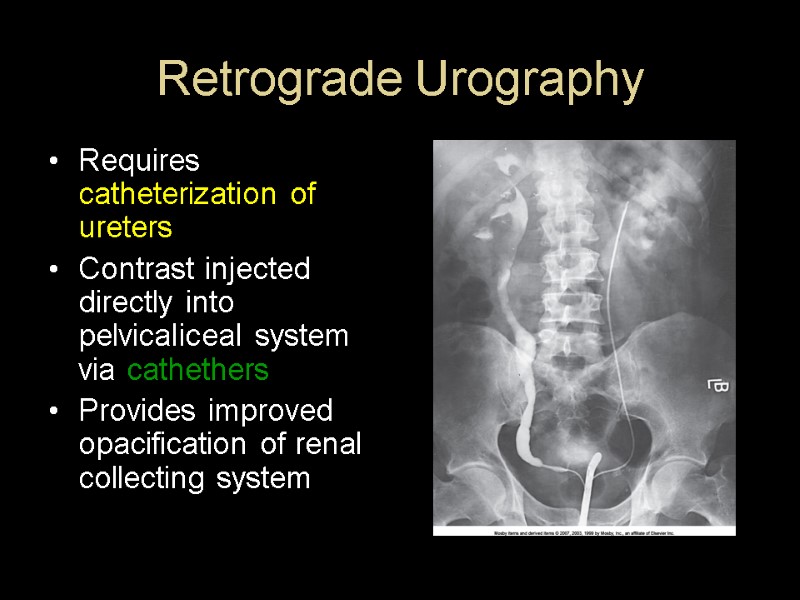 Retrograde Urography Requires catheterization of ureters Contrast injected directly into pelvicaliceal system via cathethers Provides improved opacification of renal collecting system
Retrograde Urography Requires catheterization of ureters Contrast injected directly into pelvicaliceal system via cathethers Provides improved opacification of renal collecting system
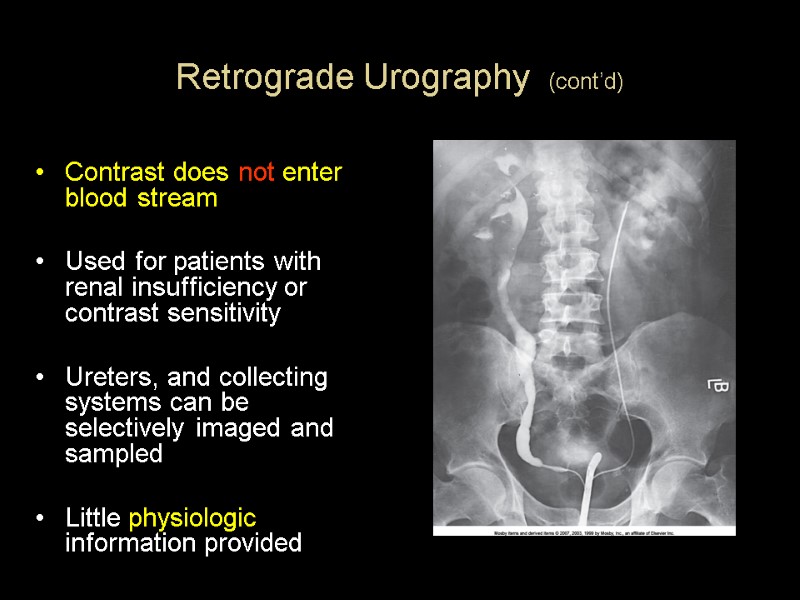
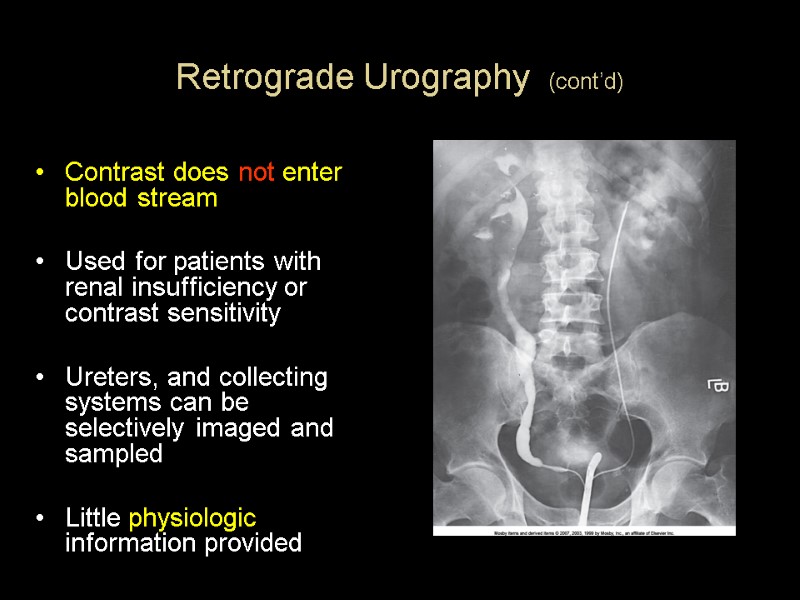 Retrograde Urography (cont’d) Contrast does not enter blood stream Used for patients with renal insufficiency or contrast sensitivity Ureters, and collecting systems can be selectively imaged and sampled Little physiologic information provided
Retrograde Urography (cont’d) Contrast does not enter blood stream Used for patients with renal insufficiency or contrast sensitivity Ureters, and collecting systems can be selectively imaged and sampled Little physiologic information provided

 Cystography
Cystography
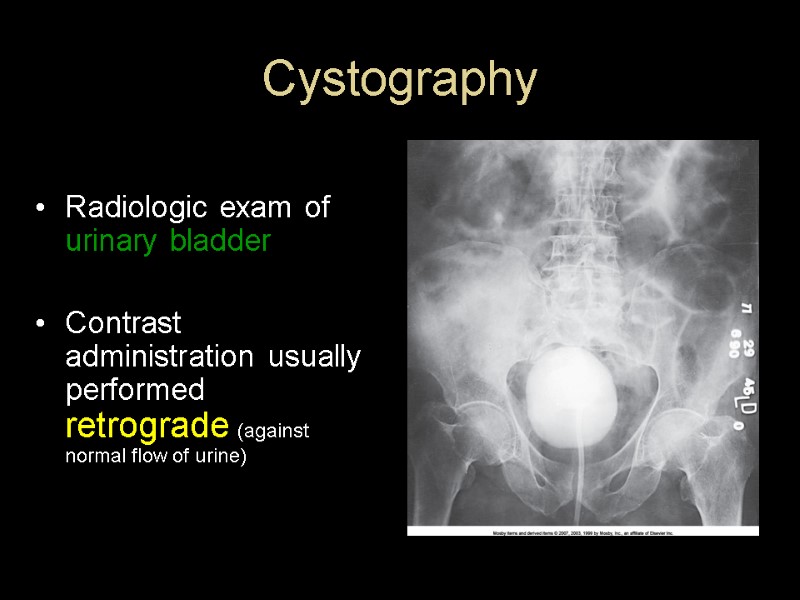
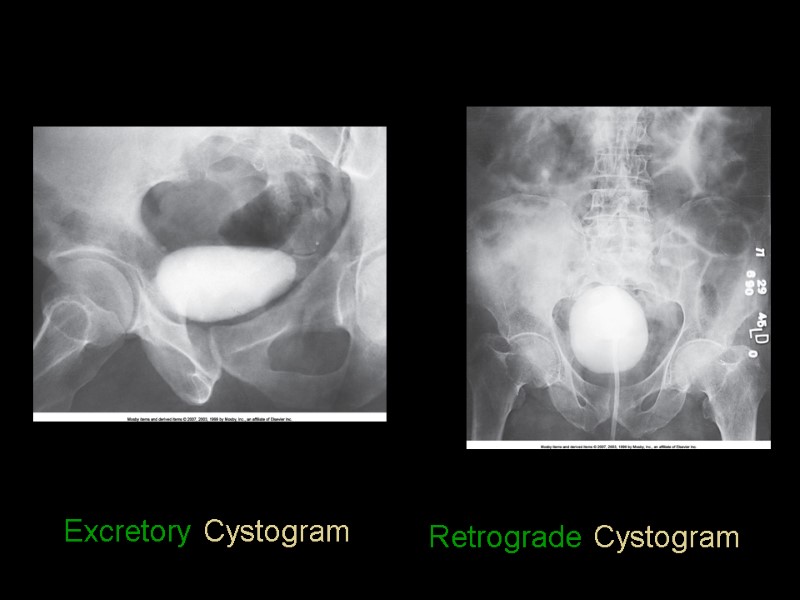
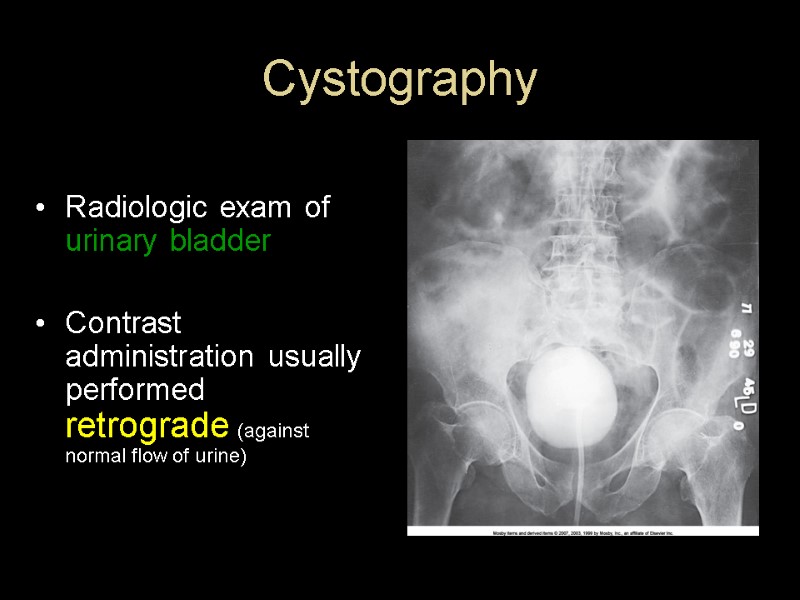 Cystography Radiologic exam of urinary bladder Contrast administration usually performed retrograde (against normal flow of urine)
Cystography Radiologic exam of urinary bladder Contrast administration usually performed retrograde (against normal flow of urine)
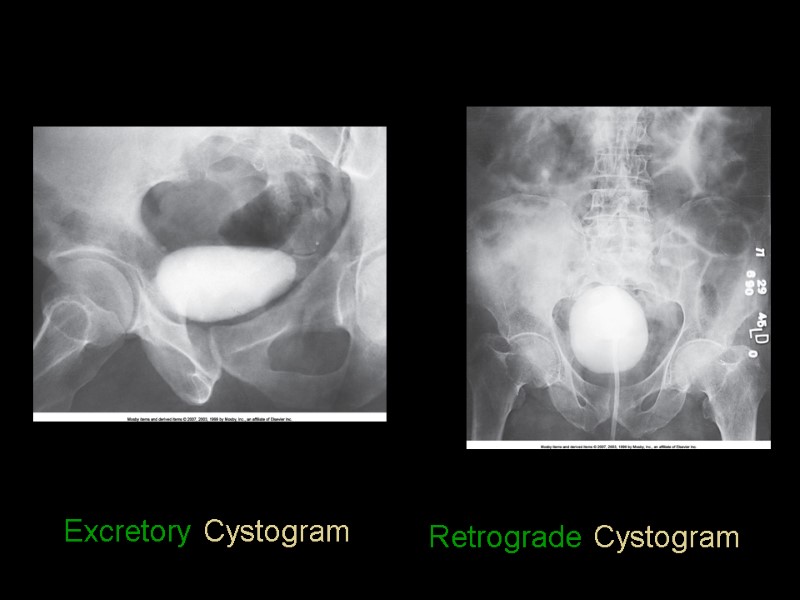 Excretory Cystogram Retrograde Cystogram
Excretory Cystogram Retrograde Cystogram
 Cystography Indicated for: Vesicoureteral reflux (backward flow of urine into ureters) Recurrent lower urinary tract infection Neurogenic bladder: (dysfunction due to disease of central nervous system or peripheral nerves)
Cystography Indicated for: Vesicoureteral reflux (backward flow of urine into ureters) Recurrent lower urinary tract infection Neurogenic bladder: (dysfunction due to disease of central nervous system or peripheral nerves)
 Cystography indications cont’d Bladder trauma Prostate enlargement Lower urinary tract fistulae Urethral stricture Posterior urethral valves (obstructive congenital defect of the male urethra)
Cystography indications cont’d Bladder trauma Prostate enlargement Lower urinary tract fistulae Urethral stricture Posterior urethral valves (obstructive congenital defect of the male urethra)
 Cystography Contraindications – anything related to catheterization of urethra!
Cystography Contraindications – anything related to catheterization of urethra!
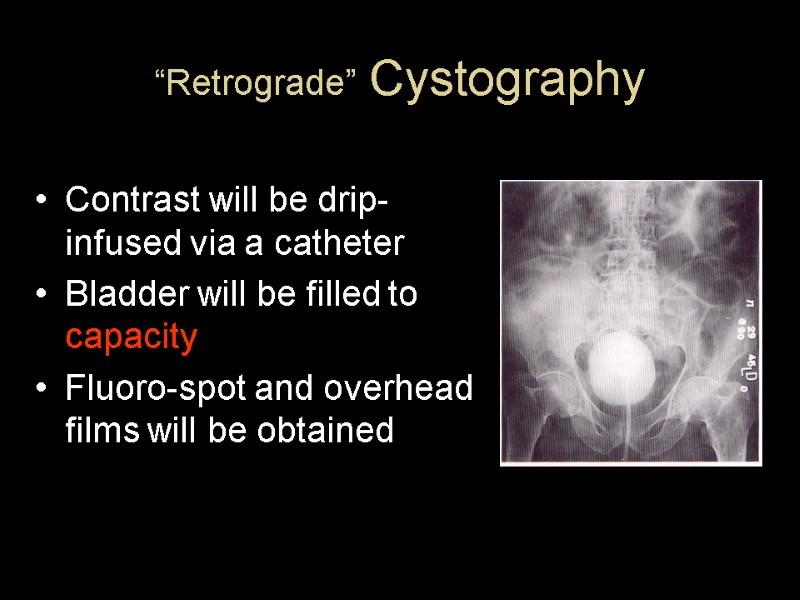
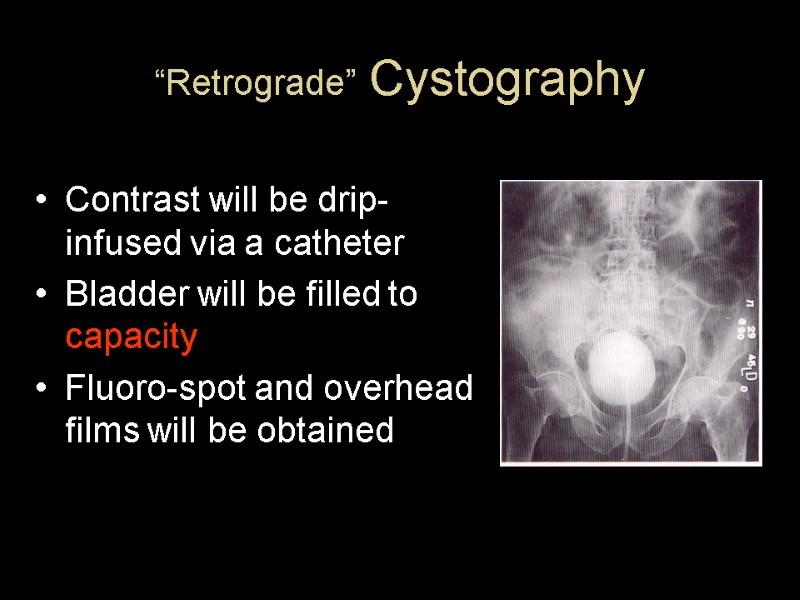 “Retrograde” Cystography Contrast will be drip-infused via a catheter Bladder will be filled to capacity Fluoro-spot and overhead films will be obtained
“Retrograde” Cystography Contrast will be drip-infused via a catheter Bladder will be filled to capacity Fluoro-spot and overhead films will be obtained
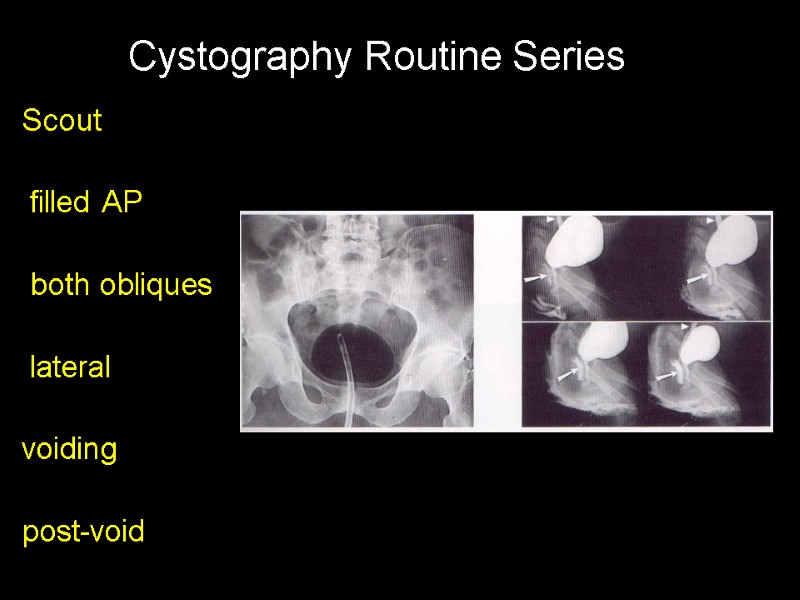
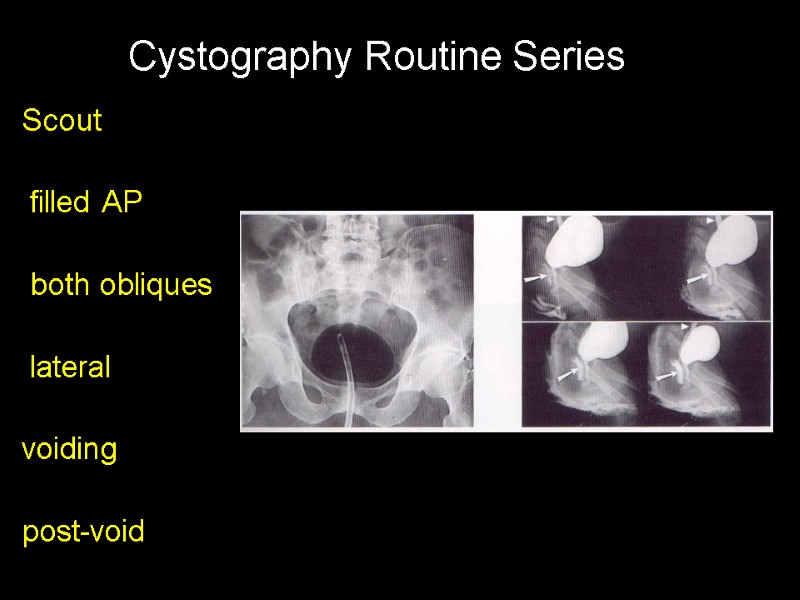 Scout filled AP both obliques lateral voiding post-void Cystography Routine Series
Scout filled AP both obliques lateral voiding post-void Cystography Routine Series
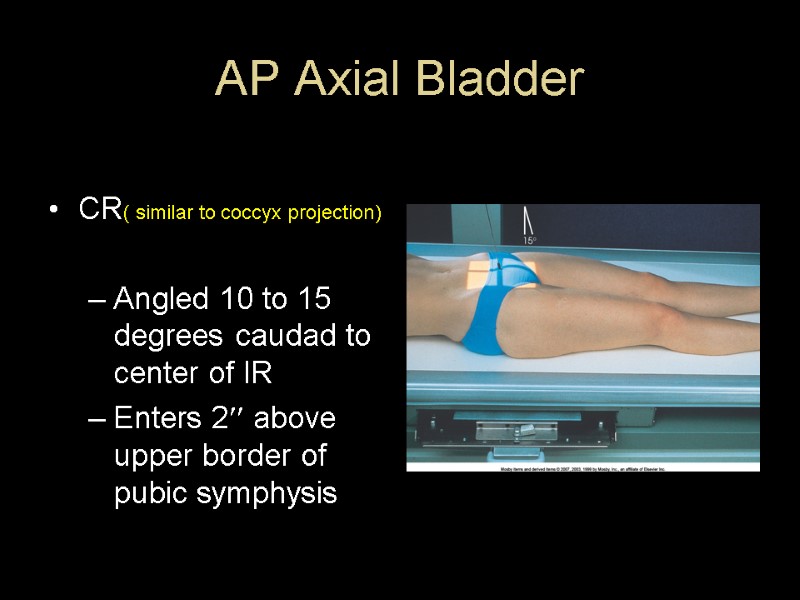
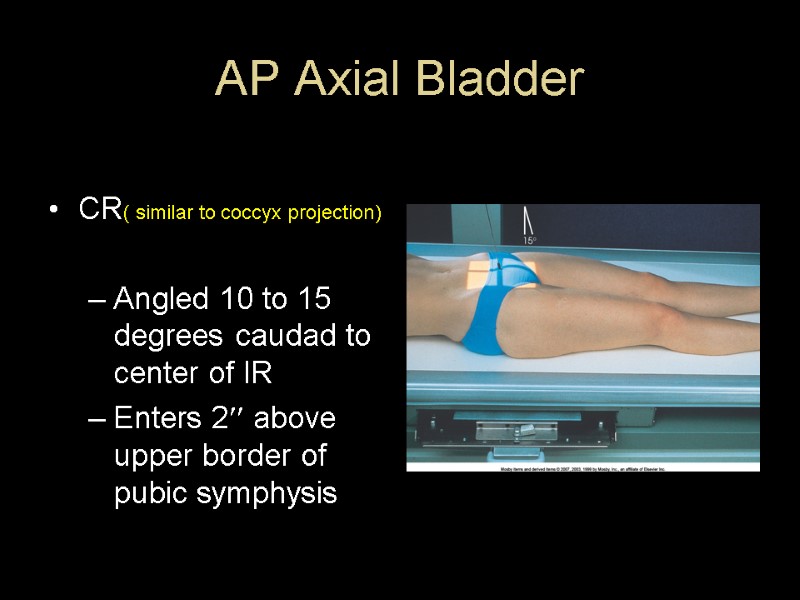 AP Axial Bladder CR( similar to coccyx projection) Angled 10 to 15 degrees caudad to center of IR Enters 2 above upper border of pubic symphysis
AP Axial Bladder CR( similar to coccyx projection) Angled 10 to 15 degrees caudad to center of IR Enters 2 above upper border of pubic symphysis
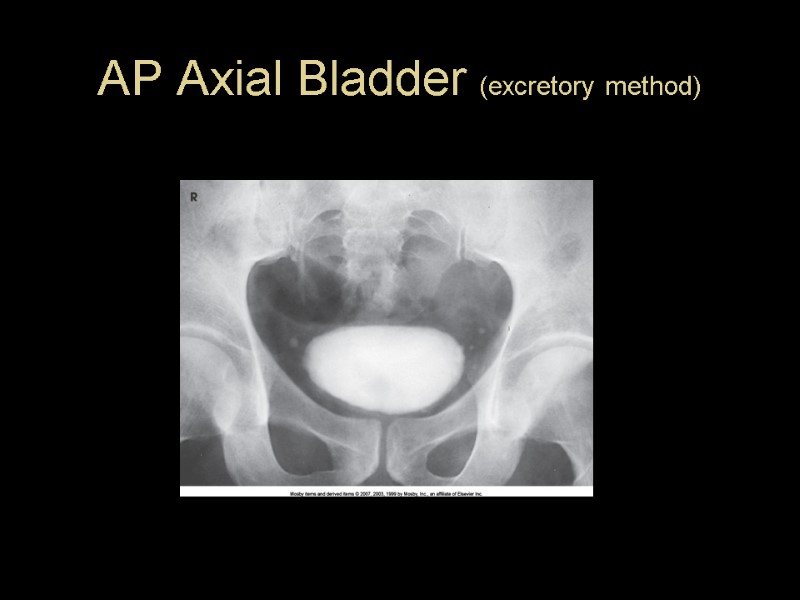
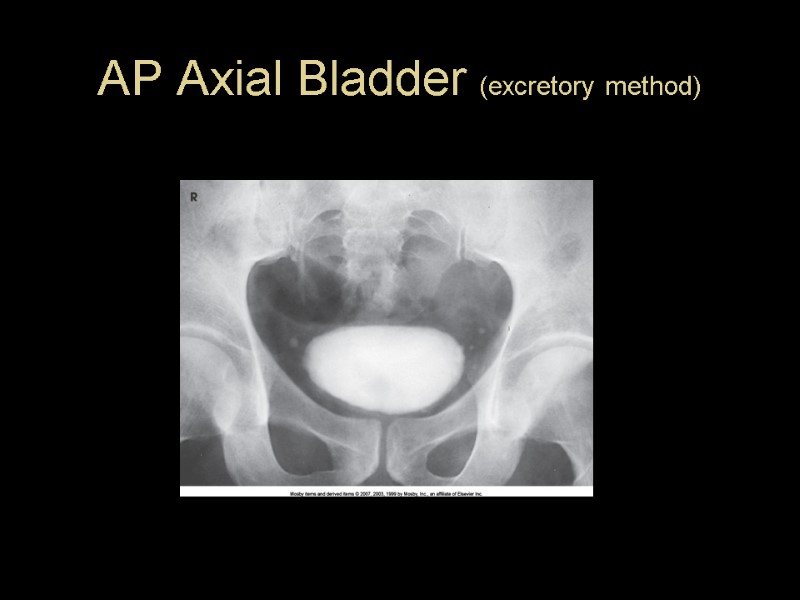 AP Axial Bladder (excretory method)
AP Axial Bladder (excretory method)
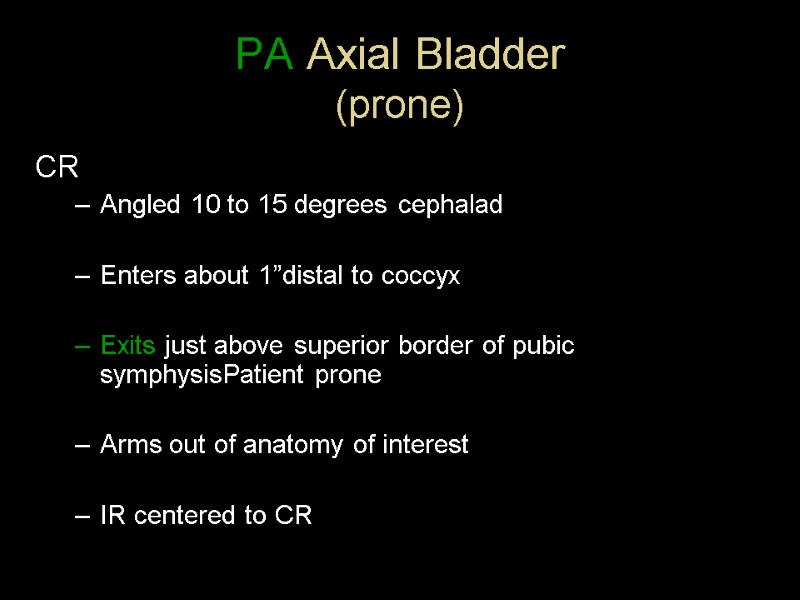 PA Axial Bladder (prone) CR Angled 10 to 15 degrees cephalad Enters about 1”distal to coccyx Exits just above superior border of pubic symphysisPatient prone Arms out of anatomy of interest IR centered to CR
PA Axial Bladder (prone) CR Angled 10 to 15 degrees cephalad Enters about 1”distal to coccyx Exits just above superior border of pubic symphysisPatient prone Arms out of anatomy of interest IR centered to CR
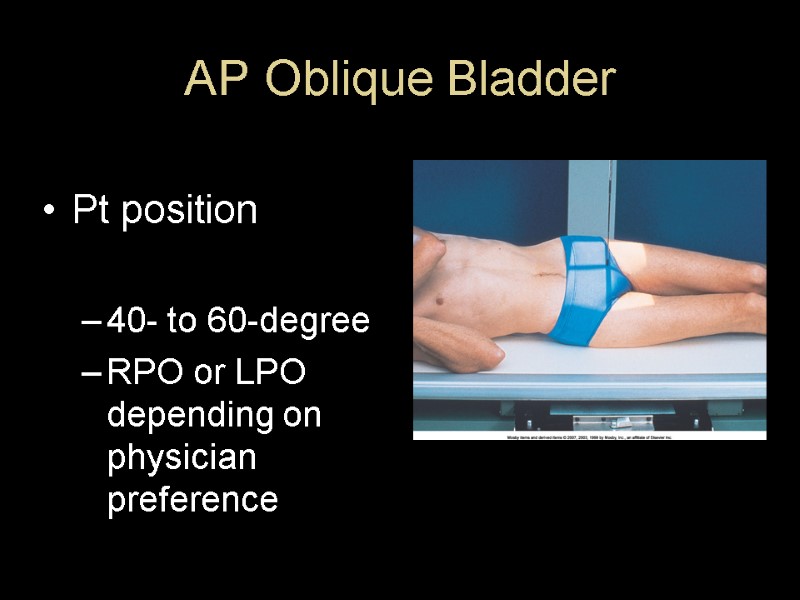
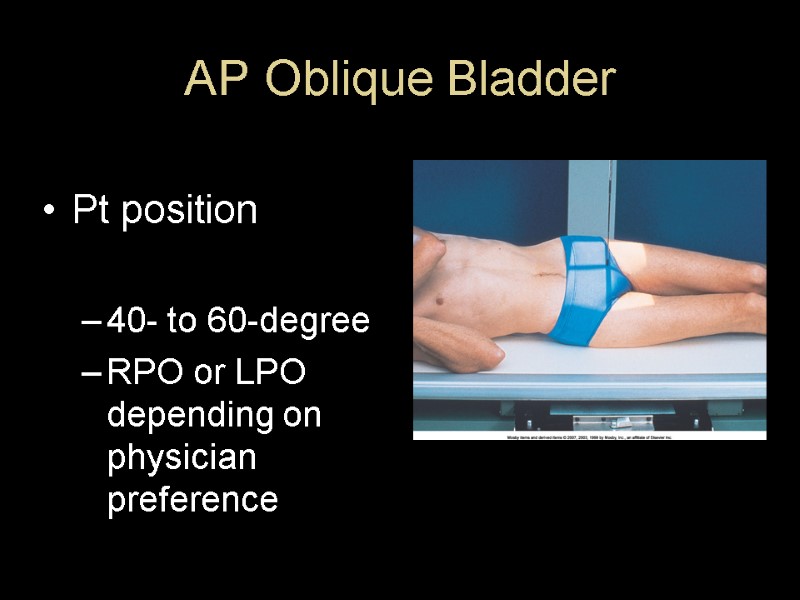 AP Oblique Bladder Pt position 40- to 60-degree RPO or LPO depending on physician preference
AP Oblique Bladder Pt position 40- to 60-degree RPO or LPO depending on physician preference
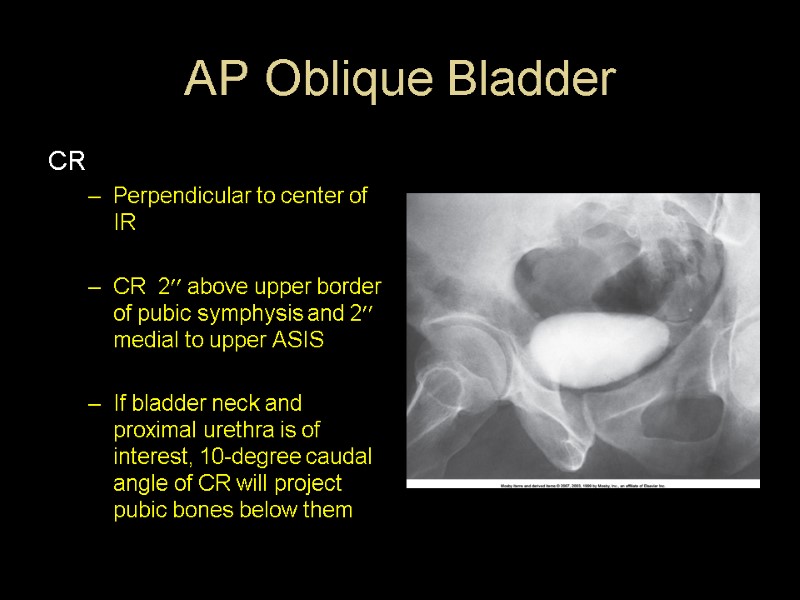
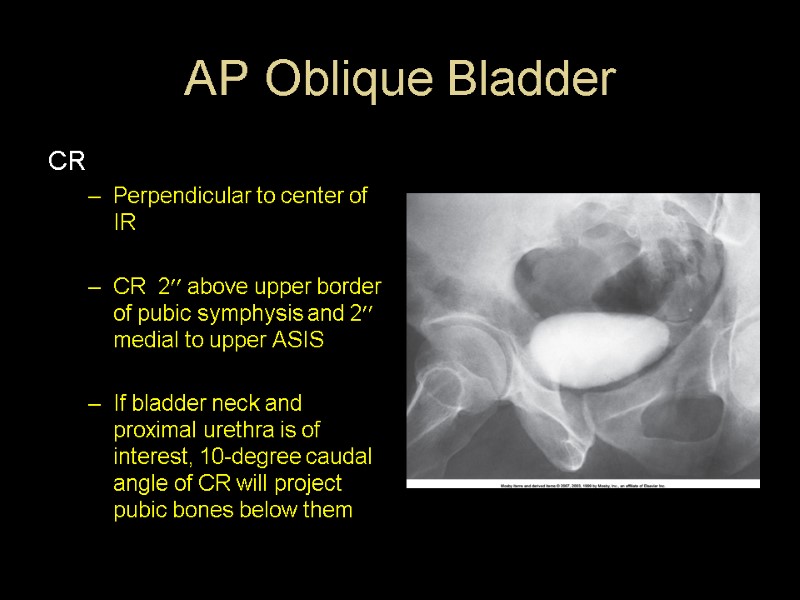 AP Oblique Bladder CR Perpendicular to center of IR CR 2 above upper border of pubic symphysis and 2 medial to upper ASIS If bladder neck and proximal urethra is of interest, 10-degree caudal angle of CR will project pubic bones below them
AP Oblique Bladder CR Perpendicular to center of IR CR 2 above upper border of pubic symphysis and 2 medial to upper ASIS If bladder neck and proximal urethra is of interest, 10-degree caudal angle of CR will project pubic bones below them
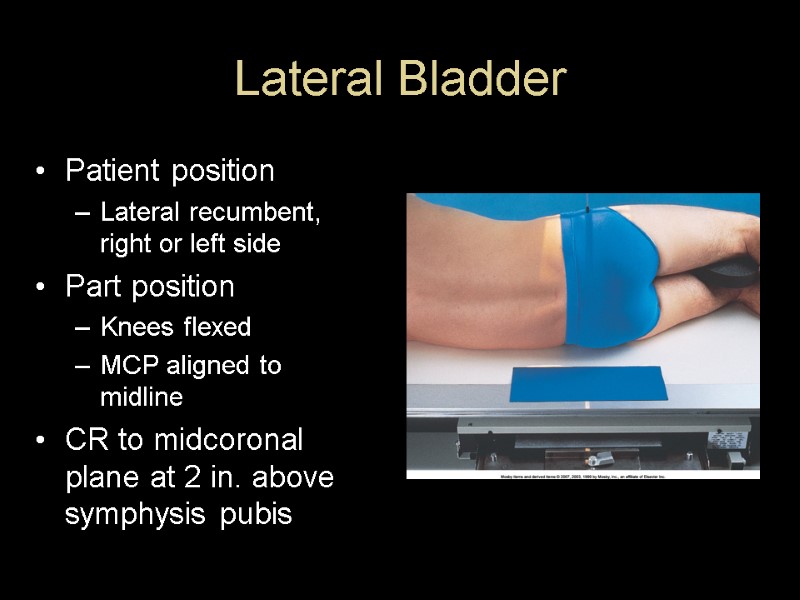
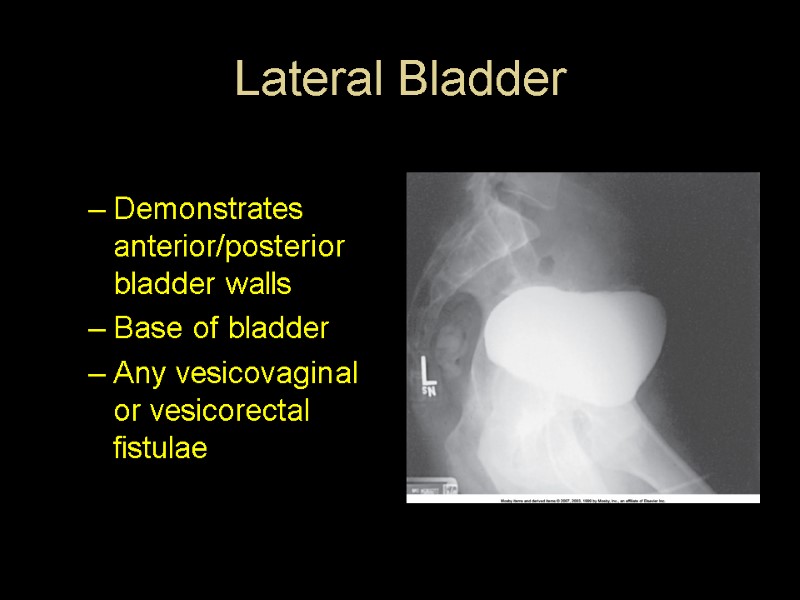
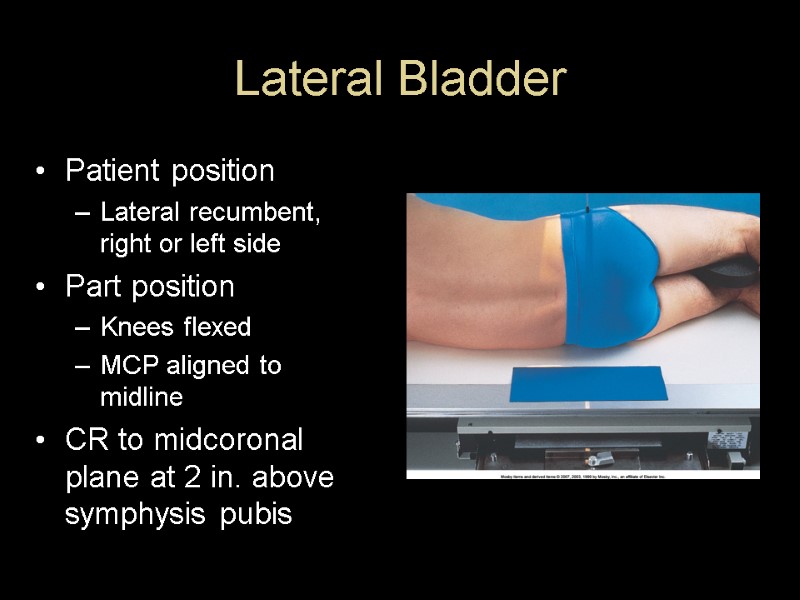 Lateral Bladder Patient position Lateral recumbent, right or left side Part position Knees flexed MCP aligned to midline CR to midcoronal plane at 2 in. above symphysis pubis
Lateral Bladder Patient position Lateral recumbent, right or left side Part position Knees flexed MCP aligned to midline CR to midcoronal plane at 2 in. above symphysis pubis
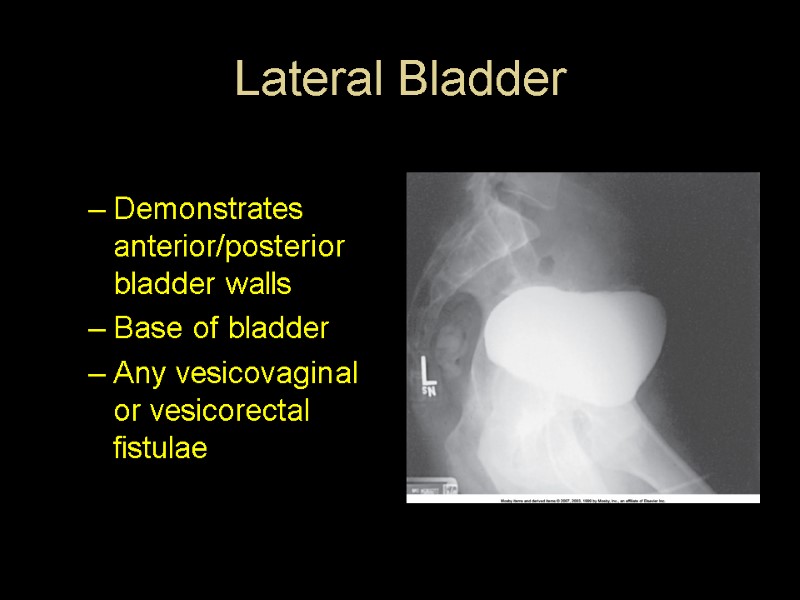 Lateral Bladder Demonstrates anterior/posterior bladder walls Base of bladder Any vesicovaginal or vesicorectal fistulae
Lateral Bladder Demonstrates anterior/posterior bladder walls Base of bladder Any vesicovaginal or vesicorectal fistulae

 Cystourethrography
Cystourethrography
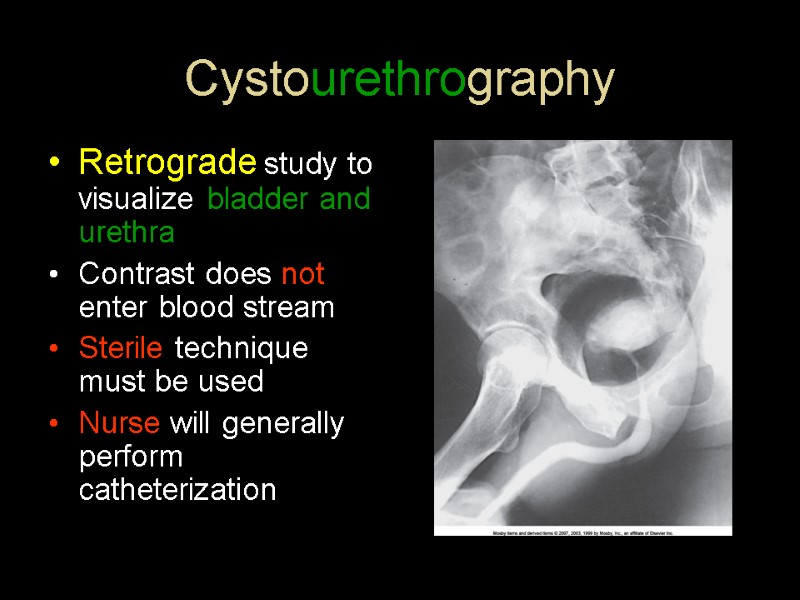
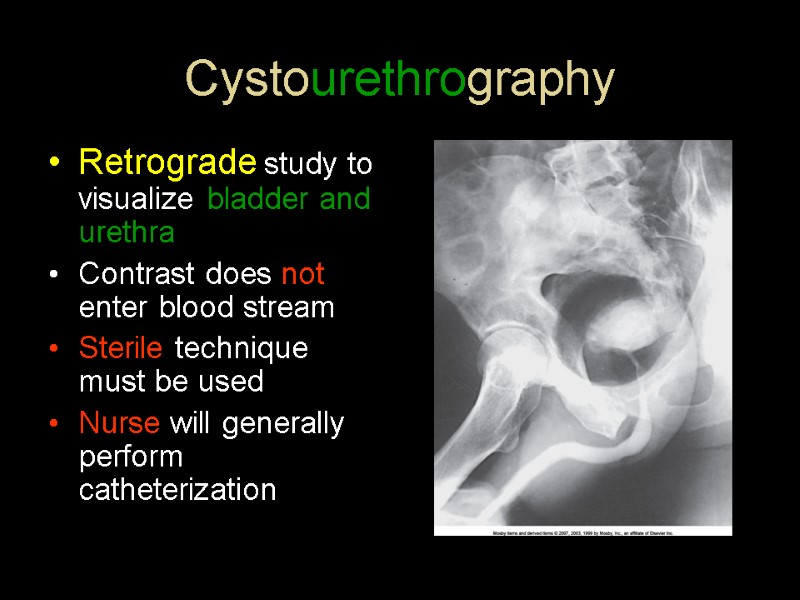 Cystourethrography Retrograde study to visualize bladder and urethra Contrast does not enter blood stream Sterile technique must be used Nurse will generally perform catheterization
Cystourethrography Retrograde study to visualize bladder and urethra Contrast does not enter blood stream Sterile technique must be used Nurse will generally perform catheterization
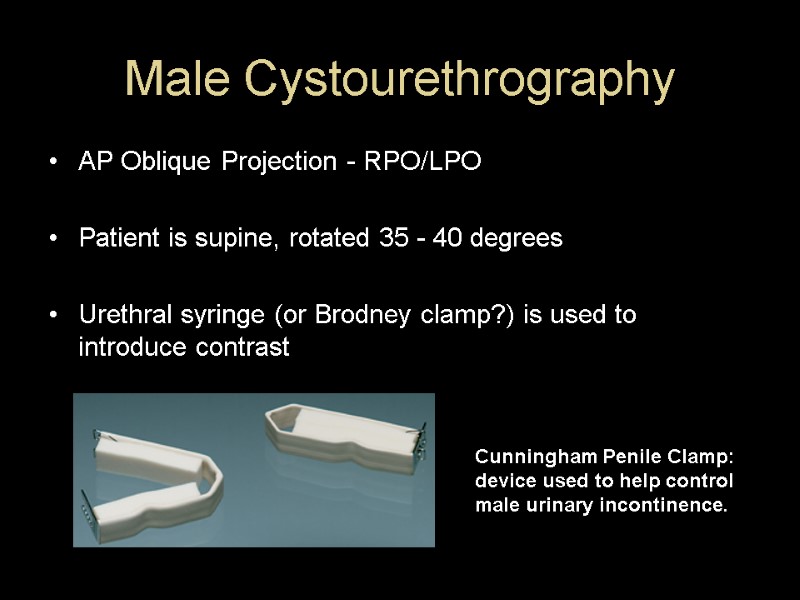
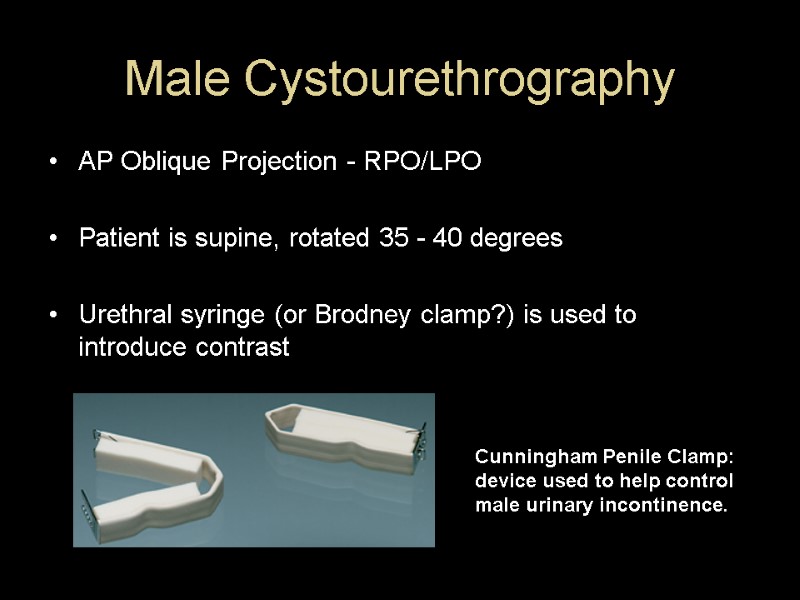 Male Cystourethrography AP Oblique Projection - RPO/LPO Patient is supine, rotated 35 - 40 degrees Urethral syringe (or Brodney clamp?) is used to introduce contrast Cunningham Penile Clamp: device used to help control male urinary incontinence.
Male Cystourethrography AP Oblique Projection - RPO/LPO Patient is supine, rotated 35 - 40 degrees Urethral syringe (or Brodney clamp?) is used to introduce contrast Cunningham Penile Clamp: device used to help control male urinary incontinence.
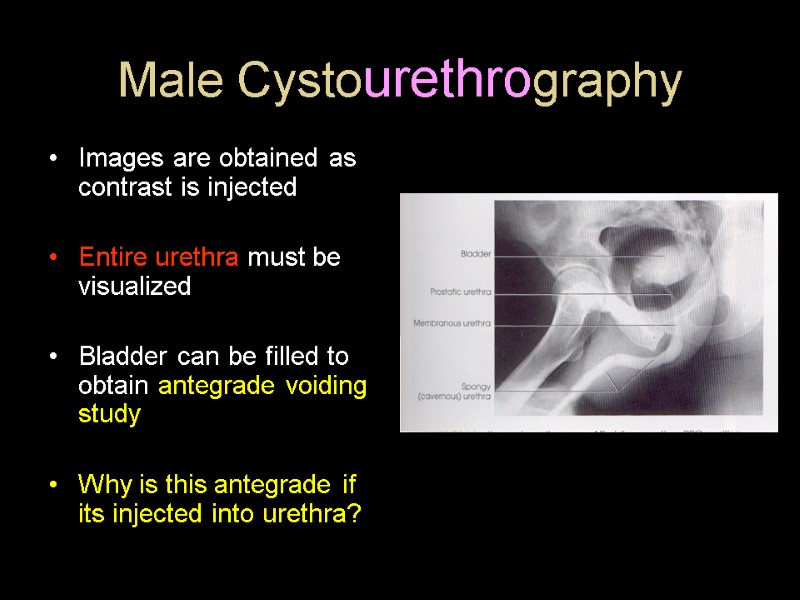
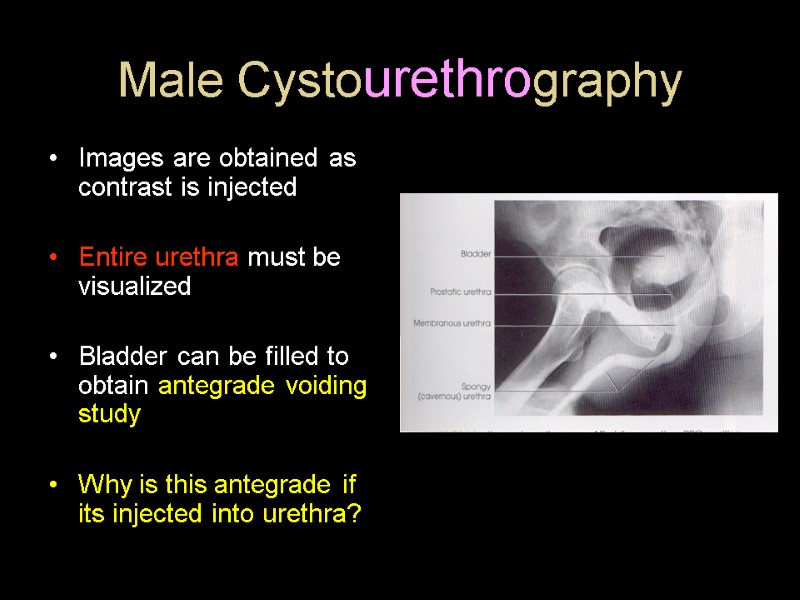 Male Cystourethrography Images are obtained as contrast is injected Entire urethra must be visualized Bladder can be filled to obtain antegrade voiding study Why is this antegrade if its injected into urethra?
Male Cystourethrography Images are obtained as contrast is injected Entire urethra must be visualized Bladder can be filled to obtain antegrade voiding study Why is this antegrade if its injected into urethra?
 Female Cystourethrography Retrograde AP Projection (maybe obliques) Bladder can be filled and patient void for antegrade studies Cassette should be centered as for cystography Abduct thighs to prevent superimposition of bone or soft tissue
Female Cystourethrography Retrograde AP Projection (maybe obliques) Bladder can be filled and patient void for antegrade studies Cassette should be centered as for cystography Abduct thighs to prevent superimposition of bone or soft tissue
 Incontinence Studies Positioning is same as retrograde cystography On lateral films, pt. asked to strain to demonstrate any prolapse or incontinence
Incontinence Studies Positioning is same as retrograde cystography On lateral films, pt. asked to strain to demonstrate any prolapse or incontinence
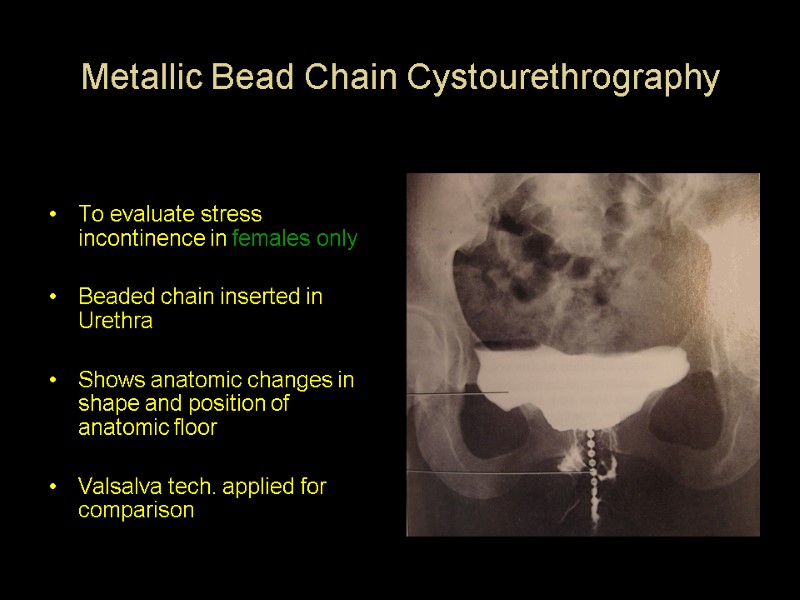
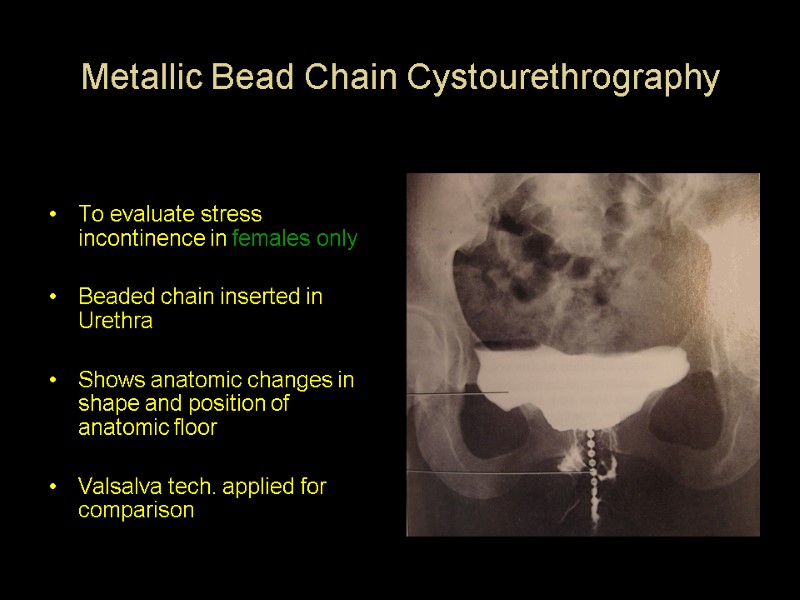 Metallic Bead Chain Cystourethrography To evaluate stress incontinence in females only Beaded chain inserted in Urethra Shows anatomic changes in shape and position of anatomic floor Valsalva tech. applied for comparison
Metallic Bead Chain Cystourethrography To evaluate stress incontinence in females only Beaded chain inserted in Urethra Shows anatomic changes in shape and position of anatomic floor Valsalva tech. applied for comparison
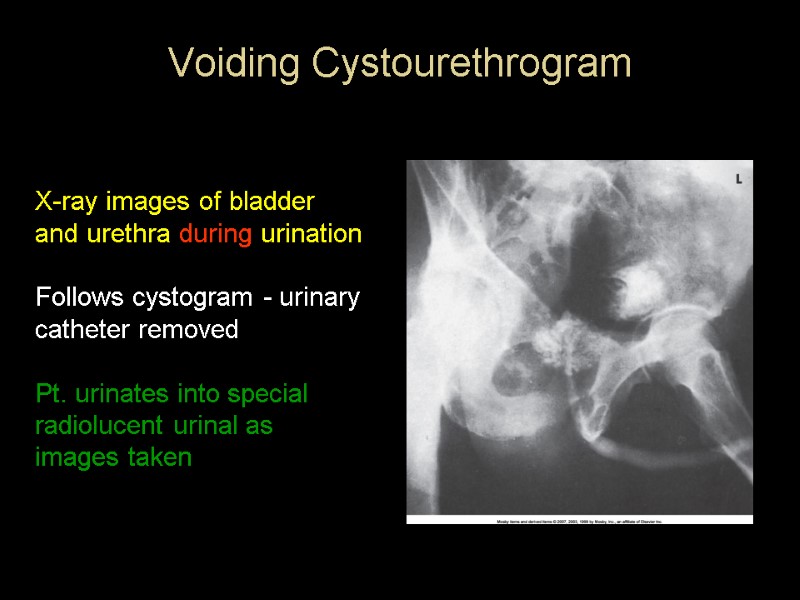
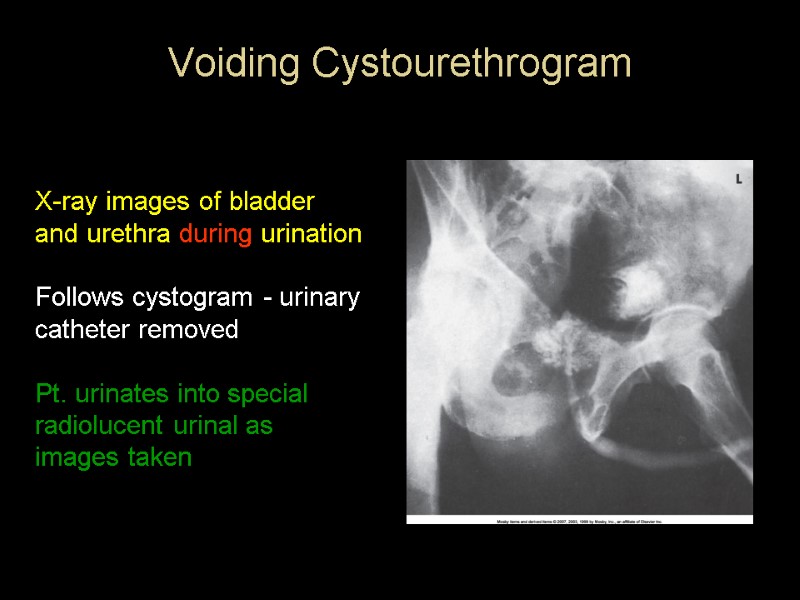 Voiding Cystourethrogram X-ray images of bladder and urethra during urination Follows cystogram - urinary catheter removed Pt. urinates into special radiolucent urinal as images taken .
Voiding Cystourethrogram X-ray images of bladder and urethra during urination Follows cystogram - urinary catheter removed Pt. urinates into special radiolucent urinal as images taken .
 Voiding Cystourethrogram cont’d Shows size and shape of bladder under stress caused by urination Demonstrates urethra functioning Most commonly used for young girls with history of recurrent bladder infections
Voiding Cystourethrogram cont’d Shows size and shape of bladder under stress caused by urination Demonstrates urethra functioning Most commonly used for young girls with history of recurrent bladder infections
 The End
The End

