21ab8920282c8db711998ea3177c84f0.ppt
- Количество слайдов: 80
 The Urinary System Assessment & Disorders 1
The Urinary System Assessment & Disorders 1
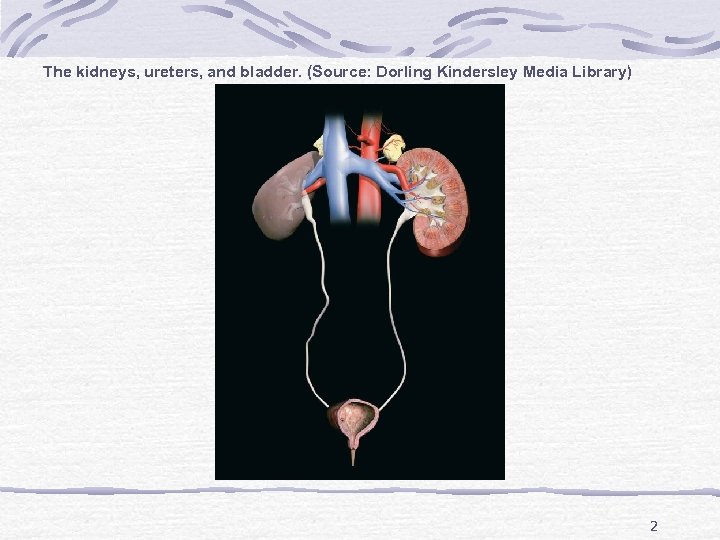 The kidneys, ureters, and bladder. (Source: Dorling Kindersley Media Library) 2
The kidneys, ureters, and bladder. (Source: Dorling Kindersley Media Library) 2
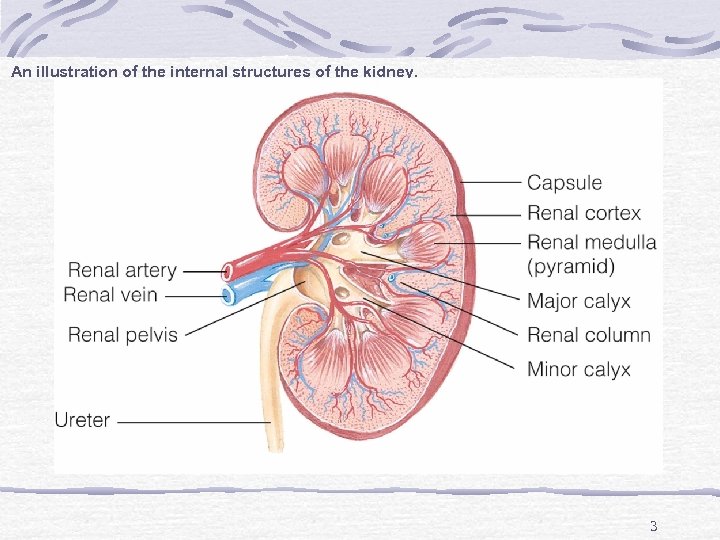 An illustration of the internal structures of the kidney. 3
An illustration of the internal structures of the kidney. 3
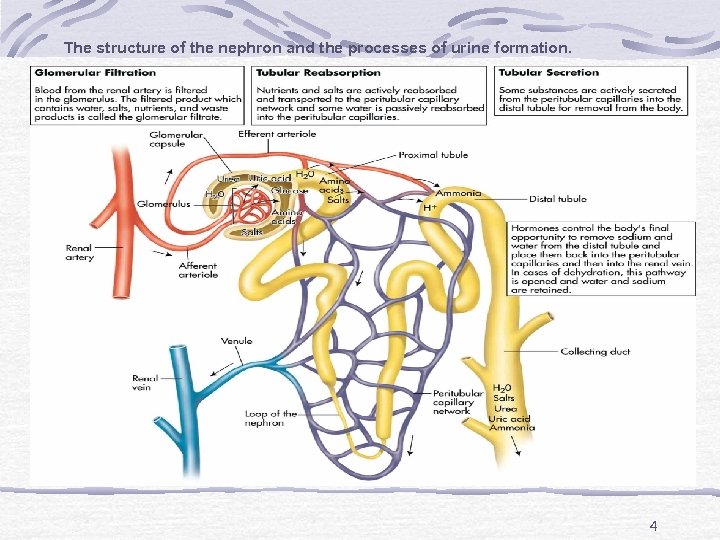 The structure of the nephron and the processes of urine formation. 4
The structure of the nephron and the processes of urine formation. 4
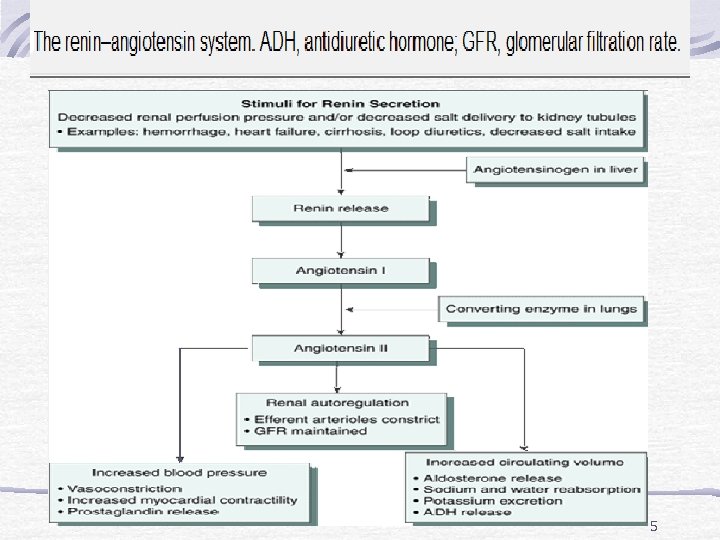 5
5
 Age-Related Changes Nephrons lost with aging Reduces kidney mass and GFR Less urine concentration Risk for dehydration 6
Age-Related Changes Nephrons lost with aging Reduces kidney mass and GFR Less urine concentration Risk for dehydration 6
 Assessment Use simple language Assess for incontinence (esp. muliparous) Family history Chief concern Location and character of pain Previous UTI, stones, urinary problems Pattern or urination 7
Assessment Use simple language Assess for incontinence (esp. muliparous) Family history Chief concern Location and character of pain Previous UTI, stones, urinary problems Pattern or urination 7
 Assessment Color, clarity, amount of urine Difficulty initiating urination or changes in stream Changes in urinary pattern Dysuria, nocturia, hematuria, pyuria 8
Assessment Color, clarity, amount of urine Difficulty initiating urination or changes in stream Changes in urinary pattern Dysuria, nocturia, hematuria, pyuria 8
 Assessment History of urinary problems Urinary or abdominal surgeries Smoking, alcohol use Chance of pregnancy History of diabetes or other endocrine disorders Unexplained anemia 9
Assessment History of urinary problems Urinary or abdominal surgeries Smoking, alcohol use Chance of pregnancy History of diabetes or other endocrine disorders Unexplained anemia 9
 Diagnostic Tests Clean-catch urine 24 -hour urine collection Culture and sensitivity BUN, creatinine and creatinine clearance = {Vol. of urine (ML/hr) x urine creatine}/serum creatinine IVP, Retrograde Pyelography 10
Diagnostic Tests Clean-catch urine 24 -hour urine collection Culture and sensitivity BUN, creatinine and creatinine clearance = {Vol. of urine (ML/hr) x urine creatine}/serum creatinine IVP, Retrograde Pyelography 10
 Diagnostic Tests Cystography, voiding cystogram CT scan, MRI Renal scan Ultrasound X-ray (KUB) Cystoscopy Renal Angiography Kidney biopsy (by needle or open procedure) 11
Diagnostic Tests Cystography, voiding cystogram CT scan, MRI Renal scan Ultrasound X-ray (KUB) Cystoscopy Renal Angiography Kidney biopsy (by needle or open procedure) 11
 Glomerulonephritis Inflammatory condition of glomerulus Antigen–antibody complexes form in the blood and become trapped in the glomerular capillaries, inducing an inflammatory response. Damages capillary membrane Blood cells and proteins escape into filtrate Hematuria, proteinuria, azotemia (increase BUN & Creatinin) 12
Glomerulonephritis Inflammatory condition of glomerulus Antigen–antibody complexes form in the blood and become trapped in the glomerular capillaries, inducing an inflammatory response. Damages capillary membrane Blood cells and proteins escape into filtrate Hematuria, proteinuria, azotemia (increase BUN & Creatinin) 12
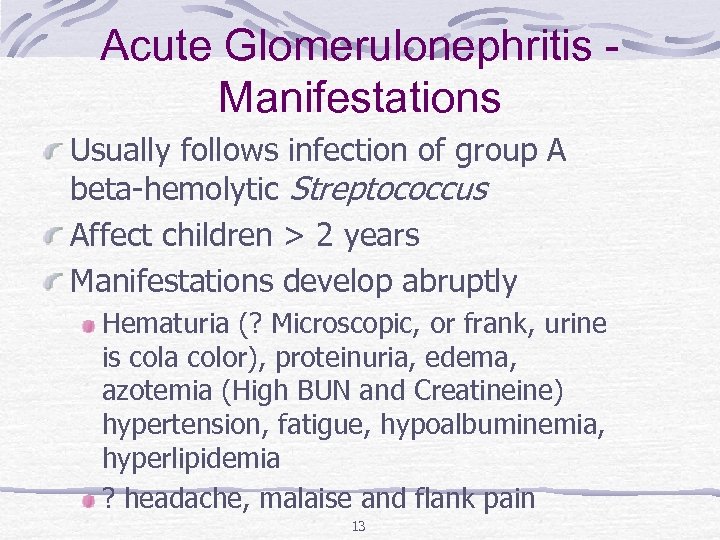 Acute Glomerulonephritis Manifestations Usually follows infection of group A beta-hemolytic Streptococcus Affect children > 2 years Manifestations develop abruptly Hematuria (? Microscopic, or frank, urine is cola color), proteinuria, edema, azotemia (High BUN and Creatineine) hypertension, fatigue, hypoalbuminemia, hyperlipidemia ? headache, malaise and flank pain 13
Acute Glomerulonephritis Manifestations Usually follows infection of group A beta-hemolytic Streptococcus Affect children > 2 years Manifestations develop abruptly Hematuria (? Microscopic, or frank, urine is cola color), proteinuria, edema, azotemia (High BUN and Creatineine) hypertension, fatigue, hypoalbuminemia, hyperlipidemia ? headache, malaise and flank pain 13
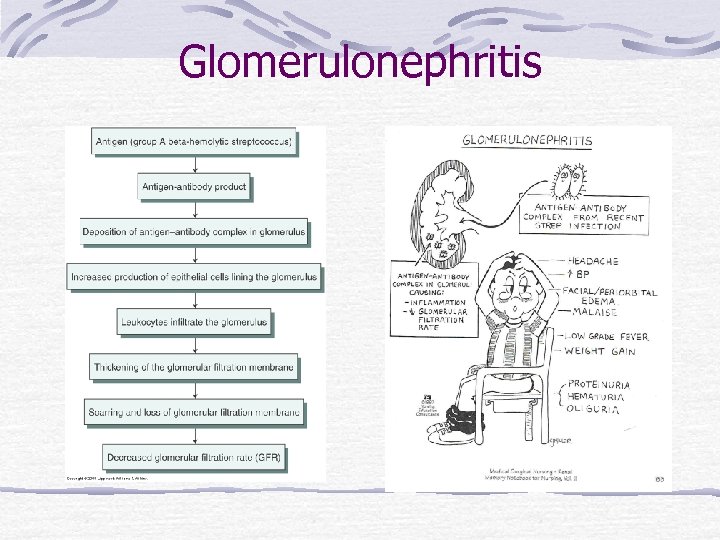 Glomerulonephritis
Glomerulonephritis
 Glomerulonephritis – Diagnostic Tests ASO titer (anti streptolysine O) BUN Serum creatinine Serum electrolytes Urinalysis KUB x-ray Kidney scan or biopsy 15
Glomerulonephritis – Diagnostic Tests ASO titer (anti streptolysine O) BUN Serum creatinine Serum electrolytes Urinalysis KUB x-ray Kidney scan or biopsy 15
 Complications of acute glomerulonephritis Hypertensive encephalopathy, Heart failure, Pulmonary edema, Without treatment, end-stage renal disease (ESRD) develops in a matter of weeks or months. 16
Complications of acute glomerulonephritis Hypertensive encephalopathy, Heart failure, Pulmonary edema, Without treatment, end-stage renal disease (ESRD) develops in a matter of weeks or months. 16
 Glomerulonephritis – Treatment Focus is on identifying and treating underlying disease process and preserving kidney function If residual streptococcal infection is suspected, penicillin. Corticosteroids and immunosuppressant medications may be prescribed for patients with rapidly progressive acute glomerulonephritis. 17
Glomerulonephritis – Treatment Focus is on identifying and treating underlying disease process and preserving kidney function If residual streptococcal infection is suspected, penicillin. Corticosteroids and immunosuppressant medications may be prescribed for patients with rapidly progressive acute glomerulonephritis. 17
 Glomerulonephritis – Treatment Dietary protein is restricted when renal insufficiency (elevated BUN) develop. Sodium is restricted when the patient has hypertension, edema, and heart failure. Loop diuretic and antihypertensive medications may be prescribed to control hypertension. Bed rest during acute phase. 18
Glomerulonephritis – Treatment Dietary protein is restricted when renal insufficiency (elevated BUN) develop. Sodium is restricted when the patient has hypertension, edema, and heart failure. Loop diuretic and antihypertensive medications may be prescribed to control hypertension. Bed rest during acute phase. 18
 Glomerulonephritis – Nursing Care Decrease protein and increase CHO to prevent protein breakdown. Accurate I & O (consider insensible loss) 19
Glomerulonephritis – Nursing Care Decrease protein and increase CHO to prevent protein breakdown. Accurate I & O (consider insensible loss) 19
 Chronic Glomerulonephritis Could be due to repeated episodes of acute glomerulonephritis, hypertensive nephrosclerosis, hyperlipidemia, glomerular sclerosis Other causes include SLE, DM Kidney size reduce to 1/5 th of original size and many scar tissue formed leading to ESRF. 20
Chronic Glomerulonephritis Could be due to repeated episodes of acute glomerulonephritis, hypertensive nephrosclerosis, hyperlipidemia, glomerular sclerosis Other causes include SLE, DM Kidney size reduce to 1/5 th of original size and many scar tissue formed leading to ESRF. 20
 Chronic Glomerulonephritis/ S&S Many are asymptomatic ? Discovered when patient diagnosed with Hypertension. ? severe nosebleed, a stroke, or a seizure, swollen feet at night. Heneral symptoms, such as loss of weight and strength, increasing irritability, nocturia, Headaches, dizziness, and digestive disturbances. Finally, S&S of renal failure. 21
Chronic Glomerulonephritis/ S&S Many are asymptomatic ? Discovered when patient diagnosed with Hypertension. ? severe nosebleed, a stroke, or a seizure, swollen feet at night. Heneral symptoms, such as loss of weight and strength, increasing irritability, nocturia, Headaches, dizziness, and digestive disturbances. Finally, S&S of renal failure. 21
 Medical Management Control BP: Na & water restriction, antihypertensive drug Monitor weight. Diuretics. Adequate CHO diet to spare protien Treat UTI ? Dialysis. 22
Medical Management Control BP: Na & water restriction, antihypertensive drug Monitor weight. Diuretics. Adequate CHO diet to spare protien Treat UTI ? Dialysis. 22
 Nephrotic Syndrome Is a cluster of clinical findings, including: Marked increase in protein (particularly albumin) in the urine (proteinuria) 2. Decrease in albumin in the blood (hypoalbuminemia) 3. Edema (periorbital, ascites, and dependent edema) 4. High serum cholesterol and low-density lipoproteins (hyperlipidemia) 1. 23
Nephrotic Syndrome Is a cluster of clinical findings, including: Marked increase in protein (particularly albumin) in the urine (proteinuria) 2. Decrease in albumin in the blood (hypoalbuminemia) 3. Edema (periorbital, ascites, and dependent edema) 4. High serum cholesterol and low-density lipoproteins (hyperlipidemia) 1. 23
 Treatment Diuretics (be careful not to cause sever hypovolemia as it may lead to ARF) Loop diuretics + ACE inhibitors lead to decreasing protienuria. Immunosuppresive agents (i. e. cytoxan). Coriticosteroids. Restrict protein and sodium. 24
Treatment Diuretics (be careful not to cause sever hypovolemia as it may lead to ARF) Loop diuretics + ACE inhibitors lead to decreasing protienuria. Immunosuppresive agents (i. e. cytoxan). Coriticosteroids. Restrict protein and sodium. 24
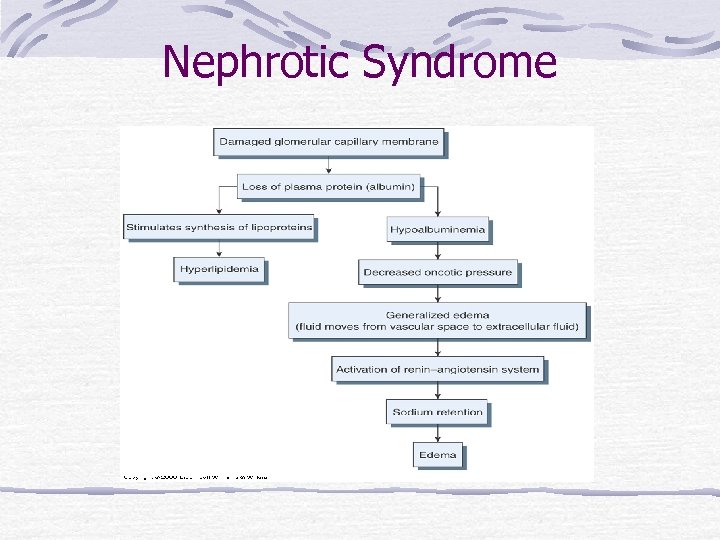 Nephrotic Syndrome
Nephrotic Syndrome
 Acute Renal Failure (ARF) Is a reversible clinical syndrome where there is a sudden and almost complete loss of kidney function (decreased GFR) over a period of hours to days with failure to excrete nitrogenous waste products and to maintain fluid and electrolyte homeostasis May progress to end stage renal disease, uremic syndrome, and death without treatment 26
Acute Renal Failure (ARF) Is a reversible clinical syndrome where there is a sudden and almost complete loss of kidney function (decreased GFR) over a period of hours to days with failure to excrete nitrogenous waste products and to maintain fluid and electrolyte homeostasis May progress to end stage renal disease, uremic syndrome, and death without treatment 26
 Acute Renal Failure Persons at Risks Major surgery Major trauma Receiving nephrotoxic medications Elderly ARF mostly occur within hospital settings 27
Acute Renal Failure Persons at Risks Major surgery Major trauma Receiving nephrotoxic medications Elderly ARF mostly occur within hospital settings 27
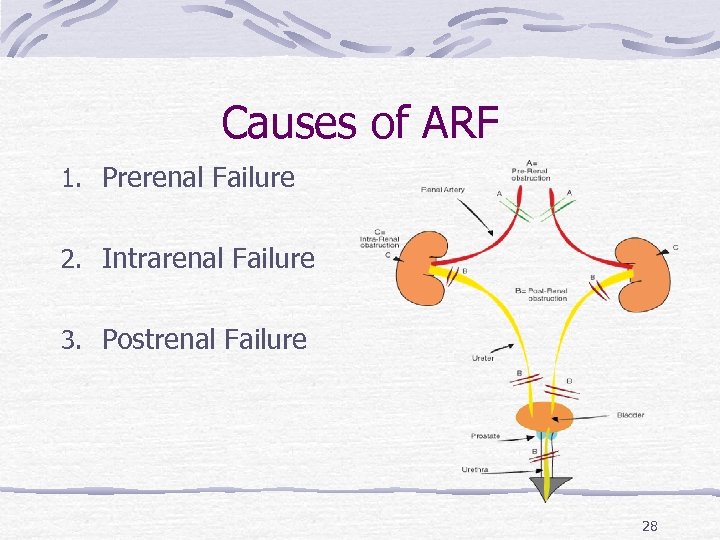 Causes of ARF 1. Prerenal Failure 2. Intrarenal Failure 3. Postrenal Failure 28
Causes of ARF 1. Prerenal Failure 2. Intrarenal Failure 3. Postrenal Failure 28
 Prerenal Failure Volume depletion resulting from: Hemorrhage Renal losses (diuretics, osmotic diuresis) Gastrointestinal losses (vomiting, diarrhea, nasogastric suction) Impaired cardiac efficiency resulting from: Myocardial infarction Heart failure Dysrhythmias Cardiogenic shock 29
Prerenal Failure Volume depletion resulting from: Hemorrhage Renal losses (diuretics, osmotic diuresis) Gastrointestinal losses (vomiting, diarrhea, nasogastric suction) Impaired cardiac efficiency resulting from: Myocardial infarction Heart failure Dysrhythmias Cardiogenic shock 29
 Prerenal Failure Vasodilation resulting from: Sepsis Anaphylaxis Antihypertensive medications or other medications that cause vasodilation 30
Prerenal Failure Vasodilation resulting from: Sepsis Anaphylaxis Antihypertensive medications or other medications that cause vasodilation 30
 Intrarenal Failure Prolonged renal ischemia resulting from: Pigment nephropathy (associated with the break -down of blood cells containing pigments that in turn occlude kidney structures) Myoglobinuria (trauma, crush injuries, burns) Hemoglobinuria (transfusion reaction, hemolytic anemia) 31
Intrarenal Failure Prolonged renal ischemia resulting from: Pigment nephropathy (associated with the break -down of blood cells containing pigments that in turn occlude kidney structures) Myoglobinuria (trauma, crush injuries, burns) Hemoglobinuria (transfusion reaction, hemolytic anemia) 31
 Intrarenal Failure Nephrotoxic agents such as: Aminoglycoside antibiotics (gentamicin, tobramycin, amicacin) Radiopaque contrast agents Heavy metals (lead, mercury) Solvents and chemicals (ethylene glycol, carbon tetrachloride, arsenic) Nonsteroidal anti-inflammatory drugs (NSAIDs) Angiotensin-converting enzyme inhibitors (ACE inhibitors) 32
Intrarenal Failure Nephrotoxic agents such as: Aminoglycoside antibiotics (gentamicin, tobramycin, amicacin) Radiopaque contrast agents Heavy metals (lead, mercury) Solvents and chemicals (ethylene glycol, carbon tetrachloride, arsenic) Nonsteroidal anti-inflammatory drugs (NSAIDs) Angiotensin-converting enzyme inhibitors (ACE inhibitors) 32
 Intrarenal Failure Infectious processes such as: Acute pyelonephritis Acute glomerulonephritis 33
Intrarenal Failure Infectious processes such as: Acute pyelonephritis Acute glomerulonephritis 33
 Postrenal failure Urinary tract obstruction, including: Calculi (stones) Tumors Benign prostatic hyperplasia Strictures Blood clots 34
Postrenal failure Urinary tract obstruction, including: Calculi (stones) Tumors Benign prostatic hyperplasia Strictures Blood clots 34
 Phases of Acute Renal Failure Initiation period: begins with the initial insult and ends when oliguria develops. Oliguria period: UOP < 400 ml/day, increase in urea, creatinine, uric acid, K & magnesium. Some people have normal urine output (2 L/d) Diuretic – UOP ^ to as much as 4000 m. L/d but BUN & Cretinine still high, at end of this stage may begin to see improvement Recovery – things go back to normal. It may take up to 3 -12 months 35
Phases of Acute Renal Failure Initiation period: begins with the initial insult and ends when oliguria develops. Oliguria period: UOP < 400 ml/day, increase in urea, creatinine, uric acid, K & magnesium. Some people have normal urine output (2 L/d) Diuretic – UOP ^ to as much as 4000 m. L/d but BUN & Cretinine still high, at end of this stage may begin to see improvement Recovery – things go back to normal. It may take up to 3 -12 months 35
 Acute Renal Failure S & S The patient may appear critically ill and lethargic. The skin and mucous membranes are dry from dehydration. Central nervous system signs and symptoms include drowsiness, headache, muscle twitching, and seizures. Urine output varies (scanty to normal volume), ? hematuria & urine has a low specific gravity 36
Acute Renal Failure S & S The patient may appear critically ill and lethargic. The skin and mucous membranes are dry from dehydration. Central nervous system signs and symptoms include drowsiness, headache, muscle twitching, and seizures. Urine output varies (scanty to normal volume), ? hematuria & urine has a low specific gravity 36
 Acute Renal Failure Diagnostic tests BUN, creatinine, potassium increase. p. H Hgb and Hct Urine studies US of kidneys High phosphorus and low calcium. 37
Acute Renal Failure Diagnostic tests BUN, creatinine, potassium increase. p. H Hgb and Hct Urine studies US of kidneys High phosphorus and low calcium. 37
 Prevention of ARF Provide adequate hydration Prevent and treat shock promptly Hourly urine output for critical patients Continuosally assess renal function Prevent and treat infections promptly Monitor for effects of toxic drugs 38
Prevention of ARF Provide adequate hydration Prevent and treat shock promptly Hourly urine output for critical patients Continuosally assess renal function Prevent and treat infections promptly Monitor for effects of toxic drugs 38
 Medical treatment of ARF Objectives of treatment are to restore normal chemical balance and prevent complications until repair of renal tissue and restoration of renal function can occur. Management includes maintaining fluid balance, avoiding fluid excesses, or possibly performing dialysis. 39
Medical treatment of ARF Objectives of treatment are to restore normal chemical balance and prevent complications until repair of renal tissue and restoration of renal function can occur. Management includes maintaining fluid balance, avoiding fluid excesses, or possibly performing dialysis. 39
 Acute Renal Failure Medical treatment Treat the cause Fluid and replacement or restrictions Monitor fluid overload Diuretics Maintain E-lytes May need dialysis (especially with high K) May need to stimulate production of urine with IV fluids, Dopomine, diuretics, etc. 40
Acute Renal Failure Medical treatment Treat the cause Fluid and replacement or restrictions Monitor fluid overload Diuretics Maintain E-lytes May need dialysis (especially with high K) May need to stimulate production of urine with IV fluids, Dopomine, diuretics, etc. 40
 Acute Renal Failure Medical treatment Hemodialysis Subclavian approach Femoral approach Peritoneal dialysis Nutritional Therapy ? Decrease Protein (according to BUN level) Increase CHO Decrease potassium and phosphrous 41
Acute Renal Failure Medical treatment Hemodialysis Subclavian approach Femoral approach Peritoneal dialysis Nutritional Therapy ? Decrease Protein (according to BUN level) Increase CHO Decrease potassium and phosphrous 41
 Acute Renal Failure Nursing Diagnosisimbalanced fluid volume= excess Altered electrolyte balance Impaired tissue perfusion: renal Anxiety Imbalanced nutrition Risk for infection Fatigue Knowledge deficit 42
Acute Renal Failure Nursing Diagnosisimbalanced fluid volume= excess Altered electrolyte balance Impaired tissue perfusion: renal Anxiety Imbalanced nutrition Risk for infection Fatigue Knowledge deficit 42
 Acute Renal Failure Plan. Promote recovery of optimal kidney function. Maintain normal fluid and electrolyte balance. Decrease anxiety. Increase knowledge. 43
Acute Renal Failure Plan. Promote recovery of optimal kidney function. Maintain normal fluid and electrolyte balance. Decrease anxiety. Increase knowledge. 43
 Nursing interventions Monitoring Fluid and Electrolyte Balance Reducing Metabolic Rate Promoting Pulmonary Function Preventing Infection Providing Skin Care 44
Nursing interventions Monitoring Fluid and Electrolyte Balance Reducing Metabolic Rate Promoting Pulmonary Function Preventing Infection Providing Skin Care 44
 Chronic Renal Failure Chronic renal failure, or ESRD, is a progressive, irreversible deterioration in renal function in which the body's ability to maintain metabolic and fluid and electrolyte balance fails, resulting in uremia or azotemia. Results from gradual, progressive loss of renal function Occasionally results from rapid progression of acute renal failure 45
Chronic Renal Failure Chronic renal failure, or ESRD, is a progressive, irreversible deterioration in renal function in which the body's ability to maintain metabolic and fluid and electrolyte balance fails, resulting in uremia or azotemia. Results from gradual, progressive loss of renal function Occasionally results from rapid progression of acute renal failure 45
 Chronic Renal Failure Conditions that cause ESRD include systemic diseases, such as diabetes mellitus (leading cause); hypertension; chronic glomerulonephritis; pyelonephritis; obstruction of the urinary tract; hereditary lesions, as in polycystic kidney disease; vascular disorders; infections; medications; or toxic agents. 46
Chronic Renal Failure Conditions that cause ESRD include systemic diseases, such as diabetes mellitus (leading cause); hypertension; chronic glomerulonephritis; pyelonephritis; obstruction of the urinary tract; hereditary lesions, as in polycystic kidney disease; vascular disorders; infections; medications; or toxic agents. 46
 Chronic Renal Failure Symptoms occur when 75% of function is lost but considered chronic if 90 -95% loss of function Dialysis is necessary D/T accumulation of uremic toxins, which produce changes in major organs 47
Chronic Renal Failure Symptoms occur when 75% of function is lost but considered chronic if 90 -95% loss of function Dialysis is necessary D/T accumulation of uremic toxins, which produce changes in major organs 47
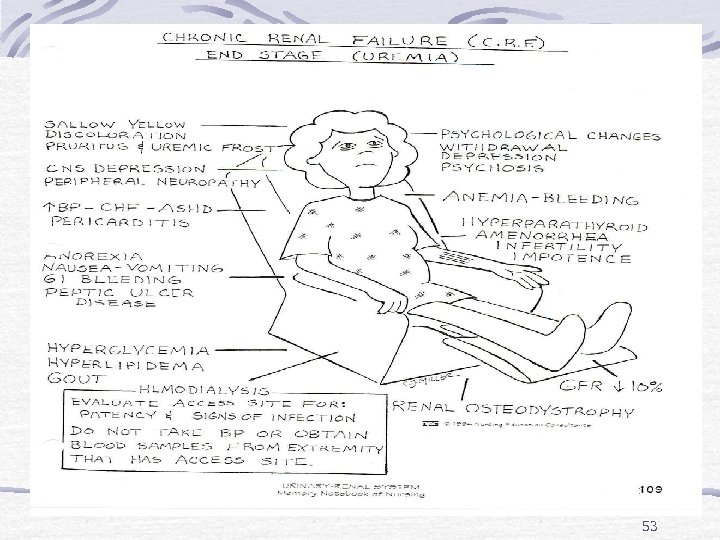
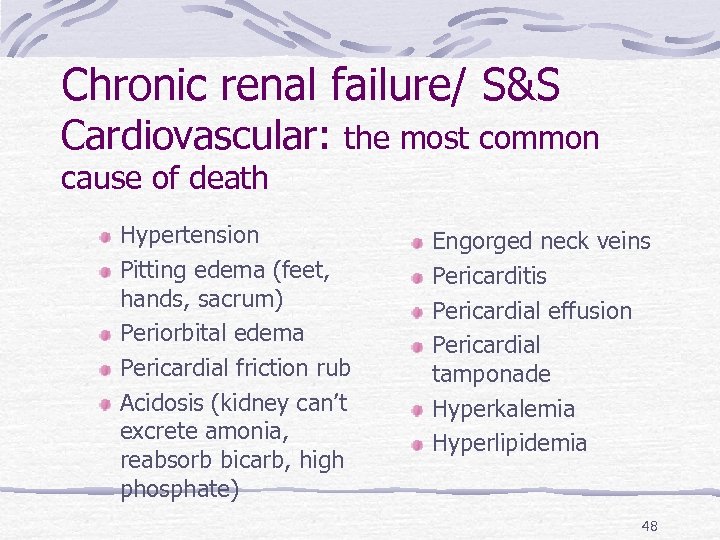 Chronic renal failure/ S&S Cardiovascular: the most common cause of death Hypertension Pitting edema (feet, hands, sacrum) Periorbital edema Pericardial friction rub Acidosis (kidney can’t excrete amonia, reabsorb bicarb, high phosphate) Engorged neck veins Pericarditis Pericardial effusion Pericardial tamponade Hyperkalemia Hyperlipidemia 48
Chronic renal failure/ S&S Cardiovascular: the most common cause of death Hypertension Pitting edema (feet, hands, sacrum) Periorbital edema Pericardial friction rub Acidosis (kidney can’t excrete amonia, reabsorb bicarb, high phosphate) Engorged neck veins Pericarditis Pericardial effusion Pericardial tamponade Hyperkalemia Hyperlipidemia 48
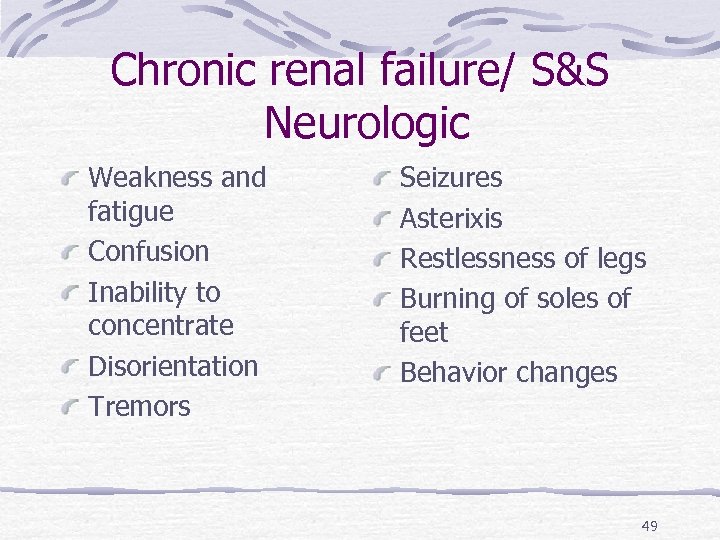 Chronic renal failure/ S&S Neurologic Weakness and fatigue Confusion Inability to concentrate Disorientation Tremors Seizures Asterixis Restlessness of legs Burning of soles of feet Behavior changes 49
Chronic renal failure/ S&S Neurologic Weakness and fatigue Confusion Inability to concentrate Disorientation Tremors Seizures Asterixis Restlessness of legs Burning of soles of feet Behavior changes 49
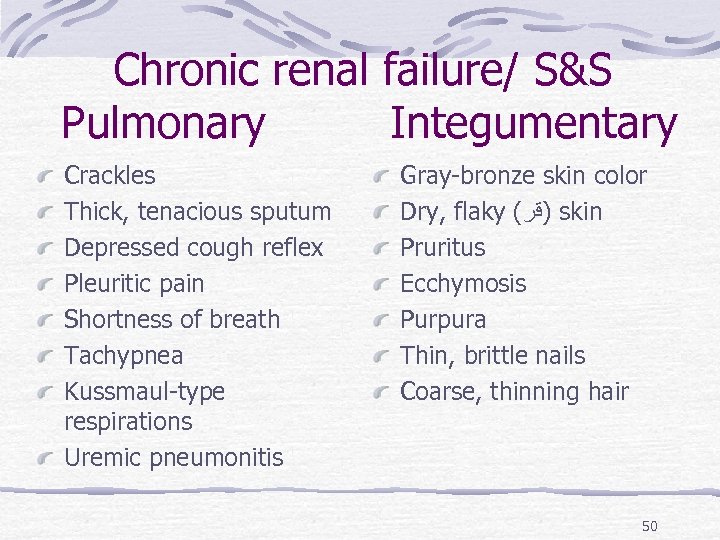 Chronic renal failure/ S&S Pulmonary Integumentary Crackles Thick, tenacious sputum Depressed cough reflex Pleuritic pain Shortness of breath Tachypnea Kussmaul-type respirations Uremic pneumonitis Gray-bronze skin color Dry, flaky ( )ﻗﺭ skin Pruritus Ecchymosis Purpura Thin, brittle nails Coarse, thinning hair 50
Chronic renal failure/ S&S Pulmonary Integumentary Crackles Thick, tenacious sputum Depressed cough reflex Pleuritic pain Shortness of breath Tachypnea Kussmaul-type respirations Uremic pneumonitis Gray-bronze skin color Dry, flaky ( )ﻗﺭ skin Pruritus Ecchymosis Purpura Thin, brittle nails Coarse, thinning hair 50
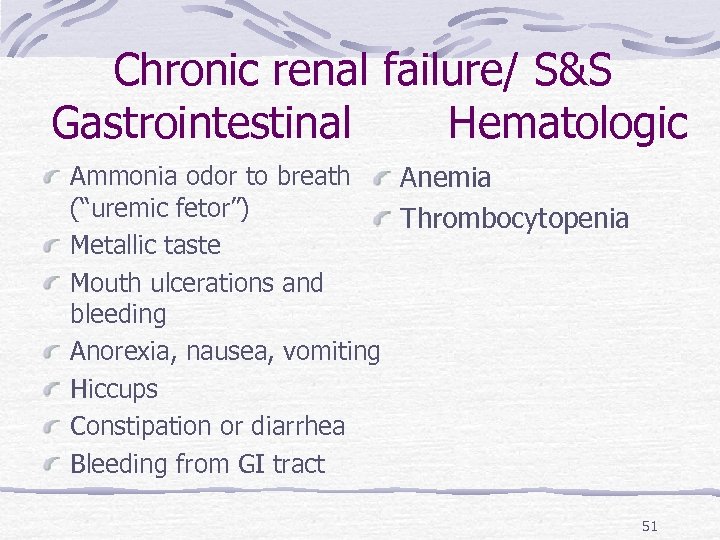 Chronic renal failure/ S&S Gastrointestinal Hematologic Ammonia odor to breath Anemia (“uremic fetor”) Thrombocytopenia Metallic taste Mouth ulcerations and bleeding Anorexia, nausea, vomiting Hiccups Constipation or diarrhea Bleeding from GI tract 51
Chronic renal failure/ S&S Gastrointestinal Hematologic Ammonia odor to breath Anemia (“uremic fetor”) Thrombocytopenia Metallic taste Mouth ulcerations and bleeding Anorexia, nausea, vomiting Hiccups Constipation or diarrhea Bleeding from GI tract 51
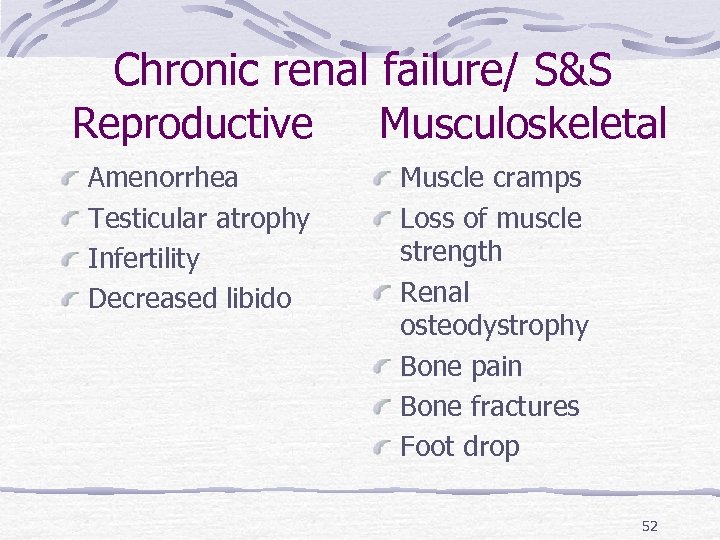 Chronic renal failure/ S&S Reproductive Musculoskeletal Amenorrhea Testicular atrophy Infertility Decreased libido Muscle cramps Loss of muscle strength Renal osteodystrophy Bone pain Bone fractures Foot drop 52
Chronic renal failure/ S&S Reproductive Musculoskeletal Amenorrhea Testicular atrophy Infertility Decreased libido Muscle cramps Loss of muscle strength Renal osteodystrophy Bone pain Bone fractures Foot drop 52
 53
53
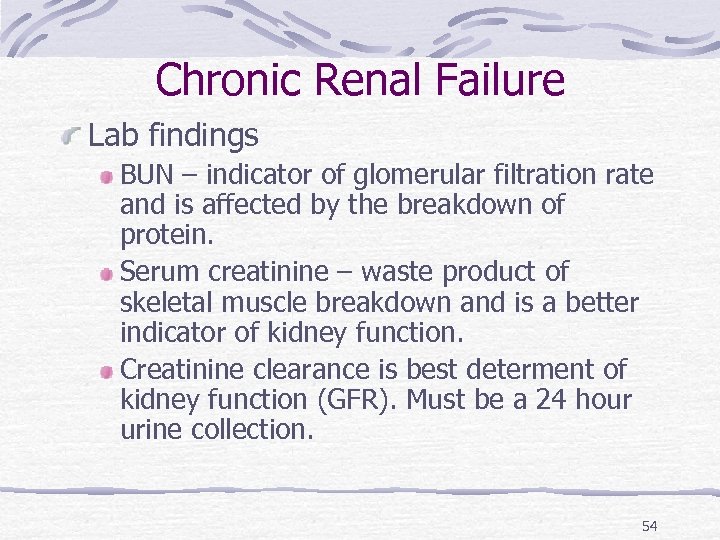 Chronic Renal Failure Lab findings BUN – indicator of glomerular filtration rate and is affected by the breakdown of protein. Serum creatinine – waste product of skeletal muscle breakdown and is a better indicator of kidney function. Creatinine clearance is best determent of kidney function (GFR). Must be a 24 hour urine collection. 54
Chronic Renal Failure Lab findings BUN – indicator of glomerular filtration rate and is affected by the breakdown of protein. Serum creatinine – waste product of skeletal muscle breakdown and is a better indicator of kidney function. Creatinine clearance is best determent of kidney function (GFR). Must be a 24 hour urine collection. 54
 Chronic Renal Failure K+ The kidneys are means which K+ is excreted. Normal is 3. 5 -5. 0 , m. Eq/L. maintains muscle contraction and is essential for cardiac function. Both elevated and decreased can cause problems with cardiac rhythm Hyperkalemia is treated with IV glucose and Na Bicarb which pushes K+ back into the cell Kayexalate (Sodium polystyrene sulfonate ) is also used to promote the exchange of sodium and potassium in the body. 55
Chronic Renal Failure K+ The kidneys are means which K+ is excreted. Normal is 3. 5 -5. 0 , m. Eq/L. maintains muscle contraction and is essential for cardiac function. Both elevated and decreased can cause problems with cardiac rhythm Hyperkalemia is treated with IV glucose and Na Bicarb which pushes K+ back into the cell Kayexalate (Sodium polystyrene sulfonate ) is also used to promote the exchange of sodium and potassium in the body. 55
 Chronic Renal Failure Ca With disease in the kidney, the enzyme for utilization of Vit D is absent Ca absorption depends upon Vit D Also, phosphate level increase leading to decreasing level of Ca Parathyroid hormone level increase in attempt to increase calcium, but because of the high phosphorus level, there is limited response. Body moves Ca out of the bone to compensate. Renal osteodystrophy is the end result Hypocalcemia = tetany 56
Chronic Renal Failure Ca With disease in the kidney, the enzyme for utilization of Vit D is absent Ca absorption depends upon Vit D Also, phosphate level increase leading to decreasing level of Ca Parathyroid hormone level increase in attempt to increase calcium, but because of the high phosphorus level, there is limited response. Body moves Ca out of the bone to compensate. Renal osteodystrophy is the end result Hypocalcemia = tetany 56
 Chronic Renal Failure Other abnormal findings Metabolic acidosis Fluid imbalance Insulin resistance Anemia Immunoligical problems 57
Chronic Renal Failure Other abnormal findings Metabolic acidosis Fluid imbalance Insulin resistance Anemia Immunoligical problems 57
 Complications Hyperkalemia Pericarditis, pericardial effusion, and pericardial tamponade Hypertension Anemia Bone disease and metastatic and vascular calcifications 58
Complications Hyperkalemia Pericarditis, pericardial effusion, and pericardial tamponade Hypertension Anemia Bone disease and metastatic and vascular calcifications 58
 Medical management Calcium carbonate, or calcium acetate: bind to phosphours and decrease its level. Antihypertensive and Cardiovascular Agents Antiseizure Agents Erythropoietin 59
Medical management Calcium carbonate, or calcium acetate: bind to phosphours and decrease its level. Antihypertensive and Cardiovascular Agents Antiseizure Agents Erythropoietin 59
 Nutritional Therapy Protein is restricted (allowed protein should be of high biologic value) Restrict fluid (500 -600 ml/day more than previous day’s urine output). Restrict K, Na, Phosphorus Increase CHO to meat caloric needs Vitamin suplements 60
Nutritional Therapy Protein is restricted (allowed protein should be of high biologic value) Restrict fluid (500 -600 ml/day more than previous day’s urine output). Restrict K, Na, Phosphorus Increase CHO to meat caloric needs Vitamin suplements 60
 Treatment Dialysis Transplantation 61
Treatment Dialysis Transplantation 61
 Chronic Renal Failure Nursing diagnosis Excess fluid volume related to decreased urine output, dietary excesses, and retention of sodium and water Imbalanced nutrition: less than body requirements related to anorexia, nausea and vomiting, dietary restrictions, and altered oral mucous membranes 62
Chronic Renal Failure Nursing diagnosis Excess fluid volume related to decreased urine output, dietary excesses, and retention of sodium and water Imbalanced nutrition: less than body requirements related to anorexia, nausea and vomiting, dietary restrictions, and altered oral mucous membranes 62
 Nursing diagnosis Deficient knowledge regarding condition and treatment regimen Activity intolerance related to fatigue, anemia, retention of waste products, and dialysis procedure Risk for situational low self-esteem related to dependency, role changes, changes in body image, and sexual dysfunction 63
Nursing diagnosis Deficient knowledge regarding condition and treatment regimen Activity intolerance related to fatigue, anemia, retention of waste products, and dialysis procedure Risk for situational low self-esteem related to dependency, role changes, changes in body image, and sexual dysfunction 63
 Chronic Renal Failure Nursing care : see world document 64
Chronic Renal Failure Nursing care : see world document 64
 Dialysis is used to remove fluid and uremic waste products from the body when the kidneys are unable to do so. Chronic: in ESRF when the kidney can’t remove waste products. Acute: high level of serum K+, fluid overload, or impending pulmonary edema, acidosis, to remove certain medications or other toxins from the blood. 65
Dialysis is used to remove fluid and uremic waste products from the body when the kidneys are unable to do so. Chronic: in ESRF when the kidney can’t remove waste products. Acute: high level of serum K+, fluid overload, or impending pulmonary edema, acidosis, to remove certain medications or other toxins from the blood. 65
 Dialysis ½ of patients with CRF eventually require dialysis Diffuse harmful waste out of body Control BP Keep safe level of chemicals in body 2 types Hemodialysis Peritoneal dialysis 66
Dialysis ½ of patients with CRF eventually require dialysis Diffuse harmful waste out of body Control BP Keep safe level of chemicals in body 2 types Hemodialysis Peritoneal dialysis 66
 Principles for dialysis Diffusion: toxins and wastes in the blood are removed Osmosis: excess water is removed from the blood Ultrafiltration: helps water to move faster under high pressure to an area of lower pressure 67
Principles for dialysis Diffusion: toxins and wastes in the blood are removed Osmosis: excess water is removed from the blood Ultrafiltration: helps water to move faster under high pressure to an area of lower pressure 67
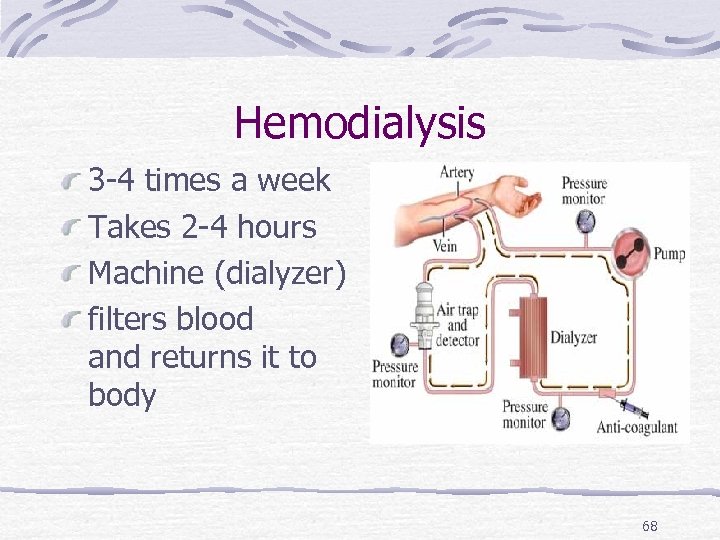 Hemodialysis 3 -4 times a week Takes 2 -4 hours Machine (dialyzer) filters blood and returns it to body 68
Hemodialysis 3 -4 times a week Takes 2 -4 hours Machine (dialyzer) filters blood and returns it to body 68
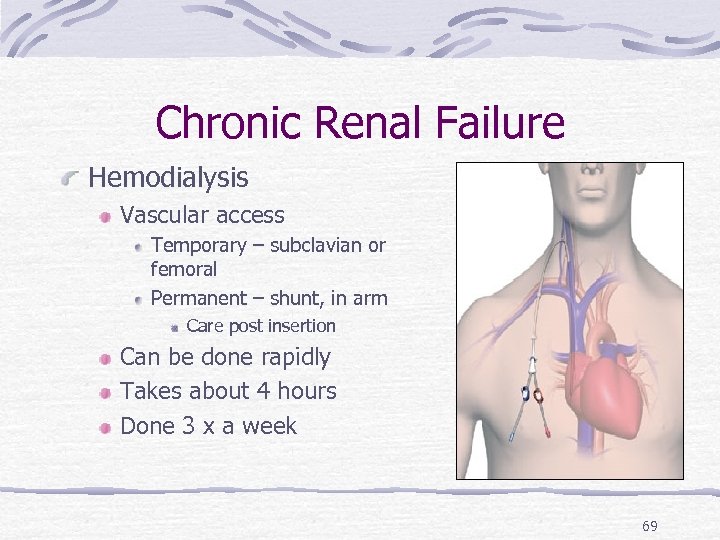 Chronic Renal Failure Hemodialysis Vascular access Temporary – subclavian or femoral Permanent – shunt, in arm Care post insertion Can be done rapidly Takes about 4 hours Done 3 x a week 69
Chronic Renal Failure Hemodialysis Vascular access Temporary – subclavian or femoral Permanent – shunt, in arm Care post insertion Can be done rapidly Takes about 4 hours Done 3 x a week 69
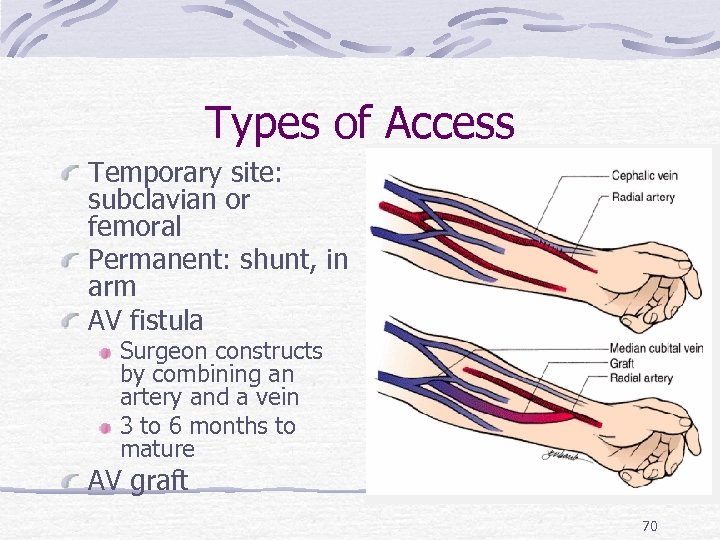 Types of Access Temporary site: subclavian or femoral Permanent: shunt, in arm AV fistula Surgeon constructs by combining an artery and a vein 3 to 6 months to mature AV graft 70
Types of Access Temporary site: subclavian or femoral Permanent: shunt, in arm AV fistula Surgeon constructs by combining an artery and a vein 3 to 6 months to mature AV graft 70
 What This Means For You No BP on same arm as fistula Protect arm from injury Never inject anything into catheter Control obvious hemorrhage Bleeding will be arterial Maintain direct pressure No IV on same arm as fistula A thrill will be felt – this is normal 71
What This Means For You No BP on same arm as fistula Protect arm from injury Never inject anything into catheter Control obvious hemorrhage Bleeding will be arterial Maintain direct pressure No IV on same arm as fistula A thrill will be felt – this is normal 71
 Complication of dialysis Hypotension Painful muscle cramping (due to rapid alterations in electrolyte balance) Dysrhythmias may result from electrolyte and p. H changes Air embolism Dialysis disequilibrium results from cerebral fluid shifts. 72
Complication of dialysis Hypotension Painful muscle cramping (due to rapid alterations in electrolyte balance) Dysrhythmias may result from electrolyte and p. H changes Air embolism Dialysis disequilibrium results from cerebral fluid shifts. 72
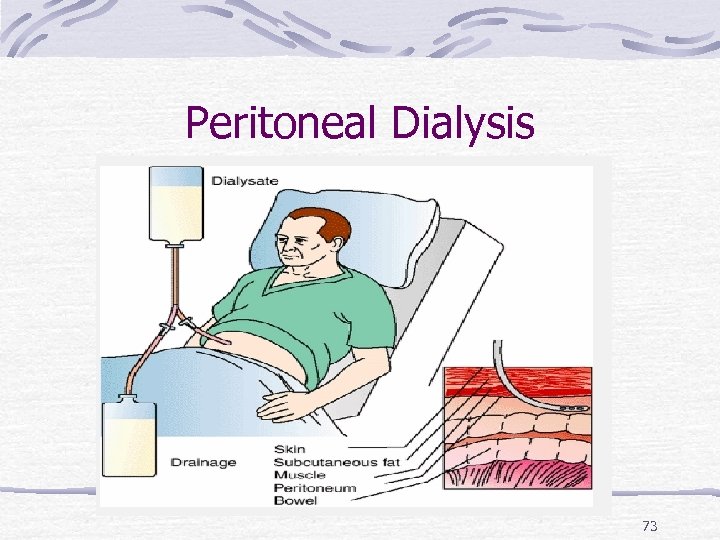 Peritoneal Dialysis 73
Peritoneal Dialysis 73
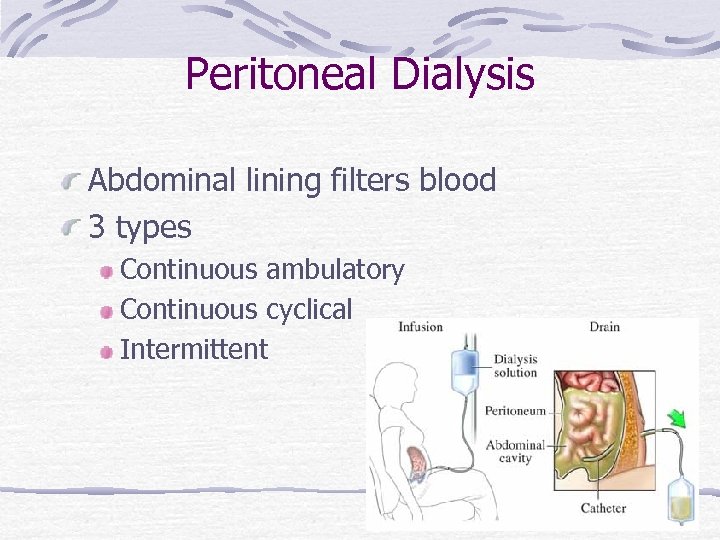 Peritoneal Dialysis Abdominal lining filters blood 3 types Continuous ambulatory Continuous cyclical Intermittent 74
Peritoneal Dialysis Abdominal lining filters blood 3 types Continuous ambulatory Continuous cyclical Intermittent 74
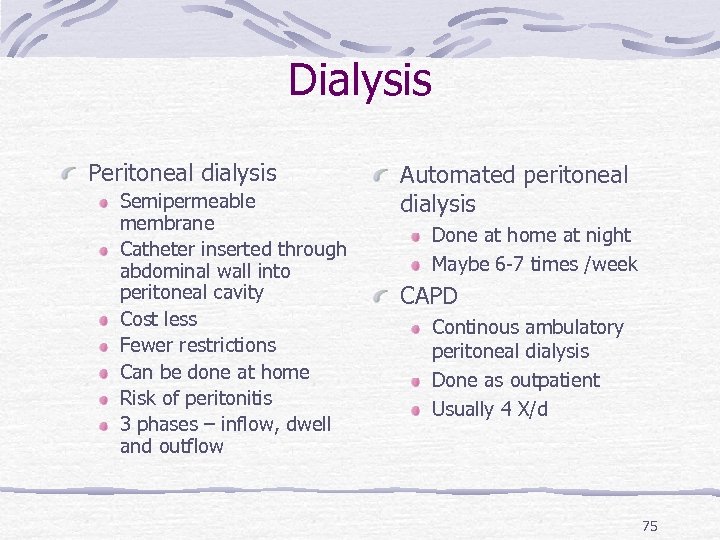 Dialysis Peritoneal dialysis Semipermeable membrane Catheter inserted through abdominal wall into peritoneal cavity Cost less Fewer restrictions Can be done at home Risk of peritonitis 3 phases – inflow, dwell and outflow Automated peritoneal dialysis Done at home at night Maybe 6 -7 times /week CAPD Continous ambulatory peritoneal dialysis Done as outpatient Usually 4 X/d 75
Dialysis Peritoneal dialysis Semipermeable membrane Catheter inserted through abdominal wall into peritoneal cavity Cost less Fewer restrictions Can be done at home Risk of peritonitis 3 phases – inflow, dwell and outflow Automated peritoneal dialysis Done at home at night Maybe 6 -7 times /week CAPD Continous ambulatory peritoneal dialysis Done as outpatient Usually 4 X/d 75
 Chronic Renal Failure Transplant Must find donor Waiting period long Good survival rate – 1 year 95 -97% Must take immunosuppressant’s for life Rejection Watch for fever, elevated B/P, and pain over site of new kidney 76
Chronic Renal Failure Transplant Must find donor Waiting period long Good survival rate – 1 year 95 -97% Must take immunosuppressant’s for life Rejection Watch for fever, elevated B/P, and pain over site of new kidney 76
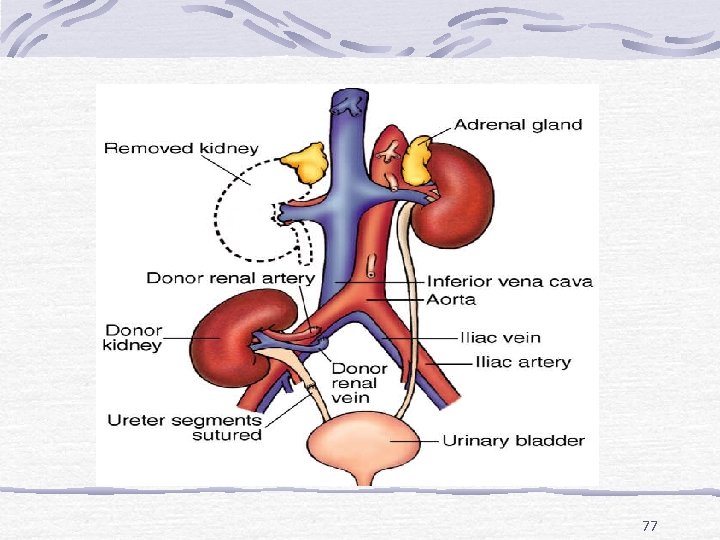 77
77
 Chronic Renal Failure Post op care ICU I/O B/P Weight changes Electrolytes May have fluid volume deficit High risk for infection 78
Chronic Renal Failure Post op care ICU I/O B/P Weight changes Electrolytes May have fluid volume deficit High risk for infection 78
 Transplant Meds Patients have decreased resistance to infection Corticosteroids – anti-inflammarory Deltosone Medrol Solu-Medrol Cytotoxic – inhibit T and B lymphocytes Imuran Cytoxan Cellcept T-cell depressors - Cyclosporin 79
Transplant Meds Patients have decreased resistance to infection Corticosteroids – anti-inflammarory Deltosone Medrol Solu-Medrol Cytotoxic – inhibit T and B lymphocytes Imuran Cytoxan Cellcept T-cell depressors - Cyclosporin 79
 Renal Trauma ? due to rib fractures or fractures vertebrae. 80% to 90% of all renal injuries are blunt injuries S & S: Pain, hematouria, S & S of shock Rx: Bed rest, antibiotics. In sever cases, need surgical repair or ? Nephrectomy. 80
Renal Trauma ? due to rib fractures or fractures vertebrae. 80% to 90% of all renal injuries are blunt injuries S & S: Pain, hematouria, S & S of shock Rx: Bed rest, antibiotics. In sever cases, need surgical repair or ? Nephrectomy. 80


