e0bbfdc1ebb51780556fcc1d33d03aca.ppt
- Количество слайдов: 46

The (unforeseen) Challenges and Benefits of Integrating Diagnostic Workflows W. Dean Wallace, MD Department of Pathology, UCLA wwallace@mednet. ucla. edu
Notice of Faculty Disclosure In accordance with ACCME guidelines, any individual in a position to influence and/or control the content of this ASCP CME activity has disclosed all relevant financial relationships within the past 12 months with commercial interests that provide products and/or services related to the content of this CME activity. The individual below has responded that he/she has no relevant financial relationship(s) with commercial interest(s) to disclose: W. Dean Wallace, MD
Content • Review current workflows • Review the UCLA experience in integrated diagnostic reporting • Discuss continuing challenges and benefits 4
Current Paradigm • Radiology and pathology are two separate specialties at the center of the diagnostic process and their findings, issued in reports from different sources, are responsible for ultimate diagnosis. • Pathologists and radiologists have lived in their own silos for years. • Feel very comfortable there • Clinicians have lived with this arrangement for a long time. • Newer testing is continually emerging and complicates the diagnostic integration. • These new tests are often reported separately • Correlations are usually performed ad hoc (eg, phone calls, tumor boards, etc) with few formalized exceptions. • The burden is on the treating clinician to discover and synthesize all reports on a given lesion.
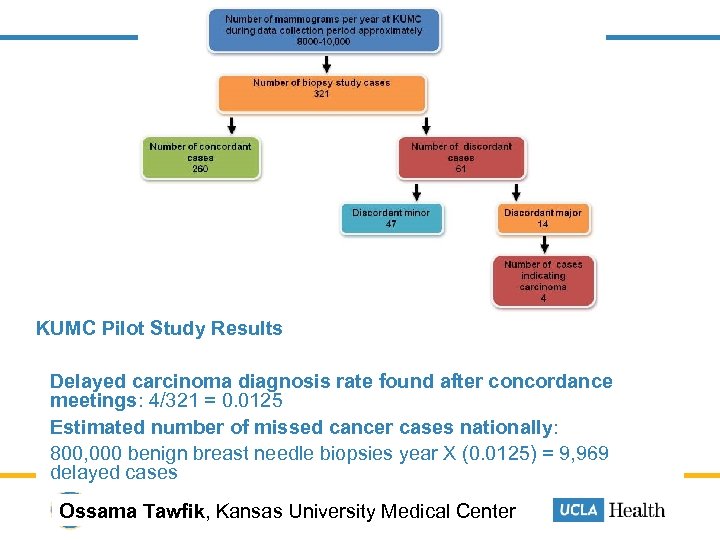
KUMC Pilot Study Results Delayed carcinoma diagnosis rate found after concordance meetings: 4/321 = 0. 0125 Estimated number of missed cancer cases nationally: 800, 000 benign breast needle biopsies year X (0. 0125) = 9, 969 delayed cases Ossama Tawfik, Kansas University Medical Center
Mammography Quality Standards Act of 1992 • BI-RADS is required by law under MQSA • Radiologists must make an attempt to correlate the results of the biopsy 8
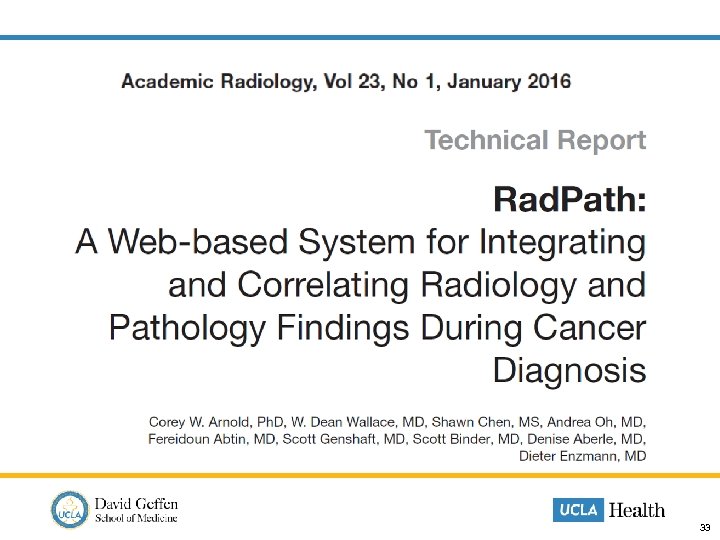
Discordance studies • Oh AS, Arnold CW, Vangala S, Wallace WD, Genshaft SJ, Sarma K, Aberle DR. Imaging-histologic discordance at percutaneous biopsy of the lung. Acad Radiol. 2015 Apr; 22(4): 481 -7. • Youk J, Kim E-K, Kim M, Kwak J, Son E. Analysis of false-negative results after USguided 14 -gauge core needle breast biopsy. Eur Radiol. 2010; 20(4): 782 -789. • Mihalik JE, Krupka L, Davenport R, Tucker L, Toevs C, Smith RS. The rate of imaging-histologic discordance of benign breast disease: a multidisciplinary approach to the management of discordance at a large university-based hospital. Am J Surg. 2010; 199(3): 319 -323. • Lee J-M, Kaplan JB, Murray MP, et al. Imaging Histologic Discordance at MRIGuided 9 -Gauge Vacuum-Assisted Breast Biopsy. Am. J. Roentgenol. October 1, 2007; 189(4): 852 -859. • Liberman L, Drotman M, Morris EA, et al. Imaging-histologic discordance at percutaneous breast biopsy. Cancer. 2000; 89(12): 2538 -2546.
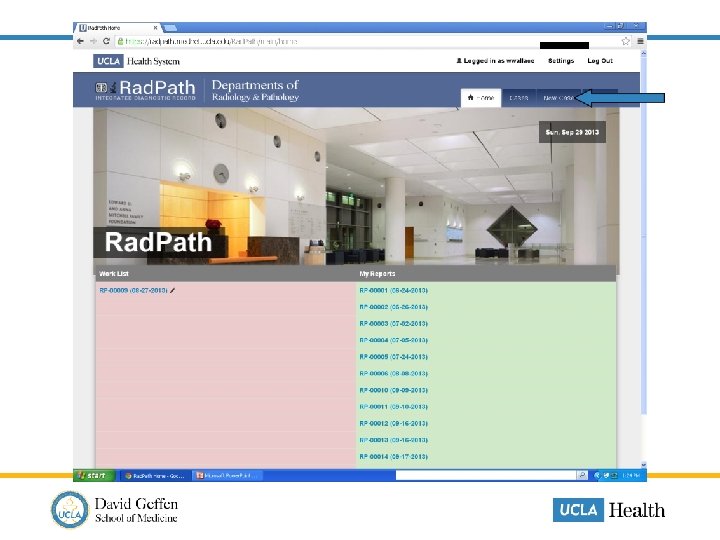
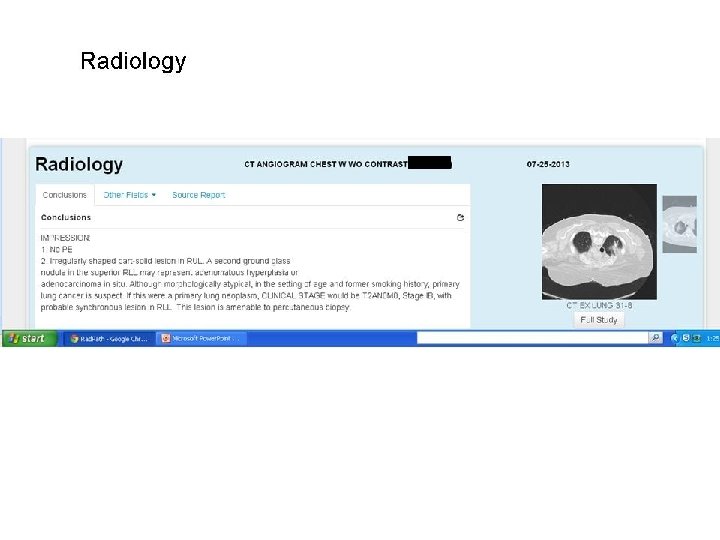
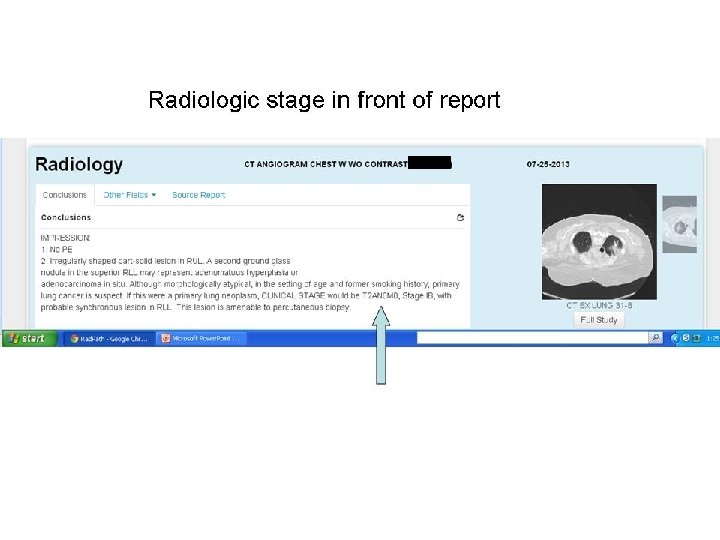
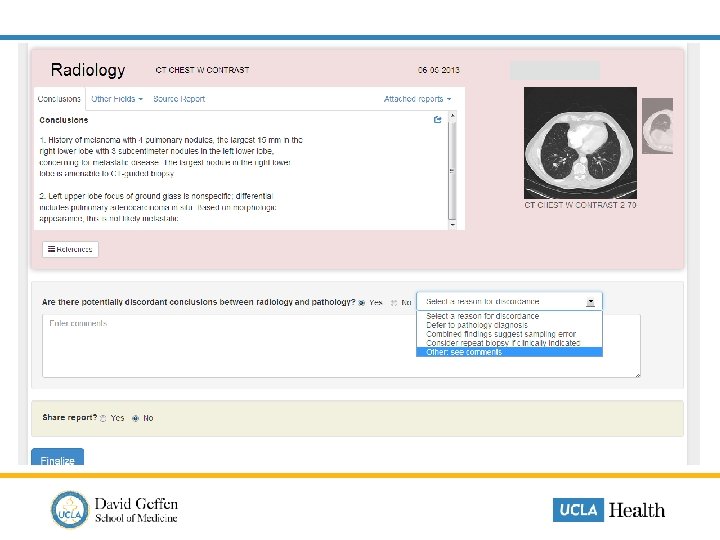
UCLA Rad. Path • Electronic web-based report that pulls data elements from pertinent radiology and pathology studies. • All diagnostic studies pertinent to a specific disease process may be accessed from a single, secure web-based portal. • The dynamic report can emphasize the most important details of a disease and provide access to the imaging studies. • Correlation functionality formalizes radiology-pathology integration. • Direct links to email facilitates contextualized and quick communication between clinician-and-diagnostician (radiologist or pathologist) and clinician-and-clinician.
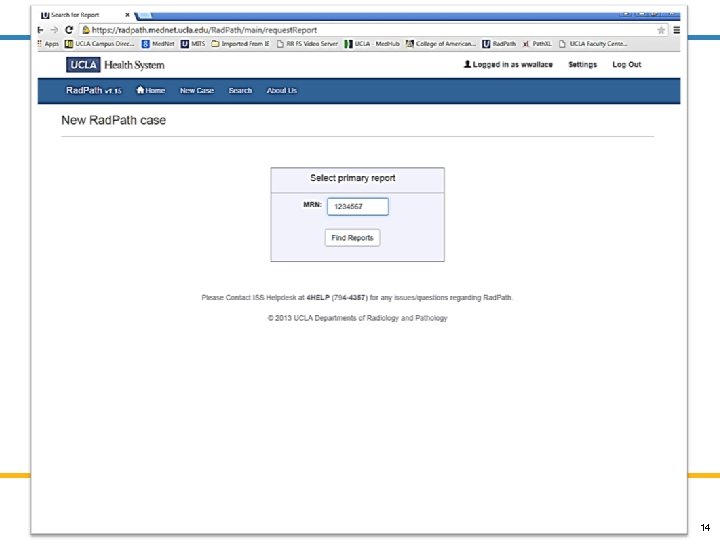
14
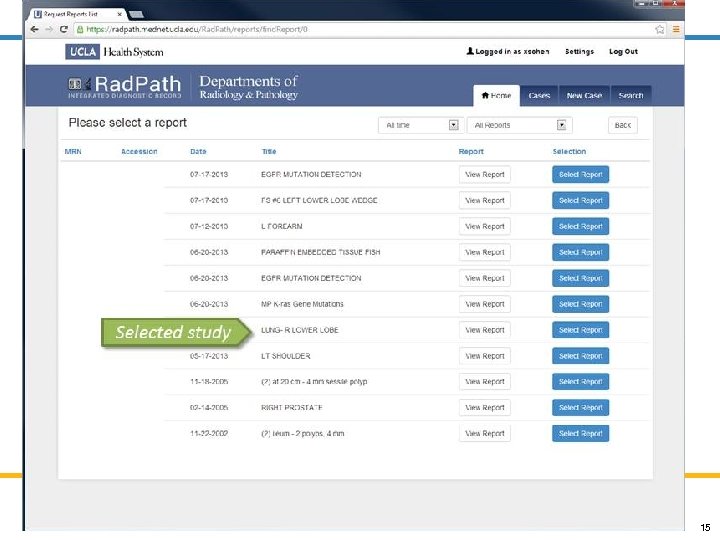
15
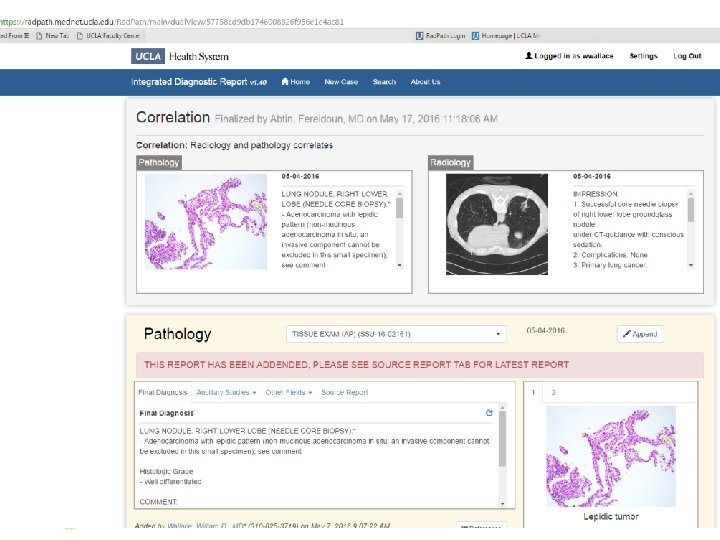
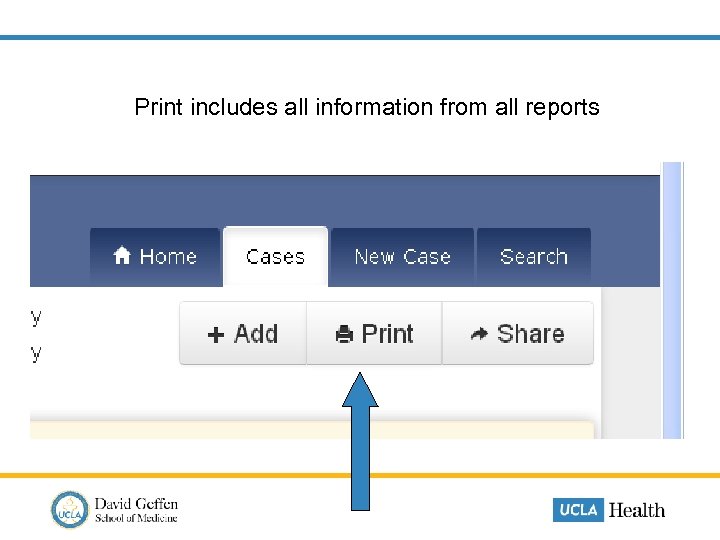
Print includes all information from all reports
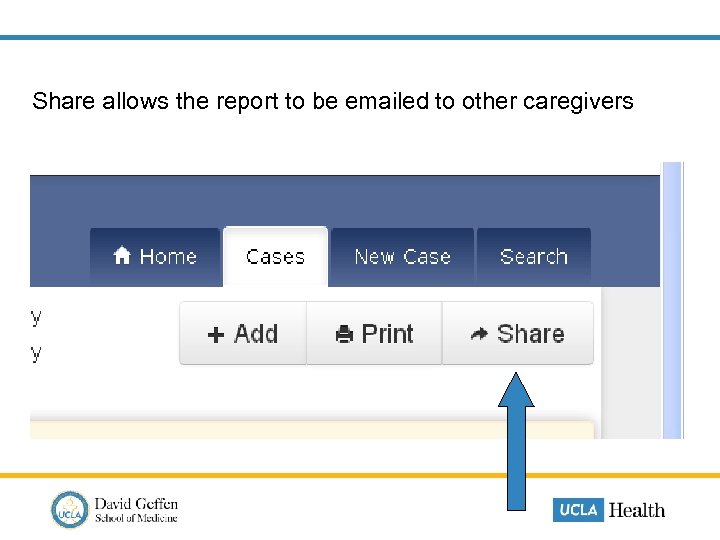
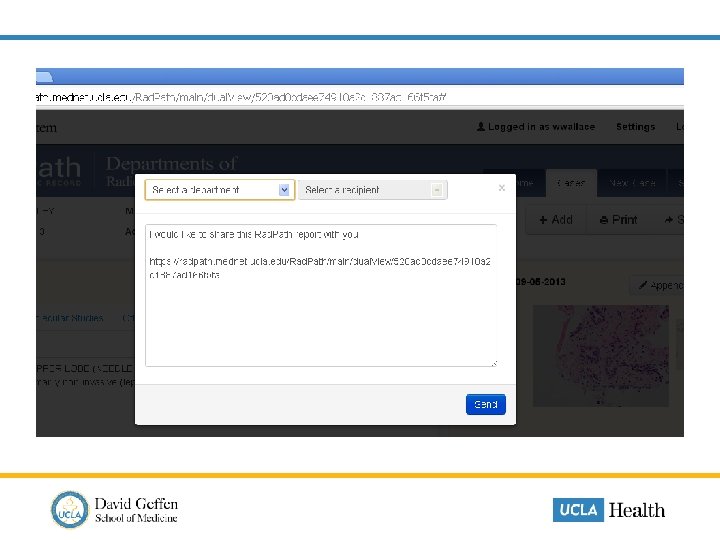
Share allows the report to be emailed to other caregivers
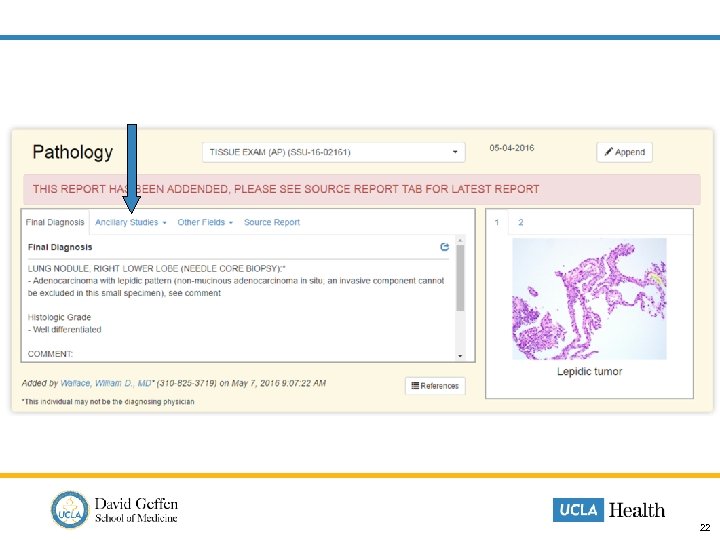
22
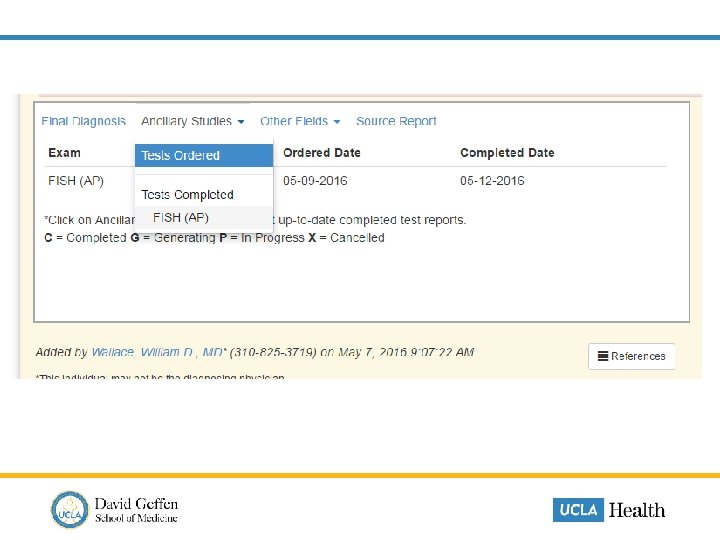
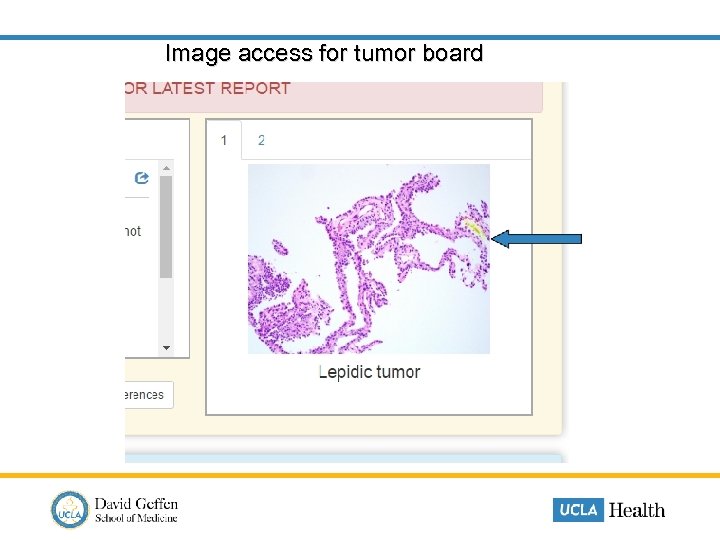
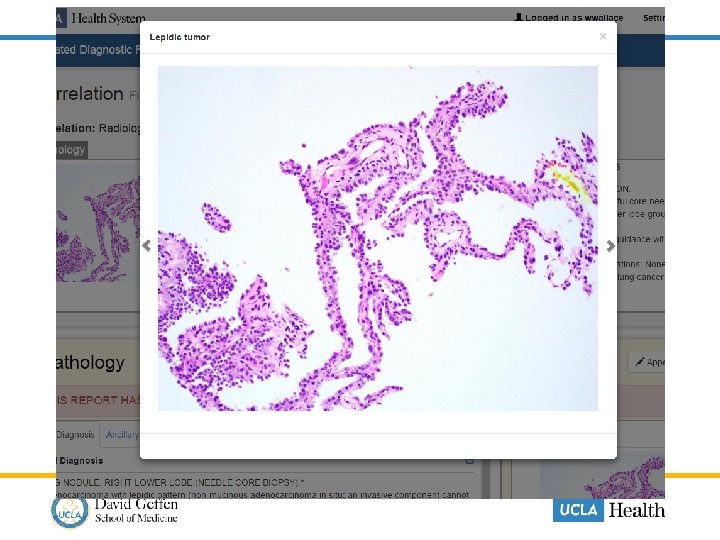
Image access for tumor board
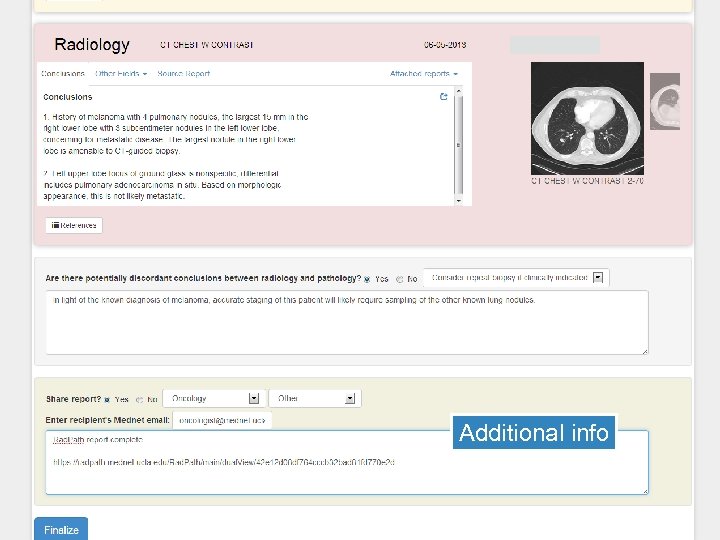
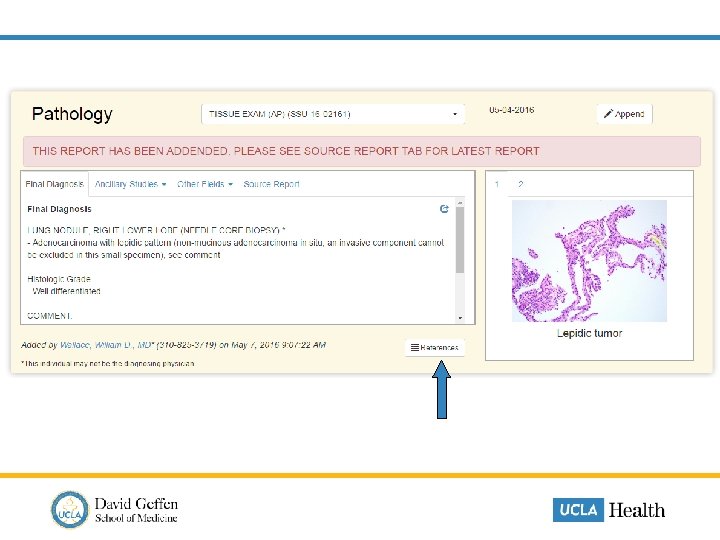
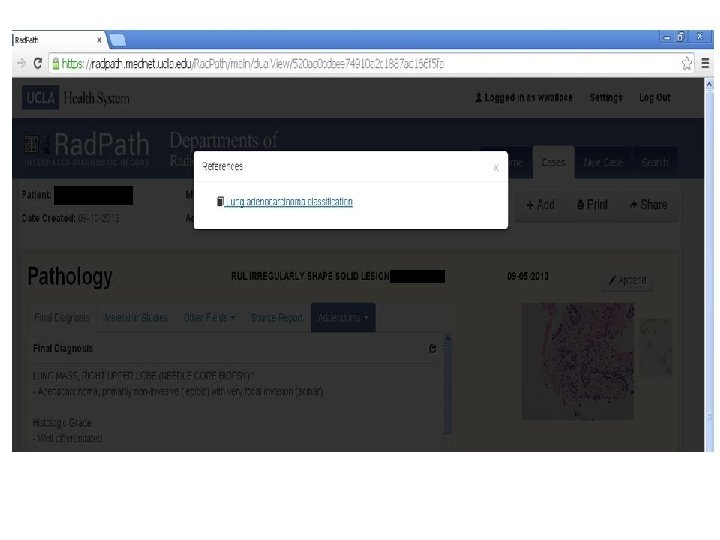
Additional info
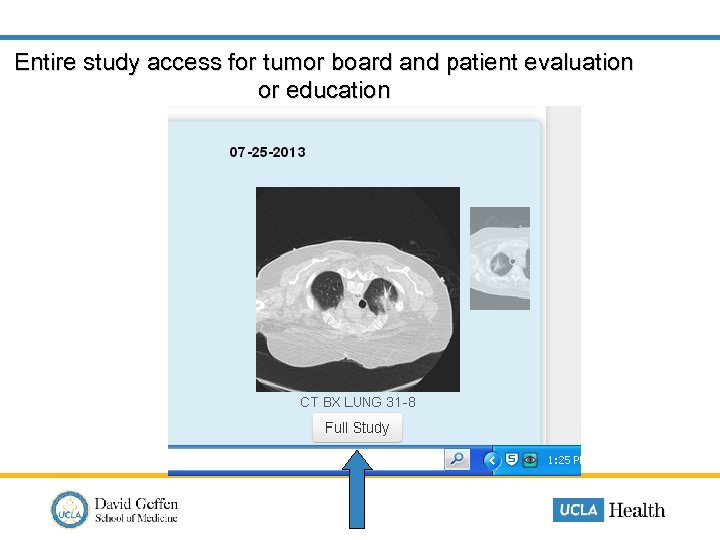
Entire study access for tumor board and patient evaluation or education
UCLA Rad. Path Summary • Single report solution • Image viewer • Communication tool • Allows easier/quicker contextualized communication between clinicians • May function as “virtual tumor board” • Important educational tool for patients
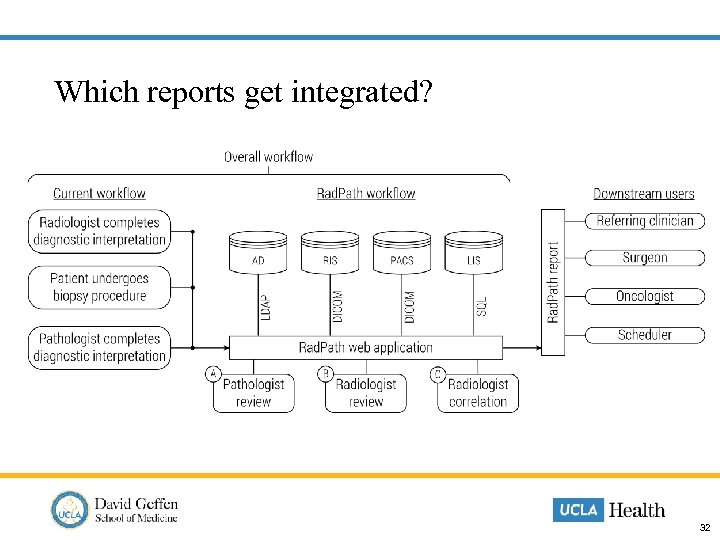
Which reports get integrated? 32
33
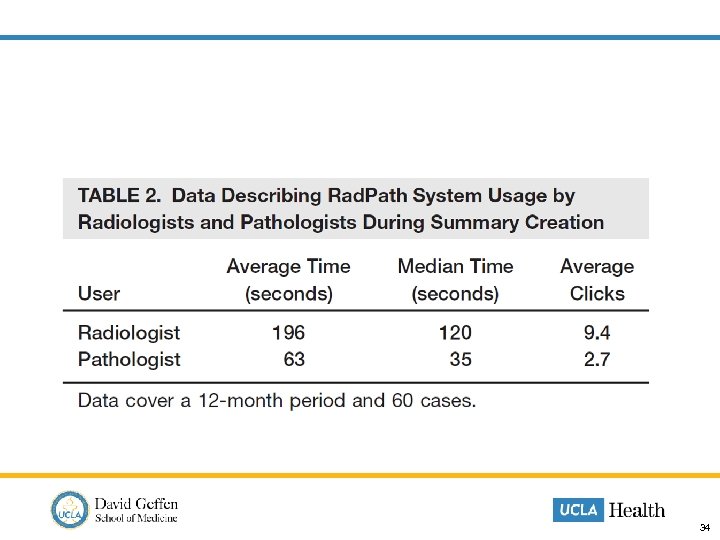
34
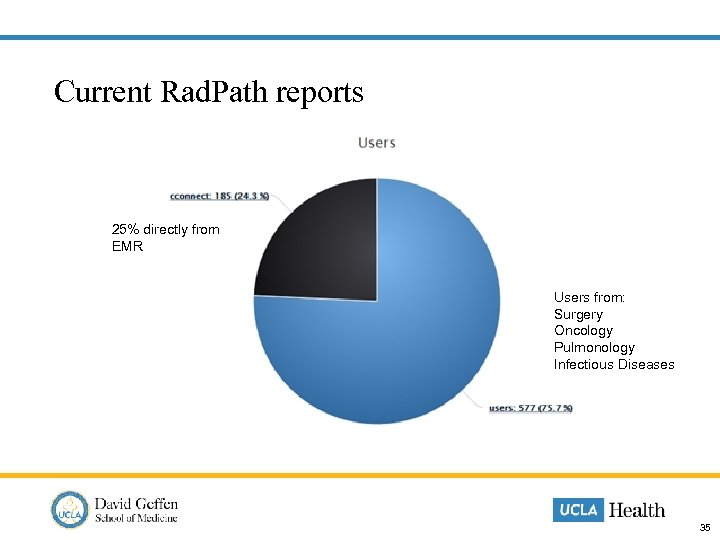
Current Rad. Path reports 25% directly from EMR Users from: Surgery Oncology Pulmonology Infectious Diseases 35
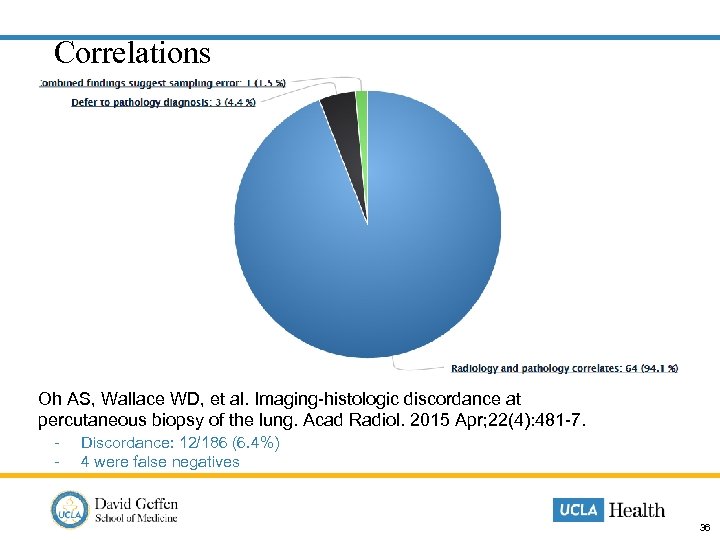
Correlations Oh AS, Wallace WD, et al. Imaging-histologic discordance at percutaneous biopsy of the lung. Acad Radiol. 2015 Apr; 22(4): 481 -7. - Discordance: 12/186 (6. 4%) 4 were false negatives 36
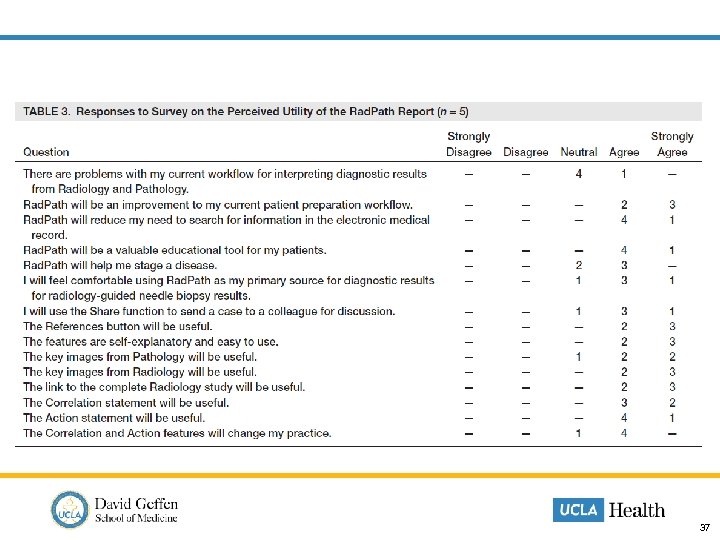
37
Continuing challenges • Lack of widespread nuanced appreciation for the role of integrated reporting • Technical • Recent LIS transition • Metrics to demonstrate real value are difficult to show • Audit use, email use • Analyze differences in time from diagnosis to definitive care, before and after implementation of Rad. Path for service lines • Analyze patient counseling effectiveness • Compliance… • Wholesale adoption by colleagues has been slow 38
Successes/Benefits • Improved understanding and interest between radiology and pathology • Improved collegiality between radiologists and pathologists; and doctors and IT • Improved clinical workflows with reduction in patient preparation time • Very powerful tumor board presentation tool • Most useful for pathology buy in • Increased exposure for lab within the medical centerprise • Generating demand from other service lines for expansion • Other centers approaching us to help development UC San Diego • UC Davis • • Industry interest 39
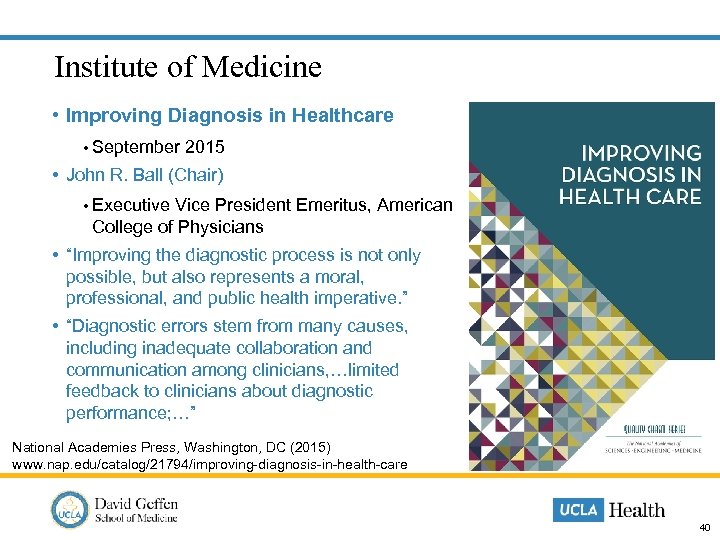
Institute of Medicine • Improving Diagnosis in Healthcare • September 2015 • John R. Ball (Chair) • Executive Vice President Emeritus, American College of Physicians • “Improving the diagnostic process is not only possible, but also represents a moral, professional, and public health imperative. ” • “Diagnostic errors stem from many causes, including inadequate collaboration and communication among clinicians, …limited feedback to clinicians about diagnostic performance; …” National Academies Press, Washington, DC (2015) www. nap. edu/catalog/21794/improving-diagnosis-in-health-care 40
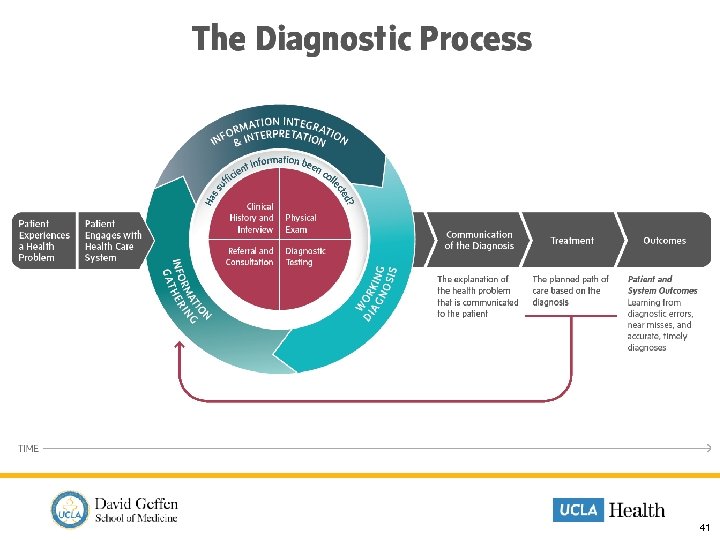
41

Eight goals for diagnostic improvement 1. Facilitate more effective teamwork in the diagnostic process. 2. Enhance training in the diagnostic process. Develop Industry Standards 3. Encourage health IT to provide more support in the diagnostic process. 4. Develop and deploy approaches to identify, learn from, and reduce diagnostic errors and near misses in clinical practice. 5. Develop a culture that supports improvements in diagnostic performance. 6. Develop an environment and medical liability system that encourages learning from diagnostic errors. 7. Create an appropriate reimbursement system for the diagnostic process. 8. Provide dedicated funding for research. 42
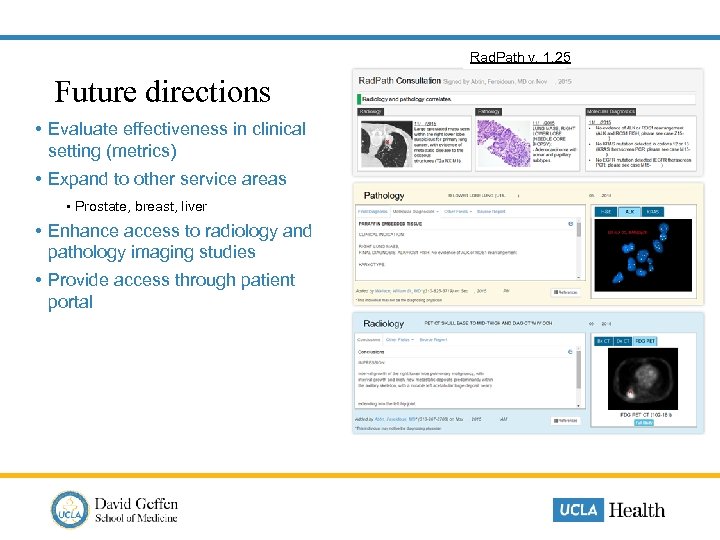
Rad. Path v. 1. 25 Future directions • Evaluate effectiveness in clinical setting (metrics) • Expand to other service areas • Prostate, breast, liver • Enhance access to radiology and pathology imaging studies • Provide access through patient portal
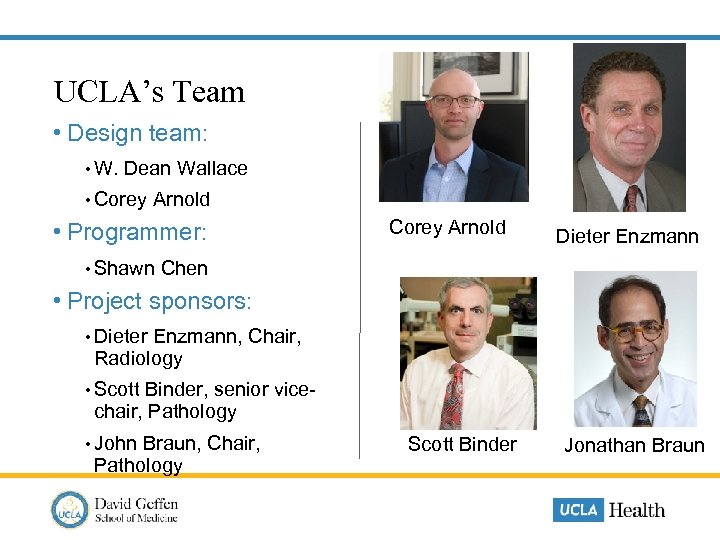
UCLA’s Team • Design team: • W. Dean Wallace • Corey Arnold • Programmer: Corey Arnold Dieter Enzmann • Shawn Chen • Project sponsors: • Dieter Enzmann, Chair, Radiology • Scott Binder, senior vice- chair, Pathology • John Braun, Chair, Pathology Scott Binder Jonathan Braun
Thank you! wwallace@mednet. ucla. edu 45

e0bbfdc1ebb51780556fcc1d33d03aca.ppt