0946b050ca821fc101930b9470df319c.ppt
- Количество слайдов: 40
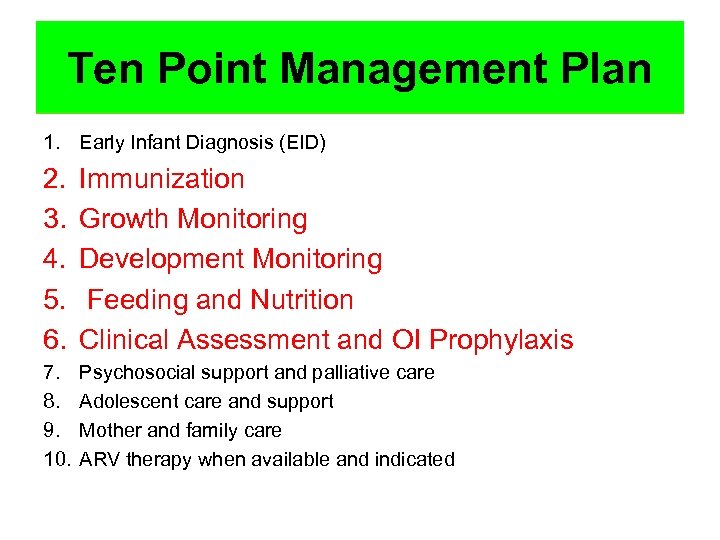 The ten point management plan for Ten Point Managementcare Plan comprehensive pediatric HIV 1. Early Infant Diagnosis (EID) 2. 3. 4. 5. 6. Immunization Growth Monitoring Development Monitoring Feeding and Nutrition Clinical Assessment and OI Prophylaxis 7. 8. 9. 10. Psychosocial support and palliative care Adolescent care and support Mother and family care ARV therapy when available and indicated
The ten point management plan for Ten Point Managementcare Plan comprehensive pediatric HIV 1. Early Infant Diagnosis (EID) 2. 3. 4. 5. 6. Immunization Growth Monitoring Development Monitoring Feeding and Nutrition Clinical Assessment and OI Prophylaxis 7. 8. 9. 10. Psychosocial support and palliative care Adolescent care and support Mother and family care ARV therapy when available and indicated
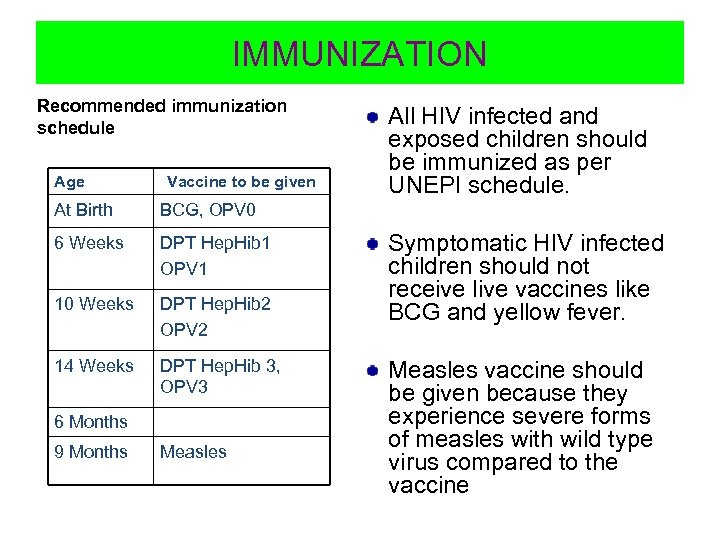 IMMUNIZATION Recommended immunization schedule Age Vaccine to be given At Birth BCG, OPV 0 6 Weeks DPT Hep. Hib 1 OPV 1 10 Weeks DPT Hep. Hib 2 OPV 2 14 Weeks DPT Hep. Hib 3, OPV 3 All HIV infected and exposed children should be immunized as per UNEPI schedule. 6 Months 9 Months Measles Symptomatic HIV infected children should not receive live vaccines like BCG and yellow fever. Measles vaccine should be given because they experience severe forms of measles with wild type virus compared to the vaccine
IMMUNIZATION Recommended immunization schedule Age Vaccine to be given At Birth BCG, OPV 0 6 Weeks DPT Hep. Hib 1 OPV 1 10 Weeks DPT Hep. Hib 2 OPV 2 14 Weeks DPT Hep. Hib 3, OPV 3 All HIV infected and exposed children should be immunized as per UNEPI schedule. 6 Months 9 Months Measles Symptomatic HIV infected children should not receive live vaccines like BCG and yellow fever. Measles vaccine should be given because they experience severe forms of measles with wild type virus compared to the vaccine
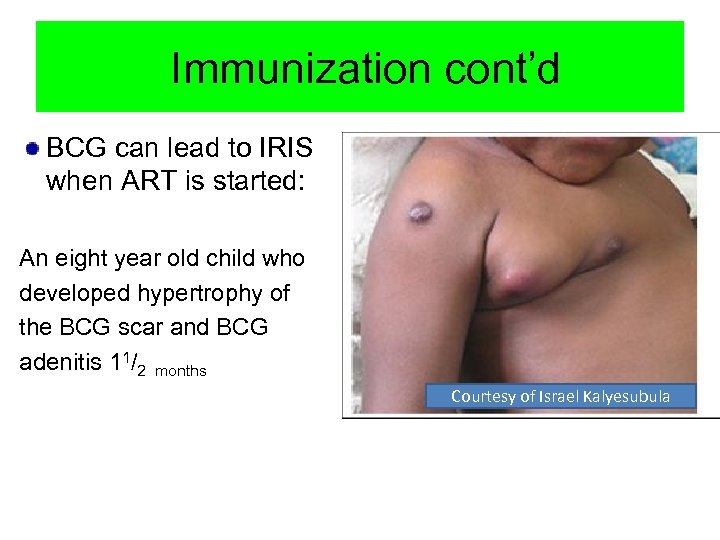 Immunization cont’d BCG can lead to IRIS when ART is started: An eight year old child who developed hypertrophy of the BCG scar and BCG adenitis 11/2 months Courtesy of Israel Kalyesubula
Immunization cont’d BCG can lead to IRIS when ART is started: An eight year old child who developed hypertrophy of the BCG scar and BCG adenitis 11/2 months Courtesy of Israel Kalyesubula
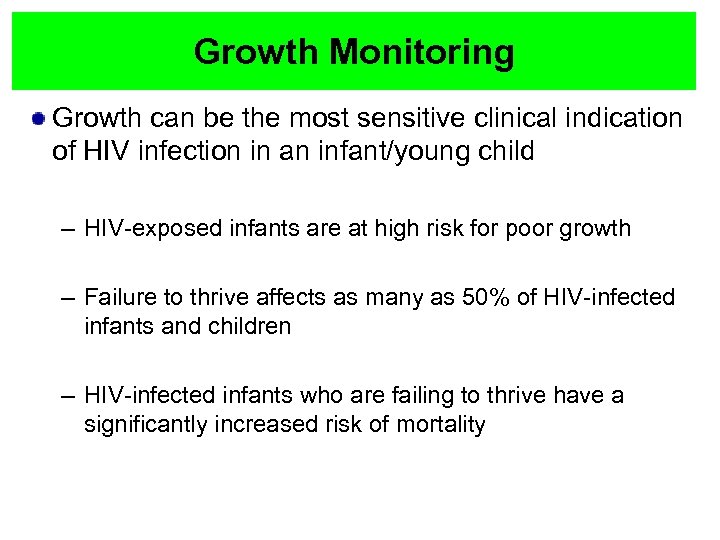 Growth Monitoring Growth can be the most sensitive clinical indication of HIV infection in an infant/young child – HIV-exposed infants are at high risk for poor growth – Failure to thrive affects as many as 50% of HIV-infected infants and children – HIV-infected infants who are failing to thrive have a significantly increased risk of mortality
Growth Monitoring Growth can be the most sensitive clinical indication of HIV infection in an infant/young child – HIV-exposed infants are at high risk for poor growth – Failure to thrive affects as many as 50% of HIV-infected infants and children – HIV-infected infants who are failing to thrive have a significantly increased risk of mortality
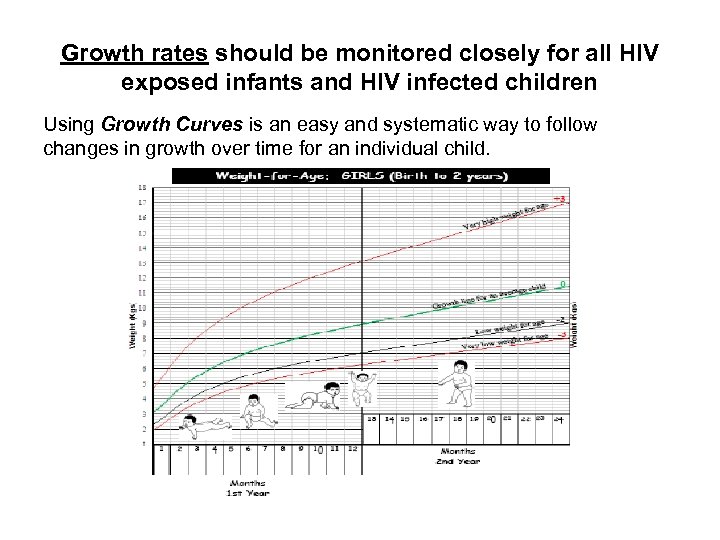 Growth rates should be monitored closely for all HIV exposed infants and HIV infected children Using Growth Curves is an easy and systematic way to follow changes in growth over time for an individual child.
Growth rates should be monitored closely for all HIV exposed infants and HIV infected children Using Growth Curves is an easy and systematic way to follow changes in growth over time for an individual child.
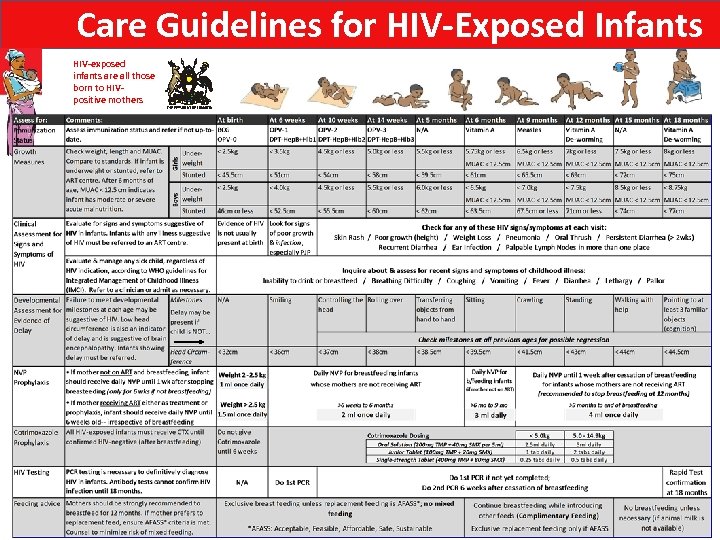 Care Guidelines for HIV-Exposed Infants HIV-exposed infants are all those born to HIVpositive mothers
Care Guidelines for HIV-Exposed Infants HIV-exposed infants are all those born to HIVpositive mothers
 Monitoring Development “Development’ represents maturation of the brain and central nervous system Delayed development or loss of milestones may be the first sign of HIV infection in an infant or young child – Development can be viewed more as snapshots of the child at specified points in time – While other causes are possible, abnormal development should raise concerns of HIV infection – Infants are at high risk for HIV encephalopathy and severe neurologic disease Early identification of developmental delay and neurologic abnormalities can facilitate intervention and remediation
Monitoring Development “Development’ represents maturation of the brain and central nervous system Delayed development or loss of milestones may be the first sign of HIV infection in an infant or young child – Development can be viewed more as snapshots of the child at specified points in time – While other causes are possible, abnormal development should raise concerns of HIV infection – Infants are at high risk for HIV encephalopathy and severe neurologic disease Early identification of developmental delay and neurologic abnormalities can facilitate intervention and remediation
 How do you assess development? The assessment should include Cognitive, Motor, Language, and Social skills Measure: Low head circumference is one of the earliest presenting signs of HIV and indicates brain encephalopathy Ask parents to report on milestones achieved in infants Observe and Examine Assess all four domains E. g. A 6 month old sits upright in mothers arms, she reaches for your stethoscope and puts it in her mouth, says gaga, gaga when you take it out of her mouth, turns to her mother for reassurance Look for red Flags (i. e. early warning signs)
How do you assess development? The assessment should include Cognitive, Motor, Language, and Social skills Measure: Low head circumference is one of the earliest presenting signs of HIV and indicates brain encephalopathy Ask parents to report on milestones achieved in infants Observe and Examine Assess all four domains E. g. A 6 month old sits upright in mothers arms, she reaches for your stethoscope and puts it in her mouth, says gaga, gaga when you take it out of her mouth, turns to her mother for reassurance Look for red Flags (i. e. early warning signs)
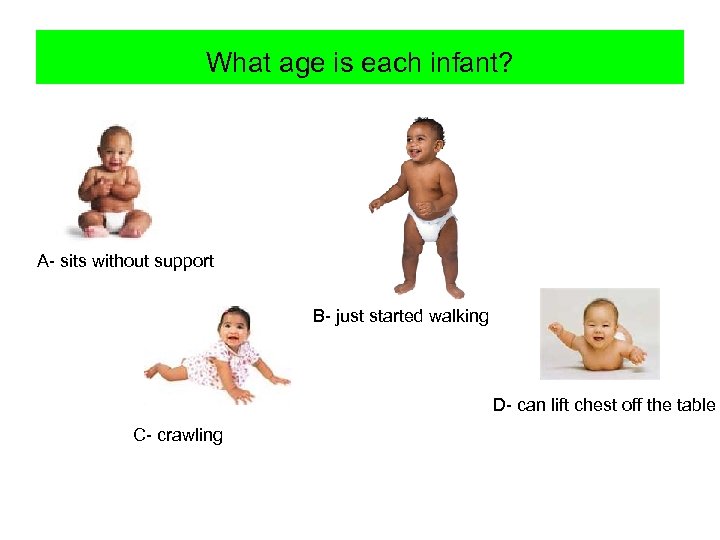 What age is each infant? A- sits without support B- just started walking D- can lift chest off the table C- crawling
What age is each infant? A- sits without support B- just started walking D- can lift chest off the table C- crawling
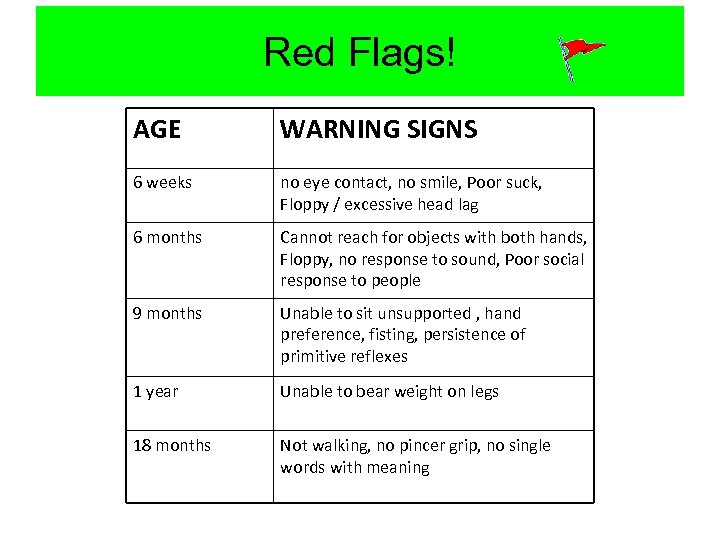 Red Flags! AGE WARNING SIGNS 6 weeks no eye contact, no smile, Poor suck, Floppy / excessive head lag 6 months Cannot reach for objects with both hands, Floppy, no response to sound, Poor social response to people 9 months Unable to sit unsupported , hand preference, fisting, persistence of primitive reflexes 1 year Unable to bear weight on legs 18 months Not walking, no pincer grip, no single words with meaning
Red Flags! AGE WARNING SIGNS 6 weeks no eye contact, no smile, Poor suck, Floppy / excessive head lag 6 months Cannot reach for objects with both hands, Floppy, no response to sound, Poor social response to people 9 months Unable to sit unsupported , hand preference, fisting, persistence of primitive reflexes 1 year Unable to bear weight on legs 18 months Not walking, no pincer grip, no single words with meaning
 Practice Exercise: Using the Care Guidelines for HIV Exposed Infants Instructions: 1) Work in Pairs 2) Use your Job Aid: Care Guidelines for HIV Exposed Infants 3) Answer the questions for the Case in your Guide.
Practice Exercise: Using the Care Guidelines for HIV Exposed Infants Instructions: 1) Work in Pairs 2) Use your Job Aid: Care Guidelines for HIV Exposed Infants 3) Answer the questions for the Case in your Guide.
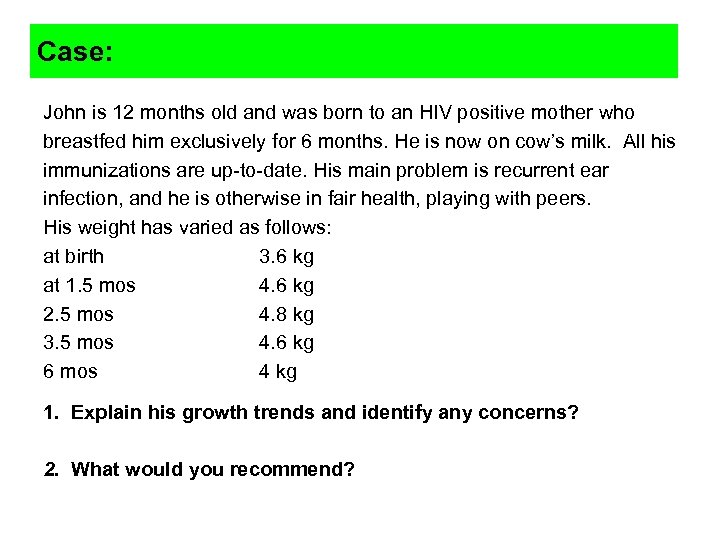 Case: John is 12 months old and was born to an HIV positive mother who breastfed him exclusively for 6 months. He is now on cow’s milk. All his immunizations are up-to-date. His main problem is recurrent ear infection, and he is otherwise in fair health, playing with peers. His weight has varied as follows: at birth 3. 6 kg at 1. 5 mos 4. 6 kg 2. 5 mos 4. 8 kg 3. 5 mos 4. 6 kg 6 mos 4 kg 1. Explain his growth trends and identify any concerns? 2. What would you recommend?
Case: John is 12 months old and was born to an HIV positive mother who breastfed him exclusively for 6 months. He is now on cow’s milk. All his immunizations are up-to-date. His main problem is recurrent ear infection, and he is otherwise in fair health, playing with peers. His weight has varied as follows: at birth 3. 6 kg at 1. 5 mos 4. 6 kg 2. 5 mos 4. 8 kg 3. 5 mos 4. 6 kg 6 mos 4 kg 1. Explain his growth trends and identify any concerns? 2. What would you recommend?
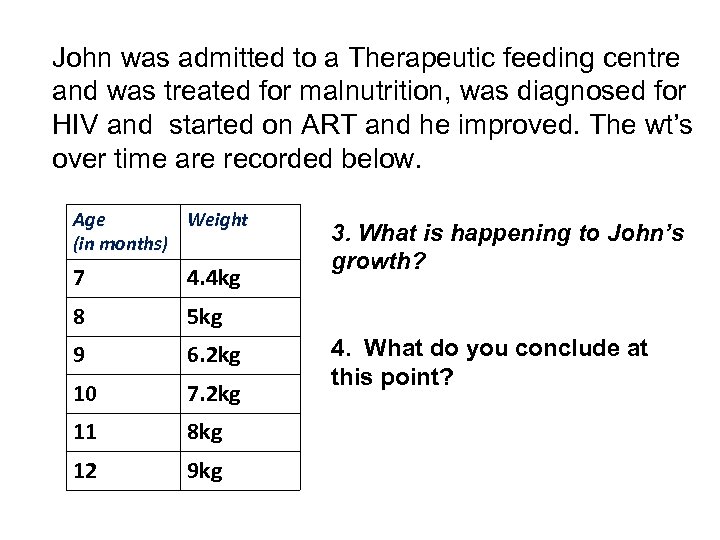 John was admitted to a Therapeutic feeding centre and was treated for malnutrition, was diagnosed for HIV and started on ART and he improved. The wt’s over time are recorded below. Age Weight (in months) 7 4. 4 kg 8 5 kg 9 6. 2 kg 10 7. 2 kg 11 8 kg 12 9 kg 3. What is happening to John’s growth? 4. What do you conclude at this point?
John was admitted to a Therapeutic feeding centre and was treated for malnutrition, was diagnosed for HIV and started on ART and he improved. The wt’s over time are recorded below. Age Weight (in months) 7 4. 4 kg 8 5 kg 9 6. 2 kg 10 7. 2 kg 11 8 kg 12 9 kg 3. What is happening to John’s growth? 4. What do you conclude at this point?
 OI prophylaxis
OI prophylaxis
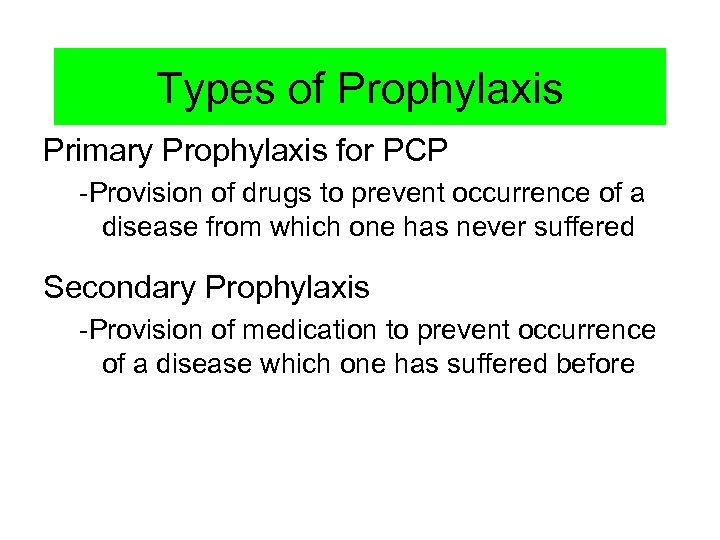 Types of Prophylaxis Primary Prophylaxis for PCP -Provision of drugs to prevent occurrence of a disease from which one has never suffered Secondary Prophylaxis -Provision of medication to prevent occurrence of a disease which one has suffered before
Types of Prophylaxis Primary Prophylaxis for PCP -Provision of drugs to prevent occurrence of a disease from which one has never suffered Secondary Prophylaxis -Provision of medication to prevent occurrence of a disease which one has suffered before
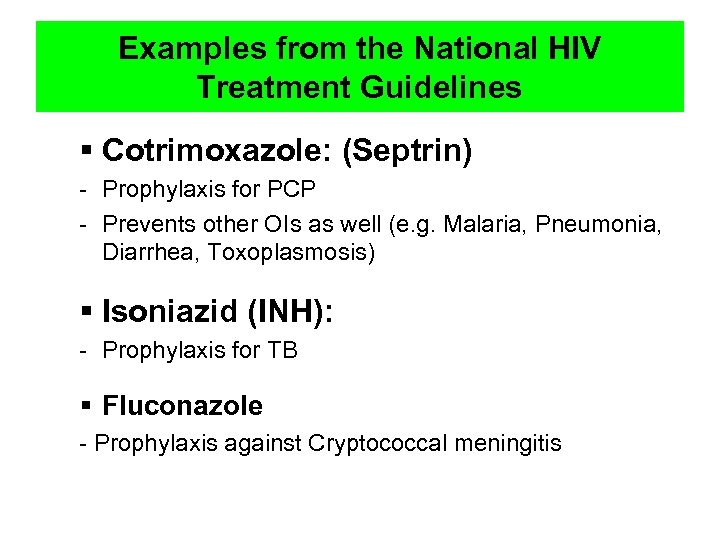 Examples from the National HIV Treatment Guidelines § Cotrimoxazole: (Septrin) - Prophylaxis for PCP - Prevents other OIs as well (e. g. Malaria, Pneumonia, Diarrhea, Toxoplasmosis) § Isoniazid (INH): - Prophylaxis for TB § Fluconazole - Prophylaxis against Cryptococcal meningitis
Examples from the National HIV Treatment Guidelines § Cotrimoxazole: (Septrin) - Prophylaxis for PCP - Prevents other OIs as well (e. g. Malaria, Pneumonia, Diarrhea, Toxoplasmosis) § Isoniazid (INH): - Prophylaxis for TB § Fluconazole - Prophylaxis against Cryptococcal meningitis
 “The best prophylaxis for OI is effective ARV”
“The best prophylaxis for OI is effective ARV”
 Which children need Cotrimoxazole prophylaxis? All children proven to be HIV infected. All HIV exposed children from 6 weeks of life till proved to be HIV negative. Continue for life Use Job Aids for Cotrimoxazole dosing: 1. Care for HIV Exposed Infants Reference Chart 2. Cotrimoxazole Dosing by Formulation and Weight Range Chart
Which children need Cotrimoxazole prophylaxis? All children proven to be HIV infected. All HIV exposed children from 6 weeks of life till proved to be HIV negative. Continue for life Use Job Aids for Cotrimoxazole dosing: 1. Care for HIV Exposed Infants Reference Chart 2. Cotrimoxazole Dosing by Formulation and Weight Range Chart
 Why Cotrimoxazole for life? Cotrimoxazole is an effective prophylaxis against: Various bacterial infections: Streptococcus pneumoniae, Salmonella species, Shigella sp, E. Coli, S. Aureus, H. Influenzae and Nocardia Pneumocystis jirovecii Toxoplasma gondii Isospora belli, Cryptosporidium parvum Malaria
Why Cotrimoxazole for life? Cotrimoxazole is an effective prophylaxis against: Various bacterial infections: Streptococcus pneumoniae, Salmonella species, Shigella sp, E. Coli, S. Aureus, H. Influenzae and Nocardia Pneumocystis jirovecii Toxoplasma gondii Isospora belli, Cryptosporidium parvum Malaria
 Severe reactions with Cotrimoxazole include: Fixed drug reaction Stevens Johnson syndrome Renal and/or hepatic failure Severe hematological toxicity For any of these reactions Cotrimoxazole should be stopped. Substitution: Dapsone
Severe reactions with Cotrimoxazole include: Fixed drug reaction Stevens Johnson syndrome Renal and/or hepatic failure Severe hematological toxicity For any of these reactions Cotrimoxazole should be stopped. Substitution: Dapsone
 Fixed drug reaction Fixed drug eruptions recur on exactly the same spot every time the responsible drug is taken. There is usually one, sometimes two or more macules or plaques, reddish-purple in colour. They may show blistering and leave persistent hyper pigmentation on healing. Photo courtesy of Dr Israel Kalyesubula
Fixed drug reaction Fixed drug eruptions recur on exactly the same spot every time the responsible drug is taken. There is usually one, sometimes two or more macules or plaques, reddish-purple in colour. They may show blistering and leave persistent hyper pigmentation on healing. Photo courtesy of Dr Israel Kalyesubula
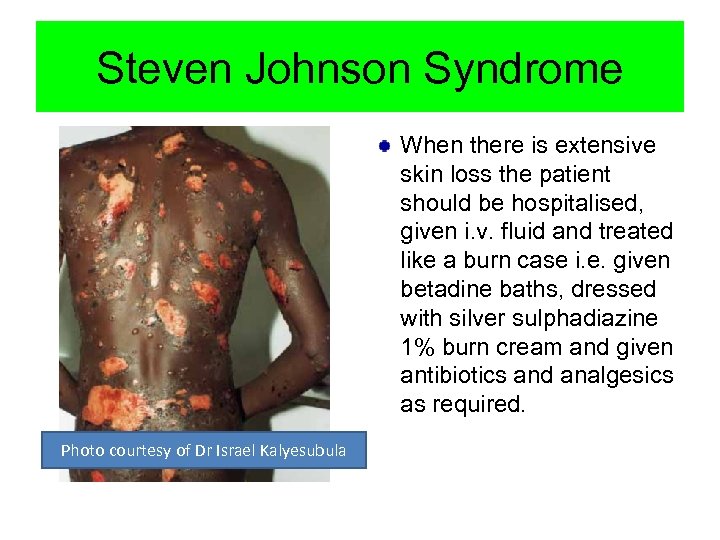 Steven Johnson Syndrome When there is extensive skin loss the patient should be hospitalised, given i. v. fluid and treated like a burn case i. e. given betadine baths, dressed with silver sulphadiazine 1% burn cream and given antibiotics and analgesics as required. Photo courtesy of Dr Israel Kalyesubula
Steven Johnson Syndrome When there is extensive skin loss the patient should be hospitalised, given i. v. fluid and treated like a burn case i. e. given betadine baths, dressed with silver sulphadiazine 1% burn cream and given antibiotics and analgesics as required. Photo courtesy of Dr Israel Kalyesubula
 Renal or Hepatic Failure May happen if patient has been on the drug for a long time. Reversible condition once the drug is stopped. Clinical suspicion and testing to confirm is needed. (Not easily visible)
Renal or Hepatic Failure May happen if patient has been on the drug for a long time. Reversible condition once the drug is stopped. Clinical suspicion and testing to confirm is needed. (Not easily visible)
 Severe hematological toxicity Causes severe anemia Causes neutropaenia Neutrophils are reduced when someone is on Cotrimoxazole for a long time Also reversible once the drug is stopped. Not easily visible. Confirmation needed by blood work.
Severe hematological toxicity Causes severe anemia Causes neutropaenia Neutrophils are reduced when someone is on Cotrimoxazole for a long time Also reversible once the drug is stopped. Not easily visible. Confirmation needed by blood work.
 Which children need INH prophylaxis? All HIV-infected infants and children exposed to TB through household contacts, but with no evidence of active disease, should begin Isoniazid preventive therapy (IPT). HIV-infected children >12 months of age should receive 6 months of INH as part of a comprehensive package of HIV care irrespective of TB exposure (provide no evidence of current active TB disease) HIV-infected infants <12 months should not receive INH but should be followed clinically including for possible TB disease as part of a comprehensive package of HIV care. Dose (New Guidelines): Recommended dose of Isoniazid (INH) for preventive therapy in HIV co-infection is 10 mg/kg/daily for 6 months (maximum 300 mg/day).
Which children need INH prophylaxis? All HIV-infected infants and children exposed to TB through household contacts, but with no evidence of active disease, should begin Isoniazid preventive therapy (IPT). HIV-infected children >12 months of age should receive 6 months of INH as part of a comprehensive package of HIV care irrespective of TB exposure (provide no evidence of current active TB disease) HIV-infected infants <12 months should not receive INH but should be followed clinically including for possible TB disease as part of a comprehensive package of HIV care. Dose (New Guidelines): Recommended dose of Isoniazid (INH) for preventive therapy in HIV co-infection is 10 mg/kg/daily for 6 months (maximum 300 mg/day).
 Which children need Prophylaxis against Cryptococcal meningitis? Patients who have been treated for Cryptococcal meningitis should receive secondary prophylaxis of Fluconazole Continue for life Dose: 6 mg/kg for children
Which children need Prophylaxis against Cryptococcal meningitis? Patients who have been treated for Cryptococcal meningitis should receive secondary prophylaxis of Fluconazole Continue for life Dose: 6 mg/kg for children
 Feeding and Nutrition
Feeding and Nutrition
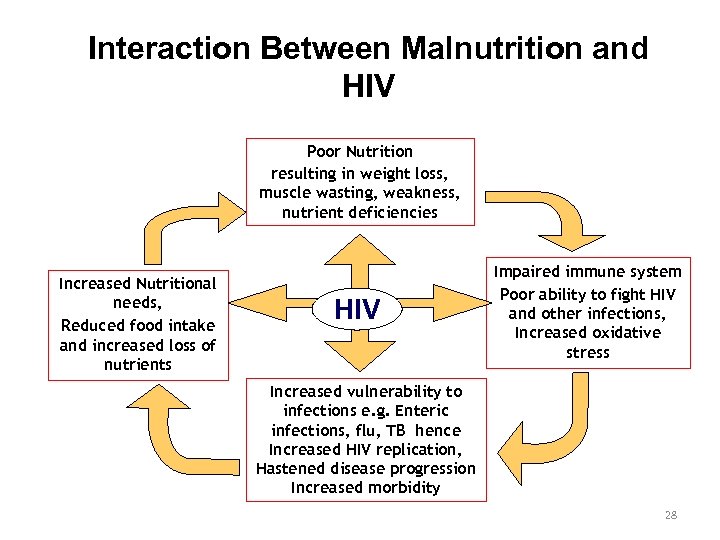 Interaction Between Malnutrition and HIV Poor Nutrition resulting in weight loss, muscle wasting, weakness, nutrient deficiencies Increased Nutritional needs, Reduced food intake and increased loss of nutrients HIV Impaired immune system Poor ability to fight HIV and other infections, Increased oxidative stress Increased vulnerability to infections e. g. Enteric infections, flu, TB hence Increased HIV replication, Hastened disease progression Increased morbidity Source: Adapted from RCQHC and FANTA 2003 28
Interaction Between Malnutrition and HIV Poor Nutrition resulting in weight loss, muscle wasting, weakness, nutrient deficiencies Increased Nutritional needs, Reduced food intake and increased loss of nutrients HIV Impaired immune system Poor ability to fight HIV and other infections, Increased oxidative stress Increased vulnerability to infections e. g. Enteric infections, flu, TB hence Increased HIV replication, Hastened disease progression Increased morbidity Source: Adapted from RCQHC and FANTA 2003 28
 Why Focus on Young Child Feeding? The young child is undergoing a period of rapid growth, requiring adequate supply of nutrients. Severely malnourished children with HIV/AIDS are about five times more likely to die than uninfected children. They rarely respond to conventional nutritional care. They take much longer to recover. The decision about how to feed an infant is rarely the mother’s alone, but is strongly influenced by her partner and her family.
Why Focus on Young Child Feeding? The young child is undergoing a period of rapid growth, requiring adequate supply of nutrients. Severely malnourished children with HIV/AIDS are about five times more likely to die than uninfected children. They rarely respond to conventional nutritional care. They take much longer to recover. The decision about how to feed an infant is rarely the mother’s alone, but is strongly influenced by her partner and her family.
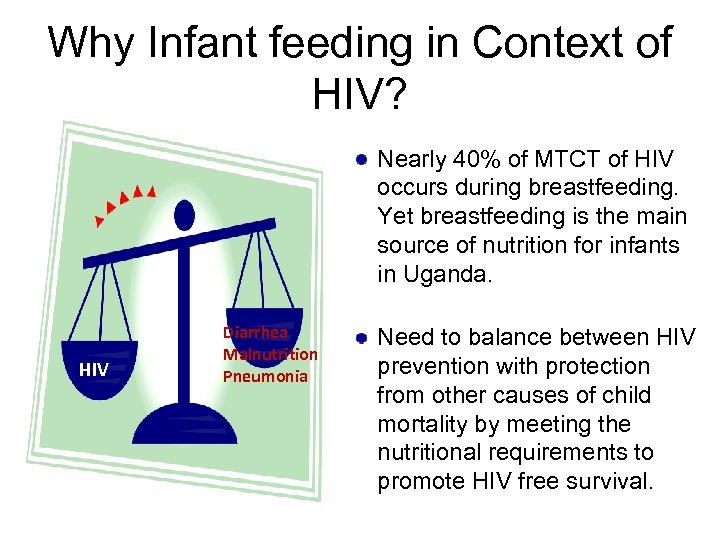 Why Infant feeding in Context of HIV? Nearly 40% of MTCT of HIV occurs during breastfeeding. Yet breastfeeding is the main source of nutrition for infants in Uganda. HIV Diarrhea Malnutrition Pneumonia Need to balance between HIV prevention with protection from other causes of child mortality by meeting the nutritional requirements to promote HIV free survival.
Why Infant feeding in Context of HIV? Nearly 40% of MTCT of HIV occurs during breastfeeding. Yet breastfeeding is the main source of nutrition for infants in Uganda. HIV Diarrhea Malnutrition Pneumonia Need to balance between HIV prevention with protection from other causes of child mortality by meeting the nutritional requirements to promote HIV free survival.
 Definitions of feeding terms Exclusive Breastfeeding: Feeding a child through only breastfeeding, giving no other liquids or solids, not even water, with the exception of prescribed drops or syrups consisting of vitamins and mineral supplements or medicines, and expressed breast milk. Replacement Feeding: The process of feeding a child who is not receiving any breast milk with a diet that provides all the nutrients the child needs, until the child is fully fed on family foods. Replacement feeds do not include black coffee/tea, fruit juices, over-diluted milk. Mixed Feeding: Feeding both breast milk and other foods or liquids to a child under 6 months Complementary feeding: Giving a child other foods (solid or semi-solid) in addition to breastfeeding or replacement feeding to meet baby’s nutrient requirements from 6 months Weaning: The process of introducing the infant to other foods while reducing the supply of breast milk (over course of 1 month) Re-lactating: Re-establishing breastfeeding after a mother had stopped, whether in the recent or distant past
Definitions of feeding terms Exclusive Breastfeeding: Feeding a child through only breastfeeding, giving no other liquids or solids, not even water, with the exception of prescribed drops or syrups consisting of vitamins and mineral supplements or medicines, and expressed breast milk. Replacement Feeding: The process of feeding a child who is not receiving any breast milk with a diet that provides all the nutrients the child needs, until the child is fully fed on family foods. Replacement feeds do not include black coffee/tea, fruit juices, over-diluted milk. Mixed Feeding: Feeding both breast milk and other foods or liquids to a child under 6 months Complementary feeding: Giving a child other foods (solid or semi-solid) in addition to breastfeeding or replacement feeding to meet baby’s nutrient requirements from 6 months Weaning: The process of introducing the infant to other foods while reducing the supply of breast milk (over course of 1 month) Re-lactating: Re-establishing breastfeeding after a mother had stopped, whether in the recent or distant past
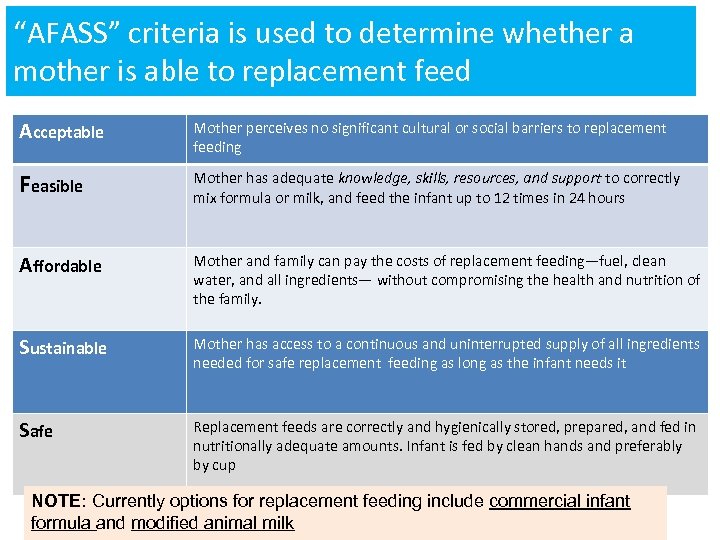 “AFASS” criteria is used to determine whether a mother is able to replacement feed Acceptable Mother perceives no significant cultural or social barriers to replacement feeding Feasible Mother has adequate knowledge, skills, resources, and support to correctly mix formula or milk, and feed the infant up to 12 times in 24 hours Affordable Mother and family can pay the costs of replacement feeding—fuel, clean water, and all ingredients— without compromising the health and nutrition of the family. Sustainable Mother has access to a continuous and uninterrupted supply of all ingredients needed for safe replacement feeding as long as the infant needs it Safe Replacement feeds are correctly and hygienically stored, prepared, and fed in nutritionally adequate amounts. Infant is fed by clean hands and preferably by cup NOTE: Currently options for replacement feeding include commercial infant formula and modified animal milk
“AFASS” criteria is used to determine whether a mother is able to replacement feed Acceptable Mother perceives no significant cultural or social barriers to replacement feeding Feasible Mother has adequate knowledge, skills, resources, and support to correctly mix formula or milk, and feed the infant up to 12 times in 24 hours Affordable Mother and family can pay the costs of replacement feeding—fuel, clean water, and all ingredients— without compromising the health and nutrition of the family. Sustainable Mother has access to a continuous and uninterrupted supply of all ingredients needed for safe replacement feeding as long as the infant needs it Safe Replacement feeds are correctly and hygienically stored, prepared, and fed in nutritionally adequate amounts. Infant is fed by clean hands and preferably by cup NOTE: Currently options for replacement feeding include commercial infant formula and modified animal milk
 Why breastfeed for 12 months? 12 months represents the duration for most HIVinfected mothers that gives the maximum benefit of breastfeeding in terms of survival (excluding any consideration of HIV transmission). In the presence of ARV intervention to reduce risk of transmission, this combination may give best balance of protection vs. risk
Why breastfeed for 12 months? 12 months represents the duration for most HIVinfected mothers that gives the maximum benefit of breastfeeding in terms of survival (excluding any consideration of HIV transmission). In the presence of ARV intervention to reduce risk of transmission, this combination may give best balance of protection vs. risk
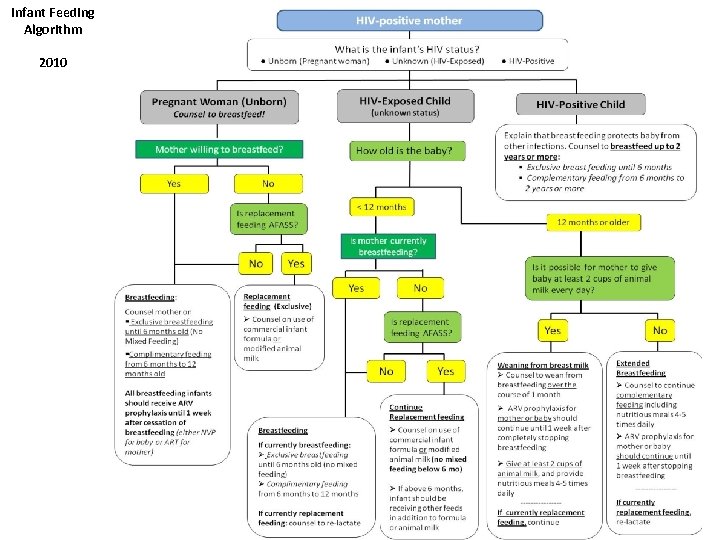 Infant Feeding Algorithm 2010 34
Infant Feeding Algorithm 2010 34
 Exercise: Practice using the Infant Feeding Algorithm to offer correct feeding advice 1) Work in pairs 2) Use your Job Aid: Infant Feeding Algorithm 3) Answer the case questions in your Guide.
Exercise: Practice using the Infant Feeding Algorithm to offer correct feeding advice 1) Work in pairs 2) Use your Job Aid: Infant Feeding Algorithm 3) Answer the case questions in your Guide.
 Use the Infant Feeding Algorithm! Case #1: You are discussing infant feeding with a newly tested positive pregnant woman in the ANC. She says she is worried about transmitting HIV through breast milk. You also have assessed that she can meet the AFASS criteria for replacement feeding. What counseling messages do you give her about feeding the baby after delivery? She will use formula or animal milk Need to discuss: Frequency, Quantity, Safety/free of contamination, Composition, Micro nutrient supplementation, Growth monitoring, Other clinical care 36
Use the Infant Feeding Algorithm! Case #1: You are discussing infant feeding with a newly tested positive pregnant woman in the ANC. She says she is worried about transmitting HIV through breast milk. You also have assessed that she can meet the AFASS criteria for replacement feeding. What counseling messages do you give her about feeding the baby after delivery? She will use formula or animal milk Need to discuss: Frequency, Quantity, Safety/free of contamination, Composition, Micro nutrient supplementation, Growth monitoring, Other clinical care 36
 Case #2: Infant Feeding An HIV-infected mother of a 6 month old baby attends the clinic. She has been exclusively breastfeeding her baby while giving NVP prophylaxis each day. She asks how she should feed her baby. According to the new feeding guidelines, what do you advise/tell her? Introduce complementary feeds Discuss possibility of re-lactating Continue with daily NVP Discuss: Frequency, Quantity, Safety/free of contamination, Composition, Micro nutrient supplementation, Growth Monitoring, Other clinical
Case #2: Infant Feeding An HIV-infected mother of a 6 month old baby attends the clinic. She has been exclusively breastfeeding her baby while giving NVP prophylaxis each day. She asks how she should feed her baby. According to the new feeding guidelines, what do you advise/tell her? Introduce complementary feeds Discuss possibility of re-lactating Continue with daily NVP Discuss: Frequency, Quantity, Safety/free of contamination, Composition, Micro nutrient supplementation, Growth Monitoring, Other clinical
 Case #3: Infant Feeding An HIV-infected mother of a 12 month old baby attends the clinic. She has been breastfeeding the baby since birth— exclusively for 6 months, and adding complimentary feeds after that. How do you assess whether she should wean the baby from breast milk or continue breastfeeding? Availability of enough complimentary feeds Has the child’s HIV status been determined Safe Growth pattern Feasibility
Case #3: Infant Feeding An HIV-infected mother of a 12 month old baby attends the clinic. She has been breastfeeding the baby since birth— exclusively for 6 months, and adding complimentary feeds after that. How do you assess whether she should wean the baby from breast milk or continue breastfeeding? Availability of enough complimentary feeds Has the child’s HIV status been determined Safe Growth pattern Feasibility
 Case #4: Infant Feeding An HIV infected mother of a 5 month old baby comes to your clinic with a positive HIV DNA PCR result and a referral letter to get her baby enrolled into care. She is concerned about how to feed her baby and was planning to stop breast feeding at 6 months of age. How do you make a decision on which feeding option she will use? What advise would you give her to ensure appropriate growth? Exclusively breast feed for 6 months Introduce complimentary feeds after 6 months Re-affirm the benefits of breast feeding Ensure that the child is started on HAART Re-test the child to as per the HIV testing algorithm for children under 18 months
Case #4: Infant Feeding An HIV infected mother of a 5 month old baby comes to your clinic with a positive HIV DNA PCR result and a referral letter to get her baby enrolled into care. She is concerned about how to feed her baby and was planning to stop breast feeding at 6 months of age. How do you make a decision on which feeding option she will use? What advise would you give her to ensure appropriate growth? Exclusively breast feed for 6 months Introduce complimentary feeds after 6 months Re-affirm the benefits of breast feeding Ensure that the child is started on HAART Re-test the child to as per the HIV testing algorithm for children under 18 months
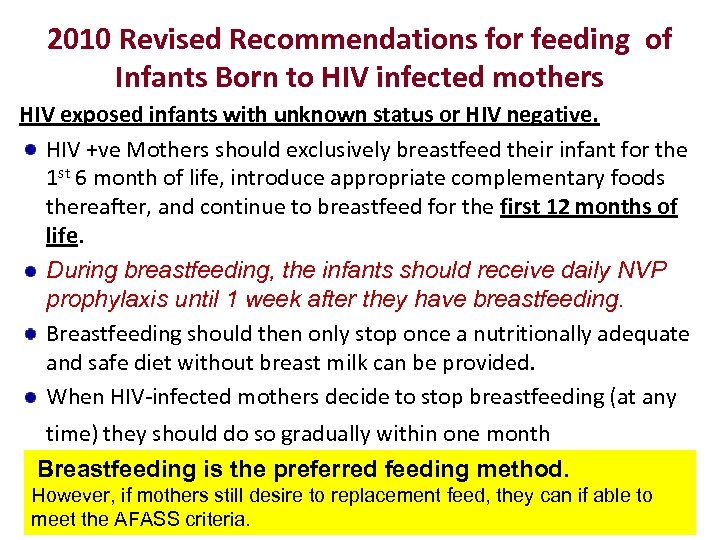 2010 Revised Recommendations for feeding of Infants Born to HIV infected mothers HIV exposed infants with unknown status or HIV negative. HIV +ve Mothers should exclusively breastfeed their infant for the 1 st 6 month of life, introduce appropriate complementary foods thereafter, and continue to breastfeed for the first 12 months of life. During breastfeeding, the infants should receive daily NVP prophylaxis until 1 week after they have breastfeeding. Breastfeeding should then only stop once a nutritionally adequate and safe diet without breast milk can be provided. When HIV-infected mothers decide to stop breastfeeding (at any time) they should do so gradually within one month Breastfeeding is the preferred feeding method. However, if mothers still desire to replacement feed, they can if able to meet the AFASS criteria.
2010 Revised Recommendations for feeding of Infants Born to HIV infected mothers HIV exposed infants with unknown status or HIV negative. HIV +ve Mothers should exclusively breastfeed their infant for the 1 st 6 month of life, introduce appropriate complementary foods thereafter, and continue to breastfeed for the first 12 months of life. During breastfeeding, the infants should receive daily NVP prophylaxis until 1 week after they have breastfeeding. Breastfeeding should then only stop once a nutritionally adequate and safe diet without breast milk can be provided. When HIV-infected mothers decide to stop breastfeeding (at any time) they should do so gradually within one month Breastfeeding is the preferred feeding method. However, if mothers still desire to replacement feed, they can if able to meet the AFASS criteria.


