5aa535ef28f0e6ae782b6d2dae231ea8.ppt
- Количество слайдов: 39
 The Stealth Geriatrician: How to learn what you need to know from your patients Tiffany Shubert, Ph. D. , MPT Zeke Zamora, MD Anthony Caprio, MD
The Stealth Geriatrician: How to learn what you need to know from your patients Tiffany Shubert, Ph. D. , MPT Zeke Zamora, MD Anthony Caprio, MD
 Course Objectives n Define “geriatric syndrome” n Identify key risk factors for falling n n n Perform a comprehensive geriatric functional assessment Identify appropriate interventions “Build a Team” – Determine disciplines, community resources, and evidence-based programs to manage patient health
Course Objectives n Define “geriatric syndrome” n Identify key risk factors for falling n n n Perform a comprehensive geriatric functional assessment Identify appropriate interventions “Build a Team” – Determine disciplines, community resources, and evidence-based programs to manage patient health
 Why falls? > 35% of your patients fall annually AAMC Minimum Competency n All adults over 65 years should be asked a falls history n All adults should be observed and assessed rising from a chair and walking n All patients who have fallen or at risk of falling should have a differential diagnosis and evaluation plan
Why falls? > 35% of your patients fall annually AAMC Minimum Competency n All adults over 65 years should be asked a falls history n All adults should be observed and assessed rising from a chair and walking n All patients who have fallen or at risk of falling should have a differential diagnosis and evaluation plan
 Standard of Care AGS/BMJ Practice Guidelines http: //www. medcats. com/FALLS/frameset. htm n All older adults screened for falls by health care provider n Key questions n n Two or more falls in prior 12 months Presents with acute fall Difficulty with walking or balance If yes to any question, then comprehensive falls assessment 4
Standard of Care AGS/BMJ Practice Guidelines http: //www. medcats. com/FALLS/frameset. htm n All older adults screened for falls by health care provider n Key questions n n Two or more falls in prior 12 months Presents with acute fall Difficulty with walking or balance If yes to any question, then comprehensive falls assessment 4
 Who is going to fall?
Who is going to fall?
 How do you identify fallers?
How do you identify fallers?
 Comprehensive Falls Risk = Comprehensive Geriatric Assessment n n n History of falls Medications Gait, balance, mobility Visual acuity Other neurological impairments n n n Muscle strength Heart rate/rhythm Postural hypotension Feet and footware Environmental hazards http: //www. medcats. com/FALLS/frameset. htm
Comprehensive Falls Risk = Comprehensive Geriatric Assessment n n n History of falls Medications Gait, balance, mobility Visual acuity Other neurological impairments n n n Muscle strength Heart rate/rhythm Postural hypotension Feet and footware Environmental hazards http: //www. medcats. com/FALLS/frameset. htm
 Comprehensive geriatric assessment = falls risk
Comprehensive geriatric assessment = falls risk
 A comprehensive exam: A standard review of systems = limited information Functional assessment and a comprehensive exam will identify multiple factors contributing to falls
A comprehensive exam: A standard review of systems = limited information Functional assessment and a comprehensive exam will identify multiple factors contributing to falls
 Geriatric Syndromes n Multiple underlying factors (interacting causes) affecting multiple systems ü n n Delirium, Incontinence, Frailty, Falls Shared risk factors such as older age, cognitive impairment, functional impairment Falls as a geriatric syndrome ü ü Dizziness, auditory, hearing Cardiovascular Orthopedic, arthritis, neuropathy Depression, cognitive impairment
Geriatric Syndromes n Multiple underlying factors (interacting causes) affecting multiple systems ü n n Delirium, Incontinence, Frailty, Falls Shared risk factors such as older age, cognitive impairment, functional impairment Falls as a geriatric syndrome ü ü Dizziness, auditory, hearing Cardiovascular Orthopedic, arthritis, neuropathy Depression, cognitive impairment
 Introducing Mrs. Jones
Introducing Mrs. Jones
 Chief Complaint n It depends on who you ask: n Patient: “No complaints, I feel fine” n Daughter: “Difficulty getting around the house, I am afraid she may fall” n MD: “Blood pressure should be better controlled”
Chief Complaint n It depends on who you ask: n Patient: “No complaints, I feel fine” n Daughter: “Difficulty getting around the house, I am afraid she may fall” n MD: “Blood pressure should be better controlled”
 History of Present Illness n What do you want to know? n Previous Falls n Changes in medications n Trips to the opthamologist n Trips to the ER n Changes in mood/activity levels
History of Present Illness n What do you want to know? n Previous Falls n Changes in medications n Trips to the opthamologist n Trips to the ER n Changes in mood/activity levels
 Past Medical History n n n Hypertension Paroxysmal Atrial Fibrillation Chronic Renal Insufficiency Anxiety/Depression “Dizziness” Osteoporosis
Past Medical History n n n Hypertension Paroxysmal Atrial Fibrillation Chronic Renal Insufficiency Anxiety/Depression “Dizziness” Osteoporosis
 Medication List n n n Metoprolol Hydrochlorothiazide Digoxin Warfarin Sertraline n n n Diazepam Zolpidem Meclizine Fosinopril Alendronate
Medication List n n n Metoprolol Hydrochlorothiazide Digoxin Warfarin Sertraline n n n Diazepam Zolpidem Meclizine Fosinopril Alendronate
 Medication Review n > 4 Drugs = Increased risk of falls n Red Flags – Classes that increase falls risk n Benzodiazepines (short and long-acting agents) n Antidepressants (tricyclics and SSRIs) n Antipsychotics n Anticonvulsants n Opioids n Antispasmodics n Over the counter medications
Medication Review n > 4 Drugs = Increased risk of falls n Red Flags – Classes that increase falls risk n Benzodiazepines (short and long-acting agents) n Antidepressants (tricyclics and SSRIs) n Antipsychotics n Anticonvulsants n Opioids n Antispasmodics n Over the counter medications
 Social History n What do you want to know? n Living Situation n Type n Social of house? Stairs? ADLs, IADLs Supports n Economic Status n Smoke/Drink n Current Activity Level n Fear of Falling
Social History n What do you want to know? n Living Situation n Type n Social of house? Stairs? ADLs, IADLs Supports n Economic Status n Smoke/Drink n Current Activity Level n Fear of Falling
 Activities of Daily Living: Ask or Observe n ADLs n IADLS n Transferring n Transportation n Toileting n Use the phone n Bathing n Buy groceries n Dressing n Meal preparation n Continence n Housework n Feeding n Medication n Pay bills
Activities of Daily Living: Ask or Observe n ADLs n IADLS n Transferring n Transportation n Toileting n Use the phone n Bathing n Buy groceries n Dressing n Meal preparation n Continence n Housework n Feeding n Medication n Pay bills
 Physical Exam Findings n n General Impression Vital Signs n n HEENT n n n Bilateral cataracts, difficulty reading magazine and wall poster CV n n BP sitting 140/90, HR 88 BP standing 110/80, HR 100 Pain Grade II/VI systolic murmur (right upper sternal border) MS Neuro
Physical Exam Findings n n General Impression Vital Signs n n HEENT n n n Bilateral cataracts, difficulty reading magazine and wall poster CV n n BP sitting 140/90, HR 88 BP standing 110/80, HR 100 Pain Grade II/VI systolic murmur (right upper sternal border) MS Neuro
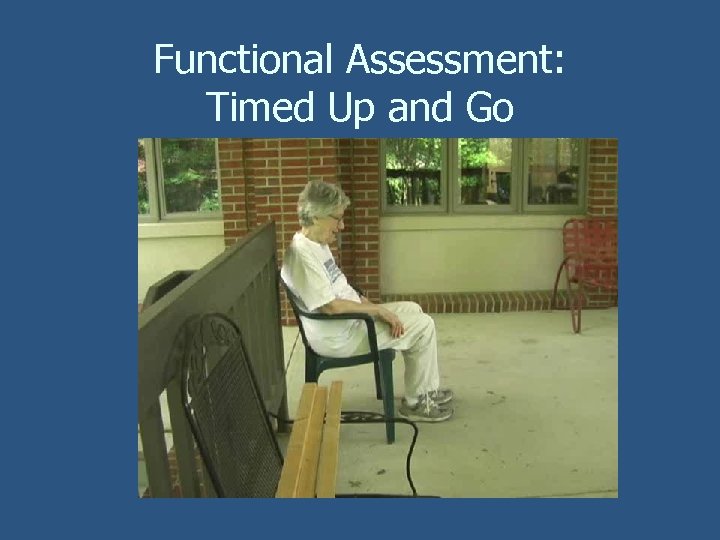 Functional Assessment: Timed Up and Go
Functional Assessment: Timed Up and Go
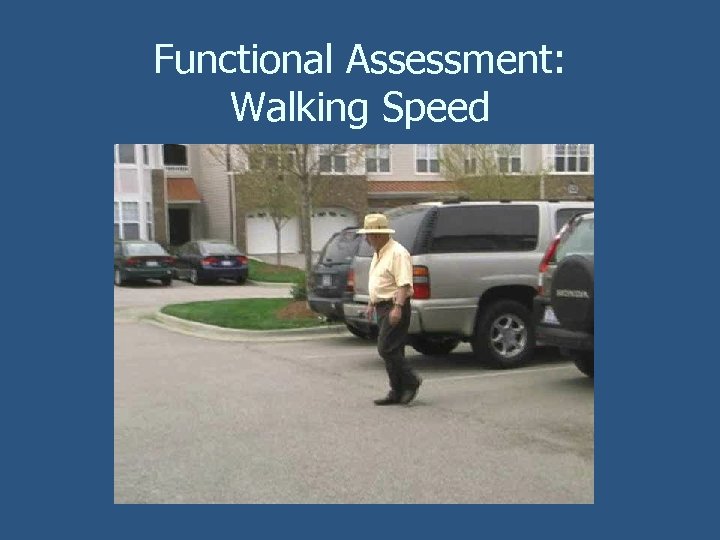 Functional Assessment: Walking Speed
Functional Assessment: Walking Speed
 Functional Assessment: Timed Chair Rise
Functional Assessment: Timed Chair Rise
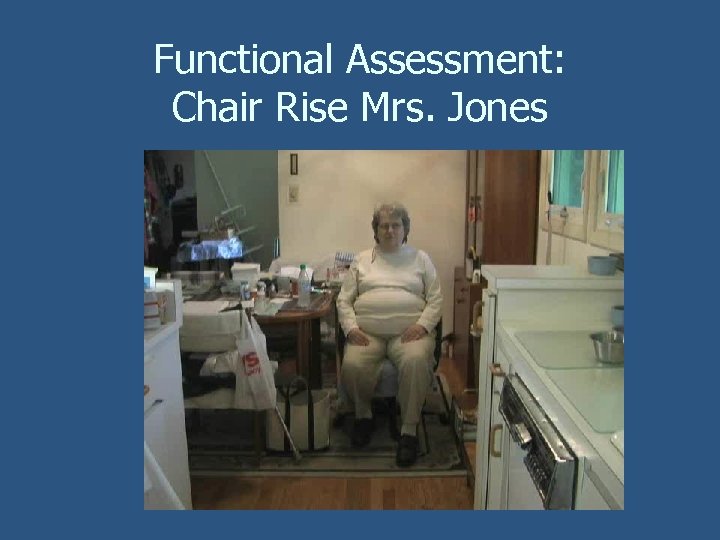 Functional Assessment: Chair Rise Mrs. Jones
Functional Assessment: Chair Rise Mrs. Jones
 Functional Assessment: Balance
Functional Assessment: Balance
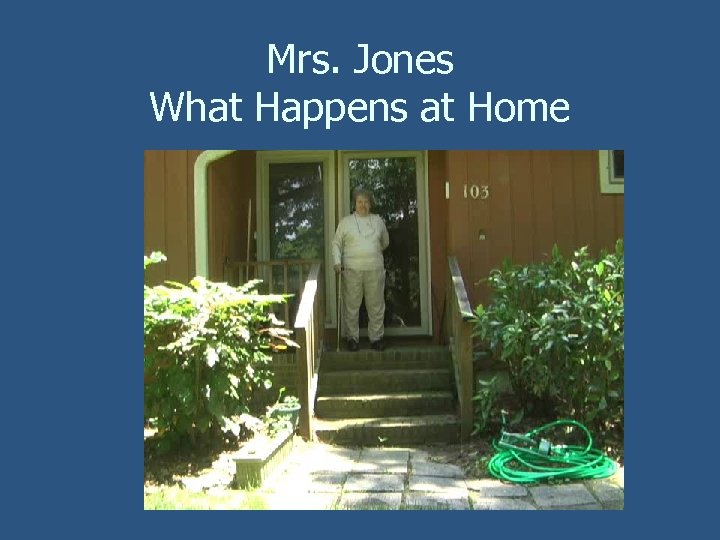 Mrs. Jones What Happens at Home
Mrs. Jones What Happens at Home
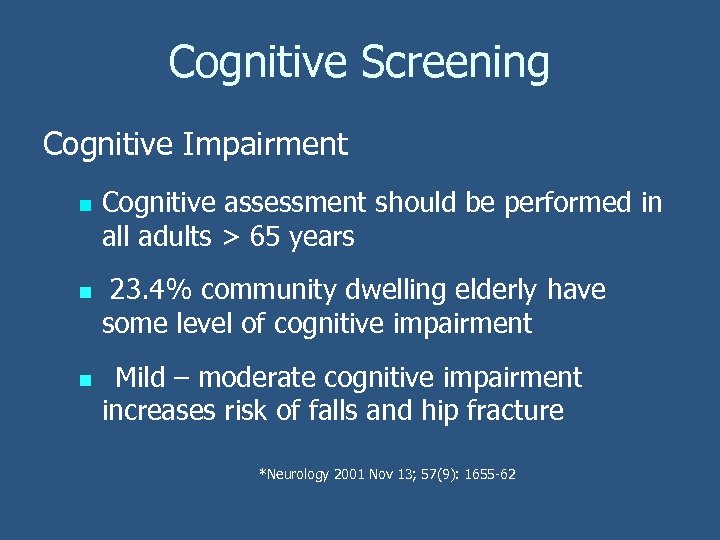 Cognitive Screening Cognitive Impairment n n n Cognitive assessment should be performed in all adults > 65 years 23. 4% community dwelling elderly have some level of cognitive impairment Mild – moderate cognitive impairment increases risk of falls and hip fracture *Neurology 2001 Nov 13; 57(9): 1655 -62
Cognitive Screening Cognitive Impairment n n n Cognitive assessment should be performed in all adults > 65 years 23. 4% community dwelling elderly have some level of cognitive impairment Mild – moderate cognitive impairment increases risk of falls and hip fracture *Neurology 2001 Nov 13; 57(9): 1655 -62
 Screening Tools: MMSE n Screens for Alzheimer’s Disease § § § n Orientation Registration Attention/Calculation Recall Language Copy Pentagons Limitations n n Age, education, cultural, socioeconomic, English proficiency affects scores Length to administer
Screening Tools: MMSE n Screens for Alzheimer’s Disease § § § n Orientation Registration Attention/Calculation Recall Language Copy Pentagons Limitations n n Age, education, cultural, socioeconomic, English proficiency affects scores Length to administer
 Screening Tools: Mini-Cog General screen for cognitive impairment 1. 2. 3. Dictate three items, ask to repeat Clock Drawing Test Ask to recall the three items
Screening Tools: Mini-Cog General screen for cognitive impairment 1. 2. 3. Dictate three items, ask to repeat Clock Drawing Test Ask to recall the three items
 Screening Tools: Mini-Cog n n Score 1 point for each recalled word Score normal/abnormal clock draw § § Score of 0 positive screen for dementia Score of 1 or 2 with abnormal clock draw positive screen for dementia Score of 1 or 2 with normal clock negative for screen for dementia Score of 3 negative screen for dementia
Screening Tools: Mini-Cog n n Score 1 point for each recalled word Score normal/abnormal clock draw § § Score of 0 positive screen for dementia Score of 1 or 2 with abnormal clock draw positive screen for dementia Score of 1 or 2 with normal clock negative for screen for dementia Score of 3 negative screen for dementia
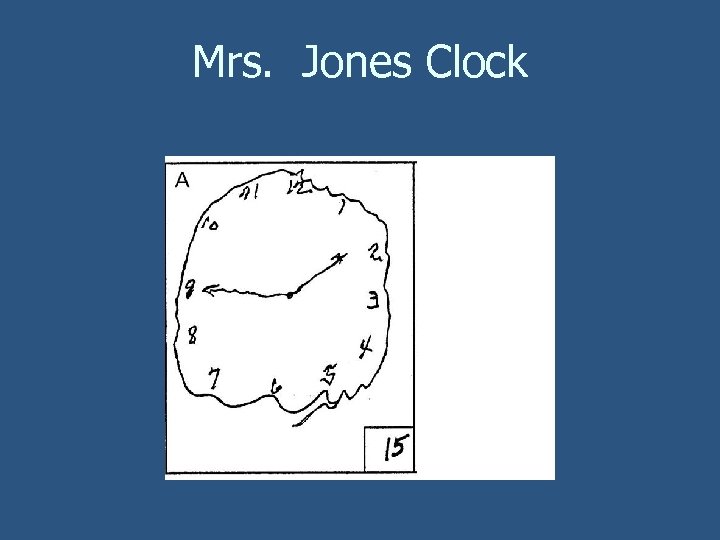 Mrs. Jones Clock
Mrs. Jones Clock
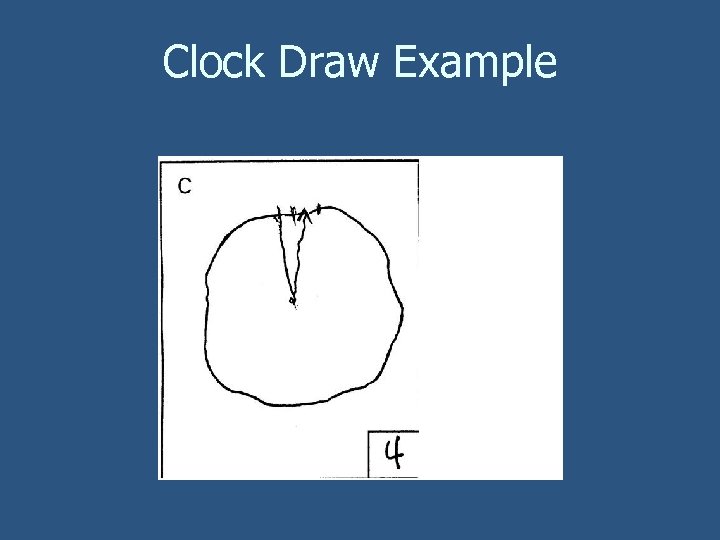 Clock Draw Example
Clock Draw Example
 Home Safety Evaluation n Use an environmental assessment sheet Must utilize occupational therapy, social work, etc to have an effect Financial difficulties may be culprit
Home Safety Evaluation n Use an environmental assessment sheet Must utilize occupational therapy, social work, etc to have an effect Financial difficulties may be culprit
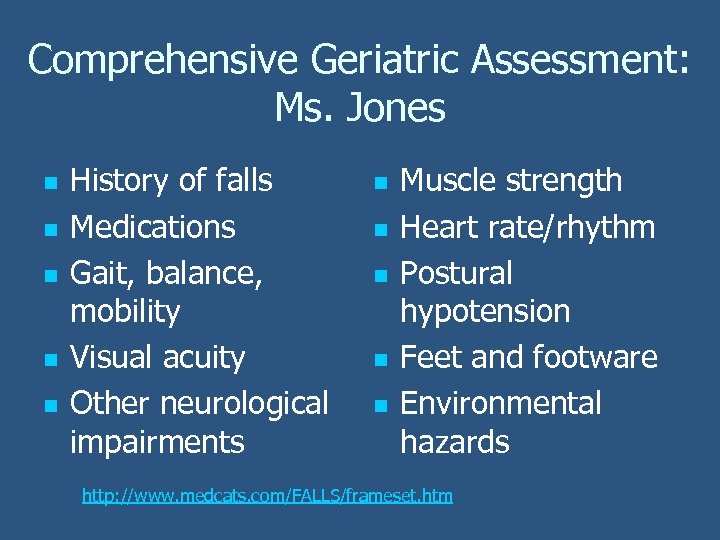 Comprehensive Geriatric Assessment: Ms. Jones n n n History of falls Medications Gait, balance, mobility Visual acuity Other neurological impairments n n n Muscle strength Heart rate/rhythm Postural hypotension Feet and footware Environmental hazards http: //www. medcats. com/FALLS/frameset. htm
Comprehensive Geriatric Assessment: Ms. Jones n n n History of falls Medications Gait, balance, mobility Visual acuity Other neurological impairments n n n Muscle strength Heart rate/rhythm Postural hypotension Feet and footware Environmental hazards http: //www. medcats. com/FALLS/frameset. htm
 Assessment: Mrs. Jones n What are the risk factors? n History of falls n Leg muscle weakness n Polypharmacy n Orthostatic Hypotension n Osteoporosis n ? Cognition
Assessment: Mrs. Jones n What are the risk factors? n History of falls n Leg muscle weakness n Polypharmacy n Orthostatic Hypotension n Osteoporosis n ? Cognition
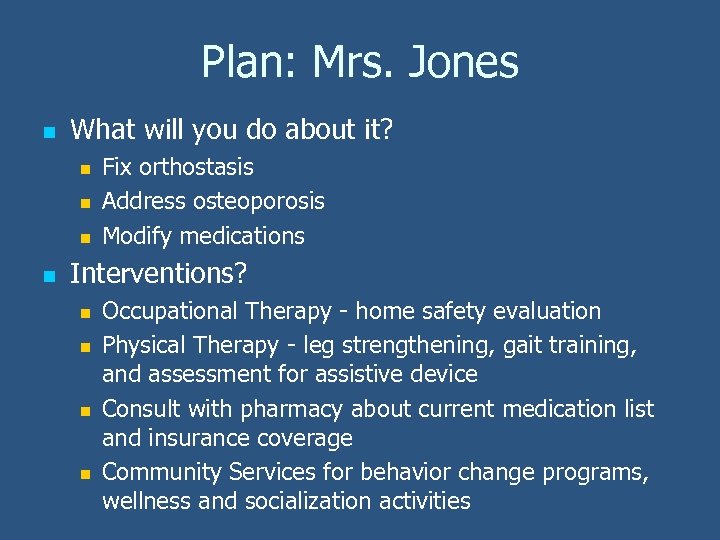 Plan: Mrs. Jones n What will you do about it? n n Fix orthostasis Address osteoporosis Modify medications Interventions? n n Occupational Therapy - home safety evaluation Physical Therapy - leg strengthening, gait training, and assessment for assistive device Consult with pharmacy about current medication list and insurance coverage Community Services for behavior change programs, wellness and socialization activities
Plan: Mrs. Jones n What will you do about it? n n Fix orthostasis Address osteoporosis Modify medications Interventions? n n Occupational Therapy - home safety evaluation Physical Therapy - leg strengthening, gait training, and assessment for assistive device Consult with pharmacy about current medication list and insurance coverage Community Services for behavior change programs, wellness and socialization activities
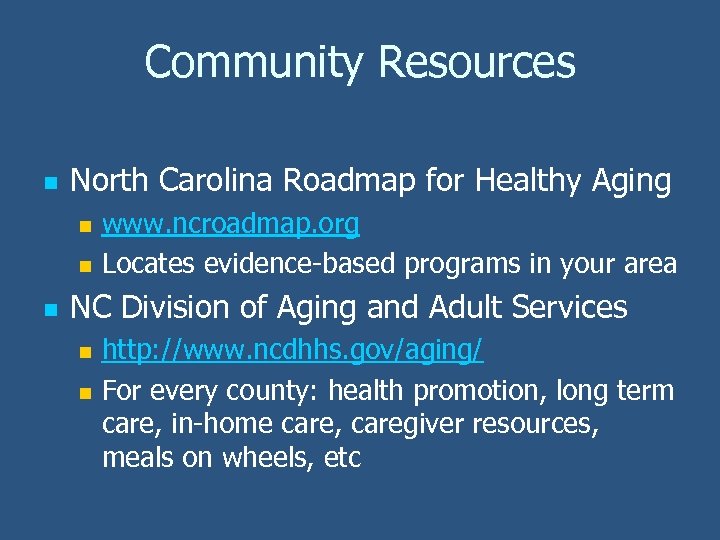 Community Resources n North Carolina Roadmap for Healthy Aging n n n www. ncroadmap. org Locates evidence-based programs in your area NC Division of Aging and Adult Services n n http: //www. ncdhhs. gov/aging/ For every county: health promotion, long term care, in-home care, caregiver resources, meals on wheels, etc
Community Resources n North Carolina Roadmap for Healthy Aging n n n www. ncroadmap. org Locates evidence-based programs in your area NC Division of Aging and Adult Services n n http: //www. ncdhhs. gov/aging/ For every county: health promotion, long term care, in-home care, caregiver resources, meals on wheels, etc
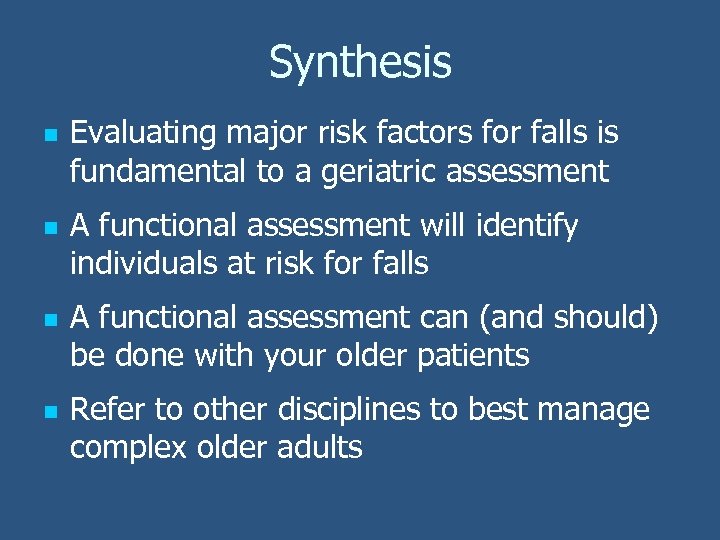 Synthesis n n Evaluating major risk factors for falls is fundamental to a geriatric assessment A functional assessment will identify individuals at risk for falls A functional assessment can (and should) be done with your older patients Refer to other disciplines to best manage complex older adults
Synthesis n n Evaluating major risk factors for falls is fundamental to a geriatric assessment A functional assessment will identify individuals at risk for falls A functional assessment can (and should) be done with your older patients Refer to other disciplines to best manage complex older adults
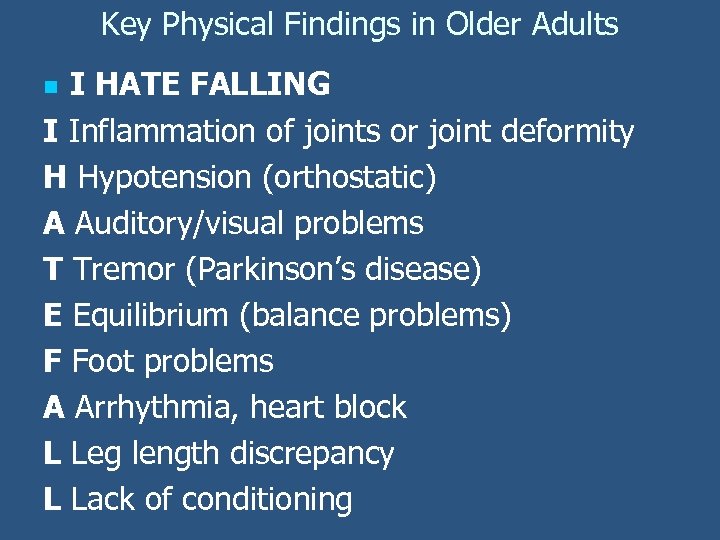 Key Physical Findings in Older Adults I HATE FALLING I Inflammation of joints or joint deformity H Hypotension (orthostatic) A Auditory/visual problems T Tremor (Parkinson’s disease) E Equilibrium (balance problems) F Foot problems A Arrhythmia, heart block L Leg length discrepancy L Lack of conditioning n
Key Physical Findings in Older Adults I HATE FALLING I Inflammation of joints or joint deformity H Hypotension (orthostatic) A Auditory/visual problems T Tremor (Parkinson’s disease) E Equilibrium (balance problems) F Foot problems A Arrhythmia, heart block L Leg length discrepancy L Lack of conditioning n
 Practice n Practice with volunteers n n Physical, Cognitive, and Medication Assessment On the wards Perform at least one mini-Cog n Shadow a physical therapist and perform 1 -2 functional assessments n Identify which of your patients are at risk for falls n
Practice n Practice with volunteers n n Physical, Cognitive, and Medication Assessment On the wards Perform at least one mini-Cog n Shadow a physical therapist and perform 1 -2 functional assessments n Identify which of your patients are at risk for falls n


