7de68d6579f5a1519e4158a2101d2e1c.ppt
- Количество слайдов: 37
 The State of Mental Health in Guilford County A presentation to the Moses Cone-Wesley Long Community Health Foundation April 29, 2010 Kelly N. Graves, Ph. D Anne Buford, MPA, NCC, LPC Sonja Frison, Ph. D, MPH Amanda Ireland, MA Terri L. Shelton, Ph. D
The State of Mental Health in Guilford County A presentation to the Moses Cone-Wesley Long Community Health Foundation April 29, 2010 Kelly N. Graves, Ph. D Anne Buford, MPA, NCC, LPC Sonja Frison, Ph. D, MPH Amanda Ireland, MA Terri L. Shelton, Ph. D
 Acknowledgements Erin Balkind Anderson Bean Korinne Chiu Frederick Douglas Kelley Richardson Megan Smell Claretta Witherspoon All the youth, families, providers, and agencies that assisted or participated in surveys and focus groups
Acknowledgements Erin Balkind Anderson Bean Korinne Chiu Frederick Douglas Kelley Richardson Megan Smell Claretta Witherspoon All the youth, families, providers, and agencies that assisted or participated in surveys and focus groups
 Mental Health as a Priority One of the nation’s top public health priorities Healthy People 2010 and 2020 mental health-related goals: Increase treatment access and engagement among various populations Reduce suicide attempts and completions Utilize consumer satisfaction measures Increase mental health services and referrals at primary care locations The World Health Organization (WHO, 2001, p. 1) noted that “mental health is as important as physical health to the overall well-being of individuals, societies and countries. ” Mental health is connected to physical health, quality of life, community well-being Important to treat mental illness and promote mental health Mental health as a continuum Herrman, Saxena, Moodie, & Walker, 2005; Keyes, 2007; U. S. DHHS, 2000, 2001, 2009
Mental Health as a Priority One of the nation’s top public health priorities Healthy People 2010 and 2020 mental health-related goals: Increase treatment access and engagement among various populations Reduce suicide attempts and completions Utilize consumer satisfaction measures Increase mental health services and referrals at primary care locations The World Health Organization (WHO, 2001, p. 1) noted that “mental health is as important as physical health to the overall well-being of individuals, societies and countries. ” Mental health is connected to physical health, quality of life, community well-being Important to treat mental illness and promote mental health Mental health as a continuum Herrman, Saxena, Moodie, & Walker, 2005; Keyes, 2007; U. S. DHHS, 2000, 2001, 2009
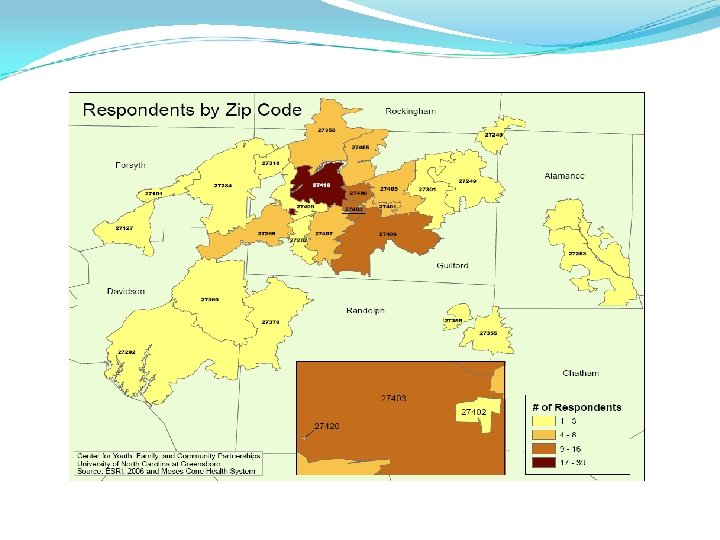
 Methodological Approach Review of national, state, and local data/trends Including preliminary examination of resources/gaps Implementation of participatory action research framework: Six focus groups Nine key informant interviews Online community survey, conducted through snowball sampling (N = 206) Feedback from community forums
Methodological Approach Review of national, state, and local data/trends Including preliminary examination of resources/gaps Implementation of participatory action research framework: Six focus groups Nine key informant interviews Online community survey, conducted through snowball sampling (N = 206) Feedback from community forums
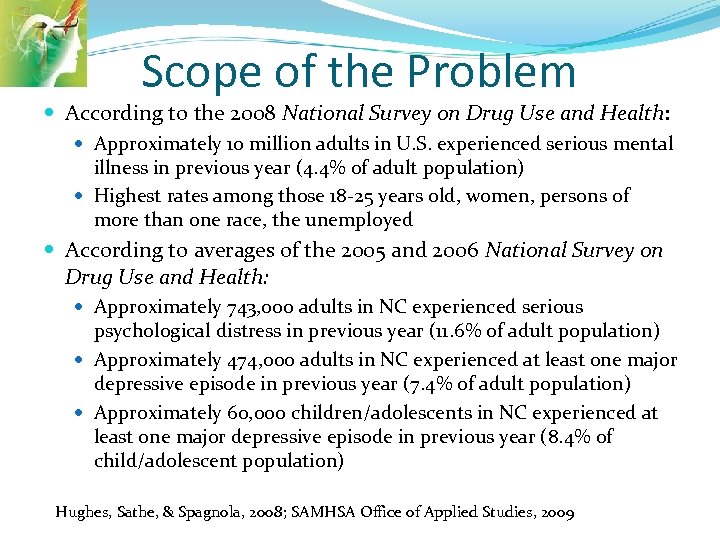 Scope of the Problem According to the 2008 National Survey on Drug Use and Health: Approximately 10 million adults in U. S. experienced serious mental illness in previous year (4. 4% of adult population) Highest rates among those 18 -25 years old, women, persons of more than one race, the unemployed According to averages of the 2005 and 2006 National Survey on Drug Use and Health: Approximately 743, 000 adults in NC experienced serious psychological distress in previous year (11. 6% of adult population) Approximately 474, 000 adults in NC experienced at least one major depressive episode in previous year (7. 4% of adult population) Approximately 60, 000 children/adolescents in NC experienced at least one major depressive episode in previous year (8. 4% of child/adolescent population) Hughes, Sathe, & Spagnola, 2008; SAMHSA Office of Applied Studies, 2009
Scope of the Problem According to the 2008 National Survey on Drug Use and Health: Approximately 10 million adults in U. S. experienced serious mental illness in previous year (4. 4% of adult population) Highest rates among those 18 -25 years old, women, persons of more than one race, the unemployed According to averages of the 2005 and 2006 National Survey on Drug Use and Health: Approximately 743, 000 adults in NC experienced serious psychological distress in previous year (11. 6% of adult population) Approximately 474, 000 adults in NC experienced at least one major depressive episode in previous year (7. 4% of adult population) Approximately 60, 000 children/adolescents in NC experienced at least one major depressive episode in previous year (8. 4% of child/adolescent population) Hughes, Sathe, & Spagnola, 2008; SAMHSA Office of Applied Studies, 2009
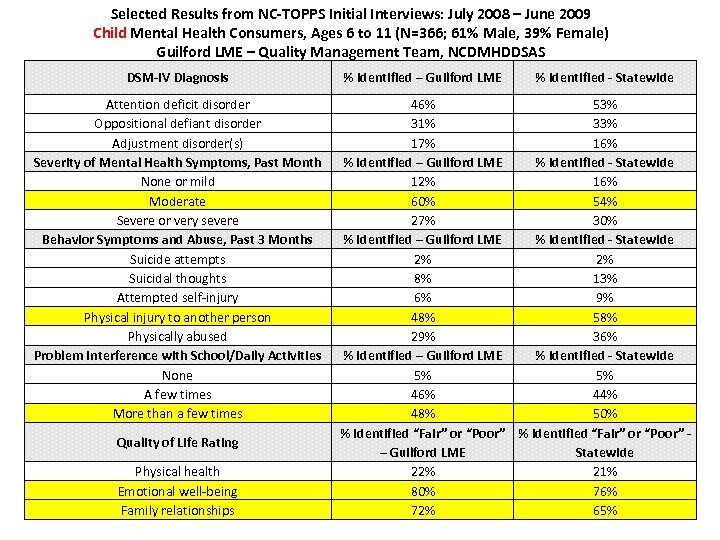 Selected Results from NC-TOPPS Initial Interviews: July 2008 – June 2009 Child Mental Health Consumers, Ages 6 to 11 (N=366; 61% Male, 39% Female) Guilford LME – Quality Management Team, NCDMHDDSAS DSM-IV Diagnosis Attention deficit disorder Oppositional defiant disorder Adjustment disorder(s) Severity of Mental Health Symptoms, Past Month None or mild Moderate Severe or very severe Behavior Symptoms and Abuse, Past 3 Months Suicide attempts Suicidal thoughts Attempted self-injury Physical injury to another person Physically abused Problem Interference with School/Daily Activities None A few times More than a few times Quality of Life Rating Physical health Emotional well-being Family relationships % Identified – Guilford LME % Identified - Statewide 46% 53% 31% 33% 17% 16% % Identified – Guilford LME % Identified - Statewide 12% 16% 60% 54% 27% 30% % Identified – Guilford LME % Identified - Statewide 2% 2% 8% 13% 6% 9% 48% 58% 29% 36% % Identified – Guilford LME % Identified - Statewide 5% 5% 46% 44% 48% 50% % Identified “Fair” or “Poor” – Guilford LME Statewide 22% 21% 80% 76% 72% 65%
Selected Results from NC-TOPPS Initial Interviews: July 2008 – June 2009 Child Mental Health Consumers, Ages 6 to 11 (N=366; 61% Male, 39% Female) Guilford LME – Quality Management Team, NCDMHDDSAS DSM-IV Diagnosis Attention deficit disorder Oppositional defiant disorder Adjustment disorder(s) Severity of Mental Health Symptoms, Past Month None or mild Moderate Severe or very severe Behavior Symptoms and Abuse, Past 3 Months Suicide attempts Suicidal thoughts Attempted self-injury Physical injury to another person Physically abused Problem Interference with School/Daily Activities None A few times More than a few times Quality of Life Rating Physical health Emotional well-being Family relationships % Identified – Guilford LME % Identified - Statewide 46% 53% 31% 33% 17% 16% % Identified – Guilford LME % Identified - Statewide 12% 16% 60% 54% 27% 30% % Identified – Guilford LME % Identified - Statewide 2% 2% 8% 13% 6% 9% 48% 58% 29% 36% % Identified – Guilford LME % Identified - Statewide 5% 5% 46% 44% 48% 50% % Identified “Fair” or “Poor” – Guilford LME Statewide 22% 21% 80% 76% 72% 65%
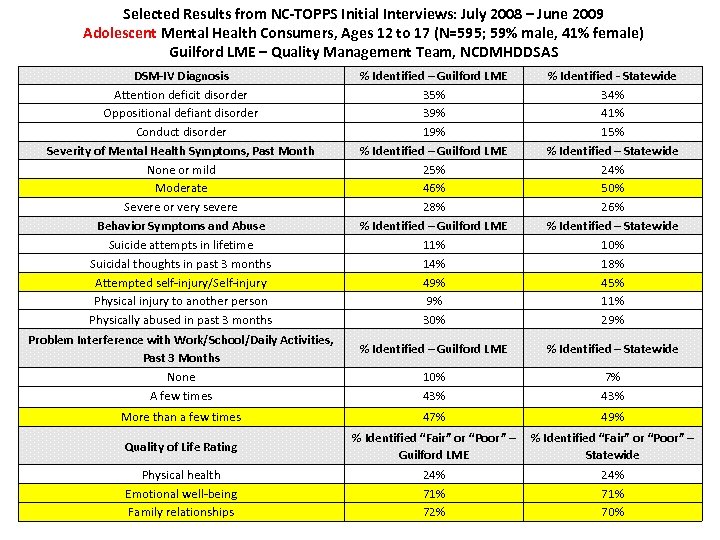 Selected Results from NC-TOPPS Initial Interviews: July 2008 – June 2009 Adolescent Mental Health Consumers, Ages 12 to 17 (N=595; 59% male, 41% female) Guilford LME – Quality Management Team, NCDMHDDSAS DSM-IV Diagnosis Attention deficit disorder Oppositional defiant disorder Conduct disorder Severity of Mental Health Symptoms, Past Month None or mild Moderate Severe or very severe Behavior Symptoms and Abuse Suicide attempts in lifetime Suicidal thoughts in past 3 months Attempted self-injury/Self-injury Physical injury to another person Physically abused in past 3 months Problem Interference with Work/School/Daily Activities, Past 3 Months None A few times More than a few times Quality of Life Rating Physical health Emotional well-being Family relationships % Identified – Guilford LME 35% 39% 19% % Identified – Guilford LME 25% 46% 28% % Identified – Guilford LME 11% 14% 49% 9% 30% % Identified - Statewide 34% 41% 15% % Identified – Statewide 24% 50% 26% % Identified – Statewide 10% 18% 45% 11% 29% % Identified – Guilford LME % Identified – Statewide 10% 43% 7% 43% 47% 49% % Identified “Fair” or “Poor” – Guilford LME 24% 71% 72% % Identified “Fair” or “Poor” – Statewide 24% 71% 70%
Selected Results from NC-TOPPS Initial Interviews: July 2008 – June 2009 Adolescent Mental Health Consumers, Ages 12 to 17 (N=595; 59% male, 41% female) Guilford LME – Quality Management Team, NCDMHDDSAS DSM-IV Diagnosis Attention deficit disorder Oppositional defiant disorder Conduct disorder Severity of Mental Health Symptoms, Past Month None or mild Moderate Severe or very severe Behavior Symptoms and Abuse Suicide attempts in lifetime Suicidal thoughts in past 3 months Attempted self-injury/Self-injury Physical injury to another person Physically abused in past 3 months Problem Interference with Work/School/Daily Activities, Past 3 Months None A few times More than a few times Quality of Life Rating Physical health Emotional well-being Family relationships % Identified – Guilford LME 35% 39% 19% % Identified – Guilford LME 25% 46% 28% % Identified – Guilford LME 11% 14% 49% 9% 30% % Identified - Statewide 34% 41% 15% % Identified – Statewide 24% 50% 26% % Identified – Statewide 10% 18% 45% 11% 29% % Identified – Guilford LME % Identified – Statewide 10% 43% 7% 43% 47% 49% % Identified “Fair” or “Poor” – Guilford LME 24% 71% 72% % Identified “Fair” or “Poor” – Statewide 24% 71% 70%
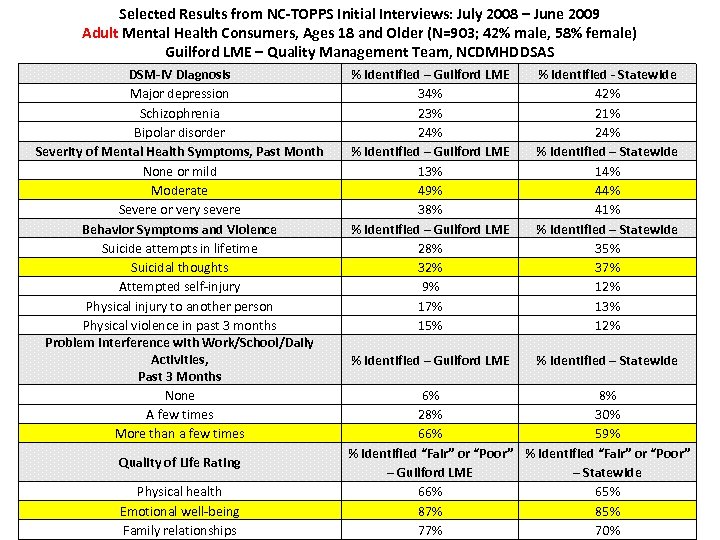 Selected Results from NC-TOPPS Initial Interviews: July 2008 – June 2009 Adult Mental Health Consumers, Ages 18 and Older (N=903; 42% male, 58% female) Guilford LME – Quality Management Team, NCDMHDDSAS DSM-IV Diagnosis Major depression Schizophrenia Bipolar disorder Severity of Mental Health Symptoms, Past Month None or mild Moderate Severe or very severe Behavior Symptoms and Violence Suicide attempts in lifetime Suicidal thoughts Attempted self-injury Physical injury to another person Physical violence in past 3 months Problem Interference with Work/School/Daily Activities, Past 3 Months None A few times More than a few times Quality of Life Rating Physical health Emotional well-being Family relationships % Identified – Guilford LME 34% 23% 24% % Identified – Guilford LME 13% 49% 38% % Identified – Guilford LME 28% 32% 9% 17% 15% % Identified - Statewide 42% 21% 24% % Identified – Statewide 14% 41% % Identified – Statewide 35% 37% 12% 13% 12% % Identified – Guilford LME % Identified – Statewide 6% 8% 28% 30% 66% 59% % Identified “Fair” or “Poor” – Guilford LME – Statewide 66% 65% 87% 85% 77% 70%
Selected Results from NC-TOPPS Initial Interviews: July 2008 – June 2009 Adult Mental Health Consumers, Ages 18 and Older (N=903; 42% male, 58% female) Guilford LME – Quality Management Team, NCDMHDDSAS DSM-IV Diagnosis Major depression Schizophrenia Bipolar disorder Severity of Mental Health Symptoms, Past Month None or mild Moderate Severe or very severe Behavior Symptoms and Violence Suicide attempts in lifetime Suicidal thoughts Attempted self-injury Physical injury to another person Physical violence in past 3 months Problem Interference with Work/School/Daily Activities, Past 3 Months None A few times More than a few times Quality of Life Rating Physical health Emotional well-being Family relationships % Identified – Guilford LME 34% 23% 24% % Identified – Guilford LME 13% 49% 38% % Identified – Guilford LME 28% 32% 9% 17% 15% % Identified - Statewide 42% 21% 24% % Identified – Statewide 14% 41% % Identified – Statewide 35% 37% 12% 13% 12% % Identified – Guilford LME % Identified – Statewide 6% 8% 28% 30% 66% 59% % Identified “Fair” or “Poor” – Guilford LME – Statewide 66% 65% 87% 85% 77% 70%
 Health Disparities Socioeconomic Level – Serious psychological stress and poverty Race/ethnicity – Prevalence - 30% more often among African American adults than non-Hispanic White adults Symptoms - Suicide attempt rates found to be almost twice as high among Hispanic adolescents (grades 9 -12) as compared to non. Hispanic White adolescents Access / Receipt of Services - Non-Hispanic White adults more often connected with mental health services (14%) than non. Hispanic Black adults (7. 4%), Hispanic adults (7. 0%), American Indian/Alaskan Native adults (10. 7%), and Asian American adults (5. 6%)
Health Disparities Socioeconomic Level – Serious psychological stress and poverty Race/ethnicity – Prevalence - 30% more often among African American adults than non-Hispanic White adults Symptoms - Suicide attempt rates found to be almost twice as high among Hispanic adolescents (grades 9 -12) as compared to non. Hispanic White adolescents Access / Receipt of Services - Non-Hispanic White adults more often connected with mental health services (14%) than non. Hispanic Black adults (7. 4%), Hispanic adults (7. 0%), American Indian/Alaskan Native adults (10. 7%), and Asian American adults (5. 6%)
 Special Populations Co-Occurring Disorders – estimates range widely in NC from 2%-68% Homeless individuals – between 20%-40% are both mentally ill and without a home (1. 4 million people in US) Point in time counts of homeless in Guilford – 1, 064 (23% are children) Adolescent parents – 57% report mental health symptoms, increased substance use Guilford County 2008 – 966 girls between 15 -19 years (3 teens each day)
Special Populations Co-Occurring Disorders – estimates range widely in NC from 2%-68% Homeless individuals – between 20%-40% are both mentally ill and without a home (1. 4 million people in US) Point in time counts of homeless in Guilford – 1, 064 (23% are children) Adolescent parents – 57% report mental health symptoms, increased substance use Guilford County 2008 – 966 girls between 15 -19 years (3 teens each day)
 Special Populations Immigrant Populations – estimates vary widely, but access, language and culture, and stigma prevent treatment in many cases Adult and juvenile justice – estimates vary widely (40%-90%), higher for females “criminalization of the mentally ill” College Populations – First time seeking services and diagnosis for many All eight colleges and universities have a counseling center and/or offer some counseling services for students, with at least crisis intervention, assessment, and/or short term counseling
Special Populations Immigrant Populations – estimates vary widely, but access, language and culture, and stigma prevent treatment in many cases Adult and juvenile justice – estimates vary widely (40%-90%), higher for females “criminalization of the mentally ill” College Populations – First time seeking services and diagnosis for many All eight colleges and universities have a counseling center and/or offer some counseling services for students, with at least crisis intervention, assessment, and/or short term counseling
 Special Populations HIV/AIDS – majority have 2 or more psychiatric diagnoses, 81% report substance use Impacts medication adherence and increased risk for suicidal behaviors Elderly – 22% of population Older, Caucasian males have highest rates of suicide in US Reductions in social contact, self-worth, and pain and frustration around physical illness
Special Populations HIV/AIDS – majority have 2 or more psychiatric diagnoses, 81% report substance use Impacts medication adherence and increased risk for suicidal behaviors Elderly – 22% of population Older, Caucasian males have highest rates of suicide in US Reductions in social contact, self-worth, and pain and frustration around physical illness
 NC’s Report Card National Alliance on Mental Illness (NAMI) – Grading the States: A Report on America’s Health Care System for Adults with Serious Mental Illness 2006 – NC received a grade of D+. Evaluation elements included: infrastructure (C-); information access (D); services (D); and recovery supports (B+) 2009 – NC received a grade of D. Evaluation elements included: health promotion/measurement (D); financing and core treatment/recovery services (C); consumer/family empowerment (F); and community integration/ social inclusion (C).
NC’s Report Card National Alliance on Mental Illness (NAMI) – Grading the States: A Report on America’s Health Care System for Adults with Serious Mental Illness 2006 – NC received a grade of D+. Evaluation elements included: infrastructure (C-); information access (D); services (D); and recovery supports (B+) 2009 – NC received a grade of D. Evaluation elements included: health promotion/measurement (D); financing and core treatment/recovery services (C); consumer/family empowerment (F); and community integration/ social inclusion (C).
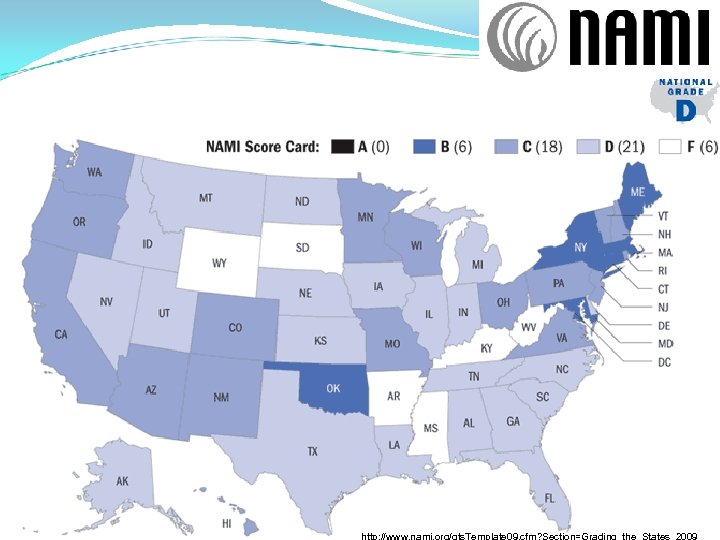 http: //www. nami. org/gts. Template 09. cfm? Section=Grading_the_States_2009
http: //www. nami. org/gts. Template 09. cfm? Section=Grading_the_States_2009
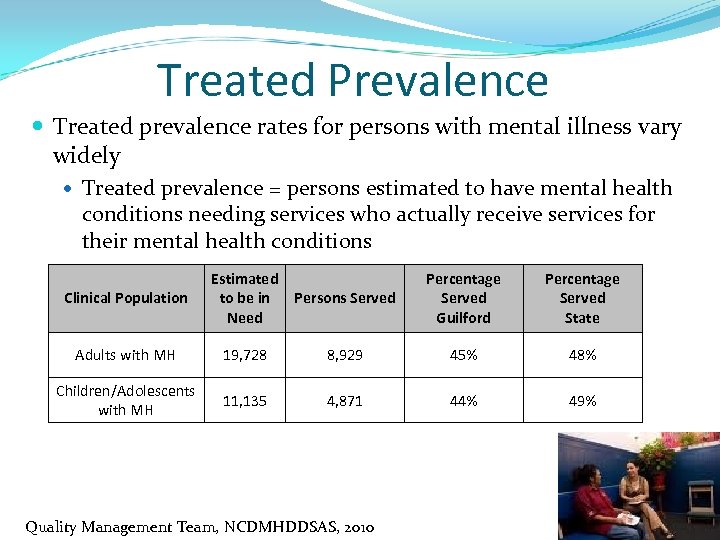 Treated Prevalence Treated prevalence rates for persons with mental illness vary widely Treated prevalence = persons estimated to have mental health conditions needing services who actually receive services for their mental health conditions Clinical Population Estimated to be in Need Persons Served Percentage Served Guilford Percentage Served State Adults with MH 19, 728 8, 929 45% 48% Children/Adolescents with MH 11, 135 4, 871 44% 49% Quality Management Team, NCDMHDDSAS, 2010
Treated Prevalence Treated prevalence rates for persons with mental illness vary widely Treated prevalence = persons estimated to have mental health conditions needing services who actually receive services for their mental health conditions Clinical Population Estimated to be in Need Persons Served Percentage Served Guilford Percentage Served State Adults with MH 19, 728 8, 929 45% 48% Children/Adolescents with MH 11, 135 4, 871 44% 49% Quality Management Team, NCDMHDDSAS, 2010
 Costs of Mental Illness Costs are direct and indirect. They include: Treatment, disability, unemployment, incarceration, homelessness, substance abuse, suicide According to the 2009 Medical Expenditure Panel Survey: Mental disorders accounted for greatest rise in medical expenses between 1996 and 2006 (from $35. 2 billion to $57. 5 billion in adjusted figures) Census of persons with mental health expense outlays grew from 19. 3 million to 36. 2 million across same time period Researchers estimate roughly $193 billion in income lost each year due to mental illness (estimates were from early part of the decade; these may be underestimates by today’s costs) Researchers link untreated mental illness to: Chronic diseases, risky health-related behaviors, violence, work absenteeism AHRQ, 2009; CDC, n. d. ; Kessler et al. , 2008; NAMI, n. d.
Costs of Mental Illness Costs are direct and indirect. They include: Treatment, disability, unemployment, incarceration, homelessness, substance abuse, suicide According to the 2009 Medical Expenditure Panel Survey: Mental disorders accounted for greatest rise in medical expenses between 1996 and 2006 (from $35. 2 billion to $57. 5 billion in adjusted figures) Census of persons with mental health expense outlays grew from 19. 3 million to 36. 2 million across same time period Researchers estimate roughly $193 billion in income lost each year due to mental illness (estimates were from early part of the decade; these may be underestimates by today’s costs) Researchers link untreated mental illness to: Chronic diseases, risky health-related behaviors, violence, work absenteeism AHRQ, 2009; CDC, n. d. ; Kessler et al. , 2008; NAMI, n. d.
 Costs of Mental Illness According to the NC State Center for Health Statistics: 3, 377 persons in NC died due to a mental health or substance abuse diagnosis in 2007 1, 093 persons in NC died due to suicide in 2007 $530 million were spent in NC in 2007 for inpatient hospitalizations According to the NC Institute of Medicine: Approximately 50, 000 Disability-Adjusted Life Years were lost in NC in 2005 due to unipolar depression In NC in 2006, per capita spending on mental health was one of the lowest (43 rd) in the nation, at $16. 80. Of that rate, the large majority goes to inpatient costs (65. 5% compared to a 37. 1% national average) Holmes, 2008; NC-CATCH Portal, n. d. ; NC State Center for Health Statistics, 2009; Thompson & Broskowski, 2006
Costs of Mental Illness According to the NC State Center for Health Statistics: 3, 377 persons in NC died due to a mental health or substance abuse diagnosis in 2007 1, 093 persons in NC died due to suicide in 2007 $530 million were spent in NC in 2007 for inpatient hospitalizations According to the NC Institute of Medicine: Approximately 50, 000 Disability-Adjusted Life Years were lost in NC in 2005 due to unipolar depression In NC in 2006, per capita spending on mental health was one of the lowest (43 rd) in the nation, at $16. 80. Of that rate, the large majority goes to inpatient costs (65. 5% compared to a 37. 1% national average) Holmes, 2008; NC-CATCH Portal, n. d. ; NC State Center for Health Statistics, 2009; Thompson & Broskowski, 2006
 Costs of Mental Illness In wake of mental health reform, researchers calculated: A 21. 9% increase in number of adult hospital admissions for Guilford Center LME, which went from 16, 570 community hospital adult admission days in SFY 2005 -2006 to 18, 939 admission days in SFY 2006 -2007 A 32. 1% increase in number of child hospital admissions for Guilford Center LME, which went from 2, 005 community hospital child admission days in SFY 2005 -2006 to 2, 849 admission days in SFY 2006 -2007 According to NCDMHDDSAS: For Q 1 SFY 2009 -2010, Guilford Center had 3 rd highest LME ER admission rate for mental health diagnoses (153. 9 per 10, 000) Guilford Center LME revenue and expenditures: Increase of $3, 143, 503, or 9. 4%, from SFY 2006 -2007 to SFY 2008 -2009 Akland & Akland, 2008; Guilford Center, 2009; Budget and Finance Team, NCDMHDDSAS, n. d. ; Quality Management Team, NCDMHDDSAS, 2010
Costs of Mental Illness In wake of mental health reform, researchers calculated: A 21. 9% increase in number of adult hospital admissions for Guilford Center LME, which went from 16, 570 community hospital adult admission days in SFY 2005 -2006 to 18, 939 admission days in SFY 2006 -2007 A 32. 1% increase in number of child hospital admissions for Guilford Center LME, which went from 2, 005 community hospital child admission days in SFY 2005 -2006 to 2, 849 admission days in SFY 2006 -2007 According to NCDMHDDSAS: For Q 1 SFY 2009 -2010, Guilford Center had 3 rd highest LME ER admission rate for mental health diagnoses (153. 9 per 10, 000) Guilford Center LME revenue and expenditures: Increase of $3, 143, 503, or 9. 4%, from SFY 2006 -2007 to SFY 2008 -2009 Akland & Akland, 2008; Guilford Center, 2009; Budget and Finance Team, NCDMHDDSAS, n. d. ; Quality Management Team, NCDMHDDSAS, 2010
 Listening to Community Voices
Listening to Community Voices
 Faith community-provider collaborations, like Congregational Nurse Program Emergency services at Guilford Center LME, Moses Cone Behavioral Health Center; mobile crisis care from Therapeutic Alternatives Peer-led support groups/family support from Mental Health Associations in Greensboro and High Point, local NAMI chapter Early-onset dementia support from Adult Center for Enrichment Homeless support from Interactive Resource Center Specialized mental health services from Tristan’s Quest, Youth Focus, Youth Villages, Therapeutic Alternatives Residential/independent life skills services from My Sister Susan’s House, Destiny House, Sanctuary House, Joseph’s House, Shepherd House
Faith community-provider collaborations, like Congregational Nurse Program Emergency services at Guilford Center LME, Moses Cone Behavioral Health Center; mobile crisis care from Therapeutic Alternatives Peer-led support groups/family support from Mental Health Associations in Greensboro and High Point, local NAMI chapter Early-onset dementia support from Adult Center for Enrichment Homeless support from Interactive Resource Center Specialized mental health services from Tristan’s Quest, Youth Focus, Youth Villages, Therapeutic Alternatives Residential/independent life skills services from My Sister Susan’s House, Destiny House, Sanctuary House, Joseph’s House, Shepherd House
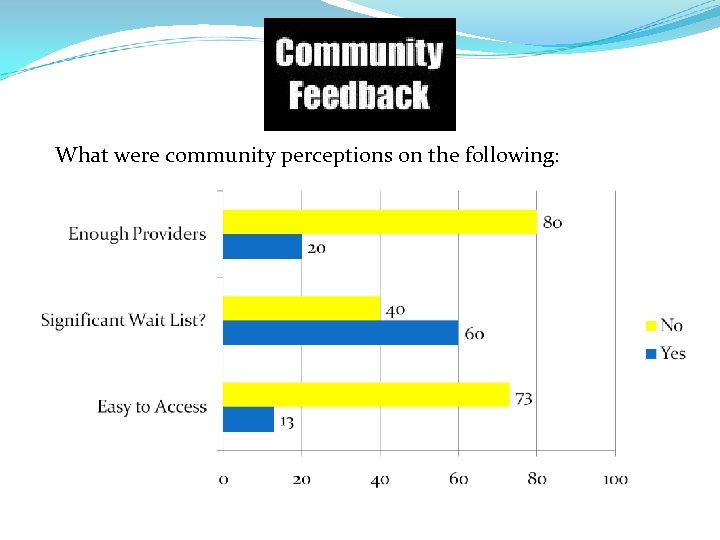 What were community perceptions on the following:
What were community perceptions on the following:
 Majority of survey respondents (73%) reported costs associated with mental health services as a barrier to accessing those services Only 14. 6% say mental health services affordable in Guilford Fewest resources exist for: Children under age 12, immigrant populations, non-English speaking populations, homeless persons
Majority of survey respondents (73%) reported costs associated with mental health services as a barrier to accessing those services Only 14. 6% say mental health services affordable in Guilford Fewest resources exist for: Children under age 12, immigrant populations, non-English speaking populations, homeless persons
 Providers and consumers noted needs for: Coordination along continuum of care, step-down services, peer support, child/adolescent psychiatrists, respite care, intensive in-home services, specialized trauma services, home health evaluations for the elderly Increasing understanding that mental illness and substance abuse often co-occur; addressing these issues in tandem
Providers and consumers noted needs for: Coordination along continuum of care, step-down services, peer support, child/adolescent psychiatrists, respite care, intensive in-home services, specialized trauma services, home health evaluations for the elderly Increasing understanding that mental illness and substance abuse often co-occur; addressing these issues in tandem
 Barriers to Treatment (Community Feedback) Difficulty navigating system, cost, waiting lists, transportation, mental health/physical symptoms, childcare needs, service locations Examination of barriers and strategic planning to minimize these may lead to increased service utilization
Barriers to Treatment (Community Feedback) Difficulty navigating system, cost, waiting lists, transportation, mental health/physical symptoms, childcare needs, service locations Examination of barriers and strategic planning to minimize these may lead to increased service utilization
 Recommendations
Recommendations
 Support Programs that Demonstrate Both Evidence-Based Practice and Practice-Based Evidence Foundation Action: ØPrioritize programs that include: 1) Cognitive-Behavioral Frameworks 2) Motivational Interviewing (MI) Techniques 3) Consumer partnering ØSupport MI trainings within currently funded programs such as Congregational Nurses and Social Workers programs. ØSupport supervision trainings on a subset of evidence-based practice models Potential Partners: Local provider networks, Guilford Center LME, NCDHHS MH/DD/SAS, and local colleges and universities to provide training and fidelity to evidence-based practice models.
Support Programs that Demonstrate Both Evidence-Based Practice and Practice-Based Evidence Foundation Action: ØPrioritize programs that include: 1) Cognitive-Behavioral Frameworks 2) Motivational Interviewing (MI) Techniques 3) Consumer partnering ØSupport MI trainings within currently funded programs such as Congregational Nurses and Social Workers programs. ØSupport supervision trainings on a subset of evidence-based practice models Potential Partners: Local provider networks, Guilford Center LME, NCDHHS MH/DD/SAS, and local colleges and universities to provide training and fidelity to evidence-based practice models.
 Improve Access to Services Foundation Action: Ø Support strategic planning, § Improvement of the available 1 -800 access number • Education and awareness of the number through marketing and billboards throughout the community • Training of staff regarding services available § Consumer-friendly website • Search for providers on the web using specific search criteria to fit unique needs • Housed in a neutral, community-based agency such as NAMI, MHA in Greensboro or High Point, or Guilford CARES • Content available in print (as well as in multiple languages) and provided on a readable level to ensure health literacy • Distributed as collaborative resource guides across the county in a similar fashion to publications such as “Apartment Finders” Potential Partners: Local provider networks, Guilford Center LME, MHA, NAMI, Guilford CARES.
Improve Access to Services Foundation Action: Ø Support strategic planning, § Improvement of the available 1 -800 access number • Education and awareness of the number through marketing and billboards throughout the community • Training of staff regarding services available § Consumer-friendly website • Search for providers on the web using specific search criteria to fit unique needs • Housed in a neutral, community-based agency such as NAMI, MHA in Greensboro or High Point, or Guilford CARES • Content available in print (as well as in multiple languages) and provided on a readable level to ensure health literacy • Distributed as collaborative resource guides across the county in a similar fashion to publications such as “Apartment Finders” Potential Partners: Local provider networks, Guilford Center LME, MHA, NAMI, Guilford CARES.
 Increase Awareness of Co-Occurring Mental Health and Substance Abuse as the Norm Rather than the Exception Foundation Action: Ø Develop a Community Action Strategic Plan (CASP) § Support community dialogue § Build capacity to deliver integrated mental health/substance abuse treatment Ø Support Workforce Development Efforts § Training (In-service and AHEC) related to co-occurring disorders (e. g. , educational, assessment, and treatment) § Special topics courses within local college and university graduate programs § Expanding the focus to include discussions regarding co-occurring disorders (modeled after local Say-It chapter) • Monthly provider meetings on evidence-best practices around co-occurring models and specific interventions. • Monitoring of implementation to ensure quality Potential Partners: Community-based mental health and substance abuse agencies, local provider networks, Guilford Center LME, local and state consumer groups (NAMI, NCFU, Guilford CARES), peer-to-peer support, AHEC, local colleges and universities.
Increase Awareness of Co-Occurring Mental Health and Substance Abuse as the Norm Rather than the Exception Foundation Action: Ø Develop a Community Action Strategic Plan (CASP) § Support community dialogue § Build capacity to deliver integrated mental health/substance abuse treatment Ø Support Workforce Development Efforts § Training (In-service and AHEC) related to co-occurring disorders (e. g. , educational, assessment, and treatment) § Special topics courses within local college and university graduate programs § Expanding the focus to include discussions regarding co-occurring disorders (modeled after local Say-It chapter) • Monthly provider meetings on evidence-best practices around co-occurring models and specific interventions. • Monitoring of implementation to ensure quality Potential Partners: Community-based mental health and substance abuse agencies, local provider networks, Guilford Center LME, local and state consumer groups (NAMI, NCFU, Guilford CARES), peer-to-peer support, AHEC, local colleges and universities.
 Co-Locate Mental Health Services Foundation Action: Ø Support co-location of faith-based communities such as Congregational Nurses and Congregational Social Workers Programs. Ø Support programs that co-locate services in primary care settings Ø Support provision of co-located services in school settings § Mental health clinician in 2 -3 schools. § Foundation can support situations in which provider cannot bill for services § Support training for staff and teachers about mental health signs and symptoms Potential Partners: Local provider networks, Guilford Center LME, Guilford County Schools, primary care clinics, pediatricians, local colleges and universities.
Co-Locate Mental Health Services Foundation Action: Ø Support co-location of faith-based communities such as Congregational Nurses and Congregational Social Workers Programs. Ø Support programs that co-locate services in primary care settings Ø Support provision of co-located services in school settings § Mental health clinician in 2 -3 schools. § Foundation can support situations in which provider cannot bill for services § Support training for staff and teachers about mental health signs and symptoms Potential Partners: Local provider networks, Guilford Center LME, Guilford County Schools, primary care clinics, pediatricians, local colleges and universities.
 Increase Attention to Special Populations Foundation Action: Ø Support programs targeting immigrant, homeless, and non-English speaking populations Ø Increase funding for interpreter training § Interpreter Access Project (http: //cnnc. uncg. edu/programs/iaptraining. htm). Ø Raise awareness and advocate for Title VI compliance among providers Ø Support continuing education opportunities in the interpreting profession Ø Support translation of materials into next 2 -3 most commonly occurring languages Potential Partners: Local provider networks, Guilford Center LME, communitybased organizations serving immigrant, homeless, and non-English speaking populations, interpreter training programs such as Center for New North Carolinians, AHEC, local colleges and universities.
Increase Attention to Special Populations Foundation Action: Ø Support programs targeting immigrant, homeless, and non-English speaking populations Ø Increase funding for interpreter training § Interpreter Access Project (http: //cnnc. uncg. edu/programs/iaptraining. htm). Ø Raise awareness and advocate for Title VI compliance among providers Ø Support continuing education opportunities in the interpreting profession Ø Support translation of materials into next 2 -3 most commonly occurring languages Potential Partners: Local provider networks, Guilford Center LME, communitybased organizations serving immigrant, homeless, and non-English speaking populations, interpreter training programs such as Center for New North Carolinians, AHEC, local colleges and universities.
 Increase Attention to Service Gaps Foundation Action: Ø Fund programs that address service gaps § availability of crisis beds, respite services, child/adolescent psychiatry services, peer-to-peer services, specialized trauma services (e. g. , sexual assault support groups, returning military), wraparound and step-down services, and services to assist in the transition from adolescence to adulthood (i. e. , emerging adulthood services). Ø Require funded programs to have a plan for addressing transportation issues if the program is not community-based or inhome Potential Partners: Local provider networks, Guilford Center LME, community-based organizations, local and state consumer groups, local colleges and universities.
Increase Attention to Service Gaps Foundation Action: Ø Fund programs that address service gaps § availability of crisis beds, respite services, child/adolescent psychiatry services, peer-to-peer services, specialized trauma services (e. g. , sexual assault support groups, returning military), wraparound and step-down services, and services to assist in the transition from adolescence to adulthood (i. e. , emerging adulthood services). Ø Require funded programs to have a plan for addressing transportation issues if the program is not community-based or inhome Potential Partners: Local provider networks, Guilford Center LME, community-based organizations, local and state consumer groups, local colleges and universities.
 Policy Implications Foundation Action: Ø Require funded direct service programs to have a supplemental or sliding fee scale Ø Fund programs implementing EBPs for a minimum of three years Ø Favor EBP implementation programs that include regularly tracked performance measures coupled with client incentives Ø Support a demonstration project that: 1) addresses one of the identified service gaps AND; 2) utilizes blended or braided funding Potential Partners: Local provider networks, Guilford Center LME, community-based organizations, local colleges and universities, local foundations (e. g. , Weaver Foundation, Cemala Foundation, Tannenbaum-Sternberger Foundation), Partners Ending Homelessness work group
Policy Implications Foundation Action: Ø Require funded direct service programs to have a supplemental or sliding fee scale Ø Fund programs implementing EBPs for a minimum of three years Ø Favor EBP implementation programs that include regularly tracked performance measures coupled with client incentives Ø Support a demonstration project that: 1) addresses one of the identified service gaps AND; 2) utilizes blended or braided funding Potential Partners: Local provider networks, Guilford Center LME, community-based organizations, local colleges and universities, local foundations (e. g. , Weaver Foundation, Cemala Foundation, Tannenbaum-Sternberger Foundation), Partners Ending Homelessness work group
 Conclusions Nationally identified public health priority Fundamental to physical health and quality of life Moving toward parity Local community priority
Conclusions Nationally identified public health priority Fundamental to physical health and quality of life Moving toward parity Local community priority
 People with mental problems are our neighbors. They are members of our congregations, members of our families; they are everywhere in this country. If we ignore their cries for help, we will be continuing to participate in the anguish from which those cries for help come. A problem of this magnitude will not go away. Because it will not go away…we are compelled to take action. ~Rosalynn Carter
People with mental problems are our neighbors. They are members of our congregations, members of our families; they are everywhere in this country. If we ignore their cries for help, we will be continuing to participate in the anguish from which those cries for help come. A problem of this magnitude will not go away. Because it will not go away…we are compelled to take action. ~Rosalynn Carter
 Questions and Comments
Questions and Comments
 Contact Information Dr. Kelly Graves: kngrave 3@uncg. edu Anne Buford: apbuford@gmail. com Dr. Sonja Frison: slfrison@uncg. edu Amanda Ireland: mandyi 05@gmail. com Dr. Terri Shelton: shelton@uncg. edu 330 S. Greene Street Suite 200 Greensboro, NC 27401 336 -217 -9713
Contact Information Dr. Kelly Graves: kngrave 3@uncg. edu Anne Buford: apbuford@gmail. com Dr. Sonja Frison: slfrison@uncg. edu Amanda Ireland: mandyi 05@gmail. com Dr. Terri Shelton: shelton@uncg. edu 330 S. Greene Street Suite 200 Greensboro, NC 27401 336 -217 -9713


