5c29bf4537e67383a6579acf9ce272ea.ppt
- Количество слайдов: 66
 The SHARE Approach Essential Steps of Shared Decision Making Workshop Course
The SHARE Approach Essential Steps of Shared Decision Making Workshop Course
 Module 1 Shared Decision Making and the SHARE Approach 2
Module 1 Shared Decision Making and the SHARE Approach 2
 Module 1 – Purpose } Present information about the five-step SHARE Approach of shared decision making and how to implement it. 3
Module 1 – Purpose } Present information about the five-step SHARE Approach of shared decision making and how to implement it. 3
 Module 1 – Learning objectives At the conclusion of this activity, the participant will be able to: } Define shared decision making. } List critical elements required in effective shared decision making. } Explain key steps for conducting shared decision making. 4
Module 1 – Learning objectives At the conclusion of this activity, the participant will be able to: } Define shared decision making. } List critical elements required in effective shared decision making. } Explain key steps for conducting shared decision making. 4
 Patient and provider perspectives } http: //vimeo. com/3527488 3 } With permission from the Stillwater Medical Group, Stillwater, MN 5
Patient and provider perspectives } http: //vimeo. com/3527488 3 } With permission from the Stillwater Medical Group, Stillwater, MN 5
 Discussion How did the patients feel about their experience with their providers? 6
Discussion How did the patients feel about their experience with their providers? 6
 The “What, ” “Why, ” and “When” of Shared Decision Making 7
The “What, ” “Why, ” and “When” of Shared Decision Making 7
 Definition } Shared decision making occurs when a health care provider and a patient work together to make a health care decision that is best for the patient. } The optimal decision takes into account evidence-based information about available options, the provider’s knowledge and experience, and the patient’s values and preferences. 8
Definition } Shared decision making occurs when a health care provider and a patient work together to make a health care decision that is best for the patient. } The optimal decision takes into account evidence-based information about available options, the provider’s knowledge and experience, and the patient’s values and preferences. 8
 Tool 1 - Essential Steps of Shared Decision Making: Quick Reference Guide 9
Tool 1 - Essential Steps of Shared Decision Making: Quick Reference Guide 9
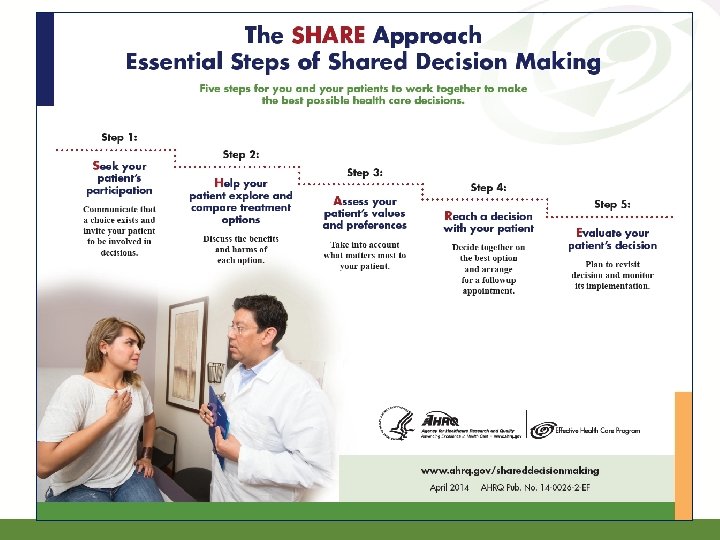
 The SHARE Approach } The SHARE Approach is a five-step process for shared decision making that includes exploring and comparing the benefits, harms, and risks of each health care option through meaningful dialogue about what matters most to the patient. 10
The SHARE Approach } The SHARE Approach is a five-step process for shared decision making that includes exploring and comparing the benefits, harms, and risks of each health care option through meaningful dialogue about what matters most to the patient. 10
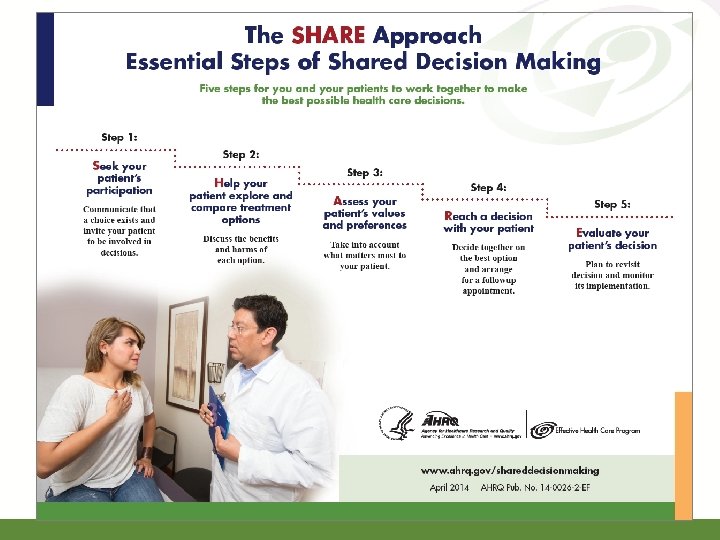
 The SHARE Approach } Step 1: Seek your patient’s participation } Step 2: Help your patient explore and compare treatment options } Step 3: Assess your patient’s values and preferences } Step 4: Reach a decision with your patient } Step 5: Evaluate your patient’s decision Refer to page 2, Tool 1. 11
The SHARE Approach } Step 1: Seek your patient’s participation } Step 2: Help your patient explore and compare treatment options } Step 3: Assess your patient’s values and preferences } Step 4: Reach a decision with your patient } Step 5: Evaluate your patient’s decision Refer to page 2, Tool 1. 11
 Nine essential elements (Makoul & Clayman)1 } Conducted a systematic review of the literature in 2006 § Identified the most frequently referenced essential elements of shared decision making § The SHARE Approach includes these nine elements. 12
Nine essential elements (Makoul & Clayman)1 } Conducted a systematic review of the literature in 2006 § Identified the most frequently referenced essential elements of shared decision making § The SHARE Approach includes these nine elements. 12
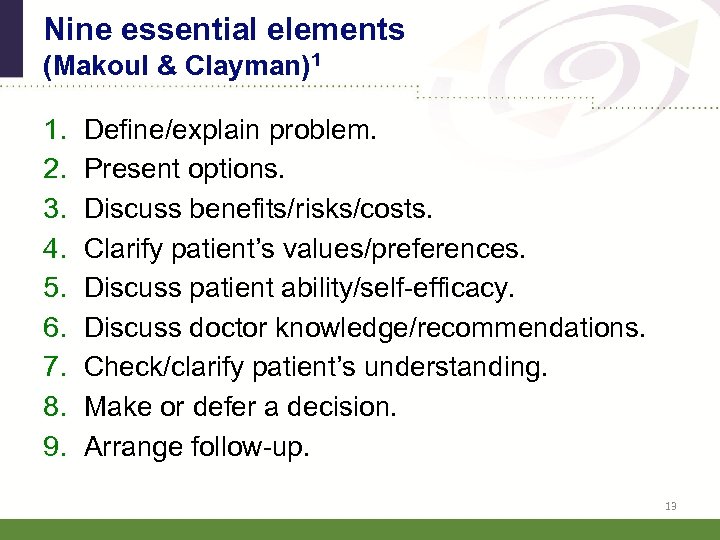 Nine essential elements (Makoul & Clayman)1 1. 2. 3. 4. 5. 6. 7. 8. 9. Define/explain problem. Present options. Discuss benefits/risks/costs. Clarify patient’s values/preferences. Discuss patient ability/self-efficacy. Discuss doctor knowledge/recommendations. Check/clarify patient’s understanding. Make or defer a decision. Arrange follow-up. 13
Nine essential elements (Makoul & Clayman)1 1. 2. 3. 4. 5. 6. 7. 8. 9. Define/explain problem. Present options. Discuss benefits/risks/costs. Clarify patient’s values/preferences. Discuss patient ability/self-efficacy. Discuss doctor knowledge/recommendations. Check/clarify patient’s understanding. Make or defer a decision. Arrange follow-up. 13
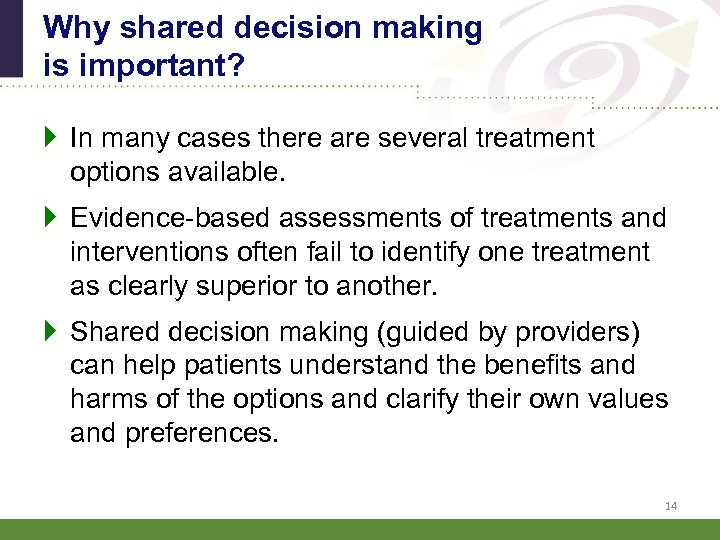 Why shared decision making is important? } In many cases there are several treatment options available. } Evidence-based assessments of treatments and interventions often fail to identify one treatment as clearly superior to another. } Shared decision making (guided by providers) can help patients understand the benefits and harms of the options and clarify their own values and preferences. 14
Why shared decision making is important? } In many cases there are several treatment options available. } Evidence-based assessments of treatments and interventions often fail to identify one treatment as clearly superior to another. } Shared decision making (guided by providers) can help patients understand the benefits and harms of the options and clarify their own values and preferences. 14
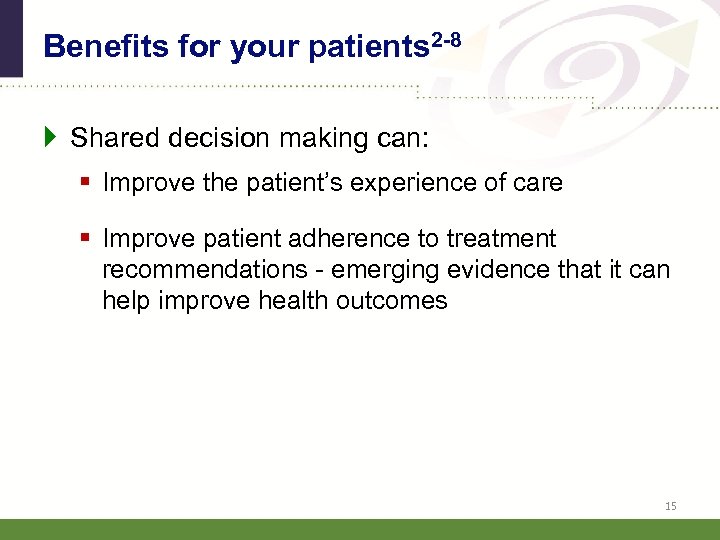 Benefits for your patients 2 -8 } Shared decision making can: § Improve the patient’s experience of care § Improve patient adherence to treatment recommendations - emerging evidence that it can help improve health outcomes 15
Benefits for your patients 2 -8 } Shared decision making can: § Improve the patient’s experience of care § Improve patient adherence to treatment recommendations - emerging evidence that it can help improve health outcomes 15
 Benefits for your organization 8 } Shared decision making can: § Improve the quality of care delivered § Increase patient satisfaction You will learn more about patient and provider benefits from shared decision making in Module 4. 16
Benefits for your organization 8 } Shared decision making can: § Improve the quality of care delivered § Increase patient satisfaction You will learn more about patient and provider benefits from shared decision making in Module 4. 16
 When to engage in shared decision making? } Engage when your patient has a health problem that needs a treatment decision. § Not every patient encounter requires shared decision making. } Some patients may not want to or be ready to participate in shared decision making. 9 -11 § A patient choosing not to participate in the decision-making process is still making a decision. 17
When to engage in shared decision making? } Engage when your patient has a health problem that needs a treatment decision. § Not every patient encounter requires shared decision making. } Some patients may not want to or be ready to participate in shared decision making. 9 -11 § A patient choosing not to participate in the decision-making process is still making a decision. 17
 What studies are showing 11 -13 } Studies suggest that many health providers believe patients are not interested in participating in health care decision making. } Evidence suggests that most patient want more information than given, and many would like to be more involved in their health decisions. 18
What studies are showing 11 -13 } Studies suggest that many health providers believe patients are not interested in participating in health care decision making. } Evidence suggests that most patient want more information than given, and many would like to be more involved in their health decisions. 18
 The “Who” and “How” of Shared Decision Making 19
The “Who” and “How” of Shared Decision Making 19
 Who is involved in shared decision making in the clinical setting? } The entire medical team should be familiar with and involved in shared decision making. 20
Who is involved in shared decision making in the clinical setting? } The entire medical team should be familiar with and involved in shared decision making. 20
 Collaborative roles in shared decision making – Key Roles } Patient § Actively participates and is the center of shared decision making } Physician, physician assistant, or nurse practitioner § Lets their patient know there is a choice and invites patient to be involved in the decision § Presents options and describes the risks and harms § Explores patient’s values and preference Refer to page 6, Tool 1. 21
Collaborative roles in shared decision making – Key Roles } Patient § Actively participates and is the center of shared decision making } Physician, physician assistant, or nurse practitioner § Lets their patient know there is a choice and invites patient to be involved in the decision § Presents options and describes the risks and harms § Explores patient’s values and preference Refer to page 6, Tool 1. 21
 Collaborative roles in shared decision making – other team members } Decision coach (nurses, social workers, health educator) § Helps assess factors impacting the patient’s decisional conflicts § Provides support § Monitors progress § Screens what is influencing implementations What does decision conflict look like? Your patient may: § Verbalize uncertainty about the choice § Waver between choices § Delay the decision § Question personal values or what is important to them § Be preoccupied with the decision § Show signs of distress or tension 22
Collaborative roles in shared decision making – other team members } Decision coach (nurses, social workers, health educator) § Helps assess factors impacting the patient’s decisional conflicts § Provides support § Monitors progress § Screens what is influencing implementations What does decision conflict look like? Your patient may: § Verbalize uncertainty about the choice § Waver between choices § Delay the decision § Question personal values or what is important to them § Be preoccupied with the decision § Show signs of distress or tension 22
 Collaborative roles in shared decision making – other team members } Shared decision making manager/support staff § Organizes the clinical practice to incorporate shared decision making § Manages the library of decision aids and technologies § Manages the clinical processes 23
Collaborative roles in shared decision making – other team members } Shared decision making manager/support staff § Organizes the clinical practice to incorporate shared decision making § Manages the library of decision aids and technologies § Manages the clinical processes 23
 Collaborative roles in shared decision making } Family members and caregivers § Lend support in clarifying the patient’s values and preferences § Serve as legal proxy for children, elderly, or seriously ill patients 24
Collaborative roles in shared decision making } Family members and caregivers § Lend support in clarifying the patient’s values and preferences § Serve as legal proxy for children, elderly, or seriously ill patients 24
 Collaborative roles in shared decision making } Medical treatment specialists § Offer input when treatment options require input from specialists 25
Collaborative roles in shared decision making } Medical treatment specialists § Offer input when treatment options require input from specialists 25
 Supportive materials from AHRQ Decision support resources are an important part of the “how” of shared decision making. 26
Supportive materials from AHRQ Decision support resources are an important part of the “how” of shared decision making. 26
 Using evidence-based decision aids to support shared decision making } Rely on materials that have reliable, unbiased summaries of evidence-based research. } AHRQ and other organizations have many evidence-based treatment option resources. } AHRQ's Effective Health Care Program is a growing library of free, easy-to-read treatment option resources for many health conditions. Refer to pages 78, Tool 1. More on decision support resources in Module 2. 27
Using evidence-based decision aids to support shared decision making } Rely on materials that have reliable, unbiased summaries of evidence-based research. } AHRQ and other organizations have many evidence-based treatment option resources. } AHRQ's Effective Health Care Program is a growing library of free, easy-to-read treatment option resources for many health conditions. Refer to pages 78, Tool 1. More on decision support resources in Module 2. 27
 Benefits of using decision aids in shared decision making 8 } Improves patient’s knowledge of options } Results in patient having more accurate expectations of possible benefits and risks } Leads to patient making decisions that are more consistent with his/her values } Increases patient’s participation in decision making 28
Benefits of using decision aids in shared decision making 8 } Improves patient’s knowledge of options } Results in patient having more accurate expectations of possible benefits and risks } Leads to patient making decisions that are more consistent with his/her values } Increases patient’s participation in decision making 28
 Health Care Encounter Without Shared Decision Making Video Presentation 29
Health Care Encounter Without Shared Decision Making Video Presentation 29
 Rebecca & Dr. Miller Is this typical of the patient-provider interactions you’ve observed? How satisfied is Rebecca with the outcome of the encounter? Why? How satisfied is Dr. Miller with the outcome of the encounter? Why? 30
Rebecca & Dr. Miller Is this typical of the patient-provider interactions you’ve observed? How satisfied is Rebecca with the outcome of the encounter? Why? How satisfied is Dr. Miller with the outcome of the encounter? Why? 30
 The SHARE Approach Step by Step 31
The SHARE Approach Step by Step 31
 32
32
 Presenting SHARE steps. . . } The mnemonic “SHARE” is a learning device to help you readily recall the steps in the SHARE Approach Model. } You may find that you do not present them in “linear order” during encounters. } The important takeaway is to address all five steps. 33
Presenting SHARE steps. . . } The mnemonic “SHARE” is a learning device to help you readily recall the steps in the SHARE Approach Model. } You may find that you do not present them in “linear order” during encounters. } The important takeaway is to address all five steps. 33
 Tool 2 - Expanded Reference Guide with Sample Conversation Starters 34
Tool 2 - Expanded Reference Guide with Sample Conversation Starters 34
 Step 1: Seek your patient’s participation } Communicate that a choice exists and invite the patient to participate in the decision-making process. Many patients are not aware that they can and should participate in their health care decision making. Many patients are not aware of the uncertainty in medicine, and that the outcomes of various treatments are variable. Refer to page 3, Tool 2. 35
Step 1: Seek your patient’s participation } Communicate that a choice exists and invite the patient to participate in the decision-making process. Many patients are not aware that they can and should participate in their health care decision making. Many patients are not aware of the uncertainty in medicine, and that the outcomes of various treatments are variable. Refer to page 3, Tool 2. 35
 Step 1: Seek your patient’s participation Tips } Summarize the health problem and communicate there may be more than one treatment choice. } Ask your patient to participate with the health care team. } Assess the role your patient wants to play. } Include family/caregivers in decisions. Use cues to continually engage your patient. For example, “I’d like you input” Refer to page 3, Tool 2. 36
Step 1: Seek your patient’s participation Tips } Summarize the health problem and communicate there may be more than one treatment choice. } Ask your patient to participate with the health care team. } Assess the role your patient wants to play. } Include family/caregivers in decisions. Use cues to continually engage your patient. For example, “I’d like you input” Refer to page 3, Tool 2. 36
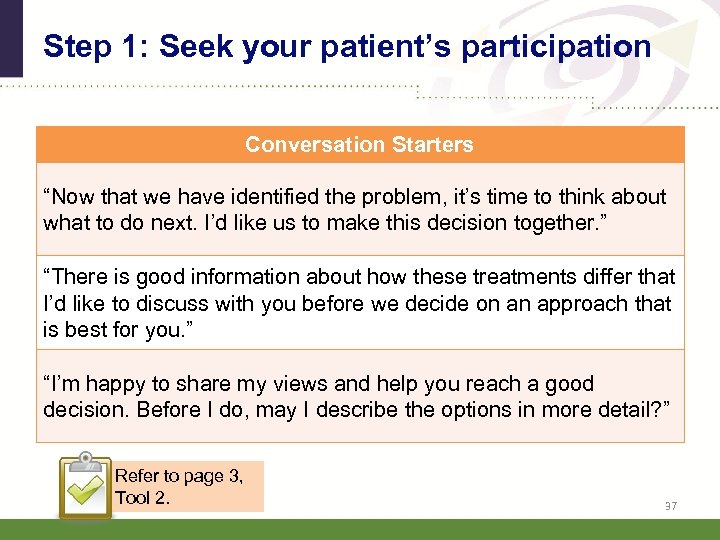 Step 1: Seek your patient’s participation Conversation Starters “Now that we have identified the problem, it’s time to think about what to do next. I’d like us to make this decision together. ” “There is good information about how these treatments differ that I’d like to discuss with you before we decide on an approach that is best for you. ” “I’m happy to share my views and help you reach a good decision. Before I do, may I describe the options in more detail? ” Refer to page 3, Tool 2. 37
Step 1: Seek your patient’s participation Conversation Starters “Now that we have identified the problem, it’s time to think about what to do next. I’d like us to make this decision together. ” “There is good information about how these treatments differ that I’d like to discuss with you before we decide on an approach that is best for you. ” “I’m happy to share my views and help you reach a good decision. Before I do, may I describe the options in more detail? ” Refer to page 3, Tool 2. 37
 Discussion Do you have other phrases that you use as conversation starters to get patients engaged? 38
Discussion Do you have other phrases that you use as conversation starters to get patients engaged? 38
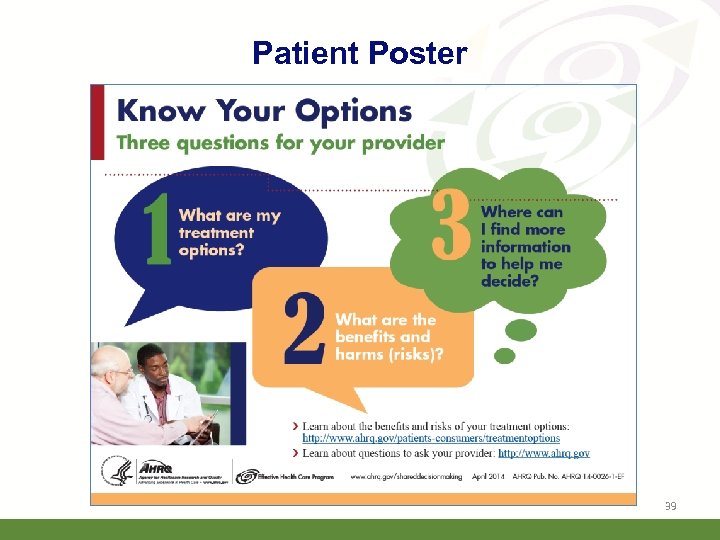 Patient Poster 39
Patient Poster 39
 Engaging your patients to ask questions } Post the “Know Your Options” poster in your waiting room and exam rooms. Find it: § On your thumb drive § In your notebook § On the AHRQ Web site at www. ahrq. gov/shareddecisionmaking } Learn about AHRQ’s “Questions are the Answer” campaign. Refer to page 8, Tool 1. 40
Engaging your patients to ask questions } Post the “Know Your Options” poster in your waiting room and exam rooms. Find it: § On your thumb drive § In your notebook § On the AHRQ Web site at www. ahrq. gov/shareddecisionmaking } Learn about AHRQ’s “Questions are the Answer” campaign. Refer to page 8, Tool 1. 40
 Step 2: Help your patient explore and compare treatment options } Discuss the benefits and risks of each treatment option. } Use evidence-based decision-making resources to compare treatment options. Read more about decision -support resources in Module 2. Refer to page 4, Tool 2. 41
Step 2: Help your patient explore and compare treatment options } Discuss the benefits and risks of each treatment option. } Use evidence-based decision-making resources to compare treatment options. Read more about decision -support resources in Module 2. Refer to page 4, Tool 2. 41
 Step 2: Help your patient explore and compare treatment options Tips } Check for patient knowledge of the options. } Clearly communicate risks and benefits of each option. } Explain the limitations of what is known about the options. } Use simple visual aids and evidence-based decision aids when possible. } Summarize by listing the options. 42
Step 2: Help your patient explore and compare treatment options Tips } Check for patient knowledge of the options. } Clearly communicate risks and benefits of each option. } Explain the limitations of what is known about the options. } Use simple visual aids and evidence-based decision aids when possible. } Summarize by listing the options. 42
 Step 2: Help your patient explore and compare treatment options Conversation Starters “Here are some choices we can consider. ” “Let me tell you what the research says about the benefits and risks of the medicine/treatments that you are considering. ” “I have some booklets I want to give you that have information about your condition and the treatment options. ” “These tools have been designed to help you to understand your options in more detail. ” Refer to pages 58, Tool 2. 43
Step 2: Help your patient explore and compare treatment options Conversation Starters “Here are some choices we can consider. ” “Let me tell you what the research says about the benefits and risks of the medicine/treatments that you are considering. ” “I have some booklets I want to give you that have information about your condition and the treatment options. ” “These tools have been designed to help you to understand your options in more detail. ” Refer to pages 58, Tool 2. 43
 Step 3: Assess your patient’s values and preferences } An optimal decision is one that takes into account patient preferences and values. } Communicate with your patient about the outcomes that are most important to him or her. What matters most to your patient? § Recovery time § Out-of-pocket costs § Being pain free § Having a specific level of functionality Refer to page 9, Tool 2. 44
Step 3: Assess your patient’s values and preferences } An optimal decision is one that takes into account patient preferences and values. } Communicate with your patient about the outcomes that are most important to him or her. What matters most to your patient? § Recovery time § Out-of-pocket costs § Being pain free § Having a specific level of functionality Refer to page 9, Tool 2. 44
 Step 3: Assess your patient’s values and preferences Tips } Encourage your patient to talk about his or her values and preferences. } Use open-ended questions. } Listen actively to the patient and show empathy and interest. } Acknowledge what matters to your patient. } Agree on what is important to your patient. 45
Step 3: Assess your patient’s values and preferences Tips } Encourage your patient to talk about his or her values and preferences. } Use open-ended questions. } Listen actively to the patient and show empathy and interest. } Acknowledge what matters to your patient. } Agree on what is important to your patient. 45
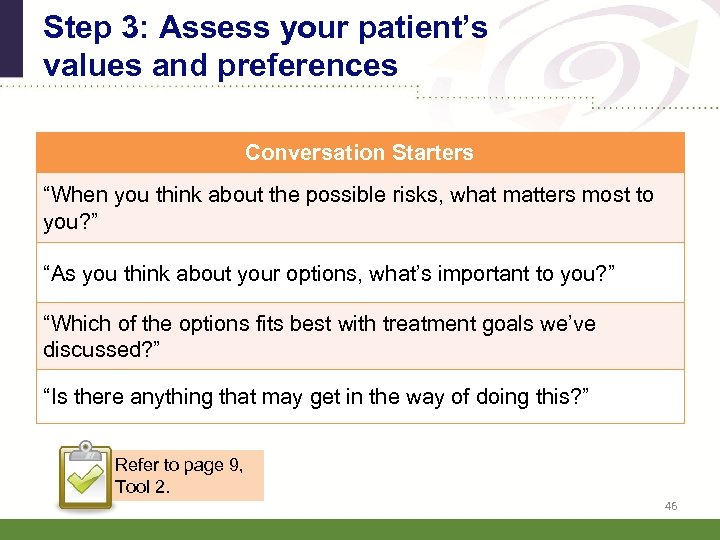 Step 3: Assess your patient’s values and preferences Conversation Starters “When you think about the possible risks, what matters most to you? ” “As you think about your options, what’s important to you? ” “Which of the options fits best with treatment goals we’ve discussed? ” “Is there anything that may get in the way of doing this? ” Refer to page 9, Tool 2. 46
Step 3: Assess your patient’s values and preferences Conversation Starters “When you think about the possible risks, what matters most to you? ” “As you think about your options, what’s important to you? ” “Which of the options fits best with treatment goals we’ve discussed? ” “Is there anything that may get in the way of doing this? ” Refer to page 9, Tool 2. 46
 Step 4: Reach a decision with your patient } Decide together on the best option. } Arrange for follow-up steps to achieve the preferred treatment. Refer to page 10, Tool 2. 47
Step 4: Reach a decision with your patient } Decide together on the best option. } Arrange for follow-up steps to achieve the preferred treatment. Refer to page 10, Tool 2. 47
 Step 4: Reach a decision with your patient Tips } Ask your patient if he/she is ready to make a decision. } Ask your patient if he/she needs more information. } Schedule another session if your patient needs more time to consider the decision. } Confirm the decision with your patient. } Schedule follow-up appointments to carry out preferred options. 48
Step 4: Reach a decision with your patient Tips } Ask your patient if he/she is ready to make a decision. } Ask your patient if he/she needs more information. } Schedule another session if your patient needs more time to consider the decision. } Confirm the decision with your patient. } Schedule follow-up appointments to carry out preferred options. 48
 Step 4 dialogue: Reach a decision with your patient Conversation Starters “It’s fine to take more time to think about the treatment choices. Would you like some more time, or are you ready to decide? ” “What additional questions do you have for me to help you make your decision? ” “Now that we had a chance to discuss your treatment options, which treatment do you think is right for you? ” Refer to page 10, Tool 2. 49
Step 4 dialogue: Reach a decision with your patient Conversation Starters “It’s fine to take more time to think about the treatment choices. Would you like some more time, or are you ready to decide? ” “What additional questions do you have for me to help you make your decision? ” “Now that we had a chance to discuss your treatment options, which treatment do you think is right for you? ” Refer to page 10, Tool 2. 49
 Step 5: Evaluate your patient’s decision } Support your patient so the treatment decision has a positive impact on health outcomes. } For management of chronic illness, revisit decision after a trial period. Refer to page 11, Tool 2. 50
Step 5: Evaluate your patient’s decision } Support your patient so the treatment decision has a positive impact on health outcomes. } For management of chronic illness, revisit decision after a trial period. Refer to page 11, Tool 2. 50
 Step 5: Evaluate your patient’s decision Tips } Make plans to review the decision in the future. } Monitor implementation of treatment decision. } Assist your patient with managing barriers to implementation. } Revisit the decision if the option does not produce the desired health outcomes. 51
Step 5: Evaluate your patient’s decision Tips } Make plans to review the decision in the future. } Monitor implementation of treatment decision. } Assist your patient with managing barriers to implementation. } Revisit the decision if the option does not produce the desired health outcomes. 51
 Step 5: Evaluate your patient’s decision Conversation Starters “Let’s plan on reviewing this decision at our next appointment. ” “If you don’t feel things are improving, please schedule a followup visit so we can plan a different approach. ” Refer to page 11, Tool 2. 52
Step 5: Evaluate your patient’s decision Conversation Starters “Let’s plan on reviewing this decision at our next appointment. ” “If you don’t feel things are improving, please schedule a followup visit so we can plan a different approach. ” Refer to page 11, Tool 2. 52
 Patient buy-in is essential to adherence } The patient is generally responsible for implementing many of the decisions that are made, particularly decisions made in a primary care setting (e. g. lifestyle changes or taking medications). } Adherence to treatment is enhanced by shared decision making!6 -7, 12 53
Patient buy-in is essential to adherence } The patient is generally responsible for implementing many of the decisions that are made, particularly decisions made in a primary care setting (e. g. lifestyle changes or taking medications). } Adherence to treatment is enhanced by shared decision making!6 -7, 12 53
 Shared Decision Making in Action Video Presentation 54
Shared Decision Making in Action Video Presentation 54
 Rebecca and Dr. Miller share a decision How satisfied is Rebecca with outcomes of the encounter? How do you think shared decision making will impact Rebecca’s health outcomes? How satisfied is Dr. Miller with the outcome of the encounter? Do you think that you might want to try using the SHARE Approach when you return to your job site? 55
Rebecca and Dr. Miller share a decision How satisfied is Rebecca with outcomes of the encounter? How do you think shared decision making will impact Rebecca’s health outcomes? How satisfied is Dr. Miller with the outcome of the encounter? Do you think that you might want to try using the SHARE Approach when you return to your job site? 55
 Putting Shared Decision Making Into Action Role Play Activity (Managing osteoarthritis pain with medicine) 56
Putting Shared Decision Making Into Action Role Play Activity (Managing osteoarthritis pain with medicine) 56
 Instructions } Break into your assigned group. } Choose roles: Provider, patient, reporter, observers. } Refer to the Conversation Starters handout and the SHARE Approach model as you role play. } Refer to your consumer and clinician summaries during this activity. } Role play: § Reporter asks for volunteers for provider and patient. § Role play a shared decision-making encounter. § Observers provide feedback. 57
Instructions } Break into your assigned group. } Choose roles: Provider, patient, reporter, observers. } Refer to the Conversation Starters handout and the SHARE Approach model as you role play. } Refer to your consumer and clinician summaries during this activity. } Role play: § Reporter asks for volunteers for provider and patient. § Role play a shared decision-making encounter. § Observers provide feedback. 57
 Debrief Summarize your group’s role play. } Could you fit all steps in? } What was most challenging? } What worked best? } How long did it take? } How difficult would this be to implement in real life? 58
Debrief Summarize your group’s role play. } Could you fit all steps in? } What was most challenging? } What worked best? } How long did it take? } How difficult would this be to implement in real life? 58
 Key takeaways } Shared decision making is a two-way street § Occurs when a health care provider and a patient work together to make a health care decision that is best for the patient. § The optimal decision takes into account evidencebased information about available options, the provider’s knowledge and experience, and the patient’s values and preferences. 59
Key takeaways } Shared decision making is a two-way street § Occurs when a health care provider and a patient work together to make a health care decision that is best for the patient. § The optimal decision takes into account evidencebased information about available options, the provider’s knowledge and experience, and the patient’s values and preferences. 59
 Key takeaways } The SHARE Approach is a five-step process for shared decision making that includes exploring and comparing the benefits, harms, and risks of each health care option through meaningful dialogue about what matters most to the patient. 60
Key takeaways } The SHARE Approach is a five-step process for shared decision making that includes exploring and comparing the benefits, harms, and risks of each health care option through meaningful dialogue about what matters most to the patient. 60
 Key takeaways } Conversation starters can help you engage patients as you present each of the SHARE Approach Model’s five steps. 61
Key takeaways } Conversation starters can help you engage patients as you present each of the SHARE Approach Model’s five steps. 61
 Key takeaways } Using evidence-based decision aids in shared decision making can: § Improve patient’s knowledge of options § Result in patient having more accurate expectations of possible benefits and risks § Lead to patient making decisions that are more consistent with their values § Increase patient’s participation in decision making 62
Key takeaways } Using evidence-based decision aids in shared decision making can: § Improve patient’s knowledge of options § Result in patient having more accurate expectations of possible benefits and risks § Lead to patient making decisions that are more consistent with their values § Increase patient’s participation in decision making 62
 63
63
 Citations 1. Makoul G, Clayman ML; An integrative model of shared decision making in medical encounters. Patient Educ Couns. 2006; 60(3): 301 -12. 2. Wilson SR, Strub P, Buist AS, Knowles SB, Lavori PW, Lapidus J, Vollmer WM; Better Outcomes of Asthma Treatment (BOAT) Study Group. Shared treatment decision making improves adherence and outcomes in poorly controlled asthma. Am J Respir Crit Care Med. 2010 Mar 15; 181(6): 566 -77. Pub. Med PMID: 20019345. 3. Clever SL, Ford DE, Rubenstein LV, Rost KM, Meredith LS, Sherbourne CD, Wang NY, Arbelaez JJ, Cooper LA. Primary care patients’ involvement in decision-making is associated with improvement in depression. Med Care. 2006 May; 44(5): 398 -405. Pub. Med PMID: 16641657. 4. Da Silva, D. Evidence: Helping people share decisions. A review of evidence considering whether shared decision making is worthwhile. 2012 June. London, England: Health Foundation. http: //www. health. org. uk/public/cms/75/76/313/3448/Helping. People. Share. Dec ision. Making. pdf? real. Name=r. FVU 5 h. pdf 64
Citations 1. Makoul G, Clayman ML; An integrative model of shared decision making in medical encounters. Patient Educ Couns. 2006; 60(3): 301 -12. 2. Wilson SR, Strub P, Buist AS, Knowles SB, Lavori PW, Lapidus J, Vollmer WM; Better Outcomes of Asthma Treatment (BOAT) Study Group. Shared treatment decision making improves adherence and outcomes in poorly controlled asthma. Am J Respir Crit Care Med. 2010 Mar 15; 181(6): 566 -77. Pub. Med PMID: 20019345. 3. Clever SL, Ford DE, Rubenstein LV, Rost KM, Meredith LS, Sherbourne CD, Wang NY, Arbelaez JJ, Cooper LA. Primary care patients’ involvement in decision-making is associated with improvement in depression. Med Care. 2006 May; 44(5): 398 -405. Pub. Med PMID: 16641657. 4. Da Silva, D. Evidence: Helping people share decisions. A review of evidence considering whether shared decision making is worthwhile. 2012 June. London, England: Health Foundation. http: //www. health. org. uk/public/cms/75/76/313/3448/Helping. People. Share. Dec ision. Making. pdf? real. Name=r. FVU 5 h. pdf 64
 Citations 5. Swanson KA, Bastani R, Rubenstein LV, Meredith LS, Ford DE. Effect of mental health care and shared decision making on patient satisfaction in a community sample of patients with depression. Med Care Res Rev. 2007 Aug; 64(4): 416 -30. Pub. Med PMID: 17684110. 6. Thompson L. , Mc. Cabe R. The effect of clinician-patient alliance and communication on treatment adherence in mental health care: a systematic review. BMC Psychiatry 2012 Jul 24; 12: 87. PMID: 22828119. 7. Duncan E. , Best C. , Hagen S. Shared decision making interventions for people with mental health conditions. Cochrane Database Syst Rev 2010 Jan 20; (1): CD 007297. PMID: 20091628. 8. Stacey D, Légaré F, Col NF, et. al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2014 Jan 28; 1: CD 001431. Pub. Med PMID: 24470076 (2014 Systematic Review; 113 studies; 34, 444 participants). 65
Citations 5. Swanson KA, Bastani R, Rubenstein LV, Meredith LS, Ford DE. Effect of mental health care and shared decision making on patient satisfaction in a community sample of patients with depression. Med Care Res Rev. 2007 Aug; 64(4): 416 -30. Pub. Med PMID: 17684110. 6. Thompson L. , Mc. Cabe R. The effect of clinician-patient alliance and communication on treatment adherence in mental health care: a systematic review. BMC Psychiatry 2012 Jul 24; 12: 87. PMID: 22828119. 7. Duncan E. , Best C. , Hagen S. Shared decision making interventions for people with mental health conditions. Cochrane Database Syst Rev 2010 Jan 20; (1): CD 007297. PMID: 20091628. 8. Stacey D, Légaré F, Col NF, et. al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2014 Jan 28; 1: CD 001431. Pub. Med PMID: 24470076 (2014 Systematic Review; 113 studies; 34, 444 participants). 65
 Citations 9. Little P. , Everitt H. , Williamson I. , et al. Preferences of patients for patient centred approach to consultation in primary care: observational study. BMJ 2001. 322(7284): 468 -72. PMID: 11222423. 10. Coulter A. , Parsons S. , Askham A. Where are the patients in decisionmaking about their own care? Health Systems and Policy Analysis 2008: p. 126. 11. Levinson W. , Kao A. , Kuby A. , et al. Not all patients want to participate in decision making. A national study of public preferences. J Gen Intern Med 2005 Jun; 20(6): 531 -5. PMID: 15987329. 12. Légaré F. , Ratté S. , Gravel K. , et al. Barriers and facilitators to implementing shared decision-making in clinical practice: update of a systematic review of health professionals’ perceptions. Patient Educ Couns 2008. Dec; 73(3): 52635. PMID: 18752915. 13. Guadagnoli E. , Ward P. Patient participation in decision-making. Soc Sci Med 1998 Aug; 47(3): 329 -39. PMID: 9681902. 14. Murray E. , Charles C. , Gafni A. Shared decision-making in primary care: tailoring the Charles et al. model to fit the context of general practice. Patient 66 Educ Couns 2006 Aug; 62(2): 205 -11. PMID: 16139467.
Citations 9. Little P. , Everitt H. , Williamson I. , et al. Preferences of patients for patient centred approach to consultation in primary care: observational study. BMJ 2001. 322(7284): 468 -72. PMID: 11222423. 10. Coulter A. , Parsons S. , Askham A. Where are the patients in decisionmaking about their own care? Health Systems and Policy Analysis 2008: p. 126. 11. Levinson W. , Kao A. , Kuby A. , et al. Not all patients want to participate in decision making. A national study of public preferences. J Gen Intern Med 2005 Jun; 20(6): 531 -5. PMID: 15987329. 12. Légaré F. , Ratté S. , Gravel K. , et al. Barriers and facilitators to implementing shared decision-making in clinical practice: update of a systematic review of health professionals’ perceptions. Patient Educ Couns 2008. Dec; 73(3): 52635. PMID: 18752915. 13. Guadagnoli E. , Ward P. Patient participation in decision-making. Soc Sci Med 1998 Aug; 47(3): 329 -39. PMID: 9681902. 14. Murray E. , Charles C. , Gafni A. Shared decision-making in primary care: tailoring the Charles et al. model to fit the context of general practice. Patient 66 Educ Couns 2006 Aug; 62(2): 205 -11. PMID: 16139467.


