47d9ac15161821384028099e88e8e364.ppt
- Количество слайдов: 30
 The Scope of Occupational Therapy Practice in Primary Care in Canada Catherine Donnelly Ph. D, Nicole Bobbette Ph. D(C), Carri Hand Ph. D, Amanda Mofina MSc. OT, Ashley Williams MSc. OT, Lori Letts Ph. D
The Scope of Occupational Therapy Practice in Primary Care in Canada Catherine Donnelly Ph. D, Nicole Bobbette Ph. D(C), Carri Hand Ph. D, Amanda Mofina MSc. OT, Ashley Williams MSc. OT, Lori Letts Ph. D

 Primary Care - Canada Hutchinson et al. , (2011). Primary Care in Canada: Systems in Motion: Milbank Quarterly, 89, 356 -288
Primary Care - Canada Hutchinson et al. , (2011). Primary Care in Canada: Systems in Motion: Milbank Quarterly, 89, 356 -288
 Interprofessional Teams in Canada Community Health Centres Integrated health networks -26 Primary care networks - 40 -70% of dr Integrated nework clinics Physician - “cliniquesintegrated re seau networks inte gre es” Family Health - 12 (CRIs), Teams -185, 25% of Ontarions Improving Primary Health Care Through Collaboration: Current Knowledge about IP Team in Canada, (2012) Conference Board of Canada
Interprofessional Teams in Canada Community Health Centres Integrated health networks -26 Primary care networks - 40 -70% of dr Integrated nework clinics Physician - “cliniquesintegrated re seau networks inte gre es” Family Health - 12 (CRIs), Teams -185, 25% of Ontarions Improving Primary Health Care Through Collaboration: Current Knowledge about IP Team in Canada, (2012) Conference Board of Canada
 What we know … The role of OT in primary care is still developing and emerging across the globe (CAOT, 2014; Donnelly et al. , 2013; Donnelly et. al, 2014; Donnelly et al; 2015) Understanding to date is largely based on self-report (Donnelly et al. , 2013; Donnelly et. al, 2014; Donnelly et al; 2015) Developing evidence: • chronic conditions (Garvey et al. , 2015; Richardson et al. , 2010; 2012) • mental health (Cook & Howe, 2003) • older adults (complex older adult, falls prevention and well elderly) (Clemson & Mc. Kenzie, 2014; Tracy et al, 2013, Clark et al. , 19)
What we know … The role of OT in primary care is still developing and emerging across the globe (CAOT, 2014; Donnelly et al. , 2013; Donnelly et. al, 2014; Donnelly et al; 2015) Understanding to date is largely based on self-report (Donnelly et al. , 2013; Donnelly et. al, 2014; Donnelly et al; 2015) Developing evidence: • chronic conditions (Garvey et al. , 2015; Richardson et al. , 2010; 2012) • mental health (Cook & Howe, 2003) • older adults (complex older adult, falls prevention and well elderly) (Clemson & Mc. Kenzie, 2014; Tracy et al, 2013, Clark et al. , 19)
 The Issue A need to measure the impact of OT and interprofessional primary care (IPC) teams (Glazier et al. , 2012; Health Quality Ontario, 2014) No data is being collected for IPC team members in Canada (Jaakkimainen, et al. , 2009) Need to further understand the scope of OT to best demonstrate value
The Issue A need to measure the impact of OT and interprofessional primary care (IPC) teams (Glazier et al. , 2012; Health Quality Ontario, 2014) No data is being collected for IPC team members in Canada (Jaakkimainen, et al. , 2009) Need to further understand the scope of OT to best demonstrate value
 Objectives 1. To gain information about the scope of clinical practice of occupational therapists working in IPC teams. 2. Develop an efficient method to collect real-time occupational therapy client visit data for use within IPC teams.
Objectives 1. To gain information about the scope of clinical practice of occupational therapists working in IPC teams. 2. Develop an efficient method to collect real-time occupational therapy client visit data for use within IPC teams.
 Methods Cross sectional observational study Mixed methods approach -Qualitative interviews -EMR data collection - Survey BEACH study - Australian study of primary care practice in Australia (Bayram et al. , 2007)
Methods Cross sectional observational study Mixed methods approach -Qualitative interviews -EMR data collection - Survey BEACH study - Australian study of primary care practice in Australia (Bayram et al. , 2007)
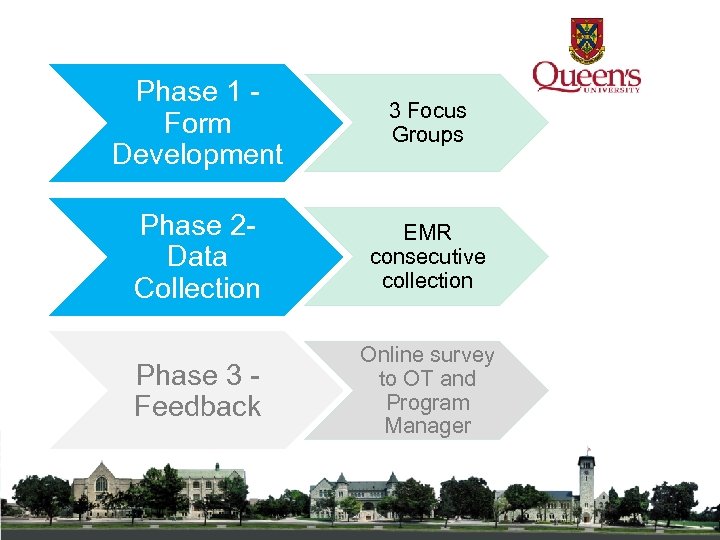 Phase 1 - Form Development 3 Focus Groups Phase 2 - Data Collection EMR consecutive collection Phase 3 - Feedback Online survey to OT and Program Manager
Phase 1 - Form Development 3 Focus Groups Phase 2 - Data Collection EMR consecutive collection Phase 3 - Feedback Online survey to OT and Program Manager
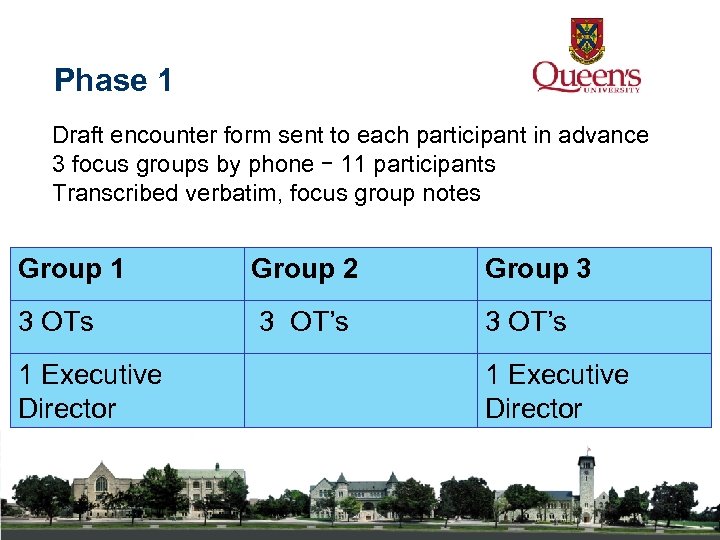 Phase 1 Draft encounter form sent to each participant in advance 3 focus groups by phone – 11 participants Transcribed verbatim, focus group notes Group 1 Group 2 Group 3 3 OTs 3 OT’s 1 Executive Director
Phase 1 Draft encounter form sent to each participant in advance 3 focus groups by phone – 11 participants Transcribed verbatim, focus group notes Group 1 Group 2 Group 3 3 OTs 3 OT’s 1 Executive Director
 Encounter Form 1. Encounter details 2. Client data 3. Reason for encounter Occupational Performance issues; new/continuing 4. Management of each issue 5. Interprofessional collaboration
Encounter Form 1. Encounter details 2. Client data 3. Reason for encounter Occupational Performance issues; new/continuing 4. Management of each issue 5. Interprofessional collaboration
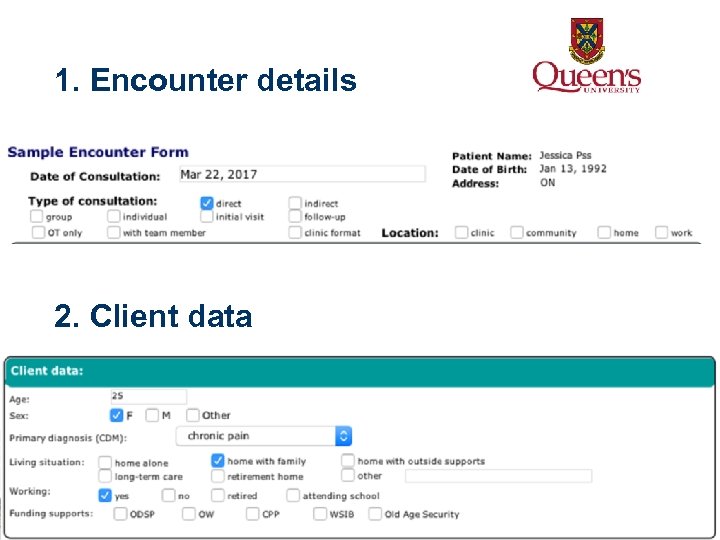 1. Encounter details 2. Client data
1. Encounter details 2. Client data
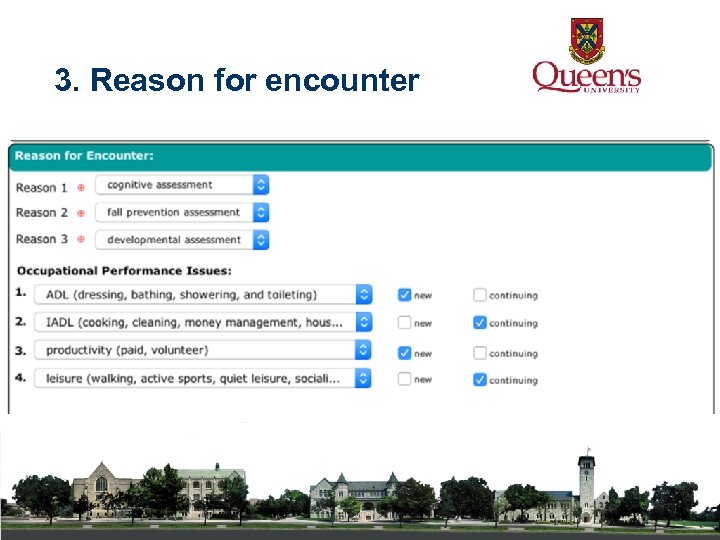 3. Reason for encounter
3. Reason for encounter
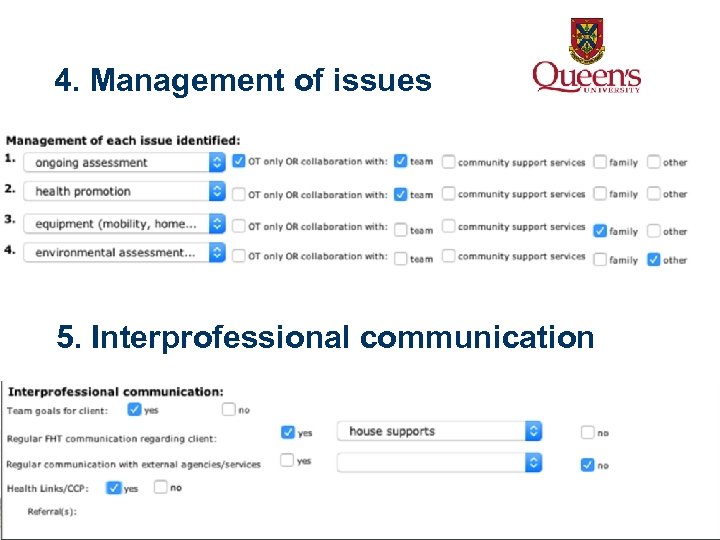 4. Management of issues 5. Interprofessional communication
4. Management of issues 5. Interprofessional communication
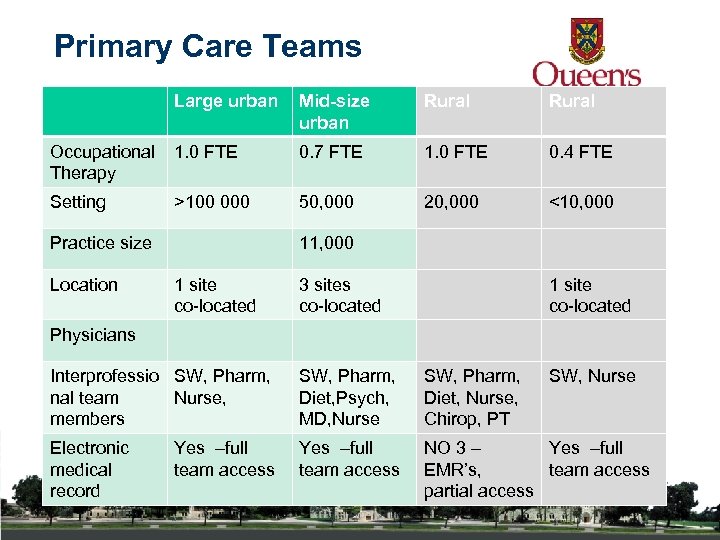 Primary Care Teams Large urban Mid-size urban Rural Occupational 1. 0 FTE Therapy 0. 7 FTE 1. 0 FTE 0. 4 FTE Setting 50, 000 20, 000 <10, 000 >100 000 Practice size Location 11, 000 1 site co-located 3 sites co-located 1 site co-located Physicians Interprofessio SW, Pharm, nal team Nurse, members SW, Pharm, Diet, Psych, MD, Nurse SW, Pharm, Diet, Nurse, Chirop, PT Electronic medical record Yes –full team access NO 3 – Yes –full EMR’s, team access partial access Yes –full team access SW, Nurse
Primary Care Teams Large urban Mid-size urban Rural Occupational 1. 0 FTE Therapy 0. 7 FTE 1. 0 FTE 0. 4 FTE Setting 50, 000 20, 000 <10, 000 >100 000 Practice size Location 11, 000 1 site co-located 3 sites co-located 1 site co-located Physicians Interprofessio SW, Pharm, nal team Nurse, members SW, Pharm, Diet, Psych, MD, Nurse SW, Pharm, Diet, Nurse, Chirop, PT Electronic medical record Yes –full team access NO 3 – Yes –full EMR’s, team access partial access Yes –full team access SW, Nurse
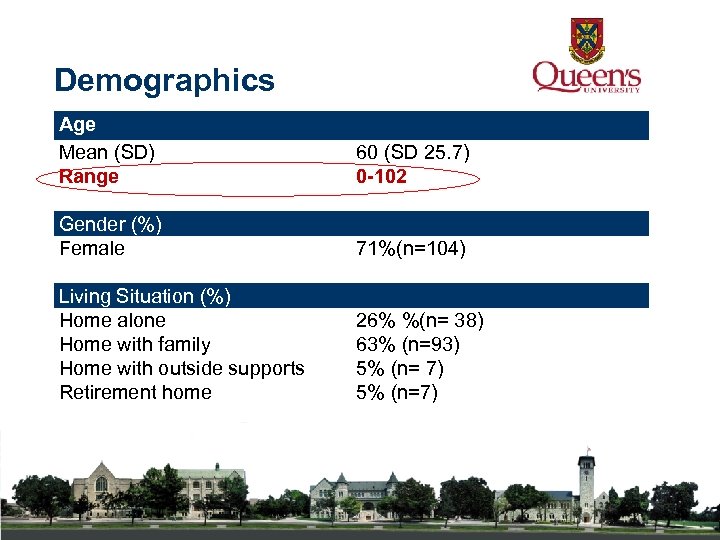 Demographics Age Mean (SD) Range 60 (SD 25. 7) 0 -102 Gender (%) Female Living Situation (%) Home alone Home with family Home with outside supports Retirement home 71%(n=104) 26% %(n= 38) 63% (n=93) 5% (n= 7) 5% (n=7)
Demographics Age Mean (SD) Range 60 (SD 25. 7) 0 -102 Gender (%) Female Living Situation (%) Home alone Home with family Home with outside supports Retirement home 71%(n=104) 26% %(n= 38) 63% (n=93) 5% (n= 7) 5% (n=7)
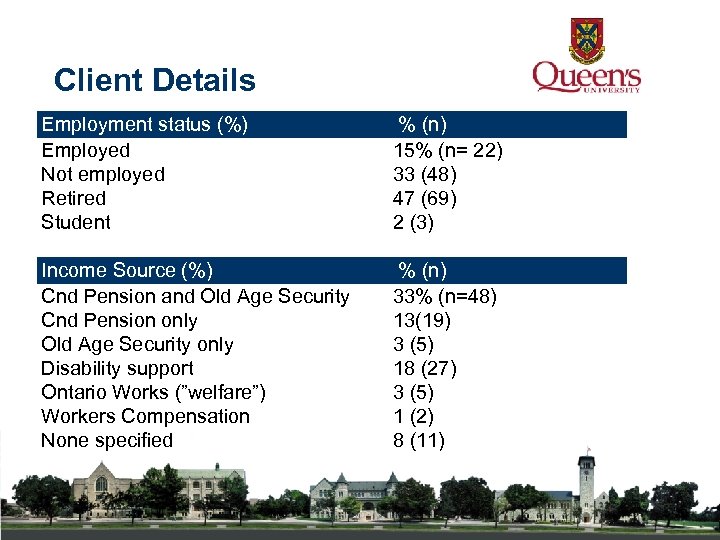 Client Details Employment status (%) Employed Not employed Retired Student Income Source (%) Cnd Pension and Old Age Security Cnd Pension only Old Age Security only Disability support Ontario Works (”welfare”) Workers Compensation None specified % (n) 15% (n= 22) 33 (48) 47 (69) 2 (3) % (n) 33% (n=48) 13(19) 3 (5) 18 (27) 3 (5) 1 (2) 8 (11)
Client Details Employment status (%) Employed Not employed Retired Student Income Source (%) Cnd Pension and Old Age Security Cnd Pension only Old Age Security only Disability support Ontario Works (”welfare”) Workers Compensation None specified % (n) 15% (n= 22) 33 (48) 47 (69) 2 (3) % (n) 33% (n=48) 13(19) 3 (5) 18 (27) 3 (5) 1 (2) 8 (11)
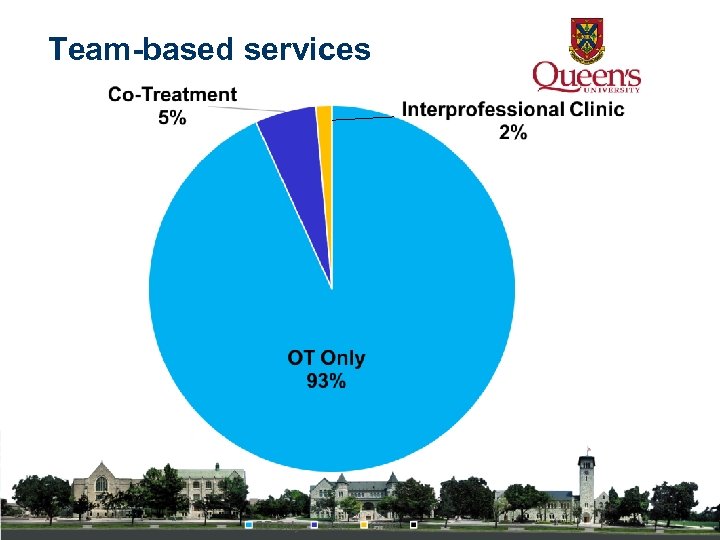 Team-based services
Team-based services
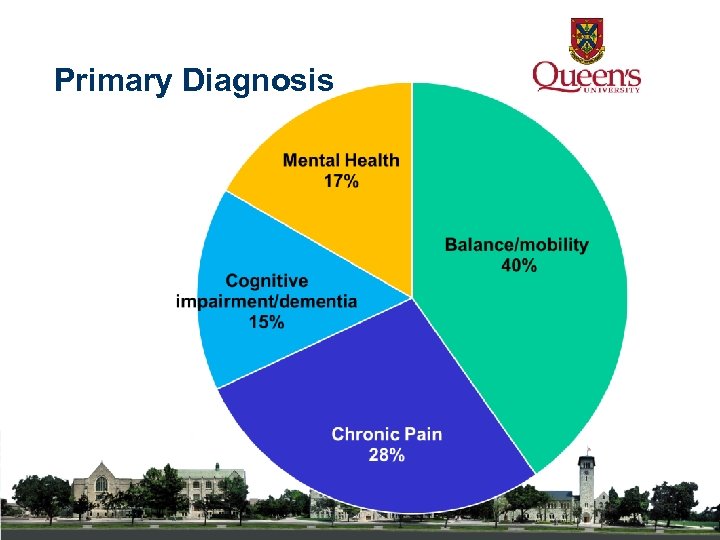 Primary Diagnosis
Primary Diagnosis
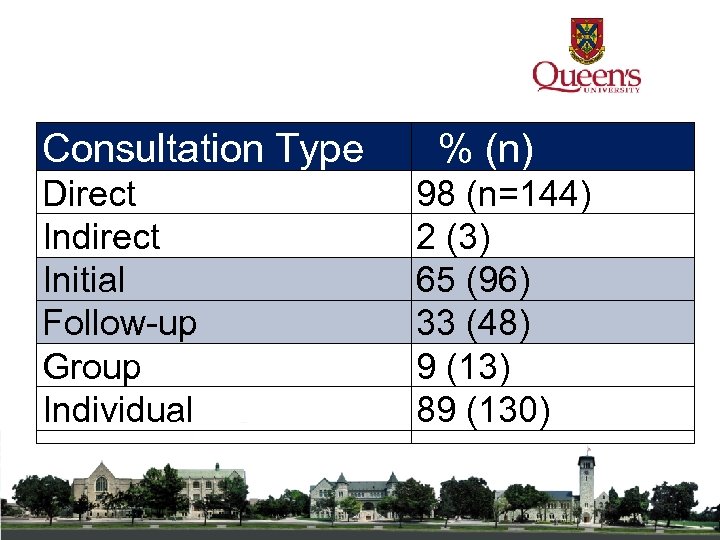 Consultation Type % (n) Direct Indirect Initial Follow-up Group Individual 98 (n=144) 2 (3) 65 (96) 33 (48) 9 (13) 89 (130)
Consultation Type % (n) Direct Indirect Initial Follow-up Group Individual 98 (n=144) 2 (3) 65 (96) 33 (48) 9 (13) 89 (130)
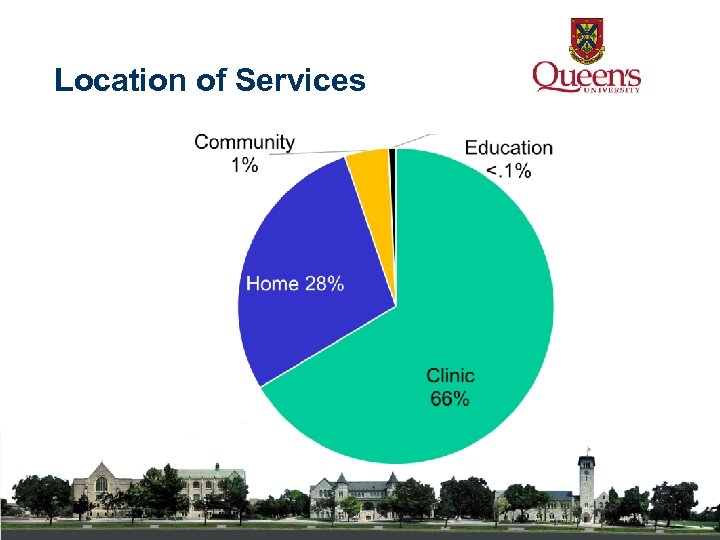 Location of Services
Location of Services
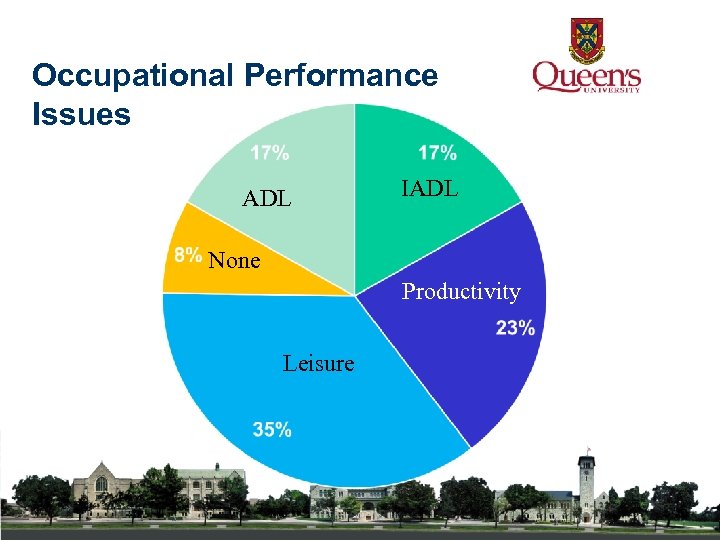 Occupational Performance Issues ADL IADL None Productivity Leisure
Occupational Performance Issues ADL IADL None Productivity Leisure
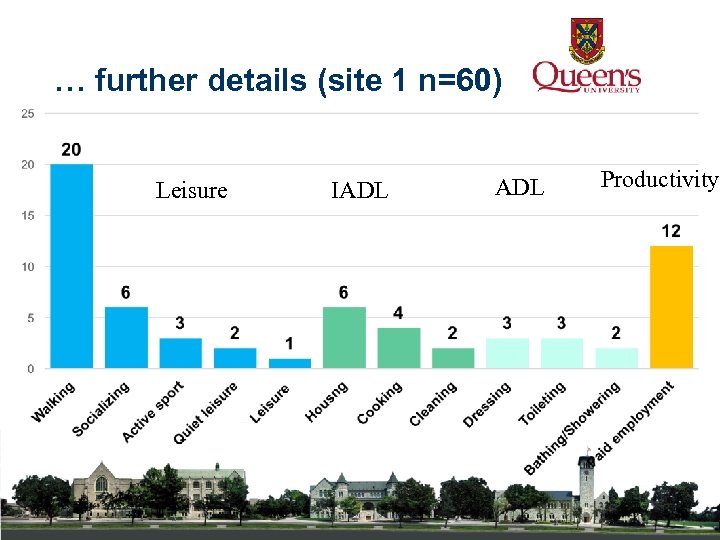 … further details (site 1 n=60) Leisure IADL Productivity
… further details (site 1 n=60) Leisure IADL Productivity
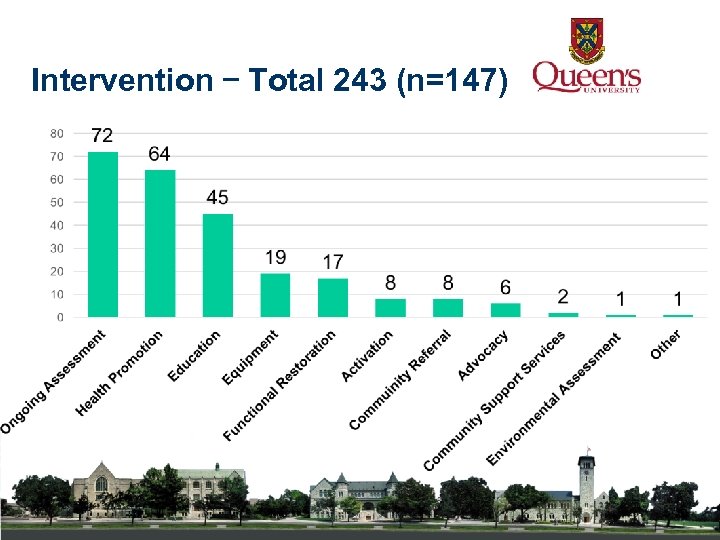 Intervention – Total 243 (n=147)
Intervention – Total 243 (n=147)
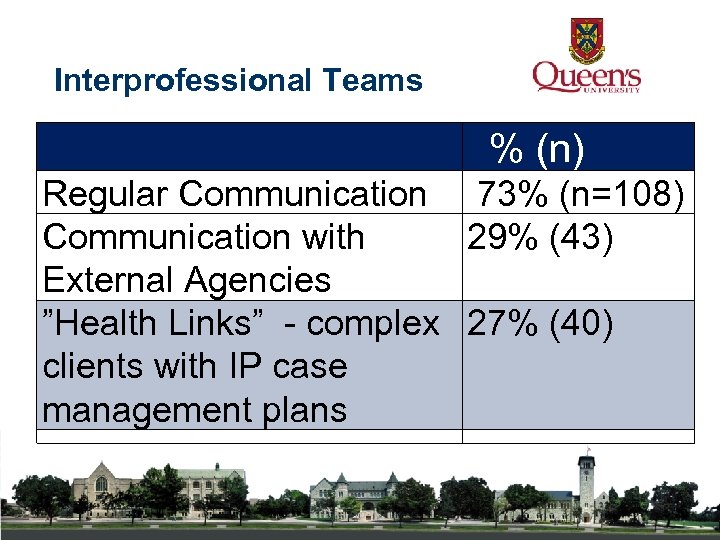 Interprofessional Teams % (n) Regular Communication 73% (n=108) Communication with 29% (43) External Agencies ”Health Links” - complex 27% (40) clients with IP case management plans
Interprofessional Teams % (n) Regular Communication 73% (n=108) Communication with 29% (43) External Agencies ”Health Links” - complex 27% (40) clients with IP case management plans
 Key Points Working as a generalist across the lifespan – predominately in clinics Emphasis on assessment - with focus on education and health promotion Working in a team with frequent communication within team and less so externally Critical need to develop evidence based interventions – with an focus on education interventions
Key Points Working as a generalist across the lifespan – predominately in clinics Emphasis on assessment - with focus on education and health promotion Working in a team with frequent communication within team and less so externally Critical need to develop evidence based interventions – with an focus on education interventions
 Next steps Expand number of sites to implement encounter form Link encounter data with population health data to compare clients who were seen by OT vs those that were not Identify OT primary care performance indicators
Next steps Expand number of sites to implement encounter form Link encounter data with population health data to compare clients who were seen by OT vs those that were not Identify OT primary care performance indicators
 References Bayram, C. , Britt, H. , & Miller, G. (2007). The quality of data on general practice: a discussion of BEACH reliability and validity. Australian Family Physician, 36(1 -2), 36 -40. Bumphrey, E. E. (1989). Occupational therapy within the primary health care team. British Journal of Occupational Therapy, 52, 251 -255. Cook, S. , & Howe, A. , (2003). Engaging people with enduring psychotic conditions in primary mental heath care and occupational therapy. British Journal of Occupational Therapy, 66(6), 236 -246. Devereaux, E. B. , & Walker, R. B. (1995). The role of occupational therapy in primary health care. American Journal of Occupational Therapy, 49, 391 -396. Mc. Coll, M. A. , Shortt, S. , Godwin, M. , Smith, K. , Rowe, K. , O’Brien, P. , & Donnelly, C. (2009). Models for integrating rehabilitation and primary care: A scoping study. Archives of Physical Medicine and Rehabilitation, 90, 523 -531. Mackenzie, L. , Clemson, L. , & Roberts, C. (2013) Occupational therapists partnering with general practitioners to prevent falls: Seizing opportunities in primary health care. Australian Journal of Occupational Therapy, 60, 66 -70 Metzler, C. A. , Hartmann, K. D. , Lowenthal, L. A. (2012). Defining primary care: Envisioning the roles of occupational therapy. The American Journal of Occupational Therapy, 66(3), 266 - 269 Muir, S. (2012). Occupational therapy in primary health care: We should be there. American Journal of Occupational Therapy, 66, 506 -510. doi: 10. 5014/ajot. 2012. 665001 Richardson, J. , Letts, L. , Chan, D. , Officer, A. , Wojkowski, S. , Oliver, D. , et al. (2012). Monitoring physical functioning as the sixth vital sign: Evaluating patient and practice engagement in chronic illness care in a primary care setting—a quasi-experimental design. BMC Family Practice, 13(29).
References Bayram, C. , Britt, H. , & Miller, G. (2007). The quality of data on general practice: a discussion of BEACH reliability and validity. Australian Family Physician, 36(1 -2), 36 -40. Bumphrey, E. E. (1989). Occupational therapy within the primary health care team. British Journal of Occupational Therapy, 52, 251 -255. Cook, S. , & Howe, A. , (2003). Engaging people with enduring psychotic conditions in primary mental heath care and occupational therapy. British Journal of Occupational Therapy, 66(6), 236 -246. Devereaux, E. B. , & Walker, R. B. (1995). The role of occupational therapy in primary health care. American Journal of Occupational Therapy, 49, 391 -396. Mc. Coll, M. A. , Shortt, S. , Godwin, M. , Smith, K. , Rowe, K. , O’Brien, P. , & Donnelly, C. (2009). Models for integrating rehabilitation and primary care: A scoping study. Archives of Physical Medicine and Rehabilitation, 90, 523 -531. Mackenzie, L. , Clemson, L. , & Roberts, C. (2013) Occupational therapists partnering with general practitioners to prevent falls: Seizing opportunities in primary health care. Australian Journal of Occupational Therapy, 60, 66 -70 Metzler, C. A. , Hartmann, K. D. , Lowenthal, L. A. (2012). Defining primary care: Envisioning the roles of occupational therapy. The American Journal of Occupational Therapy, 66(3), 266 - 269 Muir, S. (2012). Occupational therapy in primary health care: We should be there. American Journal of Occupational Therapy, 66, 506 -510. doi: 10. 5014/ajot. 2012. 665001 Richardson, J. , Letts, L. , Chan, D. , Officer, A. , Wojkowski, S. , Oliver, D. , et al. (2012). Monitoring physical functioning as the sixth vital sign: Evaluating patient and practice engagement in chronic illness care in a primary care setting—a quasi-experimental design. BMC Family Practice, 13(29).
 Richardson, J. , Letts, L. , Chan, D. , Stratford, P. , Hand, C. , Price, D. , et al. (2010). Rehabilitation in a primary care setting for persons with chronic illness: A randomized controlled trial. Primary Health Care Research and Development, 11, 382 -395. Tracy, C. A. , Bell, S. , H. , Nickell, L. A, Charles, J. , & Upshur, R. (2013) The IMPACT model of interprofessional primary care for elderly patients with complex health care needs. Canadian Family Physician. , 59, e-148 -e 155. http: //www. cfp. ca/content/59/3/e 148. full. pdf+html
Tse, S. , Penman, M. , & Simms, F. (2003). Literature review: Occupational therapy and primary health care. New Zealand Journal of Occupational Therapy, 50(20), 17 -23.
Richardson, J. , Letts, L. , Chan, D. , Stratford, P. , Hand, C. , Price, D. , et al. (2010). Rehabilitation in a primary care setting for persons with chronic illness: A randomized controlled trial. Primary Health Care Research and Development, 11, 382 -395. Tracy, C. A. , Bell, S. , H. , Nickell, L. A, Charles, J. , & Upshur, R. (2013) The IMPACT model of interprofessional primary care for elderly patients with complex health care needs. Canadian Family Physician. , 59, e-148 -e 155. http: //www. cfp. ca/content/59/3/e 148. full. pdf+html
Tse, S. , Penman, M. , & Simms, F. (2003). Literature review: Occupational therapy and primary health care. New Zealand Journal of Occupational Therapy, 50(20), 17 -23.


