8aad1a69683d9dba52af23ebcd276b03.ppt
- Количество слайдов: 7
 THE RIGHT TO LIVE AND DIE WITH DIGNITY – AT HOME Supporting Terminally Ill Patients who Wish to Live out Their Lives at Home ISRAEL S. BERGER, M. D. & DORON GARFINKEL, M. D. MACCABI HEALTHCARE SERVICES HOME CARE UNIT - DAN DISTRICT
THE RIGHT TO LIVE AND DIE WITH DIGNITY – AT HOME Supporting Terminally Ill Patients who Wish to Live out Their Lives at Home ISRAEL S. BERGER, M. D. & DORON GARFINKEL, M. D. MACCABI HEALTHCARE SERVICES HOME CARE UNIT - DAN DISTRICT
 HOME HOSPITAL
HOME HOSPITAL
 1 BACKGROUND: Aging is inevitably associated with an exponential increase in the incidence and complexity of chronic, age - related diseases. Therefore, a net increase in survival would translate into more years of compromised physical, mental and social functioning. Improved medical technology in the last decades has resulted in a sharp increase in life span even for patients suffering from chronic and terminal diseases. Accordingly, the average length of survival since a patient is first classified as “non-curative” until death, is increasing all the time. Some terminally ill patients and their families prefer to live at home even in the presence of severe debilitating disease, and for them hospitalization may represent a severe impairment of their quality of life. Obviously, due to the very high cost of hospitalization particularly in the last months or weeks of life, treating terminally ill patients at home is also a desirable goal for all medical systems. Paradoxically, physicians and health professionals sometimes pressure these patients to spend their last period of life away from home even if there is no apparent advantage of hospital over home care. This in part, may be an attempt to relieve the heavy medical and legal responsibility of caring for dying people at home. However, the comprehensive palliative approach insists on helping patients at every stage of their disease by relieving physical suffering and also attempting to alleviate mental, familial, social and financial problems. Palliative care should be given according to the patients’ individual needs, whether they wish to receive it in an institutional setting or at home.
1 BACKGROUND: Aging is inevitably associated with an exponential increase in the incidence and complexity of chronic, age - related diseases. Therefore, a net increase in survival would translate into more years of compromised physical, mental and social functioning. Improved medical technology in the last decades has resulted in a sharp increase in life span even for patients suffering from chronic and terminal diseases. Accordingly, the average length of survival since a patient is first classified as “non-curative” until death, is increasing all the time. Some terminally ill patients and their families prefer to live at home even in the presence of severe debilitating disease, and for them hospitalization may represent a severe impairment of their quality of life. Obviously, due to the very high cost of hospitalization particularly in the last months or weeks of life, treating terminally ill patients at home is also a desirable goal for all medical systems. Paradoxically, physicians and health professionals sometimes pressure these patients to spend their last period of life away from home even if there is no apparent advantage of hospital over home care. This in part, may be an attempt to relieve the heavy medical and legal responsibility of caring for dying people at home. However, the comprehensive palliative approach insists on helping patients at every stage of their disease by relieving physical suffering and also attempting to alleviate mental, familial, social and financial problems. Palliative care should be given according to the patients’ individual needs, whether they wish to receive it in an institutional setting or at home.
 2…… PATIENTS and METHODS: Over the past year, our Home Care team has been taking care of about 350 different patients, several dozens died, most of them in an institutional setting. Fifteen families of terminally ill patients requested that the patient live at home until death. They all realized that the patient had no cure and we repeatedly discussed with them in depth, the possibilities and limitations of palliative care. In each case, there was a consensus between family and patient (unless the later had severe dementia) that the patient should stay at home no matter what happens, even if the situation worsens, symptoms aggravate or death occurs. We enabled them to accomplish this by providing a 24 hour medical availability. In most patient the physician was also present at the patient’s beds in their last hours at home. RESULTS: There were 11 men, four women, most of them were living with a spouse who also served as the primary care giver in about half of the cases. The average period of treatment by our team was several months, range - one week to several years (in one patient with severe dementia). The main disease that eventually led to death was advanced cancer in seven patients; others suffered from end stage liver failure, amyotrophic lateral sclerosis (ALS), end stage pulmonary fibrosis and dementia. The age upon death ranged from 63 to 93; In all patients, only palliative care was given, most of them died with mild or no pain, with very few distressing symptoms during the last days of their life. In most patients, the Home Care physician was present at the time of death and signed the death certificate.
2…… PATIENTS and METHODS: Over the past year, our Home Care team has been taking care of about 350 different patients, several dozens died, most of them in an institutional setting. Fifteen families of terminally ill patients requested that the patient live at home until death. They all realized that the patient had no cure and we repeatedly discussed with them in depth, the possibilities and limitations of palliative care. In each case, there was a consensus between family and patient (unless the later had severe dementia) that the patient should stay at home no matter what happens, even if the situation worsens, symptoms aggravate or death occurs. We enabled them to accomplish this by providing a 24 hour medical availability. In most patient the physician was also present at the patient’s beds in their last hours at home. RESULTS: There were 11 men, four women, most of them were living with a spouse who also served as the primary care giver in about half of the cases. The average period of treatment by our team was several months, range - one week to several years (in one patient with severe dementia). The main disease that eventually led to death was advanced cancer in seven patients; others suffered from end stage liver failure, amyotrophic lateral sclerosis (ALS), end stage pulmonary fibrosis and dementia. The age upon death ranged from 63 to 93; In all patients, only palliative care was given, most of them died with mild or no pain, with very few distressing symptoms during the last days of their life. In most patients, the Home Care physician was present at the time of death and signed the death certificate.
 3…… CONCLUSION: A proper medical support group can enable patients and families who wish to die at home, to do so with dignity while experiencing a reasonable quality of life before death. Furthermore, applying this approach to large populations of incurable patients would probably have beneficial economic and social implications as well.
3…… CONCLUSION: A proper medical support group can enable patients and families who wish to die at home, to do so with dignity while experiencing a reasonable quality of life before death. Furthermore, applying this approach to large populations of incurable patients would probably have beneficial economic and social implications as well.
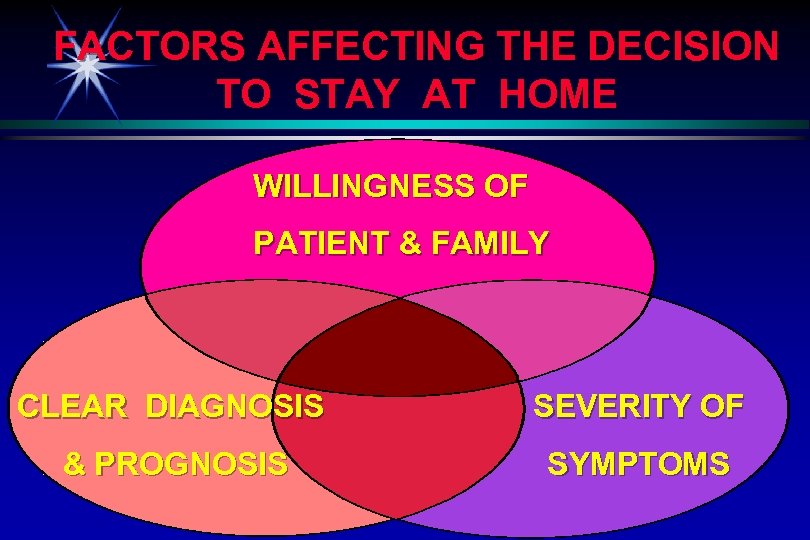 FACTORS AFFECTING THE DECISION TO STAY AT HOME WILLINGNESS OF PATIENT & FAMILY CLEAR DIAGNOSIS SEVERITY OF & PROGNOSIS SYMPTOMS
FACTORS AFFECTING THE DECISION TO STAY AT HOME WILLINGNESS OF PATIENT & FAMILY CLEAR DIAGNOSIS SEVERITY OF & PROGNOSIS SYMPTOMS
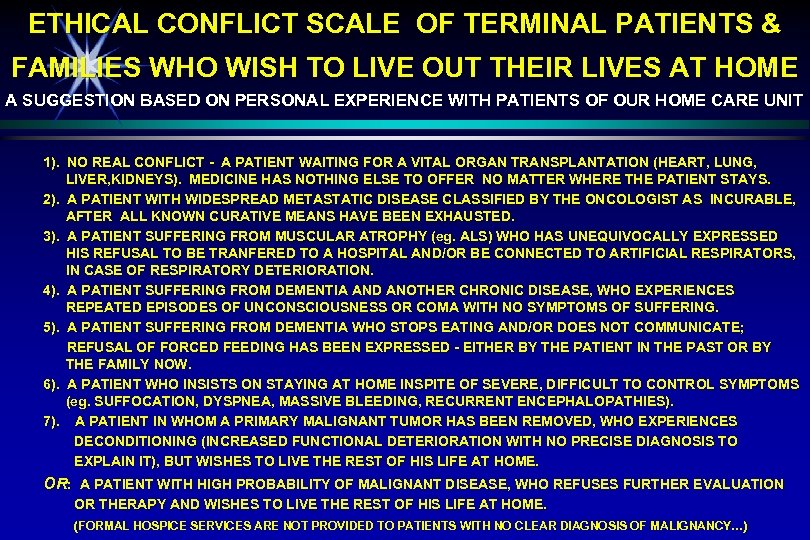 ETHICAL CONFLICT SCALE OF TERMINAL PATIENTS & FAMILIES WHO WISH TO LIVE OUT THEIR LIVES AT HOME A SUGGESTION BASED ON PERSONAL EXPERIENCE WITH PATIENTS OF OUR HOME CARE UNIT 1). NO REAL CONFLICT - A PATIENT WAITING FOR A VITAL ORGAN TRANSPLANTATION (HEART, LUNG, LIVER, KIDNEYS). MEDICINE HAS NOTHING ELSE TO OFFER NO MATTER WHERE THE PATIENT STAYS. 2). A PATIENT WITH WIDESPREAD METASTATIC DISEASE CLASSIFIED BY THE ONCOLOGIST AS INCURABLE, AFTER ALL KNOWN CURATIVE MEANS HAVE BEEN EXHAUSTED. 3). A PATIENT SUFFERING FROM MUSCULAR ATROPHY (eg. ALS) WHO HAS UNEQUIVOCALLY EXPRESSED HIS REFUSAL TO BE TRANFERED TO A HOSPITAL AND/OR BE CONNECTED TO ARTIFICIAL RESPIRATORS, IN CASE OF RESPIRATORY DETERIORATION. 4). A PATIENT SUFFERING FROM DEMENTIA AND ANOTHER CHRONIC DISEASE, WHO EXPERIENCES REPEATED EPISODES OF UNCONSCIOUSNESS OR COMA WITH NO SYMPTOMS OF SUFFERING. 5). A PATIENT SUFFERING FROM DEMENTIA WHO STOPS EATING AND/OR DOES NOT COMMUNICATE; REFUSAL OF FORCED FEEDING HAS BEEN EXPRESSED - EITHER BY THE PATIENT IN THE PAST OR BY THE FAMILY NOW. 6). A PATIENT WHO INSISTS ON STAYING AT HOME INSPITE OF SEVERE, DIFFICULT TO CONTROL SYMPTOMS (eg. SUFFOCATION, DYSPNEA, MASSIVE BLEEDING, RECURRENT ENCEPHALOPATHIES). 7). A PATIENT IN WHOM A PRIMARY MALIGNANT TUMOR HAS BEEN REMOVED, WHO EXPERIENCES DECONDITIONING (INCREASED FUNCTIONAL DETERIORATION WITH NO PRECISE DIAGNOSIS TO EXPLAIN IT), BUT WISHES TO LIVE THE REST OF HIS LIFE AT HOME. OR: A PATIENT WITH HIGH PROBABILITY OF MALIGNANT DISEASE, WHO REFUSES FURTHER EVALUATION OR THERAPY AND WISHES TO LIVE THE REST OF HIS LIFE AT HOME. (FORMAL HOSPICE SERVICES ARE NOT PROVIDED TO PATIENTS WITH NO CLEAR DIAGNOSIS OF MALIGNANCY…)
ETHICAL CONFLICT SCALE OF TERMINAL PATIENTS & FAMILIES WHO WISH TO LIVE OUT THEIR LIVES AT HOME A SUGGESTION BASED ON PERSONAL EXPERIENCE WITH PATIENTS OF OUR HOME CARE UNIT 1). NO REAL CONFLICT - A PATIENT WAITING FOR A VITAL ORGAN TRANSPLANTATION (HEART, LUNG, LIVER, KIDNEYS). MEDICINE HAS NOTHING ELSE TO OFFER NO MATTER WHERE THE PATIENT STAYS. 2). A PATIENT WITH WIDESPREAD METASTATIC DISEASE CLASSIFIED BY THE ONCOLOGIST AS INCURABLE, AFTER ALL KNOWN CURATIVE MEANS HAVE BEEN EXHAUSTED. 3). A PATIENT SUFFERING FROM MUSCULAR ATROPHY (eg. ALS) WHO HAS UNEQUIVOCALLY EXPRESSED HIS REFUSAL TO BE TRANFERED TO A HOSPITAL AND/OR BE CONNECTED TO ARTIFICIAL RESPIRATORS, IN CASE OF RESPIRATORY DETERIORATION. 4). A PATIENT SUFFERING FROM DEMENTIA AND ANOTHER CHRONIC DISEASE, WHO EXPERIENCES REPEATED EPISODES OF UNCONSCIOUSNESS OR COMA WITH NO SYMPTOMS OF SUFFERING. 5). A PATIENT SUFFERING FROM DEMENTIA WHO STOPS EATING AND/OR DOES NOT COMMUNICATE; REFUSAL OF FORCED FEEDING HAS BEEN EXPRESSED - EITHER BY THE PATIENT IN THE PAST OR BY THE FAMILY NOW. 6). A PATIENT WHO INSISTS ON STAYING AT HOME INSPITE OF SEVERE, DIFFICULT TO CONTROL SYMPTOMS (eg. SUFFOCATION, DYSPNEA, MASSIVE BLEEDING, RECURRENT ENCEPHALOPATHIES). 7). A PATIENT IN WHOM A PRIMARY MALIGNANT TUMOR HAS BEEN REMOVED, WHO EXPERIENCES DECONDITIONING (INCREASED FUNCTIONAL DETERIORATION WITH NO PRECISE DIAGNOSIS TO EXPLAIN IT), BUT WISHES TO LIVE THE REST OF HIS LIFE AT HOME. OR: A PATIENT WITH HIGH PROBABILITY OF MALIGNANT DISEASE, WHO REFUSES FURTHER EVALUATION OR THERAPY AND WISHES TO LIVE THE REST OF HIS LIFE AT HOME. (FORMAL HOSPICE SERVICES ARE NOT PROVIDED TO PATIENTS WITH NO CLEAR DIAGNOSIS OF MALIGNANCY…)


