4dc3300bb5d3339a6c0b4b772c2b6e59.ppt
- Количество слайдов: 52
 The Reproductive Health Implications of Depression: Postpartum Depression Association of Reproductive Health Professionals www. arhp. org
The Reproductive Health Implications of Depression: Postpartum Depression Association of Reproductive Health Professionals www. arhp. org
 Expert Medical Advisory Committee • Norma Jo Waxman, MD • Ellen Haller, MD • Ann Hutton, Ph. D, APRN • Kathy Besinque, Pharm. D
Expert Medical Advisory Committee • Norma Jo Waxman, MD • Ellen Haller, MD • Ann Hutton, Ph. D, APRN • Kathy Besinque, Pharm. D
 Polling Question A ?
Polling Question A ?
 Learning Objectives At the end of this session participants should be able to: • Recognize symptoms, risk factors and presentations of depression in women, including pre-menstrual and post partum mood disorders. • Screen women for depression throughout their reproductive years • Prescribe medications for depression in women and know when to refer
Learning Objectives At the end of this session participants should be able to: • Recognize symptoms, risk factors and presentations of depression in women, including pre-menstrual and post partum mood disorders. • Screen women for depression throughout their reproductive years • Prescribe medications for depression in women and know when to refer
 Postpartum Depression (PPD) A sad story… • 35 year old man, named, Moki, is a Japanese immigrant, and member of suicide survivors grief support group • His wife committed suicide two months prior to starting group • She was four months postpartum with third child; two older children 5 and 8 years old
Postpartum Depression (PPD) A sad story… • 35 year old man, named, Moki, is a Japanese immigrant, and member of suicide survivors grief support group • His wife committed suicide two months prior to starting group • She was four months postpartum with third child; two older children 5 and 8 years old
 Question 1 ? D. 80% of women who are pregnant and have symptoms of depression remain untreated.
Question 1 ? D. 80% of women who are pregnant and have symptoms of depression remain untreated.
 Significance of Postpartum Depression • During postpartum period up to 85% of women experience some type of mood disturbance, usually transient, “baby blues. ” • Depression in postpartum period not distinct from major depressive disorders in general
Significance of Postpartum Depression • During postpartum period up to 85% of women experience some type of mood disturbance, usually transient, “baby blues. ” • Depression in postpartum period not distinct from major depressive disorders in general
 Question 2 ? B. Symptom resolution within several days to 2 weeks following birth.
Question 2 ? B. Symptom resolution within several days to 2 weeks following birth.
 “Baby Blues” • Occurs in 70 -85% of women • Onset within the first few days (4 -5 days) after delivery • Resolves by 2 weeks • Symptoms include: mild depression, irritability, tearfulness, fatigue, anxiety • May have increased risk of post-partum major depression later on Beck CT. Am J Nurs. 2006. Hirst KP, Moutier CY. Am Fam Physician. 2010. Pearlstein T, et al. Am J Obstet Gynecol. 2009.
“Baby Blues” • Occurs in 70 -85% of women • Onset within the first few days (4 -5 days) after delivery • Resolves by 2 weeks • Symptoms include: mild depression, irritability, tearfulness, fatigue, anxiety • May have increased risk of post-partum major depression later on Beck CT. Am J Nurs. 2006. Hirst KP, Moutier CY. Am Fam Physician. 2010. Pearlstein T, et al. Am J Obstet Gynecol. 2009.
 Question 3 ? A. Up to 15% of women are estimated to be affected by postpartum depression.
Question 3 ? A. Up to 15% of women are estimated to be affected by postpartum depression.
 Postpartum Depression • Similar symptoms but longer duration and more severe than “baby blues” • Affects 7% to 15% of women • 0. 1% to 2% have postpartum psychosis Beck CT. Am J Nurs. 2006. Hirst KP, Moutier CY. Am Fam Physician. 2010. Pearlstein T, et al. Am J Obstet Gynecol. 2009.
Postpartum Depression • Similar symptoms but longer duration and more severe than “baby blues” • Affects 7% to 15% of women • 0. 1% to 2% have postpartum psychosis Beck CT. Am J Nurs. 2006. Hirst KP, Moutier CY. Am Fam Physician. 2010. Pearlstein T, et al. Am J Obstet Gynecol. 2009.
 Postpartum Depression • Most frequent in first 4 months following birth • Significant impact on both mother and child • Under diagnosed, universal screening needed Beck CT. Am J Nurs. 2006. Hirst KP, Moutier CY. Am Fam Physician. 2010. Pearlstein T, et al. Am J Obstet Gynecol. 2009.
Postpartum Depression • Most frequent in first 4 months following birth • Significant impact on both mother and child • Under diagnosed, universal screening needed Beck CT. Am J Nurs. 2006. Hirst KP, Moutier CY. Am Fam Physician. 2010. Pearlstein T, et al. Am J Obstet Gynecol. 2009.
 Question 4 ? C. Older age at first birth is not a factor associated with increased risk of postpartum depression.
Question 4 ? C. Older age at first birth is not a factor associated with increased risk of postpartum depression.
 Risk Factors for Depression: Pregnancy and Postpartum • History of prior depressive episodes, family history of depression • History of childhood abuse, neglect • Single parent; low SES • Absence of emotional, social support • Unplanned pregnancy • Domestic conflict, violence, abuse
Risk Factors for Depression: Pregnancy and Postpartum • History of prior depressive episodes, family history of depression • History of childhood abuse, neglect • Single parent; low SES • Absence of emotional, social support • Unplanned pregnancy • Domestic conflict, violence, abuse
 Risk Factors for Depression: Pregnancy and Postpartum • Susceptibility to hormonal changes, PMS, PMDD • Recent loss, death, stressful life events • Any infant health problems (ex: colic)
Risk Factors for Depression: Pregnancy and Postpartum • Susceptibility to hormonal changes, PMS, PMDD • Recent loss, death, stressful life events • Any infant health problems (ex: colic)
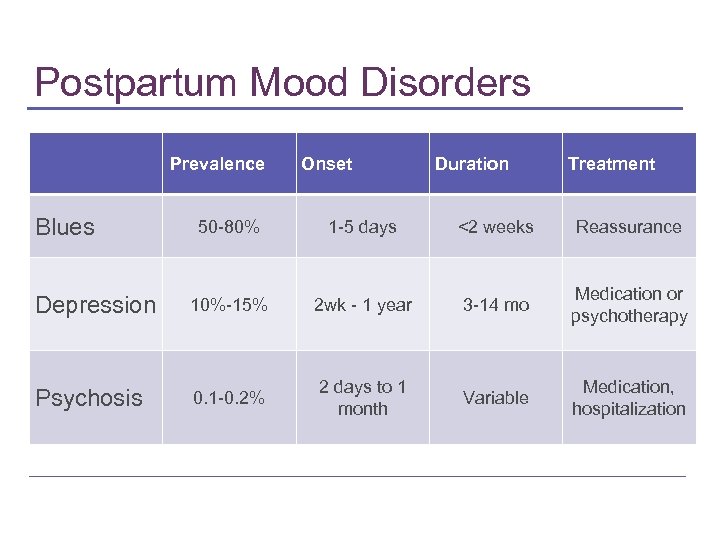 Postpartum Mood Disorders Prevalence Blues Onset Duration Treatment 50 -80% 1 -5 days <2 weeks Reassurance Depression 10%-15% 2 wk - 1 year 3 -14 mo Medication or psychotherapy Psychosis 0. 1 -0. 2% 2 days to 1 month Variable Medication, hospitalization
Postpartum Mood Disorders Prevalence Blues Onset Duration Treatment 50 -80% 1 -5 days <2 weeks Reassurance Depression 10%-15% 2 wk - 1 year 3 -14 mo Medication or psychotherapy Psychosis 0. 1 -0. 2% 2 days to 1 month Variable Medication, hospitalization
 Polling Question B ?
Polling Question B ?
 Screening for Depression • Inquire about mood history before delivery • Alert patient to note mood changes on continuum • Severity guides treatment • Tools for screening
Screening for Depression • Inquire about mood history before delivery • Alert patient to note mood changes on continuum • Severity guides treatment • Tools for screening
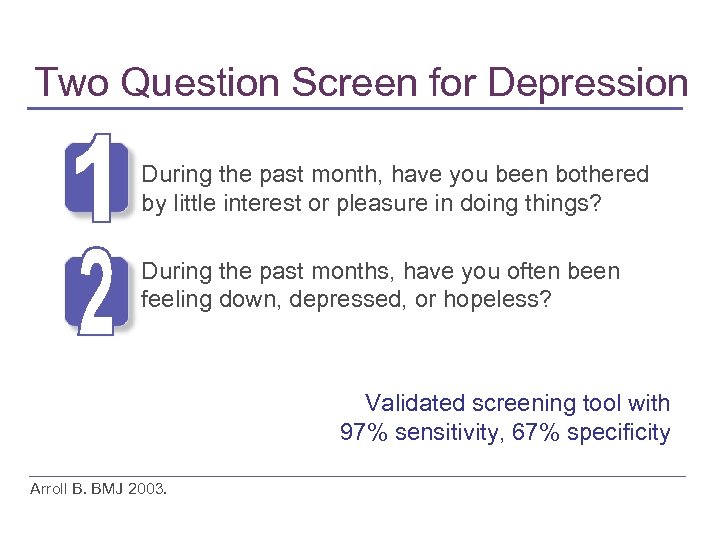 Two Question Screen for Depression During the past month, have you been bothered by little interest or pleasure in doing things? During the past months, have you often been feeling down, depressed, or hopeless? Validated screening tool with 97% sensitivity, 67% specificity Arroll B. BMJ 2003.
Two Question Screen for Depression During the past month, have you been bothered by little interest or pleasure in doing things? During the past months, have you often been feeling down, depressed, or hopeless? Validated screening tool with 97% sensitivity, 67% specificity Arroll B. BMJ 2003.
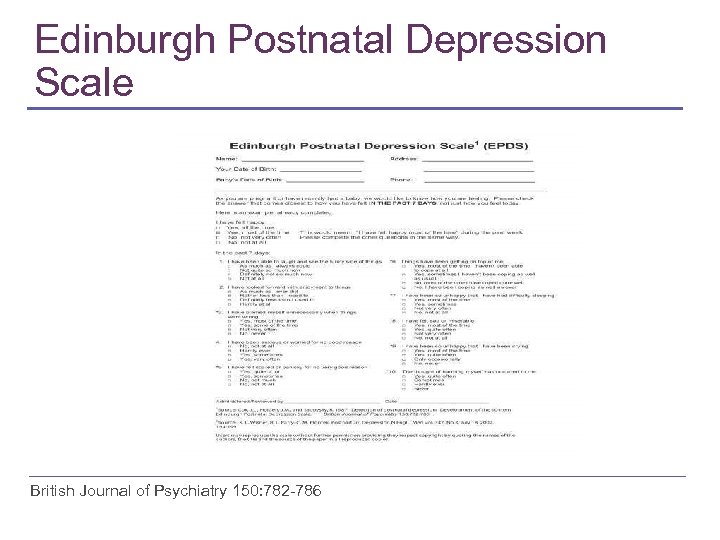 Edinburgh Postnatal Depression Scale British Journal of Psychiatry 150: 782 -786
Edinburgh Postnatal Depression Scale British Journal of Psychiatry 150: 782 -786
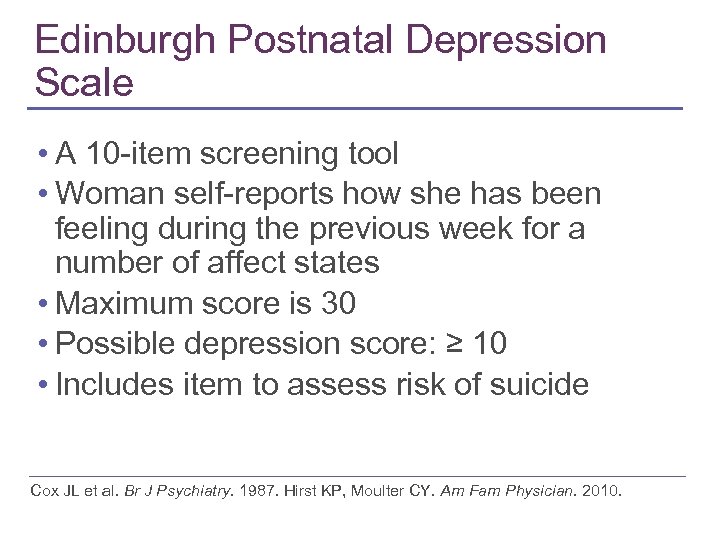 Edinburgh Postnatal Depression Scale • A 10 -item screening tool • Woman self-reports how she has been feeling during the previous week for a number of affect states • Maximum score is 30 • Possible depression score: ≥ 10 • Includes item to assess risk of suicide Cox JL et al. Br J Psychiatry. 1987. Hirst KP, Moulter CY. Am Fam Physician. 2010.
Edinburgh Postnatal Depression Scale • A 10 -item screening tool • Woman self-reports how she has been feeling during the previous week for a number of affect states • Maximum score is 30 • Possible depression score: ≥ 10 • Includes item to assess risk of suicide Cox JL et al. Br J Psychiatry. 1987. Hirst KP, Moulter CY. Am Fam Physician. 2010.
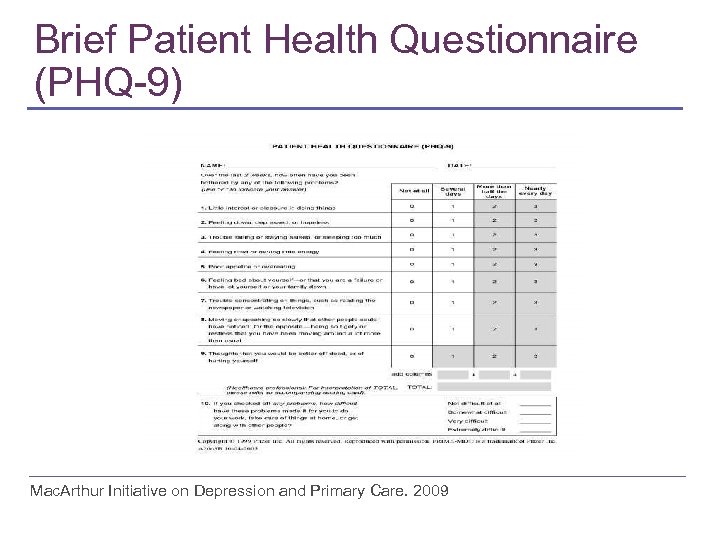 Brief Patient Health Questionnaire (PHQ-9) Mac. Arthur Initiative on Depression and Primary Care. 2009
Brief Patient Health Questionnaire (PHQ-9) Mac. Arthur Initiative on Depression and Primary Care. 2009
 PHQ-9 • 9 Questions based on DSM-IV criteria for major depression • Scores between 10 and 27 = moderate to severe depression • Used by CNMs to make referrals
PHQ-9 • 9 Questions based on DSM-IV criteria for major depression • Scores between 10 and 27 = moderate to severe depression • Used by CNMs to make referrals
 Assessment of Suicide Risk • Screen every patient suspected of depression • Asking does not insult patient or initiate thought • Ask direct questions: • "Have you had thoughts of hurting yourself? " • "Do you sometimes wish your life was over? " • "Have you had thoughts of ending your life? " Hackley et al 2010. Mac. Arthur Initiative on Depression and Primary Care. 2009
Assessment of Suicide Risk • Screen every patient suspected of depression • Asking does not insult patient or initiate thought • Ask direct questions: • "Have you had thoughts of hurting yourself? " • "Do you sometimes wish your life was over? " • "Have you had thoughts of ending your life? " Hackley et al 2010. Mac. Arthur Initiative on Depression and Primary Care. 2009
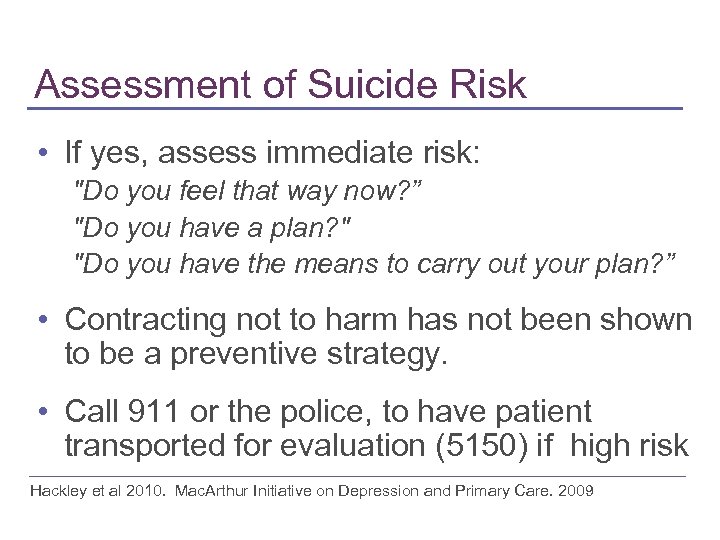 Assessment of Suicide Risk • If yes, assess immediate risk: "Do you feel that way now? ” "Do you have a plan? " "Do you have the means to carry out your plan? ” • Contracting not to harm has not been shown to be a preventive strategy. • Call 911 or the police, to have patient transported for evaluation (5150) if high risk Hackley et al 2010. Mac. Arthur Initiative on Depression and Primary Care. 2009
Assessment of Suicide Risk • If yes, assess immediate risk: "Do you feel that way now? ” "Do you have a plan? " "Do you have the means to carry out your plan? ” • Contracting not to harm has not been shown to be a preventive strategy. • Call 911 or the police, to have patient transported for evaluation (5150) if high risk Hackley et al 2010. Mac. Arthur Initiative on Depression and Primary Care. 2009
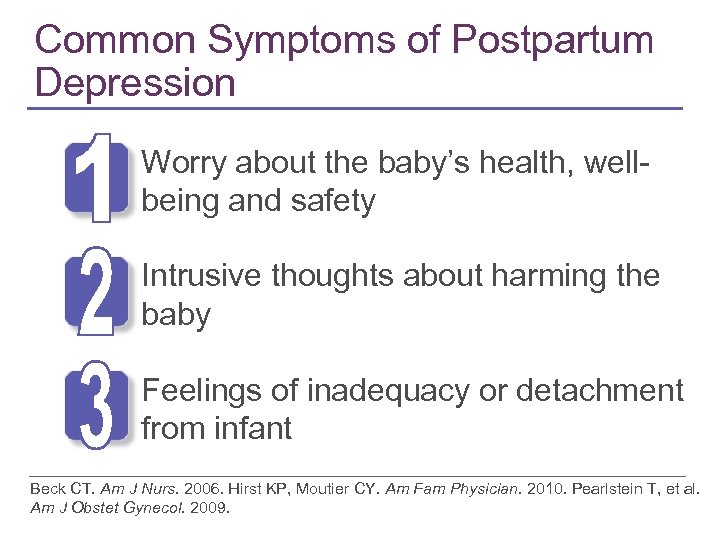 Common Symptoms of Postpartum Depression Worry about the baby’s health, wellbeing and safety Intrusive thoughts about harming the baby Feelings of inadequacy or detachment from infant Beck CT. Am J Nurs. 2006. Hirst KP, Moutier CY. Am Fam Physician. 2010. Pearlstein T, et al. Am J Obstet Gynecol. 2009.
Common Symptoms of Postpartum Depression Worry about the baby’s health, wellbeing and safety Intrusive thoughts about harming the baby Feelings of inadequacy or detachment from infant Beck CT. Am J Nurs. 2006. Hirst KP, Moutier CY. Am Fam Physician. 2010. Pearlstein T, et al. Am J Obstet Gynecol. 2009.
 Postpartum Depression with Atypical Features • Common in young women with depression, Two of the following symptoms: • Hypersomnia • Either increased appetite or weight gain • Leaden paralysis • Interpersonal rejection sensitivity and irritability
Postpartum Depression with Atypical Features • Common in young women with depression, Two of the following symptoms: • Hypersomnia • Either increased appetite or weight gain • Leaden paralysis • Interpersonal rejection sensitivity and irritability
 Comorbidities • Anxiety Disorders • Eating Disorders • Substance related disorders • Personality Disorders: ▪ ▪ ▪ Avoidant Borderline Histrionic
Comorbidities • Anxiety Disorders • Eating Disorders • Substance related disorders • Personality Disorders: ▪ ▪ ▪ Avoidant Borderline Histrionic
 Question 5 ? C. Individual or group psychotherapy can effectively manage mild to moderate depression.
Question 5 ? C. Individual or group psychotherapy can effectively manage mild to moderate depression.
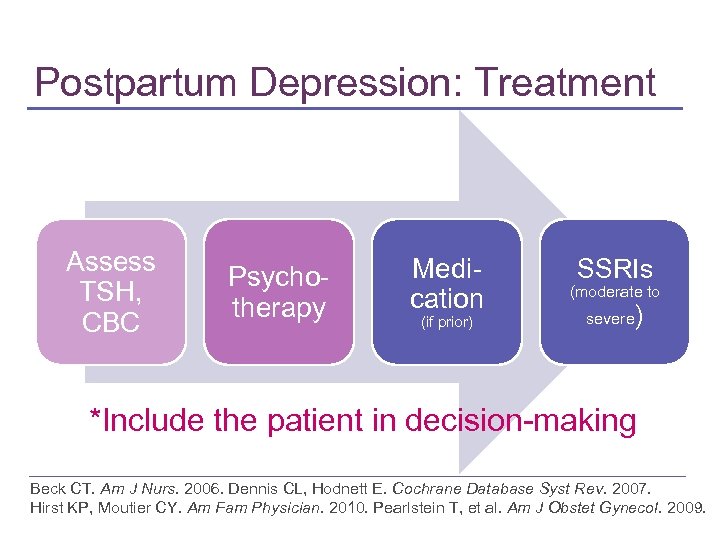 Postpartum Depression: Treatment Assess TSH, CBC Psychotherapy Medication (if prior) SSRIs (moderate to severe ) *Include the patient in decision-making Beck CT. Am J Nurs. 2006. Dennis CL, Hodnett E. Cochrane Database Syst Rev. 2007. Hirst KP, Moutier CY. Am Fam Physician. 2010. Pearlstein T, et al. Am J Obstet Gynecol. 2009.
Postpartum Depression: Treatment Assess TSH, CBC Psychotherapy Medication (if prior) SSRIs (moderate to severe ) *Include the patient in decision-making Beck CT. Am J Nurs. 2006. Dennis CL, Hodnett E. Cochrane Database Syst Rev. 2007. Hirst KP, Moutier CY. Am Fam Physician. 2010. Pearlstein T, et al. Am J Obstet Gynecol. 2009.
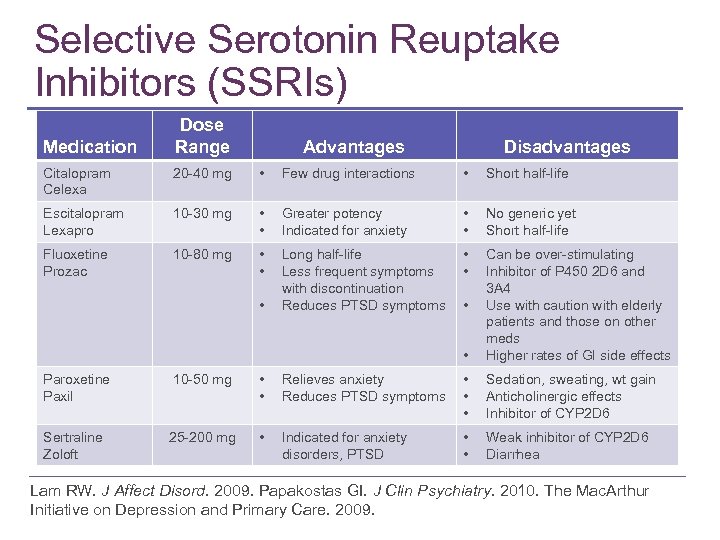 Selective Serotonin Reuptake Inhibitors (SSRIs) Medication Dose Range Advantages Disadvantages Citalopram Celexa 20 -40 mg • Few drug interactions • Short half-life Escitalopram Lexapro 10 -30 mg • • Greater potency Indicated for anxiety • • No generic yet Short half-life Fluoxetine Prozac 10 -80 mg • • Long half-life Less frequent symptoms with discontinuation Reduces PTSD symptoms • • • Can be over-stimulating Inhibitor of P 450 2 D 6 and 3 A 4 Use with caution with elderly patients and those on other meds Higher rates of GI side effects • • Paroxetine Paxil 10 -50 mg • • Relieves anxiety Reduces PTSD symptoms • • • Sedation, sweating, wt gain Anticholinergic effects Inhibitor of CYP 2 D 6 Sertraline Zoloft 25 -200 mg • Indicated for anxiety disorders, PTSD • • Weak inhibitor of CYP 2 D 6 Diarrhea Lam RW. J Affect Disord. 2009. Papakostas GI. J Clin Psychiatry. 2010. The Mac. Arthur Initiative on Depression and Primary Care. 2009.
Selective Serotonin Reuptake Inhibitors (SSRIs) Medication Dose Range Advantages Disadvantages Citalopram Celexa 20 -40 mg • Few drug interactions • Short half-life Escitalopram Lexapro 10 -30 mg • • Greater potency Indicated for anxiety • • No generic yet Short half-life Fluoxetine Prozac 10 -80 mg • • Long half-life Less frequent symptoms with discontinuation Reduces PTSD symptoms • • • Can be over-stimulating Inhibitor of P 450 2 D 6 and 3 A 4 Use with caution with elderly patients and those on other meds Higher rates of GI side effects • • Paroxetine Paxil 10 -50 mg • • Relieves anxiety Reduces PTSD symptoms • • • Sedation, sweating, wt gain Anticholinergic effects Inhibitor of CYP 2 D 6 Sertraline Zoloft 25 -200 mg • Indicated for anxiety disorders, PTSD • • Weak inhibitor of CYP 2 D 6 Diarrhea Lam RW. J Affect Disord. 2009. Papakostas GI. J Clin Psychiatry. 2010. The Mac. Arthur Initiative on Depression and Primary Care. 2009.
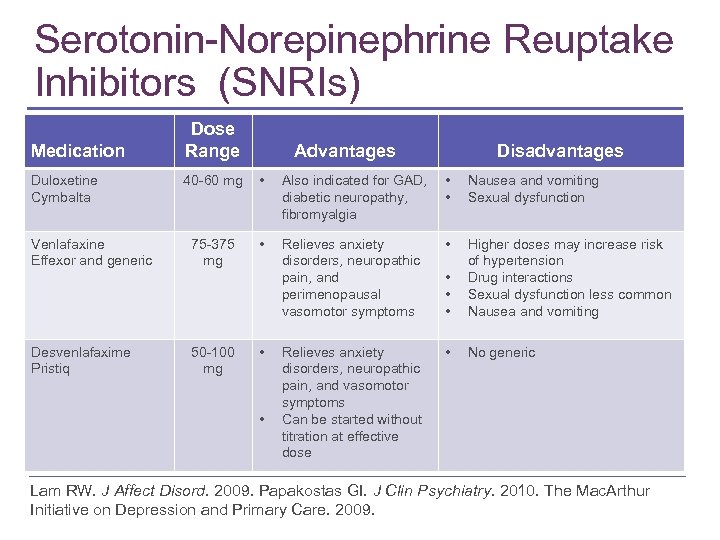 Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) Medication Duloxetine Cymbalta Venlafaxine Effexor and generic Desvenlafaxime Pristiq Dose Range Advantages Disadvantages 40 -60 mg • Also indicated for GAD, diabetic neuropathy, fibromyalgia • • Nausea and vomiting Sexual dysfunction 75 -375 mg • Relieves anxiety disorders, neuropathic pain, and perimenopausal vasomotor symptoms • • Higher doses may increase risk of hypertension Drug interactions Sexual dysfunction less common Nausea and vomiting Relieves anxiety disorders, neuropathic pain, and vasomotor symptoms Can be started without titration at effective dose • No generic 50 -100 mg • • Lam RW. J Affect Disord. 2009. Papakostas GI. J Clin Psychiatry. 2010. The Mac. Arthur Initiative on Depression and Primary Care. 2009.
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) Medication Duloxetine Cymbalta Venlafaxine Effexor and generic Desvenlafaxime Pristiq Dose Range Advantages Disadvantages 40 -60 mg • Also indicated for GAD, diabetic neuropathy, fibromyalgia • • Nausea and vomiting Sexual dysfunction 75 -375 mg • Relieves anxiety disorders, neuropathic pain, and perimenopausal vasomotor symptoms • • Higher doses may increase risk of hypertension Drug interactions Sexual dysfunction less common Nausea and vomiting Relieves anxiety disorders, neuropathic pain, and vasomotor symptoms Can be started without titration at effective dose • No generic 50 -100 mg • • Lam RW. J Affect Disord. 2009. Papakostas GI. J Clin Psychiatry. 2010. The Mac. Arthur Initiative on Depression and Primary Care. 2009.
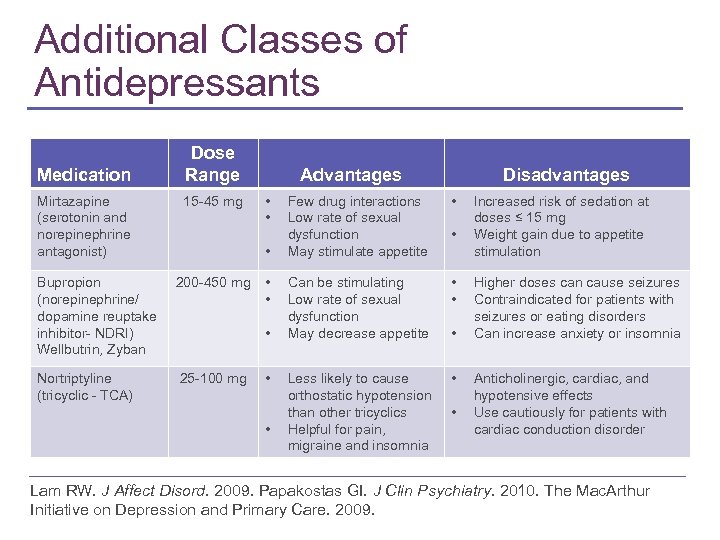 Additional Classes of Antidepressants Medication Mirtazapine (serotonin and norepinephrine antagonist) Dose Range 15 -45 mg Advantages • • • Bupropion (norepinephrine/ dopamine reuptake inhibitor- NDRI) Wellbutrin, Zyban 200 -450 mg Nortriptyline (tricyclic - TCA) 25 -100 mg • • • Disadvantages Few drug interactions Low rate of sexual dysfunction May stimulate appetite • Can be stimulating Low rate of sexual dysfunction May decrease appetite • • Less likely to cause orthostatic hypotension than other tricyclics Helpful for pain, migraine and insomnia • • Increased risk of sedation at doses ≤ 15 mg Weight gain due to appetite stimulation Higher doses can cause seizures Contraindicated for patients with seizures or eating disorders Can increase anxiety or insomnia Anticholinergic, cardiac, and hypotensive effects Use cautiously for patients with cardiac conduction disorder Lam RW. J Affect Disord. 2009. Papakostas GI. J Clin Psychiatry. 2010. The Mac. Arthur Initiative on Depression and Primary Care. 2009.
Additional Classes of Antidepressants Medication Mirtazapine (serotonin and norepinephrine antagonist) Dose Range 15 -45 mg Advantages • • • Bupropion (norepinephrine/ dopamine reuptake inhibitor- NDRI) Wellbutrin, Zyban 200 -450 mg Nortriptyline (tricyclic - TCA) 25 -100 mg • • • Disadvantages Few drug interactions Low rate of sexual dysfunction May stimulate appetite • Can be stimulating Low rate of sexual dysfunction May decrease appetite • • Less likely to cause orthostatic hypotension than other tricyclics Helpful for pain, migraine and insomnia • • Increased risk of sedation at doses ≤ 15 mg Weight gain due to appetite stimulation Higher doses can cause seizures Contraindicated for patients with seizures or eating disorders Can increase anxiety or insomnia Anticholinergic, cardiac, and hypotensive effects Use cautiously for patients with cardiac conduction disorder Lam RW. J Affect Disord. 2009. Papakostas GI. J Clin Psychiatry. 2010. The Mac. Arthur Initiative on Depression and Primary Care. 2009.
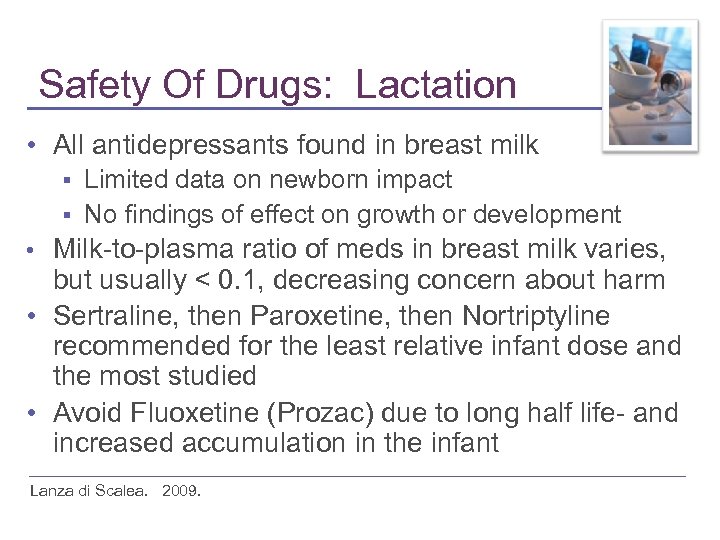 Safety Of Drugs: Lactation • All antidepressants found in breast milk Limited data on newborn impact § No findings of effect on growth or development § Milk-to-plasma ratio of meds in breast milk varies, but usually < 0. 1, decreasing concern about harm • Sertraline, then Paroxetine, then Nortriptyline recommended for the least relative infant dose and the most studied • Avoid Fluoxetine (Prozac) due to long half life- and increased accumulation in the infant • Lanza di Scalea. 2009.
Safety Of Drugs: Lactation • All antidepressants found in breast milk Limited data on newborn impact § No findings of effect on growth or development § Milk-to-plasma ratio of meds in breast milk varies, but usually < 0. 1, decreasing concern about harm • Sertraline, then Paroxetine, then Nortriptyline recommended for the least relative infant dose and the most studied • Avoid Fluoxetine (Prozac) due to long half life- and increased accumulation in the infant • Lanza di Scalea. 2009.
 Safety of SSRIs • May delay developmental milestones • Cost-benefit of SSRIs during pregnancy and postpartum • Glaxo. Smith. Kline paid $2. 5 million to settle lawsuit relating to Paxil (paroxetine) that included birth defects.
Safety of SSRIs • May delay developmental milestones • Cost-benefit of SSRIs during pregnancy and postpartum • Glaxo. Smith. Kline paid $2. 5 million to settle lawsuit relating to Paxil (paroxetine) that included birth defects.
 SSRIs in Treatment • Use of standard dosages • Start with low dosage and check for response ▪ Ex: Zoloft (sertraline) 50 mg • Some women are rapid responders, others 2 to 4 weeks, but full remission may take several months, and dose may need to be increased • May need additional meds for anxiety and sleep
SSRIs in Treatment • Use of standard dosages • Start with low dosage and check for response ▪ Ex: Zoloft (sertraline) 50 mg • Some women are rapid responders, others 2 to 4 weeks, but full remission may take several months, and dose may need to be increased • May need additional meds for anxiety and sleep
 SSRIs in Treatment • Remain on SSRI 6 to 12 months to avoid relapse • Monitoring and tracking with mood diary • Refer for evaluation to mental health provider for complex cases, comorbid conditions, or failure to achieve remission
SSRIs in Treatment • Remain on SSRI 6 to 12 months to avoid relapse • Monitoring and tracking with mood diary • Refer for evaluation to mental health provider for complex cases, comorbid conditions, or failure to achieve remission
 Complementary and Alternative Medicine Therapy for Depression • Commonly used and often not revealed • St. John’s Wort for mild-moderate depression ▪ ▪ ▪ Studies conflicting Drug-drug interactions including hormonal contraception, SSRIs and Coumadin Most guidelines discourage use • Exercise and mindfulness based stress reduction • Light therapy for seasonal affective disorder • No benefit in RCTs ▪ Accupuncture and Omega-3 fatty acids Ravindran AV, et al. J Affect Disord. 2009. Cochrane Review, 2009. Freeman, M P et al. 2010. Complementary and alternative medicine in MDD: APA Task Force Report. J Clin Psy 2010.
Complementary and Alternative Medicine Therapy for Depression • Commonly used and often not revealed • St. John’s Wort for mild-moderate depression ▪ ▪ ▪ Studies conflicting Drug-drug interactions including hormonal contraception, SSRIs and Coumadin Most guidelines discourage use • Exercise and mindfulness based stress reduction • Light therapy for seasonal affective disorder • No benefit in RCTs ▪ Accupuncture and Omega-3 fatty acids Ravindran AV, et al. J Affect Disord. 2009. Cochrane Review, 2009. Freeman, M P et al. 2010. Complementary and alternative medicine in MDD: APA Task Force Report. J Clin Psy 2010.
 Psychotherapy • Psychotherapy is important part of treatment for women who have past history of depression, developmental abuse, marital conflict, lack of support, or comorbid mental health conditions • Cognitive Behavior Therapy (CBT), Interpersonal Therapy (IPT) and Psychodynamic Therapy are all effective and may be cost-effective in improving long term outcomes
Psychotherapy • Psychotherapy is important part of treatment for women who have past history of depression, developmental abuse, marital conflict, lack of support, or comorbid mental health conditions • Cognitive Behavior Therapy (CBT), Interpersonal Therapy (IPT) and Psychodynamic Therapy are all effective and may be cost-effective in improving long term outcomes
 Joan • • 34 yo, 3 weeks postpartum Moody, irritable, exhausted Seems disconnected from her baby Tearful and difficult to focus during the visit Having a hard time caring for the baby and gave up nursing, feels very guilty No local family support, partner works “all the time” Prior history of depression Emergency C-section
Joan • • 34 yo, 3 weeks postpartum Moody, irritable, exhausted Seems disconnected from her baby Tearful and difficult to focus during the visit Having a hard time caring for the baby and gave up nursing, feels very guilty No local family support, partner works “all the time” Prior history of depression Emergency C-section
 Joan • Treatment: ▪ ▪ ▪ Sertraline 50 mg increased to 100 mg Individual psychotherapy Encourage mothers club involvement • Follow Up: ▪ ▪ ▪ Sertraline reduced irritability, stabilized mood Therapy promoted insight Meeting other new moms gave her support and outside of the house activities
Joan • Treatment: ▪ ▪ ▪ Sertraline 50 mg increased to 100 mg Individual psychotherapy Encourage mothers club involvement • Follow Up: ▪ ▪ ▪ Sertraline reduced irritability, stabilized mood Therapy promoted insight Meeting other new moms gave her support and outside of the house activities
 Question 6 ? D. All of the above care consequences of depression during pregnancy which can affect the infant.
Question 6 ? D. All of the above care consequences of depression during pregnancy which can affect the infant.
 Treat Prophylactically for Additional Pregnancies • Increased likelihood of PPD after first episode of depression • Case example: ▪ ▪ ▪ first pregnancy, possible “baby blues”; second pregnancy, psychotic depression, hallucinated; third pregnancy covered with Zoloft prior to delivery
Treat Prophylactically for Additional Pregnancies • Increased likelihood of PPD after first episode of depression • Case example: ▪ ▪ ▪ first pregnancy, possible “baby blues”; second pregnancy, psychotic depression, hallucinated; third pregnancy covered with Zoloft prior to delivery
 Hormones and CNS • Effect of estrogen and progesterone on affective states are probably not linear or dose-dependent • Estrogen and progesterone modulate each others effects on CNS and that complicates understanding of their individual effects
Hormones and CNS • Effect of estrogen and progesterone on affective states are probably not linear or dose-dependent • Estrogen and progesterone modulate each others effects on CNS and that complicates understanding of their individual effects
 Hormones and the Gender Difference • Gender difference emerges at puberty • Some women more vulnerable, sensitive to estrogen precipitous change from birth to 48 hours • Women more likely than men to become depressed in response to stressful events • Sleep deprivation with motherhood may play a role • Need for further studies of treatment with transdermal estradiol in treatment of PPD
Hormones and the Gender Difference • Gender difference emerges at puberty • Some women more vulnerable, sensitive to estrogen precipitous change from birth to 48 hours • Women more likely than men to become depressed in response to stressful events • Sleep deprivation with motherhood may play a role • Need for further studies of treatment with transdermal estradiol in treatment of PPD
 Neuroimaging Studies of Women with PPD • Dorsomedial prefrontal cortex less active in women with PPD than healthy new mothers • DMPFC involved in voluntary and automatic control and reappraisal of emotional responses in social cognition (interpret emotional responses of others) • Diminished HPA Axis drive DMPC connectivity with amygdala Am J Psych, Sept. 2010
Neuroimaging Studies of Women with PPD • Dorsomedial prefrontal cortex less active in women with PPD than healthy new mothers • DMPFC involved in voluntary and automatic control and reappraisal of emotional responses in social cognition (interpret emotional responses of others) • Diminished HPA Axis drive DMPC connectivity with amygdala Am J Psych, Sept. 2010
 “SHAPED BY LIFE IN THE WOMB”
“SHAPED BY LIFE IN THE WOMB”
 Comment on Perinatal Depression • Babies with mothers with untreated depression (Perinatal) show neurobehavioral changes, born at earlier gestational age, and have elevated stress hormones • Epigenetic changes and neurobiological models of emotion-behavior regulation are implicated; attention regulation capacities that call on brain stem and limbic system networks
Comment on Perinatal Depression • Babies with mothers with untreated depression (Perinatal) show neurobehavioral changes, born at earlier gestational age, and have elevated stress hormones • Epigenetic changes and neurobiological models of emotion-behavior regulation are implicated; attention regulation capacities that call on brain stem and limbic system networks
 Improved Outcome with Integrated Care • Integrating primary care with mental health services has shown to improve overall medical care and reduces costs • Collaborate with Certified Nurse Midwives and others who refer patients with depression and other mental health diagnoses • Screen using the Patient Health Questionnaire (PHQ-9)
Improved Outcome with Integrated Care • Integrating primary care with mental health services has shown to improve overall medical care and reduces costs • Collaborate with Certified Nurse Midwives and others who refer patients with depression and other mental health diagnoses • Screen using the Patient Health Questionnaire (PHQ-9)
 Provider Resources • Mac. Arthur Initiative on Depression in Primary Care ▪ http: //www. depression-primarycare. org/ • American Psychiatric Association ▪ http: //www. healthyminds. org/ • Cox, J. L. , Holden, J. M. , and Sagovsky, R. 1987. Detection of postnatal depression: Development of the 10 -item Edinburgh Postnatal Depression Scale.
Provider Resources • Mac. Arthur Initiative on Depression in Primary Care ▪ http: //www. depression-primarycare. org/ • American Psychiatric Association ▪ http: //www. healthyminds. org/ • Cox, J. L. , Holden, J. M. , and Sagovsky, R. 1987. Detection of postnatal depression: Development of the 10 -item Edinburgh Postnatal Depression Scale.
 Provider and Patient Resources • National Institute of Mental Health ▪ http: //www. nimh. nih. gov/health/publications/wome n-and-depression-discovering-hope/index. shtml • Womens. Health. gov • http: //www. womenshealth. gov/faq/depressionpregnancy. cfm • Mayo Clinic • http: //www. mayoclinic. com/health/depression/MH 00035
Provider and Patient Resources • National Institute of Mental Health ▪ http: //www. nimh. nih. gov/health/publications/wome n-and-depression-discovering-hope/index. shtml • Womens. Health. gov • http: //www. womenshealth. gov/faq/depressionpregnancy. cfm • Mayo Clinic • http: //www. mayoclinic. com/health/depression/MH 00035
 Provider and Patient Resources • Healthy Place ▪ http: //www. healthyplace. com/depression/women/d epression-in-women/menu-id-68/. • Massachusetts General Hospital Center for Women’s Mental Health ▪ http: //www. womensmentalhealth. org/.
Provider and Patient Resources • Healthy Place ▪ http: //www. healthyplace. com/depression/women/d epression-in-women/menu-id-68/. • Massachusetts General Hospital Center for Women’s Mental Health ▪ http: //www. womensmentalhealth. org/.


