The pulmonary database2.pptx
- Количество слайдов: 65
The pulmonary database Dr. A. Solomonov. Pulmonology
Respiratory symptoms 1 o Dyspnea • Acute (over a period of hours to days) An acute attack of asthma Acute pulmonary edema Bacterial pneumonia A pneumothorax A pulmonary embolus Dr. A. Solomonov. Pulmonology
Respiratory symptoms 2 o A subacute dyspnea (over days to weeks) • Exacerbation of preexisting airways disease (asthma or chronic bronchitis) • Infection or a noninfectious inflammatory process (PCP, mycobacterial or fungal pneumonia, eosinophilic or organizing pneumonia and others) • Neuromuscular disease (Guillain-Barre syndrome, myasthenia gravis) • Pleural effusion • Chronic cardiac disease (congestive heart failure) Dr. A. Solomonov. Pulmonology
Respiratory symptoms 3 o A chronic dyspnea (over months to years) • Chronic obstructive lung disease • Chronic interstitial lung disease • Chronic cardiac disease o Cough and sputum production • Suggeststs airway disease as asthma, chronic bronchitis, or bronchiectasis Dr. A. Solomonov. Pulmonology
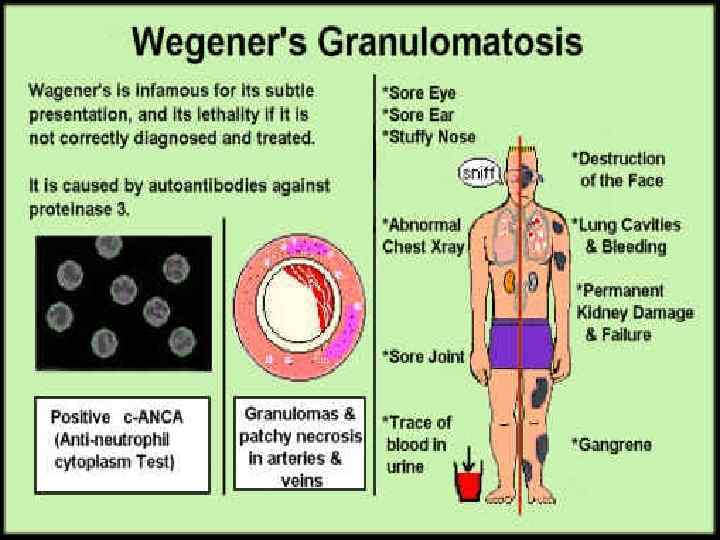
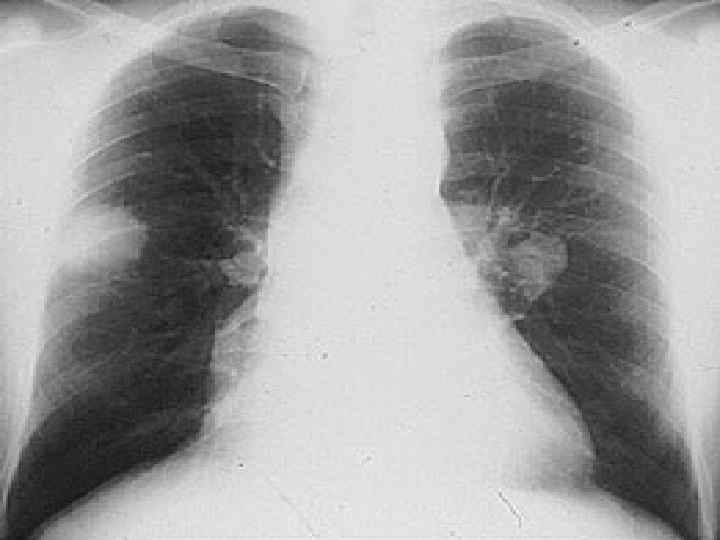
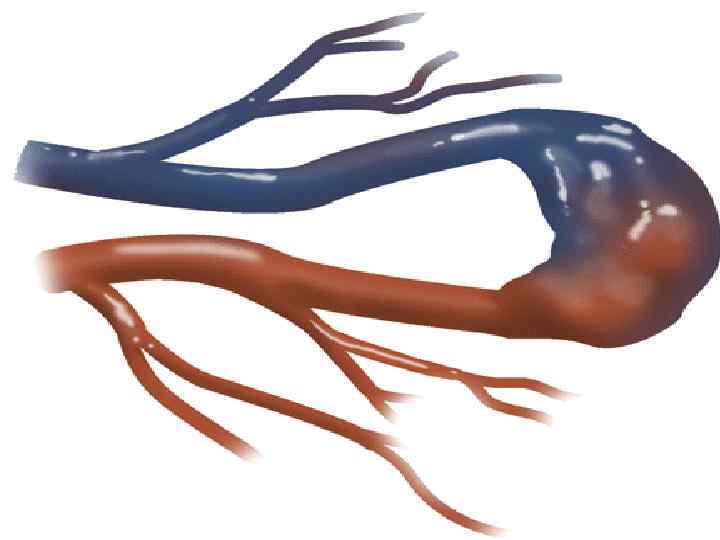
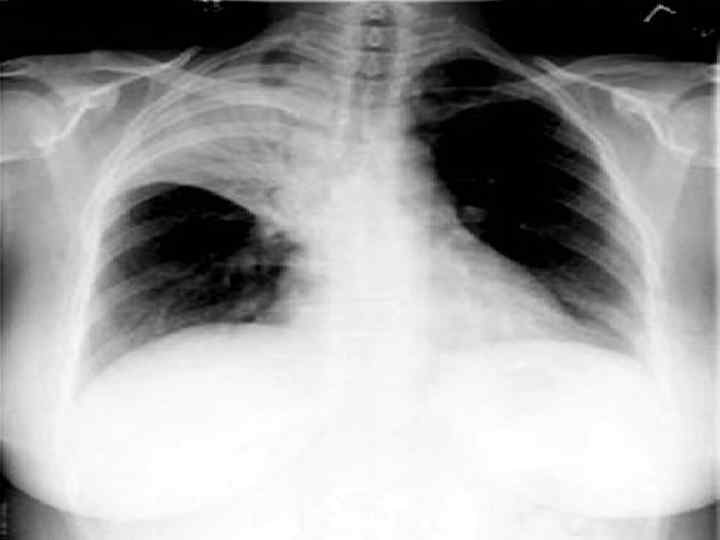
Hemoptysis o o o Massive hemoptysis - >100 ml/24 h The most common site of bleeding is the airwais • Acute or chronic bronchitis & bronchiectasis • Bronchogenic carcinoma Blood originating from the parenchyma • From a localized source (lung abscess, tuberculosis) • From a diffuse diseases (an autoimmune process such as Goodpasture’s syndrome, Wegener’s granulomatosis or lupus) Dr. A. Solomonov. Pulmonology

Dr. A. Solomonov. Pulmonology

Dr. A. Solomonov. Pulmonology
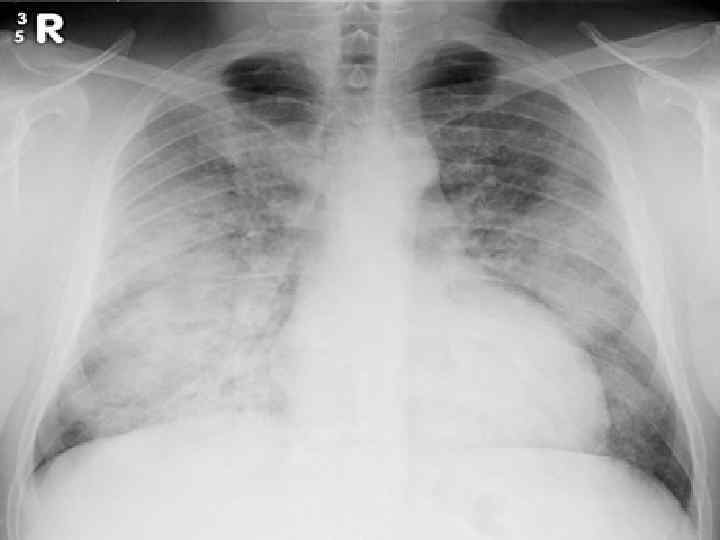
Goodpasture syndrom o o o Genetical predisposition Typically affected young male smokers Progressive glomerulonephritis & renal failure Diffuse pulmonary hemorrhage Anti-GBM antibody – against type IV collagen Treatment: plasmaphersis, steroids & cytotoxic agents Dr. A. Solomonov. Pulmonology
Dr. A. Solomonov. Pulmonology
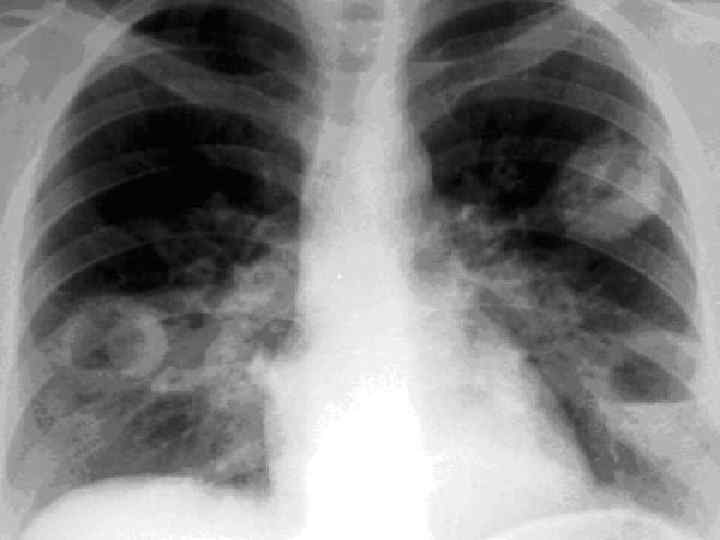
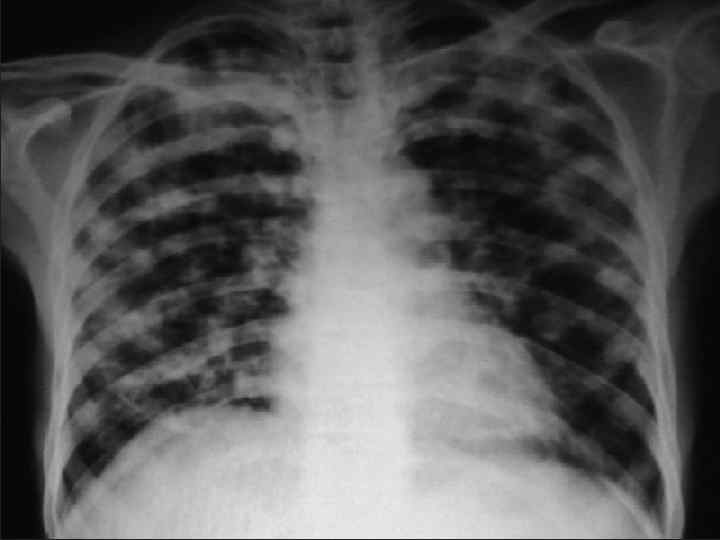
Wegener granulomatosis o Gramulomatous inflammation and vasculitis of: • Upper airways (rinitis, ulceration, perforation of septum, nose deformity, sinusitis, otitis media) • Lung: large, multiple nodules and often cavitated • Glomerulonephritis • Same times a disseminated vasculitis • Anticytoplasmic antibody – c-ANCA • Treatment: cyclophosphamide and prednisone Dr. A. Solomonov. Pulmonology
Dr. A. Solomonov. Pulmonology
Dr. A. Solomonov. Pulmonology
Dr. A. Solomonov. Pulmonology
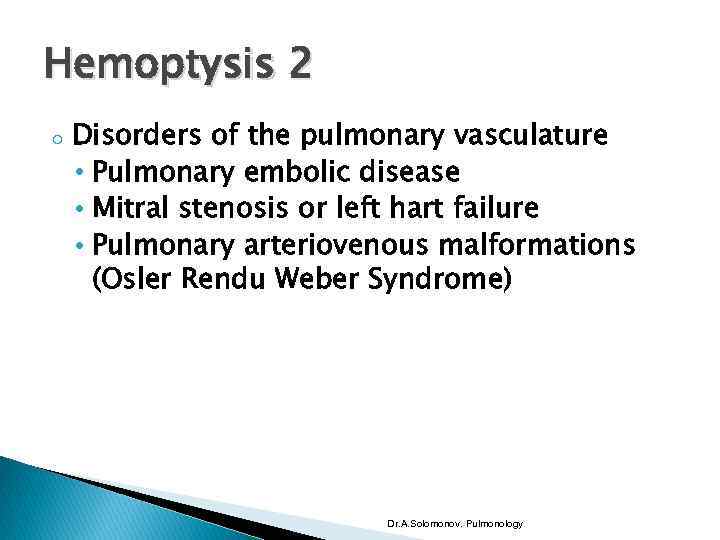
Hemoptysis 2 o Disorders of the pulmonary vasculature • Pulmonary embolic disease • Mitral stenosis or left hart failure • Pulmonary arteriovenous malformations (Osler Rendu Weber Syndrome) Dr. A. Solomonov. Pulmonology
Dr. A. Solomonov. Pulmonology

Dr. A. Solomonov. Pulmonology

Dr. A. Solomonov. Pulmonology
Respiratory symptoms 4 o o Chest pain from involvement of the parietal pleura • Pleural neoplasm or inflammatory disorders • Pneumonia or pulmonary infartion hoarseness (tumor involvement o the left recurrent laryngeal nerve) Dr. A. Solomonov. Pulmonology
History 1 o o Cigarette smoking • Chronic obstructive lung disease – COPD and lung cancer are the two most important respiratory complications of smoking Occupational exposures o Inorganic dust : Silica, silicates (asbestos, talc), hard metal, beryllium. o Organic dust : Thermophilic bacteria (e. g. farmer’s lung); animal proteins (e. g. bird fancier’s lung). Dr. A. Solomonov. Pulmonology
History 2 o A history of coexisting systemic disease • Systemic rheumatic diseases associated with pleural or parenchymal lung disease • Metastatic neoplastic disease in the lung • Hematologic malignancies Dr. A. Solomonov. Pulmonology
Pulmonary complication of connective tissue diseases 1 o Rheumatoid arthritis – is common in women, but lung complicationmore frequntly in men • Pleural affusion: small & unilateral exudate • Very low glucose < 15 mg/dl • Low compliment • High titer of RF • Pulmonary fibrosis – basal distribution • Organizing pneumonia • Pulmonary nodules & silicosis (Caplan syndrome) • Obliterative bronchiolitis Dr. A. Solomonov. Pulmonology
Pulmonary complication of connective tissue diseases 2 o Systemic lupus erythematosus (SLE) • Pleural effusions – small and bilateral in 50% of cases • High titer of ANF & LE cells • Pulmonary fibrosis • Organising pneumonia • Pulmonary hypertension as result of venous thromboses (lupus anticoagulant) • Pulmonary infection • Pulmonary haemorrhage Dr. A. Solomonov. Pulmonology
Pulmonary complication of connective tissue diseases 3 o o Systemic sclerosis • Pulmonary fibrosis (nearly in all patients) • Pulmonary arterial hypertension Intimal proliferation of small blood vessels • Aspiration pneumonia Dermatomyositis • Pulmonary fibrosis • Respiratory muscle weakness Dr. A. Solomonov. Pulmonology
History 2 o o Risk factors for AIDS Previous treatment • Chemotherapy, radiation therapy, or treatment with amiodarone can cause interstitial lung disease • Beta-blocking agents causing airflow obstruction • Angiotensin converting enzyme inhibitors causing cough Dr. A. Solomonov. Pulmonology
History 3 o Family history of diseases that have a genetic component • Cystic fibrosis • A 1 – antitrypsin deficiency • asthma Dr. A. Solomonov. Pulmonology
Physical examination 1 o o Inspection • Rate and pattern of breathing • Asymmetric expansion of the chest and/or deviation of the trachea Endobronchial obstruction of a large airway Unilateral parenchymal or pleural disease (pneumothorax) Unilateral phrenic nerve paralysis Kyphoscoliosis and ankylosing spondilitis Dr. A. Solomonov. Pulmonology
Physical examination 2 o o Palpation • Fremitus is decreased or absent in pleural effusion or in endobronchial obstruction • Fremitus is increased over an area of underlying pulmonary consolidation Percussion • Dullness – over the consolidated lung or a pleural effusion • Hyperresonant – over the air in the pleural space Dr. A. Solomonov. Pulmonology
Auscultation o o o Vesicular breath sounds, in which inspiration is louder and longer than expiration Breath sounds are weaker or absent • Endobronchial obstruction • Liquid in the pleural space Bronchial breath sounds • Over the consolidated lung (a more pronounced expiratory phase) Dr. A. Solomonov. Pulmonology
Abnormal breath sounds o o o Crackles (rales) • Interstitial lung disease or filling of alveoli by liquid Wheezes (airflow limitation as bronchospasm) Rhonchiis – a low-pitched vibratory sounds created when there is free liquid in the airway lumen Pleural friction rubs Stridor – occurs primarily during inspiration represent flow through a narrowed upper airway Dr. A. Solomonov. Pulmonology
General physical examination 1 o o Enlarged lymph nodes Disturbances of mentation in acute carbone dioxide retention and hypoxemia Infected teeth and gums predispose to aspiration pneumonitis and lung abscess Clubbing of digits can be found in: • Lung cancer • Interstitial lung disease • Chronic infections in the thorax, such as bronchiectasis, lung abscess and empyema Dr. A. Solomonov. Pulmonology
General physical examination 2 o o A systemic diseases may be associated with pulmonary complications such as systemic lupus erythematosus, scleroderma and rheumatoid arthritis Sarcoidosis can have findings on physical examination • Ocular findings (uveitis, conjunctival granulomas) • Skin findings (erythema nodosum, cutaneous granulomas) Dr. A. Solomonov. Pulmonology
Imaging 1 o o o Chest radiography is normal in 10% of patients with parenchymal lung diseases Infiltrates • Alveolar • Interstitial • Nodular pattern Increased radiolucency • Localized (cyst or bulla) • Generalized (emphysema) Dr. A. Solomonov. Pulmonology
Dr. A. Solomonov. Pulmonology

Dr. A. Solomonov. Pulmonology

Dr. A. Solomonov. Pulmonology
Dr. A. Solomonov. Pulmonology
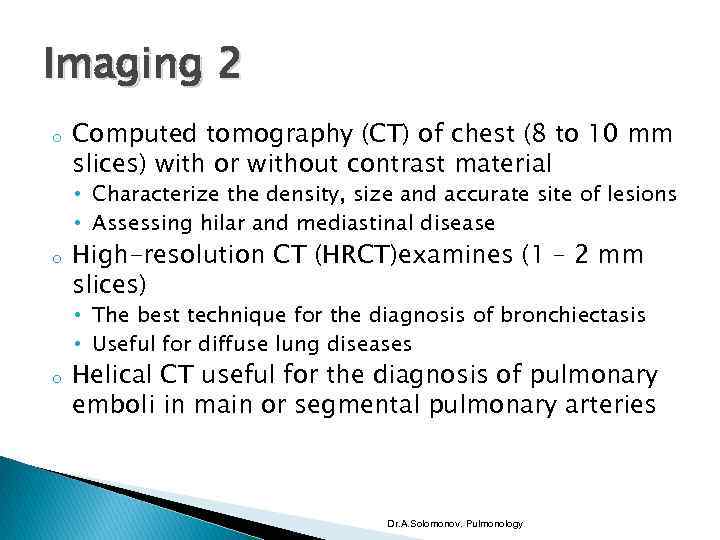
Imaging 2 o Computed tomography (CT) of chest (8 to 10 mm slices) with or without contrast material • Characterize the density, size and accurate site of lesions • Assessing hilar and mediastinal disease o High-resolution CT (HRCT)examines (1 – 2 mm slices) • The best technique for the diagnosis of bronchiectasis • Useful for diffuse lung diseases o Helical CT useful for the diagnosis of pulmonary emboli in main or segmental pulmonary arteries Dr. A. Solomonov. Pulmonology
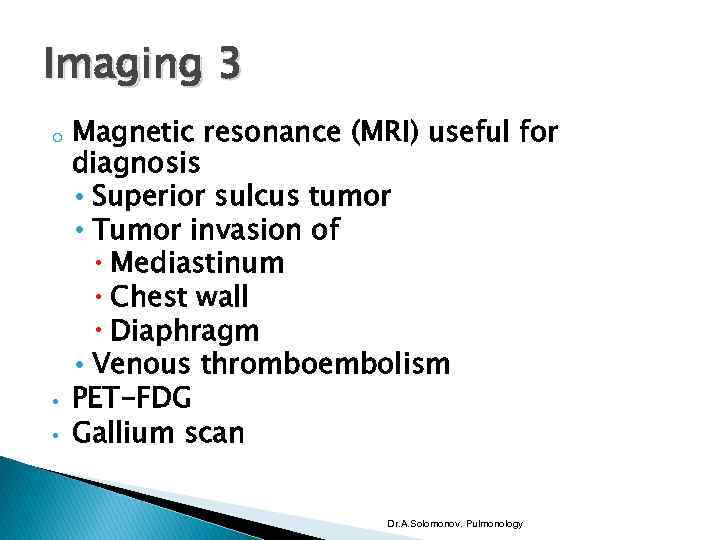
Imaging 3 o • • Magnetic resonance (MRI) useful for diagnosis • Superior sulcus tumor • Tumor invasion of Mediastinum Chest wall Diaphragm • Venous thromboembolism PET-FDG Gallium scan Dr. A. Solomonov. Pulmonology
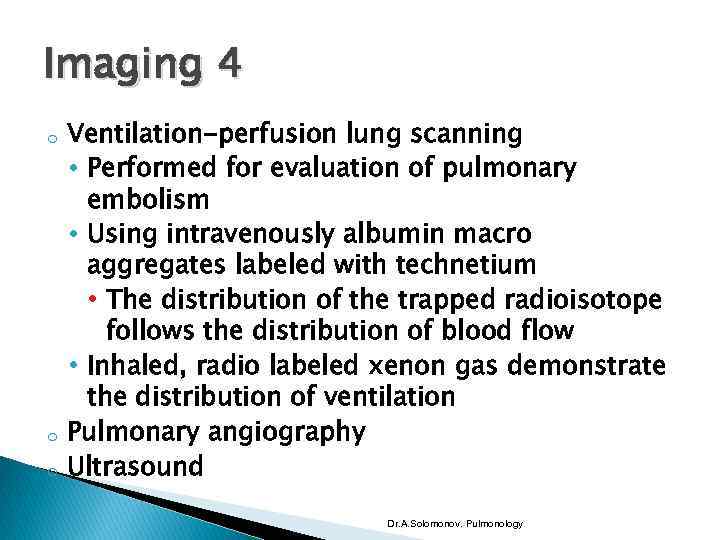
Imaging 4 o o o Ventilation-perfusion lung scanning • Performed for evaluation of pulmonary embolism • Using intravenously albumin macro aggregates labeled with technetium • The distribution of the trapped radioisotope follows the distribution of blood flow • Inhaled, radio labeled xenon gas demonstrate the distribution of ventilation Pulmonary angiography Ultrasound Dr. A. Solomonov. Pulmonology
Physiologic features o o The primary functions of the respiratory system • To remove CO 2 to blood • Provide adequate O 2 to blood For these functions, there must be adequate • Ventilation • Circulation of blood through the pulmonary vasculature (perfusion) • Movement of gas between alveoli and pulmonary capillaries (diffusion) • Contact between alveolar gas and pulmonary capillary blood (ventilation-perfusion matching) Dr. A. Solomonov. Pulmonology
Disturbance of respiratory function o o o Disturbances in ventilatory function • Restrictive pattern (decrease in lung volumes) • Obstructive pattern (decrease in expiratory flow rates) Dissturbances in gas exchsnge Disorders relating to CNS of ventilation Dr. A. Solomonov. Pulmonology
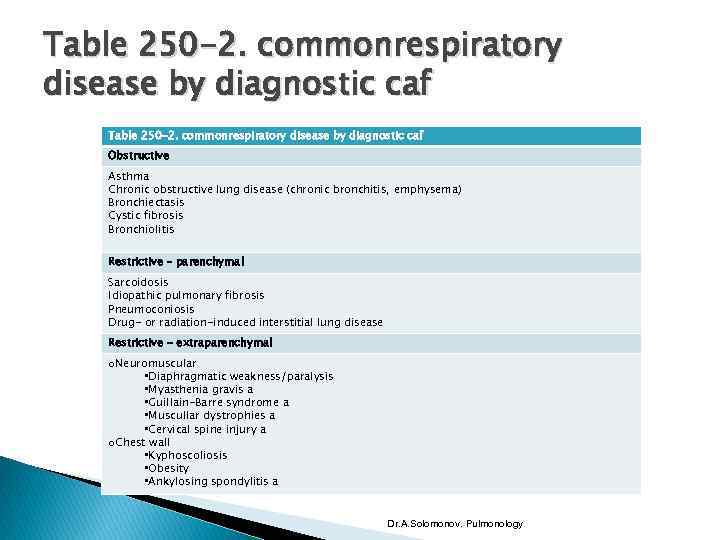
Table 250 -2. commonrespiratory disease by diagnostic caf Obstructive Asthma Chronic obstructive lung disease (chronic bronchitis, emphysema) Bronchiectasis Cystic fibrosis Bronchiolitis Restrictive – parenchymal Sarcoidosis Idiopathic pulmonary fibrosis Pneumoconiosis Drug- or radiation-induced interstitial lung disease Restrictive - extraparenchymal o. Neuromuscular • Diaphragmatic weakness/paralysis • Myasthenia gravis a • Guillain-Barre syndrome a • Muscullar dystrophies a • Cervical spine injury a o. Chest wall • Kyphoscoliosis • Obesity • Ankylosing spondylitis a Dr. A. Solomonov. Pulmonology
Disturbances in the pulmonary circulation o o Output of the rught ventricle is 5 l/min & mean pulmonary artery pressure is 15 mm. Hg in a normal adult rest • Can be measured via pulmonary arterial Swan-Ganz catheter Mean pulmonary arterial pressure remain stable, even with a three to fourfold increase in cardiac output Dr. A. Solomonov. Pulmonology
Pulmonary hypertension o o Alveolar hypoxia is a very potent stimulus for pulmonary vasoconstriction • Chronic obstructive lung disease (COPD) interstitial lung disease (ILD), chest wall disease, and the obesity hypoventilationsleep apnea syndrome (SAS) Diseases affecting the pulmonary vessels • Recurrent pulmonary emboli • Primary pulmonary hypertension or scleroderma Dr. A. Solomonov. Pulmonology
Primary Pulmonary hypertension o o o Rare Death from right heart failure (2 -3 years without treatment) Association with diet pills Familial in 6% of cases (autosomal dominant) 2 female: 1 male Dr. A. Solomonov. Pulmonology
Pulmonary hypertension o Mean PAP • At rest • Exercise > 20 – 25 mm. Hg > 30 mm. Hg Dr. A. Solomonov. Pulmonology
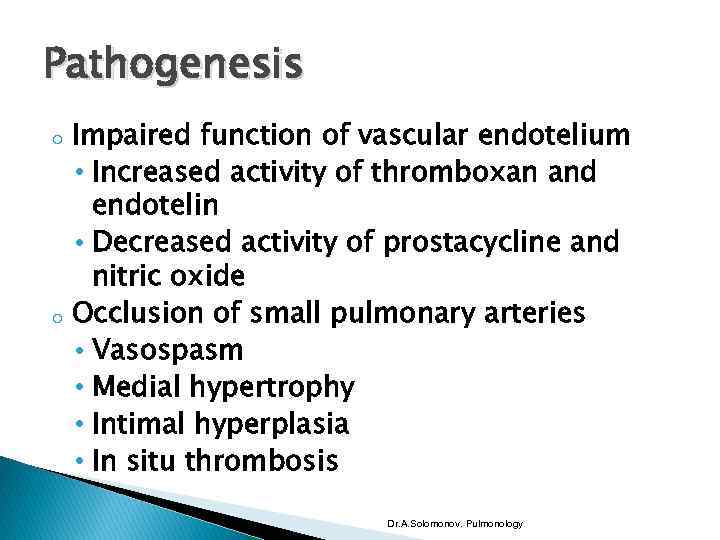
Pathogenesis o o Impaired function of vascular endotelium • Increased activity of thromboxan and endotelin • Decreased activity of prostacycline and nitric oxide Occlusion of small pulmonary arteries • Vasospasm • Medial hypertrophy • Intimal hyperplasia • In situ thrombosis Dr. A. Solomonov. Pulmonology
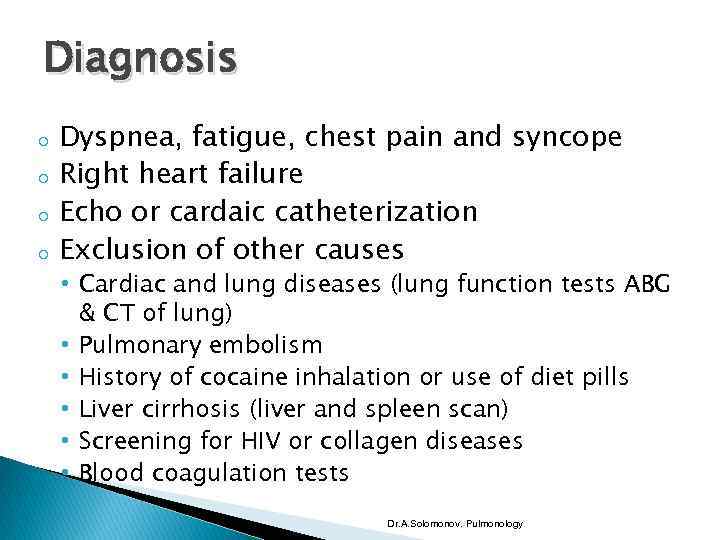
Diagnosis o o Dyspnea, fatigue, chest pain and syncope Right heart failure Echo or cardaic catheterization Exclusion of other causes • Cardiac and lung diseases (lung function tests ABG & CT of lung) • Pulmonary embolism • History of cocaine inhalation or use of diet pills • Liver cirrhosis (liver and spleen scan) • Screening for HIV or collagen diseases • Blood coagulation tests Dr. A. Solomonov. Pulmonology
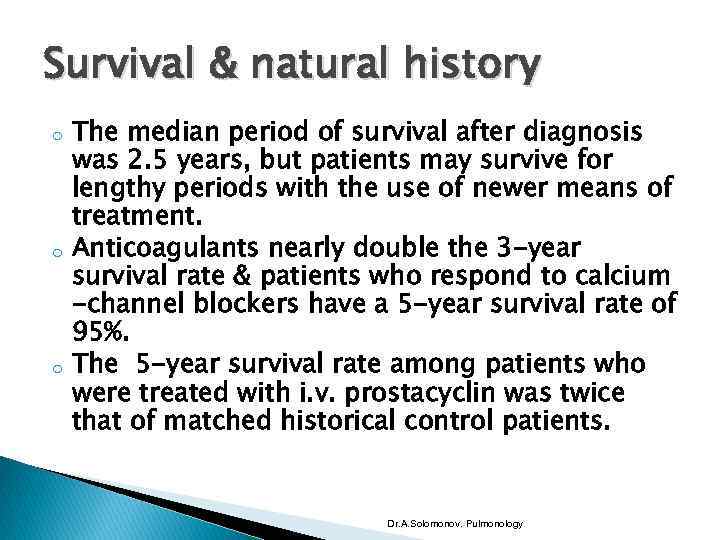
Survival & natural history o o o The median period of survival after diagnosis was 2. 5 years, but patients may survive for lengthy periods with the use of newer means of treatment. Anticoagulants nearly double the 3 -year survival rate & patients who respond to calcium -channel blockers have a 5 -year survival rate of 95%. The 5 -year survival rate among patients who were treated with i. v. prostacyclin was twice that of matched historical control patients. Dr. A. Solomonov. Pulmonology
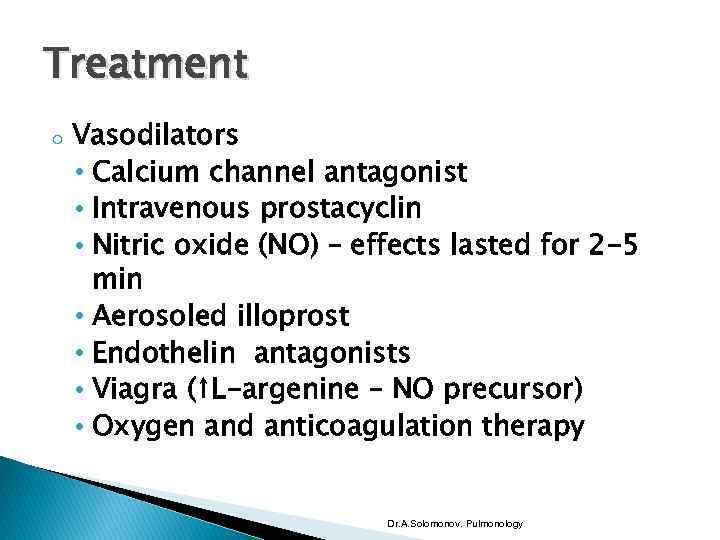
Treatment o Vasodilators • Calcium channel antagonist • Intravenous prostacyclin • Nitric oxide (NO) – effects lasted for 2 -5 min • Aerosoled illoprost • Endothelin antagonists • Viagra (↑L-argenine – NO precursor) • Oxygen and anticoagulation therapy Dr. A. Solomonov. Pulmonology
Arterial blood gases o o o Pao 2 – partial pressures of O 2 in arterial blood Paco 2 – partial pressures of CO 2 on arterial blood Oxygenated Hg is the primary form in which O 2 is transported in blood The small amount of O 2 is dissolved in plasma The normal Pao 2 in arterial blood is 100 mm. Hg and O 2 saturation is about 97, 5% The Po 2 in venous blood is 40 mm. Hg and O 2 saturation is about 75% Dr. A. Solomonov. Pulmonology
Additional diagnostic evaluation o o Pulse oximetry continuously measure O 2 saturation – not measure Pa. CO 2 Misleading results in the presence of • Increased level of carboxyhemoglobin • Increased level of methemoglobin • Hyperbilirubinemia • Dark skin pigmentation • Fingernail polish • Poor perfusion Dr. A. Solomonov. Pulmonology
Dr. A. Solomonov. Pulmonology
Normal acid – base homeostasis 1 o o o The normal Paco 2 in arterial blood is 40 mm. Hg The normal Pco 2 in venous blood is 46 mm. Hg The Paco 2 controlled by the central nervous system and respiratory systems Underexcretion of CO 2 produced hypercapnia (usually the result of hypoventilation) Overexcretion causes hypocapnia Primary changes in Paco 2 can cause respiratory acidosis (Paco 2 > 40 mm. Hg)or alkalosis (PAco 2 < 40 mm. Hg) Dr. A. Solomonov. Pulmonology
Normal acid – base homeostasis 2 o o o The normal plasma bicarbonate [ HCO 3 ⁻] is 24 m. Eq/l Regulated by the kidneys through • “reabsorption” of filtered HCO 3 ⁻ • Excretion of NH 4 ⁺ in the urine A primary change in the plasma [HCO 3 ⁻] can cause metabolic acidosis or alkalosis • Results in compensatory changes in ventilation that blunt the changes in blood p. H Dr. A. Solomonov. Pulmonology
Normal acid – base homeostasis 3 o o o The normal arterial p. H is maintained between 7. 35 and 7. 45 The p. H regulated by respiratory (Paco 2) and renal [HCO 3 ⁻] mechanisms CO 2+H 2 O ↔ H 2 CO 3 ↔ H⁺ + HCO 3⁻ Dr. A. Solomonov. Pulmonology
General types of acid – base disorders o o o Simple acid-base disorders • Metabolic acidosis or alkalosis • Respiratory acidosis or alkalosis Since compensation is not complete, the p. H is abnormal in simple disturbances Mixed acid-base disturbances Dr. A. Solomonov. Pulmonology
Metabolic acidosis o o o “metabolic” means a primery changes in HCO 3⁻ Can occur because of • An increase in endogenouse acid production (such as lactate and ketoacids) • Loss of bicarbonate (as in diarrhea) • Accumulation of endogenous acid (as in renal failure) p. H is low base excess negative Ventilation is increases that lowers the Pco 2 The Paco 2 ↓ 1. 25 mm. Hg for each 1 mmol/L ↓ in HCO 3⁻ Dr. A. Solomonov. Pulmonology
Metabolic alkalosis o o It is manifested by: • An increase in the serum [HCO 3⁻] • An elevated arterial p. H • An increase in Paco 2 as a result of compensatory alveolar hypoventilation It is often accompanied by hypochloremia and hypokalemia The Paco 2 increases 6 mm. Hg for each 10 mmol/L increase in the [HCO 3⁻] above normal Base excess is increased Dr. A. Solomonov. Pulmonology
Respiratory acidosis 1 o o o Caused by an increase in Pco 2 • Chronic obstructive pulmonary disease • A sedative drug overdose • Respiratory muscle fatigue p. H is low (acidemia) Increase in bicarbonate (compensation) • In acute acidosis – HCO 3⁻ - increases 1 mmol/L for every 10 mm. Hg increase in Paco 2 Dr. A. Solomonov. Pulmonology
Respiratory acidosis 2 o o o • In chronic acidosis (> 24 h), renal adaptation occurs and the HCO 3 – increases by 4 mmol/L for every 10 mm. Hg increase in Paco 2 • The serum HCO 3 – usually does not increase above 38 mmol/L p. H does not fully return to its normal level of 7. 4 A rapid increase in Paco 2 may cause anxiety, dyspnea, confusion and coma Chronic hypercapnia results in loss of memory, daytime somnolence and headaches (due to raised intracranial pressure) Dr. A. Solomonov. Pulmonology
Respiratory alkalosis 1 o o o Alveolar hyperventilation decreases Paco 2 and increase p. H (alkalemia) It is important to rule out pulmonary embolism Bicarbonate is low (it is unusual to observe a plasma HCO 3⁻ < 12 mmol/L) • In acute alkalosis cellular buffers consuming HCO 3⁻ • In chronic hypocapnia (> 2 -6 h) renal compensation is develop→ increased HCO 3⁻ excretion (10 mm. Hg fall in Paco 2 causes 5 mmol/L drop in HCO 3⁻) Dr. A. Solomonov. Pulmonology
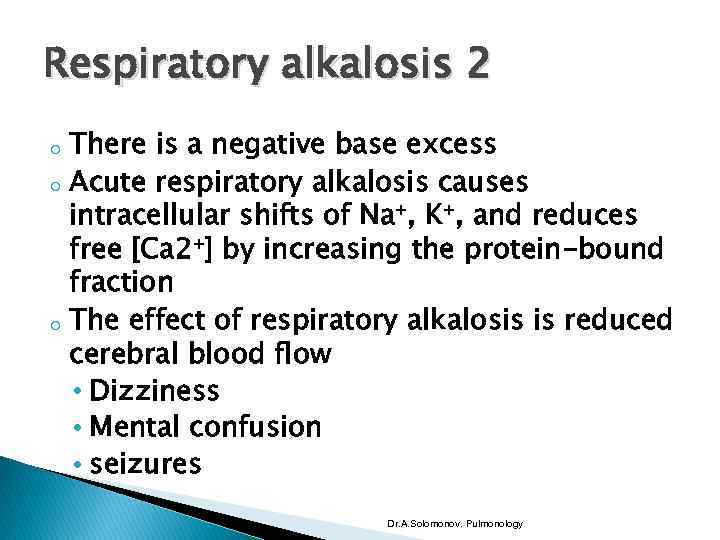
Respiratory alkalosis 2 o o o There is a negative base excess Acute respiratory alkalosis causes intracellular shifts of Na⁺, K⁺, and reduces free [Ca 2⁺] by increasing the protein-bound fraction The effect of respiratory alkalosis is reduced cerebral blood flow • Dizziness • Mental confusion • seizures Dr. A. Solomonov. Pulmonology
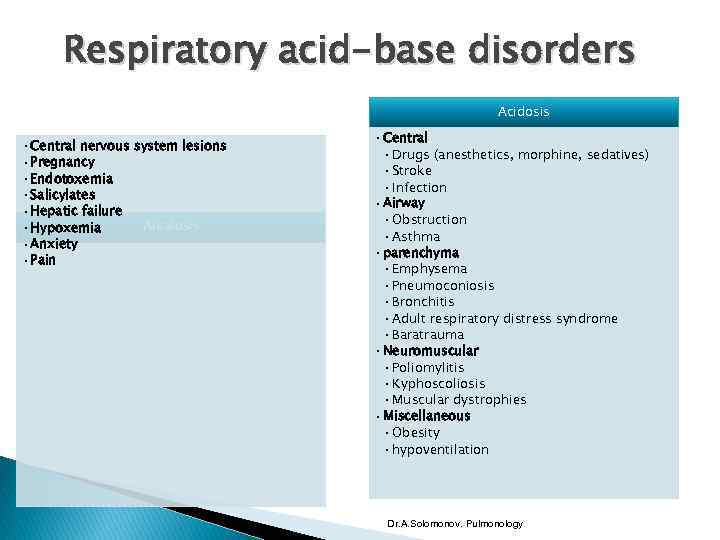
Respiratory acid-base disorders Acidosis • Central nervous system lesions • Pregnancy • Endotoxemia • Salicylates • Hepatic failure Alkalosis • Hypoxemia • Anxiety • Pain • Central • Drugs (anesthetics, morphine, sedatives) • Stroke • Infection • Airway • Obstruction • Asthma • parenchyma • Emphysema • Pneumoconiosis • Bronchitis • Adult respiratory distress syndrome • Baratrauma • Neuromuscular • Poliomylitis • Kyphoscoliosis • Muscular dystrophies • Miscellaneous • Obesity • hypoventilation Dr. A. Solomonov. Pulmonology
Dr. A. Solomonov. Pulmonology
The pulmonary database2.pptx