0ab0e256d176608b6e040dd870c73eb3.ppt
- Количество слайдов: 64
The Prevention Collaborative: An Overview Ronda L. Cochran, MPH Division of Healthcare Quality Promotion
Background: The Admiral Stockdale Dilemma “Who am I and why am I here? ” 2
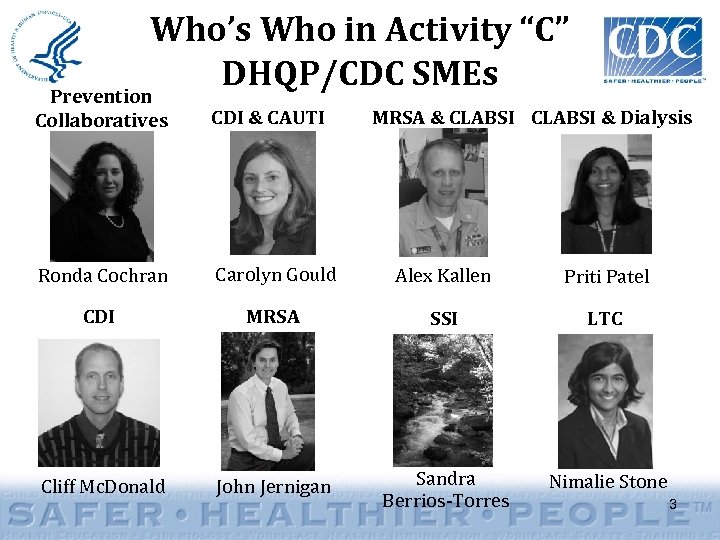
Who’s Who in Activity “C” DHQP/CDC SMEs Prevention Collaboratives CDI & CAUTI Ronda Cochran Carolyn Gould Alex Kallen Priti Patel CDI MRSA SSI LTC Cliff Mc. Donald John Jernigan Sandra Berrios-Torres Nimalie Stone MRSA & CLABSI & Dialysis 3
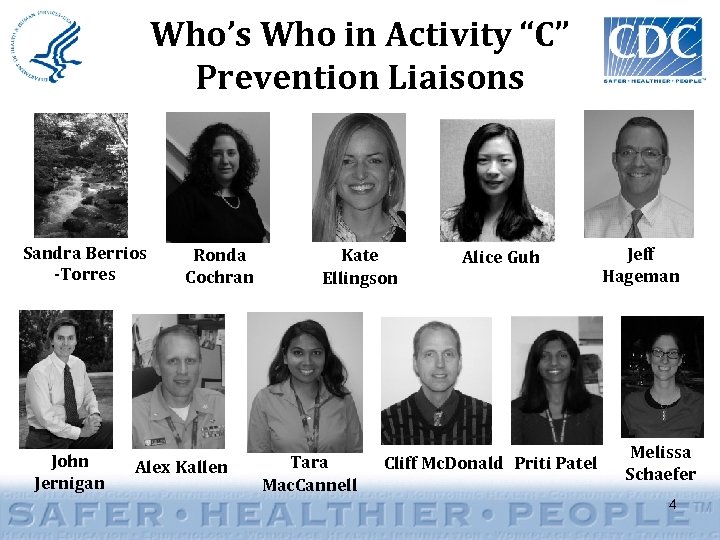
Who’s Who in Activity “C” Prevention Liaisons Sandra Berrios -Torres John Jernigan Ronda Cochran Alex Kallen Kate Ellingson Tara Mac. Cannell Alice Guh Cliff Mc. Donald Priti Patel Jeff Hageman Melissa Schaefer 4
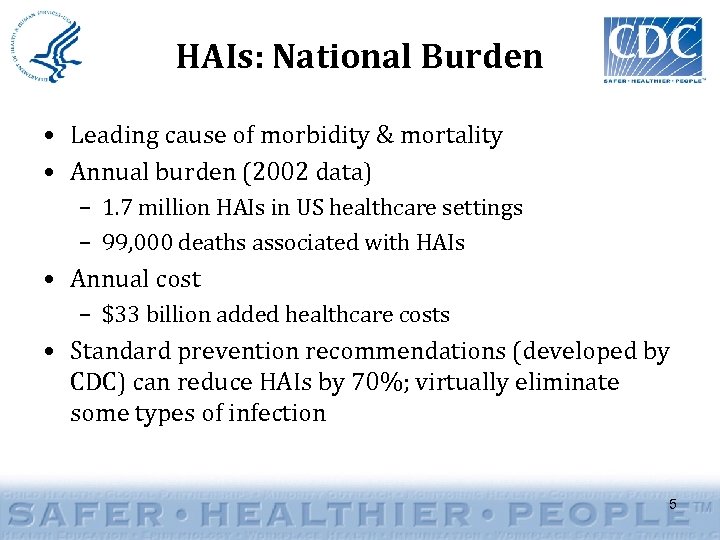
HAIs: National Burden • Leading cause of morbidity & mortality • Annual burden (2002 data) – 1. 7 million HAIs in US healthcare settings – 99, 000 deaths associated with HAIs • Annual cost – $33 billion added healthcare costs • Standard prevention recommendations (developed by CDC) can reduce HAIs by 70%; virtually eliminate some types of infection 5
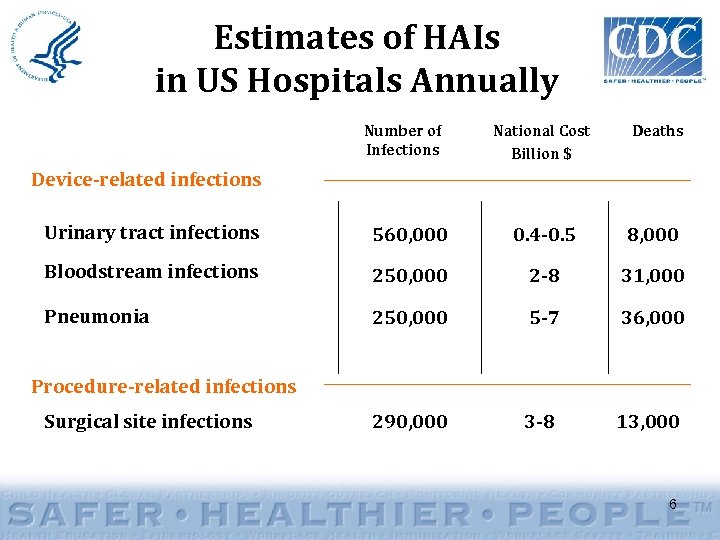
Estimates of HAIs in US Hospitals Annually Number of Infections National Cost Billion $ Deaths Device-related infections Urinary tract infections 560, 000 0. 4 -0. 5 8, 000 Bloodstream infections 250, 000 2 -8 31, 000 Pneumonia 250, 000 5 -7 36, 000 290, 000 3 -8 13, 000 Procedure-related infections Surgical site infections 6
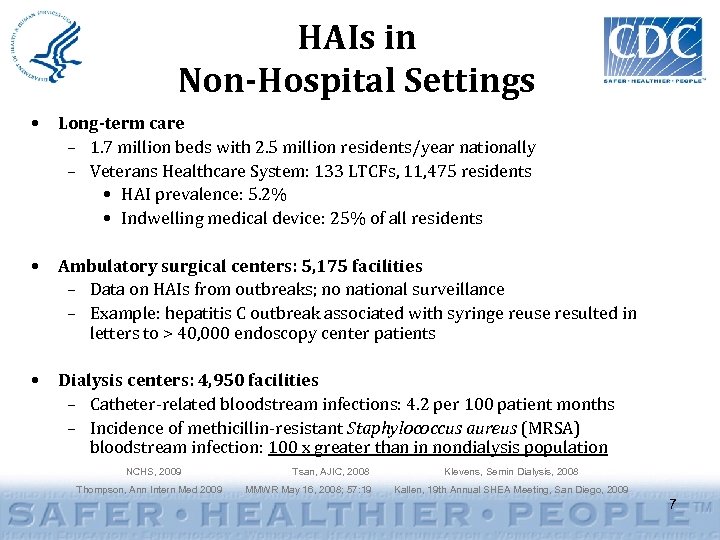
HAIs in Non-Hospital Settings • Long-term care – 1. 7 million beds with 2. 5 million residents/year nationally – Veterans Healthcare System: 133 LTCFs, 11, 475 residents • HAI prevalence: 5. 2% • Indwelling medical device: 25% of all residents • Ambulatory surgical centers: 5, 175 facilities – Data on HAIs from outbreaks; no national surveillance – Example: hepatitis C outbreak associated with syringe reuse resulted in letters to > 40, 000 endoscopy center patients • Dialysis centers: 4, 950 facilities – Catheter-related bloodstream infections: 4. 2 per 100 patient months – Incidence of methicillin-resistant Staphylococcus aureus (MRSA) bloodstream infection: 100 x greater than in nondialysis population NCHS, 2009 Thompson, Ann Intern Med 2009 Tsan, AJIC, 2008 MMWR May 16, 2008; 57: 19 Klevens, Semin Dialysis, 2008 Kallen, 19 th Annual SHEA Meeting, San Diego, 2009 7
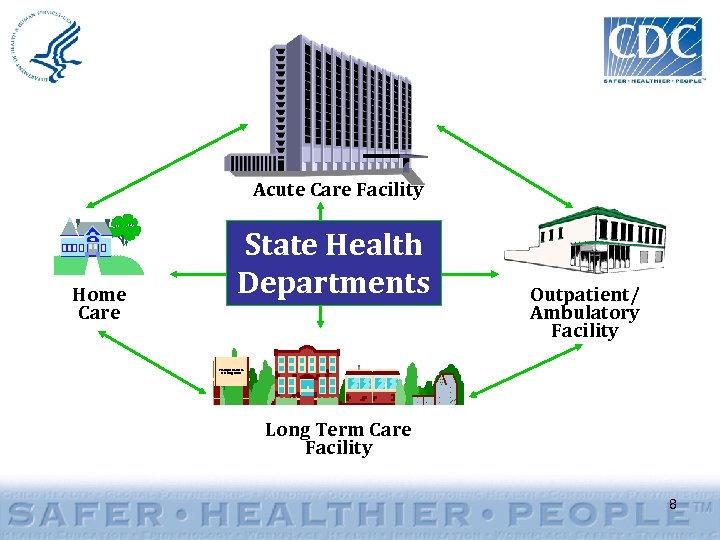
Acute Care Facility Home Care State Health Departments Outpatient/ Ambulatory Facility Tranquil Gardens Nursing Home Long Term Care Facility 8
HHS Action Plan In January 2009, the Department of Health and Human Services (HHS) released the HHS Action Plan to Prevent Healthcare-Associated Infections (http: //www. hhs. gov/ophs/initiatives/hai). 9
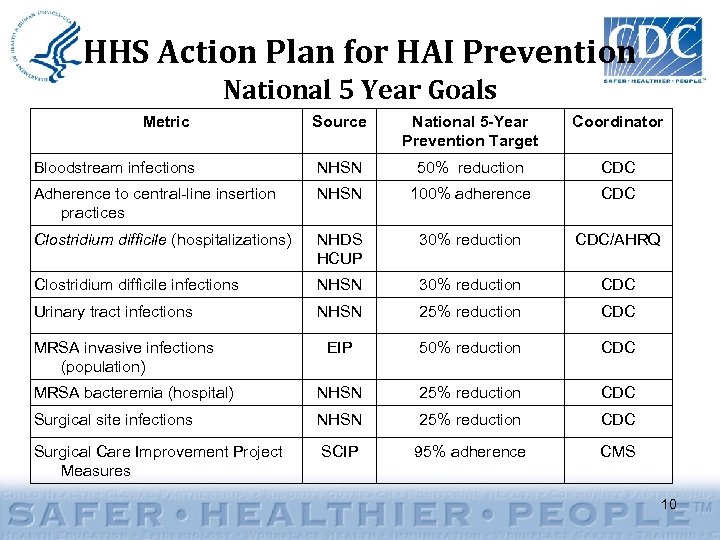
HHS Action Plan for HAI Prevention National 5 Year Goals Metric Source National 5 -Year Prevention Target Coordinator Bloodstream infections NHSN 50% reduction CDC Adherence to central-line insertion practices NHSN 100% adherence CDC Clostridium difficile (hospitalizations) NHDS HCUP 30% reduction CDC/AHRQ Clostridium difficile infections NHSN 30% reduction CDC Urinary tract infections NHSN 25% reduction CDC EIP 50% reduction CDC MRSA bacteremia (hospital) NHSN 25% reduction CDC Surgical site infections NHSN 25% reduction CDC Surgical Care Improvement Project Measures SCIP 95% adherence CMS MRSA invasive infections (population) 10
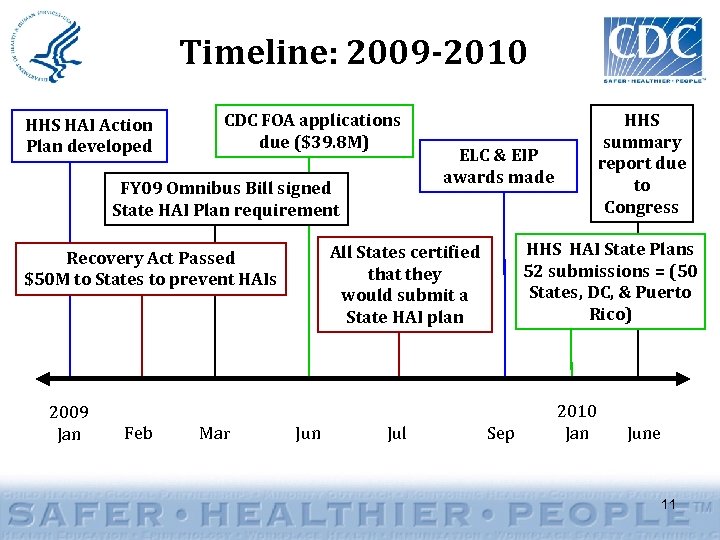
Timeline: 2009 -2010 HHS HAI Action Plan developed CDC FOA applications due ($39. 8 M) FY 09 Omnibus Bill signed State HAI Plan requirement Feb Mar HHS HAI State Plans 52 submissions = (50 States, DC, & Puerto Rico) All States certified that they would submit a State HAI plan Recovery Act Passed $50 M to States to prevent HAIs 2009 Jan ELC & EIP awards made Jun Jul HHS summary report due to Congress Sep 2010 Jan June 11
Recovery Act Overview • February 13, 2009: Congress passed American Recovery and Reinvestment Act of 2009 – February 17, 2009: President signed into law • 3 primary goals: – Create and save jobs – Spur economic activity and invest in long-term economic growth – Foster unprecedented levels of accountability and transparency in government spending 12
Recovery Act for HAI Overview • Prevention and Wellness Fund – HHS Office of the Secretary: provide to states to reduce healthcare-associated infections (HAI) • Focus: U. S. healthcare infrastructure / costs • Requires merit-based selection of recipients – Deliver programmatic results – Achieve economic stimulus • $50 million for HAI prevention – $10 million to Centers for Medicare & Medicaid Services (CMS) – $40 million to CDC • Eligibility limited to states 13
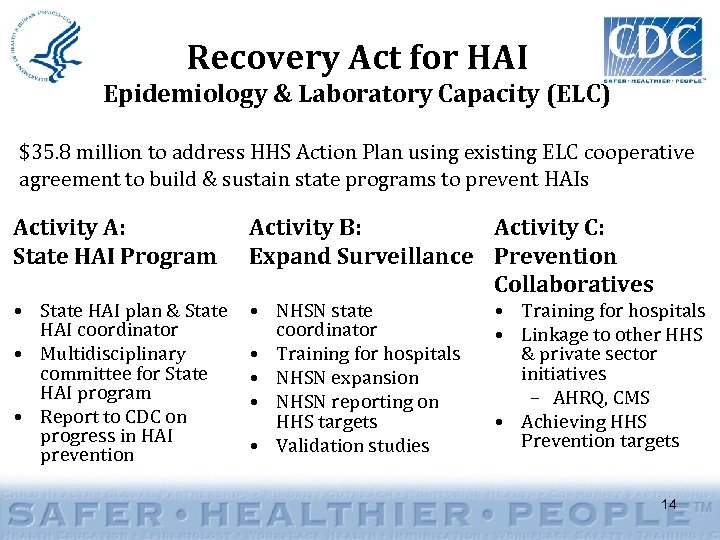
Recovery Act for HAI Epidemiology & Laboratory Capacity (ELC) $35. 8 million to address HHS Action Plan using existing ELC cooperative agreement to build & sustain state programs to prevent HAIs Activity A: State HAI Program • State HAI plan & State HAI coordinator • Multidisciplinary committee for State HAI program • Report to CDC on progress in HAI prevention Activity B: Activity C: Expand Surveillance Prevention Collaboratives • NHSN state coordinator • Training for hospitals • NHSN expansion • NHSN reporting on HHS targets • Validation studies • Training for hospitals • Linkage to other HHS & private sector initiatives – AHRQ, CMS • Achieving HHS Prevention targets 14
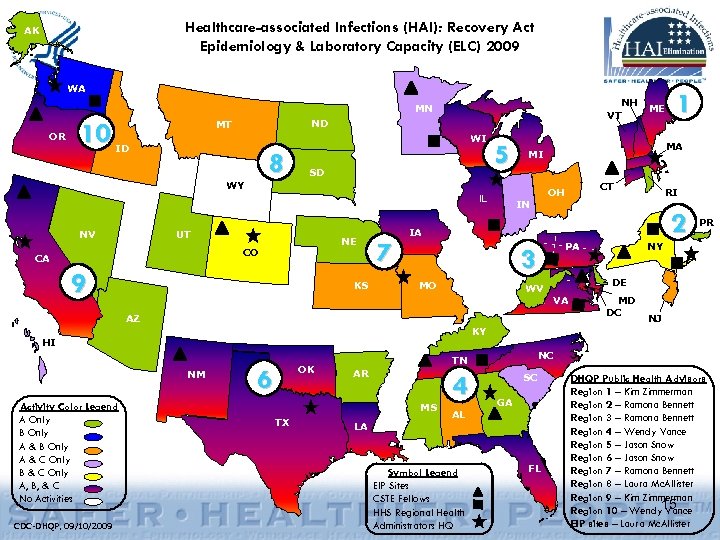
Healthcare-associated Infections (HAI): Recovery Act Epidemiology & Laboratory Capacity (ELC) 2009 AK WA WA NH ME VT ME MN OR OR 10 ND MT ID WI ID 8 WY SD 5 IL NV UT NE CO CA 9 KS 7 MA MI 2 PA 3 MO WV PR NY NY DE VA MD DC NJ KY KY HI NM CDC-DHQP, 09/10/2009 RI IA AZ Activity Color Legend A Only B Only A & C Only B & C Only A, B, & C No Activities CT OH IN 1 OK 6 AR MS TX NC NC TN 4 AL SC GA LA Symbol Legend EIP Sites CSTE Fellows HHS Regional Health Administrators HQ FL DHQP Public Health Advisors Region 1 – Kim Zimmerman Region 2 – Ramona Bennett Region 3 – Ramona Bennett Region 4 – Wendy Vance Region 5 – Jason Snow Region 6 – Jason Snow Region 7 – Ramona Bennett Region 8 – Laura Mc. Allister Region 9 – Kim Zimmerman Region 10 – Wendy 15 Vance EIP sites – Laura Mc. Allister
Performance Analysis • Quarterly Performance Reporting for HAI programs underway. • Preliminary Data – ELC § Recipients that have identified an HAI Coordinator: 51 (100%) § New hospitals enrolled in NHSN since 9/1/10: 467 § State plans submitted: 51 (they were due 1/1/10) 16
Recovery Act for HAI Opportunity & Impact • Promote rapid development and expansion of state-based efforts on HAI prevention • Develop and expand HAI prevention expertise in State Health Departments • Strengthen collaboration with HHS and HHS agencies— AHRQ, CMS • Provide a model for population-based prevention of healthcare safety challenges • Prevent infections, reduce deaths 17
Establishing HAI Prevention Collaboratives using ARRA Funds Planned State HAI Activities Prevention Surveillance Prevention Collaborative 18
Why Collaborate? 19
Definition from Merriam Webster • • • Main Entry: col·lab·o·rate Pronunciation: kə-ˈla-bə-ˌrāt Function: intransitive verb Inflected Form(s): col·lab·o·rat·ed; col·lab·o·rat·ing Etymology: Late Latin collaboratus, past participle of collaborare to labor together, from Latin com- + laborare to labor • Date: 1871 • 1 : to work jointly with others or together especially in an intellectual endeavor 2 : to cooperate with an agency or instrumentality with which one is not immediately connected 20
“Collaboration” – What does it mean? • “Coming together is a beginning. Keeping together is progress. Working together is success. ” – Henry Ford. • “Teamwork divides the task and multiplies the success. ” - Author Unknown • “Individual commitment to a group effort - that is what makes a team work, a company work, a society work, a civilization work. ” - Vince Lombardi • “Alone we can do so little; together we can do so much. ” – Helen Keller • “Teamwork is the ability to work together toward a common vision; the ability to direct individual accomplishment toward organizational objectives. It is the fuel that allows common people to attain uncommon results. ” – Andrew Carnegie • “Strength is derived from unity. The range of our collective vision is far greater when individual insights become one. ” – Andrew Carnegie • “Collaboration equals innovation. ” - Michael Dell • “The most important single ingredient in the formula of success is knowing how to get along with people. ” – Theodore Roosevelt • “In the long history of humankind (and animal kind, too) those who learned to collaborate most effectively have prevailed. ” – Charles Darwin 21

Why Is The Prevention Collaborative Model Important? 22
What is the Preventable Fraction of Healthcare Associated Infections? • Study on the Efficacy of Nosocomial Infection Control (SENIC) study results – 1971 -1976 – Suggested 6% of all nosocomial infections could be prevented by minimal infection control efforts, 32% by “well organized and highly effective infection control programs” • Harbarth et al: at least 20% of infections are preventable J Hosp Infection 2003; 54: 258 23
What is the Preventable Fraction of Healthcare Associated Infections? • Some may have interpreted these data to mean that most healthcare associated infections are inevitable – What impact has this had on the psychology of prevention? • How has this influenced the way infection control programs operate? – Difficult to define success when achievable results unknown-what should the goal be? 24
Eliminating catheter-related bloodstream infections in the intensive care unit Berenholtz, S et al. Critical Care Medicine. 32(10): 2014 -2020, October 2004. 25
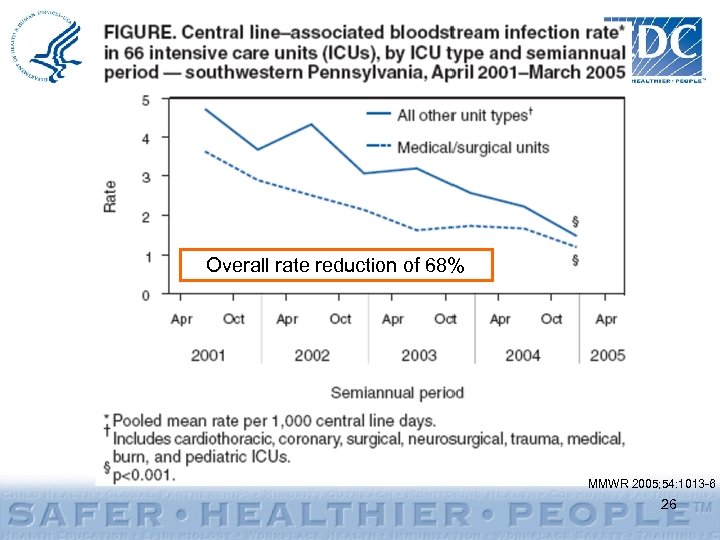
Overall rate reduction of 68% MMWR 2005; 54: 1013 -6 26
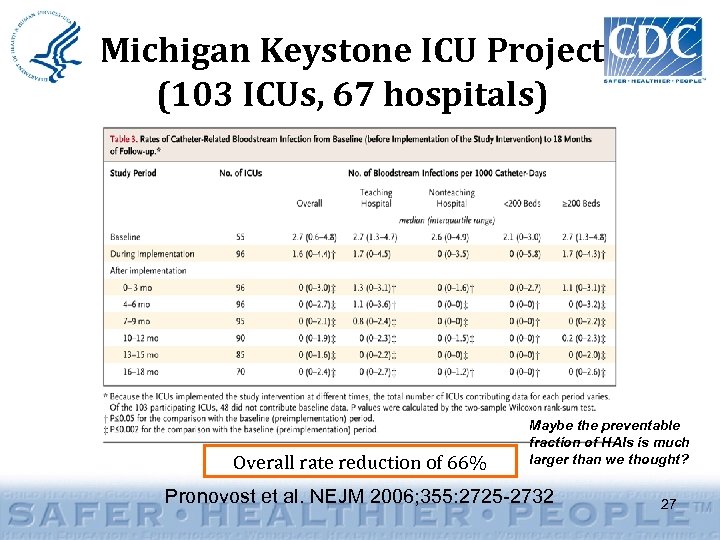
Michigan Keystone ICU Project (103 ICUs, 67 hospitals) Overall rate reduction of 66% Maybe the preventable fraction of HAIs is much larger than we thought? Pronovost et al. NEJM 2006; 355: 2725 -2732 27
Conclusions from Pittsburgh and Michigan Experiences • Decreases in central line-associated BSI rates >60% achieved in hospital ICUs of varying types • The prevention practices utilized during these interventions were not novel – Improving adherence to existing evidencebased practices can prevent BSIs – Collaboration may be helpful in identifying and overcoming commonly shared barriers to adherence 28
Conclusions from Pittsburgh and Michigan Experiences • Results from successful collaborative demonstration projects may be an important strategy for influencing global changes in practice in ways that improve quality – Disarms uncertainties about preventability that can hamper improvement efforts – Helps identify practical strategies that can be successful across many facilities 29
Successful, multi-center, regional Prevention Collaboratives will have national impact! • Must involve motivated acute and/or long-term care facilities who are interested in working in partnership with others to: – Identify setting-specific barriers and challenges (i. e. , because long-term care is very different from acute care) – Identify workable and practical solutions to those barriers – Take responsibility as a region of healthcare facilities, work together to address the problem • Create connections and relationships that bridge the gaps between facilities • “Intervention clusters” – – Be open to innovation Collect and share data in a uniform fashion Be in it for the long haul Contribute to an effort that will likely have major and enduring impact on the health of patients not only in your center, but across the Nation 30
How Do You Collaborate? A “Cookbook” to Collaboration Establishing HAI Prevention Collaboratives using ARRA Funds .
Cookbook Outline • Recipes* for Success – Staffing: Where to begin – Multidisciplinary Advisory Group – Participating Healthcare Facilities (e. g. , Hospitals) – Meetings – Measurement – Communication: How to sustain momentum *Note: “Season” to local taste 32
Where to Begin? : Staffing • Collaboration Metrics: – Project coordinator on staff – Infection control and prevention expertise available or on staff – Expertise in multicenter collaborative improvement projects available or on staff 33
Staffing: Suggested Ingredients • Infection Prevention and Clinical Expertise – Available at Health Department or as a consultant – Review the literature from expert(s) in your state – Important to have experts who are passionate and committed to infection prevention, suitable for championing concepts – Contact local APIC (Association for Professionals in Infection Control and Epidemiology) chapters - http: //www. apic. org/ – Consult with academic partners and experts in healthcare epidemiology at local hospitals and/or universities (i. e. , Society for Healthcare Epidemiology of America [SHEA] members - http: //www. sheaonline. org/) – CDC SME expert (Prevention Liaisons) 34
Staffing: Suggested Ingredients • Infection Prevention and Clinical Expertise – Provide facilities with suggestions for performing tasks and assist with data validation • All facilities using same criteria and data elements • Training for hospital staff on data elements and criteria – Help guide facility information sharing sessions • Encourage discussion of what is working and what is not to improve prevention activities • Front line personnel working in the individual hospitals should be involved in finding solutions to problems 35
Create and Convene a Multidisciplinary Advisory Group • Collaboration Metrics: – Letters of commitment from steering group members – Face to face meetings – Selection of targets for prevention collaborative – Selection of specific prevention goal – Feedback of outcomes to steering group 36
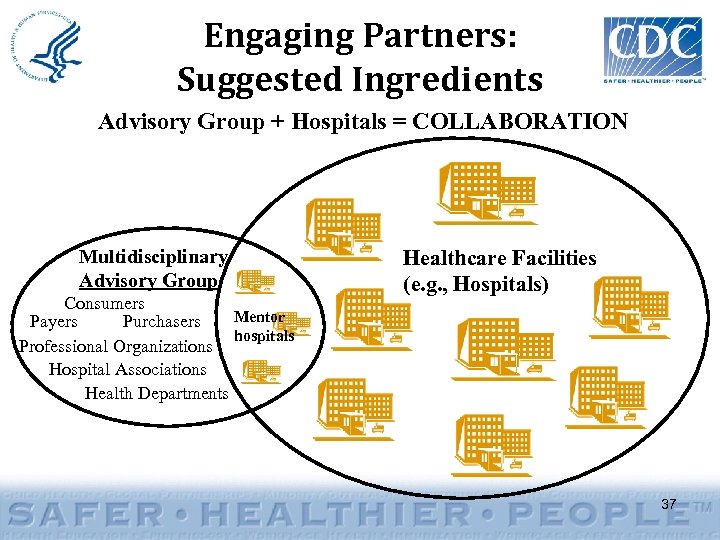
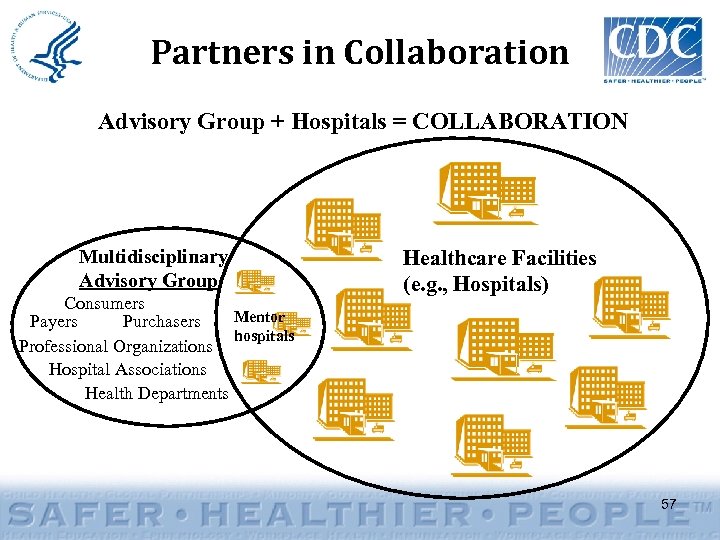
Engaging Partners: Suggested Ingredients Advisory Group + Hospitals = COLLABORATION Multidisciplinary Advisory Group Consumers Mentor Payers Purchasers hospitals Professional Organizations Hospital Associations Health Departments Healthcare Facilities (e. g. , Hospitals) 37
Engaging Partners • • Main Entry: part·ner Pronunciation: pärt-nər also pärd- Function: noun Etymology: Middle English partener, alteration of parcener, from Anglo-French, coparcener • Date: 14 th century • 1 archaic : one that shares 2: one associated with another especially in an action --- entities/groups working together towards a common HAI prevention goal 38
Partner Groups • Composition (representation/diverse experts) – involve multiple stakeholders – E. g. , Health Department, healthcare facilities (i. e. , approximately 2 -3 mentor hospitals), payors, purchasers, consumers, hospital associations, quality improvement organizations, professional organizations • Not all hospitals participating in the Collaborative should be part of the Multidisciplinary Advisory Group – just the 2 -3 mentor hospitals – Consider formalizing structure (i. e. , a charter or a memorandum of understanding) – including leadership (Chair, Co-Chair), operating rules, other policies (e. g. , conflicts of interest, financial relationships), etc. – Note: the more people involved, the greater the number of communications and coordination needed. 39
Partnering with Hospitals • Identify, recruit, and enroll participating hospitals – Initial contact suggested: Administration/hospital leadership (i. e. , CEO, CMO) – Obtaining Hospital Buy-in • Focus on the positives, such as: – The prevention of HAIs are best pursued and served through a collaboration rather than through individual efforts – Immediate and long-range consequences for the public, government, beneficiaries – The specific impact the hospital is likely to experience because of the collaboration effort • Think about what would want to make them join or barriers that may be in place – why is this mutually beneficial? 40
Partnering with Hospitals: Suggested Ingredients • Should be committed and enthusiastic about prevention and able to identify local champion(s) • Encourage active support and engagement from hospital leadership (e. g. , CEO, CMO, CNO, CQO) • Also should encourage ideas from unexpected sources (e. g. , housekeeping, transport) • Willing to communicate and share ideas including a willingness to participate in measurement system and share data with central coordinator • Get it in writing… letters of support and permission to use data 41

Implementation and Intervention Packages 42
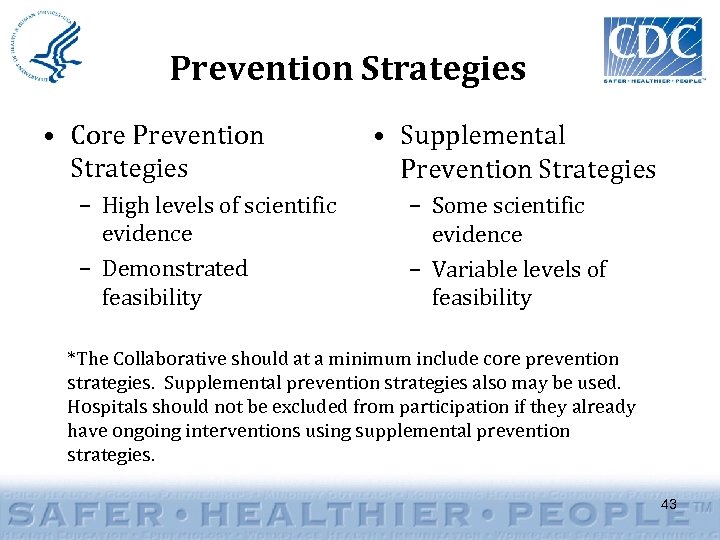
Prevention Strategies • Core Prevention Strategies – High levels of scientific evidence – Demonstrated feasibility • Supplemental Prevention Strategies – Some scientific evidence – Variable levels of feasibility *The Collaborative should at a minimum include core prevention strategies. Supplemental prevention strategies also may be used. Hospitals should not be excluded from participation if they already have ongoing interventions using supplemental prevention strategies. 43
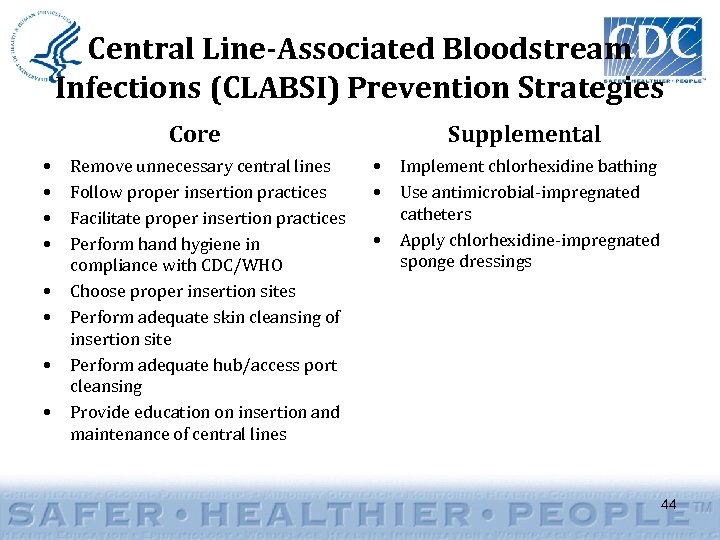
Central Line-Associated Bloodstream Infections (CLABSI) Prevention Strategies Core • • Remove unnecessary central lines Follow proper insertion practices Facilitate proper insertion practices Perform hand hygiene in compliance with CDC/WHO Choose proper insertion sites Perform adequate skin cleansing of insertion site Perform adequate hub/access port cleansing Provide education on insertion and maintenance of central lines Supplemental • • • Implement chlorhexidine bathing Use antimicrobial-impregnated catheters Apply chlorhexidine-impregnated sponge dressings 44
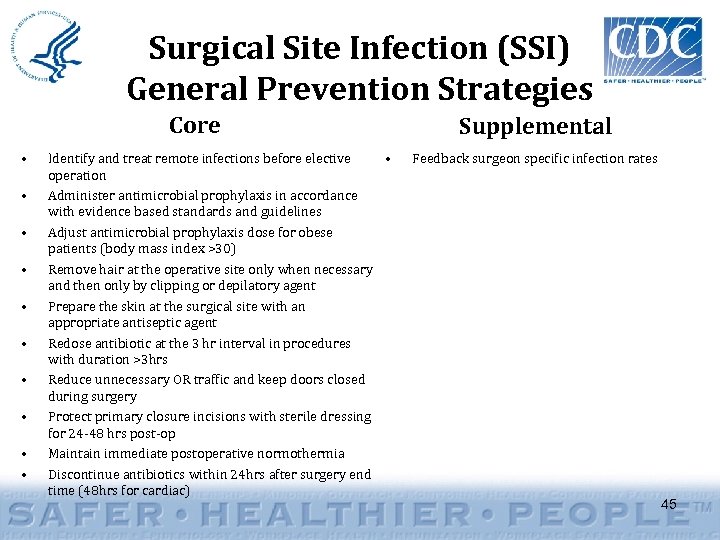
Surgical Site Infection (SSI) General Prevention Strategies Core • • • Identify and treat remote infections before elective • operation Administer antimicrobial prophylaxis in accordance with evidence based standards and guidelines Adjust antimicrobial prophylaxis dose for obese patients (body mass index >30) Remove hair at the operative site only when necessary and then only by clipping or depilatory agent Prepare the skin at the surgical site with an appropriate antiseptic agent Redose antibiotic at the 3 hr interval in procedures with duration >3 hrs Reduce unnecessary OR traffic and keep doors closed during surgery Protect primary closure incisions with sterile dressing for 24 -48 hrs post-op Maintain immediate postoperative normothermia Discontinue antibiotics within 24 hrs after surgery end time (48 hrs for cardiac) Supplemental Feedback surgeon specific infection rates 45
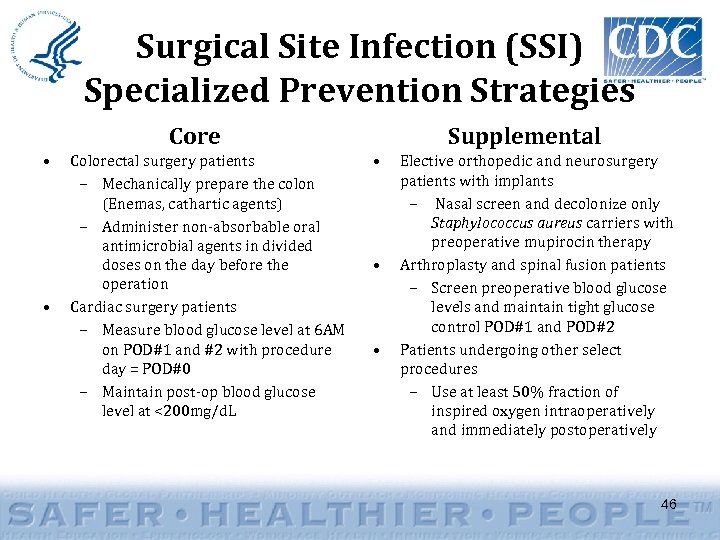
Surgical Site Infection (SSI) Specialized Prevention Strategies Core • • Colorectal surgery patients – Mechanically prepare the colon (Enemas, cathartic agents) – Administer non-absorbable oral antimicrobial agents in divided doses on the day before the operation Cardiac surgery patients – Measure blood glucose level at 6 AM on POD#1 and #2 with procedure day = POD#0 – Maintain post-op blood glucose level at <200 mg/d. L Supplemental • • • Elective orthopedic and neurosurgery patients with implants – Nasal screen and decolonize only Staphylococcus aureus carriers with preoperative mupirocin therapy Arthroplasty and spinal fusion patients – Screen preoperative blood glucose levels and maintain tight glucose control POD#1 and POD#2 Patients undergoing other select procedures – Use at least 50% fraction of inspired oxygen intraoperatively and immediately postoperatively 46

Measurement and Feedback 47
Measurement • Collaboration Metrics: – Select measurement system (e. g. , NHSN) – Demonstrate willingness of facilities to participate in measurement system and share data with central coordinator (i. e. , letters of commitment) – Demonstrate regular feedback of outcome data to participating facilities, to include a comparison of their individual performance to aggregate performance of others 48
Measurement: Suggested Ingredients • Use NHSN – Consistency with NHSN definitions is required • Evaluate prevention practices using standardized questions from CDC (infection toolkits) – Conduct surveys at designated time periods/intervals (i. e. , baseline and 6 -12 months into collaboration) • Communicate and Feedback Results (Shared Learnings) 49
Measurement: Suggested Ingredients • Identify goals and targets: “The goal is where you want to be. The objectives are the steps needed to get there. " • Be “SMART”: Specific – Measurable – Attainable – Relevant – Timely • Define the “who”, “what”, “when”, “why”, and “how” • Evaluate both process and outcome measures – Process: how have specific prevention measures been implemented (i. e. , compliance with hand hygiene, insertion practices – available in NHSN) – Outcome: what was the impact of the program and what were the program effects (i. e. , a reduction in 50 infection rates using NHSN)
Communication Strategy: How to Sustain Momentum • Collaboration Metrics: – Demonstrate face to face meetings – Demonstrate regularly scheduled teleconferences between face to face meetings – Demonstrate other supportive communication infrastructure for regular sharing between participants 51
Communication: Suggested Ingredients • Multimodal communication is best and information can be provided by a variety of means – – – – – E-mail Instant messaging/group chats Listservs Web (i. e. , centrally managed site/bulletin boards) Newsletters Meeting minutes Memos/letters/faxes Teleconference/Videoconference Face-to-face meetings 52
Communication: Suggested Ingredients • Successful prevention collaboratives are dependent upon mechanisms to facilitate sharing of information and data among participating facilities • Realtime communication via multiple channels is recommended • Feedback of data/results as soon as available • Many options for feedback using NHSN as standardized tool 53
Communication: Suggested Ingredients • Successful prevention collaboratives have standardized and uniform outcome measures that allow sharing of progress among participants and tracking aggregate group progress • Demonstrate regular feedback of outcome data to participating facilities, to include a comparison of their individual performance to aggregate performance of others • Using NHSN, data can be exported to various other programs for review, analysis, and sharing 54
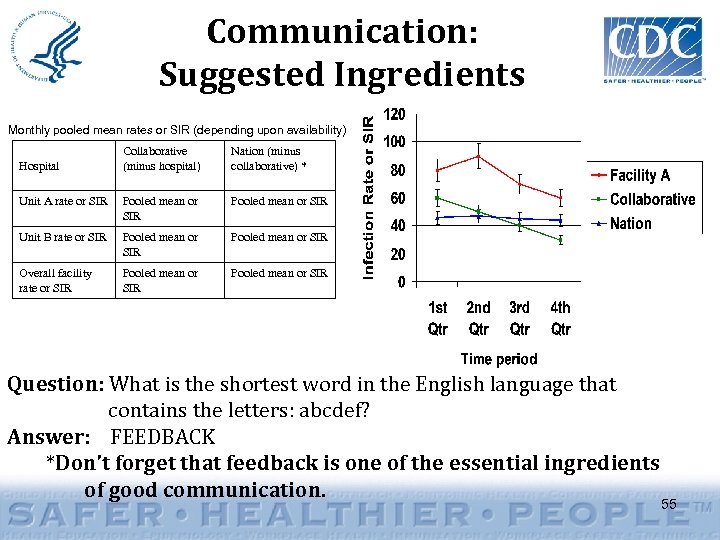
Communication: Suggested Ingredients Monthly pooled mean rates or SIR (depending upon availability) Collaborative (minus hospital) Nation (minus collaborative) * Unit A rate or SIR Pooled mean or SIR Unit B rate or SIR Pooled mean or SIR Overall facility rate or SIR Pooled mean or SIR Hospital Question: What is the shortest word in the English language that contains the letters: abcdef? Answer: FEEDBACK *Don’t forget that feedback is one of the essential ingredients of good communication. 55
“Who are we and why are we here? ” 56
Partners in Collaboration Advisory Group + Hospitals = COLLABORATION Multidisciplinary Advisory Group Consumers Mentor Payers Purchasers hospitals Professional Organizations Hospital Associations Health Departments Healthcare Facilities (e. g. , Hospitals) 57
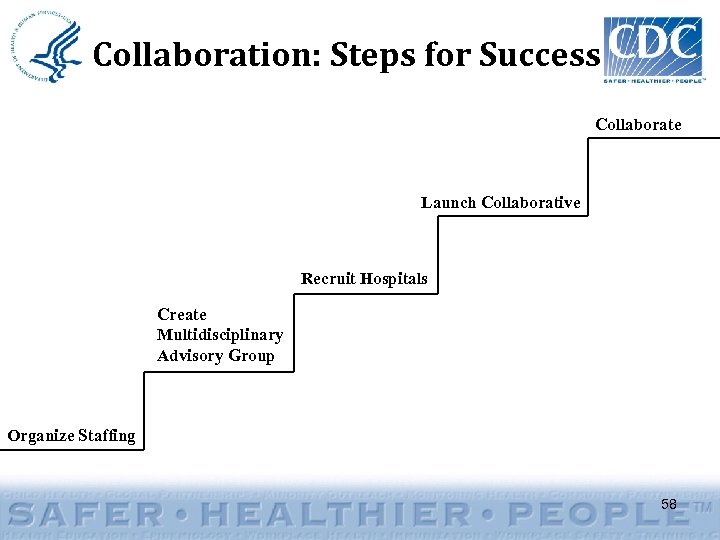
Collaboration: Steps for Success Collaborate Launch Collaborative Recruit Hospitals Create Multidisciplinary Advisory Group Organize Staffing 58
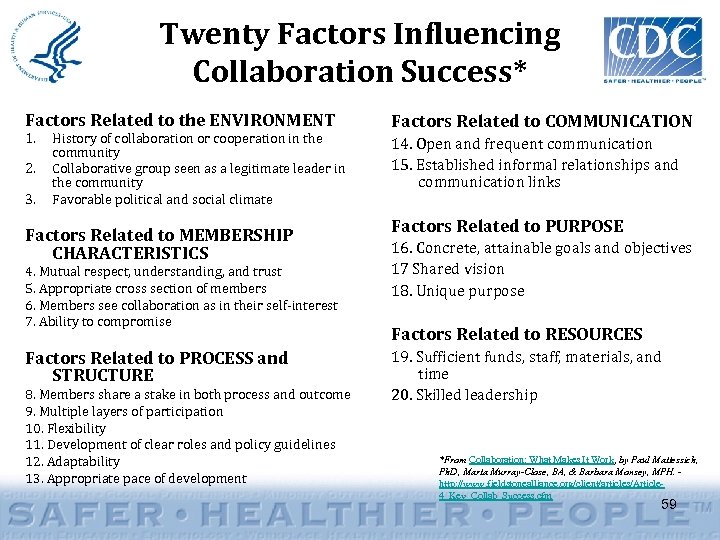
Twenty Factors Influencing Collaboration Success* Factors Related to the ENVIRONMENT 1. 2. 3. History of collaboration or cooperation in the community Collaborative group seen as a legitimate leader in the community Favorable political and social climate Factors Related to MEMBERSHIP CHARACTERISTICS 4. Mutual respect, understanding, and trust 5. Appropriate cross section of members 6. Members see collaboration as in their self-interest 7. Ability to compromise Factors Related to PROCESS and STRUCTURE 8. Members share a stake in both process and outcome 9. Multiple layers of participation 10. Flexibility 11. Development of clear roles and policy guidelines 12. Adaptability 13. Appropriate pace of development Factors Related to COMMUNICATION 14. Open and frequent communication 15. Established informal relationships and communication links Factors Related to PURPOSE 16. Concrete, attainable goals and objectives 17 Shared vision 18. Unique purpose Factors Related to RESOURCES 19. Sufficient funds, staff, materials, and time 20. Skilled leadership *From Collaboration: What Makes It Work, by Paul Mattessich, Ph. D, Marta Murray-Close, BA, & Barbara Monsey, MPH. http: //www. fieldstonealliance. org/client/articles/Article 4_Key_Collab_Success. cfm 59
Key Elements in Quality Improvement Collaboratives* • • Don’t recreate the wheel! Measure, measure and provide feedback Measure over time Test on a small scale, multiple times, multiple ways before implementing • Transparency • Keep it simple and sensible • Aim high *From IHI - http: //www. ihi. org/IHI/ 60
Summary • HAIs are an important public health problem that continue to evolve • Prevention collaboratives work! • The epidemiology suggests that regional efforts to prevent transmission of HAIs may have best chance of making a difference • • • Institute for Healthcare Improvement Breakthrough Collaboratives – http: //www. ihi. org/IHI/ Michigan Keystone – http: //www. mhakeystonecenter. org/ Pittsburgh Regional Healthcare Initiative – http: //www. prhi. org/ Rochester Health Commission – http: //www. grrhio. org/ Vermont-Oxford Neonatal Network – http: //www. vtoxford. org/ Veteran’s Health Affairs – http: //www. pittsburgh. va. gov/MRSA_Prevention_Initiative. asp 61
Summary • The Texas HAI Prevention Collaborative is off to a great start! – Focus and flexibility are key – “Season to taste” – local variation is important as not every hospital is going to do the same thing -- the more you can harmonize the Collaboration, the richer the shared learnings – Hospitals should learn from one another and share their experiences • If successful, it could change the way infection control is practiced in this country 62
“Collaboration” – What does it mean? • “Coming together is a beginning. Keeping together is progress. Working together is success. ” – Henry Ford. • “Teamwork divides the task and multiplies the success. ” - Author Unknown • “Individual commitment to a group effort - that is what makes a team work, a company work, a society work, a civilization work. ” - Vince Lombardi • “Alone we can do so little; together we can do so much. ” – Helen Keller • “Teamwork is the ability to work together toward a common vision; the ability to direct individual accomplishment toward organizational objectives. It is the fuel that allows common people to attain uncommon results. ” – Andrew Carnegie • “Strength is derived from unity. The range of our collective vision is far greater when individual insights become one. ” – Andrew Carnegie • “Collaboration equals innovation. ” - Michael Dell • “The most important single ingredient in the formula of success is knowing how to get along with people. ” – Theodore Roosevelt • “In the long history of humankind (and animal kind, too) those who learned to collaborate most effectively have prevailed. ” – Charles Darwin 63

Thank you! Questions? http: //www. cdc. gov/hai/recoveryact/ 64
0ab0e256d176608b6e040dd870c73eb3.ppt