e631cf794b7a293e814153a49c22e2eb.ppt
- Количество слайдов: 77
The pregnant trauma patient Tom Archer MD, MBA UCSD Anesthesia
Outline • • Epidemiology General approach to the patient Anesthesia and diagnostic studies. Obstetric complications of trauma – (What the obstetrician will be thinking about) • Relevant maternal / fetal physiology • FHR monitoring • Perimortem cesarean section
Trauma in pregnancy • Trauma is most common non-obstetric cause of maternal death. • Common major traumas: MVAs, falls and assaults. • 5 -10% of pregnancies are marred by some sort of trauma (usually very minor and not seen in hospital). • In one study, 0. 2% of all pregnant women were seen in hospital for trauma during a given pregnancy. Chestnut chap 53, El Kady D et al 2004
Trauma in pregnancy • Incidence of trauma increases as pregnancy progresses: – 8% in first trimester – 40% in second trimester – 52% in third trimester
Causes of maternal death • Most maternal deaths are due to head trauma or hemorrhagic shock.
Commonest causes of fetal death • In severe maternal injury, it is maternal death. • In “minor” injury, it is placental abruption
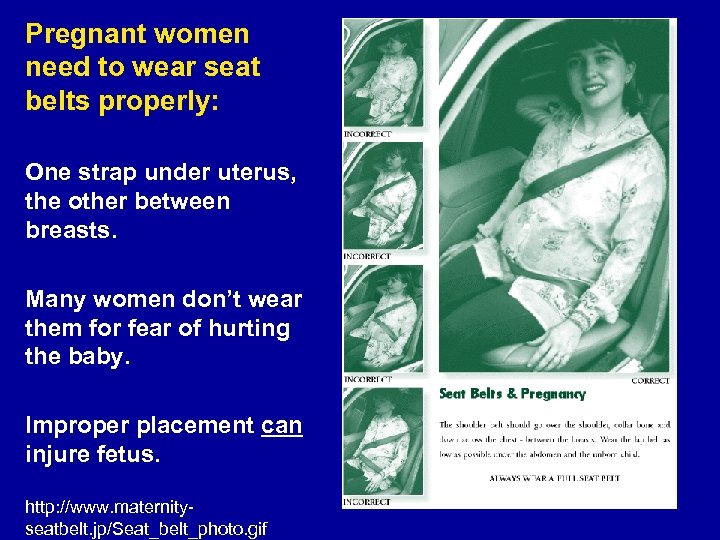
Pregnant women need to wear seat belts properly: One strap under uterus, the other between breasts. Many women don’t wear them for fear of hurting the baby. Improper placement can injure fetus. http: //www. maternityseatbelt. jp/Seat_belt_photo. gif
Domestic violence • Domestic violence knows no boundaries of race or economic status. • Pregnancy often represents dependency and loss of autonomy and control. • Abusers will take advantage of this. They may feel threatened by pregnancy and attack abdomen as a way of retaliating against fetus.
Domestic violence • Think of it as a possibility! • Look for emotional withdrawal, depression, selfblame. • Look for other (older) signs of injury. • Face-to-face, one-on-one interviews. Calm, matter-of-fact tone helps elicit Hx.
“What will happen to my baby? ” • “Trauma appears to affect the fetus only in the short-term…” • “…if there is no early placental abruption, fetal death, premature rupture of membranes, or urgent delivery, there is no significant difference in pregnancy outcome…” • Shah KH 1998
Trauma management in pregnancy • Best way to take care of baby is to take care of mother. All ACLS guidelines apply. • Know how physiological / anatomical changes of pregnancy affect vulnerability of patient to stresses. • Plan for specific obstetric concerns (without getting obsessed). • Common worries (patient, nurse, MD) : radiation, drugs, abruption, anesthesia.
Anesthesia in OB trauma • Maintain good anesthesia, oxygenation, normotension, normothermia, normocarbia (Pa. CO 2 = 30) and LUD. Avoid ketamine > 2 mg /kg (uterine hypertonus). • Monitor FHTs if practical. Loss of variability is normal, but fetal tachy- or bradycardia may mean hypoxia. • Defensive medicine: probably avoid benzodiazepines and N 2 O early in gestation (little to no solid evidence for this).
X-ray studies in pregnant patients • Use x-ray studies judiciously– but USE THEM when needed! • Shield uterus when possible. • Consult with radiologist on minimizing exposure.
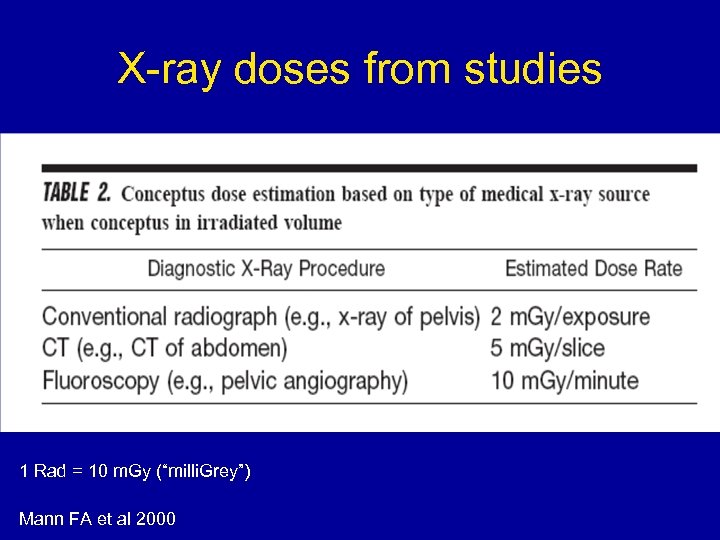
X-ray doses from studies 1 Rad = 10 m. Gy (“milli. Grey”) Mann FA et al 2000
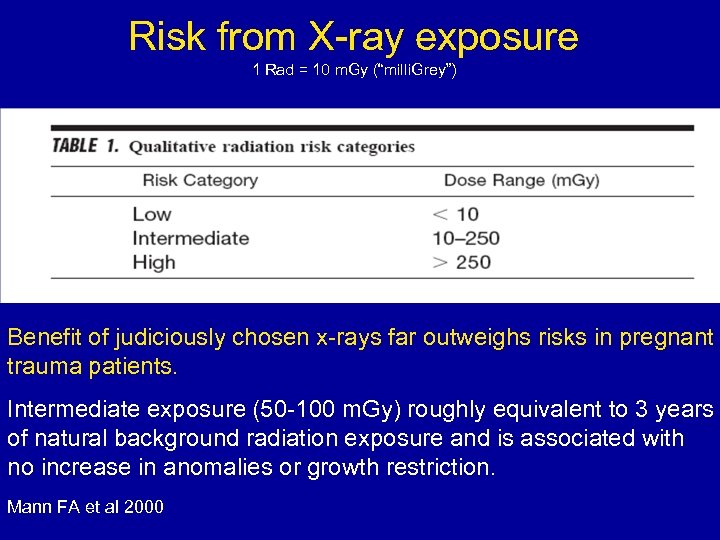
Risk from X-ray exposure 1 Rad = 10 m. Gy (“milli. Grey”) Benefit of judiciously chosen x-rays far outweighs risks in pregnant trauma patients. Intermediate exposure (50 -100 m. Gy) roughly equivalent to 3 years of natural background radiation exposure and is associated with no increase in anomalies or growth restriction. Mann FA et al 2000
X-ray studies in pregnant patients • CT is gold standard for Dx of blunt abdominal trauma. • Transport from ER to CT scanner and radiation risks / fears remain as obstacles to CT. Miller MT 2003
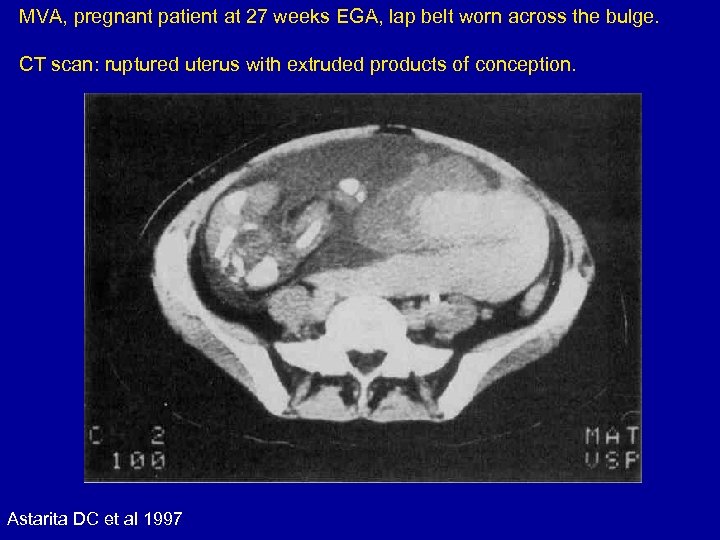
MVA, pregnant patient at 27 weeks EGA, lap belt worn across the bulge. CT scan: ruptured uterus with extruded products of conception. Astarita DC et al 1997
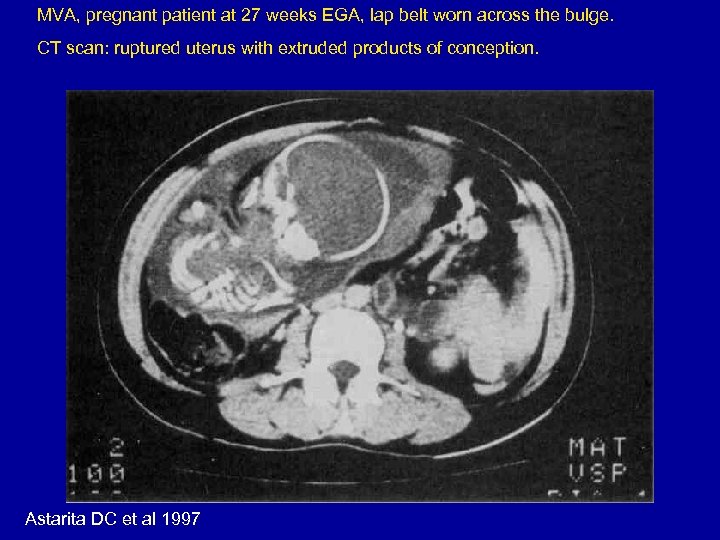
MVA, pregnant patient at 27 weeks EGA, lap belt worn across the bulge. CT scan: ruptured uterus with extruded products of conception. Astarita DC et al 1997
Ultrasound in trauma evaluation • Can ultrasound substitute for CT? Modality is called FAST (“Focused Abdominal Sonography for Trauma”). • Focus of FAST is detecting free fluid, presumed to be blood. • FAST is part of screening process, but can miss injuries (e. g. solid organ). Miller MT 2003

Lateral pelvic ultrasound: free fluid in cul-de-sac (+ Foley in bladder). Richards JR 2004
Obstetric complications of trauma • Abruption Pre-term labor • Ruptured membranes • Uterine rupture • Direct fetal injury (usually penetrating trauma) • Rare: amniotic fluid embolus, chorionic villus embolus Kingston NJ 2003 Judich A 1998
Predisposing factors to DIC / ARDS after trauma in pregnancy: • • • Abruption. Dead fetus. Shock Sepsis Traumatic amniotic fluid embolus (rare). – Factors in common are release of abnormal substances into circulation. • Hypothermia and acidosis exacerbate coagulopathy. Ferrara A 1990
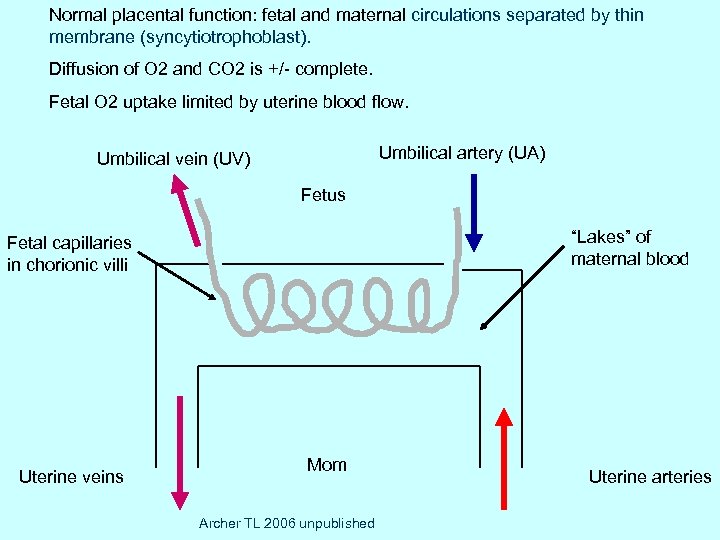
Normal placental function: fetal and maternal circulations separated by thin membrane (syncytiotrophoblast). ) Diffusion of O 2 and CO 2 is +/- complete. Fetal O 2 uptake limited by uterine blood flow. Umbilical artery (UA) Umbilical vein (UV) Fetus “Lakes” of maternal blood Fetal capillaries in chorionic villi Uterine veins Mom Archer TL 2006 unpublished Uterine arteries
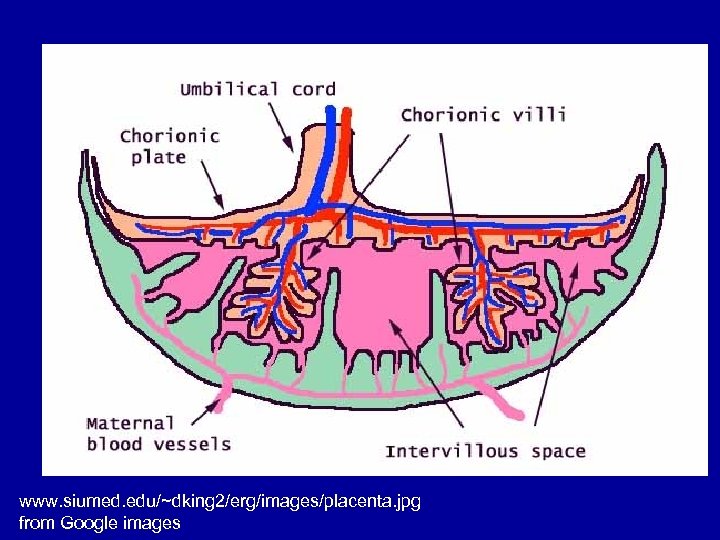
www. siumed. edu/~dking 2/erg/images/placenta. jpg from Google images
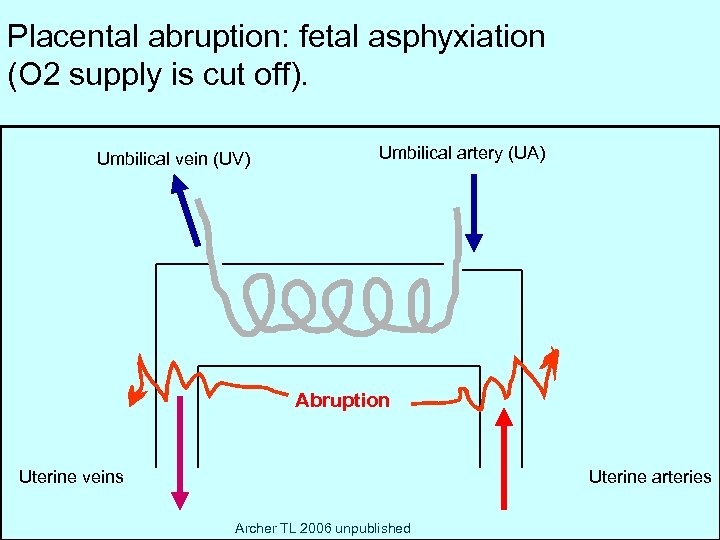
Placental abruption: fetal asphyxiation ) (O 2 supply is cut off). Umbilical vein (UV) Umbilical artery (UA) Abruption Uterine veins Uterine arteries Archer TL 2006 unpublished
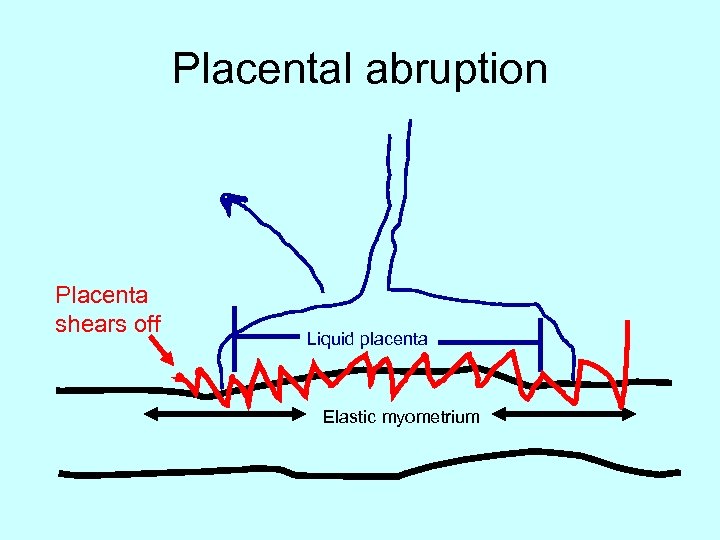
Placental abruption Placenta shears off Liquid placenta Elastic myometrium
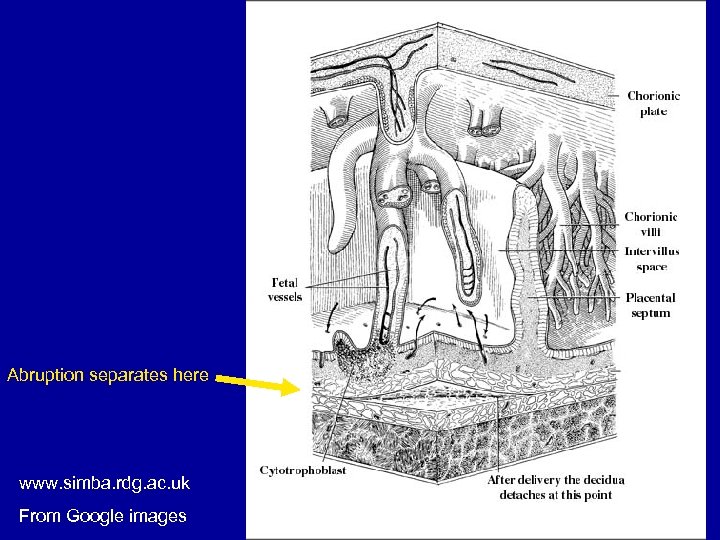
Abruption separates here www. simba. rdg. ac. uk From Google images
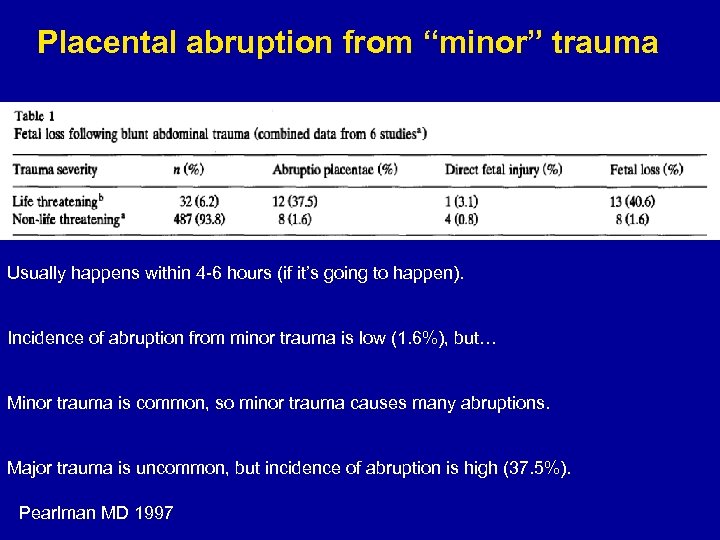
Placental abruption from “minor” trauma Usually happens within 4 -6 hours (if it’s going to happen). Incidence of abruption from minor trauma is low (1. 6%), but… Minor trauma is common, so minor trauma causes many abruptions. Major trauma is uncommon, but incidence of abruption is high (37. 5%). Pearlman MD 1997
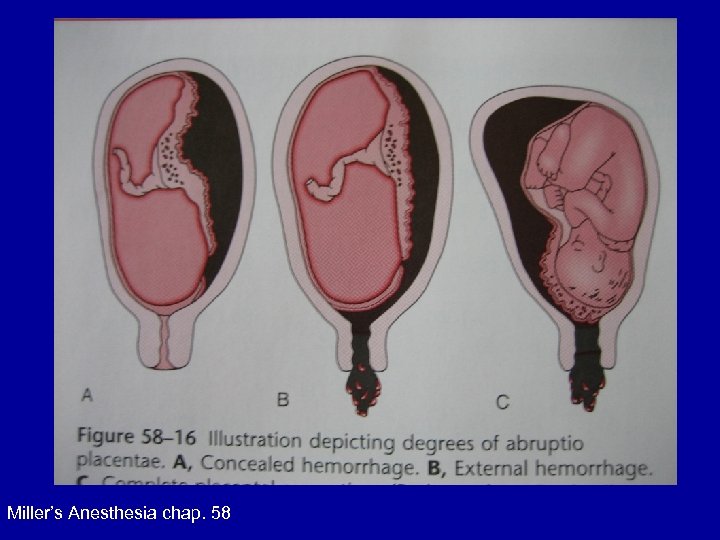
Miller’s Anesthesia chap. 58
Placental abruption • Accompanies 1 -5% of minor injuries, 20 -50% of major injuries. • • Abdominal tenderness Uterine contractions Vaginal bleeding– but hemorrhage may be hidden.
Placental trauma (+/- abruption): Feto-maternal hemorrhage • More common with anterior placenta? (Pearlman 1990) • Chorionic villi break, releasing fetal RBCs into lakes of maternal blood. • Dangers: – Iso-immunization of Rh- mother by Rh+ fetal cells. – Fetal exsanguination / anemia / hydrops / brain damage. – Premature labor (due to release of thrombin, lysozymes or prostaglandins into maternal circulation? ).
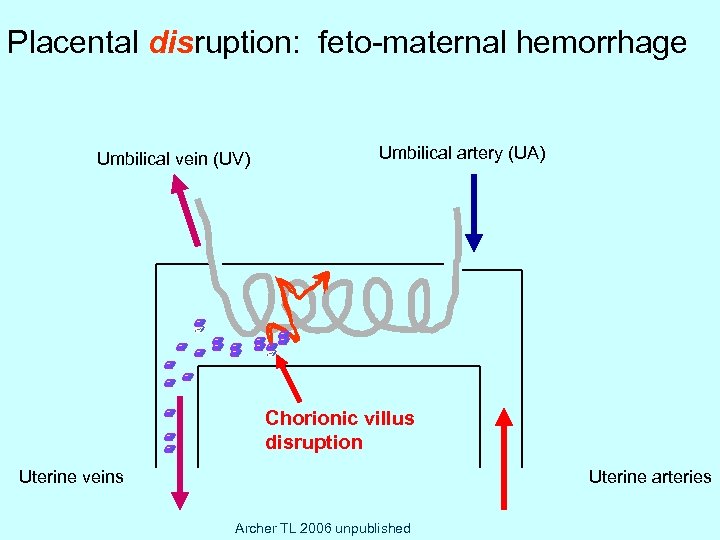
) Placental disruption: feto-maternal hemorrhage Umbilical vein (UV) Umbilical artery (UA) Chorionic villus disruption Uterine veins Uterine arteries Archer TL 2006 unpublished
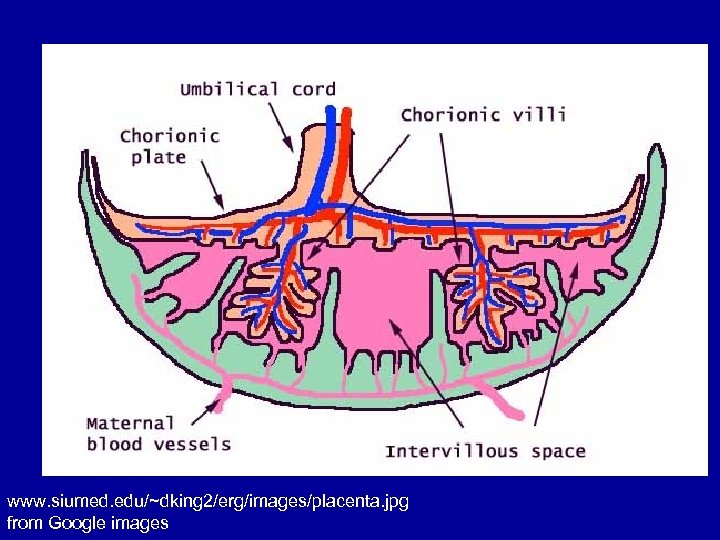
www. siumed. edu/~dking 2/erg/images/placenta. jpg from Google images
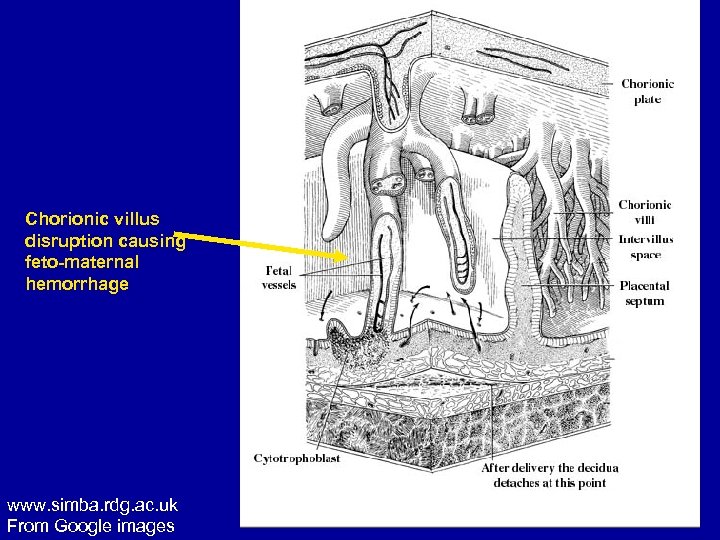
Chorionic villus disruption causing feto-maternal hemorrhage www. simba. rdg. ac. uk From Google images
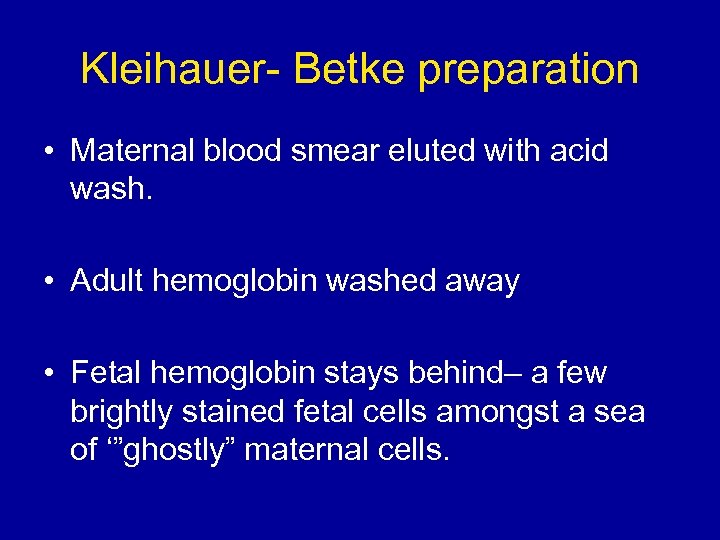
Kleihauer- Betke preparation • Maternal blood smear eluted with acid wash. • Adult hemoglobin washed away • Fetal hemoglobin stays behind– a few brightly stained fetal cells amongst a sea of ‘”ghostly” maternal cells.
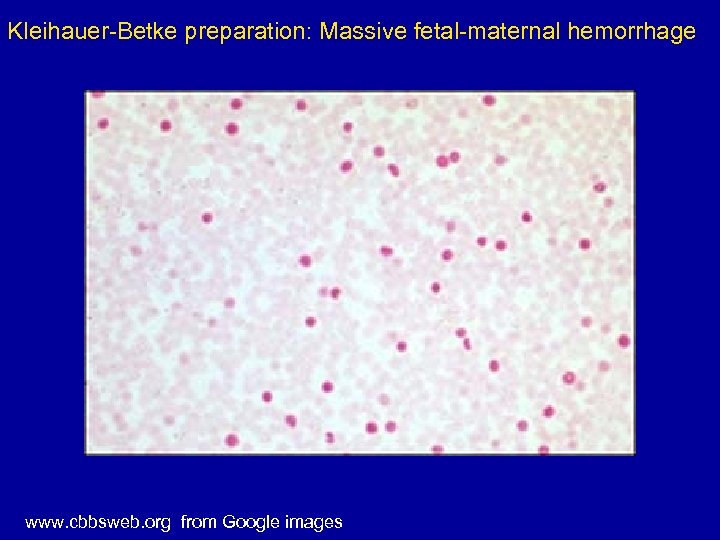
Kleihauer-Betke preparation: Massive fetal-maternal hemorrhage www. cbbsweb. org from Google images
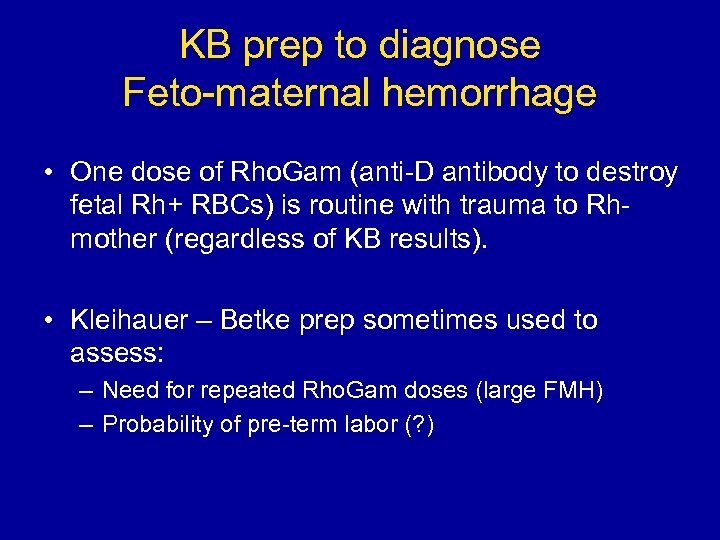
KB prep to diagnose Feto-maternal hemorrhage • One dose of Rho. Gam (anti-D antibody to destroy fetal Rh+ RBCs) is routine with trauma to Rh- mother (regardless of KB results). • Kleihauer – Betke prep sometimes used to assess: – Need for repeated Rho. Gam doses (large FMH) – Probability of pre-term labor (? )
Does feto-maternal hemorrhage promote pre-term labor?
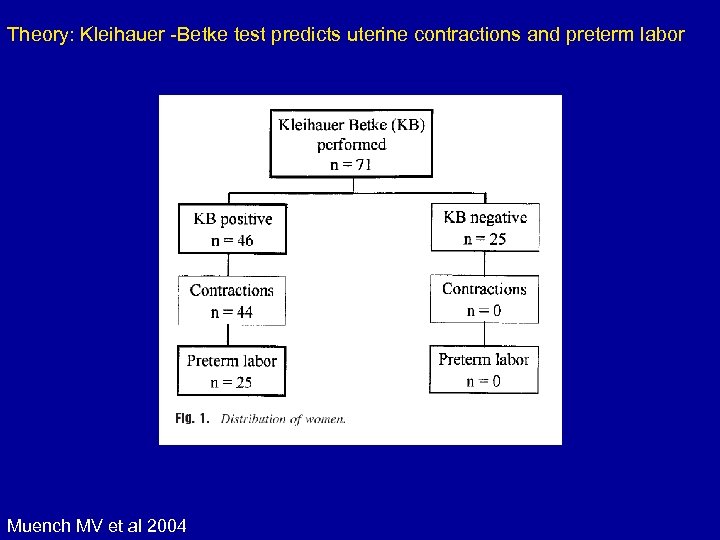
Theory: Kleihauer -Betke test predicts uterine contractions and preterm labor Muench MV et al 2004
Fetal heart rate monitoring (for hypoxia) after trauma • • Worry is abruption. Usually combined with contraction monitoring. 4 hours is routine. >4 hours if: – – – Abruption suspected Frequent uterine activity Rupture of membranes FHR abnormalities present Mother is in critical condition Chestnut chap 53
Ruptured uterus • Life-threatening emergency, 10% maternal mortality • Fetus almost always dies.
Ruptured amniotic membranes • Vaginal fluid leak– avenue for infection. • By itself, not an emergency.
Maternal / fetal physiology and anatomy relevant to trauma
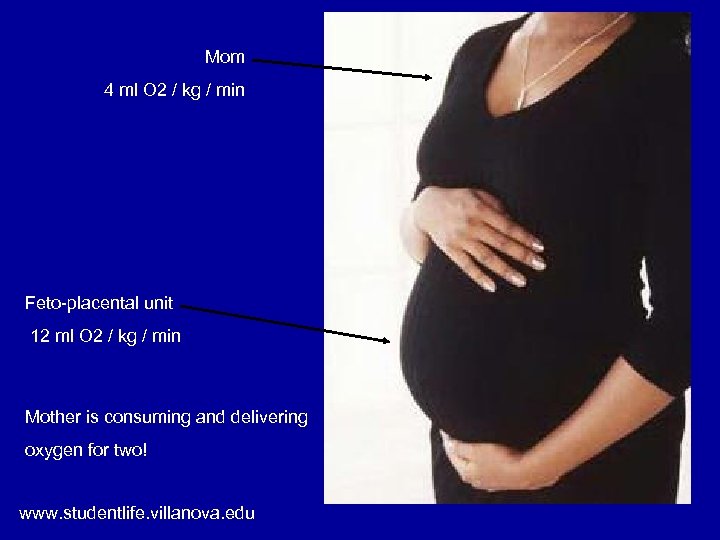
Mom 4 ml O 2 / kg / min Feto-placental unit 12 ml O 2 / kg / min Mother is consuming and delivering oxygen for two! www. studentlife. villanova. edu
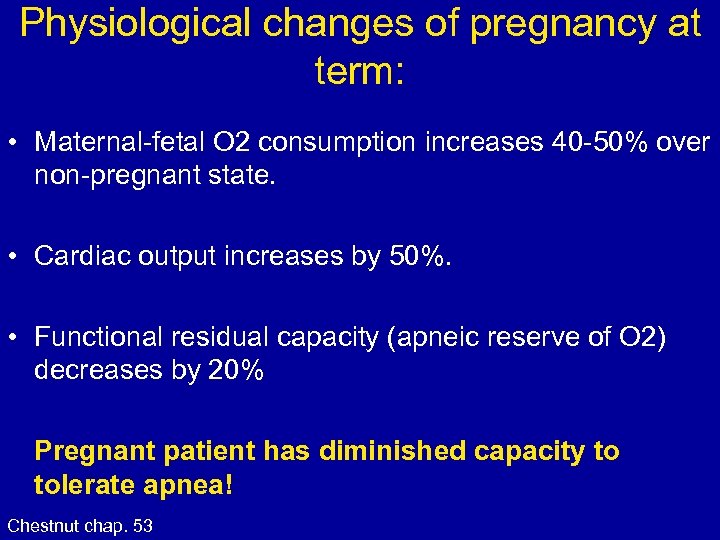
Physiological changes of pregnancy at term: • Maternal-fetal O 2 consumption increases 40 -50% over non-pregnant state. • Cardiac output increases by 50%. • Functional residual capacity (apneic reserve of O 2) decreases by 20% Pregnant patient has diminished capacity to tolerate apnea! Chestnut chap. 53

Functional residual capacity (FRC) is our “air tank” for apnea. www. picture-newsletter. com/scuba-diving/scuba. . . from Google images

Pregnant Mom has a smaller “air tank”. Non-pregnant woman www. pyramydair. co m/blog/images/scuba -web. jpg
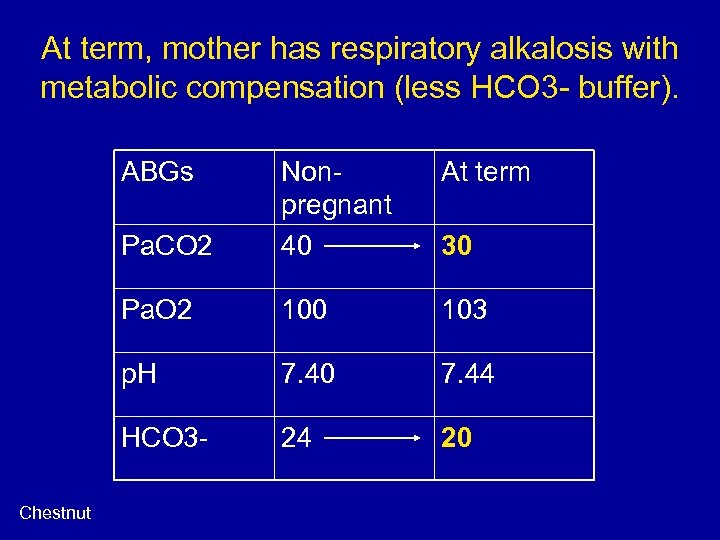
At term, mother has respiratory alkalosis with metabolic compensation (less HCO 3 - buffer). ABGs Pa. O 2 100 103 p. H 7. 40 7. 44 HCO 3 Chestnut At term Pa. CO 2 Nonpregnant 40 24 20 30
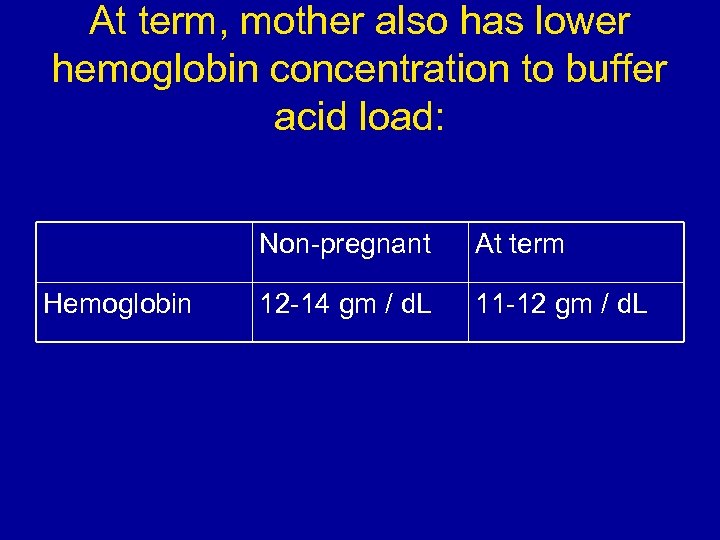
At term, mother also has lower hemoglobin concentration to buffer acid load: Non-pregnant Hemoglobin At term 12 -14 gm / d. L 11 -12 gm / d. L
Compared to non-pregnant state, pregnant woman has less tolerance for: • Apnea • Acidosis
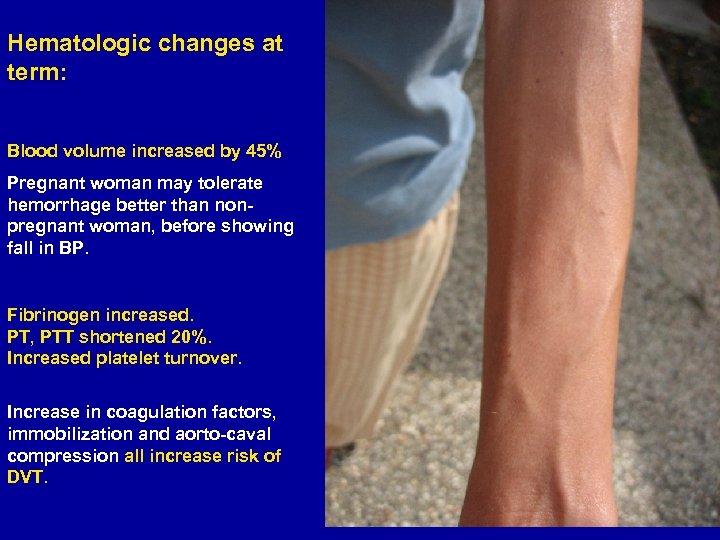
Hematologic changes at term: Blood volume increased by 45% Pregnant woman may tolerate hemorrhage better than nonpregnant woman, before showing fall in BP. Fibrinogen increased. PT, PTT shortened 20%. Increased platelet turnover. Increase in coagulation factors, immobilization and aorto-caval compression all increase risk of DVT.
Vascular congestion • Swelling of respiratory mucosa (nose, rest of airway). • Don’t put anything through the nose if you can avoid it prevent bad nose bleed.
GI tract • Decreased gastric emptying • Increase GERD • Full stomach precautions
Avoid aorto-caval compression: use left uterine displacement (LUD) • LUD helps venous return. C/S as part of resuscitation? • LUD decreases chance of DVT • LUD increases O 2 delivery to fetus: – Increases uterine artery pressure and decreases uterine venous pressure. • Why we don’t do it: It doesn’t look right!
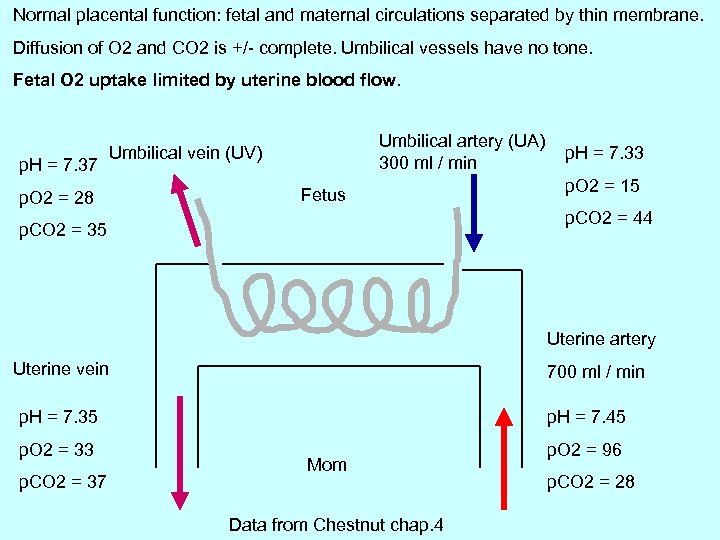
Normal placental function: fetal and maternal circulations separated by thin membrane. ) Diffusion of O 2 and CO 2 is +/- complete. Umbilical vessels have no tone. Fetal O 2 uptake limited by uterine blood flow. p. H = 7. 37 p. O 2 = 28 Umbilical artery (UA) 300 ml / min Umbilical vein (UV) Fetus p. H = 7. 33 p. O 2 = 15 p. CO 2 = 44 p. CO 2 = 35 Uterine artery Uterine vein 700 ml / min p. H = 7. 35 p. H = 7. 45 p. O 2 = 33 p. O 2 = 96 p. CO 2 = 37 Mom Data from Chestnut chap. 4 p. CO 2 = 28
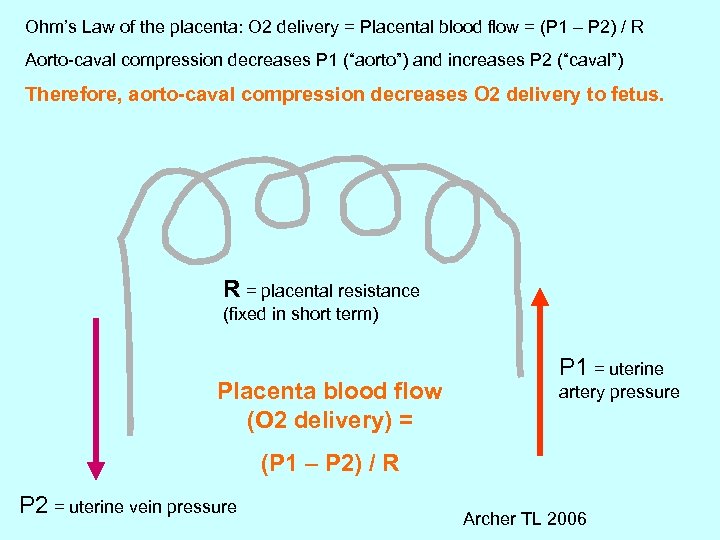
Ohm’s Law of the placenta: O 2 delivery = Placental blood flow = (P 1 – P 2) / R Aorto-caval compression decreases P 1 (“aorto”) and increases P 2 (“caval”) Therefore, aorto-caval compression decreases O 2 delivery to fetus. R = placental resistance (fixed in short term) Placenta blood flow (O 2 delivery) = P 1 = uterine artery pressure (P 1 – P 2) / R P 2 = uterine vein pressure Archer TL 2006
Colman-Brochu S 2004
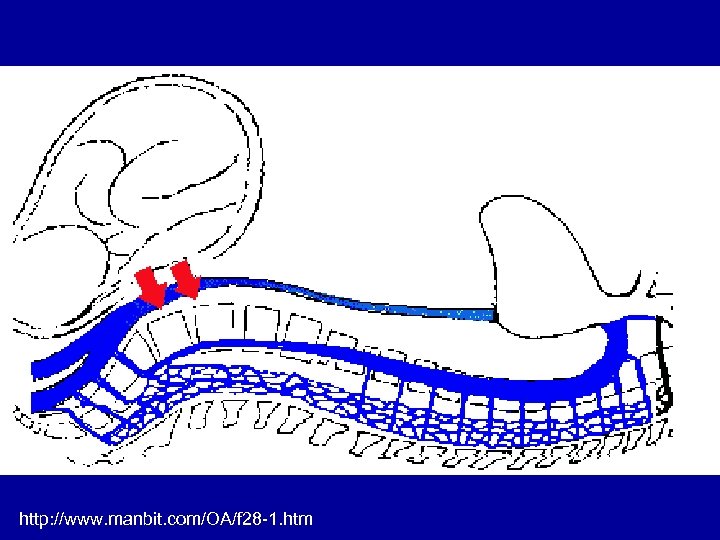
http: //www. manbit. com/OA/f 28 -1. htm
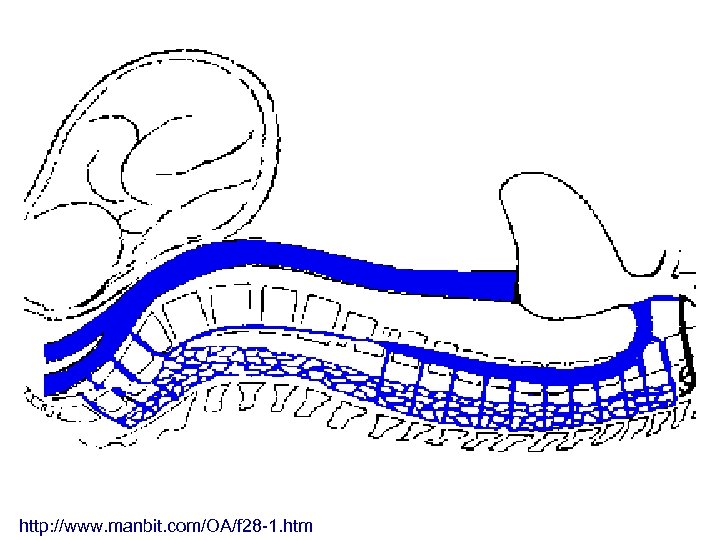
http: //www. manbit. com/OA/f 28 -1. htm Manbit images
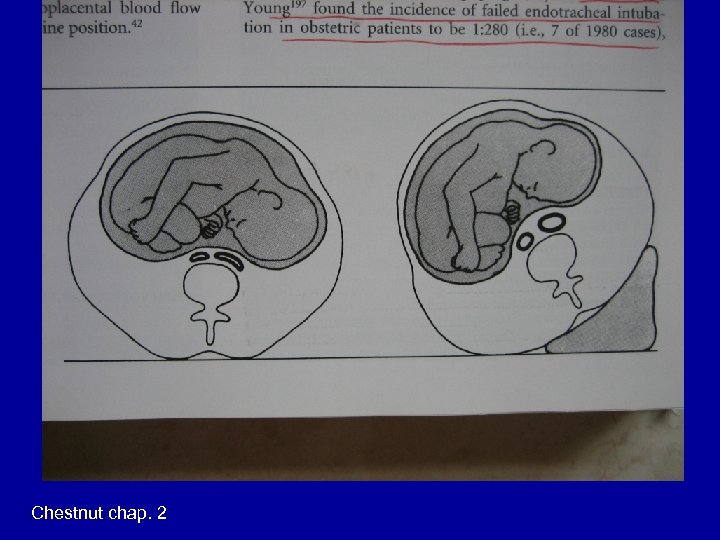
Chestnut chap. 2
What happens if fetus doesn’t get enough oxygen? (What is the mammalian diving response? ) www. doc. govt. nz/. . . /images/diving-whale-tail. jpg
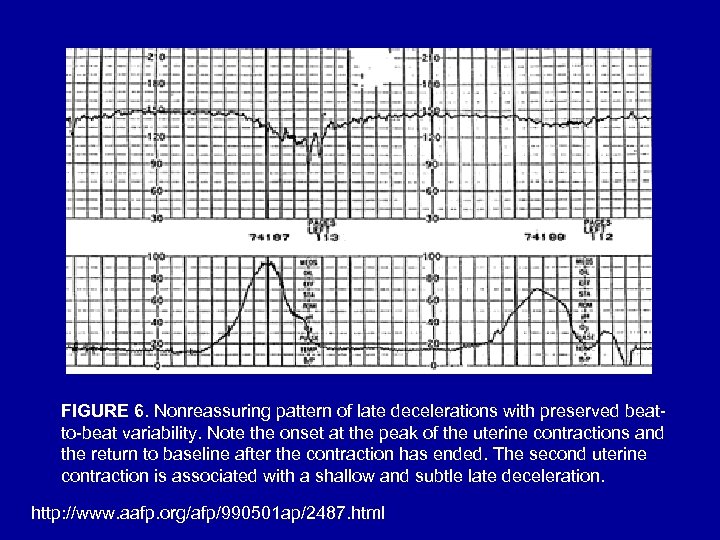
FIGURE 6. Nonreassuring pattern of late decelerations with preserved beatto-beat variability. Note the onset at the peak of the uterine contractions and the return to baseline after the contraction has ended. The second uterine contraction is associated with a shallow and subtle late deceleration. http: //www. aafp. org/afp/990501 ap/2487. html
Humans have diving responses too! Univ of Lund Thesis Johan Andersson http: //www. biol. lu. se/zoof ysiol/Johan/Avhandling. h tml#Sv
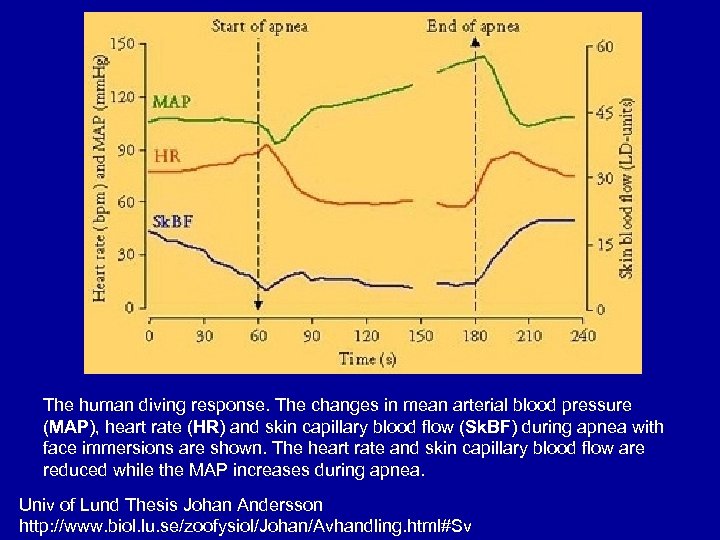
The human diving response. The changes in mean arterial blood pressure (MAP), heart rate (HR) and skin capillary blood flow (Sk. BF) during apnea with face immersions are shown. The heart rate and skin capillary blood flow are reduced while the MAP increases during apnea. Univ of Lund Thesis Johan Andersson http: //www. biol. lu. se/zoofysiol/Johan/Avhandling. html#Sv
The mammalian diving reflex shuts down blood flow to all organs except the heart and brain, in order to conserve oxygen. The fetus’ response to hypoxia is related to this reflex. See Univ of lund thesis Johan Andersson http: //www. biol. lu. se/zoofysiol/Johan/Avhandling. html#Sv
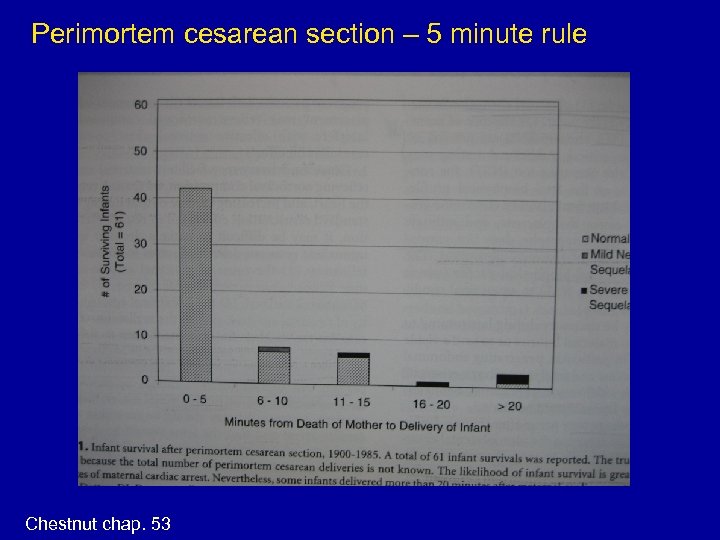
Perimortem cesarean section – 5 minute rule Chestnut chap. 53
Summary • MVAs, falls and assaults are the commonest traumatic mechanisms in pregnancy. • Think of the possibility of domestic violence / partner abuse. • Pregnant women need to wear seat belts properly.
Summary • Don’t over-react to the fact that patient is pregnant. • ACLS and all usual diagnostic studies should be performed. Ultrasound may be useful, but perform needed x-ray studies! • Management of pregnancy is part of secondary survey.
Summary • Abruption is commonest cause of fetal death in non-life-threatening trauma to mother. • Abruption most likely with abdominal trauma. • Abdominal trauma can also cause fetomaternal hemorrhage, uterine rupture, rupture of membranes and pre-term labor.
Summary • Feto-maternal hemorrhage may be a cause of pre-term labor. • KB prep may have value in screening for severe feto-maternal hemorrhage and risk of pre-term labor. • One dose of Rho. Gam is routine in trauma to Rh- mother, regardless of KB results.
Summary • Pregnant women are vulnerable to apnea and have swollen airways. • They may be tolerant of blood loss, with delayed fall in BP. • LUD is important for 3 reasons: – Maternal hemodynamics – Fetal oxygenation – DVT prophylaxis
Summary • Fetal oxygen uptake is proportional to placental blood flow. • The fetus will drop heart rate in response to hypoxia. This is the basis for FHR monitoring after maternal trauma. • This response is related to the “mammalian diving reflex. ”
Summary • To deliver an intact newborn, perimortem cesarean section should deliver baby within 5 minutes of cessation of maternal circulation and oxygenation.
My Website • You can download this talk from: • www. archeranesthesia. info
Thank you! The End
References • Astarita: J Trauma, Volume 42(4). April 1997. 738 -740 • Chestnut DH, Obstetric Anesthesia, Principles and Practice, third edition. • Colman-Brochu S American Journal of Maternal Child Nursing. 29(3): 186 -92, 2004 May-Jun. • El Kady D et al American Journal of Obstetrics and Gynecology (2004) 190, 1661 e 8 • Elovitz MA American Journal of Obstetrics & Gynecology. 185(5): 1059 -63, 2001 Nov. • Ferrara A American Journal of Surgery. 160(5): 515 -8, 1990 Nov. • Judich A Injury, Vol. 29, No. 6, 475 -477, 1998. • Kingston NJ Am J Forensic Med Pathol 2003; 24: 193– 197
References Mann FA et al The Journal of Trauma (2000) Vol. 48, No. 2, pp. 354 -357 Miller MT Journal of Trauma Volume 54(1), January 2003, pp 52 -60 Muench MV J Trauma. 2004; 57: 1094– 1098. Pearlman MD et al American Journal of Obstetrics & Gynecology. 162(6): 1502 -7; discussion 1507 -10, 1990 Jun. Pearlman MD International Journal of Gynecology & Obstetrics 57 (1997) 127 -132 Richards JR Radiology 2004; 233: 463– 470 Shah KH J Trauma Volume 45(1), July 1998, pp 83 -86 Warner MW ANZ J. Surg. 2004; 74: 125– 128
e631cf794b7a293e814153a49c22e2eb.ppt