3d898b4650dc9b1b7c01671be773c591.ppt
- Количество слайдов: 122
The PDD Behavior Inventory (PDDBI)* Ira L. Cohen, Ph. D. Chairman, Psychology Dept. NYS IBR/DD *Cohen and Sudhalter (2005) Psychological Assessment Resources, Inc. 1
PDD Behavior Inventory (PDDBI) Cohen, I. L. , Schmidt-Lackner, S. , Romanczyk, R. , and Sudhalter, V. (2003). The PDD Behavior Inventory: A rating scale for assessing response to intervention in children with PDD. Journal of Autism and Developmental Disorders, 33(1), 31 -45. Cohen, I. L. (2003). Criterion-related validity of the PDD Behavior Inventory. Journal of Autism and Developmental Disorders, 33(1), 47 -53. Cohen, I. L. , and Sudhalter, V. (2005). The PDD Behavior Inventory. Lutz, Fl: Psychological Assessment Resources, Inc. 2
Goals of Workshop • Understanding why the PDDBI was developed and it’s uses • Learning about autism and the related PDDs • Learning about administration and scoring of the PDDBI • Learning about the reliability and validity of the PDDBI • Learning about interpretation of PDDBI score profiles and score discrepancies and their implications for diagnosis and intervention 3
Why was the PDDBI Developed? • I had clinical and research questions that could not easily be answered with rating scales developed to assess autism – Children’s Psychiatric Rating Scale – Childhood Autism Rating Scale – Autism Behavioral Checklist – Behavioral Summarized Evaluation scale – Global Impression-Type Scales (CGI) – Gilliam Autism Rating Scale – Autism Diagnostic Interview-Revised – Autism Diagnostic Observation Schedule-Generic 4
Clinical Questions When a child with autism shows “challenging behaviors”. . • Is it because he or she has autism? (i. e. , other children with autism show similar problems at the same level of intensity) • Is something else going on? (i. e. , child’s behavior is beyond what we would expect or is restricted to certain settings) But there’s a problem • Assessment tools for autism are not standardized on children with autism • Assessment tools for autism are not standardized on different types of informants 5
Research/Clinical Questions When a child is treated with medication and repetitive behaviors decrease. . . • Is there also an improvement in social communication skills? • Is there a decrease in social communication skills? But there’s a problem • Most assessment tools for autism don’t assess the social communication skills that are important in distinguishing children with autism from typically developing children • Instead, they emphasize their problems with communication • None are standardized on well-diagnosed samples and none are age-normed 6
Clinical Questions When a child with autism has difficulty communicating. . • Is it because he or she has autism? (i. e. , other children with autism show similar problems at the same skills level) • Is something else going on? (i. e. , child’s communication is much worse than we would expect or is restricted to certain settings) But there’s a problem • Assessment tools for autism are not age-standardized on children with autism • Assessment tools for autism are not standardized on different types of informants 7
Problems with Existing Assessment Tools 1. Except for the ADI-R and ADOS-G, all of the assessment tools focus exclusively on problem behaviors and do not reflect current research on behaviors that differentiate children with autism from other groups 2. None of the assessment tools are age-normed 3. Only one provides standard scores (GARS) but the diagnostic criteria defining the standardization sample are poorly described 4. Except for the ADI-R and ADOS-G, all focus on behavior problems seen in the more severely affected cases 5. None of the assessment tools are tailored to inputs from teachers/therapists (important for assessing generalization) 8

PDD Behavior Inventory (PDDBI) • The PDDBI can be used to assess response to intervention, assist in diagnosis and treatment planning, and help with research • It: – Assesses both problem behaviors and appropriate social communication behaviors (important in assessing improvement) – Is age-normed (because there is a need to assess change due to age from that due to treatment) – Includes items that are based on the latest research on behaviors that discriminate autism from other conditions – Is standardized on a well-diagnosed autism sample 9
Uses of the PDDBI • Clinical – Assisting in Diagnosis and Treatment Recommendations – Monitoring Changes at Follow-Ups, etc. • Educational – Assisting in Placement Decisions – Assisting in Treatment Planning – Monitoring Students’ Progress, etc. • Research – Measuring Response to Novel Treatments – Identifying Meaningful Sub-Groups – Assessing (Endo)phenotypes in Genetic Studies, etc. 10
Assisting in Diagnosis • Does the child’s profile of domain scores look like someone his/her age with autism? – Is the profile consistent with your observations? – Does the profile suggest an alternate and/or “comorbid” diagnosis that needs to be considered (diagnostic overshadowing? )? • Do the domain profiles of parent and “teacher” agree? – If not, which scores differ? – If they differ, does this say something about diagnosis (e. g. , Selective Mutism)? 11
Assisting in Placement Decisions • Is the child’s problem behavior profile typical of someone his/her age with autism? – If not, are some scores so high that a special treatment setting may be necessary? 12
Treatment Planning • Is the child’s “social-communication” behavior profile typical of someone his/her age with autism? – If not, do domain scores suggest some other diagnosis should be considered, e. g. , Asperger’s? 13

Research • The PDDBI can be helpful and is being used for measuring meaningful change as a result of intervention (e. g. , medication, ABA, dietary, etc. ) for people in the autism spectrum – For groups (e. g. , Are people in my school improving? ; Is my intervention associated with improvement? ) – For individuals (Has this person improved? ) • If so, in what areas? • If so, is it a meaningful decrease in autism traits? • It is also being used in large scale genetics studies to identify genes associated with certain types of autistic behaviors 14
Some Research Programs Using PDDBI • • • • • Arizona State University Arkansas Children’s Hospital Research Unit ASD-Canadian American Research Consortium Baylor College of Medicine Binghamton University Carlos Albizu University Cleveland Clinic Center for Autism Columbia University - Psychiatric Institute Massachusetts General Hospital M. I. N. D. Institute Mount Sinai Hospital – Seaver Center (Manhattan) National Institute of Mental Health (NIMH) Ohio State University Royal Prince Alfred Hospital, Sydney, Australia St. Mary’s Hospital (Wisconsin) University of California San Diego University of Illinois University of North Carolina – Chapel Hill Washington State University 15
PDDBI • As will be shown, we have found the PDDBI to be both reliable and valid • It can be used for assessing children on the autism spectrum who are between 18 months and 12 -1/2 years of age 16

Autism and the Related PDDs 17
http: //www. time. com/time/covers/1101030120 18
Autism and the Related PDDs 19

Earliest Description of Autism? “If a woman gives birth and the infant rejects the mother” Summa Izbu IV 42 Ancient Mesopotamian medical text (translated by M. Coleman, M. D. ) 20
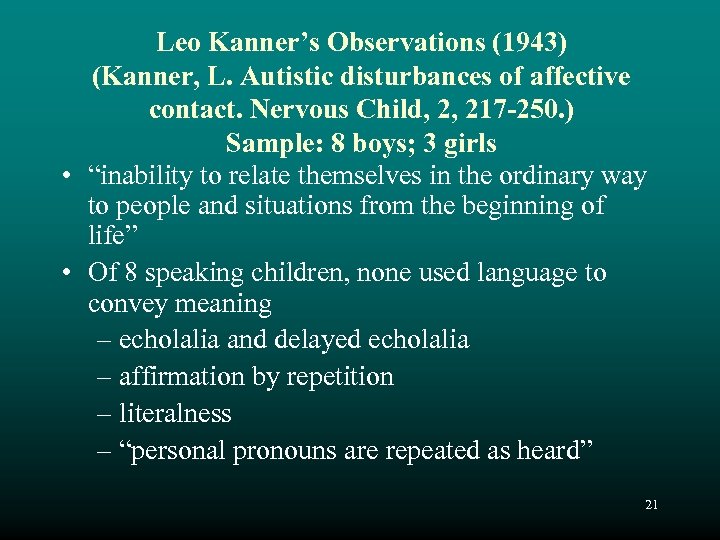
Leo Kanner’s Observations (1943) (Kanner, L. Autistic disturbances of affective contact. Nervous Child, 2, 217 -250. ) Sample: 8 boys; 3 girls • “inability to relate themselves in the ordinary way to people and situations from the beginning of life” • Of 8 speaking children, none used language to convey meaning – echolalia and delayed echolalia – affirmation by repetition – literalness – “personal pronouns are repeated as heard” 21
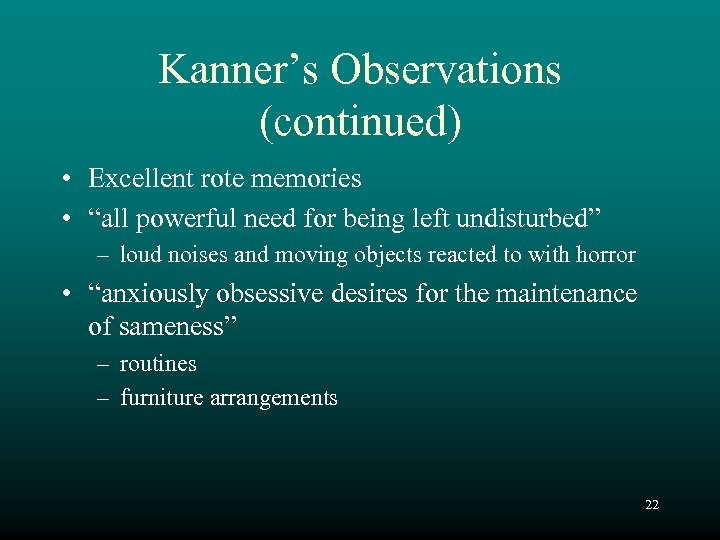
Kanner’s Observations (continued) • Excellent rote memories • “all powerful need for being left undisturbed” – loud noises and moving objects reacted to with horror • “anxiously obsessive desires for the maintenance of sameness” – routines – furniture arrangements 22
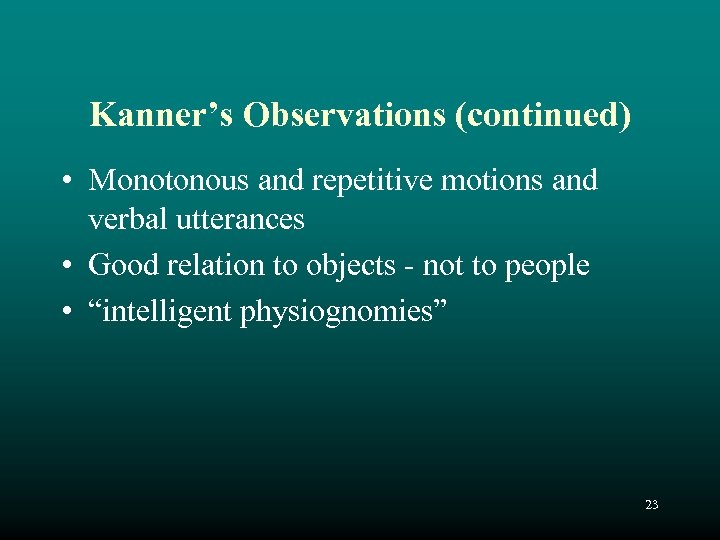
Kanner’s Observations (continued) • Monotonous and repetitive motions and verbal utterances • Good relation to objects - not to people • “intelligent physiognomies” 23
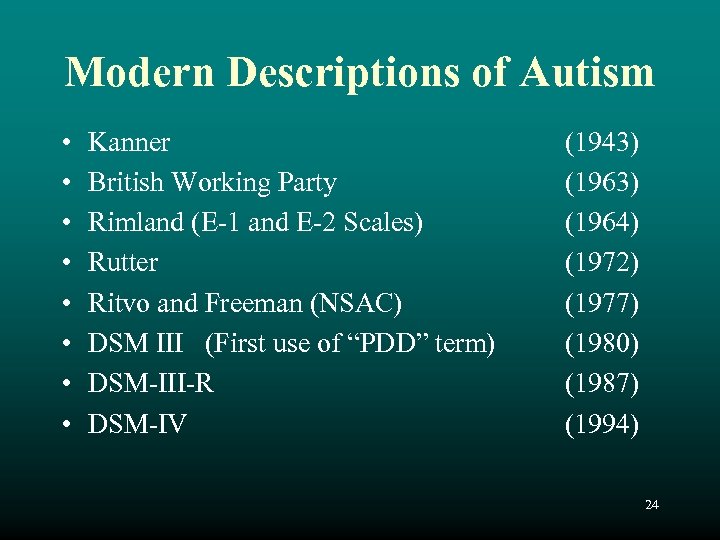
Modern Descriptions of Autism • • Kanner British Working Party Rimland (E-1 and E-2 Scales) Rutter Ritvo and Freeman (NSAC) DSM III (First use of “PDD” term) DSM-III-R DSM-IV (1943) (1964) (1972) (1977) (1980) (1987) (1994) 24
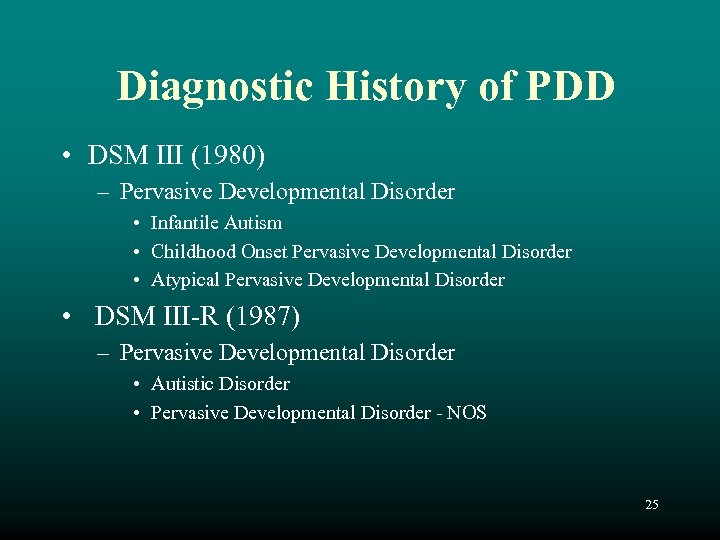
Diagnostic History of PDD • DSM III (1980) – Pervasive Developmental Disorder • Infantile Autism • Childhood Onset Pervasive Developmental Disorder • Atypical Pervasive Developmental Disorder • DSM III-R (1987) – Pervasive Developmental Disorder • Autistic Disorder • Pervasive Developmental Disorder - NOS 25
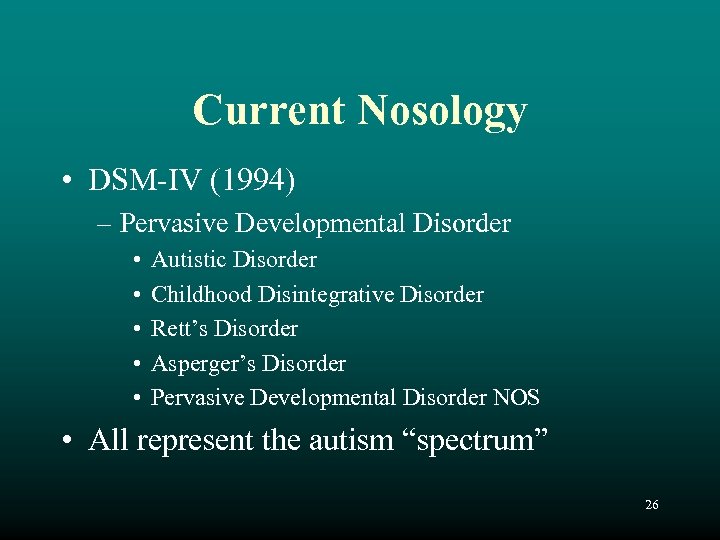
Current Nosology • DSM-IV (1994) – Pervasive Developmental Disorder • • • Autistic Disorder Childhood Disintegrative Disorder Rett’s Disorder Asperger’s Disorder Pervasive Developmental Disorder NOS • All represent the autism “spectrum” 26
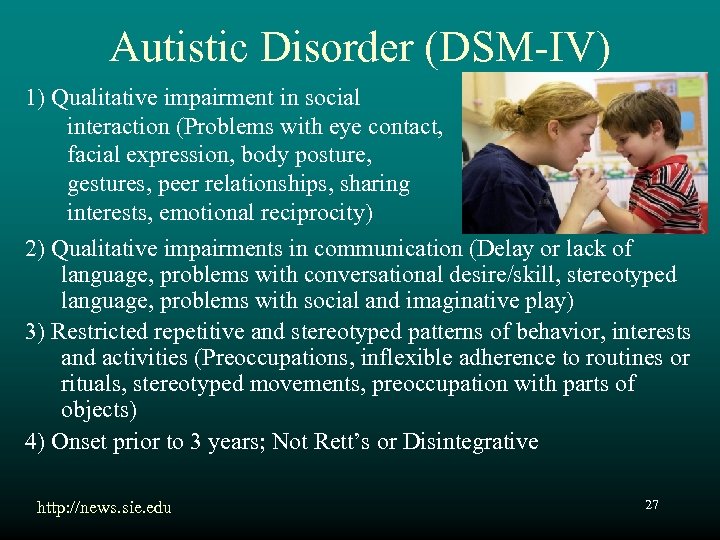
Autistic Disorder (DSM-IV) 1) Qualitative impairment in social interaction (Problems with eye contact, facial expression, body posture, gestures, peer relationships, sharing interests, emotional reciprocity) 2) Qualitative impairments in communication (Delay or lack of language, problems with conversational desire/skill, stereotyped language, problems with social and imaginative play) 3) Restricted repetitive and stereotyped patterns of behavior, interests and activities (Preoccupations, inflexible adherence to routines or rituals, stereotyped movements, preoccupation with parts of objects) 4) Onset prior to 3 years; Not Rett’s or Disintegrative http: //news. sie. edu 27

Candle fixation at birthdays 28
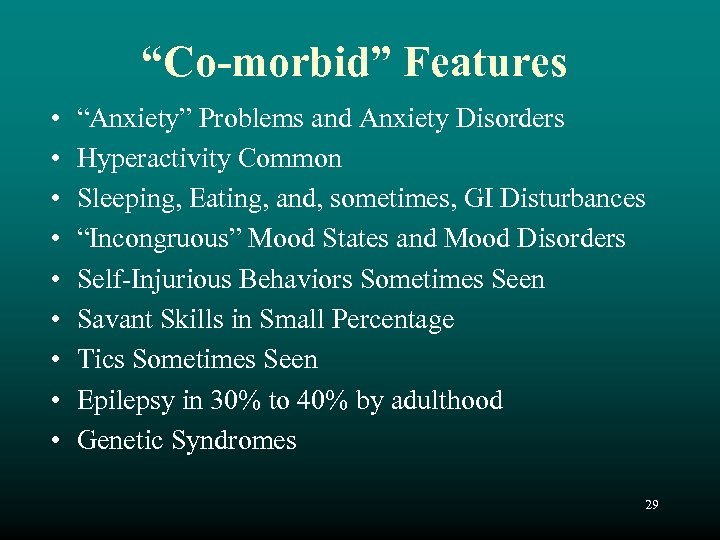
“Co-morbid” Features • • • “Anxiety” Problems and Anxiety Disorders Hyperactivity Common Sleeping, Eating, and, sometimes, GI Disturbances “Incongruous” Mood States and Mood Disorders Self-Injurious Behaviors Sometimes Seen Savant Skills in Small Percentage Tics Sometimes Seen Epilepsy in 30% to 40% by adulthood Genetic Syndromes 29
PDD-NOS • Also known as “Atypical Autism” – Criteria not met for one of the other PDDs due to age of onset, or atypical symptoms, or subthreshold symptoms or all of these – There is severe and pervasive impairment in development of reciprocal social interaction skills and impairment in communication skills OR presence of stereotyped behaviors, interests, and activities 30

? Asperger’s Disorder • Same characteristics as Autistic Disorder, but: “Jerry Espenson” “Boston Legal” – No general language delay (single words by 2 years; communicative phrases by 3 years) – No delay in cognitive development or self-help skills or curiosity about the environment • Not other PDD or schizophrenia ? 31

Rett’s Disorder • • • Normal pre- and peri-natal development Normal psychomotor development up to 5 mos. Normal HC at birth-HC deceleration 5 -48 mos. Loss of purposeful hand skills (hand wringing) Loss of social engagement Poorly coordinated gait and trunk movements Severe language disorder and retardation Breathing abnormalities common Due to MECP 2 gene mutation absence of MECP 2 protein absence of gene suppression – “Leaky genes” http: //www. rettsyndrome. org. uk 32

Childhood Disintegrative Disorder • Normal development first 2 years • Loss of skills before 10 years in at least 2: – – – Expressive or receptive language Social or adaptive skills Bowel/bladder control Play Motor skills • Abnormalities in at least 2: – Qualitative social interaction – Qualitative impairment in communication – Repetitive behaviors, restricted interests • Not other PDD or schizophrenia 33
Differential Diagnosis Issues • • • Receptive-Expressive Language Disorder Mental Retardation without PDD ADHD Deafness/Hearing Impairment Selective Mutism Reactive Attachment Disorder 34
Autism/PDD-NOS Characteristics • Most are males (about 75%-50%) • Developmental delay is common (about 70%) • Parents recognize problems around 18 months, sometimes with loss of skills • Enlarged head circumference sometimes seen in younger children (about 37%) • Genes play a strong role in etiology 35
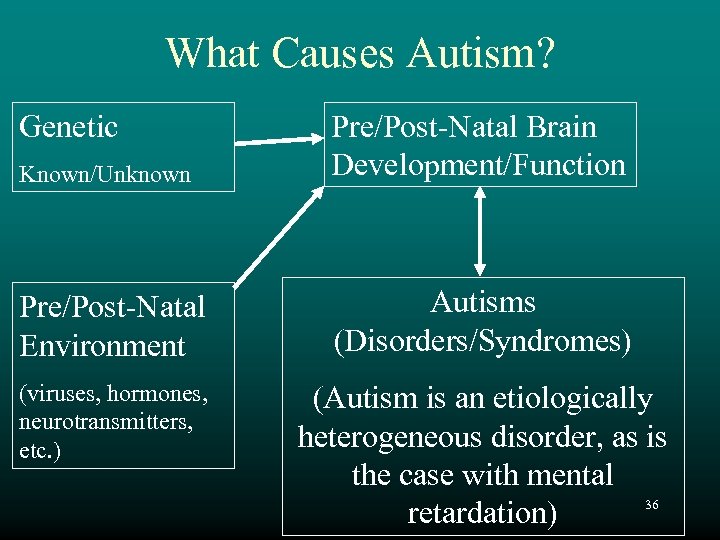
What Causes Autism? Genetic Known/Unknown Pre/Post-Natal Brain Development/Function Pre/Post-Natal Environment Autisms (Disorders/Syndromes) (viruses, hormones, neurotransmitters, etc. ) (Autism is an etiologically heterogeneous disorder, as is the case with mental 36 retardation)
Known Genetic Conditions Associated With Autism • Fragile X Syndrome – About 2 to 8 % in males or females with autism – About 15 % of fragile X males have autism • Other Genetic Disorders/Conditions – Untreated Phenylketonuria (PKU) – Tuberous Sclerosis in about 3% of cases – Angelman’s Syndrome – Chromosome 15 q 11 -13 Duplications (maternal origin) (Cook, et al. , 1997) - Same region as Prader-Willi (maternal) and Angelman’s 37 (paternal) Deletion Syndromes

Genetics of Autism • Twin studies (Bailey, et al 1995) – 60% concordance for autism in 25 MZ twins; None in DZ – 92% concordance for cognitive impairment in MZ twins; 10% in DZ twins 38
The Broader Phenotype • Autism, per se, may not be inherited • Rather, there appears to be a Spectrum of social and language problems inherited in some families. 39
Genetic Factors in Autism • Family Studies – – Risk of Autism in siblings of proband 5% to 9% Risk of Autism itself in the population: about 0. 5% Risk of Asperger’s or PDDNOS in siblings ~ 3% Risk of other social or communication impairments or restricted interests ~20% in siblings • Risk of Mood Disorders is elevated in family (siblings, parents, extended family) 40
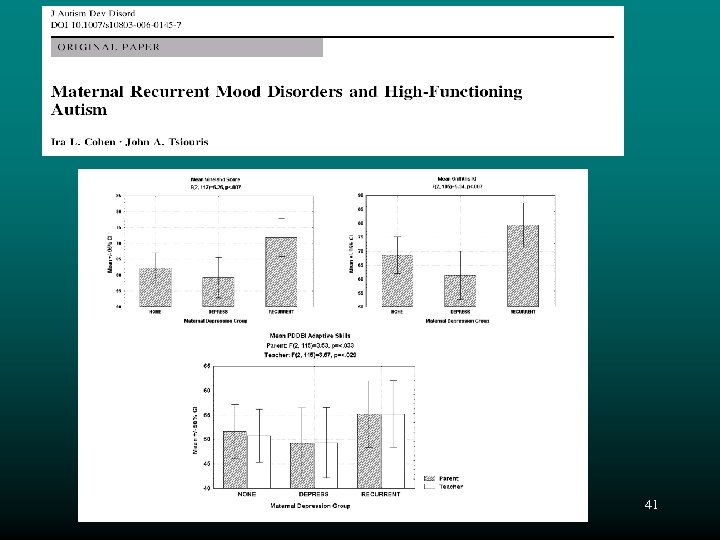
41
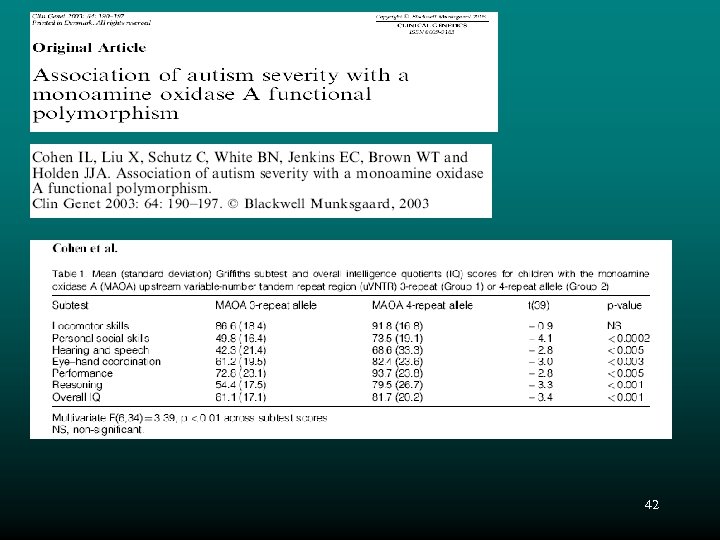
42
Other Medical Issues • There is very little evidence for the role of the following in causing autism: – Heavy metals such as mercury – Vaccines such as MMR and DPT – Gastro-intestinal problems • Many of these issues are currently being investigated at various centers • The role of immune system problems and CNS inflammation in autism are also major questions 43
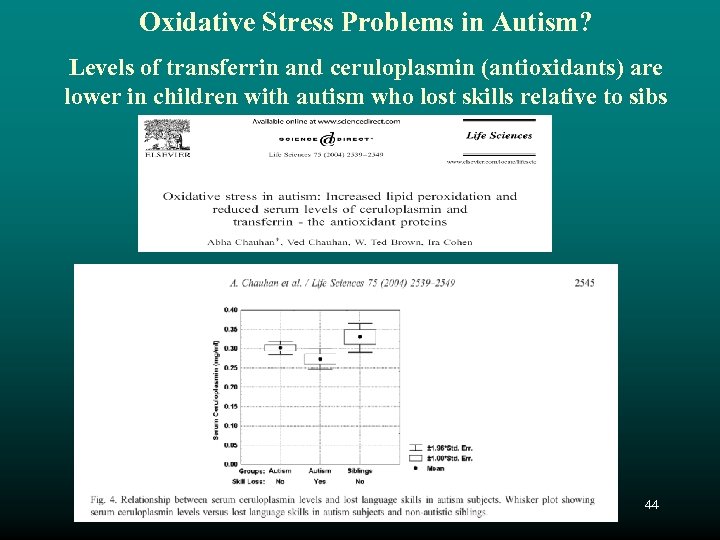
Oxidative Stress Problems in Autism? Levels of transferrin and ceruloplasmin (antioxidants) are lower in children with autism who lost skills relative to sibs 44
Administration and Scoring 45

Administration • Can be completed at home, school, or clinician’s office (should be free from distractions) • Ensure confidentiality in reporting • Clinician should indicate with an X or check mark whether informant is to complete standard or extended form – Standard: if primary concern is with autism diagnosisrelated behaviors (e. g. , prevalence studies) – Extended: if concern is with autism behaviors and more generic behavior issues 46
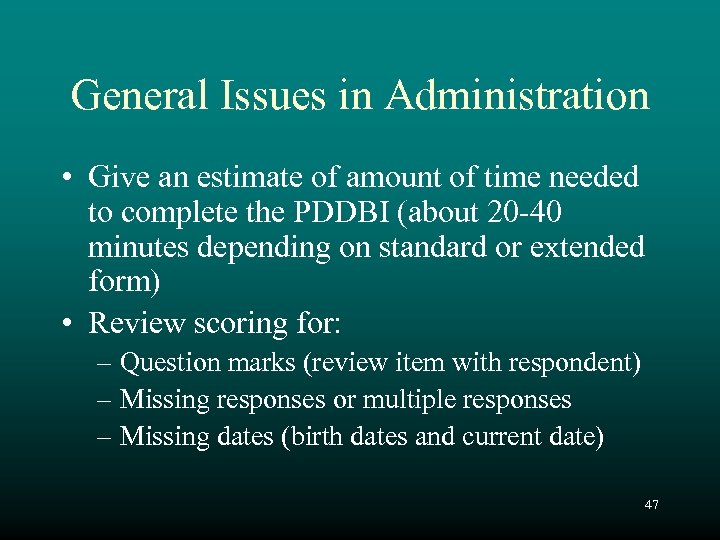
General Issues in Administration • Give an estimate of amount of time needed to complete the PDDBI (about 20 -40 minutes depending on standard or extended form) • Review scoring for: – Question marks (review item with respondent) – Missing responses or multiple responses – Missing dates (birth dates and current date) 47
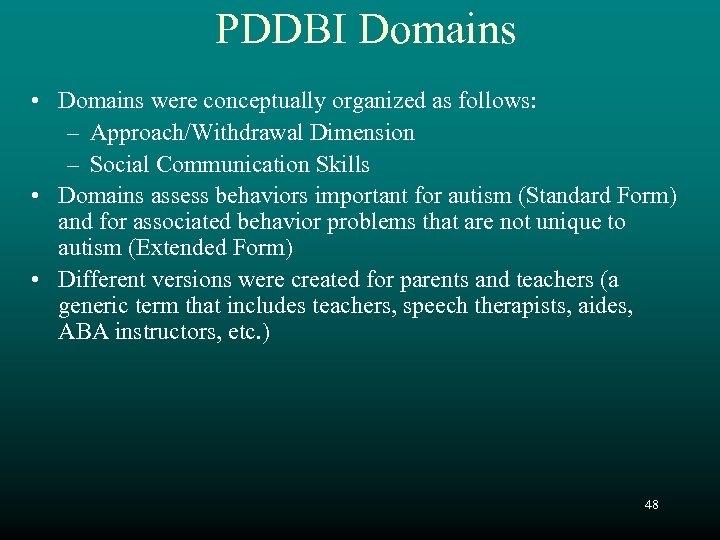
PDDBI Domains • Domains were conceptually organized as follows: – Approach/Withdrawal Dimension – Social Communication Skills • Domains assess behaviors important for autism (Standard Form) and for associated behavior problems that are not unique to autism (Extended Form) • Different versions were created for parents and teachers (a generic term that includes teachers, speech therapists, aides, ABA instructors, etc. ) 48
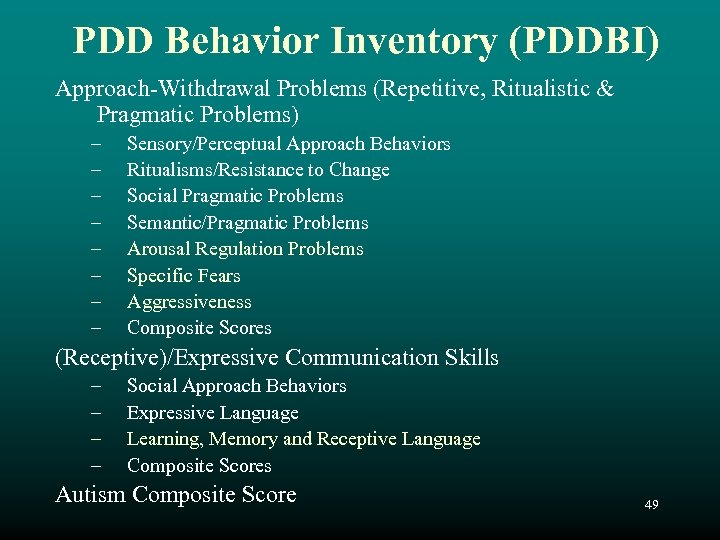
PDD Behavior Inventory (PDDBI) Approach-Withdrawal Problems (Repetitive, Ritualistic & Pragmatic Problems) – – – – Sensory/Perceptual Approach Behaviors Ritualisms/Resistance to Change Social Pragmatic Problems Semantic/Pragmatic Problems Arousal Regulation Problems Specific Fears Aggressiveness Composite Scores (Receptive)/Expressive Communication Skills – – Social Approach Behaviors Expressive Language Learning, Memory and Receptive Language Composite Scores Autism Composite Score 49
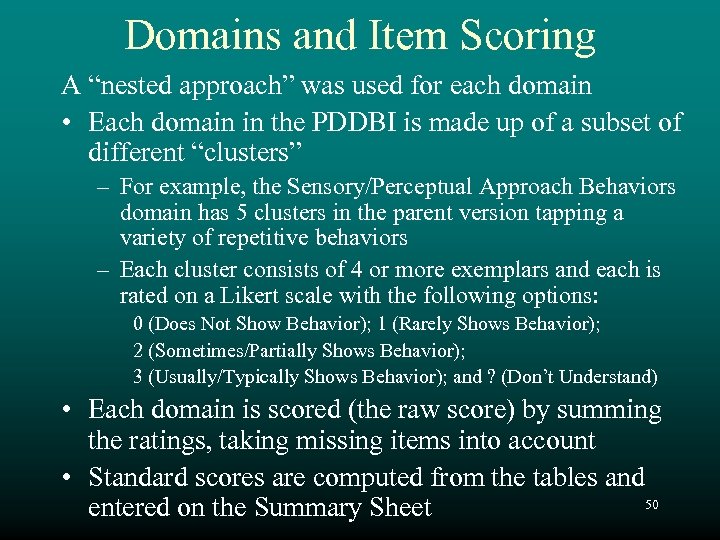
Domains and Item Scoring A “nested approach” was used for each domain • Each domain in the PDDBI is made up of a subset of different “clusters” – For example, the Sensory/Perceptual Approach Behaviors domain has 5 clusters in the parent version tapping a variety of repetitive behaviors – Each cluster consists of 4 or more exemplars and each is rated on a Likert scale with the following options: 0 (Does Not Show Behavior); 1 (Rarely Shows Behavior); 2 (Sometimes/Partially Shows Behavior); 3 (Usually/Typically Shows Behavior); and ? (Don’t Understand) • Each domain is scored (the raw score) by summing the ratings, taking missing items into account • Standard scores are computed from the tables and 50 entered on the Summary Sheet
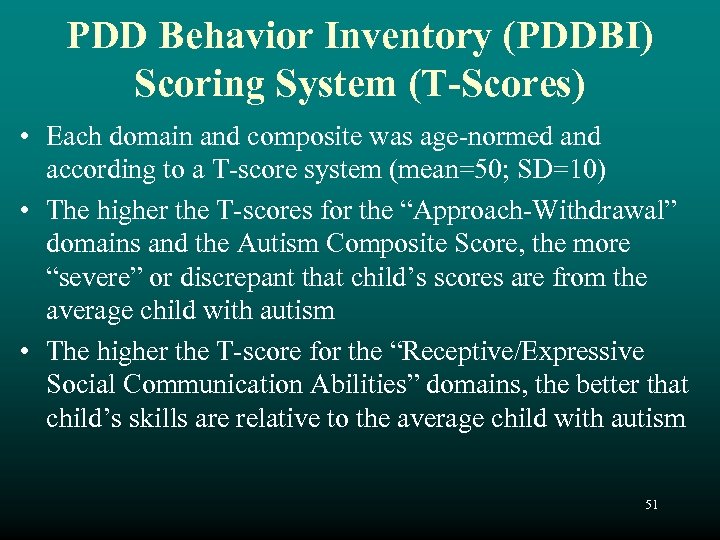
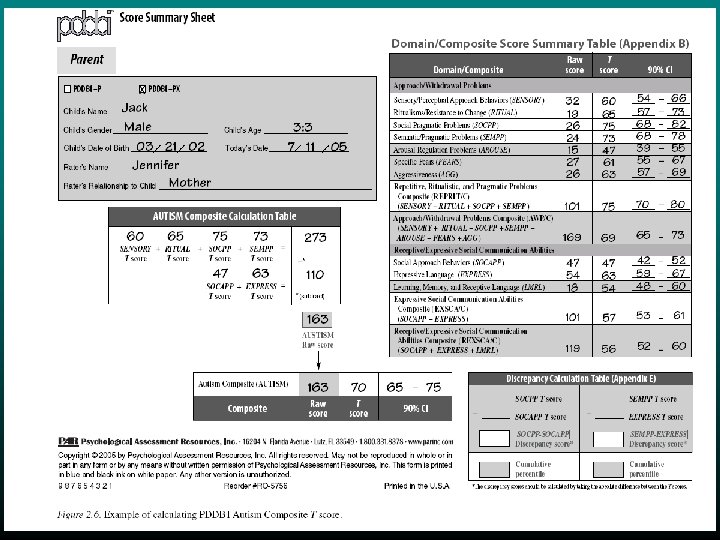
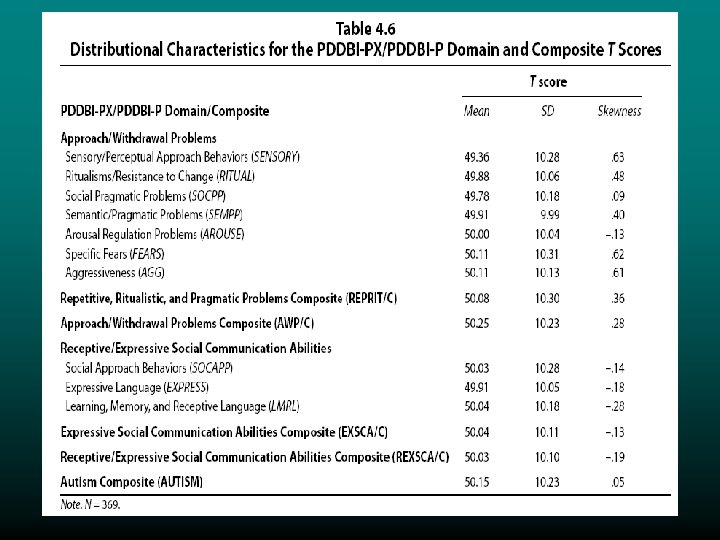
PDD Behavior Inventory (PDDBI) Scoring System (T-Scores) • Each domain and composite was age-normed and according to a T-score system (mean=50; SD=10) • The higher the T-scores for the “Approach-Withdrawal” domains and the Autism Composite Score, the more “severe” or discrepant that child’s scores are from the average child with autism • The higher the T-score for the “Receptive/Expressive Social Communication Abilities” domains, the better that child’s skills are relative to the average child with autism 51
52
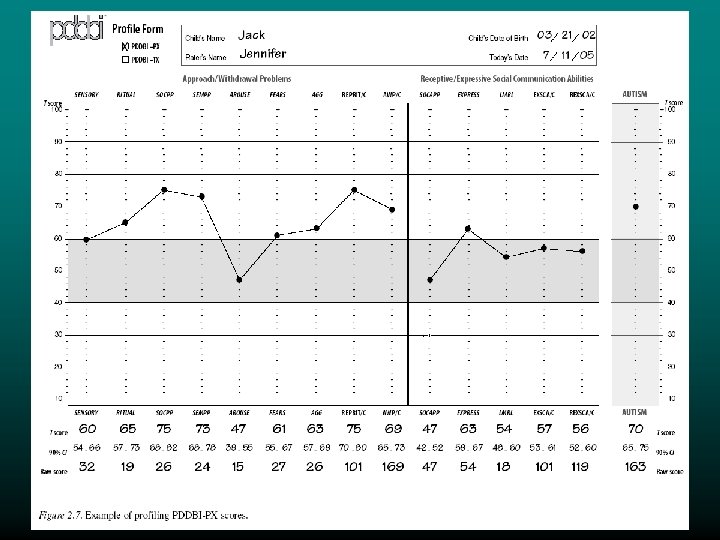
Domain Profile Form • Standardized T-scores (refer to tables or software) can be plotted on the Profile Form 53
54
Cluster Score Summary Table • Cluster scores within domains can be qualitatively examined along an ordinal dimension for their clinical importance 55
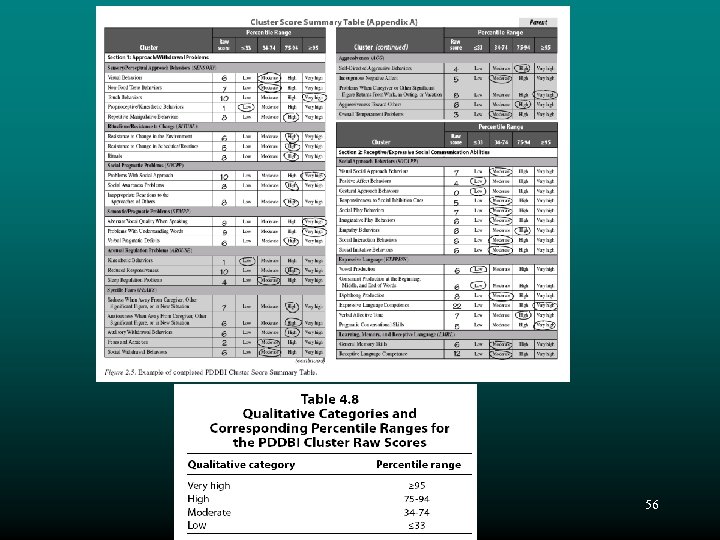
56
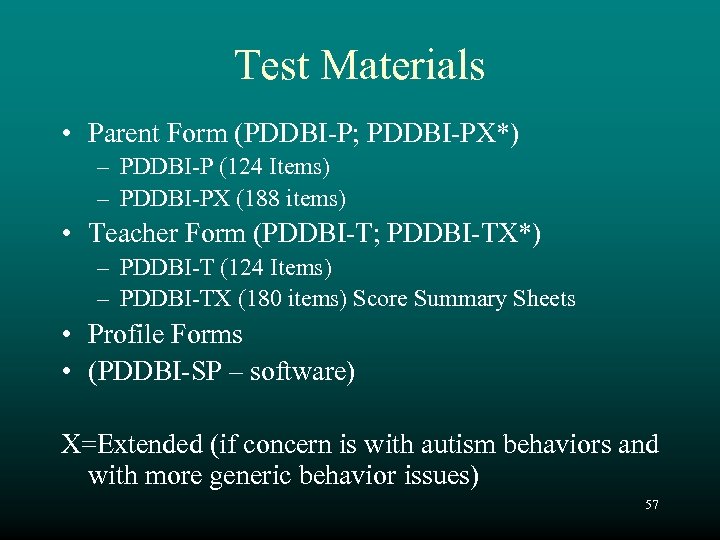
Test Materials • Parent Form (PDDBI-P; PDDBI-PX*) – PDDBI-P (124 Items) – PDDBI-PX (188 items) • Teacher Form (PDDBI-T; PDDBI-TX*) – PDDBI-T (124 Items) – PDDBI-TX (180 items) Score Summary Sheets • Profile Forms • (PDDBI-SP – software) X=Extended (if concern is with autism behaviors and with more generic behavior issues) 57

Appropriate Populations • Any child with a Pervasive Developmental Disorder • Ages 18 months through 12 years, 5 months • English speaking informants – Flesch-Kincaid Reading Level – Grade 4. 7 – Gunning Fog Index – 7. 8 (“Reader’s Digest” level) 58
Selecting Raters • Parent – Parent or legal guardian with the most recent and frequent contact over the previous 6 months (ideally both parents) • Teacher – Teacher or other professional (speech therapist; teacher’s aide, etc. ) must have had at least daily contact for at least one month or more than 4 weeks of several days per week contact 59
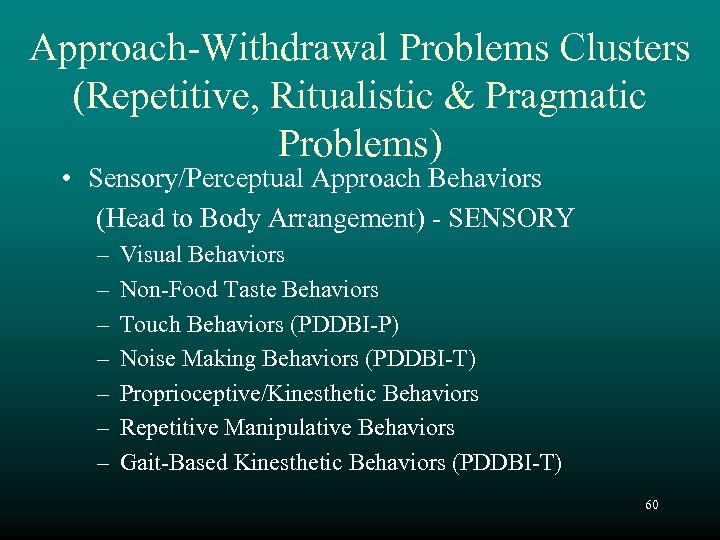
Approach-Withdrawal Problems Clusters (Repetitive, Ritualistic & Pragmatic Problems) • Sensory/Perceptual Approach Behaviors (Head to Body Arrangement) - SENSORY – – – – Visual Behaviors Non-Food Taste Behaviors Touch Behaviors (PDDBI-P) Noise Making Behaviors (PDDBI-T) Proprioceptive/Kinesthetic Behaviors Repetitive Manipulative Behaviors Gait-Based Kinesthetic Behaviors (PDDBI-T) 60
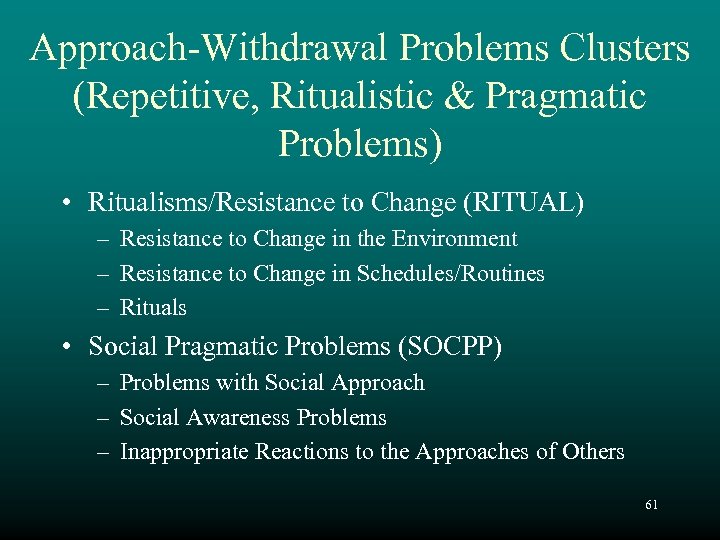
Approach-Withdrawal Problems Clusters (Repetitive, Ritualistic & Pragmatic Problems) • Ritualisms/Resistance to Change (RITUAL) – Resistance to Change in the Environment – Resistance to Change in Schedules/Routines – Rituals • Social Pragmatic Problems (SOCPP) – Problems with Social Approach – Social Awareness Problems – Inappropriate Reactions to the Approaches of Others 61
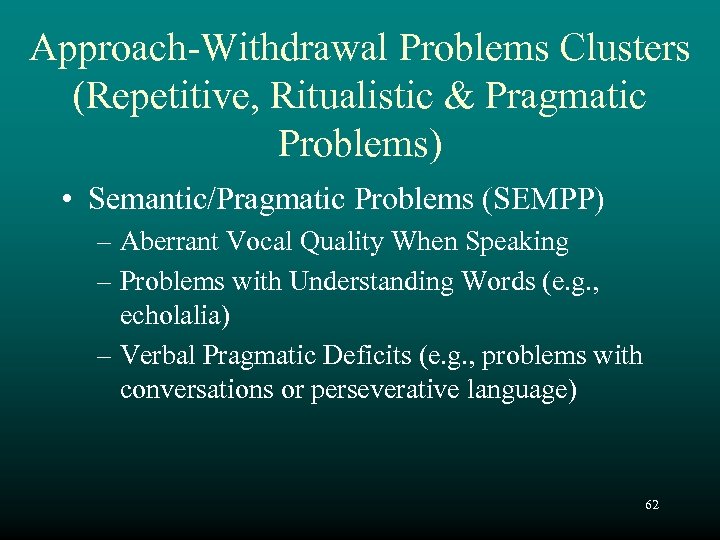
Approach-Withdrawal Problems Clusters (Repetitive, Ritualistic & Pragmatic Problems) • Semantic/Pragmatic Problems (SEMPP) – Aberrant Vocal Quality When Speaking – Problems with Understanding Words (e. g. , echolalia) – Verbal Pragmatic Deficits (e. g. , problems with conversations or perseverative language) 62
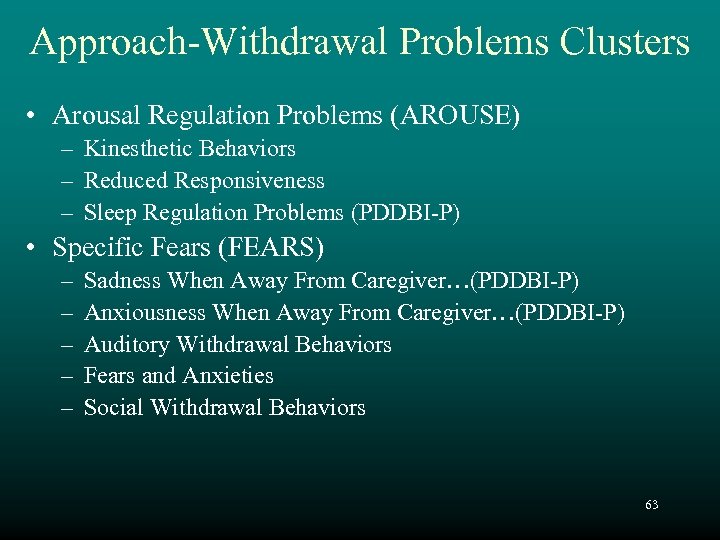
Approach-Withdrawal Problems Clusters • Arousal Regulation Problems (AROUSE) – Kinesthetic Behaviors – Reduced Responsiveness – Sleep Regulation Problems (PDDBI-P) • Specific Fears (FEARS) – – – Sadness When Away From Caregiver…(PDDBI-P) Anxiousness When Away From Caregiver…(PDDBI-P) Auditory Withdrawal Behaviors Fears and Anxieties Social Withdrawal Behaviors 63
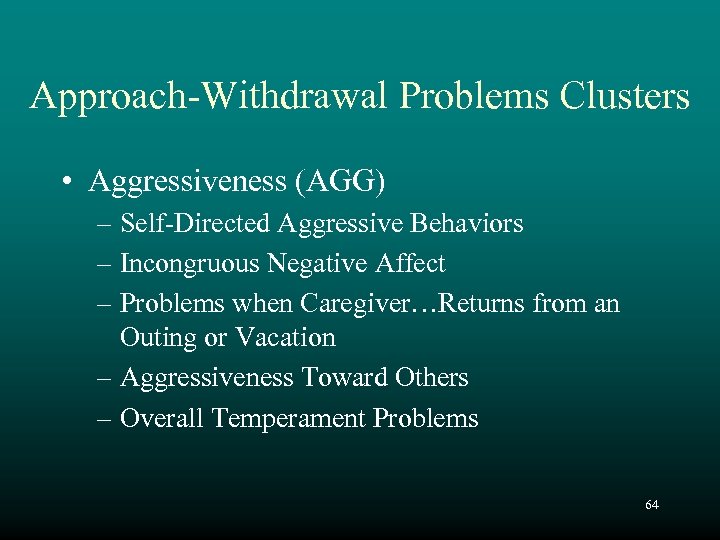
Approach-Withdrawal Problems Clusters • Aggressiveness (AGG) – Self-Directed Aggressive Behaviors – Incongruous Negative Affect – Problems when Caregiver…Returns from an Outing or Vacation – Aggressiveness Toward Others – Overall Temperament Problems 64
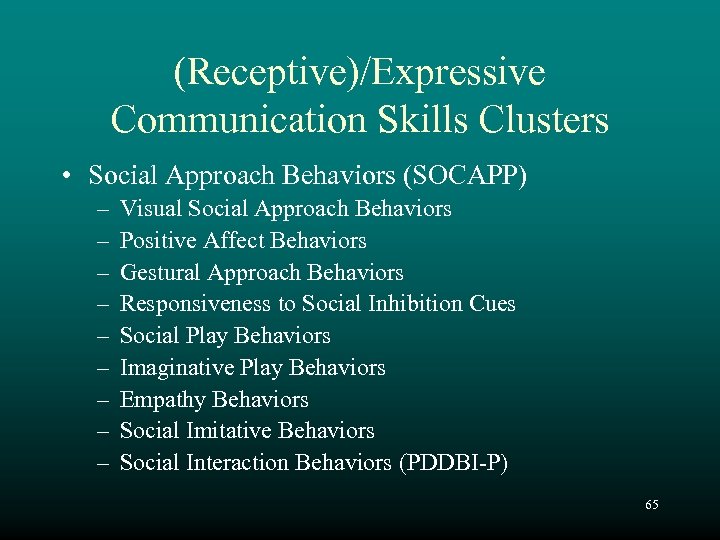
(Receptive)/Expressive Communication Skills Clusters • Social Approach Behaviors (SOCAPP) – – – – – Visual Social Approach Behaviors Positive Affect Behaviors Gestural Approach Behaviors Responsiveness to Social Inhibition Cues Social Play Behaviors Imaginative Play Behaviors Empathy Behaviors Social Imitative Behaviors Social Interaction Behaviors (PDDBI-P) 65
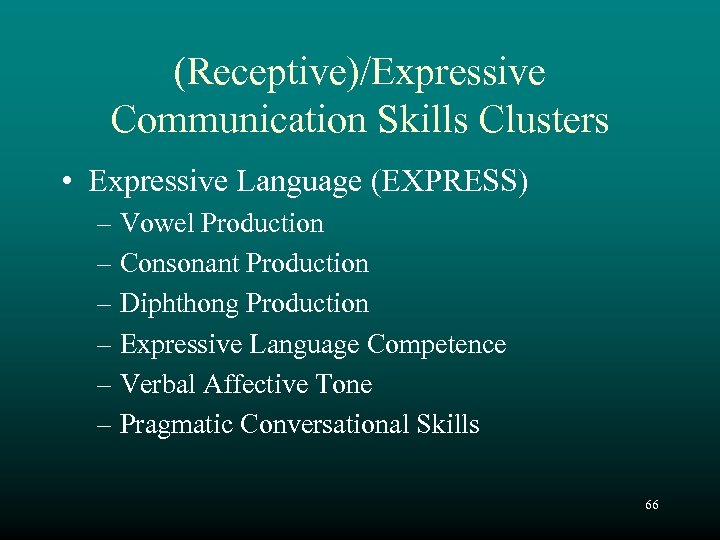
(Receptive)/Expressive Communication Skills Clusters • Expressive Language (EXPRESS) – Vowel Production – Consonant Production – Diphthong Production – Expressive Language Competence – Verbal Affective Tone – Pragmatic Conversational Skills 66

Receptive/Expressive Communication Skills Clusters • Learning, Memory, and Receptive Language (LMRL) – General Memory Skills – Receptive Language Competence – Associative Learning (PDDBI-T) 67

Composite Scores • Approach-Withdrawal Problems (AWP) • Repetitive, Ritualistic & Pragmatic Problems (REPRIT) • Receptive/Expressive Social Communication Skills (REXSCA) • Expressive Social Communication Skills (EXSCA) • Autism (SENSORY+RITUAL+SOCPP+SEMPP) – (SOCAPP + EXPRESS) 68

Discrepancy Scores • Social Pragmatic Problems – Social Approach Behaviors • Semantic/Pragmatic Problems – Expressive Language • Parent - Teacher 69
Development and Standardization 70
“You can observe a lot by just watching” Yogi Berra 71
Development • Items were selected based on observation and by review of research studies • The items were chosen to best represent the cluster to which they were assigned 72
73
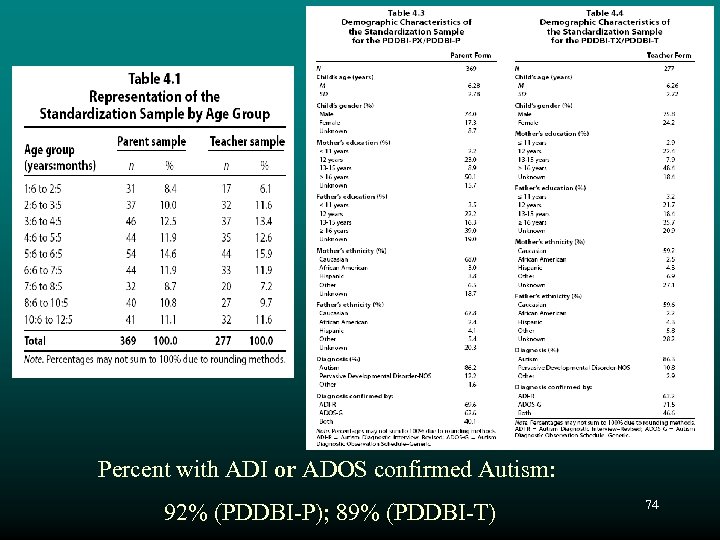
Percent with ADI or ADOS confirmed Autism: 92% (PDDBI-P); 89% (PDDBI-T) 74
Reliability • Internal Consistency (Alpha) • Stability (Test-Retest) • Interrater 75
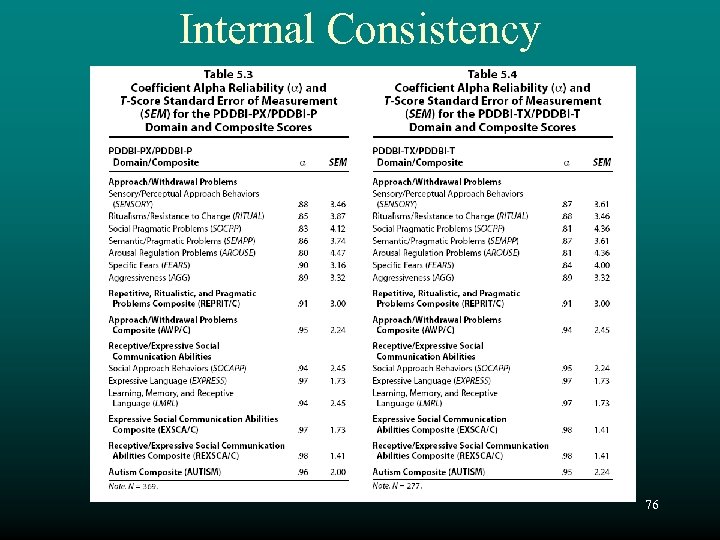
Internal Consistency 76

Internal Consistency G. Leonard Burns, Ph. D. , Washington State University, Pullman, WA Mother Approach-Withdrawal Problems Receptive/Expressive ……… Father (. 81 -. 90) (. 85 -. 92) (. 83 -. 90) * (. 92 -. 98) (. 94 -. 98) (. 91 -. 95) * Teacher Aide (. 82 -. 92) (. 81 -. 89)* (. 95 -. 99) (. 93 -. 95) (. 95 -. 97)* *PDDBI Manual Data 77
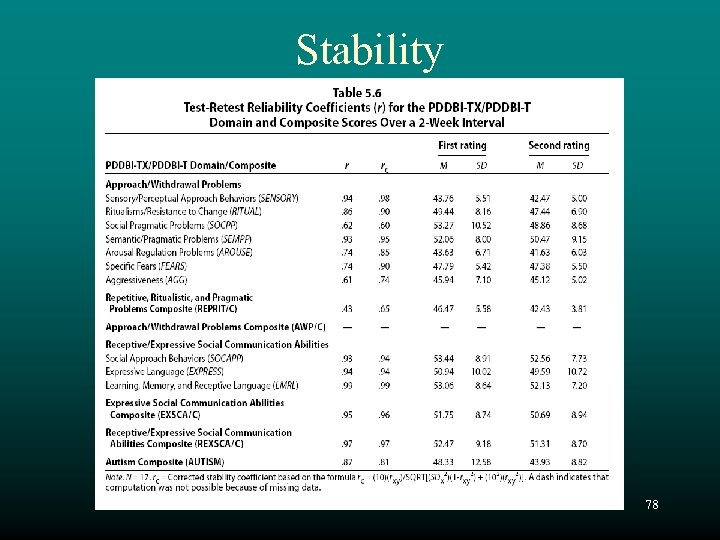
Stability 78
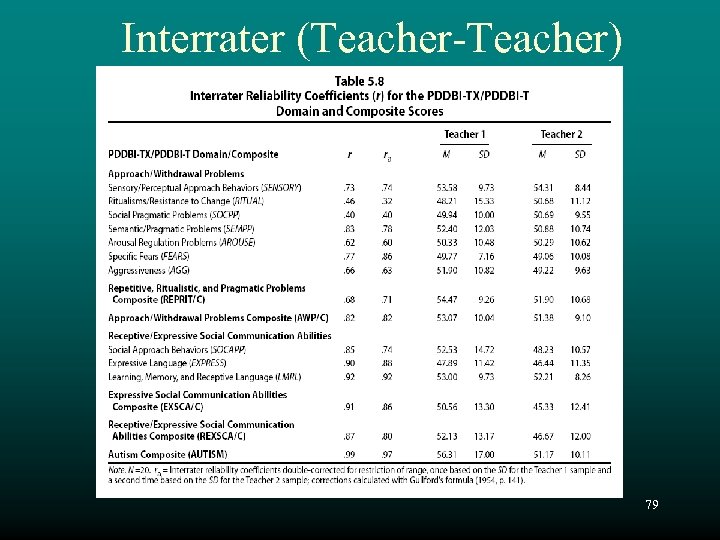
Interrater (Teacher-Teacher) 79
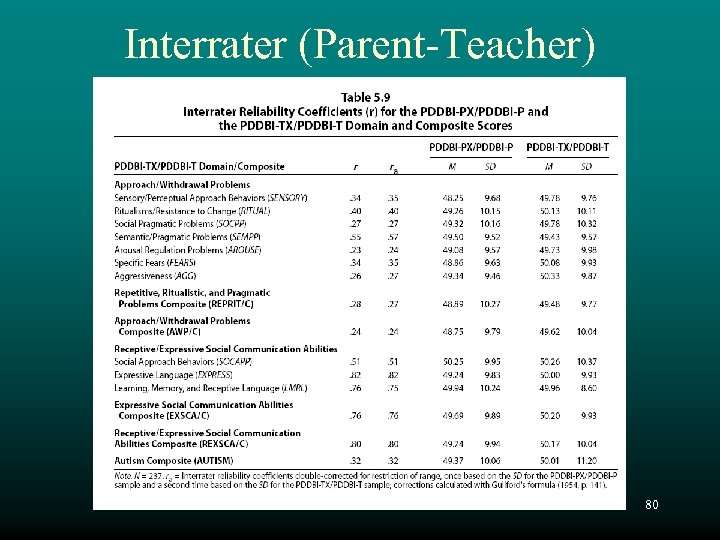
Interrater (Parent-Teacher) 80
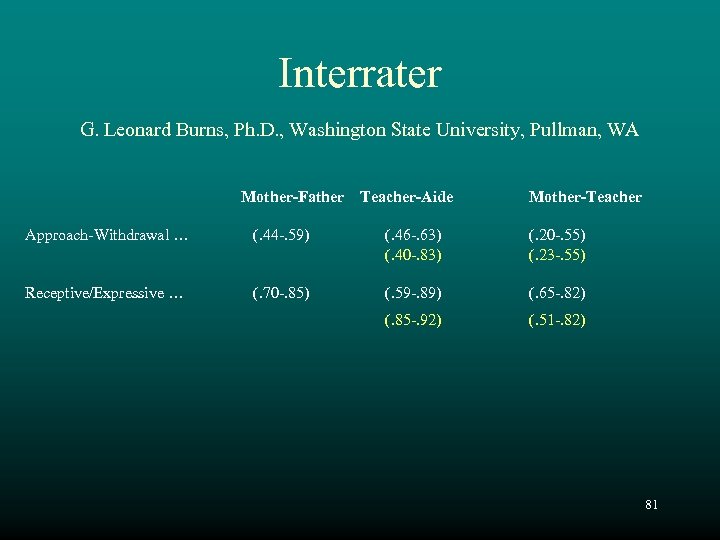
Interrater G. Leonard Burns, Ph. D. , Washington State University, Pullman, WA Mother-Father Teacher-Aide Mother-Teacher Approach-Withdrawal … (. 44 -. 59) (. 46 -. 63) (. 40 -. 83) (. 20 -. 55) (. 23 -. 55) Receptive/Expressive … (. 70 -. 85) (. 59 -. 89) (. 65 -. 82) (. 85 -. 92) (. 51 -. 82) 81
Validity • • • Internal Structure (intercorrelation matrices) Construct (principal components analyses) Developmental Criterion-Related Clinical 82

Internal Structure 83
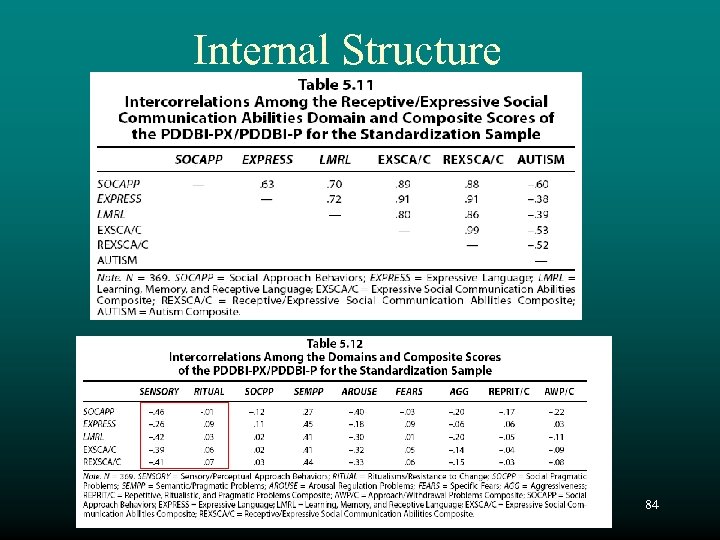
Internal Structure 84
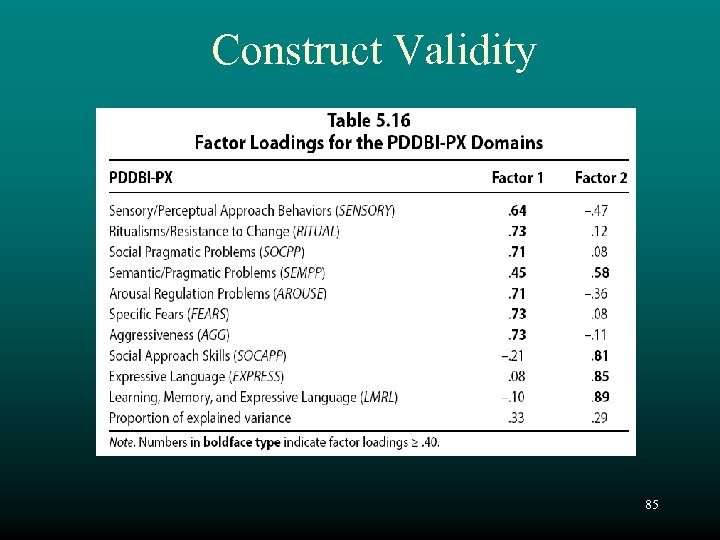
Construct Validity 85
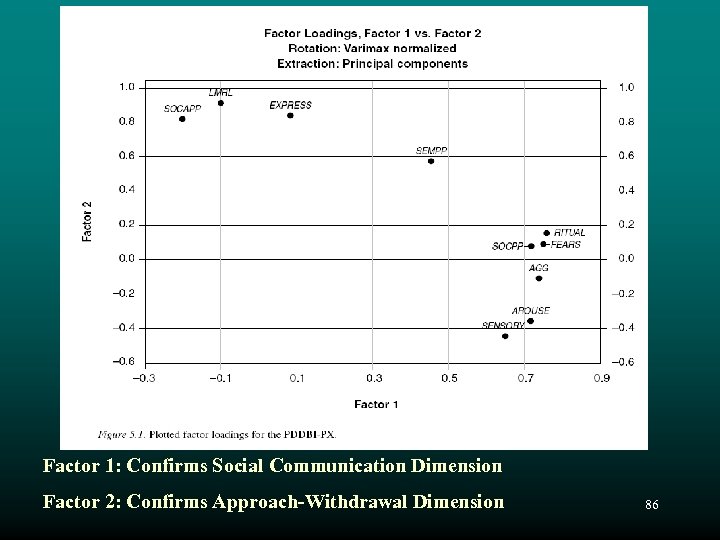
Factor 1: Confirms Social Communication Dimension Factor 2: Confirms Approach-Withdrawal Dimension 86
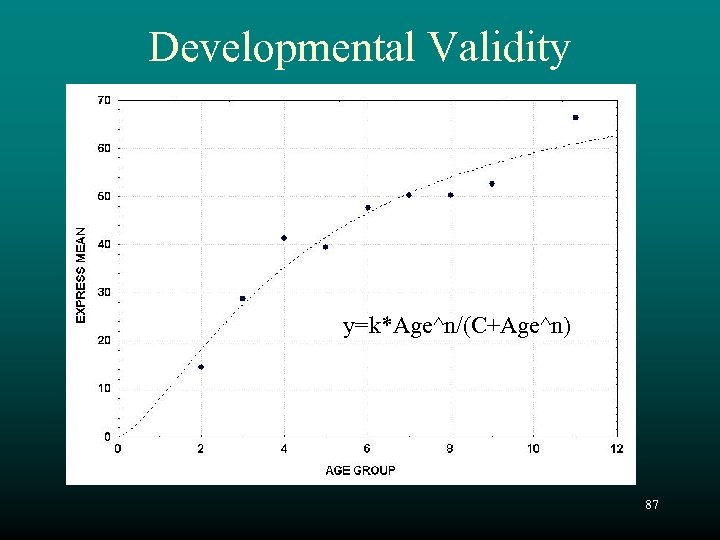
Developmental Validity y=k*Age^n/(C+Age^n) 87
Criterion-Related Validity • Childhood Autism Rating Scale (CARS) • Nisonger Child Behavior Rating Form (CBRF) • Vineland Adaptive Behavior Scales • Griffiths Mental Development Scales 88
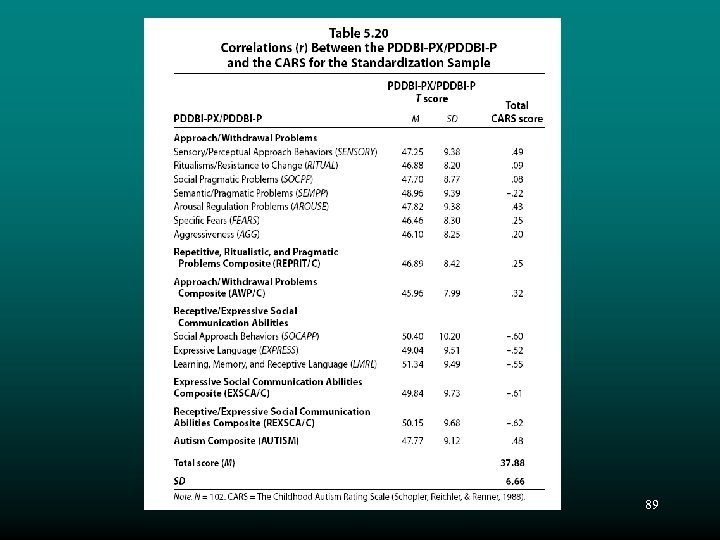
89
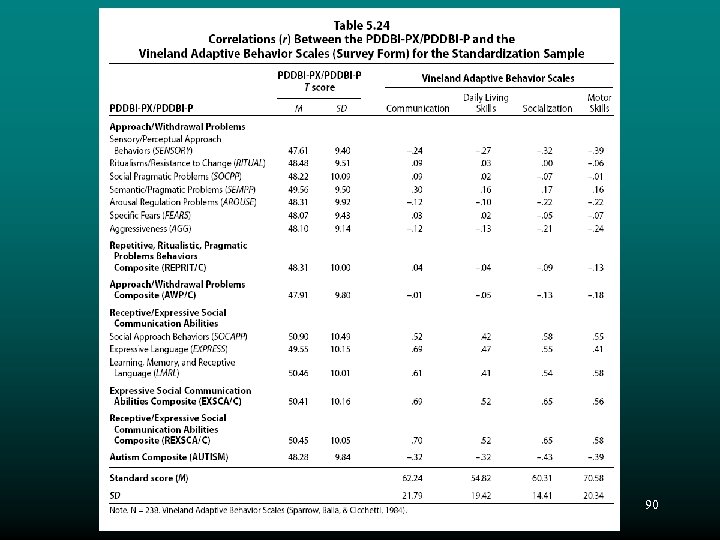
90

91
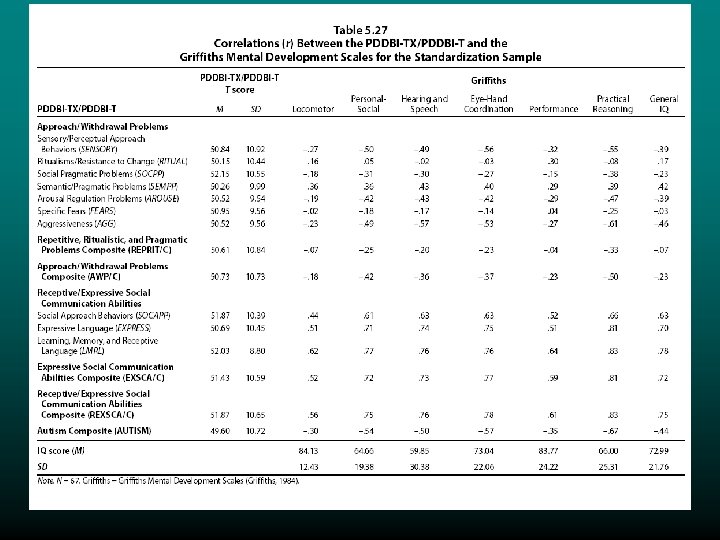
92
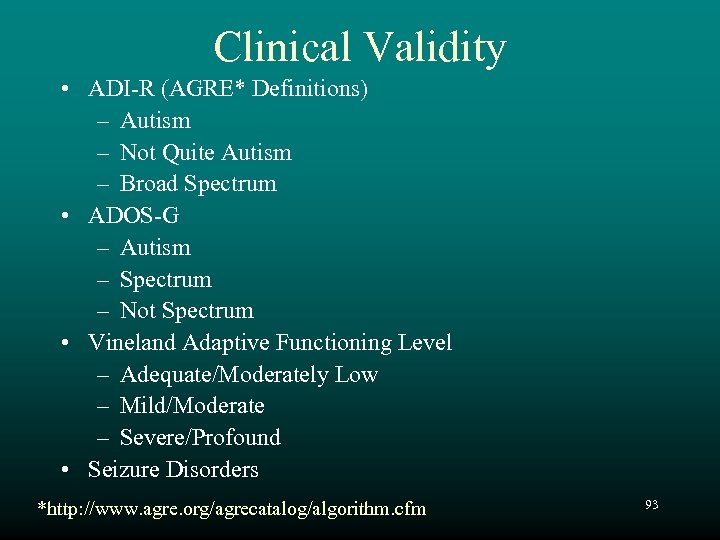
Clinical Validity • ADI-R (AGRE* Definitions) – Autism – Not Quite Autism – Broad Spectrum • ADOS-G – Autism – Spectrum – Not Spectrum • Vineland Adaptive Functioning Level – Adequate/Moderately Low – Mild/Moderate – Severe/Profound • Seizure Disorders *http: //www. agre. org/agrecatalog/algorithm. cfm 93
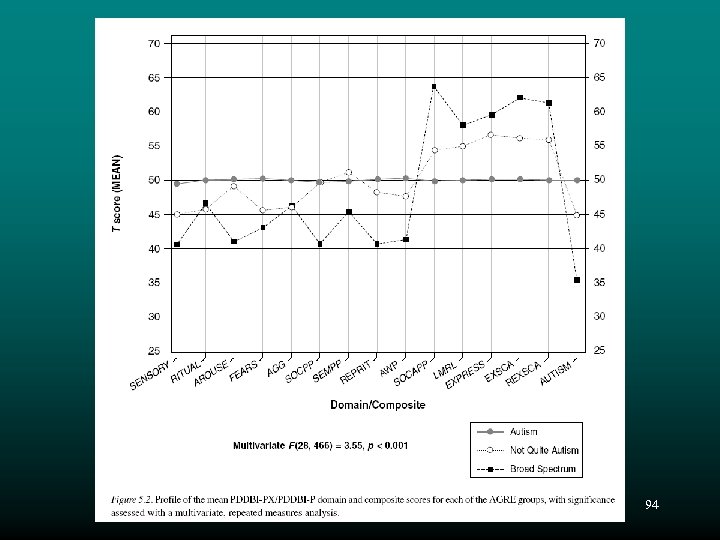
94
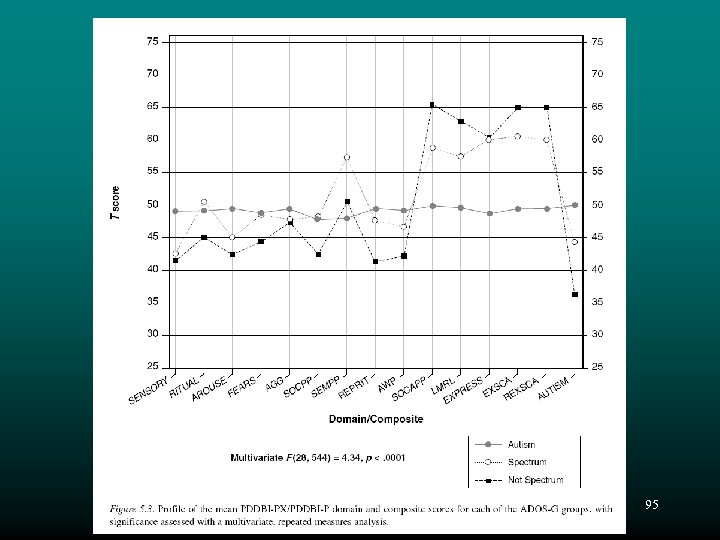
95
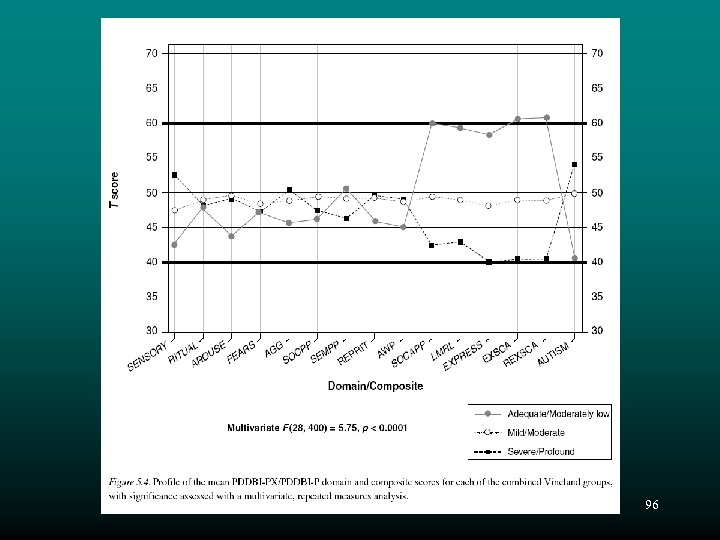
96
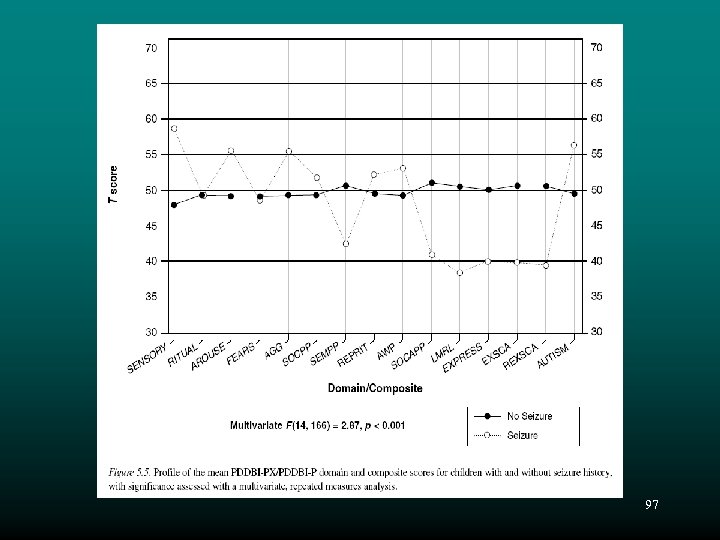
97
Clinical Interpretation 98
PDDBI Profiles • For clinical and research purposes, it is important to examine the overall profile of scores, as well as the magnitude of the composite scores, for both parent and teacher observations • Such profiles can provide important information about the child, and identify behaviorally-defined sub-groups • Remember that the PDDBI is standardized on an autism sample. 99
Case 1 - Michael • Visit 1 (23 months of age): – Vineland • Communication – 6 months • Socialization – 11 months • Motor Skills – 23 months – ADOS-G: Autism • Visit 2 (28 months of age; After 25 hrs/wk of ABA and O. T. ): – Vineland • Communication – 21 months • Socialization – 20 months • Motor Skills – 28 months – ADOS-G: Autism Spectrum Disorder 100
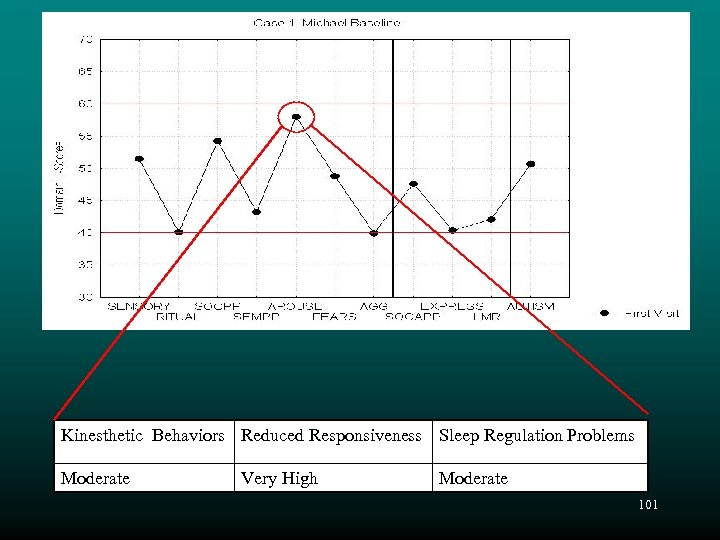
Kinesthetic Behaviors Reduced Responsiveness Sleep Regulation Problems Moderate Very High Moderate 101
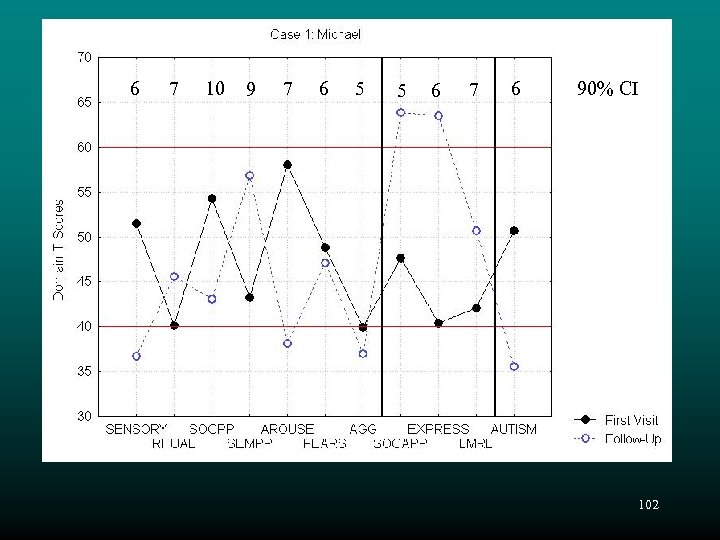
6 7 10 9 7 6 5 5 6 7 6 90% CI 102

103
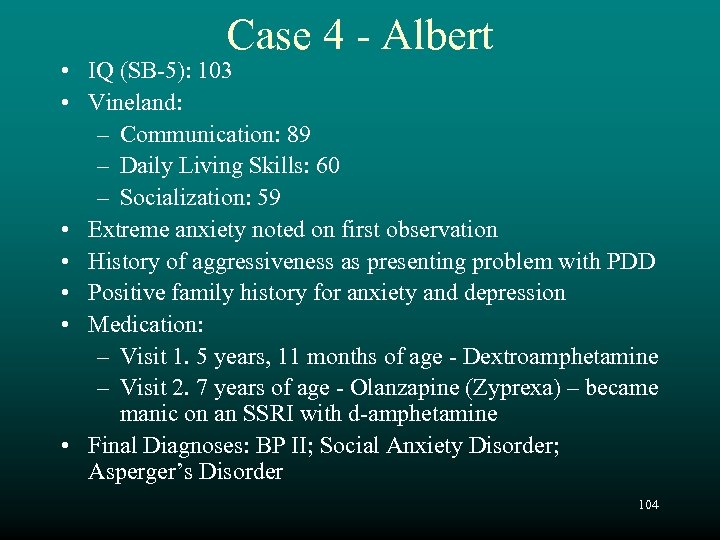
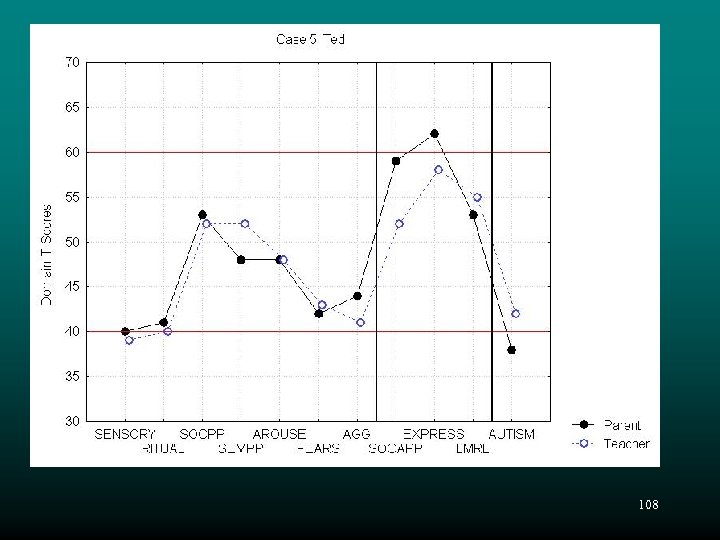
Case 4 - Albert • IQ (SB-5): 103 • Vineland: – Communication: 89 – Daily Living Skills: 60 – Socialization: 59 • Extreme anxiety noted on first observation • History of aggressiveness as presenting problem with PDD • Positive family history for anxiety and depression • Medication: – Visit 1. 5 years, 11 months of age - Dextroamphetamine – Visit 2. 7 years of age - Olanzapine (Zyprexa) – became manic on an SSRI with d-amphetamine • Final Diagnoses: BP II; Social Anxiety Disorder; Asperger’s Disorder 104

105
106

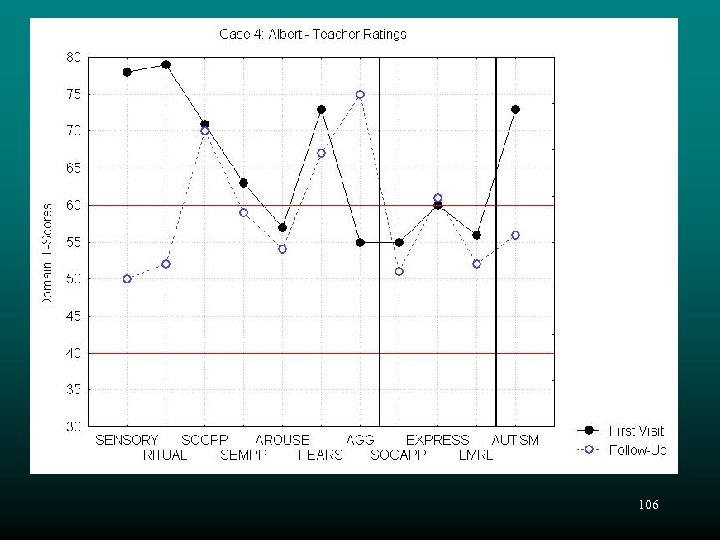
Case 5 - Ted • Boy, 10 years of age with Fragile X Syndrome • Vineland: – Communication: 63 – Daily Living Skills: 46 – Socialization: 65 • Medication: Methylphenidate (Ritalin) • History of delayed milestones 107
108
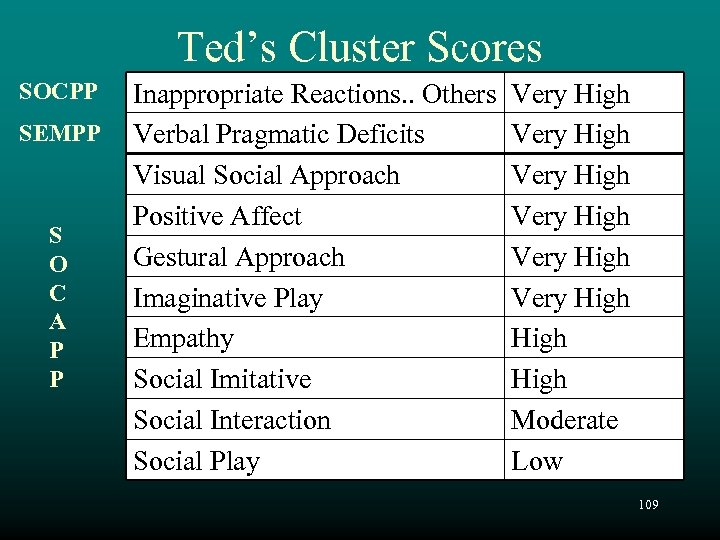
Ted’s Cluster Scores SOCPP SEMPP S O C A P P Inappropriate Reactions. . Others Verbal Pragmatic Deficits Visual Social Approach Positive Affect Gestural Approach Imaginative Play Empathy Social Imitative Social Interaction Social Play Very High Very High Moderate Low 109

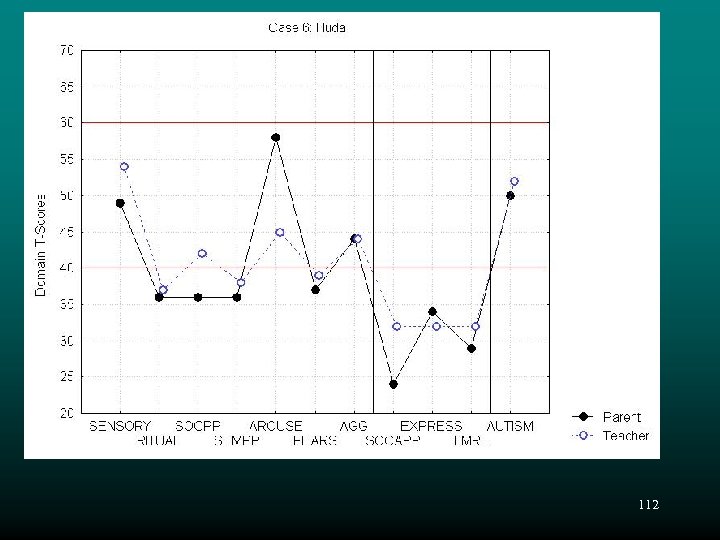
Case 6 - Huda • Girl, age 3 years, 2 months • Rett’s Disorder • Vineland: – Communication: 43 – Daily Living Skills: 42 – Socialization: 50 – Motor Skills: 39 • ADOS-G: Autism 110

Rett’s Disorder • • • Normal pre- and peri-natal development Normal psychomotor development up to 5 mos. Normal HC at birth-HC deceleration 5 -48 mos. Loss of purposeful hand skills (hand wringing) Loss of social engagement Poorly coordinated gait and trunk movements Severe language disorder and retardation Breathing abnormalities common Due to MECP 2 gene mutation absence of MECP 2 protein absence of gene suppression – “Leaky genes” 111
112
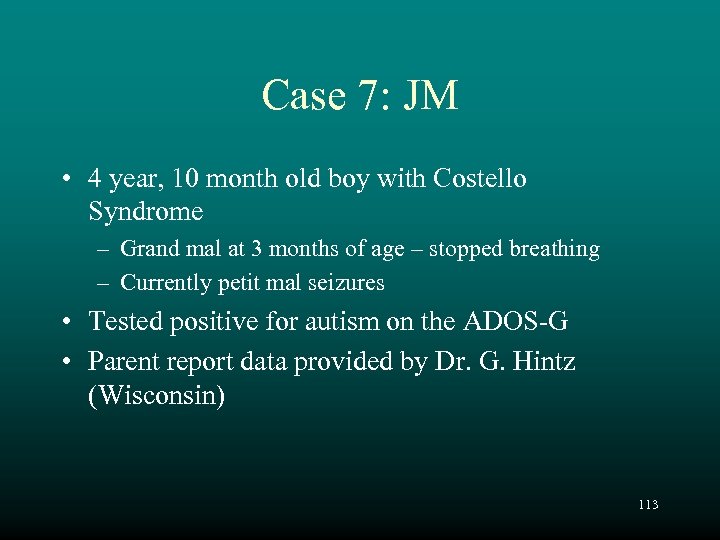
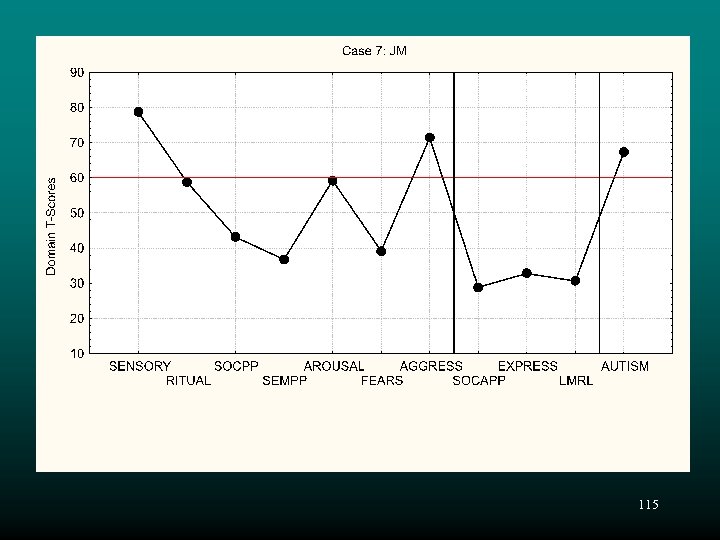
Case 7: JM • 4 year, 10 month old boy with Costello Syndrome – Grand mal at 3 months of age – stopped breathing – Currently petit mal seizures • Tested positive for autism on the ADOS-G • Parent report data provided by Dr. G. Hintz (Wisconsin) 113

Costello Syndrome • Rare multi-organ disorder of unknown etiology • Physical characteristics – Growth delay – Short stature – Excessive skin on neck, palms, fingers, soles – Characteristic facial appearance • Macrocephaly • Low set ears • Thick ear lobes and lips, wide nostrils • Cognitive delay • Behavior – “Warm, sociable, and humorous” 114
115

Do PDDBI Domains Reflect Improvement? 116
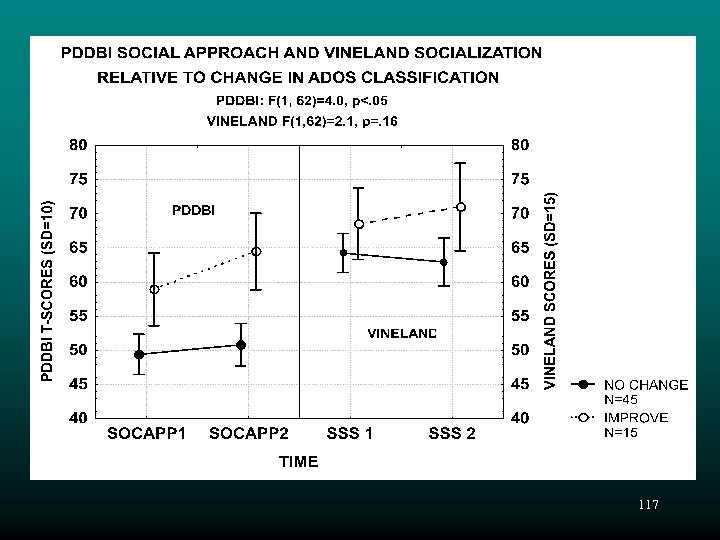
117
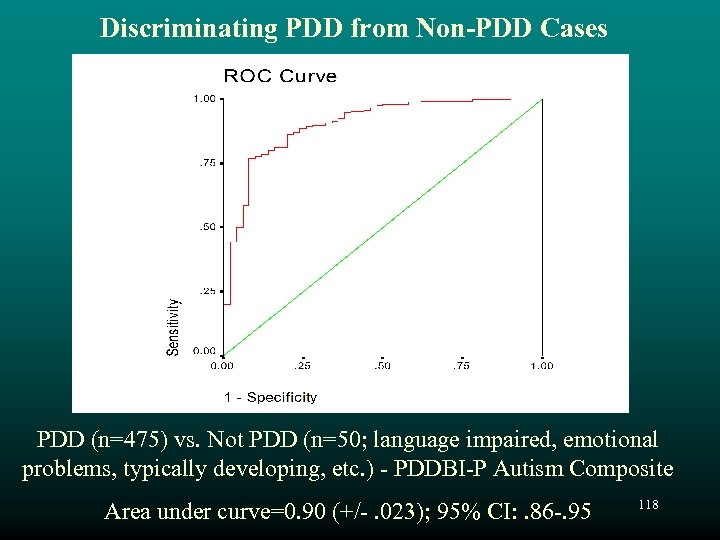
Discriminating PDD from Non-PDD Cases PDD (n=475) vs. Not PDD (n=50; language impaired, emotional problems, typically developing, etc. ) - PDDBI-P Autism Composite Area under curve=0. 90 (+/-. 023); 95% CI: . 86 -. 95 118
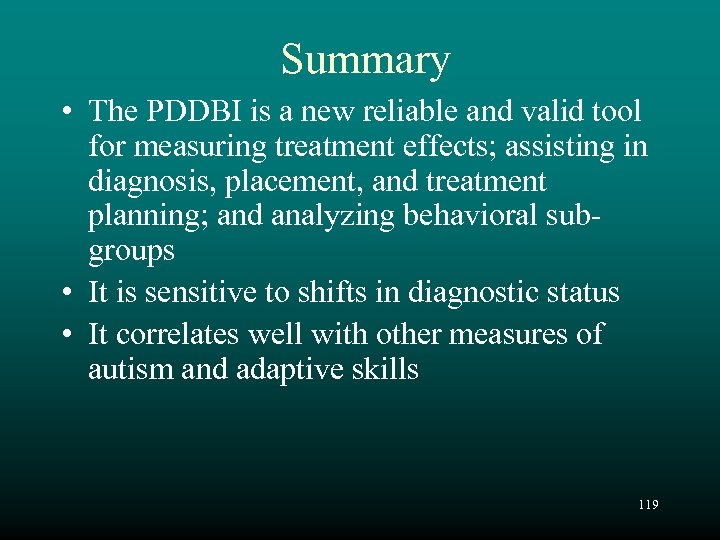
Summary • The PDDBI is a new reliable and valid tool for measuring treatment effects; assisting in diagnosis, placement, and treatment planning; and analyzing behavioral subgroups • It is sensitive to shifts in diagnostic status • It correlates well with other measures of autism and adaptive skills 119
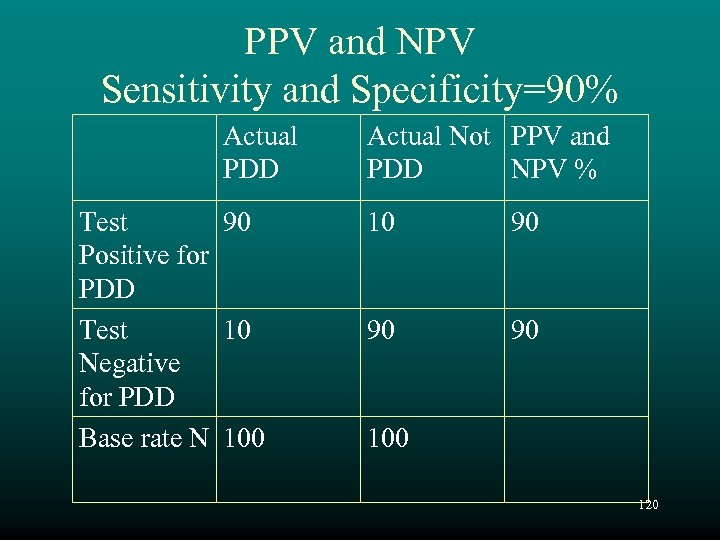
PPV and NPV Sensitivity and Specificity=90% Actual PDD Test 90 Positive for PDD Test 10 Negative for PDD Base rate N 100 Actual Not PPV and PDD NPV % 10 90 90 90 100 120
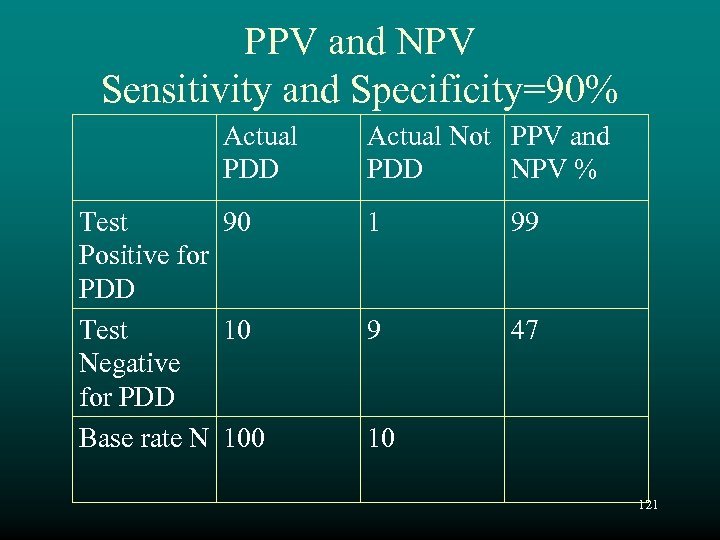
PPV and NPV Sensitivity and Specificity=90% Actual PDD Test 90 Positive for PDD Test 10 Negative for PDD Base rate N 100 Actual Not PPV and PDD NPV % 1 99 9 47 10 121
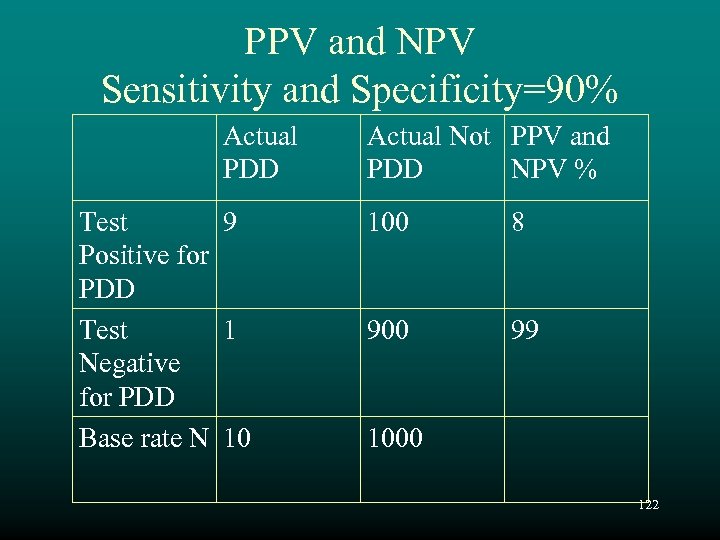
PPV and NPV Sensitivity and Specificity=90% Actual PDD Test 9 Positive for PDD Test 1 Negative for PDD Base rate N 10 Actual Not PPV and PDD NPV % 100 8 900 99 1000 122
3d898b4650dc9b1b7c01671be773c591.ppt