59f8c7aa0754ff58a71e91a868c67c79.ppt
- Количество слайдов: 60
The Patient Experience: Changing the Culture Patty Ledbetter, BA, CHAM Manager, Revenue Cycle Management, Tucson Medical Center
The Patient Experience: Changing the Culture Presented by: Patty Ledbetter, BA, CHAM Manager, Revenue Cycle Management Tucson Medical Center Tucson, Arizona
Objectives 1. 2. 3. 4. 5. 6. 7. Define the problem Identify the root cause(s) associated with patient dissatisfaction and the problems associated with our poor patient satisfaction scores Analyze various approaches and obstacles to affect a change within the organization Develop and implement a model to change the culture and behaviors within the organization Monitor and maintain the culture climate Measure benefits as reported in our HCAHPS scores Plan for organizational integration


About Us Largest single level facility in the country Established as a community hospital in 1943 Buildings and grounds spread over 120 acres Nearly 27 miles of combined hallways, TMC's campus also serves as home to the Tucson Orthopedic Institute, the Cancer Care Center of Southern Arizona and the Children's Clinics for Rehabilitative Services Licensed for 615 adult, pediatric and behavioral health beds serving more than 38, 000 inpatients and 115, 000 outpatients annually.

The Problem as Defined by Our Scores

Voice of the Customer recorded third party surveys
HCAHPS-Hospital Consumer Assessment of Health Plans Survey (or Hospital CAHPS®). A nationally standardized survey developed by CMS and AHRQ for measuring how patients perceive the care they receive in hospitals.
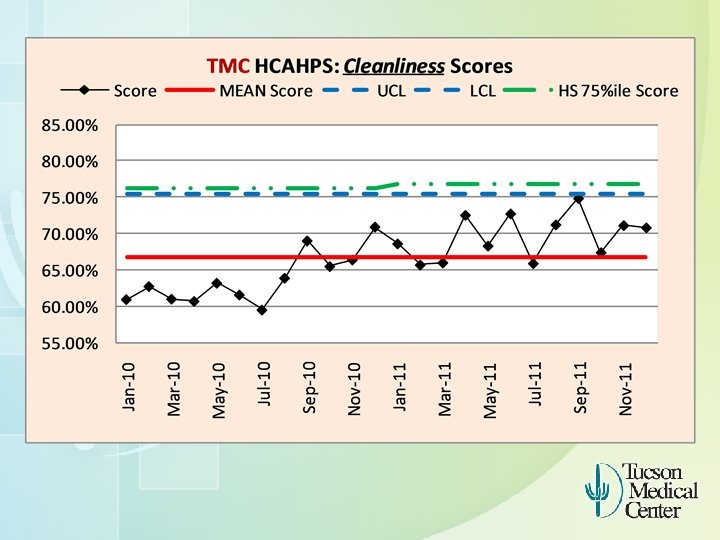
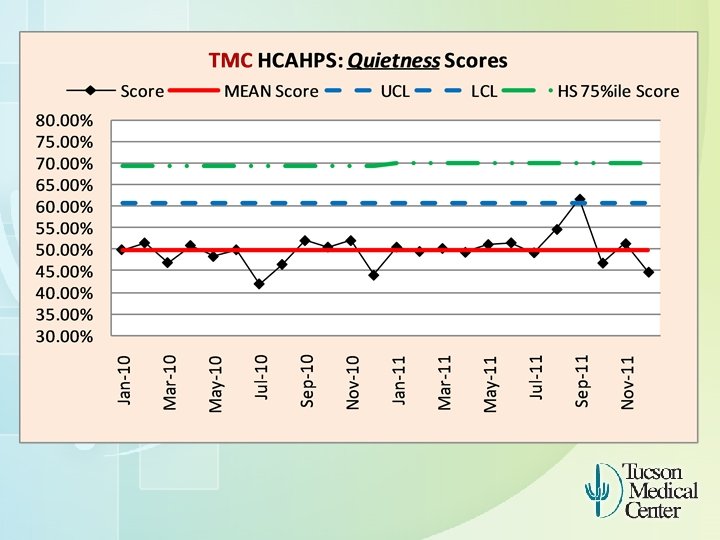

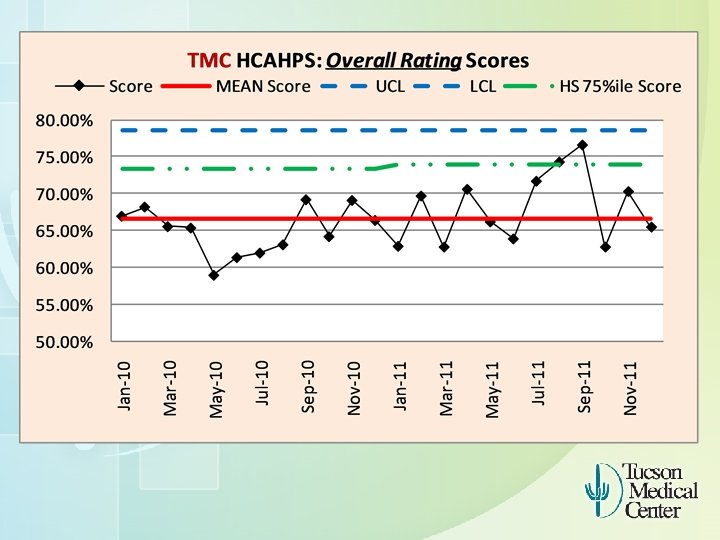
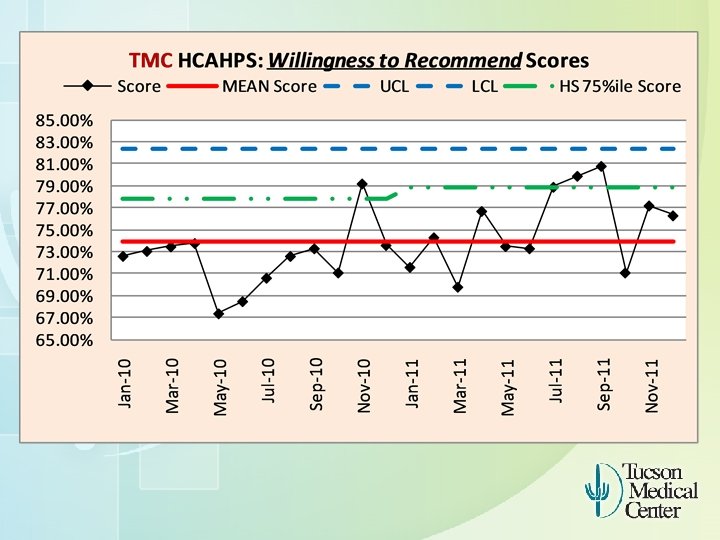
Our Goal To achieve the 75% percentile or top 25% of all hospitals is our goal.
Analyzing Options Buy it versus make it? Contract with an outside company to design and implement a plan Researched examples of organizational success how companies created the “wow” factor for their customers

Getting Started

Starting the Patient Experience Project Champion and vision from our COO We began with a few initiatives Say Hello Image Caring for the environment Discharge rounds

Communicating our Progress More teams grew from there and focused on key areas aimed at improving communication and physical impressions in the facility. Including: Way finding Lunch with Linda Say Hello Points of Entrances Communication Expectations-Excellent Customer Service Adopt A Hallway HCAHPS Service Recovery Dress Code Mission Moments Be the Nicest Quiet at Night
Quality objectives were developed Best Practices (Health. Streams) were studied Ownership and Accountability were identified as essential pieces of the project Acknowledged that our Volunteer population played a key role and must be included Right the wrong-value in immediate service recovery
Evaluating our Project Progress We lacked the combined focus and other key elements that kept the project organized and making a bigger impact. We needed to reorganize our efforts for a more unified approach and delivery of a stronger message.
Reorganization of the Project The Project Team was updated Guidance Council was created IHI bundle model

The New Patient Experience Project Who is IHI? The Institute for Healthcare Improvement (IHI)
The Bundle Approach Development of Behavioral Bundles to address target areas of greatest need outlined above
A bundle is a small, straightforward set of evidence-based practices — generally three to five — that, when performed collectively and reliably, have been proven to improve patient outcomes.
Components of a bundle Care bundles are groupings of best practices with respect to a disease process that individually improve care, but when applied together may result in substantially greater improvement. The bundle is an effort to design a standard approach to delivering these core elements of care.

Data Collection & Tracking Capture improvement measures Track improvement measures over time Develop & implement data collection tools Communicate success!
New Patient Experience Structure

Patient Experience Structure Putting it all together Current efforts Councils : A familiar structure that has been successful at TMC ◦ HCAHPS Bundle Teams ◦ Patient Experience Guiding Council Fresh new look with interdisciplinary team
Team Responsibilities Bundle Teams Responsibility: ◦ Review the care experience from data collected by the Shadower ◦ Define Touchpoints ◦ Build bundles to improve care experiences Team make-up: ◦ ◦ ◦ HCAHPS Bundle Leader Patient Experience Bundle Leader Shadow Team Facilitators Members
Guidance Council make-up: ◦ Administrative Champion ◦ Care experience champions ◦ Data expert ◦ Facilitator
Guidance Council Responsibilities Guidance Council Responsibilities: ◦ Review care experience requests ◦ Charter teams ◦ Assign Bundle Leaders and assists in selecting Team members and shadowers as needed ◦ Review Bundle Team’s progress ◦ Assist in removing barriers, makes suggestions ◦ Communicate Team’s work to organization
Selecting Areas of Focus to Address the Problem We were way off the mark in Cleanliness and Quietness Addressing the communication piece
Patient Feedback We wanted to infuse feedback from patients and families into the process. Shadowed patient experiences Interviewed patients and volunteers Voice of the Customer-third party patient surveys
What is Shadowing? Uncovering opportunities to deliver exceptional patient and family care experiences. Process in which a Shadower follows the patient and family through the entire care experience
Benefits of Shadowing Focus on patient’s & family’s point of view alone. Provides timely information Enables patients & families to become partners in care Allows us to map the patient flow Enables us to view interactions at each touchpoint
Six Steps to Shadowing 1. 2. 3. 4. 5. 6. Define the care experience Select the patient and family Shadower Gather information for the project Connect & coordinate with the patient & family Observe, Record, Evaluate the experience Report finding
Step 1 – Define the Care Experience Example: Emergency Department ◦ Parking to point of entry ◦ ER Admitting ◦ Registration/Triage ◦ Exam Room Lab, radiology Physician interaction ◦ Discharge process
Step 2 – Select the Shadower The Shadower should: ◦ Be a good observer and listener ◦ Have a positive and supportive attitude ◦ Approach shadowing with “open eyes” ◦ Be empathetic, compassionate & reliable ◦ Have good verbal and written communication skills
Step 3 - Gather Information Identify the patient Know the current flow of the care experience Know what other patients & families have experienced Identify an ideal time of day Communicate shadowing to caregivers Tour the area prior
Step 4 - Connect and Coordinate with the Patient & Family Make arrangements with patient and family in advance ◦ Reduces anxiety ◦ Helps ensure success Explain your role to patient and family Let them know how their participation will benefit others
Step 5 - Shadow Observe, Record and Evaluate! ◦ Who are the caregivers? ◦ What are the touchpoints? ◦ How long does each process take? ◦ What are the comments and concerns? ◦ What are your impressions and observations?
Step 6 – Record Findings Collect: ◦ Comments, questions and suggestions ◦ Touchpoints ◦ Amount of time spent at each touchpoint ◦ Quality of interactions with all caregivers Observational Report: ◦ Include highlights, bottlenecks, redundancies ◦ Include a time study
Shadowing Issues Summarized Many issues identified with physical space Snacks and beverages in surgery waiting areas need to be improved Poor eye contact and communication from staff with patients and visitors Many patient conversations easily overheard by others Better maps and signs needed
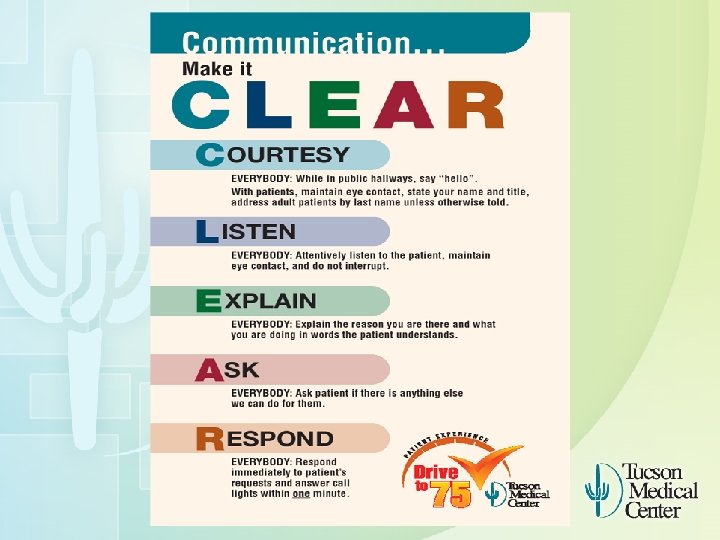
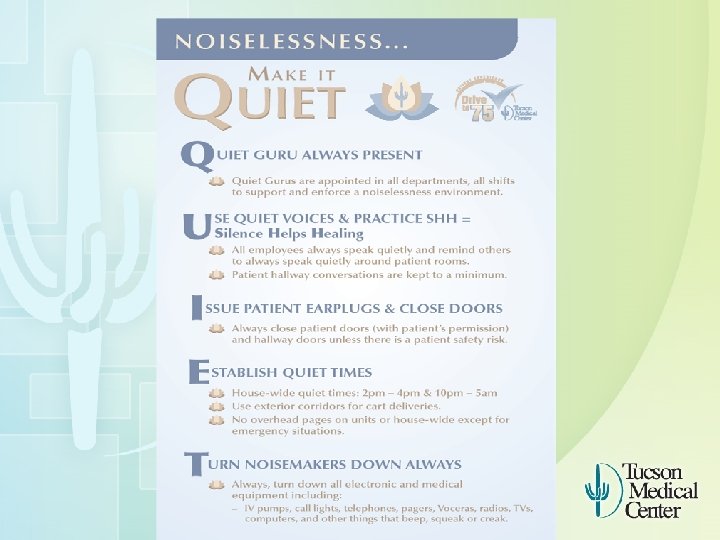
Rolling Out the New Bundles The first bundles were identified to address: Communication Quietness Cleanliness (after the kick off)
The Kick Off! Mandatory Educational Meetings were planned and organized to orchestrate the delivery of this new bundle information. The first two bundles were completed to address: ◦ Communication & Quiet The Team held the meetings (it was a marathon!) and participated in the delivery of the information to all staff. Personal accountability and on going expectations were communicated.


The Message The project and background were communicated. The Scores were examined and new goals explained. The first two Bundles were explained in detail.

Senior Leadership delivered an inspirational message about the importance of these steps and their integration into our organizational culture. The development of our new performance appraisal tool to develop behavioral expectations and measurements was communicated. The importance of recognizing and rewarding the new positive behavior bundles was explained and emphasized.



Results For the two months following the kick off, our scores rose! We noticed that there was an obvious buzz in the halls. ◦ And we noticed that the excitement created was quickly fading ◦ We developed an assignment calendar to ensure rounding on the units ◦ We revised our Service Recovery policy
Next Steps Keeping the momentum has been our biggest challenge. While we continue to feel the positive effects from the project today, clearly people change and programs lose their strength over time. How to keep this behavior alive is our current focus. New bundles are in the works and new teams have been developed to continue communication efforts and keep the project alive.
A Mission Moment In celebration of the work we do every day at TMC, staff members, patients, visitors and physicians are invited to share examples of extraordinary care and kindness. These stories are reflections of how Tucson Medical Center brings compassion, healing and hope, to those we serve.
I went to Wal-Mart this morning and was wearing my scrubs that say TMC Health. Care on them and the associate noticed that I worked there. She told me that her husband was at TMC for about 2 months (he was passing away) she told me the staff were wonderful to both her and her husband. They made her feel comfortable and welcomed and took excellent care of her husband. She decided to do home hospice and before he was discharged TMC handled all the arrangements for a home health nurse to come, gave her grievance counseling to prepare for his passing. She took the names of everyone they encountered during the hospital stay to thank them and make sure those employees were recognized for excellent care. The home health nurse was very kind to them and she told me TMC even gave her pamphlets on funeral arrangements and support groups to attend after husband passed. She told she will always go to TMC and recommends TMC to everyone because of the staff. Even though her husband passed over 2 months ago she still remembers the great care she received. I told her thank you for letting me know. It is nice to hear wonderful comments from the public.

Contact Information Patty Ledbetter Patty. ledbetter@tmcaz. com 520. 324. 3331
59f8c7aa0754ff58a71e91a868c67c79.ppt