b56ead4cbcd29b82f60599f7b4ab3fae.ppt
- Количество слайдов: 30
 The Patient-Centered Medical Home April 15, 2011 Presented by Christine Hughes to the Missouri Association of Osteopathic Physicians and Surgeons
The Patient-Centered Medical Home April 15, 2011 Presented by Christine Hughes to the Missouri Association of Osteopathic Physicians and Surgeons
 Agenda What is a Medical Home? The Business Case for Developing Medical Homes Key Lessons from Multi-Payer Medical Home Initiatives in the U. S. Missouri Foundation for Health’s “Missouri Medical Home Collaborative” Questions/Discussion The Patient-Centered Medical Home 2
Agenda What is a Medical Home? The Business Case for Developing Medical Homes Key Lessons from Multi-Payer Medical Home Initiatives in the U. S. Missouri Foundation for Health’s “Missouri Medical Home Collaborative” Questions/Discussion The Patient-Centered Medical Home 2
 What is a Medical Home? Pediatric origins in 1960 with focus on children with special needs NCQA physician recognition standards built off the Chronic Care Model which was developed by Dr. Ed Wagner Joint Principles released in February 2007 by primary care professional organizations NCQA physician recognition standards modified for PCMH with revised standards Continuing and ongoing evolution The Patient-Centered Medical Home 3
What is a Medical Home? Pediatric origins in 1960 with focus on children with special needs NCQA physician recognition standards built off the Chronic Care Model which was developed by Dr. Ed Wagner Joint Principles released in February 2007 by primary care professional organizations NCQA physician recognition standards modified for PCMH with revised standards Continuing and ongoing evolution The Patient-Centered Medical Home 3
 What is a Medical Home? Specific system changes (intense practice transformation) designed to result in: – informed activated patients and proactive practice teams – an improved system of care, leading to better quality and reduced costs Foundation for developing Accountable Care Organizations The Patient-Centered Medical Home 4
What is a Medical Home? Specific system changes (intense practice transformation) designed to result in: – informed activated patients and proactive practice teams – an improved system of care, leading to better quality and reduced costs Foundation for developing Accountable Care Organizations The Patient-Centered Medical Home 4
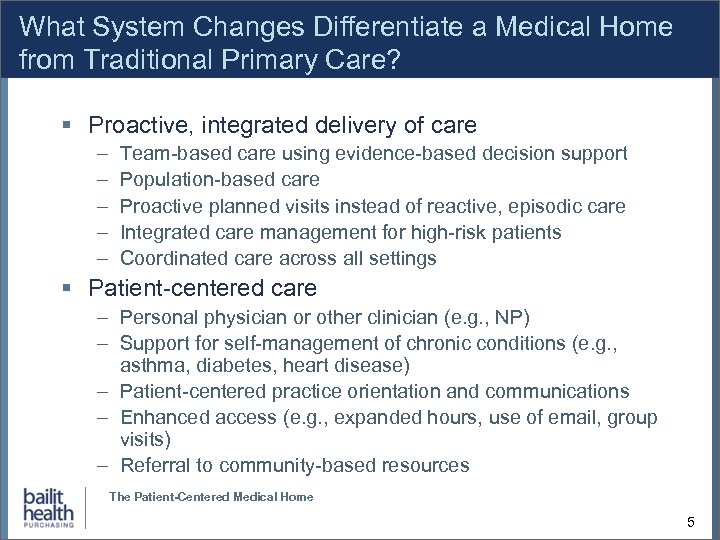 What System Changes Differentiate a Medical Home from Traditional Primary Care? Proactive, integrated delivery of care – – – Team-based care using evidence-based decision support Population-based care Proactive planned visits instead of reactive, episodic care Integrated care management for high-risk patients Coordinated care across all settings Patient-centered care – Personal physician or other clinician (e. g. , NP) – Support for self-management of chronic conditions (e. g. , asthma, diabetes, heart disease) – Patient-centered practice orientation and communications – Enhanced access (e. g. , expanded hours, use of email, group visits) – Referral to community-based resources The Patient-Centered Medical Home 5
What System Changes Differentiate a Medical Home from Traditional Primary Care? Proactive, integrated delivery of care – – – Team-based care using evidence-based decision support Population-based care Proactive planned visits instead of reactive, episodic care Integrated care management for high-risk patients Coordinated care across all settings Patient-centered care – Personal physician or other clinician (e. g. , NP) – Support for self-management of chronic conditions (e. g. , asthma, diabetes, heart disease) – Patient-centered practice orientation and communications – Enhanced access (e. g. , expanded hours, use of email, group visits) – Referral to community-based resources The Patient-Centered Medical Home 5
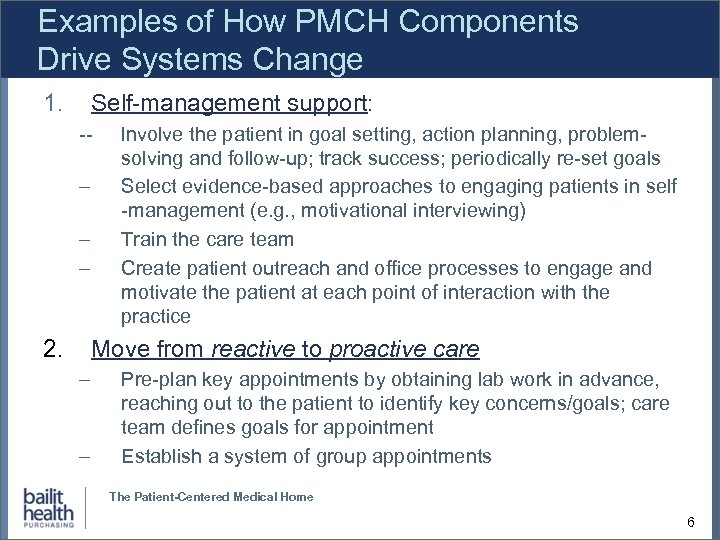 Examples of How PMCH Components Drive Systems Change 1. Self-management support: -- – – – 2. Involve the patient in goal setting, action planning, problemsolving and follow-up; track success; periodically re-set goals Select evidence-based approaches to engaging patients in self -management (e. g. , motivational interviewing) Train the care team Create patient outreach and office processes to engage and motivate the patient at each point of interaction with the practice Move from reactive to proactive care – – Pre-plan key appointments by obtaining lab work in advance, reaching out to the patient to identify key concerns/goals; care team defines goals for appointment Establish a system of group appointments The Patient-Centered Medical Home 6
Examples of How PMCH Components Drive Systems Change 1. Self-management support: -- – – – 2. Involve the patient in goal setting, action planning, problemsolving and follow-up; track success; periodically re-set goals Select evidence-based approaches to engaging patients in self -management (e. g. , motivational interviewing) Train the care team Create patient outreach and office processes to engage and motivate the patient at each point of interaction with the practice Move from reactive to proactive care – – Pre-plan key appointments by obtaining lab work in advance, reaching out to the patient to identify key concerns/goals; care team defines goals for appointment Establish a system of group appointments The Patient-Centered Medical Home 6
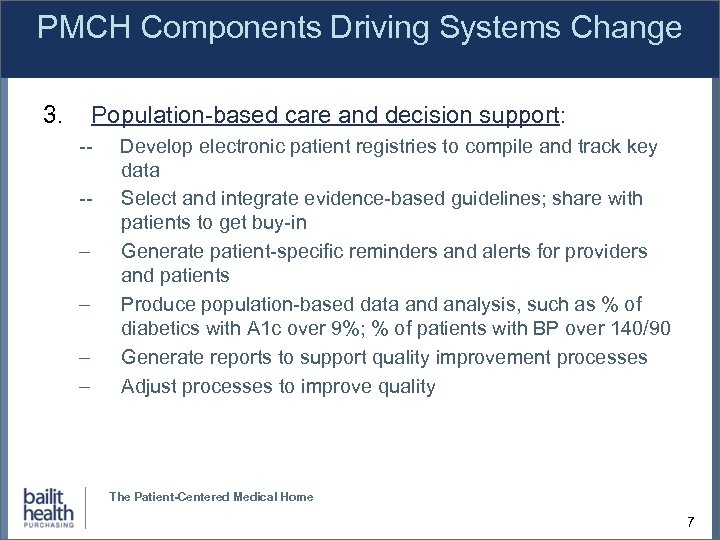 PMCH Components Driving Systems Change 3. Population-based care and decision support: --- – – Develop electronic patient registries to compile and track key data Select and integrate evidence-based guidelines; share with patients to get buy-in Generate patient-specific reminders and alerts for providers and patients Produce population-based data and analysis, such as % of diabetics with A 1 c over 9%; % of patients with BP over 140/90 Generate reports to support quality improvement processes Adjust processes to improve quality The Patient-Centered Medical Home 7
PMCH Components Driving Systems Change 3. Population-based care and decision support: --- – – Develop electronic patient registries to compile and track key data Select and integrate evidence-based guidelines; share with patients to get buy-in Generate patient-specific reminders and alerts for providers and patients Produce population-based data and analysis, such as % of diabetics with A 1 c over 9%; % of patients with BP over 140/90 Generate reports to support quality improvement processes Adjust processes to improve quality The Patient-Centered Medical Home 7
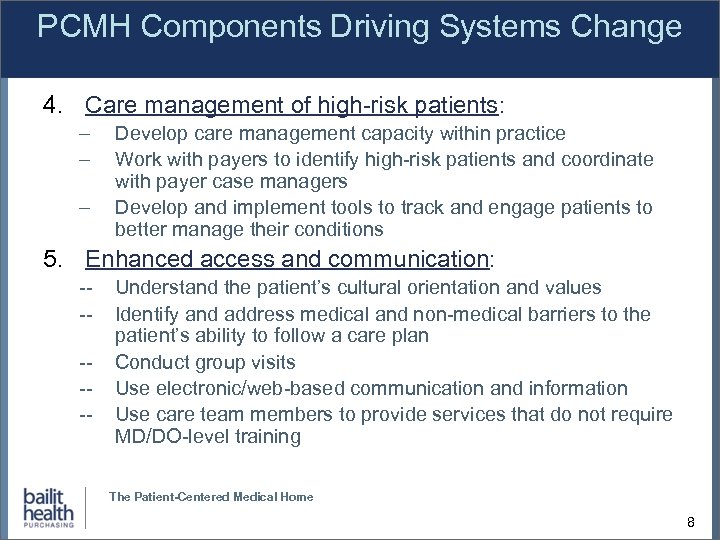 PCMH Components Driving Systems Change 4. Care management of high-risk patients: – – – Develop care management capacity within practice Work with payers to identify high-risk patients and coordinate with payer case managers Develop and implement tools to track and engage patients to better manage their conditions 5. Enhanced access and communication: ------ Understand the patient’s cultural orientation and values Identify and address medical and non-medical barriers to the patient’s ability to follow a care plan Conduct group visits Use electronic/web-based communication and information Use care team members to provide services that do not require MD/DO-level training The Patient-Centered Medical Home 8
PCMH Components Driving Systems Change 4. Care management of high-risk patients: – – – Develop care management capacity within practice Work with payers to identify high-risk patients and coordinate with payer case managers Develop and implement tools to track and engage patients to better manage their conditions 5. Enhanced access and communication: ------ Understand the patient’s cultural orientation and values Identify and address medical and non-medical barriers to the patient’s ability to follow a care plan Conduct group visits Use electronic/web-based communication and information Use care team members to provide services that do not require MD/DO-level training The Patient-Centered Medical Home 8
 Payment Reform • Creates a culture that emphasizes high quality, integrated care – Payers provide incentives to encourage quality and efficiency – Payers provide reimbursement for traditionally nonreimbursable services, such as patient outreach, care coordination, and peer-based, self-management training – Payers may also provide incentive payments linked to improved quality and efficiency or share savings generated by such care Payment reform is essential for sustainability of system changes The Patient-Centered Medical Home 9
Payment Reform • Creates a culture that emphasizes high quality, integrated care – Payers provide incentives to encourage quality and efficiency – Payers provide reimbursement for traditionally nonreimbursable services, such as patient outreach, care coordination, and peer-based, self-management training – Payers may also provide incentive payments linked to improved quality and efficiency or share savings generated by such care Payment reform is essential for sustainability of system changes The Patient-Centered Medical Home 9
 Research on Effectiveness of Medical Homes May 2010 edition of Health Affairs examined issues associated with primary care, including the Medical Home as an approach to practice transformation One article, “Driving Quality Gains and Cost Savings through Adoption of Medical Homes, ”* examined annual outcomes of 7 successful Medical Home projects and tried to identify common success factors Projects demonstrated both improved quality and reduced costs and provide suggested best practices *Fields D, Leshen E and Patel K, “Driving Quality Gains and Cost Savings through Adoption of Medical Homes. ” Health Affairs, May 2010, Volume 29, Number 5, pages 819 -826. The Patient-Centered Medical Home 10
Research on Effectiveness of Medical Homes May 2010 edition of Health Affairs examined issues associated with primary care, including the Medical Home as an approach to practice transformation One article, “Driving Quality Gains and Cost Savings through Adoption of Medical Homes, ”* examined annual outcomes of 7 successful Medical Home projects and tried to identify common success factors Projects demonstrated both improved quality and reduced costs and provide suggested best practices *Fields D, Leshen E and Patel K, “Driving Quality Gains and Cost Savings through Adoption of Medical Homes. ” Health Affairs, May 2010, Volume 29, Number 5, pages 819 -826. The Patient-Centered Medical Home 10
 Business Case for Medical Homes Findings from most recent research of successful Medical Home models indicates reduced costs and improved patient health status – Costs compared to either control groups or historical trends Savings are generally due to reduced use of ER and inpatient services Changes observed for general primary care patient population and for populations of high-risk patients Changes also seen among privately insured, Medicaid, SCHIP and Medicare populations The Patient-Centered Medical Home 11
Business Case for Medical Homes Findings from most recent research of successful Medical Home models indicates reduced costs and improved patient health status – Costs compared to either control groups or historical trends Savings are generally due to reduced use of ER and inpatient services Changes observed for general primary care patient population and for populations of high-risk patients Changes also seen among privately insured, Medicaid, SCHIP and Medicare populations The Patient-Centered Medical Home 11
 Business Case Observations Business case is growing more solid as we get more experience with Medical Homes Growing evidence that there are key components at the practice level required for success, particularly: – – – Engaged leadership Dedicated care managers Expanded access Performance management tools Effective financial incentives Ability to increase opportunities for success by designing a model based on best practices The Patient-Centered Medical Home 12
Business Case Observations Business case is growing more solid as we get more experience with Medical Homes Growing evidence that there are key components at the practice level required for success, particularly: – – – Engaged leadership Dedicated care managers Expanded access Performance management tools Effective financial incentives Ability to increase opportunities for success by designing a model based on best practices The Patient-Centered Medical Home 12
 Medical Home Projects and Demonstrations There are currently at least 28 multi-stakeholder PCMH projects underway in 21 states. Medicare will join at least 6 of these in mid 2011. The Patient-Centered Medical Home 13
Medical Home Projects and Demonstrations There are currently at least 28 multi-stakeholder PCMH projects underway in 21 states. Medicare will join at least 6 of these in mid 2011. The Patient-Centered Medical Home 13
 General Keys to Sustainability Strong champions among stakeholders and within transforming practices Adequate project management support for the duration of the initiative Financial and non-financial support for provider adoption – Payment from payers – Technical assistance Regular feedback to practices and stakeholders on performance improvement Process for ensuring practice improvement Durable cost savings and quality improvement will only happen when the care delivery process changes, and when patients are engaged in prevention and self-management. Models are continuing to be refined in many ways The Patient-Centered Medical Home 14
General Keys to Sustainability Strong champions among stakeholders and within transforming practices Adequate project management support for the duration of the initiative Financial and non-financial support for provider adoption – Payment from payers – Technical assistance Regular feedback to practices and stakeholders on performance improvement Process for ensuring practice improvement Durable cost savings and quality improvement will only happen when the care delivery process changes, and when patients are engaged in prevention and self-management. Models are continuing to be refined in many ways The Patient-Centered Medical Home 14
 What is Happening in Missouri? Several practices independently seeking NCQA recognition Several single-payor initiatives Missouri Foundation for Health (MFH) hosting a multipayor/stakeholder Collaborative (MMHC) The Patient-Centered Medical Home 15
What is Happening in Missouri? Several practices independently seeking NCQA recognition Several single-payor initiatives Missouri Foundation for Health (MFH) hosting a multipayor/stakeholder Collaborative (MMHC) The Patient-Centered Medical Home 15
 Missouri Medical Home Collaborative (MMHC) – Activities to Date MFH contracted with Bailit Health Purchasing to assess interest and readiness – Spring 2010 Conducted key stakeholder interviews and PCP provider survey – spring/summer 2010 MFH committed to convening a multi-stakeholder initiative and provide 2011 funding for: – Project Management of MMHC – Evaluation: Hire a contractor to develop an evaluation plan to determine impact of initiative – Learning Collaborative(s): Hire a contractor to offer intensive multi-day PCMH practice transformation trainings for primary care providers The Patient-Centered Medical Home 16
Missouri Medical Home Collaborative (MMHC) – Activities to Date MFH contracted with Bailit Health Purchasing to assess interest and readiness – Spring 2010 Conducted key stakeholder interviews and PCP provider survey – spring/summer 2010 MFH committed to convening a multi-stakeholder initiative and provide 2011 funding for: – Project Management of MMHC – Evaluation: Hire a contractor to develop an evaluation plan to determine impact of initiative – Learning Collaborative(s): Hire a contractor to offer intensive multi-day PCMH practice transformation trainings for primary care providers The Patient-Centered Medical Home 16
 MMHC – Activities to Date continued Established a planning council consisting of key stakeholders – November 2010 – – Payers/Insurers (public and private) Employers Providers (Hospitals/Health Systems; PCP practices; FQHCs; RHCs) “Thought Leaders” Council met every 2 weeks to develop framework for Collaborative - November 2010 through January 2011 – Background and Proposed Approach – Collaborative goals and duration, defining and verifying Medical Home Status – Payment model – Technical support for practices, clinical focus, practice participation requirements – Consumer engagement, evaluation Payment Model and ‘statewide’ expansion - February through April 2011 – Payer only & payer/provider meetings to develop payment model – Coordination efforts with Health Care Foundation of Greater Kansas City – Steering Committee Formation The Patient-Centered Medical Home 17
MMHC – Activities to Date continued Established a planning council consisting of key stakeholders – November 2010 – – Payers/Insurers (public and private) Employers Providers (Hospitals/Health Systems; PCP practices; FQHCs; RHCs) “Thought Leaders” Council met every 2 weeks to develop framework for Collaborative - November 2010 through January 2011 – Background and Proposed Approach – Collaborative goals and duration, defining and verifying Medical Home Status – Payment model – Technical support for practices, clinical focus, practice participation requirements – Consumer engagement, evaluation Payment Model and ‘statewide’ expansion - February through April 2011 – Payer only & payer/provider meetings to develop payment model – Coordination efforts with Health Care Foundation of Greater Kansas City – Steering Committee Formation The Patient-Centered Medical Home 17
 Medical Home Initiative Framework: Framework Document defines the following Critical Design Areas: Defining medical home Supporting practice transformation Validating transformation Reforming payment Engaging patients Soliciting and selecting practices Evaluating impact The Patient-Centered Medical Home 18
Medical Home Initiative Framework: Framework Document defines the following Critical Design Areas: Defining medical home Supporting practice transformation Validating transformation Reforming payment Engaging patients Soliciting and selecting practices Evaluating impact The Patient-Centered Medical Home 18
 Objectives of the Missouri Medical Home Collaborative (MMHC) Design, implement and evaluate a Medical Home with the longterm goal of impacting all Missourians in all primary care practices Sustainably promote practice transformation through both process change and payment reform with the goal of improving patient-specific and population-based quality of care, reducing costs, and improving patient experience. Promote innovation in order to reach a broad spectrum of Missouri residents, including the under-insured and uninsured populations. The Patient-Centered Medical Home 19
Objectives of the Missouri Medical Home Collaborative (MMHC) Design, implement and evaluate a Medical Home with the longterm goal of impacting all Missourians in all primary care practices Sustainably promote practice transformation through both process change and payment reform with the goal of improving patient-specific and population-based quality of care, reducing costs, and improving patient experience. Promote innovation in order to reach a broad spectrum of Missouri residents, including the under-insured and uninsured populations. The Patient-Centered Medical Home 19
 MMHC Definition of the Medical Home: Core competencies that practices must achieve in order to become a Medical Home: Personal patient - primary care clinician relationships; Comprehensive care coordination across all settings and providers; Care management for the highest risk patients; Whole patient orientation to care, including access to needed services, and an understanding of and respect for cultural and linguistic preferences; Promotion of two-way communications and active involvement of patients in care decisions and self-management of chronic conditions; Use of patient registries to proactively identify patient and population gaps in care against evidence-based benchmarks; Adoption of Medical Home care processes, such as planned care at every visit, development of patient self-management plans and risk assessment and tailored interventions, to minimize gaps in care; Promotion of preventive care; Use of data reporting to promote quality improvement; Improve access to care through use of a variety of office-based and electronicbased approaches; and Use of quality improvement strategies and techniques to promote continuous improvement. The Patient-Centered Medical Home 20
MMHC Definition of the Medical Home: Core competencies that practices must achieve in order to become a Medical Home: Personal patient - primary care clinician relationships; Comprehensive care coordination across all settings and providers; Care management for the highest risk patients; Whole patient orientation to care, including access to needed services, and an understanding of and respect for cultural and linguistic preferences; Promotion of two-way communications and active involvement of patients in care decisions and self-management of chronic conditions; Use of patient registries to proactively identify patient and population gaps in care against evidence-based benchmarks; Adoption of Medical Home care processes, such as planned care at every visit, development of patient self-management plans and risk assessment and tailored interventions, to minimize gaps in care; Promotion of preventive care; Use of data reporting to promote quality improvement; Improve access to care through use of a variety of office-based and electronicbased approaches; and Use of quality improvement strategies and techniques to promote continuous improvement. The Patient-Centered Medical Home 20
 MMHC Participating Practice Selection Criteria: To apply to participate in the Collaborative, practices must have: – – a substantial percentage of patients covered by participating payers, have strong engaged leadership, have patients assigned to individual primary care clinicians, and meet minimum access requirements. can not be implementing an EMR at the same time At least 66% of selected practices must be MO Health. Net providers (either FFS or a network provider of a Missouri Medicaid managed care plan). Ongoing Provider Participation Requirements: Practices selected to participate in the MMMC must achieve clearly defined interim transformation milestones. The Patient-Centered Medical Home 21
MMHC Participating Practice Selection Criteria: To apply to participate in the Collaborative, practices must have: – – a substantial percentage of patients covered by participating payers, have strong engaged leadership, have patients assigned to individual primary care clinicians, and meet minimum access requirements. can not be implementing an EMR at the same time At least 66% of selected practices must be MO Health. Net providers (either FFS or a network provider of a Missouri Medicaid managed care plan). Ongoing Provider Participation Requirements: Practices selected to participate in the MMMC must achieve clearly defined interim transformation milestones. The Patient-Centered Medical Home 21
 Practice Transformation MMHC Clinical Approach: The practice transformation processes relative to the provision of care management services will be systematically rolled out as follows: – – adults with diabetes and cardiovascular disease, and children with asthma and mental health conditions (either ADHD or bipolar). highest risk patients, other chronic conditions, beginning with the most prevalent chronic conditions first, healthy patients The Patient-Centered Medical Home 22
Practice Transformation MMHC Clinical Approach: The practice transformation processes relative to the provision of care management services will be systematically rolled out as follows: – – adults with diabetes and cardiovascular disease, and children with asthma and mental health conditions (either ADHD or bipolar). highest risk patients, other chronic conditions, beginning with the most prevalent chronic conditions first, healthy patients The Patient-Centered Medical Home 22
 MMHC Technical Assistance Each Learning Collaborative accommodates up to 50 practice sites, and includes: – a pre-work period – nine all-day learning sessions held over a 24 -month period – inter-session conference calls to reinforce key lessons from the learning sessions MFH has committed to funding at least one Learning Collaborative and Health Care Foundation of Greater Kansas City expressed interest as well. Tentative Learning Collaboratives to be offered, depending on funding availability are: – – CMHC September 2011 St. Louis area primary care practices November 2011 Kansas City area primary care practices Jan/Feb 2012 Mid-Missouri area primary care practices March/April 2012 The Patient-Centered Medical Home 23
MMHC Technical Assistance Each Learning Collaborative accommodates up to 50 practice sites, and includes: – a pre-work period – nine all-day learning sessions held over a 24 -month period – inter-session conference calls to reinforce key lessons from the learning sessions MFH has committed to funding at least one Learning Collaborative and Health Care Foundation of Greater Kansas City expressed interest as well. Tentative Learning Collaboratives to be offered, depending on funding availability are: – – CMHC September 2011 St. Louis area primary care practices November 2011 Kansas City area primary care practices Jan/Feb 2012 Mid-Missouri area primary care practices March/April 2012 The Patient-Centered Medical Home 23
 MMHC Consumer Engagement: To develop an informed, engaged patient, participating practices will: – Develop consumer engagement skills, such as using motivational interviewing, using tools to gauge a patient’s level of self-management readiness, and developing with the patient a self-management plan; – Use educational materials to clarify health care roles and responsibilities; – Obtain patient input on a regular basis regarding effectiveness of meeting patient-centered goals; – Increase use of existing community-based resources; and – Integrate existing payer and employer consumer incentive programs and wellness benefits into care plans. The Patient-Centered Medical Home 24
MMHC Consumer Engagement: To develop an informed, engaged patient, participating practices will: – Develop consumer engagement skills, such as using motivational interviewing, using tools to gauge a patient’s level of self-management readiness, and developing with the patient a self-management plan; – Use educational materials to clarify health care roles and responsibilities; – Obtain patient input on a regular basis regarding effectiveness of meeting patient-centered goals; – Increase use of existing community-based resources; and – Integrate existing payer and employer consumer incentive programs and wellness benefits into care plans. The Patient-Centered Medical Home 24
 Validating Practice Transformation Provides an external documentation of efforts Required by payors to justify $ spent Verification of Medical Homeness for MMHC: – Participating practices must obtain by month 18 of the Collaborative Medical Home designation by an external accreditation body selected by the Council. – NCQA is the most recognized accreditation body The Patient-Centered Medical Home 25
Validating Practice Transformation Provides an external documentation of efforts Required by payors to justify $ spent Verification of Medical Homeness for MMHC: – Participating practices must obtain by month 18 of the Collaborative Medical Home designation by an external accreditation body selected by the Council. – NCQA is the most recognized accreditation body The Patient-Centered Medical Home 25
 Payment Reform Essential to sustainability of practice transformation Usually funded by payer participants for specified time period with goal of instituting permanent changes when the evaluation demonstrates value Most effective if a single payment model is used across payers Requires governmental oversight to mitigate anti-trust risks while payers and providers work on a payment model Need enough payer participation that at least 50% of a practice’s patient population is covered by the reformed payment arrangement The Patient-Centered Medical Home 26
Payment Reform Essential to sustainability of practice transformation Usually funded by payer participants for specified time period with goal of instituting permanent changes when the evaluation demonstrates value Most effective if a single payment model is used across payers Requires governmental oversight to mitigate anti-trust risks while payers and providers work on a payment model Need enough payer participation that at least 50% of a practice’s patient population is covered by the reformed payment arrangement The Patient-Centered Medical Home 26
 Payment Reform: Types of Payments Infrastructure payments to cover initial start-up costs, e. g. , – Forming practice teams – Building and populating a patient registry – Attending learning collaborative sessions Payments for Medical Home activities not traditionally reimbursed, such as: – – – Team meetings Pre-planning key patient appointments Care Coordination Clinical Care Management Producing patient registry and analyzing reports for QI purposes Reward or incentive payments, such as P 4 P or shared savings, to align practice incentives with desired Medical Home performance The Patient-Centered Medical Home 27
Payment Reform: Types of Payments Infrastructure payments to cover initial start-up costs, e. g. , – Forming practice teams – Building and populating a patient registry – Attending learning collaborative sessions Payments for Medical Home activities not traditionally reimbursed, such as: – – – Team meetings Pre-planning key patient appointments Care Coordination Clinical Care Management Producing patient registry and analyzing reports for QI purposes Reward or incentive payments, such as P 4 P or shared savings, to align practice incentives with desired Medical Home performance The Patient-Centered Medical Home 27
 MMHC Proposed Payment Model Year 1: in addition to traditional FFS payments – pmpm payments to practices for traditionally non-reimbursed medical home services – Pmpm payments for clinical care management for highest-risk patients with some proposed stratification based on age of member Year 2: pmpm payments continue so long as practice submits performance data, attends learning collaborative, demonstrates transformation ; If perform well on quality measures and demonstrate savings then performance incentive payment will begin based on savings from reduced ER visits and Inpatient admissions prior yr compared to current year – adjusted for high-cost outliers both prior and measurement year; small practices grouped with other like practices; up to 40% on sliding care based on quality measures. Separate shared savings calculations for Medicaid and commercial The Patient-Centered Medical Home 28
MMHC Proposed Payment Model Year 1: in addition to traditional FFS payments – pmpm payments to practices for traditionally non-reimbursed medical home services – Pmpm payments for clinical care management for highest-risk patients with some proposed stratification based on age of member Year 2: pmpm payments continue so long as practice submits performance data, attends learning collaborative, demonstrates transformation ; If perform well on quality measures and demonstrate savings then performance incentive payment will begin based on savings from reduced ER visits and Inpatient admissions prior yr compared to current year – adjusted for high-cost outliers both prior and measurement year; small practices grouped with other like practices; up to 40% on sliding care based on quality measures. Separate shared savings calculations for Medicaid and commercial The Patient-Centered Medical Home 28
 Next Steps April through June 2011 Steering Committee meets five times to develop details regarding participation requirements for providers and payment methodology Payer only meetings, as needed to address operational issues related to payment model RFP released for Learning Collaborative Vendor MFH obtains payer engagement Council reconvenes 6/20/11 to review and approve work of Steering Committee RFPs issued for learning collaborative vendor and evaluator contractor June through September 2011 Request for application released for practices Development of Learning Collaborative curriculum Practices selected October 2011 Learning Collaborative launched by beginning pre-work activities The Patient-Centered Medical Home 29
Next Steps April through June 2011 Steering Committee meets five times to develop details regarding participation requirements for providers and payment methodology Payer only meetings, as needed to address operational issues related to payment model RFP released for Learning Collaborative Vendor MFH obtains payer engagement Council reconvenes 6/20/11 to review and approve work of Steering Committee RFPs issued for learning collaborative vendor and evaluator contractor June through September 2011 Request for application released for practices Development of Learning Collaborative curriculum Practices selected October 2011 Learning Collaborative launched by beginning pre-work activities The Patient-Centered Medical Home 29
 Questions/Discussion The Patient-Centered Medical Home 30
Questions/Discussion The Patient-Centered Medical Home 30


