cd8d42f3a2d25fff8e0bd67078f45bf7.ppt
- Количество слайдов: 70
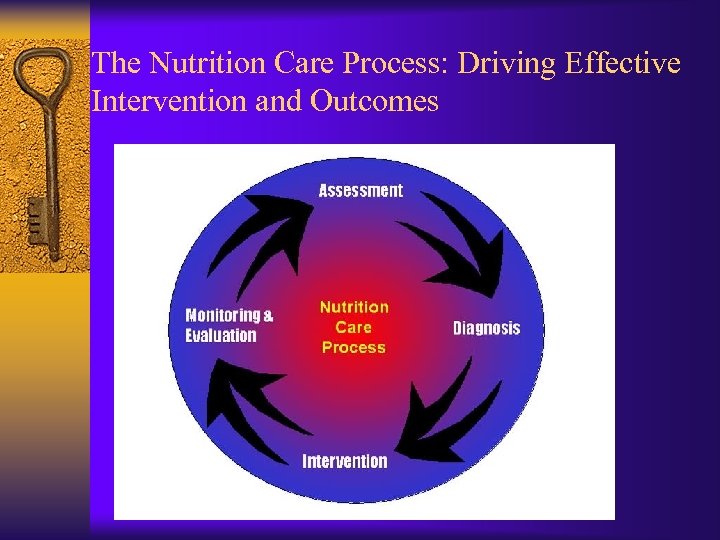 The Nutrition Care Process: Driving Effective Intervention and Outcomes
The Nutrition Care Process: Driving Effective Intervention and Outcomes
 Nutrition Care Process ¨ Process for identifying, planning for, and meeting nutritional needs ¨ Malnutrition increases: – morbidity – length of hospital stay = more care – mortality – higher costs ($$$$$$$)
Nutrition Care Process ¨ Process for identifying, planning for, and meeting nutritional needs ¨ Malnutrition increases: – morbidity – length of hospital stay = more care – mortality – higher costs ($$$$$$$)
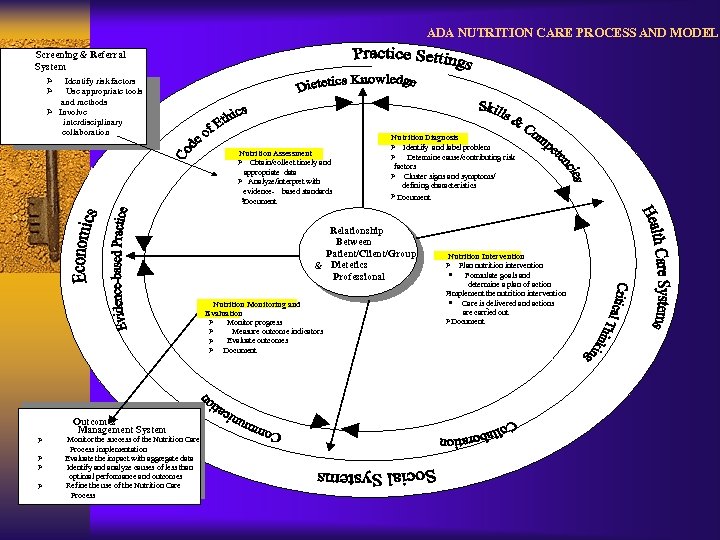 ADA NUTRITION CARE PROCESS AND MODEL Screening & Referral System Ø Ø Identify risk factors Use appropriate tools and methods Ø Involve interdisciplinary collaboration Nutrition Assessment Ø Obtain/collect timely and appropriate data Ø nalyze/interpret with A evidence- based standards Ø Document Nutrition Diagnosis Ø Identify and label problem Ø Determine cause/contributing risk factors Ø Cluster signs and symptoms/ defining characteristics Ø Document Relationship Between atient/Client/Group P & Dietetics Professional Nutrition Monitoring and Evaluation Monitor progress Ø Measure outcome indicators Ø Evaluate outcomes Ø Ø Document Ø Nutrition Intervention Ø Plan nutrition intervention · Formulate goals and determine a plan of action Implement the nutrition intervention Ø · Care is delivered and actions - are carried out ØDocument Outcomes Management System Monitor the success of the Nutrition Care Process implementation Evaluate the impact with aggregate data Ø Identify and analyze causes of less than Ø optimal performance and outcomes Refine the use of the Nutrition Care Ø Process
ADA NUTRITION CARE PROCESS AND MODEL Screening & Referral System Ø Ø Identify risk factors Use appropriate tools and methods Ø Involve interdisciplinary collaboration Nutrition Assessment Ø Obtain/collect timely and appropriate data Ø nalyze/interpret with A evidence- based standards Ø Document Nutrition Diagnosis Ø Identify and label problem Ø Determine cause/contributing risk factors Ø Cluster signs and symptoms/ defining characteristics Ø Document Relationship Between atient/Client/Group P & Dietetics Professional Nutrition Monitoring and Evaluation Monitor progress Ø Measure outcome indicators Ø Evaluate outcomes Ø Ø Document Ø Nutrition Intervention Ø Plan nutrition intervention · Formulate goals and determine a plan of action Implement the nutrition intervention Ø · Care is delivered and actions - are carried out ØDocument Outcomes Management System Monitor the success of the Nutrition Care Process implementation Evaluate the impact with aggregate data Ø Identify and analyze causes of less than Ø optimal performance and outcomes Refine the use of the Nutrition Care Ø Process
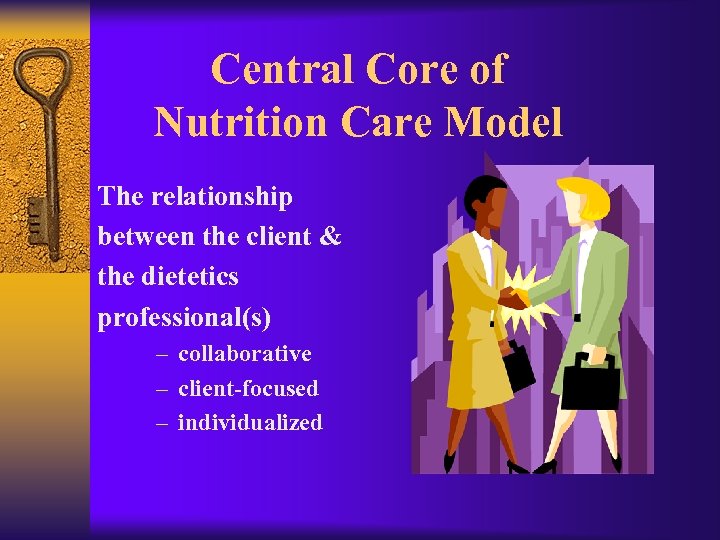 Central Core of Nutrition Care Model The relationship between the client & the dietetics professional(s) – collaborative – client-focused – individualized
Central Core of Nutrition Care Model The relationship between the client & the dietetics professional(s) – collaborative – client-focused – individualized
 Outer Rings of Nutrition Care Model ¨ Strengths brought to process by dietetics professional – dietetics knowledge – skills of critical thinking, collaboration, communication – evidence-based practice ¨ Factors of external environment – health care system, practice setting – social support, economics, education level
Outer Rings of Nutrition Care Model ¨ Strengths brought to process by dietetics professional – dietetics knowledge – skills of critical thinking, collaboration, communication – evidence-based practice ¨ Factors of external environment – health care system, practice setting – social support, economics, education level
 ADA’s Nutrition Care Process Steps ¨ Nutrition Assessment ¨ Nutrition Diagnosis ¨ Nutrition Intervention ¨ Nutrition Monitoring and Evaluation For more information, access the ADA member page in the Quality Management section. http: //www. eatright. org/Member/83_12962. cfm
ADA’s Nutrition Care Process Steps ¨ Nutrition Assessment ¨ Nutrition Diagnosis ¨ Nutrition Intervention ¨ Nutrition Monitoring and Evaluation For more information, access the ADA member page in the Quality Management section. http: //www. eatright. org/Member/83_12962. cfm
 Nutrition Assessment Components ¨ Gather data, considering – Dietary intake – Nutrition related consequences of health and disease condition – Psycho-social, functional, and behavioral factors – Knowledge, readiness, and potential for change ¨ Compare to relevant standards ¨ Identify possible problem areas
Nutrition Assessment Components ¨ Gather data, considering – Dietary intake – Nutrition related consequences of health and disease condition – Psycho-social, functional, and behavioral factors – Knowledge, readiness, and potential for change ¨ Compare to relevant standards ¨ Identify possible problem areas
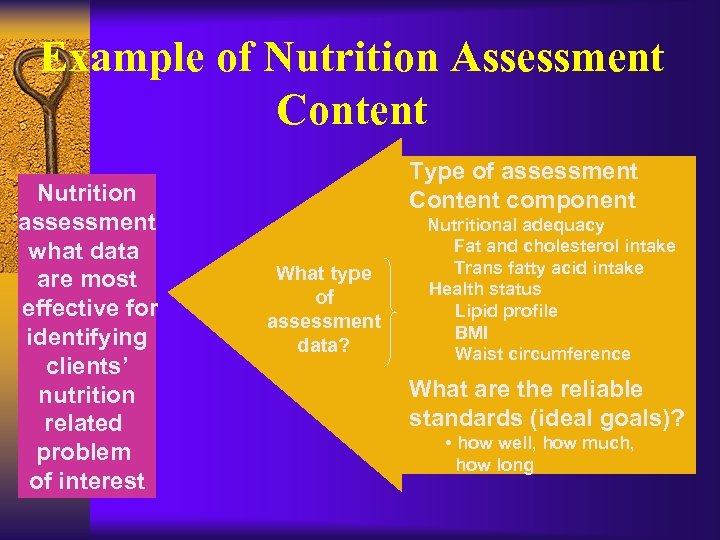 Example of Nutrition Assessment Content Nutrition assessment what data are most effective for identifying clients’ nutrition related problem of interest Type of assessment Content component What type of assessment data? Nutritional adequacy Fat and cholesterol intake Trans fatty acid intake Health status Lipid profile BMI Waist circumference What are the reliable standards (ideal goals)? • how well, how much, how long
Example of Nutrition Assessment Content Nutrition assessment what data are most effective for identifying clients’ nutrition related problem of interest Type of assessment Content component What type of assessment data? Nutritional adequacy Fat and cholesterol intake Trans fatty acid intake Health status Lipid profile BMI Waist circumference What are the reliable standards (ideal goals)? • how well, how much, how long
 How do we get from Assessment to Intervention? Nutrition Diagnosis A crucial element of providing quality nutrition care
How do we get from Assessment to Intervention? Nutrition Diagnosis A crucial element of providing quality nutrition care
 Nutrition Diagnosis Purpose ¨ Identify and label the nutrition problem ¨ Nutrition diagnosis NOT medical diagnosis ¨ EXPLICIT statement of nutrition diagnosis Note: Documentation is an on-going process that supports all the steps in the Nutrition Care Process
Nutrition Diagnosis Purpose ¨ Identify and label the nutrition problem ¨ Nutrition diagnosis NOT medical diagnosis ¨ EXPLICIT statement of nutrition diagnosis Note: Documentation is an on-going process that supports all the steps in the Nutrition Care Process
 Nutrition Intervention Purpose ¨ Plan and implement purposeful actions to address the identified nutrition problem – – bring about change set goals and expected outcomes client-driven based on scientific principles and best available evidence Note: Documentation is an on-going process that supports all the steps in the Nutrition Care Process
Nutrition Intervention Purpose ¨ Plan and implement purposeful actions to address the identified nutrition problem – – bring about change set goals and expected outcomes client-driven based on scientific principles and best available evidence Note: Documentation is an on-going process that supports all the steps in the Nutrition Care Process
 Nutrition Monitoring & Evaluation Purpose ¨ Determine the progress that is being made toward the clien goals or desired outcomes Monitoring: review and measurement of status at scheduled times ¨ Evaluation: systematic comparison with previous status, intervention goals, reference standard Note: Documentation is an on-going process that supports all the steps in the Nutrition Care Process
Nutrition Monitoring & Evaluation Purpose ¨ Determine the progress that is being made toward the clien goals or desired outcomes Monitoring: review and measurement of status at scheduled times ¨ Evaluation: systematic comparison with previous status, intervention goals, reference standard Note: Documentation is an on-going process that supports all the steps in the Nutrition Care Process
 Nutrition Screening ¨ Purpose: To quickly identify individuals who are malnourished or at nutritional risk and to determine if a more detailed assessment is warranted ¨ Usually completed by DTR, nurse, physician, or other qualified health care professional ¨ At-risk patients referred to RD
Nutrition Screening ¨ Purpose: To quickly identify individuals who are malnourished or at nutritional risk and to determine if a more detailed assessment is warranted ¨ Usually completed by DTR, nurse, physician, or other qualified health care professional ¨ At-risk patients referred to RD
 Characteristics of Nutrition Screening ¨ Simple and easy to complete ¨ Routine data ¨ Cost effective ¨ Effective in identifying nutritional problems ¨ Reliable and valid
Characteristics of Nutrition Screening ¨ Simple and easy to complete ¨ Routine data ¨ Cost effective ¨ Effective in identifying nutritional problems ¨ Reliable and valid
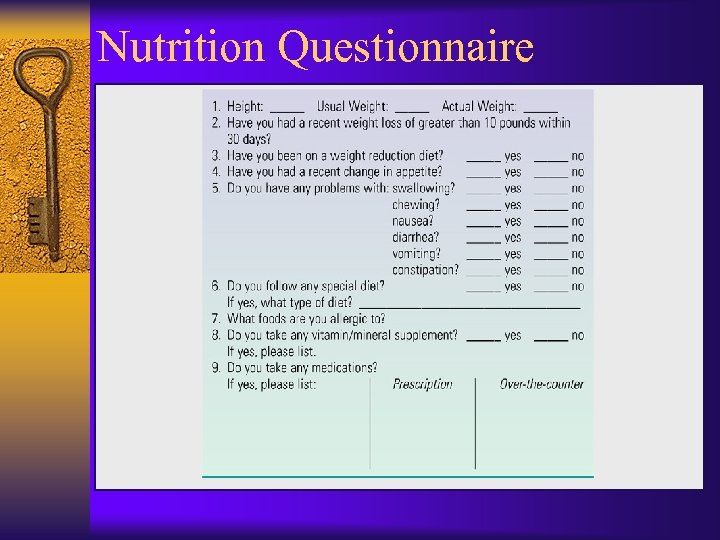 Nutrition Questionnaire
Nutrition Questionnaire
 Nutrition Screening Tools ¨ Acute-care hospital or residential setting ¨ Perinatal service ¨ Pediatric practice ¨ Malnutrition Universal Screening Tool (MUST) ¨ Nutrition Screening Initiative (NSI)
Nutrition Screening Tools ¨ Acute-care hospital or residential setting ¨ Perinatal service ¨ Pediatric practice ¨ Malnutrition Universal Screening Tool (MUST) ¨ Nutrition Screening Initiative (NSI)
 Food and Nutrient Intake Risk Factors ¨ Calorie or protein, vitamin and mineral intake greater or less than required ¨ Swallowing difficulties ¨ Gastrointestinal disturbances, bowel irregularity ¨ Impaired cognitive function or depression ¨ Unusual food habits (pica) ¨ Misuse of supplements ¨ Restricted diet ¨ Inability or unwillingness to consume food ¨ Increase or decrease in activities of daily living Hammond KA. Assessment: Dietary and Clinical Data. In Krause, 12 th edition, p. 386
Food and Nutrient Intake Risk Factors ¨ Calorie or protein, vitamin and mineral intake greater or less than required ¨ Swallowing difficulties ¨ Gastrointestinal disturbances, bowel irregularity ¨ Impaired cognitive function or depression ¨ Unusual food habits (pica) ¨ Misuse of supplements ¨ Restricted diet ¨ Inability or unwillingness to consume food ¨ Increase or decrease in activities of daily living Hammond KA. Assessment: Dietary and Clinical Data. In Krause, 12 th edition, p. 386
 Psychological/Social Risk Factors ¨ ¨ ¨ ¨ ¨ Language barriers Low literacy Cultural or religious factors Emotional disturbances associated with feeding difficulties (e. g. , depression) Limited resources for food preparation or obtaining food or supplies Alcohol or drug addiction Limited or low income Lack of ability to communicate needs Limited use or understanding of community resources Hammond KA. Assessment: Dietary and Clinical Data. In Krause, 12 th edition, p. 386
Psychological/Social Risk Factors ¨ ¨ ¨ ¨ ¨ Language barriers Low literacy Cultural or religious factors Emotional disturbances associated with feeding difficulties (e. g. , depression) Limited resources for food preparation or obtaining food or supplies Alcohol or drug addiction Limited or low income Lack of ability to communicate needs Limited use or understanding of community resources Hammond KA. Assessment: Dietary and Clinical Data. In Krause, 12 th edition, p. 386
 Physical Risk Factors ¨ Extreme age (adults >80 years, premature infants, very young children) ¨ Pregnancy: adolescent, closely spaced, or three or more pregnancies ¨ Alterations in anthropometric measurements, marked overweight/ underweight for age, height, both; depressed somatic fat and muscle stores ¨ NOTE: recent unintentional weight loss is more predictive of morbidity/mortality than wt/ht status Hammond KA. Assessment: Dietary and Clinical Data. In Krause, 12 th edition, p. 386
Physical Risk Factors ¨ Extreme age (adults >80 years, premature infants, very young children) ¨ Pregnancy: adolescent, closely spaced, or three or more pregnancies ¨ Alterations in anthropometric measurements, marked overweight/ underweight for age, height, both; depressed somatic fat and muscle stores ¨ NOTE: recent unintentional weight loss is more predictive of morbidity/mortality than wt/ht status Hammond KA. Assessment: Dietary and Clinical Data. In Krause, 12 th edition, p. 386
 Physical Risk Factors (cont) ¨ Chronic renal/cardiac disease, diabetes, pressure ulcers, cancer, AIDS, GI complications, hypermetabolic stress, immobility, osteoporosis, neurological impairments, visual impairments Hammond KA. Assessment: Dietary and Clinical Data. In Krause, 12 th edition, p. 386
Physical Risk Factors (cont) ¨ Chronic renal/cardiac disease, diabetes, pressure ulcers, cancer, AIDS, GI complications, hypermetabolic stress, immobility, osteoporosis, neurological impairments, visual impairments Hammond KA. Assessment: Dietary and Clinical Data. In Krause, 12 th edition, p. 386
 Abnormal Laboratory Values ¨ Visceral proteins (albumin, prealbumin, transferrin) ¨ Lipid profile (cholesterol, HDL, LDL, triglycerides) ¨ Hemoglobin, hematocrit, other blood tests ¨ BUN, creatinine, electrolytes ¨ Fasting and PP blood glucose levels, A 1 C Hammond KA. Assessment: Dietary and Clinical Data. In Krause, 12 th edition, p. 386
Abnormal Laboratory Values ¨ Visceral proteins (albumin, prealbumin, transferrin) ¨ Lipid profile (cholesterol, HDL, LDL, triglycerides) ¨ Hemoglobin, hematocrit, other blood tests ¨ BUN, creatinine, electrolytes ¨ Fasting and PP blood glucose levels, A 1 C Hammond KA. Assessment: Dietary and Clinical Data. In Krause, 12 th edition, p. 386
 Medications ¨ Chronic use ¨ Multiple and concurrent use (polypharmacy) ¨ Drug-nutrient interactions
Medications ¨ Chronic use ¨ Multiple and concurrent use (polypharmacy) ¨ Drug-nutrient interactions
 Joint Commission Standards Drive Nutrition Screening in Health Care Organizations
Joint Commission Standards Drive Nutrition Screening in Health Care Organizations
 Nutrition Care Process: Screening ¨ The Joint Commission (TJC) requires that nutritional risk be identified within 24 hrs in all hospitalized pts ¨ TJC also requires nutrition screening in accredited ambulatory facilities ¨ Standards of Care protocols determines process; evidence-based guidelines ¨ Use simple techniques, available info ¨ May be done by other than RD ¨ Usually simple form with targeted info
Nutrition Care Process: Screening ¨ The Joint Commission (TJC) requires that nutritional risk be identified within 24 hrs in all hospitalized pts ¨ TJC also requires nutrition screening in accredited ambulatory facilities ¨ Standards of Care protocols determines process; evidence-based guidelines ¨ Use simple techniques, available info ¨ May be done by other than RD ¨ Usually simple form with targeted info
 Standard PC. 2. 20: The hospital defines in writing the data and information gathered during assessment and reassessment Elements of Performance ¨ The information. . . to be gathered during the initial assessment includes the following, as relevant. . . : – Each patient's nutrition and hydration status, as appropriate ¨ The hospital has defined criteria for when nutritional plans must be developed
Standard PC. 2. 20: The hospital defines in writing the data and information gathered during assessment and reassessment Elements of Performance ¨ The information. . . to be gathered during the initial assessment includes the following, as relevant. . . : – Each patient's nutrition and hydration status, as appropriate ¨ The hospital has defined criteria for when nutritional plans must be developed
 Standard PC. 2. 120: The hospital defines in writing the time frame(s) for conducting the initial assessment(s). Elements of Performance ¨ A nutritional screening, when warranted by the patient's needs or condition, is completed within no more than 24 hours of inpatient admission – CAMH online version, 2006
Standard PC. 2. 120: The hospital defines in writing the time frame(s) for conducting the initial assessment(s). Elements of Performance ¨ A nutritional screening, when warranted by the patient's needs or condition, is completed within no more than 24 hours of inpatient admission – CAMH online version, 2006
 Standards Relating to Nutrition Assessment Standard PC. 2. 130 ¨ Initial assessments are performed as defined by the hospital. Standard PC. 2. 150 ¨ Patients are reassessed 5 as needed. CAMH online version, 2006
Standards Relating to Nutrition Assessment Standard PC. 2. 130 ¨ Initial assessments are performed as defined by the hospital. Standard PC. 2. 150 ¨ Patients are reassessed 5 as needed. CAMH online version, 2006
 Screening for Malnutrition in Acute Care Settings “The consensus of the committee is that while screening for nutrition risk in the acute care setting is crucial, the JCAHO requirement that nutrition screening be completed within 24 hours of admission is not evidence-based and may produce inaccurate and misleading results. ” • Institute of Medicine, 1999
Screening for Malnutrition in Acute Care Settings “The consensus of the committee is that while screening for nutrition risk in the acute care setting is crucial, the JCAHO requirement that nutrition screening be completed within 24 hours of admission is not evidence-based and may produce inaccurate and misleading results. ” • Institute of Medicine, 1999
 Commonly Used Criteria for Nutrition Risk Screening-Acute Care ¨ Diagnosis ¨ Problems with ¨ Weight chewing or swallowing ¨ Diarrhea ¨ Constipation ¨ Food dislikes or intolerance ¨ Weight change ¨ Need for diet modification or education ¨ Laboratory values (s. albumin, cholesterol, hemoglobin, TLC Institute of Medicine, 1999
Commonly Used Criteria for Nutrition Risk Screening-Acute Care ¨ Diagnosis ¨ Problems with ¨ Weight chewing or swallowing ¨ Diarrhea ¨ Constipation ¨ Food dislikes or intolerance ¨ Weight change ¨ Need for diet modification or education ¨ Laboratory values (s. albumin, cholesterol, hemoglobin, TLC Institute of Medicine, 1999
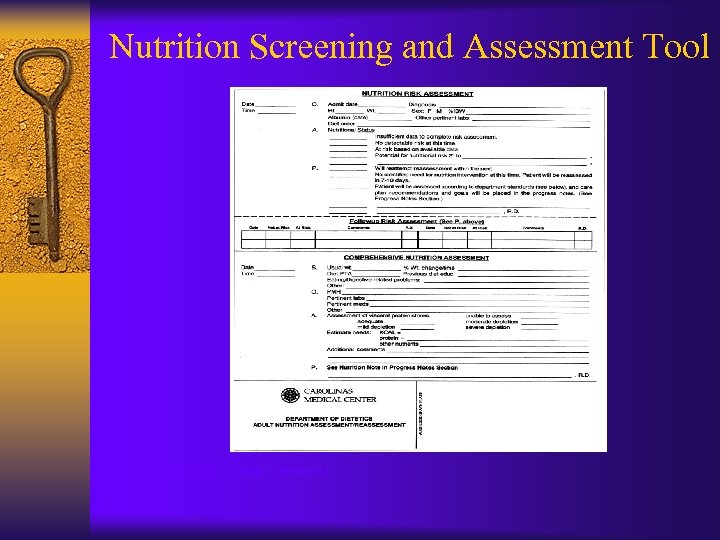 Nutrition Screening and Assessment Tool Courtesy Carolinas Medical Center, Charlotte, N. C.
Nutrition Screening and Assessment Tool Courtesy Carolinas Medical Center, Charlotte, N. C.
 Prevalence of Nutrition Risk in Acute Care ¨ The prevalence of nutrition risk will vary depending on the population screened and the criteria used for screening ¨ In published studies, prevalence of malnutrition in hospitalized patients has ranged from 12% to more than 50% ¨ There is little published data regarding nutrition screening for other purposes
Prevalence of Nutrition Risk in Acute Care ¨ The prevalence of nutrition risk will vary depending on the population screened and the criteria used for screening ¨ In published studies, prevalence of malnutrition in hospitalized patients has ranged from 12% to more than 50% ¨ There is little published data regarding nutrition screening for other purposes
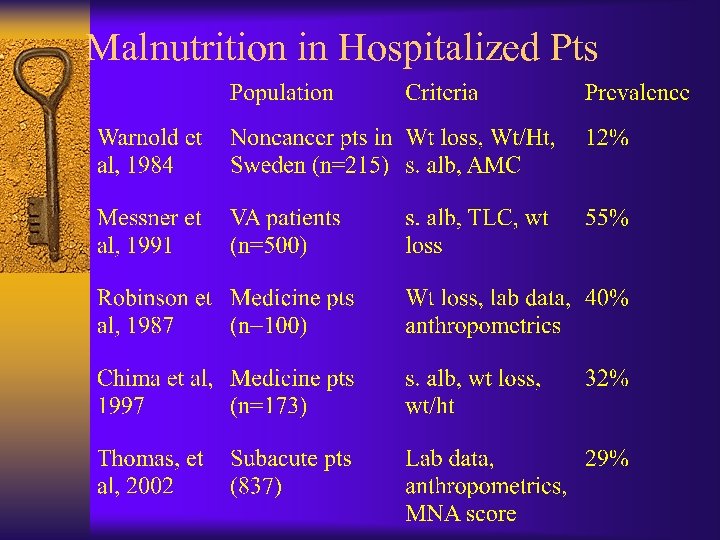 Malnutrition in Hospitalized Pts
Malnutrition in Hospitalized Pts
 CNM Nutrition Screening Survey Chima and Seher, 2007 ¨ Blast email sent to 1668 members of the Clinical Nutrition Management dietetic practice group in May, 2007 ¨ 522 usable surveys were returned, for a response rate of 31%
CNM Nutrition Screening Survey Chima and Seher, 2007 ¨ Blast email sent to 1668 members of the Clinical Nutrition Management dietetic practice group in May, 2007 ¨ 522 usable surveys were returned, for a response rate of 31%
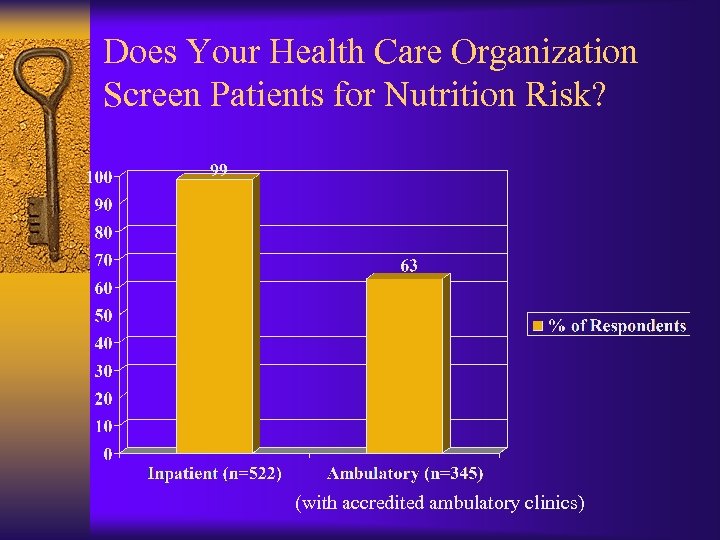 Does Your Health Care Organization Screen Patients for Nutrition Risk? (with accredited ambulatory clinics)
Does Your Health Care Organization Screen Patients for Nutrition Risk? (with accredited ambulatory clinics)
 Screening in Acute Care
Screening in Acute Care
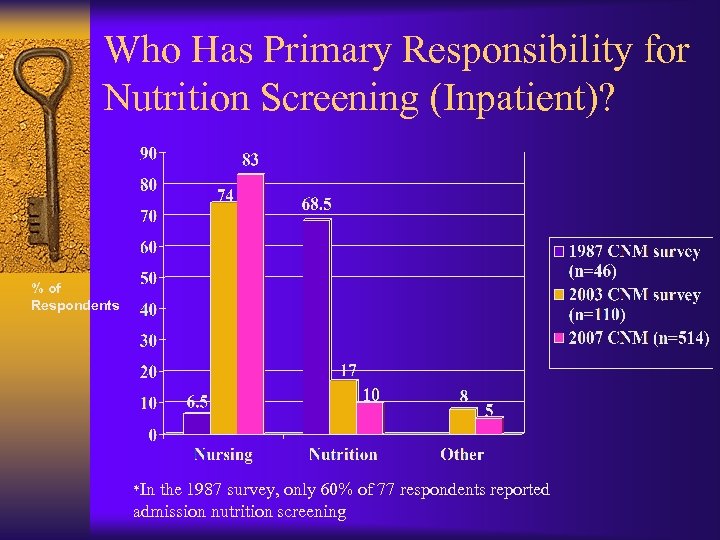 Who Has Primary Responsibility for Nutrition Screening (Inpatient)? % of Respondents *In the 1987 survey, only 60% of 77 respondents reported admission nutrition screening
Who Has Primary Responsibility for Nutrition Screening (Inpatient)? % of Respondents *In the 1987 survey, only 60% of 77 respondents reported admission nutrition screening
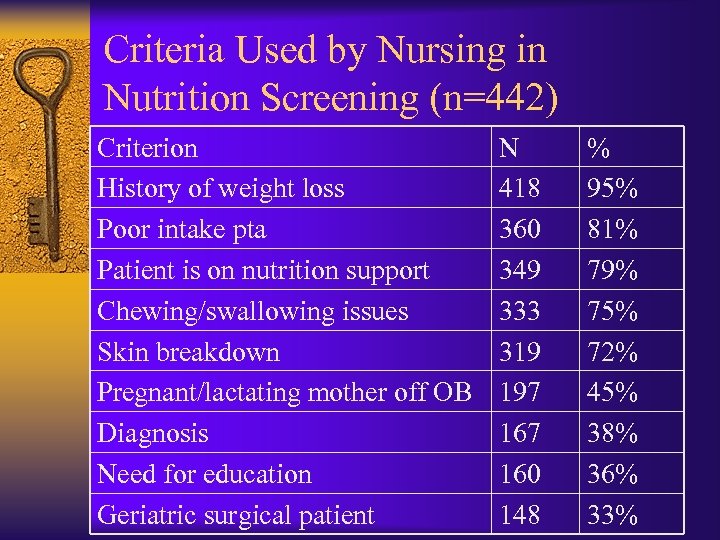 Criteria Used by Nursing in Nutrition Screening (n=442) Criterion History of weight loss Poor intake pta Patient is on nutrition support Chewing/swallowing issues Skin breakdown Pregnant/lactating mother off OB Diagnosis Need for education Geriatric surgical patient N 418 360 349 333 319 197 160 148 % 95% 81% 79% 75% 72% 45% 38% 36% 33%
Criteria Used by Nursing in Nutrition Screening (n=442) Criterion History of weight loss Poor intake pta Patient is on nutrition support Chewing/swallowing issues Skin breakdown Pregnant/lactating mother off OB Diagnosis Need for education Geriatric surgical patient N 418 360 349 333 319 197 160 148 % 95% 81% 79% 75% 72% 45% 38% 36% 33%
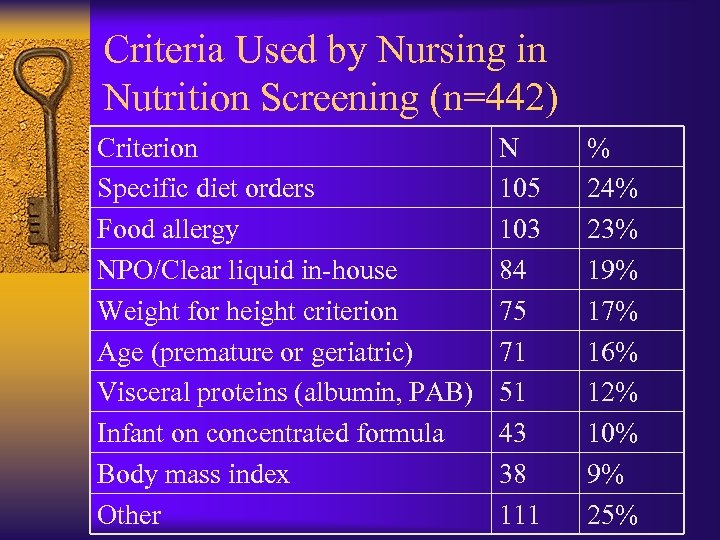 Criteria Used by Nursing in Nutrition Screening (n=442) Criterion Specific diet orders Food allergy NPO/Clear liquid in-house Weight for height criterion Age (premature or geriatric) Visceral proteins (albumin, PAB) Infant on concentrated formula Body mass index Other N 105 103 84 75 71 51 43 38 111 % 24% 23% 19% 17% 16% 12% 10% 9% 25%
Criteria Used by Nursing in Nutrition Screening (n=442) Criterion Specific diet orders Food allergy NPO/Clear liquid in-house Weight for height criterion Age (premature or geriatric) Visceral proteins (albumin, PAB) Infant on concentrated formula Body mass index Other N 105 103 84 75 71 51 43 38 111 % 24% 23% 19% 17% 16% 12% 10% 9% 25%
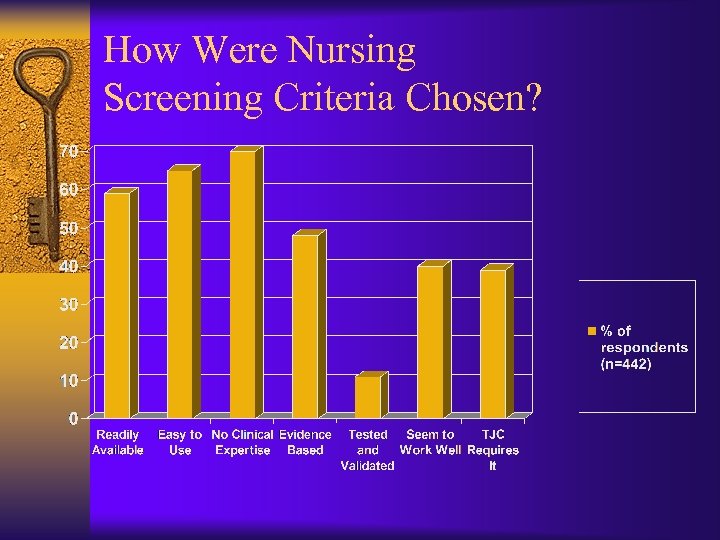 How Were Nursing Screening Criteria Chosen?
How Were Nursing Screening Criteria Chosen?
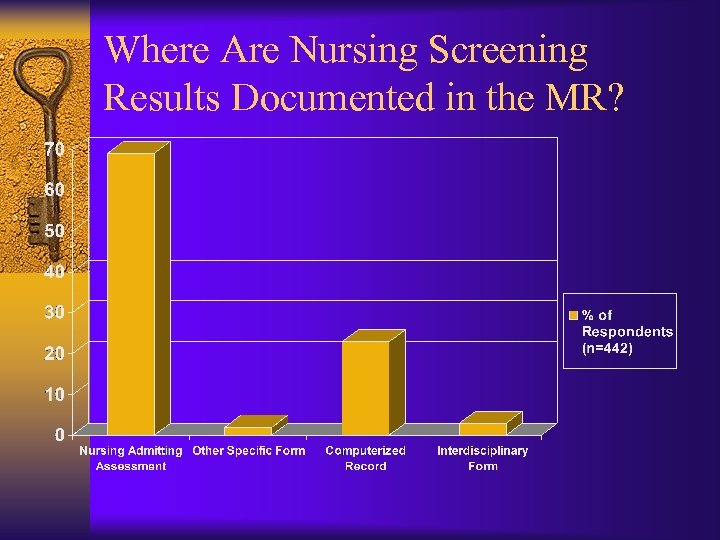 Where Are Nursing Screening Results Documented in the MR?
Where Are Nursing Screening Results Documented in the MR?
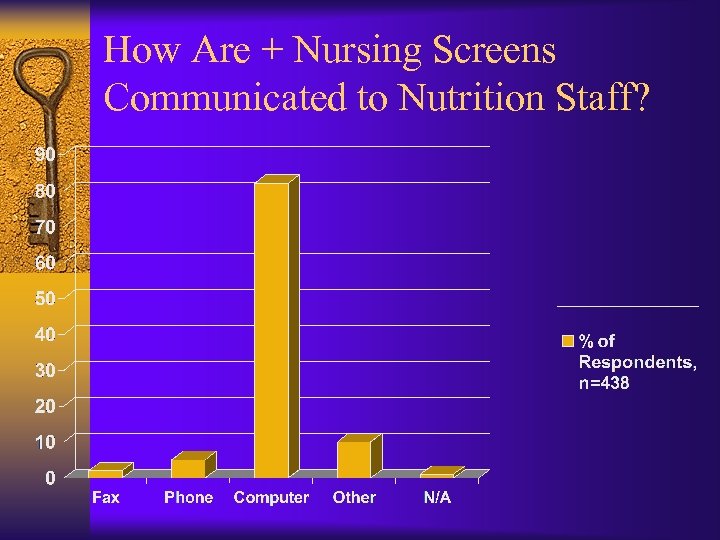 How Are + Nursing Screens Communicated to Nutrition Staff?
How Are + Nursing Screens Communicated to Nutrition Staff?
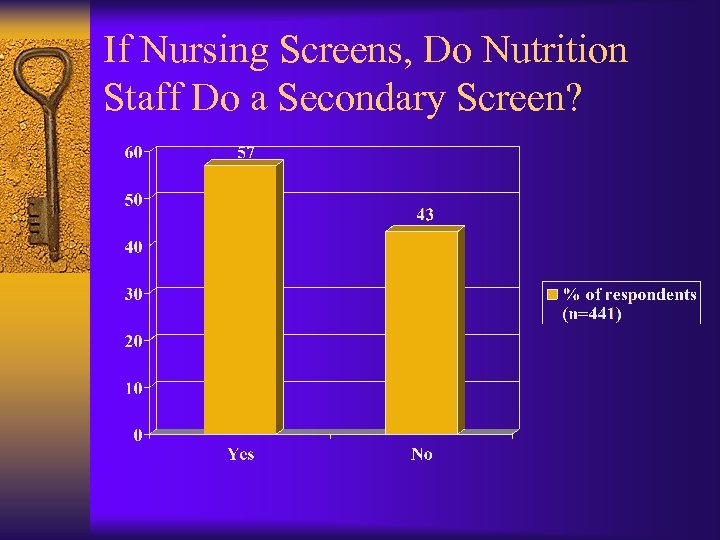 If Nursing Screens, Do Nutrition Staff Do a Secondary Screen?
If Nursing Screens, Do Nutrition Staff Do a Secondary Screen?
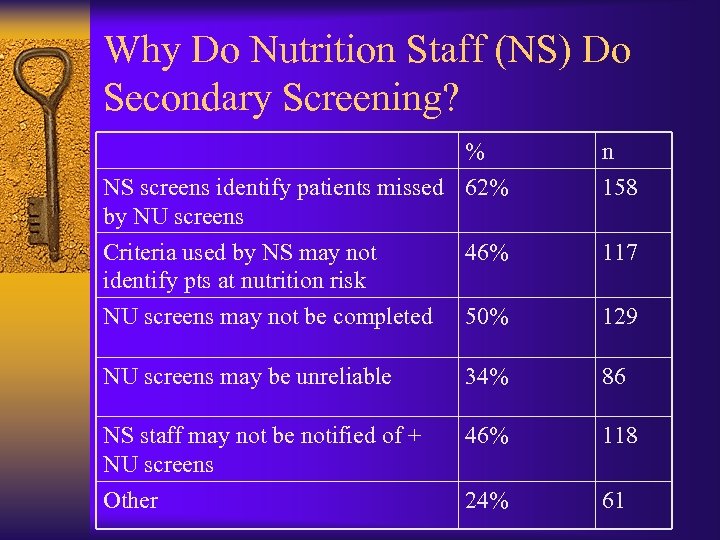 Why Do Nutrition Staff (NS) Do Secondary Screening? % NS screens identify patients missed 62% by NU screens n 158 Criteria used by NS may not identify pts at nutrition risk 46% 117 NU screens may not be completed 50% 129 NU screens may be unreliable 34% 86 NS staff may not be notified of + NU screens Other 46% 118 24% 61
Why Do Nutrition Staff (NS) Do Secondary Screening? % NS screens identify patients missed 62% by NU screens n 158 Criteria used by NS may not identify pts at nutrition risk 46% 117 NU screens may not be completed 50% 129 NU screens may be unreliable 34% 86 NS staff may not be notified of + NU screens Other 46% 118 24% 61
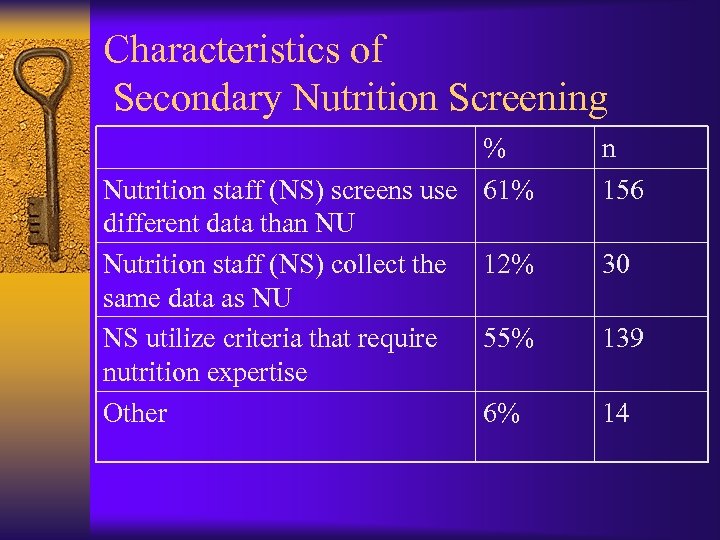 Characteristics of Secondary Nutrition Screening % Nutrition staff (NS) screens use 61% different data than NU Nutrition staff (NS) collect the 12% same data as NU NS utilize criteria that require 55% nutrition expertise Other 6% n 156 30 139 14
Characteristics of Secondary Nutrition Screening % Nutrition staff (NS) screens use 61% different data than NU Nutrition staff (NS) collect the 12% same data as NU NS utilize criteria that require 55% nutrition expertise Other 6% n 156 30 139 14
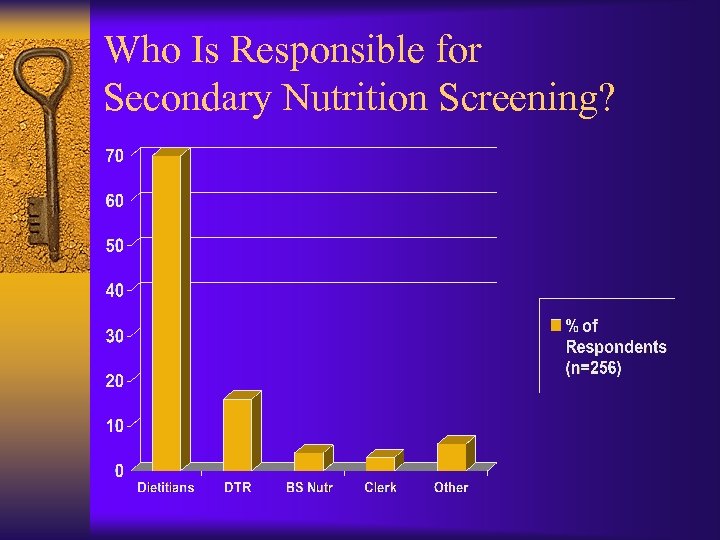 Who Is Responsible for Secondary Nutrition Screening?
Who Is Responsible for Secondary Nutrition Screening?
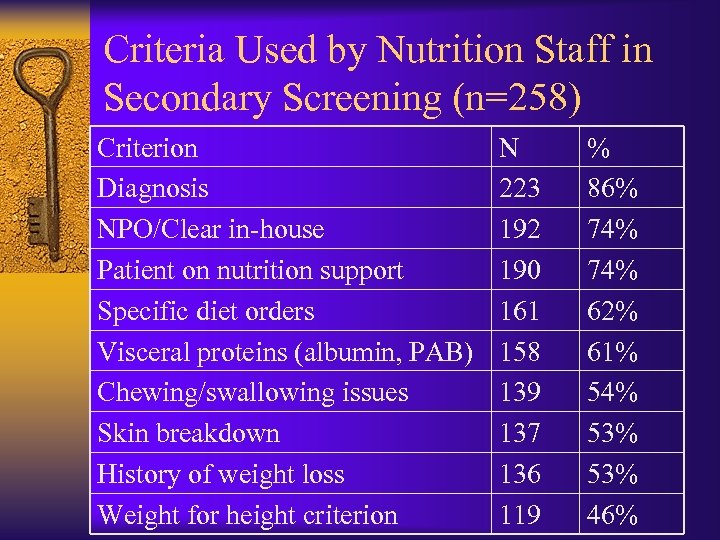 Criteria Used by Nutrition Staff in Secondary Screening (n=258) Criterion Diagnosis NPO/Clear in-house Patient on nutrition support Specific diet orders Visceral proteins (albumin, PAB) Chewing/swallowing issues Skin breakdown History of weight loss Weight for height criterion N 223 192 190 161 158 139 137 136 119 % 86% 74% 62% 61% 54% 53% 46%
Criteria Used by Nutrition Staff in Secondary Screening (n=258) Criterion Diagnosis NPO/Clear in-house Patient on nutrition support Specific diet orders Visceral proteins (albumin, PAB) Chewing/swallowing issues Skin breakdown History of weight loss Weight for height criterion N 223 192 190 161 158 139 137 136 119 % 86% 74% 62% 61% 54% 53% 46%
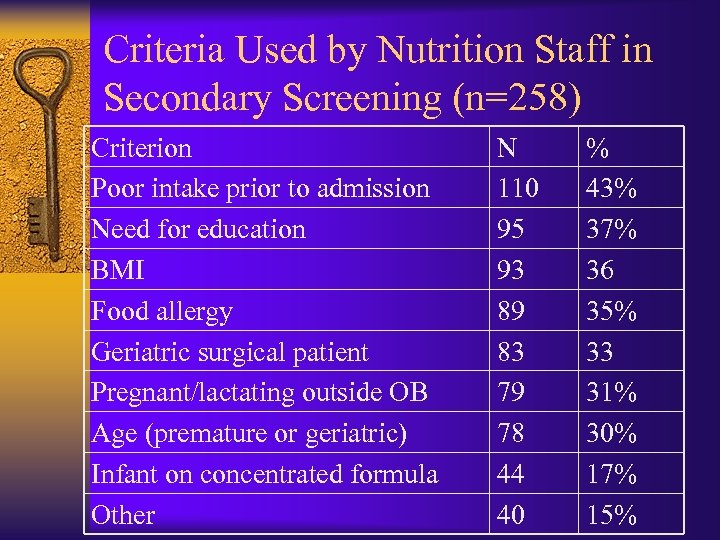 Criteria Used by Nutrition Staff in Secondary Screening (n=258) Criterion Poor intake prior to admission Need for education BMI Food allergy Geriatric surgical patient Pregnant/lactating outside OB Age (premature or geriatric) Infant on concentrated formula Other N 110 95 93 89 83 79 78 44 40 % 43% 37% 36 35% 33 31% 30% 17% 15%
Criteria Used by Nutrition Staff in Secondary Screening (n=258) Criterion Poor intake prior to admission Need for education BMI Food allergy Geriatric surgical patient Pregnant/lactating outside OB Age (premature or geriatric) Infant on concentrated formula Other N 110 95 93 89 83 79 78 44 40 % 43% 37% 36 35% 33 31% 30% 17% 15%
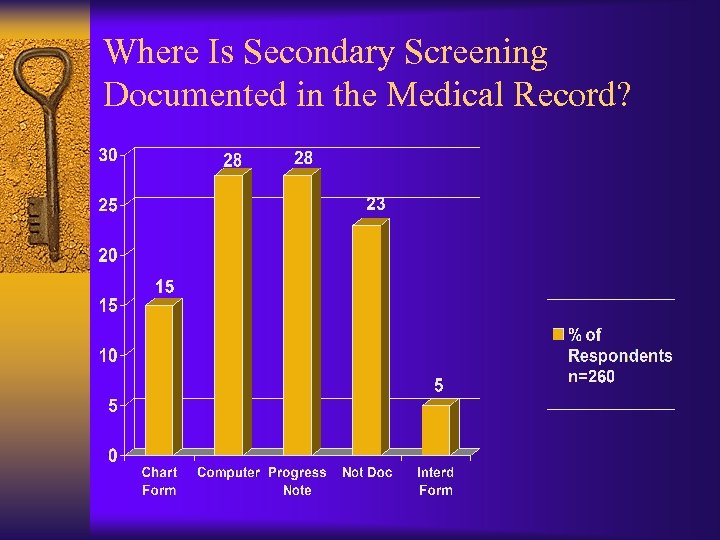 Where Is Secondary Screening Documented in the Medical Record?
Where Is Secondary Screening Documented in the Medical Record?
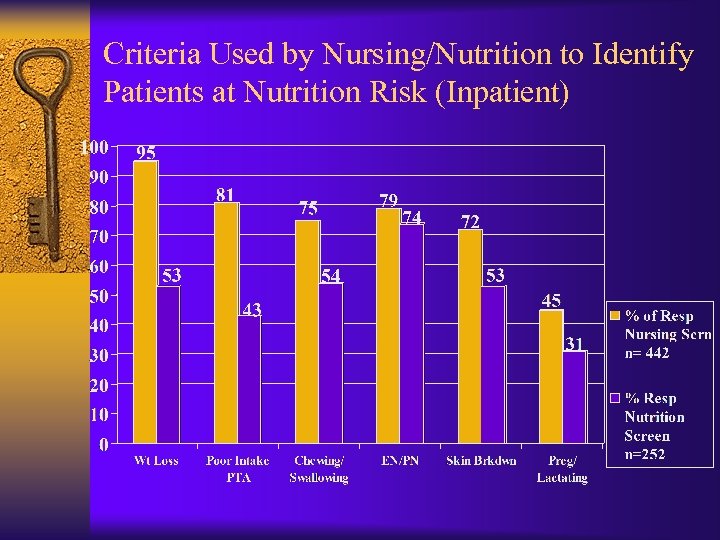 Criteria Used by Nursing/Nutrition to Identify Patients at Nutrition Risk (Inpatient)
Criteria Used by Nursing/Nutrition to Identify Patients at Nutrition Risk (Inpatient)
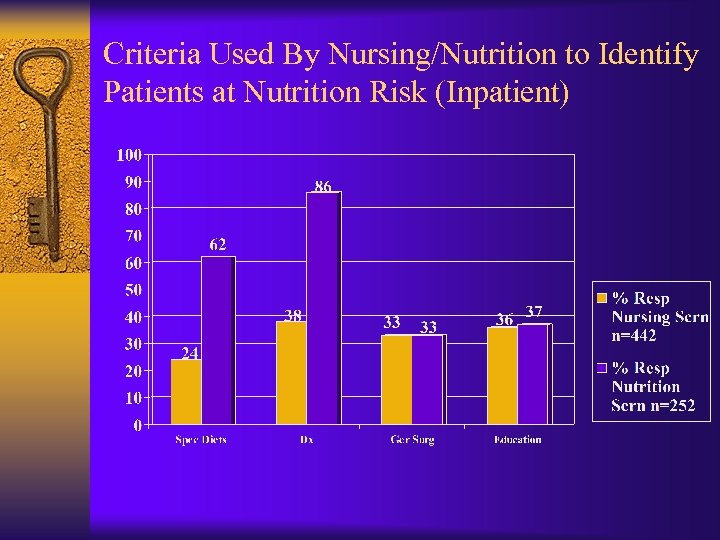 Criteria Used By Nursing/Nutrition to Identify Patients at Nutrition Risk (Inpatient)
Criteria Used By Nursing/Nutrition to Identify Patients at Nutrition Risk (Inpatient)
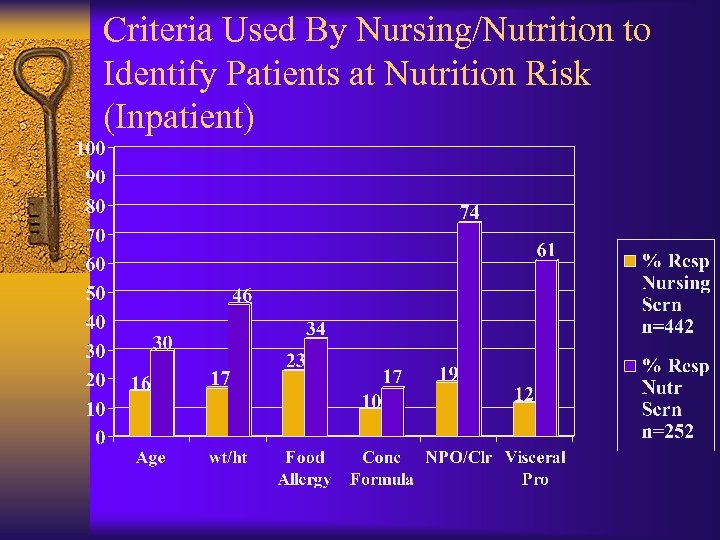 Criteria Used By Nursing/Nutrition to Identify Patients at Nutrition Risk (Inpatient)
Criteria Used By Nursing/Nutrition to Identify Patients at Nutrition Risk (Inpatient)
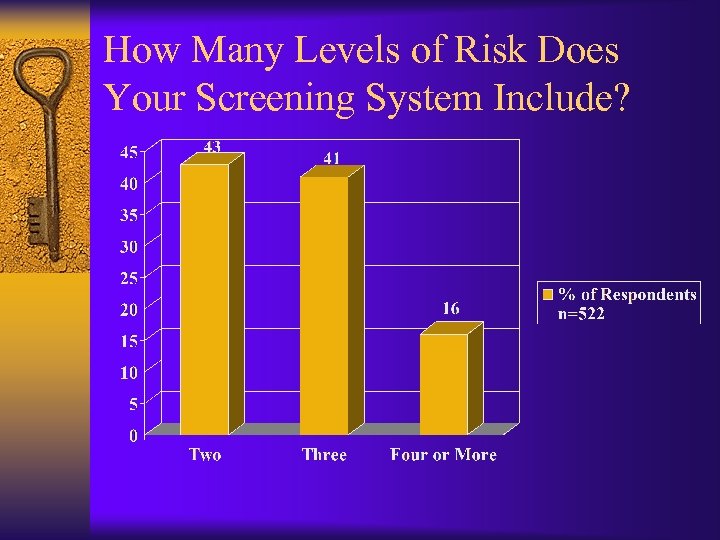 How Many Levels of Risk Does Your Screening System Include?
How Many Levels of Risk Does Your Screening System Include?
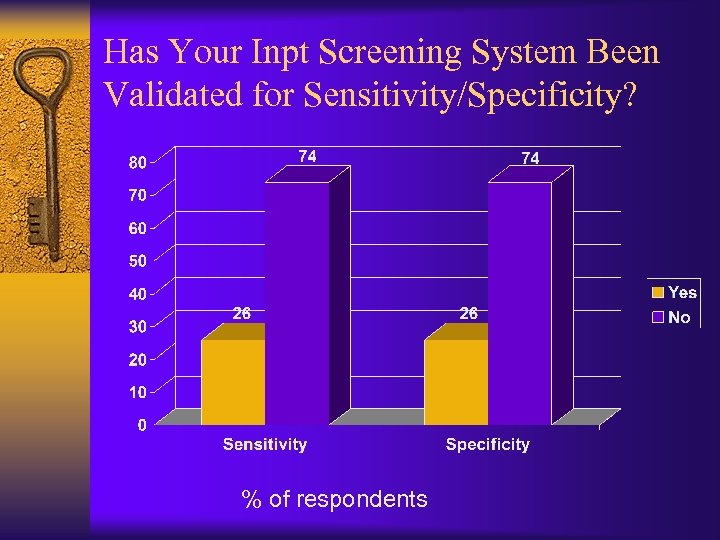 Has Your Inpt Screening System Been Validated for Sensitivity/Specificity? % of respondents
Has Your Inpt Screening System Been Validated for Sensitivity/Specificity? % of respondents
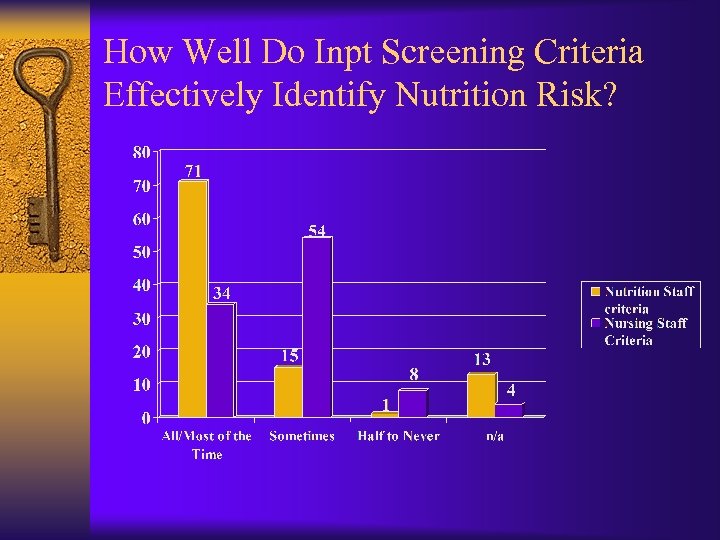 How Well Do Inpt Screening Criteria Effectively Identify Nutrition Risk?
How Well Do Inpt Screening Criteria Effectively Identify Nutrition Risk?
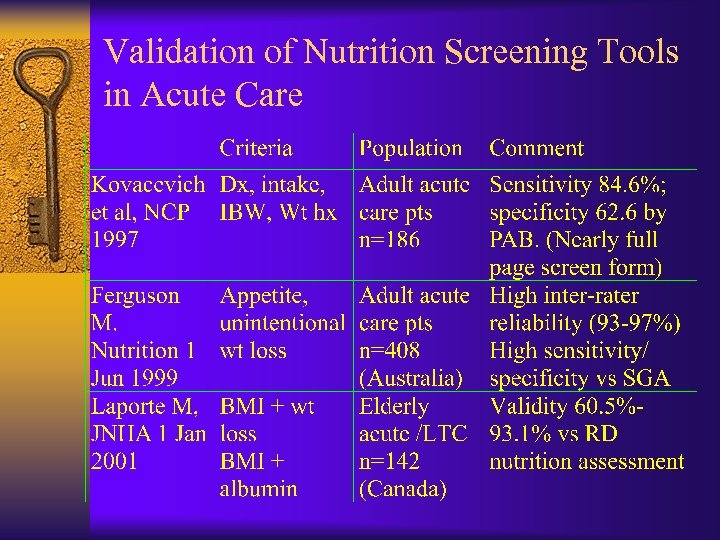 Validation of Nutrition Screening Tools in Acute Care
Validation of Nutrition Screening Tools in Acute Care
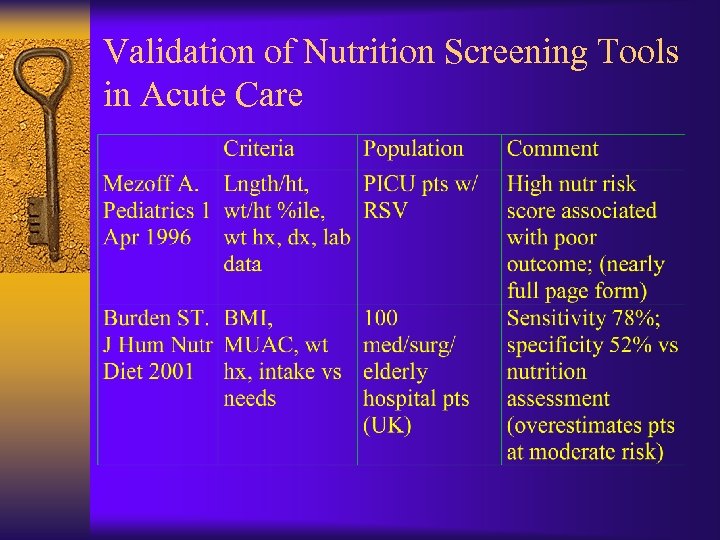 Validation of Nutrition Screening Tools in Acute Care
Validation of Nutrition Screening Tools in Acute Care
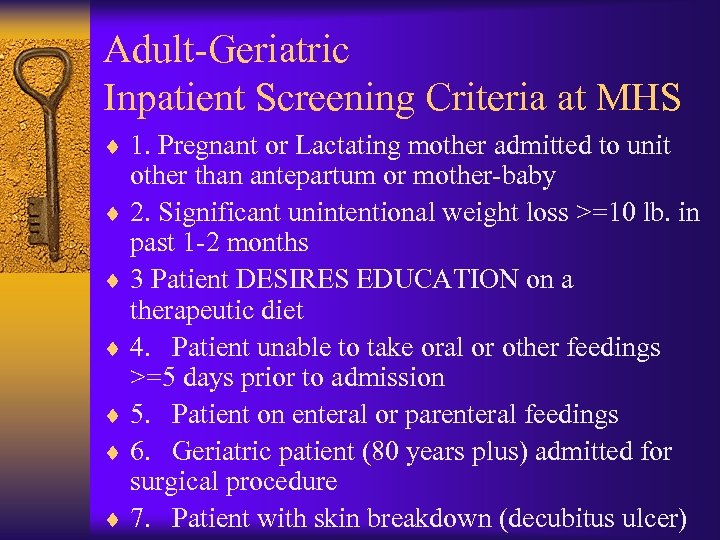 Adult-Geriatric Inpatient Screening Criteria at MHS ¨ 1. Pregnant or Lactating mother admitted to unit other than antepartum or mother-baby ¨ 2. Significant unintentional weight loss >=10 lb. in past 1 -2 months ¨ 3 Patient DESIRES EDUCATION on a therapeutic diet ¨ 4. Patient unable to take oral or other feedings >=5 days prior to admission ¨ 5. Patient on enteral or parenteral feedings ¨ 6. Geriatric patient (80 years plus) admitted for surgical procedure ¨ 7. Patient with skin breakdown (decubitus ulcer)
Adult-Geriatric Inpatient Screening Criteria at MHS ¨ 1. Pregnant or Lactating mother admitted to unit other than antepartum or mother-baby ¨ 2. Significant unintentional weight loss >=10 lb. in past 1 -2 months ¨ 3 Patient DESIRES EDUCATION on a therapeutic diet ¨ 4. Patient unable to take oral or other feedings >=5 days prior to admission ¨ 5. Patient on enteral or parenteral feedings ¨ 6. Geriatric patient (80 years plus) admitted for surgical procedure ¨ 7. Patient with skin breakdown (decubitus ulcer)
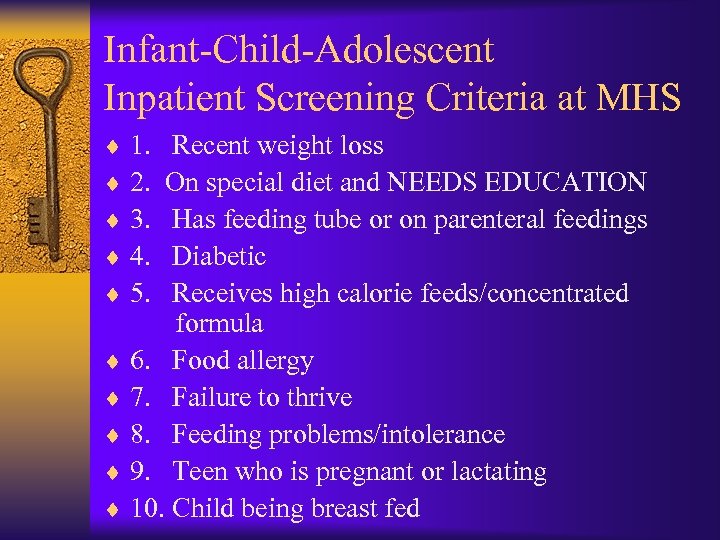 Infant-Child-Adolescent Inpatient Screening Criteria at MHS ¨ 1. Recent weight loss ¨ 2. On special diet and NEEDS EDUCATION ¨ 3. Has feeding tube or on parenteral feedings ¨ 4. Diabetic ¨ 5. Receives high calorie feeds/concentrated formula ¨ 6. Food allergy ¨ 7. Failure to thrive ¨ 8. Feeding problems/intolerance ¨ 9. Teen who is pregnant or lactating ¨ 10. Child being breast fed
Infant-Child-Adolescent Inpatient Screening Criteria at MHS ¨ 1. Recent weight loss ¨ 2. On special diet and NEEDS EDUCATION ¨ 3. Has feeding tube or on parenteral feedings ¨ 4. Diabetic ¨ 5. Receives high calorie feeds/concentrated formula ¨ 6. Food allergy ¨ 7. Failure to thrive ¨ 8. Feeding problems/intolerance ¨ 9. Teen who is pregnant or lactating ¨ 10. Child being breast fed
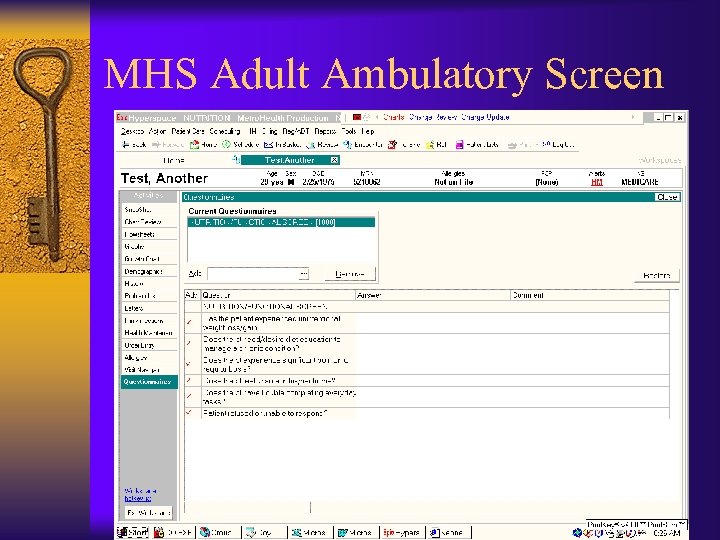 MHS Adult Ambulatory Screen
MHS Adult Ambulatory Screen
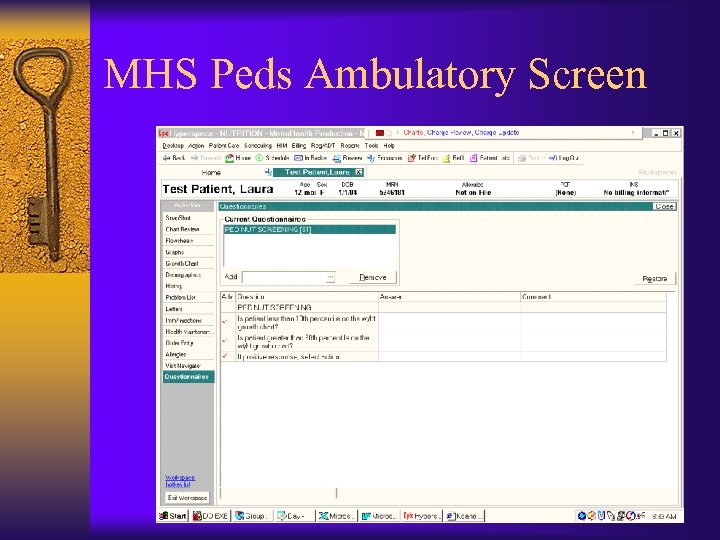 MHS Peds Ambulatory Screen
MHS Peds Ambulatory Screen
 Metro. Health Screening Prompt Criteria in Peds Ambulatory Clinics Children <2 Years ¨ <10 %ile weight/length ¨ >90 %ile weight/length Children 2 -18 Years ¨ < 10 %ile BMI/age ¨ >85 %ile BMI/age
Metro. Health Screening Prompt Criteria in Peds Ambulatory Clinics Children <2 Years ¨ <10 %ile weight/length ¨ >90 %ile weight/length Children 2 -18 Years ¨ < 10 %ile BMI/age ¨ >85 %ile BMI/age
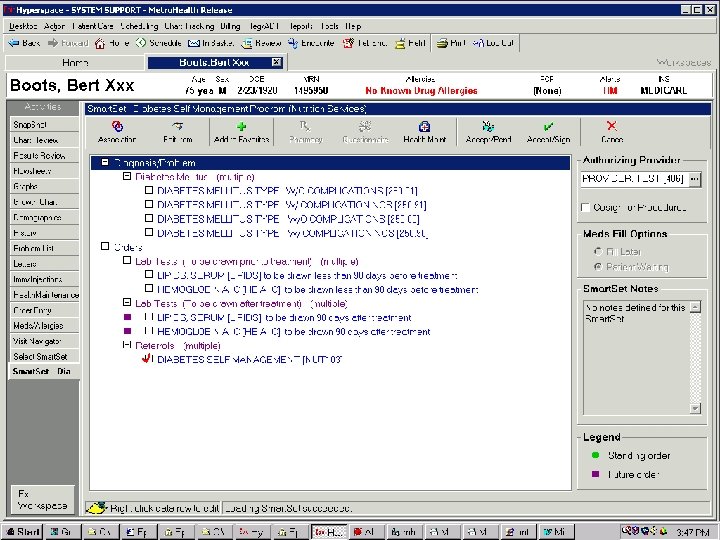
 Nursing Admission Screens: Most Common Criteria MHMC (Feb 17 -Mar 2, 2003)
Nursing Admission Screens: Most Common Criteria MHMC (Feb 17 -Mar 2, 2003)
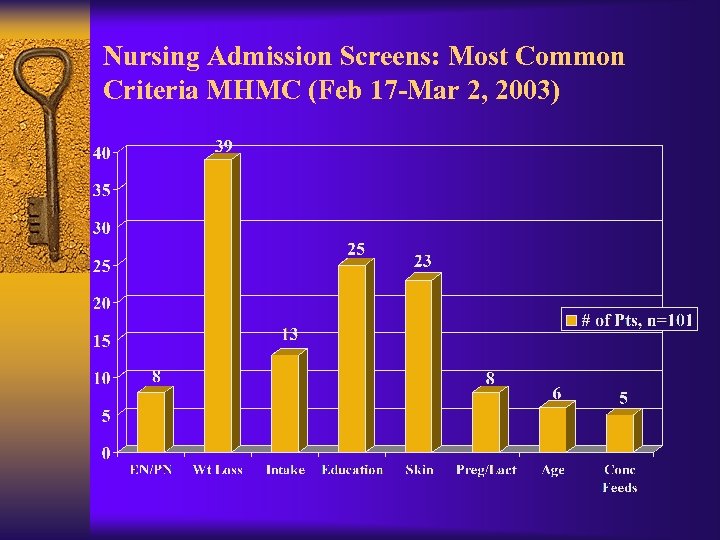
 % of Positive Nutrition Screens Classified as High Risk after Review (by Criterion)
% of Positive Nutrition Screens Classified as High Risk after Review (by Criterion)
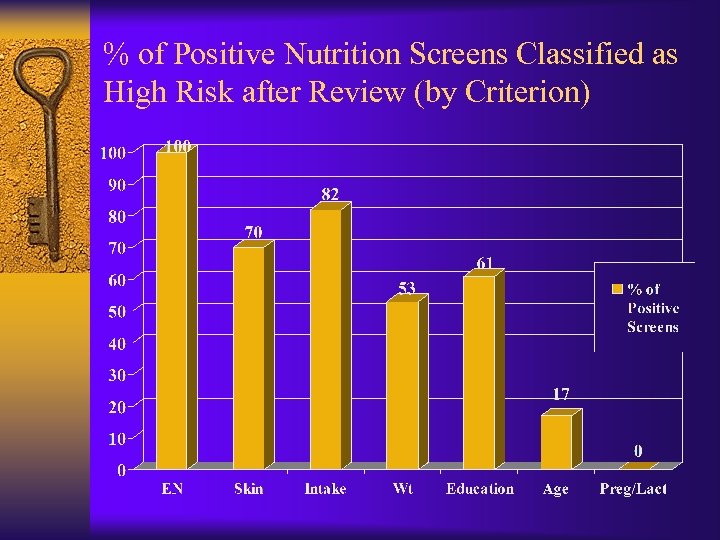
 Nutrition Screening at Metro. Health ¨ Consistent with national practice in terms of criteria, procedures, and time frames ¨ With the exception of TJC-mandated criteria, specificity ranges from 50 -100% ¨ TJC-mandated criteria are poor predictors of nutrition risk ¨ No data on sensitivity (e. g. what percentage of at risk pts are we discovering? )
Nutrition Screening at Metro. Health ¨ Consistent with national practice in terms of criteria, procedures, and time frames ¨ With the exception of TJC-mandated criteria, specificity ranges from 50 -100% ¨ TJC-mandated criteria are poor predictors of nutrition risk ¨ No data on sensitivity (e. g. what percentage of at risk pts are we discovering? )
 Issues in Nutrition Screening ¨ Most nutrition screening in acute and ambulatory settings is done by staff other than nutrition professionals ¨ Based on a national survey, identified at-risk patients are referred to nutrition professionals less than half the time
Issues in Nutrition Screening ¨ Most nutrition screening in acute and ambulatory settings is done by staff other than nutrition professionals ¨ Based on a national survey, identified at-risk patients are referred to nutrition professionals less than half the time
 Issues in Nutrition Screening ¨ Much of the research that exists validates more comprehensive nutrition screening tools, e. g. MNA in the elderly ¨ Little research has been done to validate or evaluate nutrition screening as it currently exists in most acute care institutions: a process using limited data obtained on admission by nursing staff. ¨ There is no “gold standard” of nutrition status that can be used as a benchmark
Issues in Nutrition Screening ¨ Much of the research that exists validates more comprehensive nutrition screening tools, e. g. MNA in the elderly ¨ Little research has been done to validate or evaluate nutrition screening as it currently exists in most acute care institutions: a process using limited data obtained on admission by nursing staff. ¨ There is no “gold standard” of nutrition status that can be used as a benchmark
 ADA Screening Evidence Analysis Work Group ¨ Convened fall, 2007 ¨ Will develop definitions and formulate questions for evidence analysis regarding nutrition screening
ADA Screening Evidence Analysis Work Group ¨ Convened fall, 2007 ¨ Will develop definitions and formulate questions for evidence analysis regarding nutrition screening
 Members of Screening EAL Work Group ¨ Chair: Pam Charney, Ph. D, RD, CNSD, consultant ¨ Vicki Castellanos, Ph. D, RD, Florida International University, educator ¨ Cinda Chima, MS, RD, University of Akron, educator ¨ Maree Ferguson, MBA, Ph. D, RD, Queensland, Australia, clinical manager ¨ Nancy Nevin-Folino, MEd, RD, CSP, LD, FADA, Children’s Hospital, Dayton, Oh, practitioner ¨ Judy Porcari, MBA, MS, RD, Clinical Manager ¨ Annalynn Skipper, Ph. D, RD, FADA, Consultant
Members of Screening EAL Work Group ¨ Chair: Pam Charney, Ph. D, RD, CNSD, consultant ¨ Vicki Castellanos, Ph. D, RD, Florida International University, educator ¨ Cinda Chima, MS, RD, University of Akron, educator ¨ Maree Ferguson, MBA, Ph. D, RD, Queensland, Australia, clinical manager ¨ Nancy Nevin-Folino, MEd, RD, CSP, LD, FADA, Children’s Hospital, Dayton, Oh, practitioner ¨ Judy Porcari, MBA, MS, RD, Clinical Manager ¨ Annalynn Skipper, Ph. D, RD, FADA, Consultant


