a06e6f4fb927ca5deffc094ff0e485b8.ppt
- Количество слайдов: 32
The Nutri Lao Study ¡¾ ¦ô¡¦¾²¾¸½ ² ½ ¾¡¾ ນ ຊ ນ ນ ¢º¤ì ¸¾ Vilabouly and Sepon Districts Savannakhet Province 2016 – 2019 Funded by the Australian National Health and Medical Research Council
Study Title Integrated solutions for healthy birth, growth, and development: A cluster-randomized controlled trial to evaluate the effectiveness of a mixed nutrition intervention package in reducing child undernutrition in Lao PDR ¡¾ Á¡ÉÄ¢®ñ ¹¾Á®®À¦ˆºມ¦¾ ¢º¤¡¾ນÀ¡ó©, ນ ນ ນ ¡¾ ¥½Àìó Àªó® ª, Áì½ ນ ນ ²ñ©ê½ ¾¡¾ນ ©É¸ ¡¾ນມ󲾸½ສ ນ ຍ ¢½²¾®ê†©ó: ¡¾ນ £í ນ £É¸¾êö©ìº¤£¸® ຄ ມ©É¸ຍ¡¾ນ ມກ ມ ສ ªö¸µÈ¾¤ À²ˆº¯½Àມóນ ¯½¦ò©êò ຜöນ ¢º¤ ©¡ò©¥½¡¿Áຊ¡ຄ ມ ຊ 꾤©É¾ ນ ² ½ນ ¾¡¾ Á®®¯½¦ö ຊ ນ ມ¯½¦¾ນ À²ˆºÍЩຜȺ ¡¾ ນ¢¾©¦¾ º¾¹¾ à ກ ມ ນ ນ ນ À©ñ¡µøÈà ¦¾ê¾ì½ ນ ນ½ìñ© ¯½ຊ¾êò¯½Äª ¯½ຊ¾ຊ ນ 쾸.

Research Partners Burnet Institute (Melbourne) Western Sydney University National Institute of Public Health (Vientiane) Deakin University (Melbourne) Monash University (Melbourne) Savannakhet Provincial Health Office Vilabouly & Sepon District Health Offices
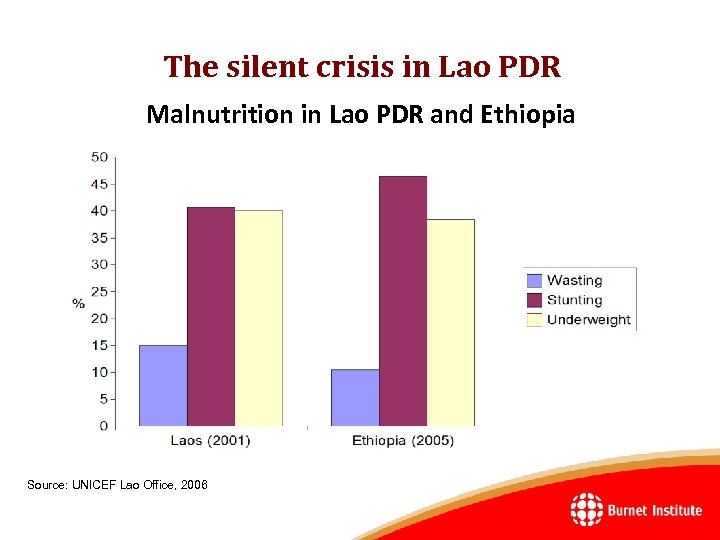
The silent crisis in Lao PDR Malnutrition in Lao PDR and Ethiopia Source: UNICEF Lao Office, 2006
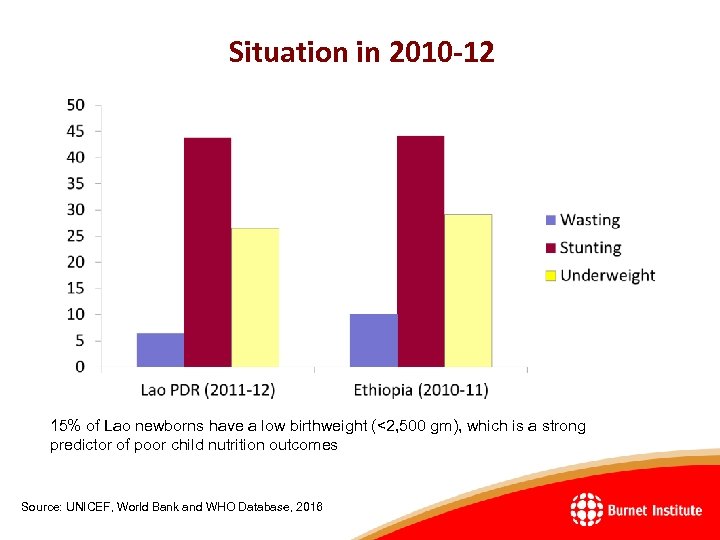
Situation in 2010 -12 15% of Lao newborns have a low birthweight (<2, 500 gm), which is a strong predictor of poor child nutrition outcomes Source: UNICEF, World Bank and WHO Database, 2016
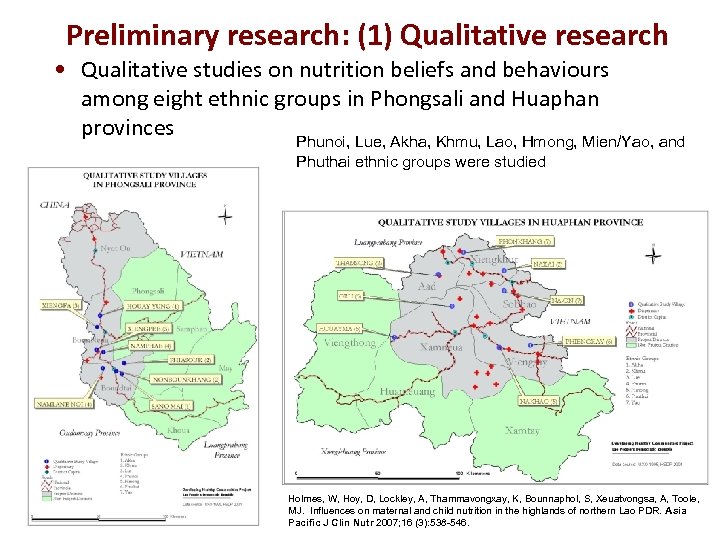
Preliminary research: (1) Qualitative research • Qualitative studies on nutrition beliefs and behaviours among eight ethnic groups in Phongsali and Huaphan provinces Phunoi, Lue, Akha, Khmu, Lao, Hmong, Mien/Yao, and Phuthai ethnic groups were studied Holmes, W, Hoy, D, Lockley, A, Thammavongxay, K, Bounnaphol, S, Xeuatvongsa, A, Toole, MJ. Influences on maternal and child nutrition in the highlands of northern Lao PDR. Asia Pacific J Clin Nutr 2007; 16 (3): 538 546.
Main findings • Most ethnic groups do not give colostrum to their babies. • Most women routinely breastfeed. However, exclusive breastfeeding until four or six months of age is rare. • Complementary foods are often given in the first few days of life, except among the Hmong and Akha. • Some mothers stop breastfeeding when they are ill, although most continue. • The duration of breast-feeding varies and is not associated with ethnicity. Most mothers feed their babies for one or more years; however, many mothers cease breast-feeding before one year.
Child nutrition (continued) • Malnutrition among children was reported by parents as being common, especially among the Akha. • There are numerous locally available foods rich in nutrients that are not commonly given to young children, including several varieties of yellow fruit, peanuts, sesame seeds, beans, peas, eggs, and pork fat • Food taboos are common in infancy although there is variation within each ethnic group: – Many ethnic groups, however, reported that they rarely give fruit to children – There also often food taboos for when a child is ill.
Women’s Nutrition • Food taboos among women are less common and less widely adhered to during pregnancy than food taboos after delivery. • The Akha appeared to be the group that most commonly had food taboos during pregnancy. • Food taboos after childbirth are common in all ethnic groups. • However, again, these are not always consistent between villages or even within villages of the same ethnic group. • There is an impression that many food taboos are not deeply rooted in ethnic cultures but are rather localised traditions, often confined to the family or clan. • Symptoms that indicate the possible presence of thiamine deficiency were also reported.
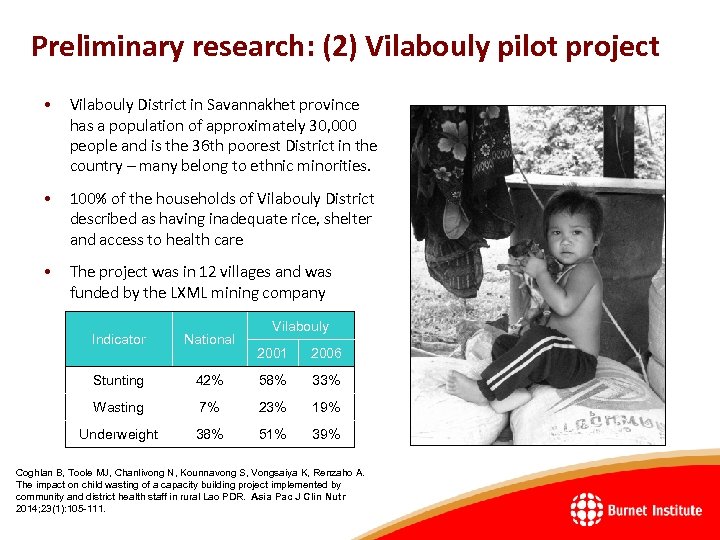
Preliminary research: (2) Vilabouly pilot project • Vilabouly District in Savannakhet province has a population of approximately 30, 000 people and is the 36 th poorest District in the country – many belong to ethnic minorities. • 100% of the households of Vilabouly District described as having inadequate rice, shelter and access to health care • The project was in 12 villages and was funded by the LXML mining company Indicator National Stunting Vilabouly 2001 2006 42% 58% 33% Wasting 7% 23% 19% Underweight 38% 51% 39% Coghlan B, Toole MJ, Chanlivong N, Kounnavong S, Vongsaiya K, Renzaho A. The impact on child wasting of a capacity building project implemented by community and district health staff in rural Lao PDR. Asia Pac J Clin Nutr 2014; 23(1): 105 111.
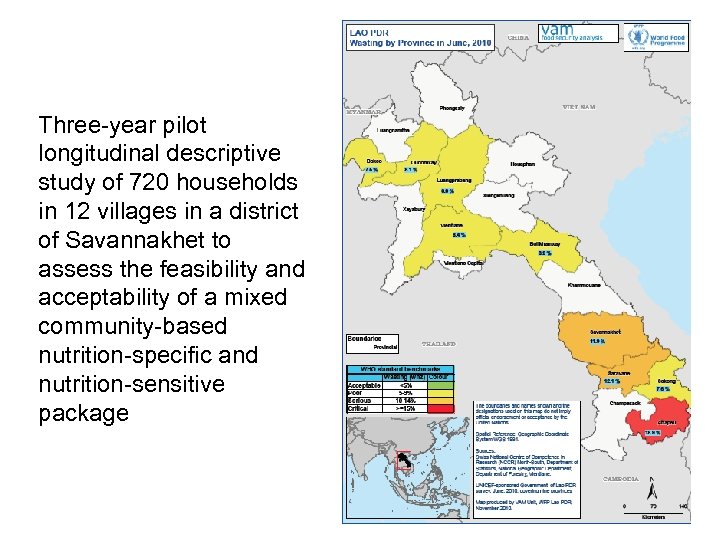
Three year pilot longitudinal descriptive study of 720 households in 12 villages in a district of Savannakhet to assess the feasibility and acceptability of a mixed community based nutrition specific and nutrition sensitive package
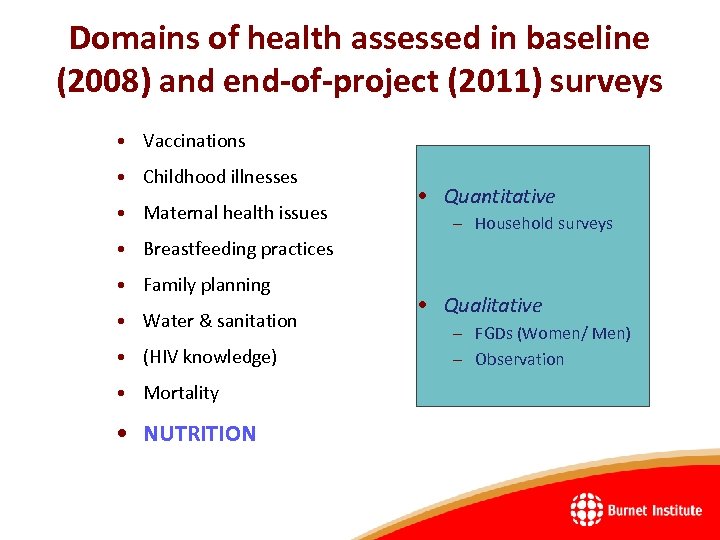
Domains of health assessed in baseline (2008) and end-of-project (2011) surveys • Vaccinations • Childhood illnesses • Maternal health issues • Quantitative – Household surveys • Breastfeeding practices • Family planning • Water & sanitation • (HIV knowledge) • Mortality • NUTRITION • Qualitative – FGDs (Women/ Men) – Observation


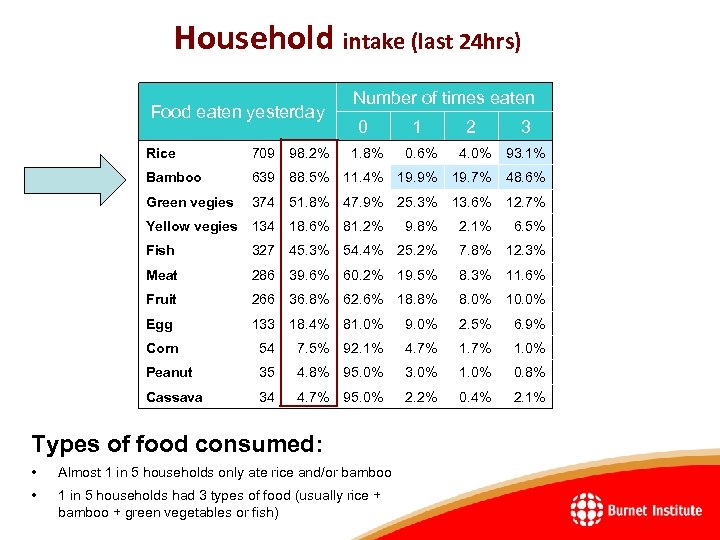
Household intake (last 24 hrs) Food eaten yesterday Number of times eaten 0 1 2 3 Rice 709 98. 2% 1. 8% 0. 6% 4. 0% 93. 1% Bamboo 639 88. 5% 11. 4% 19. 9% 19. 7% 48. 6% Green vegies 374 51. 8% 47. 9% 25. 3% 13. 6% 12. 7% Yellow vegies 134 18. 6% 81. 2% 9. 8% 2. 1% 6. 5% Fish 327 45. 3% 54. 4% 25. 2% 7. 8% 12. 3% Meat 286 39. 6% 60. 2% 19. 5% 8. 3% 11. 6% Fruit 266 36. 8% 62. 6% 18. 8% 8. 0% 10. 0% Egg 133 18. 4% 81. 0% 9. 0% 2. 5% 6. 9% Corn 54 7. 5% 92. 1% 4. 7% 1. 0% Peanut 35 4. 8% 95. 0% 3. 0% 1. 0% 0. 8% Cassava 34 4. 7% 95. 0% 2. 2% 0. 4% 2. 1% Types of food consumed: • Almost 1 in 5 households only ate rice and/or bamboo • 1 in 5 households had 3 types of food (usually rice + bamboo + green vegetables or fish)
Project inputs • Nutrition-specific: The project aimed to reduce acute malnutrition in children through the establishment of volunteer community nutrition teams in each village to monitor child growth and promote exclusive breast-feeding, healthy infant feeding practices and child diets. – This project took place before the introduction of multiple micronutrient supplements for children were introduced into Savannakhet province. • District health staff were trained to support these teams with monthly outreach to formally assess child growth and to manage severe acute malnutrition in children. • Nutrition-sensitive: Outreach activities also aimed to increase immunization coverage, teach mothers how to manage children with diarrhoea, improve access to antenatal and postnatal care, and promote family planning.
Project outcomes (2011) • • Feeding behaviours and child nutrition More new mothers fed their child soon after birth: 72% breastfed within 2 hrs of delivery compared with 40% in 2008. Fewer women discarded the colostrum: 92% fed their baby colostrum, up from 69%. Fewer women fed their baby solids before 6 months: 41% down from 87% in 2008. Far fewer children suffered from wasting: 12. 4% of children were acutely malnourished in 2008 compared with just 5. 3% in 2011
Other project outcomes Antenatal care • More pregnant women could access antenatal care: 88% had at least 1 visit by a skilled health professional up from 69%, while 53% had 4 or more visits up from 32%. • More pregnant women received supplements: 86% received iron tablets compared with 55% in 2008, and 79% received Vitamin B 1 compared with 0%. Family planning • A little over half of all women aged 15 -45 years had received family planning advice in August 2008. This had increased to 69% during the evaluation in December 2011.
Care during childbirth • More women delivered at the district hospital: 52% had a baby at the hospital increased from 38%. Fewer women gave birth at home: 39% compare with 53%. • More deliveries were attended by a trained health professional: 62% compared with 52% in 2008 Child immunizations • More children have an immunization care: improving from 30% to 51%. • More children received birth doses of BCG and hepatitis B: coverage of BCG vaccine went from 62% to 83%, and hepatitis B from 24% to 64%. • More children are protected against measles: from 31% in 2008 to 87% in 2011.
The pilot demonstrated the readiness of local authorities and communities to implement the interventions; showed that health services can be improved and that unsafe feeding practices can be changed; and suggested that the combination of interventions can improve the nutritional status of children.
Nutri-Lao Study • Primary Hypothesis: Compared with those in the control group (who will receive a standard primary health care package), the intervention package delivered to pregnant women from 6 months gestation and their infants until 18 months of age will reduce the prevalence of stunting (height-for-age <-2 Z score) by 10% (44% control vs. 34% intervention) in children at 18 months of age. • Secondary Hypotheses: The intervention package will reduce (i) the prevalence of LBW by 5% (control 11% vs intervention 6%) and (ii) the prevalence of wasting (weight-for-height <-2 Z score) by 6% (12% control vs. 6% intervention) in children at 18 months of age. • Tertiary hypothesis: The mixed CBNP will be cost-effective compared to the standard PHC package currently implemented by the Lao Ministry of Health (MOH).

Cluster randomised controlled trial • A total of 22 health centres serving 204 villages (150 in Sepon and 54 in Vilabouly) with a total population of 77, 027 residents will be included in the trial. Each HC catchment area will be considered a separate cluster for practical reasons. • Each arm will include 102 villages. Based on Go. L projections of the district population and district crude birth rate from 2005 -2013 data, we anticipate that about 3, 302 children will be born during the 12 month enrolment phase across all 204 villages in 2016. • We will enrol: (1) all pregnant women in the third trimester who plan to stay in the village for the next 21 months, this enrolment period will last 12 months; and (2) their infants born during this 12 month period and within approximately 3 months after the end of the enrolment period.
Data collection • Senior research manager and four field coordinators based in Vilabouly • We will measure primary and secondary outcomes at birth (birthweight only), 6, 12, and 18 months of age. • Blood spots will be taken from pregnant women upon recruitment by HC staff for haemoglobin and malaria. • The primary and secondary outcomes are expected to be mediated through a number of improvements in nutritional behaviours and health service coverage indicators. • These variables will be measured (at the individual level and reported for clusters) using questionnaires based on the Lao Social Indicator Survey (2011 -12). • Casual data collectors will be recruited (for example, teachers and students) – 22 (one per HC catchment area).
• The intervention will be delivered by staff from each intervention arm HC and the community nutrition team (CNT) in each village with oversight by multisectoral district project implementation teams (Health, Education, Agriculture, and Communications Departments, the District Governor’s Office, and the Lao Women’s and Youth Unions). • The CNTs will be developed and trained by the project and will include four members – the village head or elder, village health volunteer (VHV), traditional birth attendant (TBA), and one HC staff. • Both intervention and control villages will receive all seven standard PHC components either at the HC or during routine 4 -monthly outreach. • The intervention group will receive an additional six nutrition-specific components either from the CNT in the village or at 4 -monthly visits by HC staff.
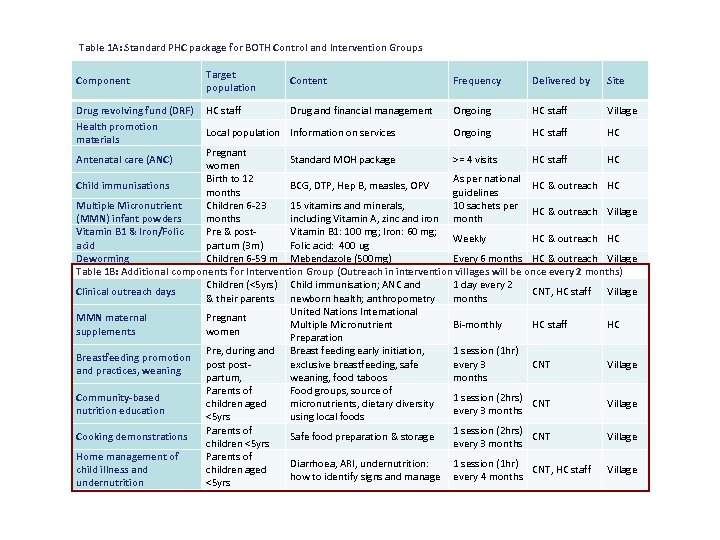
Table 1 A: Standard PHC package for BOTH Control and Intervention Groups Component Drug revolving fund (DRF) Health promotion materials Target population Content Frequency Delivered by Site HC staff Drug and financial management Ongoing HC staff Village Ongoing HC staff HC Local population Information on services Pregnant Standard MOH package >= 4 visits HC staff HC women Birth to 12 As per national Child immunisations BCG, DTP, Hep B, measles, OPV HC & outreach HC months guidelines Multiple Micronutrient Children 6 -23 15 vitamins and minerals, 10 sachets per HC & outreach Village (MMN) infant powders months including Vitamin A, zinc and iron month Vitamin B 1 & Iron/Folic Pre & post. Vitamin B 1: 100 mg; Iron: 60 mg; Weekly HC & outreach HC acid partum (3 m) Folic acid: 400 ug Deworming Children 6 -59 m Mebendazole (500 mg) Every 6 months HC & outreach Village Table 1 B: Additional components for Intervention Group (Outreach in intervention villages will be once every 2 months) Children (<5 yrs) Child immunisation; ANC and 1 day every 2 Clinical outreach days CNT, HC staff Village & their parents newborn health; anthropometry months United Nations International MMN maternal Pregnant Multiple Micronutrient Bi-monthly HC staff HC supplements women Preparation Pre, during and Breast feeding early initiation, 1 session (1 hr) Breastfeeding promotion postexclusive breastfeeding, safe every 3 CNT Village and practices, weaning partum, weaning, food taboos months Parents of Food groups, source of Community-based 1 session (2 hrs) children aged micronutrients, dietary diversity CNT Village nutrition education every 3 months <5 yrs using local foods Parents of 1 session (2 hrs) Cooking demonstrations Safe food preparation & storage CNT Village children <5 yrs every 3 months Home management of Parents of Diarrhoea, ARI, undernutrition: 1 session (1 hr) child illness and children aged CNT, HC staff Village how to identify signs and manage every 4 months undernutrition <5 yrs Antenatal care (ANC)
Cascade-style “train the trainer” model • At the district level, the project implementation teams (PIT) members will be trained by research staff in project management, supervision, data collection, financial management, communication, and reporting, as well as an overview of the intervention components. • At the community level, the four participants (CNT) in each intervention village will undertake a series of modules in the form of one-day participatory workshops. • Modules will cover nutrition education, cooking demonstrations, home fortified food supplementation with multiple micronutrients, home management of child illness and undernutrition, antenatal and postnatal care, and bimonthly growth monitoring. • Upon graduation, trained participants will implement the intervention using individual and group behaviour change communication techniques and outreach by HC staff
Tertiary outcome – cost-effectiveness analysis • An economic evaluation will be conducted from the perspective of the Lao MOH. • Outcome and resource/cost data will be prospectively collected at the HC and individual levels. • The results will be based on the primary outcome measure and expressed as “cost or saving per 5 percent change in the incidence of acute undernutrition in infants aged 18 months” calculated from the differences in mean costs and outcomes between the intervention and control groups, to generate an incremental cost-effectiveness ratio (ICER). • The outcome measures for the ICERs will be expressed as cost per 6% reduction in wasting and 10% reduction in stunting at 18 months.
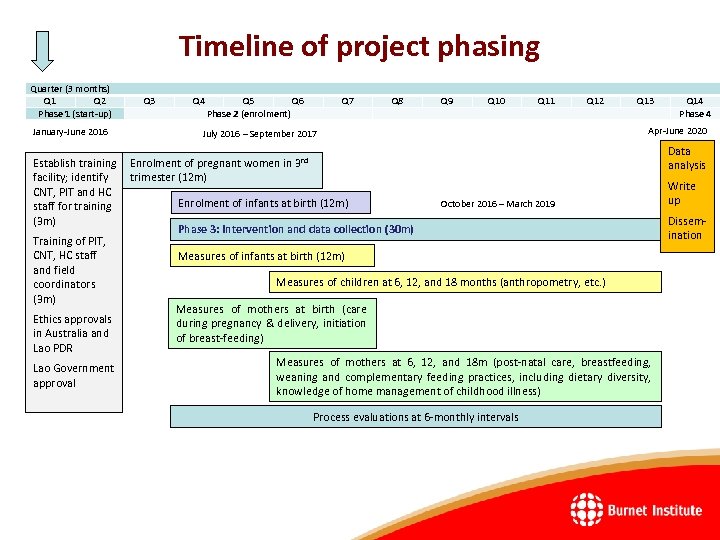
Timeline of project phasing Quarter (3 months) Q 1 Q 2 Phase 1 (start-up) January-June 2016 Q 3 Q 4 Q 5 Q 6 Phase 2 (enrolment) Q 7 Q 8 Q 9 Q 10 Q 11 Q 12 Q 13 July 2016 – September 2017 Apr-June 2020 Establish training Enrolment of pregnant women in 3 rd trimester (12 m) facility; identify CNT, PIT and HC Enrolment of infants at birth (12 m) October 2016 – March 2019 staff for training (3 m) Phase 3: Intervention and data collection (30 m) Training of PIT, CNT, HC staff Measures of infants at birth (12 m) and field Measures of children at 6, 12, and 18 months (anthropometry, etc. ) coordinators (3 m) Measures of mothers at birth (care Ethics approvals during pregnancy & delivery, initiation in Australia and of breast-feeding) Lao PDR Measures of mothers at 6, 12, and 18 m (post-natal care, breastfeeding, Lao Government weaning and complementary feeding practices, including dietary diversity, approval knowledge of home management of childhood illness) Process evaluations at 6 -monthly intervals Q 14 Phase 4 Data analysis Write up Dissemination
Dissemination of findings • Dr Sengchanh (National Institute of Public Health) and Dr Panom Phongmany, the provincial health director of Savannakhet province, will lead Go. L efforts to disseminate, adapt and scale up the findings of the proposed study if they demonstrate the cost-effectiveness of the community-based nutrition package. • The National Nutrition Centre (MOPH) will be a key stakeholder. • Publication of the findings in peer-reviewed journals and dissemination through academic and development forums will ensure findings are disseminated beyond Lao PDR. • A policy brief will be prepared for the Australian aid program which has established a multi-sectoral Nutrition Working Group and is currently in the process of developing a strategy to effectively address maternal and child undernutrition.
Good reference Victora, Cesar G et al. “Maternal and Child Undernutrition: Consequences for Adult Health and Human Capital. ” Lancet 371. 9609 (2008): 340– 357. PMC. Web. 16 Mar. 2016. Based on data from cohorts followed up from birth into late adolescence or adult age in Brazil, Guatemala, India, the Philippines, and South Africa Height-for-age at 2 years of age the best predictor of human capital, defined as: • Adult height • Educational achievements • Adult income • For females: birthweight of offspring Poor foetal growth or stunting in the first 2 years of life leads to irreversible damage, including shorter adult height, lower attained schooling, reduced adult income, and decreased offspring birthweight

Thank you ຂອບໃຈ
a06e6f4fb927ca5deffc094ff0e485b8.ppt