723b1fa98dbb7cd7e253c36114148041.ppt
- Количество слайдов: 63
 The Nursing Challenges of Caring for Patients with NORSE Syndrome Melissa V Moreda RN BSN CNRN
The Nursing Challenges of Caring for Patients with NORSE Syndrome Melissa V Moreda RN BSN CNRN
 disclosures • Merz
disclosures • Merz
 Case #1 K. S. • KS is a 28 yo Korean American female • Admitted to OSH – flu-like symptoms for 4 -5 days. – nausea/vomiting and 105. 0 Fever. • She became disoriented and confused & had a witnessed tonic clonic seizure. • Recurrent seizures continued.
Case #1 K. S. • KS is a 28 yo Korean American female • Admitted to OSH – flu-like symptoms for 4 -5 days. – nausea/vomiting and 105. 0 Fever. • She became disoriented and confused & had a witnessed tonic clonic seizure. • Recurrent seizures continued.
 Case #1 K. S. • Transferred to Duke in Status Epilepticus • Workup unremarkable • NO past hx of childhood epilepsy, febrile seizure, no head trauma, no meningitis • NO family hx of sz, no predisposing evidence
Case #1 K. S. • Transferred to Duke in Status Epilepticus • Workup unremarkable • NO past hx of childhood epilepsy, febrile seizure, no head trauma, no meningitis • NO family hx of sz, no predisposing evidence
 Case #1 K. S. • Social hx: ANY exposure--- what do they work with? any unusual circumstances or any family/friends with recent sickness? • Habits: drinking/drugs/etc • Allergies: none • Medications (any herbals/supplements) • Extensive negative workup
Case #1 K. S. • Social hx: ANY exposure--- what do they work with? any unusual circumstances or any family/friends with recent sickness? • Habits: drinking/drugs/etc • Allergies: none • Medications (any herbals/supplements) • Extensive negative workup
 Case #1 K. S. Initial lines of anticonvulsants started. Quick escalation of medication dosages and additional anticonvulsants added. Seizures continued. Paralytics added, max therapies reached.
Case #1 K. S. Initial lines of anticonvulsants started. Quick escalation of medication dosages and additional anticonvulsants added. Seizures continued. Paralytics added, max therapies reached.
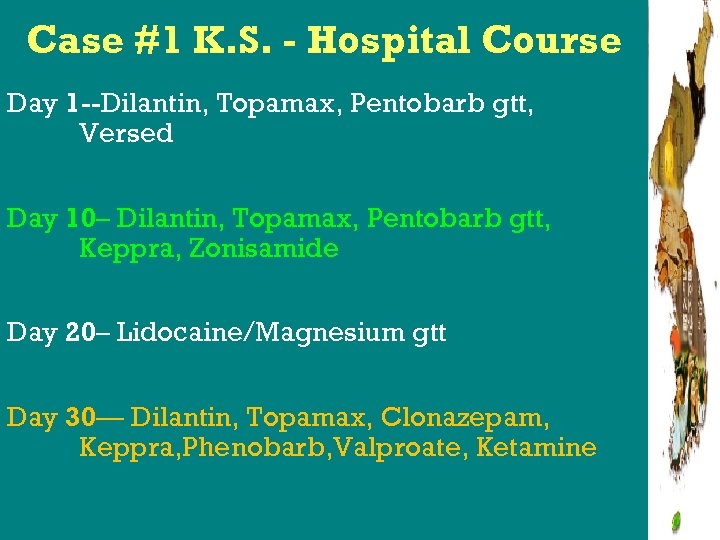 Case #1 K. S. - Hospital Course Day 1 --Dilantin, Topamax, Pentobarb gtt, Versed Day 10– Dilantin, Topamax, Pentobarb gtt, Keppra, Zonisamide Day 20– Lidocaine/Magnesium gtt Day 30— Dilantin, Topamax, Clonazepam, Keppra, Phenobarb, Valproate, Ketamine
Case #1 K. S. - Hospital Course Day 1 --Dilantin, Topamax, Pentobarb gtt, Versed Day 10– Dilantin, Topamax, Pentobarb gtt, Keppra, Zonisamide Day 20– Lidocaine/Magnesium gtt Day 30— Dilantin, Topamax, Clonazepam, Keppra, Phenobarb, Valproate, Ketamine
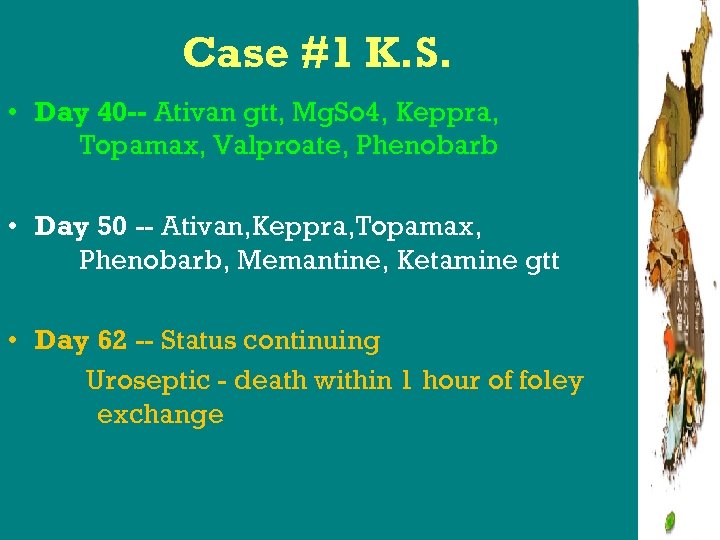 Case #1 K. S. • Day 40 -- Ativan gtt, Mg. So 4, Keppra, Topamax, Valproate, Phenobarb • Day 50 -- Ativan, Keppra, Topamax, Phenobarb, Memantine, Ketamine gtt • Day 62 -- Status continuing Uroseptic - death within 1 hour of foley exchange
Case #1 K. S. • Day 40 -- Ativan gtt, Mg. So 4, Keppra, Topamax, Valproate, Phenobarb • Day 50 -- Ativan, Keppra, Topamax, Phenobarb, Memantine, Ketamine gtt • Day 62 -- Status continuing Uroseptic - death within 1 hour of foley exchange
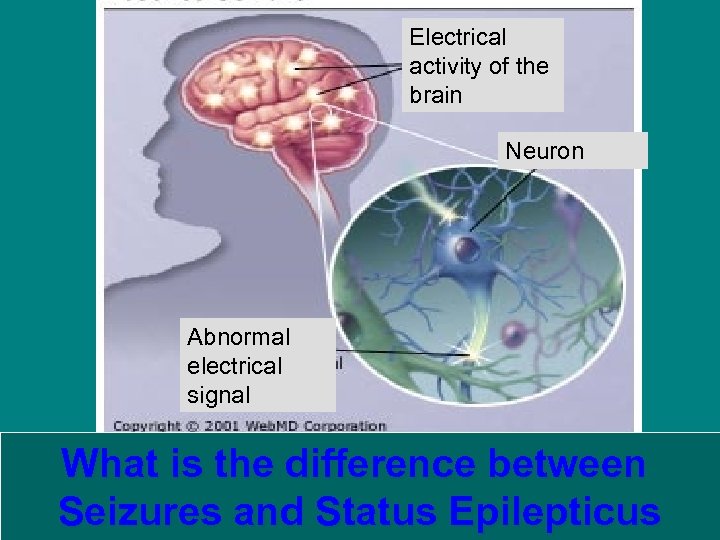 Electrical activity of the brain Neuron Abnormal electrical signal What is the difference between Seizures and Status Epilepticus
Electrical activity of the brain Neuron Abnormal electrical signal What is the difference between Seizures and Status Epilepticus
 What is seizure? • A single (finite) event of abnormal discharge in the brain that results in an abrupt and temporary altered state of cerebral function.
What is seizure? • A single (finite) event of abnormal discharge in the brain that results in an abrupt and temporary altered state of cerebral function.
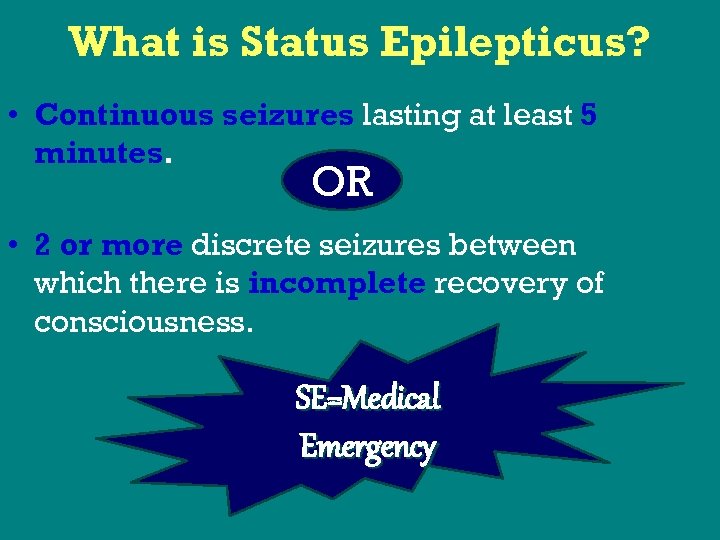 What is Status Epilepticus? • Continuous seizures lasting at least 5 minutes. OR • 2 or more discrete seizures between which there is incomplete recovery of consciousness. SE=Medical Emergency
What is Status Epilepticus? • Continuous seizures lasting at least 5 minutes. OR • 2 or more discrete seizures between which there is incomplete recovery of consciousness. SE=Medical Emergency
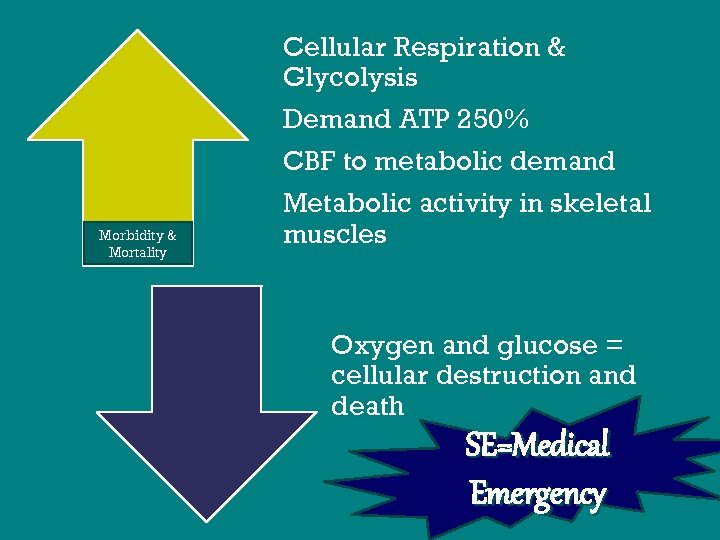 Morbidity & Mortality Cellular Respiration & Glycolysis Demand ATP 250% CBF to metabolic demand Metabolic activity in skeletal muscles Oxygen and glucose = cellular destruction and death SE=Medical Emergency
Morbidity & Mortality Cellular Respiration & Glycolysis Demand ATP 250% CBF to metabolic demand Metabolic activity in skeletal muscles Oxygen and glucose = cellular destruction and death SE=Medical Emergency
 Status Epilepticus • Repeated partial seizures manifesting as focal motor convulsions, focal sensory symptoms, or focal impairment of function (ie: aphasia not associated with LOC) • Tonic-clonic most common type. • Convulsive more easily seen clinically. Partial less obvious and more difficult to identify. Subclinical only identifiable on c. EEG. • Wittman & Hirsch--Neurocritical Care 2005: increasing awareness of nonconvulsive seizures in critically ill
Status Epilepticus • Repeated partial seizures manifesting as focal motor convulsions, focal sensory symptoms, or focal impairment of function (ie: aphasia not associated with LOC) • Tonic-clonic most common type. • Convulsive more easily seen clinically. Partial less obvious and more difficult to identify. Subclinical only identifiable on c. EEG. • Wittman & Hirsch--Neurocritical Care 2005: increasing awareness of nonconvulsive seizures in critically ill
 What is refractory SE? Failure of max doses of dilantin Benzos not stopping the seizures
What is refractory SE? Failure of max doses of dilantin Benzos not stopping the seizures
 Safety & Nursing Care: Convulsive vs Anticonvulsive External Safety: padded rails suction present bed in low position pulse ox/ vitals staying with the patient obtaining benzos & AEDS Family needs education and reassurance
Safety & Nursing Care: Convulsive vs Anticonvulsive External Safety: padded rails suction present bed in low position pulse ox/ vitals staying with the patient obtaining benzos & AEDS Family needs education and reassurance
 Safety & Nursing Care: Convulsive vs Anticonvulsive Internal Safety: A seizure represents actual danger to brain tissue Time is BRAIN
Safety & Nursing Care: Convulsive vs Anticonvulsive Internal Safety: A seizure represents actual danger to brain tissue Time is BRAIN
 Returning to Case Study #1 K. S. • KS has the flu, spikes a fever, starts seizing and doesn’t stop despite multiple line anticonvulsants. Full life support. • Completely negative workup. • Family, Nurses, MD’s, PRM’s, want to know…. What’s going on here? ? ?
Returning to Case Study #1 K. S. • KS has the flu, spikes a fever, starts seizing and doesn’t stop despite multiple line anticonvulsants. Full life support. • Completely negative workup. • Family, Nurses, MD’s, PRM’s, want to know…. What’s going on here? ? ?

 NORSE New Onset Status Refractory Epilepticus
NORSE New Onset Status Refractory Epilepticus
 What is it? ? ? • *2005 Wilder-Smith , Lim, Teoh, Sharma, Tan, Chen, et al documented and claimed this phenomenon in Singapore.
What is it? ? ? • *2005 Wilder-Smith , Lim, Teoh, Sharma, Tan, Chen, et al documented and claimed this phenomenon in Singapore.
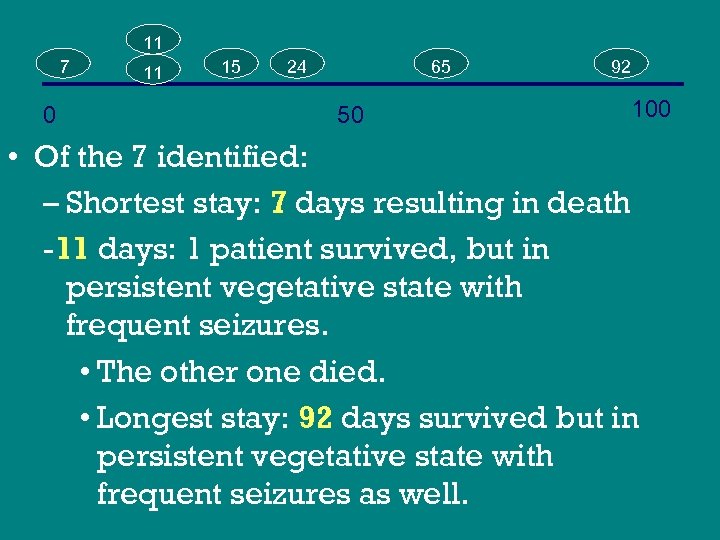 11 7 0 11 15 24 65 50 92 100 • Of the 7 identified: – Shortest stay: 7 days resulting in death -11 days: 1 patient survived, but in persistent vegetative state with frequent seizures. • The other one died. • Longest stay: 92 days survived but in persistent vegetative state with frequent seizures as well.
11 7 0 11 15 24 65 50 92 100 • Of the 7 identified: – Shortest stay: 7 days resulting in death -11 days: 1 patient survived, but in persistent vegetative state with frequent seizures. • The other one died. • Longest stay: 92 days survived but in persistent vegetative state with frequent seizures as well.
 NORSE-EEG Relationships • Initial eeg captured ictal discharges in all. • In 3, eeg showed ictal discharges from bilateral fronto-temporal regions with no side preference. • In 1, continuous parasagital ictal discharge. • In 3, fronto-temporal discharges originating from the right on 2 occasions and once on the left
NORSE-EEG Relationships • Initial eeg captured ictal discharges in all. • In 3, eeg showed ictal discharges from bilateral fronto-temporal regions with no side preference. • In 1, continuous parasagital ictal discharge. • In 3, fronto-temporal discharges originating from the right on 2 occasions and once on the left
 • Status Epilepticus Clinical Guidelines 2003 – Benzodiazepines – Phenytoin loads + maintenance doses – Barbiturates Why use these meds? ? ?
• Status Epilepticus Clinical Guidelines 2003 – Benzodiazepines – Phenytoin loads + maintenance doses – Barbiturates Why use these meds? ? ?
 Wilder-Smith et al • Treatments included: – Benzodiazepines Levetiracetam – Phenytoin IVIG – Valproate – Propofol – Thiopental – Topiramate
Wilder-Smith et al • Treatments included: – Benzodiazepines Levetiracetam – Phenytoin IVIG – Valproate – Propofol – Thiopental – Topiramate
 Benzos • Lorazepam (Ativan ): – increases action of GABA which inhibits neurotransmission, depressing all levels of CNS Problem: hypotension, caution in renal or hepatic impairment, MG ICUadmit*ICUadmit*ICUadmit BP BP BP
Benzos • Lorazepam (Ativan ): – increases action of GABA which inhibits neurotransmission, depressing all levels of CNS Problem: hypotension, caution in renal or hepatic impairment, MG ICUadmit*ICUadmit*ICUadmit BP BP BP
 Benzos • Diazepam (Valium): • Short acting , ½ life 16 -90 minutes, the later ½ eliminated slower. • High does and accumulation of active diazepam metabolites = respiratory depression and hypotension • 5 -20 mg IV slowly at 1 -2 mg/min Repeat 5 -10 mg every 5 -10 minutes to a maximum of 100 mg/24 hours
Benzos • Diazepam (Valium): • Short acting , ½ life 16 -90 minutes, the later ½ eliminated slower. • High does and accumulation of active diazepam metabolites = respiratory depression and hypotension • 5 -20 mg IV slowly at 1 -2 mg/min Repeat 5 -10 mg every 5 -10 minutes to a maximum of 100 mg/24 hours
 Benzos • Midazolam(Versed): – Large number of trials reflecting that this medication works – Rapid absorption into brain – Benign from a hemodynamic standpoint – Peds: success of breaking seizures without intubation – Load: 0. 2 mg/kg, maintenance: up to 2 mcg/kg/min, most effective as a gtt – Problem: tachyphylaxis (wears off), accumulates in critically ill.
Benzos • Midazolam(Versed): – Large number of trials reflecting that this medication works – Rapid absorption into brain – Benign from a hemodynamic standpoint – Peds: success of breaking seizures without intubation – Load: 0. 2 mg/kg, maintenance: up to 2 mcg/kg/min, most effective as a gtt – Problem: tachyphylaxis (wears off), accumulates in critically ill.
 Phenytoin / Fosphenytoin – may work in motor cortex, may stop spread of activity – Brain stem centers stop tonic phase of grand mal sz – 18 -20 mg/kg, if refractory – may use 30 mg/kg – Problem: hypotension, purple glove syndrome, fever, cardiac death from widened QRS
Phenytoin / Fosphenytoin – may work in motor cortex, may stop spread of activity – Brain stem centers stop tonic phase of grand mal sz – 18 -20 mg/kg, if refractory – may use 30 mg/kg – Problem: hypotension, purple glove syndrome, fever, cardiac death from widened QRS
 Refractory Status Epilepticus • 30 minutes to 1 hour of seizure activity not broken • No interval of time between failed treatment and next therapy • Start infusions of Benzodiazepines, Propofol, Barbitruates • Keep giving bolus doses
Refractory Status Epilepticus • 30 minutes to 1 hour of seizure activity not broken • No interval of time between failed treatment and next therapy • Start infusions of Benzodiazepines, Propofol, Barbitruates • Keep giving bolus doses
 Barbiturates • Pentobarbital: – Extremely effective halting seizures on eeg by inducing coma – Load: 5 -12 mg/kg, maintenance: 1 -10 mg/kg Problem: high doses suppress cardiac function, difficult to monitor levels, poor chemotaxis of wbc, paralysis of resp cilia, poikilothermia Dr. Borel
Barbiturates • Pentobarbital: – Extremely effective halting seizures on eeg by inducing coma – Load: 5 -12 mg/kg, maintenance: 1 -10 mg/kg Problem: high doses suppress cardiac function, difficult to monitor levels, poor chemotaxis of wbc, paralysis of resp cilia, poikilothermia Dr. Borel
 Barbiturates • Phenobarbital: – Introduced 1912 – CNS depressant – elevates seizure threshold by decreasing postsynaptic excitation, possibly excitation stimulating postsynaptic GABA inhibitor responses. – Sometimes given in combo with dilantin – Rapidly absorbed by all routes, 3 -4 weeks to reach steady state
Barbiturates • Phenobarbital: – Introduced 1912 – CNS depressant – elevates seizure threshold by decreasing postsynaptic excitation, possibly excitation stimulating postsynaptic GABA inhibitor responses. – Sometimes given in combo with dilantin – Rapidly absorbed by all routes, 3 -4 weeks to reach steady state
 Medicinal Management • Traditional goal of therapy: achieve burst suppression on EEG 12 -24 hours to control or prevent recurrent seizures. • Termination of the seizures should occur rapidly to minimize neural damage, correction of metabolic defects, and resuscitation SE=Medical Emergency
Medicinal Management • Traditional goal of therapy: achieve burst suppression on EEG 12 -24 hours to control or prevent recurrent seizures. • Termination of the seizures should occur rapidly to minimize neural damage, correction of metabolic defects, and resuscitation SE=Medical Emergency
 When your clinical guidelines fail in stopping seizures… What do you do? ? ?
When your clinical guidelines fail in stopping seizures… What do you do? ? ?
 Medicinal Management of Refractory Status Epilepticus 1 st Maximize Phenytoin & Benzodiazepine loads. This usually controls 70% of patients. 2 nd Midazolam boluses infusion, Propofol, Barbiturates 3 rd. Topiramate, phenobarbital, midazolam, pentobarbital, valproate, levetiracetam, lidocaine, ketamine, thiopental, or isoflurane
Medicinal Management of Refractory Status Epilepticus 1 st Maximize Phenytoin & Benzodiazepine loads. This usually controls 70% of patients. 2 nd Midazolam boluses infusion, Propofol, Barbiturates 3 rd. Topiramate, phenobarbital, midazolam, pentobarbital, valproate, levetiracetam, lidocaine, ketamine, thiopental, or isoflurane
 Medicinal Management • Other treatments we have tried – Antivirals upon arrival – Magnesium drips – Memantine – Ketamine drips – Prn ativan, phenobarb, pentobarb, versed – Giving “holidays” to reintroduce the medications, hopefully to “break through” the seizures.
Medicinal Management • Other treatments we have tried – Antivirals upon arrival – Magnesium drips – Memantine – Ketamine drips – Prn ativan, phenobarb, pentobarb, versed – Giving “holidays” to reintroduce the medications, hopefully to “break through” the seizures.
 Wilder-Smith et al Thiopental: anesthetic that is barbiturate based. IVIG: ? autoimmune, does not cross the BBB Propofol: difficult to suppress sz while titrating/ balancing hemodynamics – Rosetti et al 2004 burst suppression 31 patients/ 21 successfully suppressed – 1 interesting side effect: EPILEPTIFORM ACTIVITY!!!!
Wilder-Smith et al Thiopental: anesthetic that is barbiturate based. IVIG: ? autoimmune, does not cross the BBB Propofol: difficult to suppress sz while titrating/ balancing hemodynamics – Rosetti et al 2004 burst suppression 31 patients/ 21 successfully suppressed – 1 interesting side effect: EPILEPTIFORM ACTIVITY!!!!
 Alternative Therapies • Robakis, Hirch 2006 lit review + expert neurointensivists/ epileptologists • Tx included: ketamine, gammaglobulin, plasmapheresis, steroids, adrenocorticotropic hormone, high dose phenobarb, isoflurane, lidocaine, ect, ketogenic diet, hypothermia, mag
Alternative Therapies • Robakis, Hirch 2006 lit review + expert neurointensivists/ epileptologists • Tx included: ketamine, gammaglobulin, plasmapheresis, steroids, adrenocorticotropic hormone, high dose phenobarb, isoflurane, lidocaine, ect, ketogenic diet, hypothermia, mag
 Lidocaine • CNS depression with cessation of convulsions • Biphasic: – Blocks inhibitory CNS pathways resulting in stimulation – Blocks inhibitory/excitatory impulses resulting in CNS inhibition (Peralta 2007) • Walker, Slovis 1997 effective in peds not responding to barbs • Bolus + maintenance dose • Toxicity Rare
Lidocaine • CNS depression with cessation of convulsions • Biphasic: – Blocks inhibitory CNS pathways resulting in stimulation – Blocks inhibitory/excitatory impulses resulting in CNS inhibition (Peralta 2007) • Walker, Slovis 1997 effective in peds not responding to barbs • Bolus + maintenance dose • Toxicity Rare
 Ketamine • Good Stops Seizures through anesthesia: NMDA antagonist with intrinsic sympathomimetic properties – 1 -4. 5 mg/kg – Borris et al 2000 • Bad Neurotoxicity • Diffuse cerebellar atrophy • 44 yo male, tx for status 3 months later- consistent with animal models Nmethyl-D-aspartate antagonist –mediated neurotoxicity • Ubogu et al 2003 • SE: Pyschotic
Ketamine • Good Stops Seizures through anesthesia: NMDA antagonist with intrinsic sympathomimetic properties – 1 -4. 5 mg/kg – Borris et al 2000 • Bad Neurotoxicity • Diffuse cerebellar atrophy • 44 yo male, tx for status 3 months later- consistent with animal models Nmethyl-D-aspartate antagonist –mediated neurotoxicity • Ubogu et al 2003 • SE: Pyschotic
 Using Anesthesia for Treatment of Refractory Status Epilepticus • Rosetti in Epilepsia 2007 – Each anesthetic has advantages/risks – Depends on the protocols regarding duration and depth of sedation – The biological background of the patient remains the prognostic determinant of SE
Using Anesthesia for Treatment of Refractory Status Epilepticus • Rosetti in Epilepsia 2007 – Each anesthetic has advantages/risks – Depends on the protocols regarding duration and depth of sedation – The biological background of the patient remains the prognostic determinant of SE
 Alternative Therapies • Hypothermia (31 -35 C) • Corry, Dhar, Murphy, Diringer 2006
Alternative Therapies • Hypothermia (31 -35 C) • Corry, Dhar, Murphy, Diringer 2006
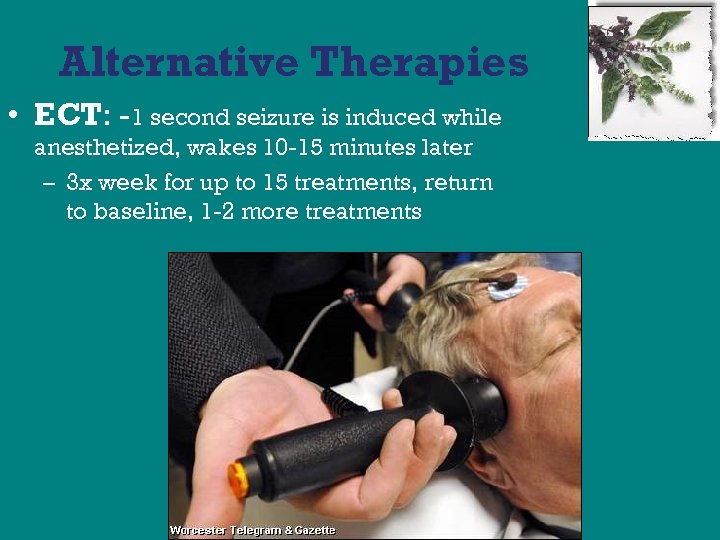 Alternative Therapies • ECT: -1 second seizure is induced while anesthetized, wakes 10 -15 minutes later – 3 x week for up to 15 treatments, return to baseline, 1 -2 more treatments
Alternative Therapies • ECT: -1 second seizure is induced while anesthetized, wakes 10 -15 minutes later – 3 x week for up to 15 treatments, return to baseline, 1 -2 more treatments
 Alternative Therapies • Ketogenic Diet: – High fats, low carbs – Strict diet requiring medical supervision – Body burns fat instead of glucose – Kids usually on for 2 years – Should we consider this in tube feeds?
Alternative Therapies • Ketogenic Diet: – High fats, low carbs – Strict diet requiring medical supervision – Body burns fat instead of glucose – Kids usually on for 2 years – Should we consider this in tube feeds?
 Nursing Considerations • Airway/Breathing: vented, full support, possiblity of VAP, need for aggressive pulmonary toileting • Circulation: hemodynamically unstable due to AEDs/coma inducing meds requiring vasoactive agents, increased risk of DVTS • Disability: (Neuro exam): pupils sometimes work. Can’t see more damage due to coma
Nursing Considerations • Airway/Breathing: vented, full support, possiblity of VAP, need for aggressive pulmonary toileting • Circulation: hemodynamically unstable due to AEDs/coma inducing meds requiring vasoactive agents, increased risk of DVTS • Disability: (Neuro exam): pupils sometimes work. Can’t see more damage due to coma
 Nursing Considerations • Expose: what does their skin/lines look like? Usually generally edematous, pressure sores common. Med rashes. • Fahrenheit: Poikilothermic, immune system suppressed, may need routine pan cultures • Family Finances…Increased anxiety • Gadgets: Scds, afo boots, hand splints, various machines for life support, eeg electrodes
Nursing Considerations • Expose: what does their skin/lines look like? Usually generally edematous, pressure sores common. Med rashes. • Fahrenheit: Poikilothermic, immune system suppressed, may need routine pan cultures • Family Finances…Increased anxiety • Gadgets: Scds, afo boots, hand splints, various machines for life support, eeg electrodes
 Nursing Considerations • Head to Toe: Assessment of physical appearance. Oh, how I wish I could wash their hair. • IV’s: site appearance, correct iv doses, do you have enough access? Do you need to make more pentobarb or levophed? Are you waiting for more depakote or an abx? • JP/Drains: hopefully, not needed.
Nursing Considerations • Head to Toe: Assessment of physical appearance. Oh, how I wish I could wash their hair. • IV’s: site appearance, correct iv doses, do you have enough access? Do you need to make more pentobarb or levophed? Are you waiting for more depakote or an abx? • JP/Drains: hopefully, not needed.
 Nursing Considerations • Keep Family Informed: This is the tricky part. I usually want to cry at this point. • Labs: Are you therapeutic? Have any of the weirdo labs come back from Mayo or the state? • Legal: Have we discussed DNR?
Nursing Considerations • Keep Family Informed: This is the tricky part. I usually want to cry at this point. • Labs: Are you therapeutic? Have any of the weirdo labs come back from Mayo or the state? • Legal: Have we discussed DNR?
 Nursing Considerations • Meds: Besides the AEDs, anticoagulants, GI motility agents, ABX, acid reduction agents, blood products, SSI… Do you have any more room on your Medication Administration Record? • Movement: PROM • Nutrition: Are they actually getting any with their gut shut down? High residuals? Have they developed an ileus? Are they on a bowel regimen with daily stimulation?
Nursing Considerations • Meds: Besides the AEDs, anticoagulants, GI motility agents, ABX, acid reduction agents, blood products, SSI… Do you have any more room on your Medication Administration Record? • Movement: PROM • Nutrition: Are they actually getting any with their gut shut down? High residuals? Have they developed an ileus? Are they on a bowel regimen with daily stimulation?
 ? ? ? NORSE at DUKE • In the last 10 years at Duke, we can identify at least 8 patients – All young (<35) – Previous good health – Initially Flu-like symptoms or pyschotic behavior, then status – Negative workup Survivors! – 4 AA female, 1 Asian female, 1 Lebanese male, 1 caucasian male and female 4
? ? ? NORSE at DUKE • In the last 10 years at Duke, we can identify at least 8 patients – All young (<35) – Previous good health – Initially Flu-like symptoms or pyschotic behavior, then status – Negative workup Survivors! – 4 AA female, 1 Asian female, 1 Lebanese male, 1 caucasian male and female 4
 Diagnosis: • By exclusion only • When? ? ?
Diagnosis: • By exclusion only • When? ? ?
 Workup Includes: *Radiographic Imagery (ct, mri) *Continuous eeg *Serum samples: Heavy Metals, Complex Virus, RMSF, Arbovirus, Rabies, Leptospiral Abs, Autoimmune *Brain Biopsy
Workup Includes: *Radiographic Imagery (ct, mri) *Continuous eeg *Serum samples: Heavy Metals, Complex Virus, RMSF, Arbovirus, Rabies, Leptospiral Abs, Autoimmune *Brain Biopsy
 Workup includes: • *CSF(culture, gram stains, cryptococcal antigens, herpes PCR polymerase chain reactions- replicate DNA) • *Stool (organisms/parasites) • *Infection Disease Consult
Workup includes: • *CSF(culture, gram stains, cryptococcal antigens, herpes PCR polymerase chain reactions- replicate DNA) • *Stool (organisms/parasites) • *Infection Disease Consult
 Why does having an actual diagnosis matter? • YOU TELL ME
Why does having an actual diagnosis matter? • YOU TELL ME
 Difference b/w TBI &NORSE?
Difference b/w TBI &NORSE?
 Why does having an actual diagnosis matter? • Merle Mishel Ph. D, FAAN- UNC Chapel Hill Uncertainty in Illness Theory
Why does having an actual diagnosis matter? • Merle Mishel Ph. D, FAAN- UNC Chapel Hill Uncertainty in Illness Theory
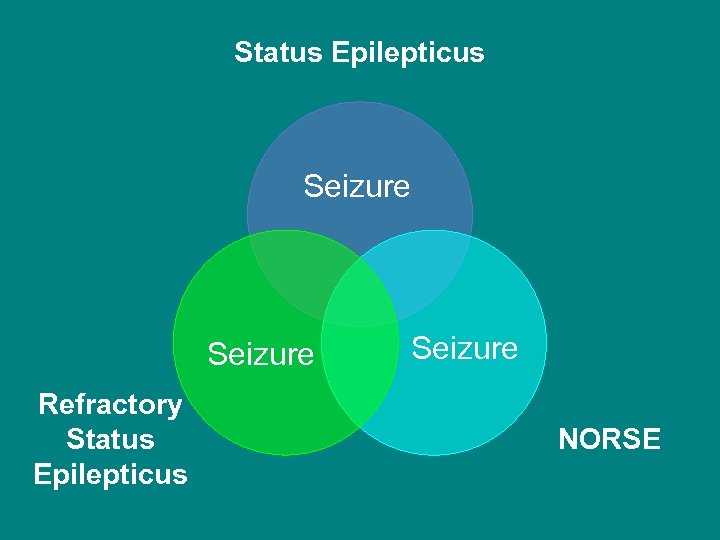 Status Epilepticus Seizure Refractory Status Epilepticus Seizure NORSE
Status Epilepticus Seizure Refractory Status Epilepticus Seizure NORSE
 Ladessa
Ladessa
 I’m a NORSE SURVIVOR!!!!
I’m a NORSE SURVIVOR!!!!
 Case Study #2 K. C. § 19 yo female with URI and fever 101. 0 § Z pack started § 2 days later, in car with family, started seizing and turning blue, incontinent of urine. § OSH- tonic clonic sz, intubated § Negative primary workup
Case Study #2 K. C. § 19 yo female with URI and fever 101. 0 § Z pack started § 2 days later, in car with family, started seizing and turning blue, incontinent of urine. § OSH- tonic clonic sz, intubated § Negative primary workup
 Case Study #2 K. C. • 2 days later extubated • Another sz, meds given, intubated • Sz continues, bradycardic and cyanotic • Transfer to Duke • 3 weeks after initial sz, off pentobarb, and smiling at dad
Case Study #2 K. C. • 2 days later extubated • Another sz, meds given, intubated • Sz continues, bradycardic and cyanotic • Transfer to Duke • 3 weeks after initial sz, off pentobarb, and smiling at dad
 Another Survivor!
Another Survivor!
 • • Bibliography Jirsch J. Hirsch LJ. Nonconvulsive seizures: developing a rational approach to the diagnosis and management in the critically ill population. Clin Neurophysiol. 2007118(8): 1660 -70. Robakis TK, Hirsch LJ. Literature review, case report, and expert discussion of prolonged refractory status epilepticus. Neurocrit Care. 2006. 4(1): 35 -46. Khaled KJ, Hirsch LJ. Advances in the Management of Seizures and Status Epilepticus in Critically Ill Patients. Crit Care Clin. 2007. (22): 637 -659. Wilder-Smith EPV, Lim ECH, Teoh HL, Sharma VK, Tan JJH, Chan BPL, Ong BKC. The NORSE (New Onset Refractory Status Epilepticus) Syndrome: Defining a Disease Entity. Ann Acad Med Singapore. 2005, 34: 417 -20. Hirsch LJ. , Kull L. Continuous EEG Monitoring in the Intensive Care Unit. Am. J. END Technol. 2004 (44): 137 -158. Hickey JV. The Clinical Practice of Neurological and Neurosurgical Nursing. Philadelphia: Lippincott, 1997. Corry JJ, Dhar R, Murphy T, Diringer MN. Hypothermia for Refractory Status Epilepticus. Neurocrit Care 2008: 9(2): 189 -97. Rosetti AO. Anesthesia for Treatment of Refractory Status Epilepticus. Epilepsia 2007. 48 (8): 52 -55
• • Bibliography Jirsch J. Hirsch LJ. Nonconvulsive seizures: developing a rational approach to the diagnosis and management in the critically ill population. Clin Neurophysiol. 2007118(8): 1660 -70. Robakis TK, Hirsch LJ. Literature review, case report, and expert discussion of prolonged refractory status epilepticus. Neurocrit Care. 2006. 4(1): 35 -46. Khaled KJ, Hirsch LJ. Advances in the Management of Seizures and Status Epilepticus in Critically Ill Patients. Crit Care Clin. 2007. (22): 637 -659. Wilder-Smith EPV, Lim ECH, Teoh HL, Sharma VK, Tan JJH, Chan BPL, Ong BKC. The NORSE (New Onset Refractory Status Epilepticus) Syndrome: Defining a Disease Entity. Ann Acad Med Singapore. 2005, 34: 417 -20. Hirsch LJ. , Kull L. Continuous EEG Monitoring in the Intensive Care Unit. Am. J. END Technol. 2004 (44): 137 -158. Hickey JV. The Clinical Practice of Neurological and Neurosurgical Nursing. Philadelphia: Lippincott, 1997. Corry JJ, Dhar R, Murphy T, Diringer MN. Hypothermia for Refractory Status Epilepticus. Neurocrit Care 2008: 9(2): 189 -97. Rosetti AO. Anesthesia for Treatment of Refractory Status Epilepticus. Epilepsia 2007. 48 (8): 52 -55
 Please contact me with questions or insight… mored 001@mc. duke. edu
Please contact me with questions or insight… mored 001@mc. duke. edu


