5116e849f02623f0b1715fc9e5efe5ec.ppt
- Количество слайдов: 113
 The Michigan Primary Care Transformation (Mi. PCT) Project WELCOME TO THE 2015 Mi. PCT SUMMIT!
The Michigan Primary Care Transformation (Mi. PCT) Project WELCOME TO THE 2015 Mi. PCT SUMMIT!
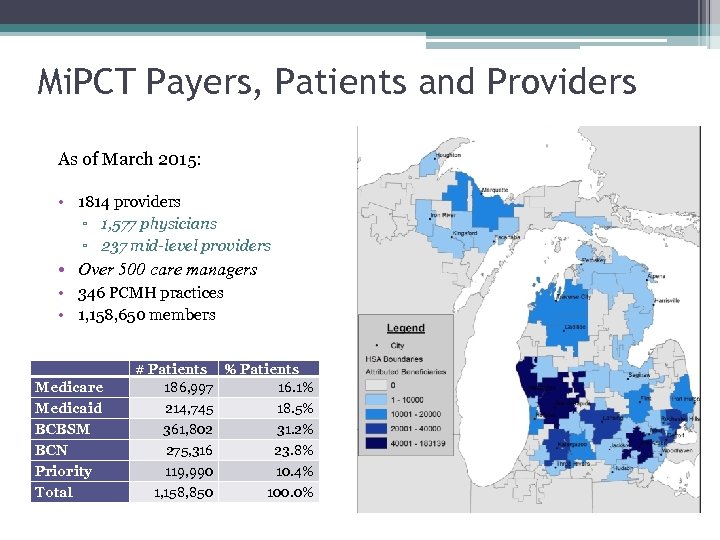 Mi. PCT Payers, Patients and Providers As of March 2015: • 1814 providers ▫ 1, 577 physicians ▫ 237 mid-level providers • Over 500 care managers • 346 PCMH practices • 1, 158, 650 members Medicare Medicaid BCBSM BCN Priority Total # Patients % Patients 186, 997 16. 1% 214, 745 18. 5% 361, 802 31. 2% 275, 316 23. 8% 119, 990 10. 4% 1, 158, 850 100. 0%
Mi. PCT Payers, Patients and Providers As of March 2015: • 1814 providers ▫ 1, 577 physicians ▫ 237 mid-level providers • Over 500 care managers • 346 PCMH practices • 1, 158, 650 members Medicare Medicaid BCBSM BCN Priority Total # Patients % Patients 186, 997 16. 1% 214, 745 18. 5% 361, 802 31. 2% 275, 316 23. 8% 119, 990 10. 4% 1, 158, 850 100. 0%
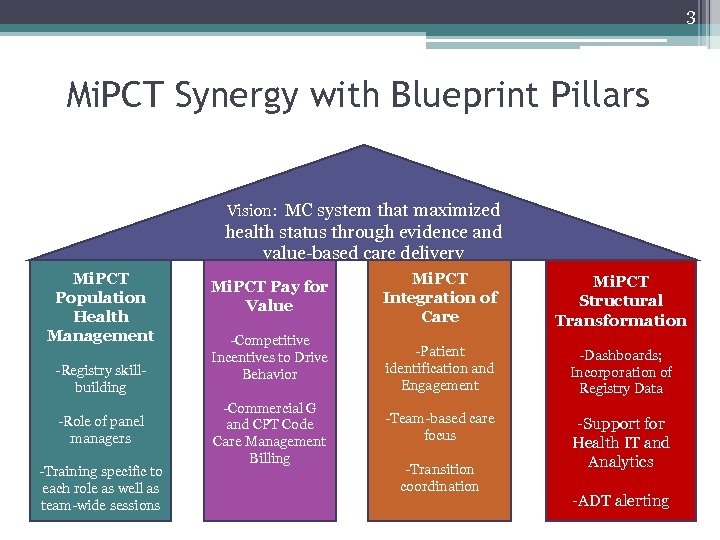 3 Mi. PCT Synergy with Blueprint Pillars Vision: MC system that maximized health status through evidence and value-based care delivery Mi. PCT Population Health Management -Registry skillbuilding -Role of panel managers -Training specific to each role as well as team-wide sessions Mi. PCT Pay for Value -Competitive Incentives to Drive Behavior -Commercial G and CPT Code Care Management Billing Mi. PCT Integration of Care Mi. PCT Structural Transformation -Patient identification and Engagement -Dashboards; Incorporation of Registry Data -Team-based care focus -Support for Health IT and Analytics -Transition coordination -ADT alerting
3 Mi. PCT Synergy with Blueprint Pillars Vision: MC system that maximized health status through evidence and value-based care delivery Mi. PCT Population Health Management -Registry skillbuilding -Role of panel managers -Training specific to each role as well as team-wide sessions Mi. PCT Pay for Value -Competitive Incentives to Drive Behavior -Commercial G and CPT Code Care Management Billing Mi. PCT Integration of Care Mi. PCT Structural Transformation -Patient identification and Engagement -Dashboards; Incorporation of Registry Data -Team-based care focus -Support for Health IT and Analytics -Transition coordination -ADT alerting
 The Michigan Primary Care Transformation (Mi. PCT) Project Evaluation and Program Updates 8: 40 -9: 10 AM
The Michigan Primary Care Transformation (Mi. PCT) Project Evaluation and Program Updates 8: 40 -9: 10 AM
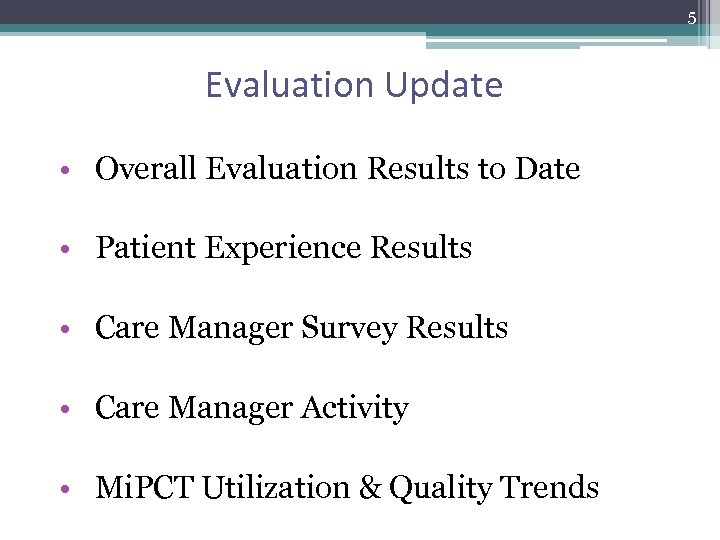 5 Evaluation Update • Overall Evaluation Results to Date • Patient Experience Results • Care Manager Survey Results • Care Manager Activity • Mi. PCT Utilization & Quality Trends
5 Evaluation Update • Overall Evaluation Results to Date • Patient Experience Results • Care Manager Survey Results • Care Manager Activity • Mi. PCT Utilization & Quality Trends
 6 Overall evaluation results to date • Cost savings for Medicare beneficiaries ▫ Caveat: quarter to quarter variation • All-payer utilization, 2011 - 2013 ▫ Increase in ED rates ▫ Moderate decline in hospitalizations • Patient experience (2015) ▫ Mi. PCT Adults generally more positive than non -Mi. PCT ▫ Mi. PCT parents about the same as non-Mi. PCT
6 Overall evaluation results to date • Cost savings for Medicare beneficiaries ▫ Caveat: quarter to quarter variation • All-payer utilization, 2011 - 2013 ▫ Increase in ED rates ▫ Moderate decline in hospitalizations • Patient experience (2015) ▫ Mi. PCT Adults generally more positive than non -Mi. PCT ▫ Mi. PCT parents about the same as non-Mi. PCT
 7 Overall evaluation results to date • Provider/staff survey reveals satisfaction with Care Management model • Care Management survey and PO data collection reveal progress on embedment • Care Manager activity leveling off: 25, 000 – 30, 000 unique patients per quarter
7 Overall evaluation results to date • Provider/staff survey reveals satisfaction with Care Management model • Care Management survey and PO data collection reveal progress on embedment • Care Manager activity leveling off: 25, 000 – 30, 000 unique patients per quarter
 8 Patient Experience Survey
8 Patient Experience Survey
 9 Methods • Stratified random sample ▫ Mi. PCT and comparison group status ▫ Payer ▫ High/very high risk concurrent risk category • Multi-modal (mail with phone follow-up) • Response rates ▫ Medicare ▫ Medicaid ▫ Commercial
9 Methods • Stratified random sample ▫ Mi. PCT and comparison group status ▫ Payer ▫ High/very high risk concurrent risk category • Multi-modal (mail with phone follow-up) • Response rates ▫ Medicare ▫ Medicaid ▫ Commercial
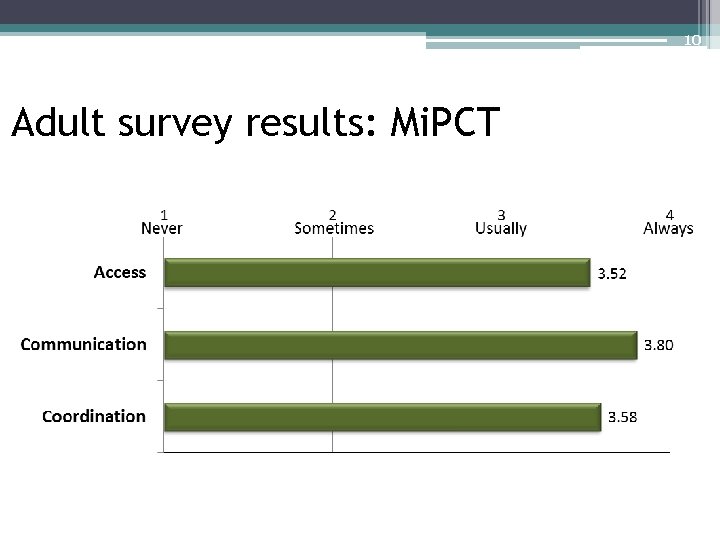 10 Adult survey results: Mi. PCT
10 Adult survey results: Mi. PCT
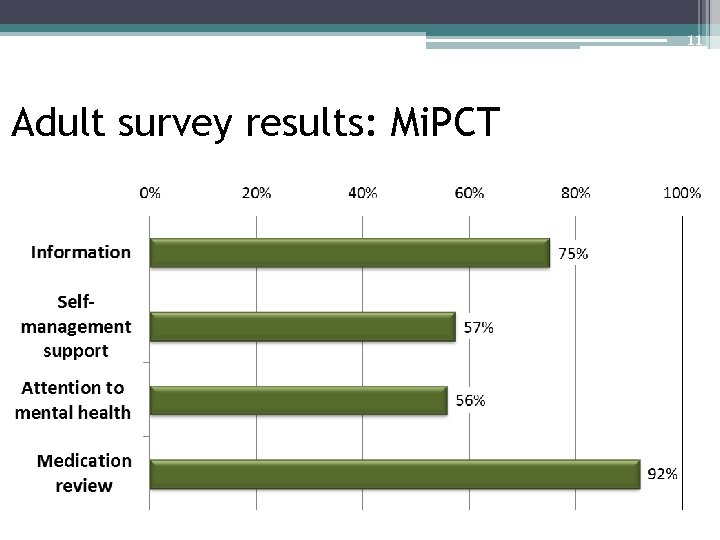 11 Adult survey results: Mi. PCT
11 Adult survey results: Mi. PCT
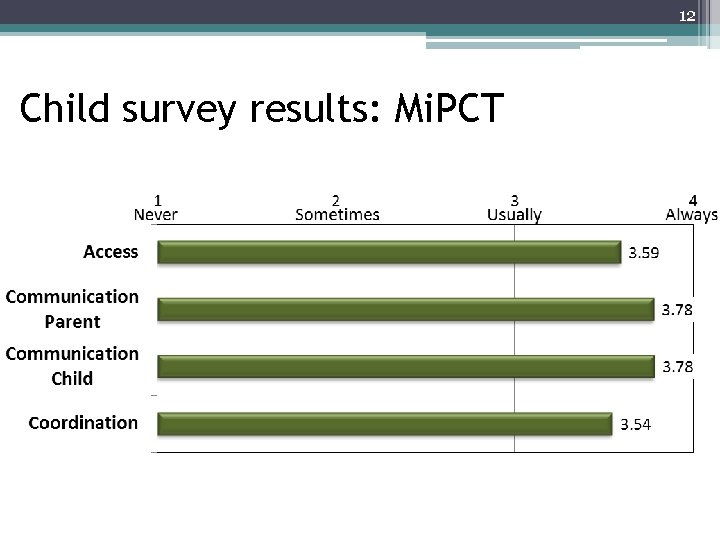 12 Child survey results: Mi. PCT
12 Child survey results: Mi. PCT
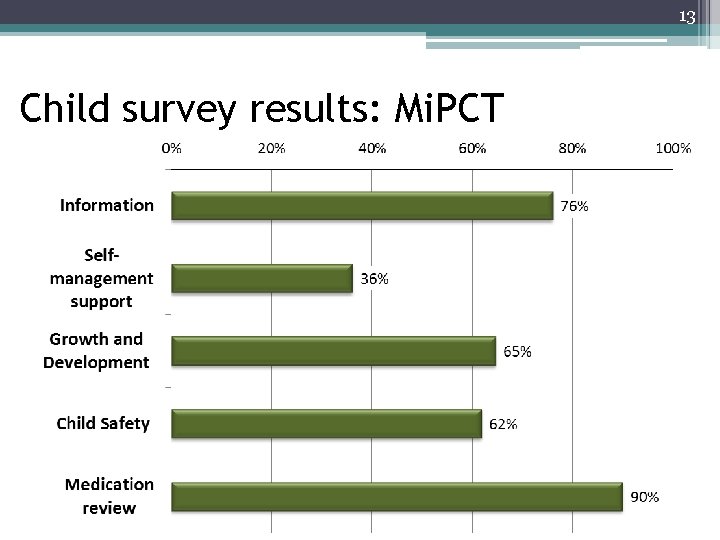 13 Child survey results: Mi. PCT Reported occurrence
13 Child survey results: Mi. PCT Reported occurrence
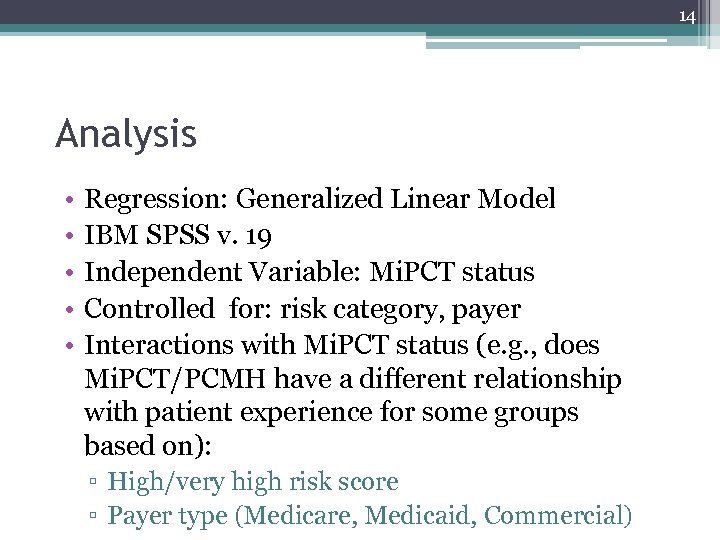 14 Analysis • • • Regression: Generalized Linear Model IBM SPSS v. 19 Independent Variable: Mi. PCT status Controlled for: risk category, payer Interactions with Mi. PCT status (e. g. , does Mi. PCT/PCMH have a different relationship with patient experience for some groups based on): ▫ High/very high risk score ▫ Payer type (Medicare, Medicaid, Commercial)
14 Analysis • • • Regression: Generalized Linear Model IBM SPSS v. 19 Independent Variable: Mi. PCT status Controlled for: risk category, payer Interactions with Mi. PCT status (e. g. , does Mi. PCT/PCMH have a different relationship with patient experience for some groups based on): ▫ High/very high risk score ▫ Payer type (Medicare, Medicaid, Commercial)
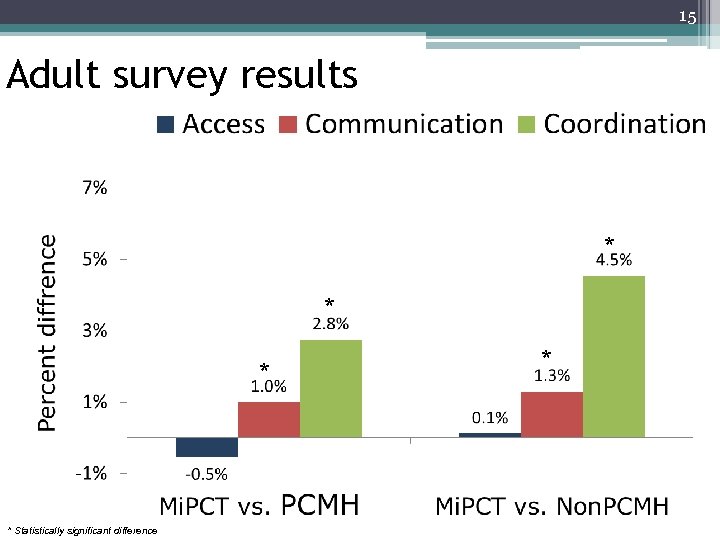 15 Adult survey results * * Statistically significant difference *
15 Adult survey results * * Statistically significant difference *
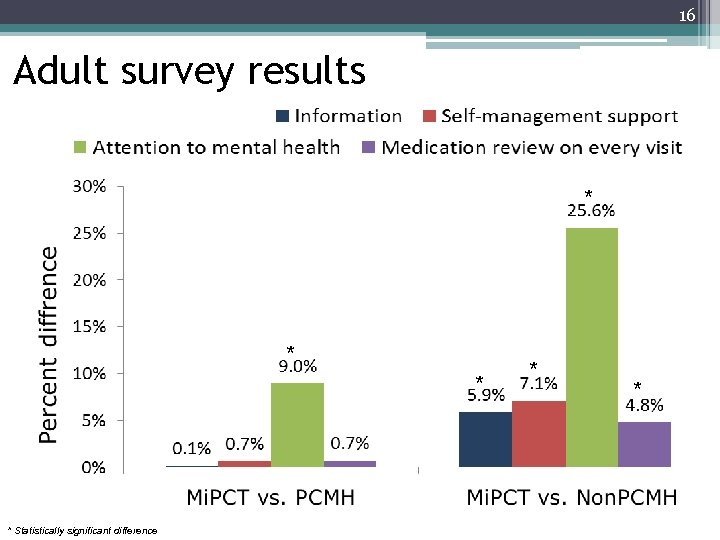 16 Adult survey results * * * Statistically significant difference * *
16 Adult survey results * * * Statistically significant difference * *
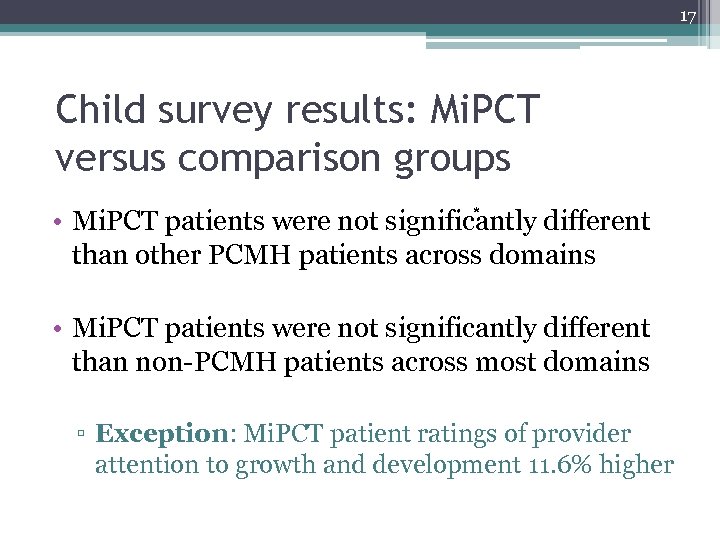 17 Child survey results: Mi. PCT versus comparison groups * • Mi. PCT patients were not significantly different than other PCMH patients across domains • Mi. PCT patients were not significantly different than non-PCMH patients across most domains ▫ Exception: Mi. PCT patient ratings of provider attention to growth and development 11. 6% higher
17 Child survey results: Mi. PCT versus comparison groups * • Mi. PCT patients were not significantly different than other PCMH patients across domains • Mi. PCT patients were not significantly different than non-PCMH patients across most domains ▫ Exception: Mi. PCT patient ratings of provider attention to growth and development 11. 6% higher
 18 Care Manager Survey Results
18 Care Manager Survey Results
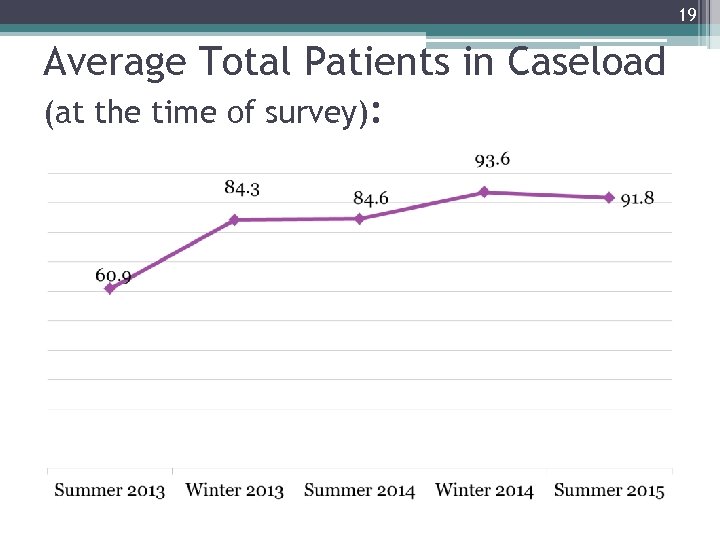 19 Average Total Patients in Caseload (at the time of survey):
19 Average Total Patients in Caseload (at the time of survey):
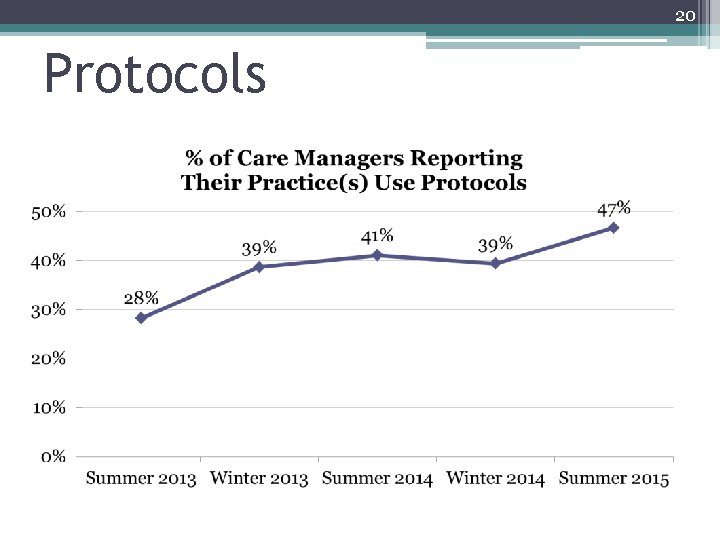 20 Protocols
20 Protocols
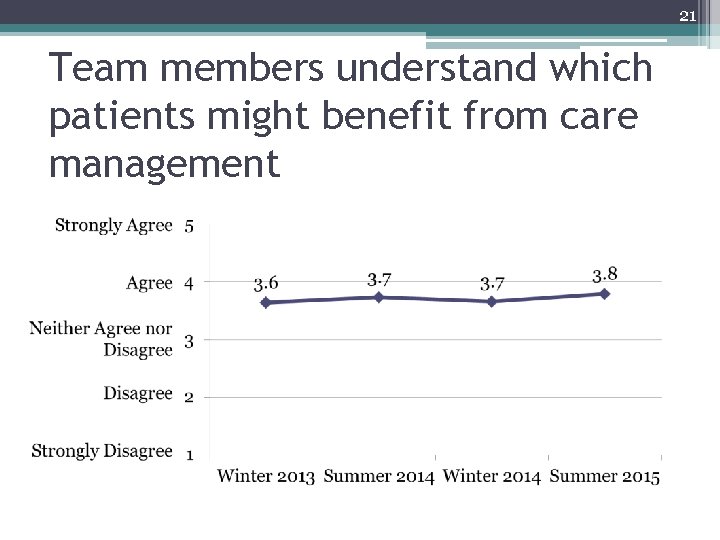 21 Team members understand which patients might benefit from care management
21 Team members understand which patients might benefit from care management
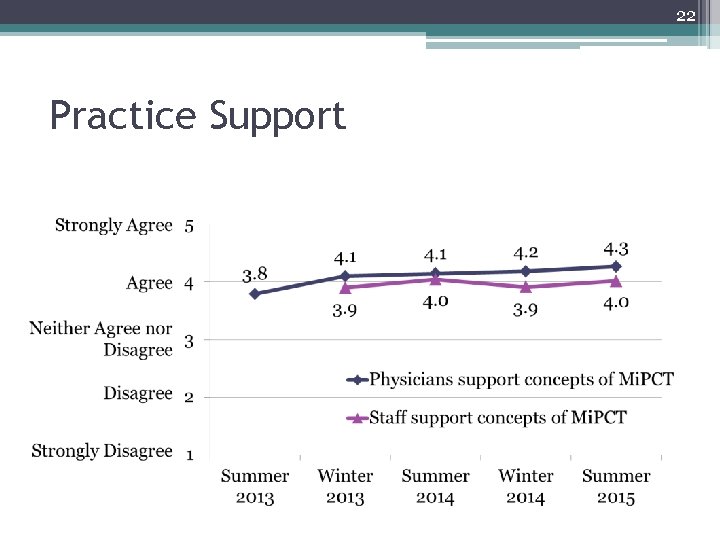 22 Practice Support
22 Practice Support
 23 Quarterly Report – Care Manager Activity
23 Quarterly Report – Care Manager Activity
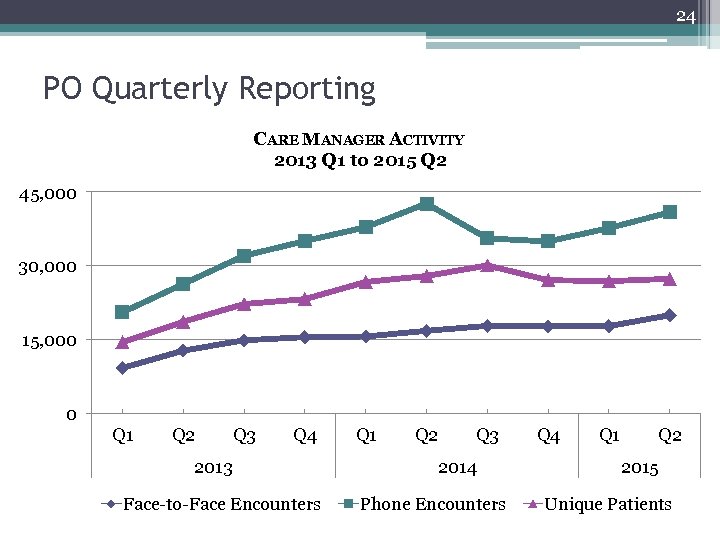 24 PO Quarterly Reporting CARE MANAGER ACTIVITY 2013 Q 1 to 2015 Q 2 45, 000 30, 000 15, 000 0 Q 1 Q 2 Q 3 Q 4 2013 Face-to-Face Encounters Q 1 Q 2 Q 3 2014 Phone Encounters Q 4 Q 1 Q 2 2015 Unique Patients
24 PO Quarterly Reporting CARE MANAGER ACTIVITY 2013 Q 1 to 2015 Q 2 45, 000 30, 000 15, 000 0 Q 1 Q 2 Q 3 Q 4 2013 Face-to-Face Encounters Q 1 Q 2 Q 3 2014 Phone Encounters Q 4 Q 1 Q 2 2015 Unique Patients
 25 Mi. PCT Utilization & Quality Trends 2011, 2012, & 2013
25 Mi. PCT Utilization & Quality Trends 2011, 2012, & 2013
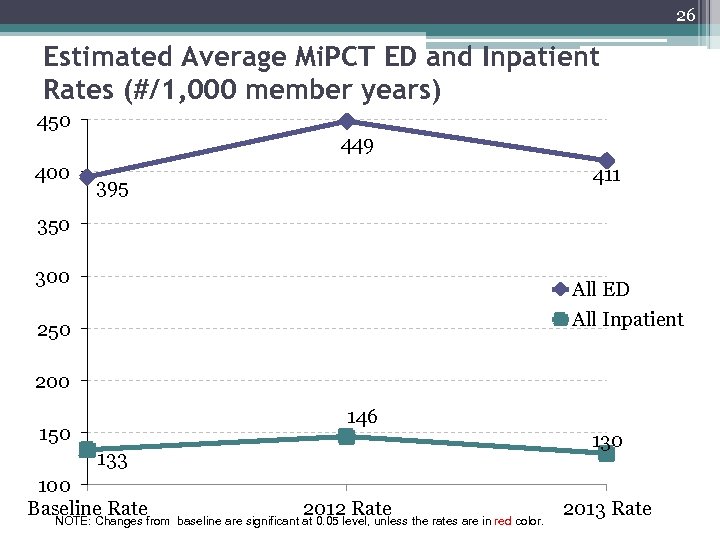 26 Estimated Average Mi. PCT ED and Inpatient Rates (#/1, 000 member years) 450 449 400 411 395 350 300 All ED All Inpatient 250 200 146 150 133 100 Baseline Ratefrom NOTE: Changes 2012 Rate baseline are significant at 0. 05 level, unless the rates are in red color. 2013 Rate
26 Estimated Average Mi. PCT ED and Inpatient Rates (#/1, 000 member years) 450 449 400 411 395 350 300 All ED All Inpatient 250 200 146 150 133 100 Baseline Ratefrom NOTE: Changes 2012 Rate baseline are significant at 0. 05 level, unless the rates are in red color. 2013 Rate
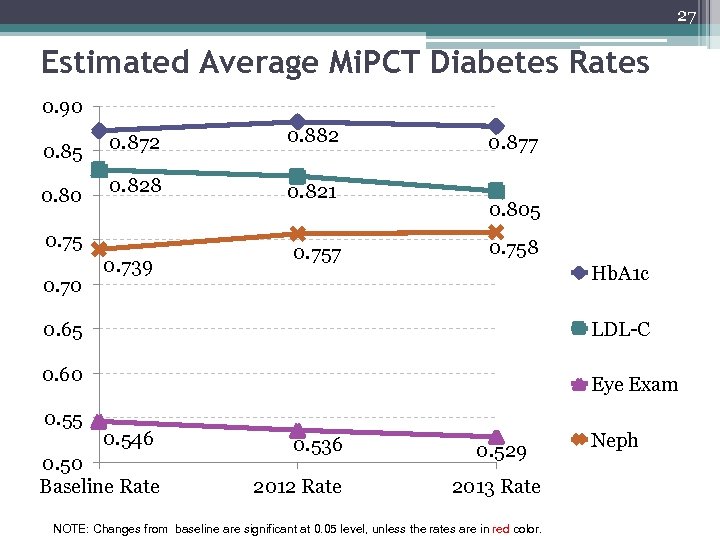 27 Estimated Average Mi. PCT Diabetes Rates 0. 90 0. 85 0. 80 0. 872 0. 882 0. 828 0. 821 0. 75 0. 70 0. 739 0. 757 0. 877 0. 805 0. 758 Hb. A 1 c LDL-C 0. 65 0. 60 0. 55 Eye Exam 0. 546 0. 50 Baseline Rate 0. 536 2012 Rate 0. 529 2013 Rate NOTE: Changes from baseline are significant at 0. 05 level, unless the rates are in red color. Neph
27 Estimated Average Mi. PCT Diabetes Rates 0. 90 0. 85 0. 80 0. 872 0. 882 0. 828 0. 821 0. 75 0. 70 0. 739 0. 757 0. 877 0. 805 0. 758 Hb. A 1 c LDL-C 0. 65 0. 60 0. 55 Eye Exam 0. 546 0. 50 Baseline Rate 0. 536 2012 Rate 0. 529 2013 Rate NOTE: Changes from baseline are significant at 0. 05 level, unless the rates are in red color. Neph
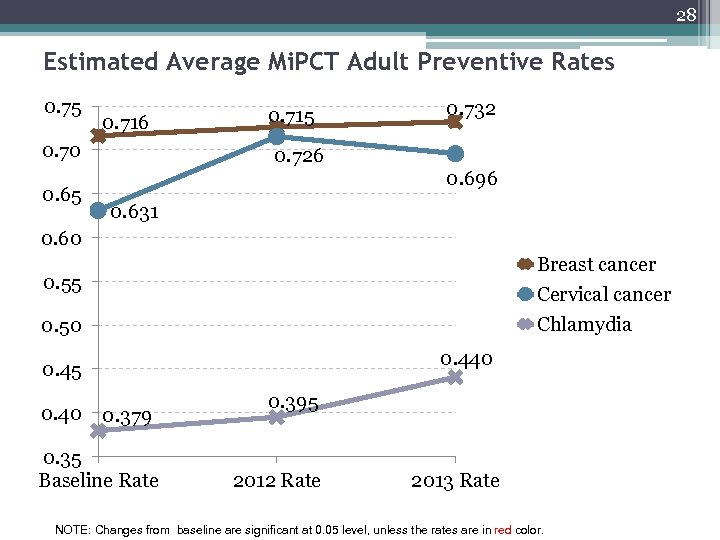 28 Estimated Average Mi. PCT Adult Preventive Rates 0. 75 0. 716 0. 70 0. 65 0. 715 0. 732 0. 726 0. 696 0. 631 0. 60 Breast cancer Cervical cancer Chlamydia 0. 55 0. 50 0. 440 0. 45 0. 40 0. 379 0. 35 Baseline Rate 0. 395 2012 Rate 2013 Rate NOTE: Changes from baseline are significant at 0. 05 level, unless the rates are in red color.
28 Estimated Average Mi. PCT Adult Preventive Rates 0. 75 0. 716 0. 70 0. 65 0. 715 0. 732 0. 726 0. 696 0. 631 0. 60 Breast cancer Cervical cancer Chlamydia 0. 55 0. 50 0. 440 0. 45 0. 40 0. 379 0. 35 Baseline Rate 0. 395 2012 Rate 2013 Rate NOTE: Changes from baseline are significant at 0. 05 level, unless the rates are in red color.
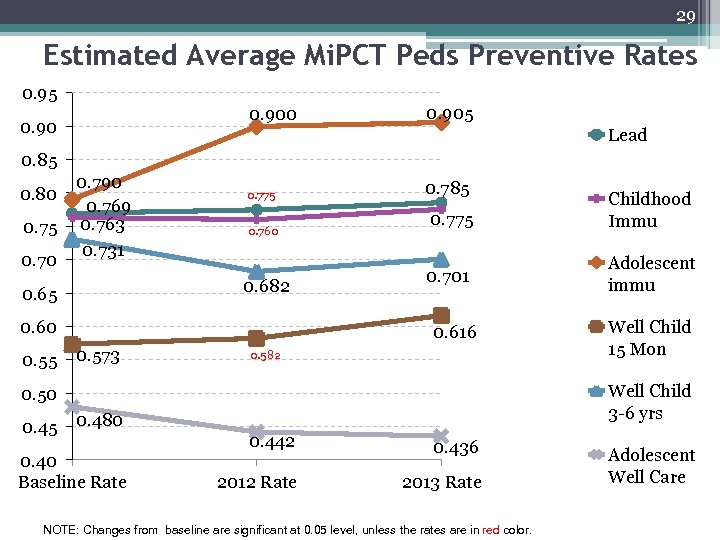 29 Estimated Average Mi. PCT Peds Preventive Rates 0. 95 0. 900 0. 905 Lead 0. 85 0. 80 0. 75 0. 70 0. 790 0. 769 0. 763 0. 731 0. 775 0. 760 0. 682 0. 65 0. 60 0. 55 0. 785 0. 775 Childhood Immu 0. 701 Adolescent immu 0. 616 0. 573 0. 582 Well Child 3 -6 yrs 0. 50 0. 45 0. 480 0. 40 Baseline Rate Well Child 15 Mon 0. 442 0. 436 2012 Rate 2013 Rate NOTE: Changes from baseline are significant at 0. 05 level, unless the rates are in red color. Adolescent Well Care
29 Estimated Average Mi. PCT Peds Preventive Rates 0. 95 0. 900 0. 905 Lead 0. 85 0. 80 0. 75 0. 70 0. 790 0. 769 0. 763 0. 731 0. 775 0. 760 0. 682 0. 65 0. 60 0. 55 0. 785 0. 775 Childhood Immu 0. 701 Adolescent immu 0. 616 0. 573 0. 582 Well Child 3 -6 yrs 0. 50 0. 45 0. 480 0. 40 Baseline Rate Well Child 15 Mon 0. 442 0. 436 2012 Rate 2013 Rate NOTE: Changes from baseline are significant at 0. 05 level, unless the rates are in red color. Adolescent Well Care
 30 Mi. PCT Clinical Update
30 Mi. PCT Clinical Update
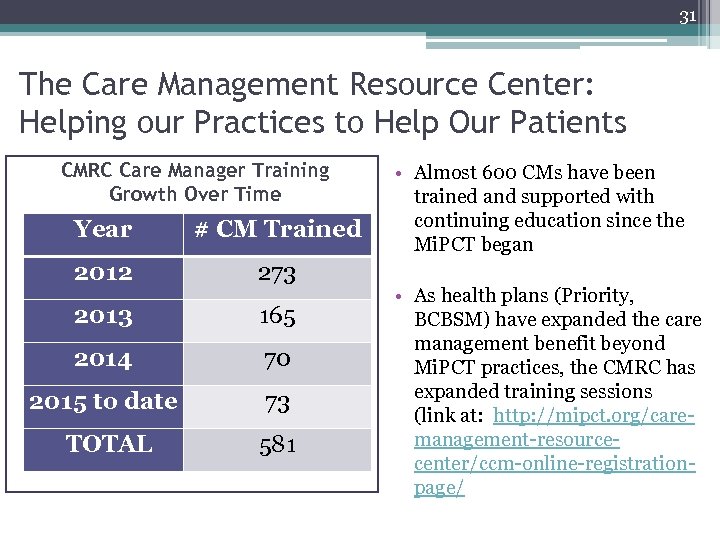 31 The Care Management Resource Center: Helping our Practices to Help Our Patients CMRC Care Manager Training Growth Over Time Year # CM Trained 2012 273 2013 165 2014 70 2015 to date 73 TOTAL 581 • Almost 600 CMs have been trained and supported with continuing education since the Mi. PCT began • As health plans (Priority, BCBSM) have expanded the care management benefit beyond Mi. PCT practices, the CMRC has expanded training sessions (link at: http: //mipct. org/caremanagement-resourcecenter/ccm-online-registrationpage/
31 The Care Management Resource Center: Helping our Practices to Help Our Patients CMRC Care Manager Training Growth Over Time Year # CM Trained 2012 273 2013 165 2014 70 2015 to date 73 TOTAL 581 • Almost 600 CMs have been trained and supported with continuing education since the Mi. PCT began • As health plans (Priority, BCBSM) have expanded the care management benefit beyond Mi. PCT practices, the CMRC has expanded training sessions (link at: http: //mipct. org/caremanagement-resourcecenter/ccm-online-registrationpage/
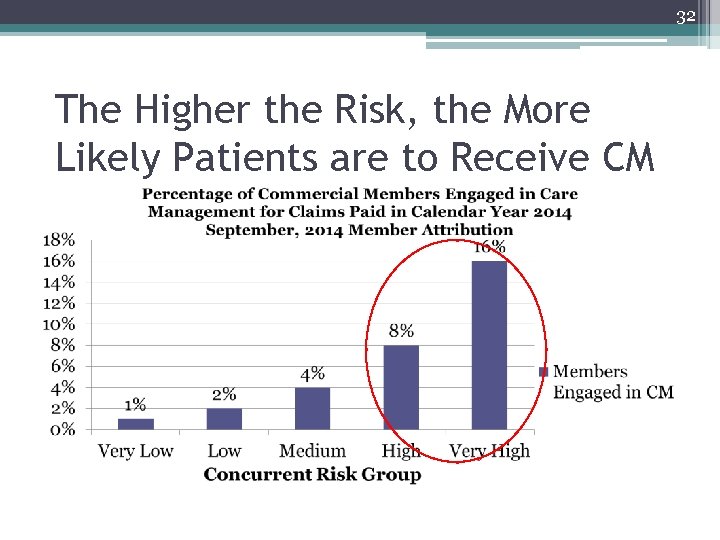 32 The Higher the Risk, the More Likely Patients are to Receive CM
32 The Higher the Risk, the More Likely Patients are to Receive CM
 33 Progress Recap 2015 -16 Clinical Focus Areas • Addressing social determinants of health and overcoming barriers ▫ Mary Ellen Benzik, Tiger Team Lead ▫ Toolkit and white paper in development • Integrating behavioral health ▫ ▫ Kevin Taylor, Tiger Team Lead Tiger Team tookit and white paper in development Advocacy: proposed CMS collaborative care model Coordinating with BCBSM/Priority Health work
33 Progress Recap 2015 -16 Clinical Focus Areas • Addressing social determinants of health and overcoming barriers ▫ Mary Ellen Benzik, Tiger Team Lead ▫ Toolkit and white paper in development • Integrating behavioral health ▫ ▫ Kevin Taylor, Tiger Team Lead Tiger Team tookit and white paper in development Advocacy: proposed CMS collaborative care model Coordinating with BCBSM/Priority Health work
 34 Progress Recap 2015 -16 Clinical Focus Areas • Patient registry and data support for population health ▫ Registry and EHR User groups being formed for systems most-used by Mi. PCT practices ▫ CMRC site visits to better understand spread processes highly linked to HEDIS and STAR improvement • Integrating palliative and end-of-life care ▫ Advocacy for CMS proposed advance care planning codes ▫ Ongoing work with Palliative Care subject matter experts • Addressing appropriateness of care (e. g. , Choosing Wisely program, etc. ) ▫ To launch in 2016
34 Progress Recap 2015 -16 Clinical Focus Areas • Patient registry and data support for population health ▫ Registry and EHR User groups being formed for systems most-used by Mi. PCT practices ▫ CMRC site visits to better understand spread processes highly linked to HEDIS and STAR improvement • Integrating palliative and end-of-life care ▫ Advocacy for CMS proposed advance care planning codes ▫ Ongoing work with Palliative Care subject matter experts • Addressing appropriateness of care (e. g. , Choosing Wisely program, etc. ) ▫ To launch in 2016
 35 Preparing for Sustainability: Never Too Early!
35 Preparing for Sustainability: Never Too Early!
 36 Strategy Avenue 1: CMS and State Policy • CMS Policy ▫ Potential 2017 Expansion of Comprehensive Primary Care Program (CPC) (our “sister” program) ▫ CPC milestones are very similar to the Mi. PCT Enhanced patient access and continuity of care, Planned chronic and preventive care, Risk-stratified care management, Patient and caregiver engagement, and Coordination of care across a “medical neighborhood” • State Policy ▫ SIM synergy ▫ Medicaid Managed Care Plan Rebid and Care Management
36 Strategy Avenue 1: CMS and State Policy • CMS Policy ▫ Potential 2017 Expansion of Comprehensive Primary Care Program (CPC) (our “sister” program) ▫ CPC milestones are very similar to the Mi. PCT Enhanced patient access and continuity of care, Planned chronic and preventive care, Risk-stratified care management, Patient and caregiver engagement, and Coordination of care across a “medical neighborhood” • State Policy ▫ SIM synergy ▫ Medicaid Managed Care Plan Rebid and Care Management
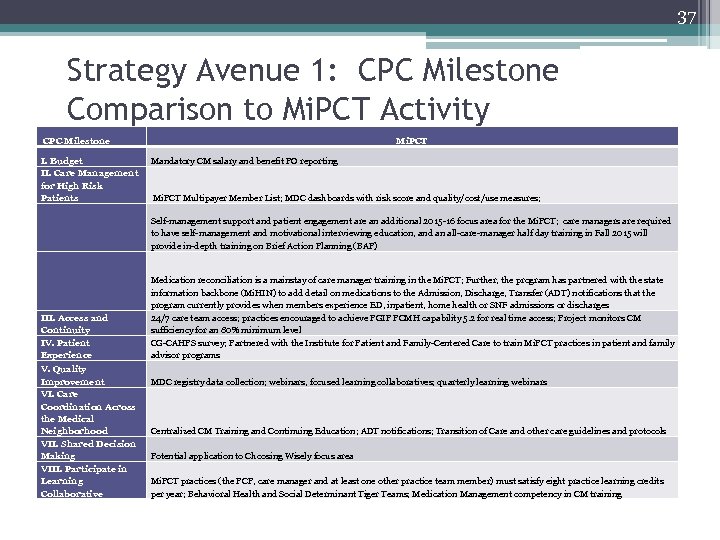 37 Strategy Avenue 1: CPC Milestone Comparison to Mi. PCT Activity CPC Milestone I. Budget II. Care Management for High Risk Patients Mi. PCT Mandatory CM salary and benefit PO reporting Mi. PCT Multipayer Member List; MDC dashboards with risk score and quality/cost/use measures; Self-management support and patient engagement are an additional 2015 -16 focus area for the Mi. PCT; care managers are required to have self-management and motivational interviewing education, and an all-care-manager half day training in Fall 2015 will provide in-depth training on Brief Action Planning (BAP) III. Access and Continuity IV. Patient Experience Medication reconciliation is a mainstay of care manager training in the Mi. PCT; Further, the program has partnered with the state information backbone (Mi. HIN) to add detail on medications to the Admission, Discharge, Transfer (ADT) notifications that the program currently provides when members experience ED, inpatient, home health or SNF admissions or discharges 24/7 care team access; practices encouraged to achieve PGIP PCMH capability 5. 2 for real time access; Project monitors CM sufficiency for an 80% minimum level CG-CAHPS survey; Partnered with the Institute for Patient and Family-Centered Care to train Mi. PCT practices in patient and family advisor programs V. Quality Improvement VI. Care Coordination Across the Medical Neighborhood VII. Shared Decision Making VIII. Participate in Learning Collaborative MDC registry data collection; webinars, focused learning collaboratives; quarterly learning webinars Centralized CM Training and Continuing Education; ADT notifications; Transition of Care and other care guidelines and protocols Potential application to Choosing Wisely focus area Mi. PCT practices (the PCP, care manager and at least one other practice team member) must satisfy eight practice learning credits per year; Behavioral Health and Social Determinant Tiger Teams; Medication Management competency in CM training
37 Strategy Avenue 1: CPC Milestone Comparison to Mi. PCT Activity CPC Milestone I. Budget II. Care Management for High Risk Patients Mi. PCT Mandatory CM salary and benefit PO reporting Mi. PCT Multipayer Member List; MDC dashboards with risk score and quality/cost/use measures; Self-management support and patient engagement are an additional 2015 -16 focus area for the Mi. PCT; care managers are required to have self-management and motivational interviewing education, and an all-care-manager half day training in Fall 2015 will provide in-depth training on Brief Action Planning (BAP) III. Access and Continuity IV. Patient Experience Medication reconciliation is a mainstay of care manager training in the Mi. PCT; Further, the program has partnered with the state information backbone (Mi. HIN) to add detail on medications to the Admission, Discharge, Transfer (ADT) notifications that the program currently provides when members experience ED, inpatient, home health or SNF admissions or discharges 24/7 care team access; practices encouraged to achieve PGIP PCMH capability 5. 2 for real time access; Project monitors CM sufficiency for an 80% minimum level CG-CAHPS survey; Partnered with the Institute for Patient and Family-Centered Care to train Mi. PCT practices in patient and family advisor programs V. Quality Improvement VI. Care Coordination Across the Medical Neighborhood VII. Shared Decision Making VIII. Participate in Learning Collaborative MDC registry data collection; webinars, focused learning collaboratives; quarterly learning webinars Centralized CM Training and Continuing Education; ADT notifications; Transition of Care and other care guidelines and protocols Potential application to Choosing Wisely focus area Mi. PCT practices (the PCP, care manager and at least one other practice team member) must satisfy eight practice learning credits per year; Behavioral Health and Social Determinant Tiger Teams; Medication Management competency in CM training
 38 Strategy Avenue 1, cont. Section 115 A of the Social Security Laws • (c) Expansion of models (phase ii). —Taking into account the evaluation under subsection (b)(4), the Secretary may, through rulemaking, expand (including implementation on a nationwide basis) the duration and the scope of a model that is being tested under subsection (b) or a demonstration project under section 1866 C, to the extent determined appropriate by the Secretary, if— • (1) the Secretary determines that such expansion is expected to— • (A) reduce spending under applicable title without reducing the quality of care; or • (B) improve the quality of patient care without increasing spending; • (2) the Chief Actuary of the Centers for Medicare & Medicaid Services certifies that such expansion would reduce (or would not result in any increase in) net program spending under applicable titles; and • (3) the Secretary determines that such expansion would not deny or limit the coverage or provision of benefits under the applicable title for applicable individuals. In determining which models or demonstration projects to expand under the preceding sentence, the Secretary shall focus on models and demonstration projects that improve the quality of patient care and reduce spending.
38 Strategy Avenue 1, cont. Section 115 A of the Social Security Laws • (c) Expansion of models (phase ii). —Taking into account the evaluation under subsection (b)(4), the Secretary may, through rulemaking, expand (including implementation on a nationwide basis) the duration and the scope of a model that is being tested under subsection (b) or a demonstration project under section 1866 C, to the extent determined appropriate by the Secretary, if— • (1) the Secretary determines that such expansion is expected to— • (A) reduce spending under applicable title without reducing the quality of care; or • (B) improve the quality of patient care without increasing spending; • (2) the Chief Actuary of the Centers for Medicare & Medicaid Services certifies that such expansion would reduce (or would not result in any increase in) net program spending under applicable titles; and • (3) the Secretary determines that such expansion would not deny or limit the coverage or provision of benefits under the applicable title for applicable individuals. In determining which models or demonstration projects to expand under the preceding sentence, the Secretary shall focus on models and demonstration projects that improve the quality of patient care and reduce spending.
 39 Strategy Avenue 2: Meeting Each Payer’s Goals Payer Leadership Meetings to understand what is important to each payer group so that we can better service their members – and deliver value that can help to sustain the program in the longer term HEDIS and STAR Measure Improvement Cost Savings Improved Coordination with Proactive Outreach Admission, Discharge, Transfer alert follow-up Servicing patients from all payers -- Medicaid, Medicare, BCBSM, Priority Health and BCN – who are likely to benefit from Care Management
39 Strategy Avenue 2: Meeting Each Payer’s Goals Payer Leadership Meetings to understand what is important to each payer group so that we can better service their members – and deliver value that can help to sustain the program in the longer term HEDIS and STAR Measure Improvement Cost Savings Improved Coordination with Proactive Outreach Admission, Discharge, Transfer alert follow-up Servicing patients from all payers -- Medicaid, Medicare, BCBSM, Priority Health and BCN – who are likely to benefit from Care Management
 40 Strategy Avenue 3: Leveraging Care Management Billing Codes • Billing and Coding Collaborative offers support to practices and POs (in Resources tab of mipctdemo. org) • G and CPT Codes - Billing for commercial members with proactive eligibility checking • Codes are Payable by Medicare (e. g. , ) ▫ Complex Care Management Code (99490) ▫ Transition of Care Codes (99495, 99496)
40 Strategy Avenue 3: Leveraging Care Management Billing Codes • Billing and Coding Collaborative offers support to practices and POs (in Resources tab of mipctdemo. org) • G and CPT Codes - Billing for commercial members with proactive eligibility checking • Codes are Payable by Medicare (e. g. , ) ▫ Complex Care Management Code (99490) ▫ Transition of Care Codes (99495, 99496)
 The Michigan Primary Care Transformation (Mi. PCT) Project The State Innovation Model and Population Health in Michigan Elizabeth Hertel, Director of Health Policy Innovation, State of Michigan 9: 20 -10: 20 AM
The Michigan Primary Care Transformation (Mi. PCT) Project The State Innovation Model and Population Health in Michigan Elizabeth Hertel, Director of Health Policy Innovation, State of Michigan 9: 20 -10: 20 AM
 State Innovation Model October 29, 2015
State Innovation Model October 29, 2015
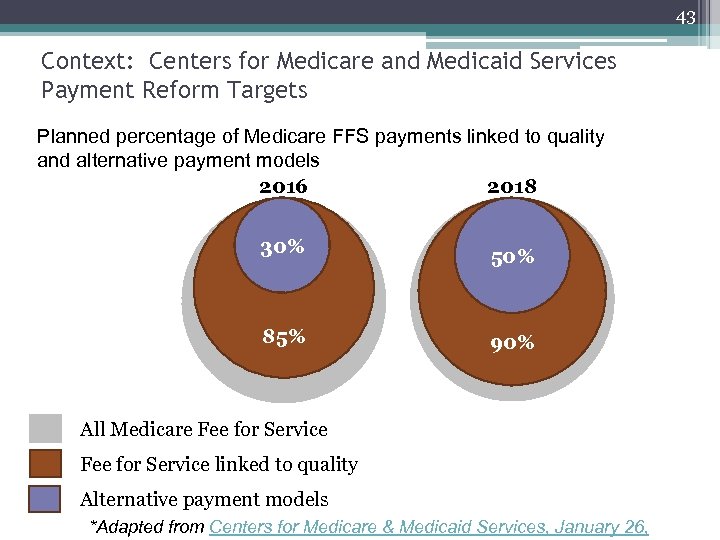 43 Context: Centers for Medicare and Medicaid Services Payment Reform Targets Planned percentage of Medicare FFS payments linked to quality and alternative payment models 2016 2018 30% 85% 50% 90% All Medicare Fee for Service linked to quality Alternative payment models *Adapted from Centers for Medicare & Medicaid Services, January 26,
43 Context: Centers for Medicare and Medicaid Services Payment Reform Targets Planned percentage of Medicare FFS payments linked to quality and alternative payment models 2016 2018 30% 85% 50% 90% All Medicare Fee for Service linked to quality Alternative payment models *Adapted from Centers for Medicare & Medicaid Services, January 26,
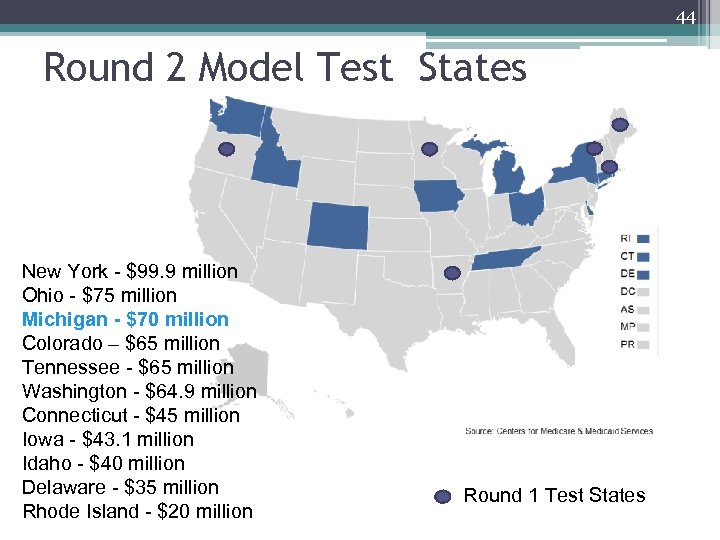 44 Round 2 Model Test States New York - $99. 9 million Ohio - $75 million Michigan - $70 million Colorado – $65 million Tennessee - $65 million Washington - $64. 9 million Connecticut - $45 million Iowa - $43. 1 million Idaho - $40 million Delaware - $35 million Rhode Island - $20 million Round 1 Test States
44 Round 2 Model Test States New York - $99. 9 million Ohio - $75 million Michigan - $70 million Colorado – $65 million Tennessee - $65 million Washington - $64. 9 million Connecticut - $45 million Iowa - $43. 1 million Idaho - $40 million Delaware - $35 million Rhode Island - $20 million Round 1 Test States
 45 Michigan State Innovation Model Proposal Overview • Michigan Blueprint for Health Innovation developed with broad stakeholder engagement in 2013 • Model Test proposal submitted July 2014 ▫ Closely follows Blueprint • Proposal presentation at Center for Medicare and Medicaid Innovation: October 2014 • $70 Million award announcement: December 2014 • Project begin date: February 1, 2015
45 Michigan State Innovation Model Proposal Overview • Michigan Blueprint for Health Innovation developed with broad stakeholder engagement in 2013 • Model Test proposal submitted July 2014 ▫ Closely follows Blueprint • Proposal presentation at Center for Medicare and Medicaid Innovation: October 2014 • $70 Million award announcement: December 2014 • Project begin date: February 1, 2015
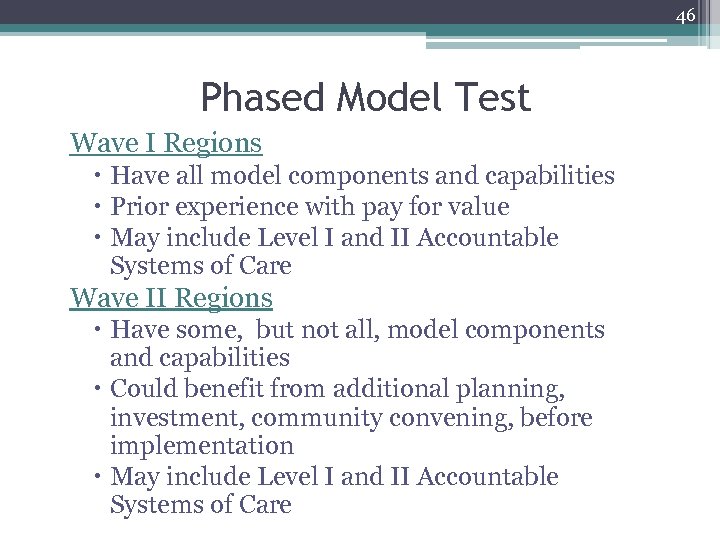 46 Phased Model Test Wave I Regions Have all model components and capabilities Prior experience with pay for value May include Level I and II Accountable Systems of Care Wave II Regions Have some, but not all, model components and capabilities Could benefit from additional planning, investment, community convening, before implementation May include Level I and II Accountable Systems of Care
46 Phased Model Test Wave I Regions Have all model components and capabilities Prior experience with pay for value May include Level I and II Accountable Systems of Care Wave II Regions Have some, but not all, model components and capabilities Could benefit from additional planning, investment, community convening, before implementation May include Level I and II Accountable Systems of Care
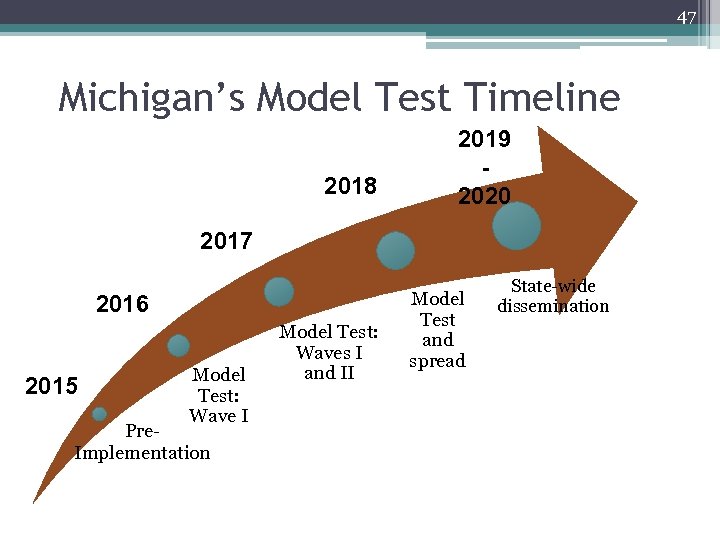 47 Michigan’s Model Test Timeline 2018 2019 2020 2017 2016 2015 Model Test: Wave I Pre. Implementation Model Test: Waves I and II Model Test and spread State-wide dissemination
47 Michigan’s Model Test Timeline 2018 2019 2020 2017 2016 2015 Model Test: Wave I Pre. Implementation Model Test: Waves I and II Model Test and spread State-wide dissemination
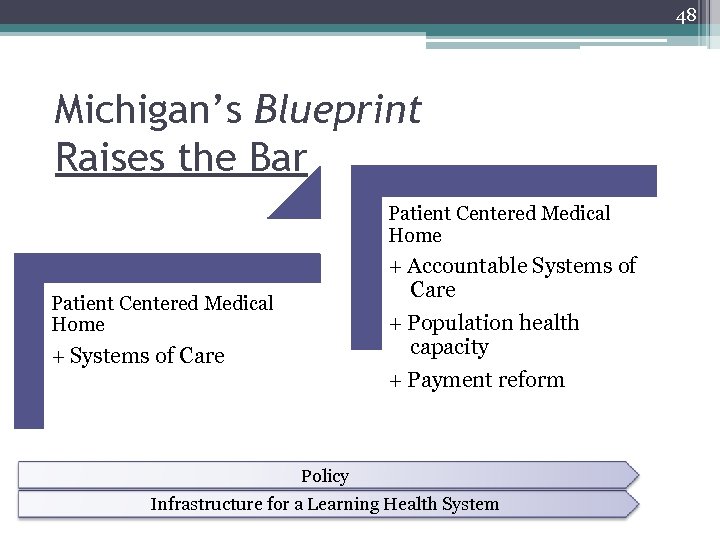 48 Michigan’s Blueprint Raises the Bar Patient Centered Medical Home + Accountable Systems of Care + Population health capacity + Payment reform Patient Centered Medical Home + Systems of Care Policy Infrastructure for a Learning Health System
48 Michigan’s Blueprint Raises the Bar Patient Centered Medical Home + Accountable Systems of Care + Population health capacity + Payment reform Patient Centered Medical Home + Systems of Care Policy Infrastructure for a Learning Health System
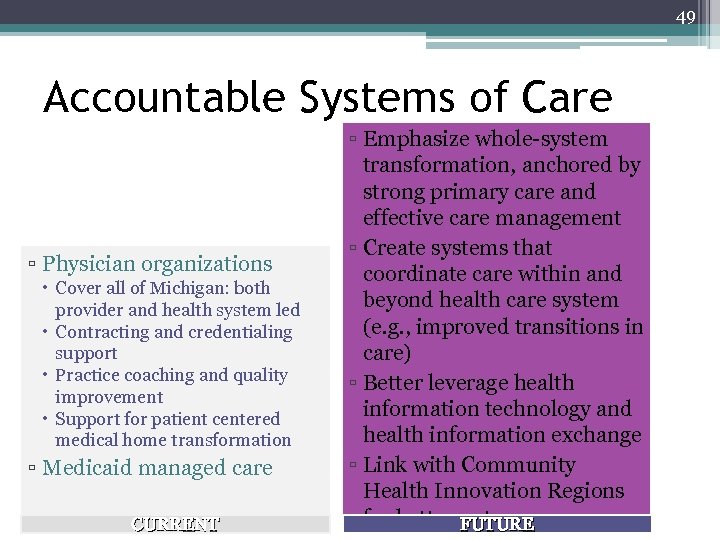 49 Accountable Systems of Care ▫ Physician organizations Cover all of Michigan: both provider and health system led Contracting and credentialing support Practice coaching and quality improvement Support for patient centered medical home transformation ▫ Medicaid managed care CURRENT ▫ Emphasize whole-system transformation, anchored by strong primary care and effective care management ▫ Create systems that coordinate care within and beyond health care system (e. g. , improved transitions in care) ▫ Better leverage health information technology and health information exchange ▫ Link with Community Health Innovation Regions for better outcomes FUTURE
49 Accountable Systems of Care ▫ Physician organizations Cover all of Michigan: both provider and health system led Contracting and credentialing support Practice coaching and quality improvement Support for patient centered medical home transformation ▫ Medicaid managed care CURRENT ▫ Emphasize whole-system transformation, anchored by strong primary care and effective care management ▫ Create systems that coordinate care within and beyond health care system (e. g. , improved transitions in care) ▫ Better leverage health information technology and health information exchange ▫ Link with Community Health Innovation Regions for better outcomes FUTURE
 50 State Innovation Model Performance Measures ▫ Drive adoption of a core set of measures ▫ Align payment and core set of measures across payers to reduce administrative complexity and provider burden Michigan State Medical Society has developed a common clinical measure list across several Michigan payers State Innovation Model Performance Measurement and Recognition Committee will establish additional process and population health measures
50 State Innovation Model Performance Measures ▫ Drive adoption of a core set of measures ▫ Align payment and core set of measures across payers to reduce administrative complexity and provider burden Michigan State Medical Society has developed a common clinical measure list across several Michigan payers State Innovation Model Performance Measurement and Recognition Committee will establish additional process and population health measures
 51 Payment Reform • Align with trend toward payment for population level performance, moving away from fee-for-service ▫ Level I: Shared savings (upside risk) ▫ Level II: Capitation models • Designed to drive: ▫ Consistent delivery of high-quality, person/family-centered care ▫ Reductions in low-value care ▫ Reductions in avoidable acute care utilization • Provide for investments in community health
51 Payment Reform • Align with trend toward payment for population level performance, moving away from fee-for-service ▫ Level I: Shared savings (upside risk) ▫ Level II: Capitation models • Designed to drive: ▫ Consistent delivery of high-quality, person/family-centered care ▫ Reductions in low-value care ▫ Reductions in avoidable acute care utilization • Provide for investments in community health
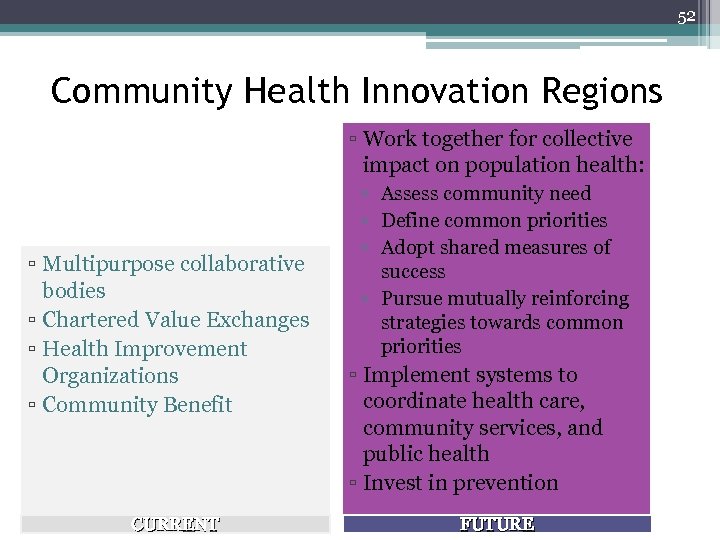 52 Community Health Innovation Regions ▫ Work together for collective impact on population health: ▫ Multipurpose collaborative bodies ▫ Chartered Value Exchanges ▫ Health Improvement Organizations ▫ Community Benefit CURRENT ▫ Assess community need ▫ Define common priorities ▫ Adopt shared measures of success ▫ Pursue mutually reinforcing strategies towards common priorities ▫ Implement systems to coordinate health care, community services, and public health ▫ Invest in prevention FUTURE
52 Community Health Innovation Regions ▫ Work together for collective impact on population health: ▫ Multipurpose collaborative bodies ▫ Chartered Value Exchanges ▫ Health Improvement Organizations ▫ Community Benefit CURRENT ▫ Assess community need ▫ Define common priorities ▫ Adopt shared measures of success ▫ Pursue mutually reinforcing strategies towards common priorities ▫ Implement systems to coordinate health care, community services, and public health ▫ Invest in prevention FUTURE
 53 Health Information Exchange/ Health Information Technology • Key functions of Health Information Exchange in State Innovation Model: ▫ Support care coordination within Accountable Systems of Care and across the health care system ▫ Support community linkages to better address social determinants ▫ Allow real-time performance monitoring, rapid-cycle improvement processes ▫ Infrastructure components ▫ Electronic Medical Record functionality ▫ Connection to sub-state Health Information Exchange ▫ Data aggregator
53 Health Information Exchange/ Health Information Technology • Key functions of Health Information Exchange in State Innovation Model: ▫ Support care coordination within Accountable Systems of Care and across the health care system ▫ Support community linkages to better address social determinants ▫ Allow real-time performance monitoring, rapid-cycle improvement processes ▫ Infrastructure components ▫ Electronic Medical Record functionality ▫ Connection to sub-state Health Information Exchange ▫ Data aggregator
 54 State Innovation Model Target Populations • Healthy babies • Emergency Department super-utilization (8+ visits/year) • Multiple chronic conditions
54 State Innovation Model Target Populations • Healthy babies • Emergency Department super-utilization (8+ visits/year) • Multiple chronic conditions
 55 Medicaid Managed Care Rebid • Managed Care Rebid ▫ Plans and regions announced October 15, 2015 ▫ Requires health plan participation in the State Innovation Model ▫ Specifically promotes key components of delivery system transformation: Patient-centered medical homes Support for care management Community health workers
55 Medicaid Managed Care Rebid • Managed Care Rebid ▫ Plans and regions announced October 15, 2015 ▫ Requires health plan participation in the State Innovation Model ▫ Specifically promotes key components of delivery system transformation: Patient-centered medical homes Support for care management Community health workers
 56 Pre-Implementation Update • Complete ▫ Accountable System of Care and Community Health Innovation Region capacity assessments reviewed • To Do ▫ Region and site selection ▫ Develop key program materials for feedback • Looking ahead ▫ Finalize programs ▫ Develop operational plans with Model Test participants ▫ Execute agreements with Model Test participants ▫ Launch Model Test learning system ▫ Implement payment reform
56 Pre-Implementation Update • Complete ▫ Accountable System of Care and Community Health Innovation Region capacity assessments reviewed • To Do ▫ Region and site selection ▫ Develop key program materials for feedback • Looking ahead ▫ Finalize programs ▫ Develop operational plans with Model Test participants ▫ Execute agreements with Model Test participants ▫ Launch Model Test learning system ▫ Implement payment reform
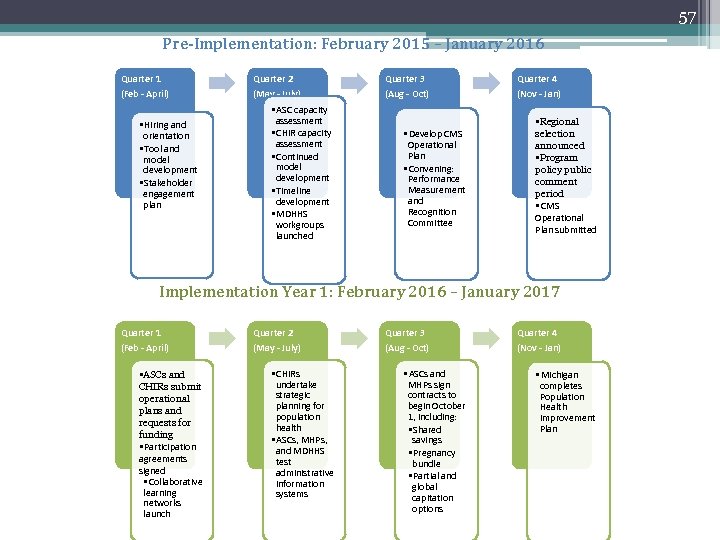 57 Pre-Implementation: February 2015 – January 2016 Quarter 1 Quarter 2 Quarter 3 Quarter 4 (Feb - April) (May - July) (Aug - Oct) (Nov - Jan) • Hiring and orientation • Tool and model development • Stakeholder engagement plan • ASC capacity assessment • CHIR capacity assessment • Continued model development • Timeline development • MDHHS workgroups launched • Develop CMS Operational Plan • Convening: Performance Measurement and Recognition Committee • Regional selection announced • Program policy public comment period • CMS Operational Plan submitted Implementation Year 1: February 2016 – January 2017 Quarter 1 Quarter 2 Quarter 3 Quarter 4 (Feb - April) (May - July) (Aug - Oct) (Nov - Jan) • ASCs and CHIRs submit operational plans and requests for funding • Participation agreements signed • Collaborative learning networks launch • CHIRs undertake strategic planning for population health • ASCs, MHPs, and MDHHS test administrative information systems • ASCs and MHPs sign contracts to begin October 1, including: • Shared savings • Pregnancy bundle • Partial and global capitation options • Michigan completes Population Health Improvement Plan
57 Pre-Implementation: February 2015 – January 2016 Quarter 1 Quarter 2 Quarter 3 Quarter 4 (Feb - April) (May - July) (Aug - Oct) (Nov - Jan) • Hiring and orientation • Tool and model development • Stakeholder engagement plan • ASC capacity assessment • CHIR capacity assessment • Continued model development • Timeline development • MDHHS workgroups launched • Develop CMS Operational Plan • Convening: Performance Measurement and Recognition Committee • Regional selection announced • Program policy public comment period • CMS Operational Plan submitted Implementation Year 1: February 2016 – January 2017 Quarter 1 Quarter 2 Quarter 3 Quarter 4 (Feb - April) (May - July) (Aug - Oct) (Nov - Jan) • ASCs and CHIRs submit operational plans and requests for funding • Participation agreements signed • Collaborative learning networks launch • CHIRs undertake strategic planning for population health • ASCs, MHPs, and MDHHS test administrative information systems • ASCs and MHPs sign contracts to begin October 1, including: • Shared savings • Pregnancy bundle • Partial and global capitation options • Michigan completes Population Health Improvement Plan
 The Michigan Primary Care Transformation (Mi. PCT) Project Celebrating Best Practices! 10: 50 -11: 50 AM
The Michigan Primary Care Transformation (Mi. PCT) Project Celebrating Best Practices! 10: 50 -11: 50 AM
 Celebrating Success in Mi. PCT Practices!
Celebrating Success in Mi. PCT Practices!
 Practice Awards-Categories • Best Overall – Adult and Family Medicine Practices • Most Improved – Adult and Family Medicine • Best Overall – Pediatric Practices • Most Improved – Pediatrics • Best Overall - Diabetes • Diabetic Metric Improvement
Practice Awards-Categories • Best Overall – Adult and Family Medicine Practices • Most Improved – Adult and Family Medicine • Best Overall – Pediatric Practices • Most Improved – Pediatrics • Best Overall - Diabetes • Diabetic Metric Improvement
 Risk Adjustment (for top overall awards) • Purpose To level the playing field so that practices are recognized for performance, not for the underlying characteristics of their population • Considerations Health status Demographics Payer mix Practice average risk score (concurrent) % Medicare, % Medicaid, % Commercial
Risk Adjustment (for top overall awards) • Purpose To level the playing field so that practices are recognized for performance, not for the underlying characteristics of their population • Considerations Health status Demographics Payer mix Practice average risk score (concurrent) % Medicare, % Medicaid, % Commercial
 Risk Adjustment (continued) • Methods ▫ Implemented by MPHI and approved by the Stewardship and Performance Committee ▫ Involves comparing how the practice actually performed to how we would have expected it to perform if we knew nothing other than these population characteristics • Application ▫ Best overall adult, diabetes and pediatric awards ▫ Not applied to award categories for most improved
Risk Adjustment (continued) • Methods ▫ Implemented by MPHI and approved by the Stewardship and Performance Committee ▫ Involves comparing how the practice actually performed to how we would have expected it to perform if we knew nothing other than these population characteristics • Application ▫ Best overall adult, diabetes and pediatric awards ▫ Not applied to award categories for most improved
 Best Overall – Adult and Family Practices – Risk Adjusted* • Composite score based on practices’ rankings in the following MDC Measures, risk adjusted by MPHI: ▫ ▫ ▫ Inpatient Admissions ED Visits per 1000 Patients PCS ED Visits Acute ACSC Admission Rate Chronic ACSC Admission Rate Diabetes Overall
Best Overall – Adult and Family Practices – Risk Adjusted* • Composite score based on practices’ rankings in the following MDC Measures, risk adjusted by MPHI: ▫ ▫ ▫ Inpatient Admissions ED Visits per 1000 Patients PCS ED Visits Acute ACSC Admission Rate Chronic ACSC Admission Rate Diabetes Overall
 Most Improved – Adult and Family • Greatest difference in Overall Ranking between baseline (calendar year 2011) and current measurement period as of the April, 2015 release (claims incurred October, 2013 – September, 2014). For example, a practice that moved from rank 200 to rank 100 would count as “more improved” than one that moved from rank 50 to rank 1.
Most Improved – Adult and Family • Greatest difference in Overall Ranking between baseline (calendar year 2011) and current measurement period as of the April, 2015 release (claims incurred October, 2013 – September, 2014). For example, a practice that moved from rank 200 to rank 100 would count as “more improved” than one that moved from rank 50 to rank 1.
 Diabetes Overall - Risk Adjusted* • Composite score based on practices’ rankings in the following MDC Clinical (non-supplemented) measures; composite (not components) are risk adjusted by MPHI: ▫ ▫ Diabetes Eye Exam Diabetes Hb. A 1 c Diabetes LDL-C Diabetes Nephropathy
Diabetes Overall - Risk Adjusted* • Composite score based on practices’ rankings in the following MDC Clinical (non-supplemented) measures; composite (not components) are risk adjusted by MPHI: ▫ ▫ Diabetes Eye Exam Diabetes Hb. A 1 c Diabetes LDL-C Diabetes Nephropathy
 Diabetes Metric Improvement • Greatest percent difference in Diabetes Overall Score between baseline (calendar year 2011) and current measurement period (claims incurred October, 2013 – September, 2014) for all non-Pediatric practices. • Note that for this measure we are looking at improvement in Score NOT improvement in Rank.
Diabetes Metric Improvement • Greatest percent difference in Diabetes Overall Score between baseline (calendar year 2011) and current measurement period (claims incurred October, 2013 – September, 2014) for all non-Pediatric practices. • Note that for this measure we are looking at improvement in Score NOT improvement in Rank.
 Best Overall – Pediatric Practices - Risk Adjusted* • Pediatric Practices are defined as those where >= 85% of attributed patients (based on current measurement period patient attribution) are <= 21 years of age. • Note that in cases where we filter to include only “pediatric” patients we will use <18 as the cutoff age for Pediatrics. This only comes into play where MPHI has requested demographic data be filtered by age for risk adjustment. All MDC measures have age limits built into their calculations (e. g. Well Child visits for different age groups only look at members in those age groups, Adult ACSC utilization measures only look at members >= 18) • Composite score based on pediatric practices’ rankings for the following MDC Measures, risk adjusted by MPHI: ▫ Pediatric Inpatient Visit Rate with Previous Asthma Diagnosis ▫ Pediatric ED Visit Rate with Previous Asthma Diagnosis ▫ Pediatric Preventive Overall
Best Overall – Pediatric Practices - Risk Adjusted* • Pediatric Practices are defined as those where >= 85% of attributed patients (based on current measurement period patient attribution) are <= 21 years of age. • Note that in cases where we filter to include only “pediatric” patients we will use <18 as the cutoff age for Pediatrics. This only comes into play where MPHI has requested demographic data be filtered by age for risk adjustment. All MDC measures have age limits built into their calculations (e. g. Well Child visits for different age groups only look at members in those age groups, Adult ACSC utilization measures only look at members >= 18) • Composite score based on pediatric practices’ rankings for the following MDC Measures, risk adjusted by MPHI: ▫ Pediatric Inpatient Visit Rate with Previous Asthma Diagnosis ▫ Pediatric ED Visit Rate with Previous Asthma Diagnosis ▫ Pediatric Preventive Overall
 Most Improved – Pediatric • Greatest change in ranking between baseline and current measurement period. See Most Improved – Adult and Family description for change in measurements period definitions.
Most Improved – Pediatric • Greatest change in ranking between baseline and current measurement period. See Most Improved – Adult and Family description for change in measurements period definitions.
 The 2015 Winning Practices!
The 2015 Winning Practices!
 Best Overall – Adult and Family Medicine Practices • Marquette Internal Medicine Pediatric Associates • Fenton Medical Center, P. C. • Jane Castillo, MD • Dhiraj Bedi, DO • Lifetime Family Care, PLLC /A Division of Michigan Healthcare Professionals PC
Best Overall – Adult and Family Medicine Practices • Marquette Internal Medicine Pediatric Associates • Fenton Medical Center, P. C. • Jane Castillo, MD • Dhiraj Bedi, DO • Lifetime Family Care, PLLC /A Division of Michigan Healthcare Professionals PC
 Winning Category: Best Overall Adult and Family Practice Name: Fenton Medical Center • WHAT MADE A DIFFERENCE (Process Change, etc. ): ▫ Improved communication among departments for care management referrals ▫ Hospital admissions and urgent care appt. notifications ▫ Staff assistance with checking Mi. PCT eligibility ▫ Improved Advanced Directives discussions ▫ Daily checking of the schedule for hospital, ED, or urgent care follow ups ▫ Resource document compiled by Clinical Leads ▫ Addition of a full time care manager has improved continuity, communication, and timely follow up ▫ Increased staff education of the Mi. PCT program and purpose • HINTS FOR OTHER PRACTICES ▫ Ensure all staff understand the value of the Mi. PCT program and their part in achieving outcomes
Winning Category: Best Overall Adult and Family Practice Name: Fenton Medical Center • WHAT MADE A DIFFERENCE (Process Change, etc. ): ▫ Improved communication among departments for care management referrals ▫ Hospital admissions and urgent care appt. notifications ▫ Staff assistance with checking Mi. PCT eligibility ▫ Improved Advanced Directives discussions ▫ Daily checking of the schedule for hospital, ED, or urgent care follow ups ▫ Resource document compiled by Clinical Leads ▫ Addition of a full time care manager has improved continuity, communication, and timely follow up ▫ Increased staff education of the Mi. PCT program and purpose • HINTS FOR OTHER PRACTICES ▫ Ensure all staff understand the value of the Mi. PCT program and their part in achieving outcomes
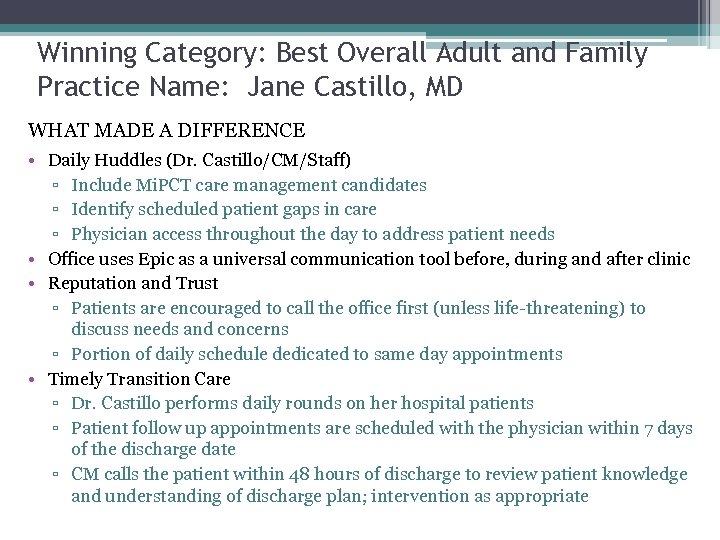 Winning Category: Best Overall Adult and Family Practice Name: Jane Castillo, MD WHAT MADE A DIFFERENCE • Daily Huddles (Dr. Castillo/CM/Staff) ▫ Include Mi. PCT care management candidates ▫ Identify scheduled patient gaps in care ▫ Physician access throughout the day to address patient needs • Office uses Epic as a universal communication tool before, during and after clinic • Reputation and Trust ▫ Patients are encouraged to call the office first (unless life-threatening) to discuss needs and concerns ▫ Portion of daily schedule dedicated to same day appointments • Timely Transition Care ▫ Dr. Castillo performs daily rounds on her hospital patients ▫ Patient follow up appointments are scheduled with the physician within 7 days of the discharge date ▫ CM calls the patient within 48 hours of discharge to review patient knowledge and understanding of discharge plan; intervention as appropriate
Winning Category: Best Overall Adult and Family Practice Name: Jane Castillo, MD WHAT MADE A DIFFERENCE • Daily Huddles (Dr. Castillo/CM/Staff) ▫ Include Mi. PCT care management candidates ▫ Identify scheduled patient gaps in care ▫ Physician access throughout the day to address patient needs • Office uses Epic as a universal communication tool before, during and after clinic • Reputation and Trust ▫ Patients are encouraged to call the office first (unless life-threatening) to discuss needs and concerns ▫ Portion of daily schedule dedicated to same day appointments • Timely Transition Care ▫ Dr. Castillo performs daily rounds on her hospital patients ▫ Patient follow up appointments are scheduled with the physician within 7 days of the discharge date ▫ CM calls the patient within 48 hours of discharge to review patient knowledge and understanding of discharge plan; intervention as appropriate
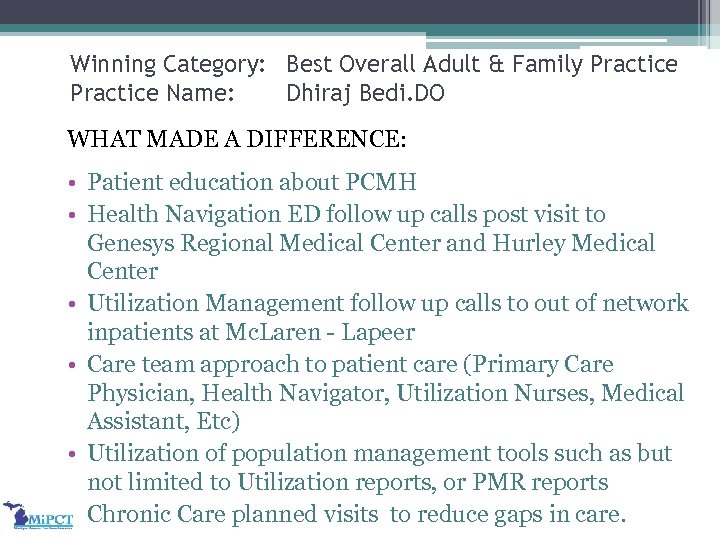 Winning Category: Best Overall Adult & Family Practice Name: Dhiraj Bedi. DO WHAT MADE A DIFFERENCE: • Patient education about PCMH • Health Navigation ED follow up calls post visit to Genesys Regional Medical Center and Hurley Medical Center • Utilization Management follow up calls to out of network inpatients at Mc. Laren - Lapeer • Care team approach to patient care (Primary Care Physician, Health Navigator, Utilization Nurses, Medical Assistant, Etc) • Utilization of population management tools such as but not limited to Utilization reports, or PMR reports • Chronic Care planned visits to reduce gaps in care.
Winning Category: Best Overall Adult & Family Practice Name: Dhiraj Bedi. DO WHAT MADE A DIFFERENCE: • Patient education about PCMH • Health Navigation ED follow up calls post visit to Genesys Regional Medical Center and Hurley Medical Center • Utilization Management follow up calls to out of network inpatients at Mc. Laren - Lapeer • Care team approach to patient care (Primary Care Physician, Health Navigator, Utilization Nurses, Medical Assistant, Etc) • Utilization of population management tools such as but not limited to Utilization reports, or PMR reports • Chronic Care planned visits to reduce gaps in care.
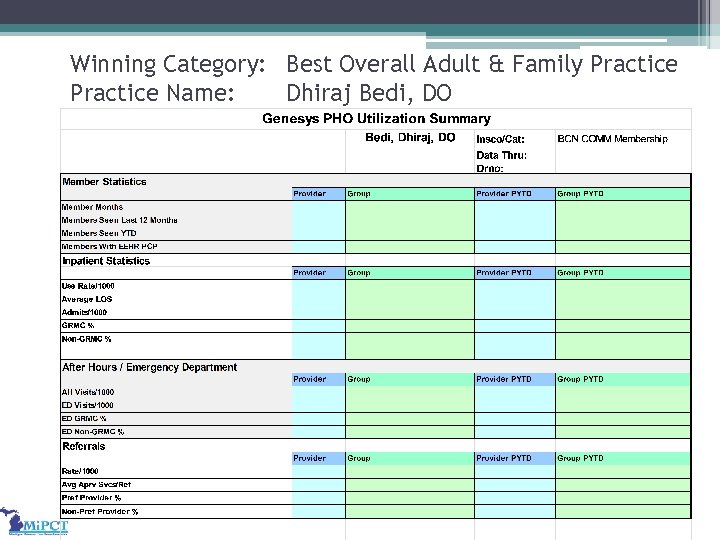 Winning Category: Best Overall Adult & Family Practice Name: Dhiraj Bedi, DO
Winning Category: Best Overall Adult & Family Practice Name: Dhiraj Bedi, DO
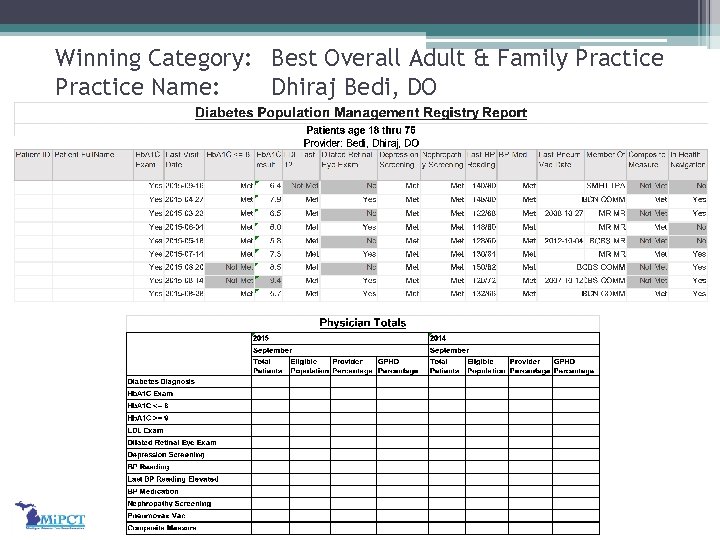 Winning Category: Best Overall Adult & Family Practice Name: Dhiraj Bedi, DO
Winning Category: Best Overall Adult & Family Practice Name: Dhiraj Bedi, DO
 Winning Category: Best Overall Adult & Family Practice Name: Dhiraj Bedi, DO • HINTS FOR OTHER PRACTICES ▫ Development of a team culture within the practice ▫ Efficient usage of technology – real time charting and documentation within the electronic medical record to avoid fragmentation. ▫ Accessibility to patients 24/7 via cell phone to ensure the patient receive the most appropriate care in the appropriate setting. ▫ Develop a network of specialists
Winning Category: Best Overall Adult & Family Practice Name: Dhiraj Bedi, DO • HINTS FOR OTHER PRACTICES ▫ Development of a team culture within the practice ▫ Efficient usage of technology – real time charting and documentation within the electronic medical record to avoid fragmentation. ▫ Accessibility to patients 24/7 via cell phone to ensure the patient receive the most appropriate care in the appropriate setting. ▫ Develop a network of specialists
 Winning Category: Best Overall- Adult and Family Practice Name: Lifetime Family Care • WHAT MADE A DIFFERENCE (Process Change, etc. ): ▫ Daily morning all-team huddle the first fifteen minutes of each day (identify who is complex, etc. ) ▫ Scheduling chronic patients on the day that the Care Manager is in the office ▫ Active use of Welcentive registry – one FT staff member enters data, identifies gaps in care for team, patients who have not been in with chronic illness, etc. ▫ Drop-down shortcuts and information codes in EHR ▫ Having a “start” physician in Dr. Keu • HINTS FOR OTHER PRACTICES ▫ Document policy and enforce it – don’t let it exist just on paper ▫ Use screening toolkit in the EHR ▫ Agreement on protocols among physicians in practice
Winning Category: Best Overall- Adult and Family Practice Name: Lifetime Family Care • WHAT MADE A DIFFERENCE (Process Change, etc. ): ▫ Daily morning all-team huddle the first fifteen minutes of each day (identify who is complex, etc. ) ▫ Scheduling chronic patients on the day that the Care Manager is in the office ▫ Active use of Welcentive registry – one FT staff member enters data, identifies gaps in care for team, patients who have not been in with chronic illness, etc. ▫ Drop-down shortcuts and information codes in EHR ▫ Having a “start” physician in Dr. Keu • HINTS FOR OTHER PRACTICES ▫ Document policy and enforce it – don’t let it exist just on paper ▫ Use screening toolkit in the EHR ▫ Agreement on protocols among physicians in practice
 Winning Category: Best Overall- Adult and Family Practice Name: Lifetime Family Care • WHAT MADE A DIFFERENCE (Process Change, etc. ): ▫ ▫ Physician lead Practice ▫ Maximize use of Technology: Wellcentive (Active Data Entry, Care Summaries, Alerts, and etc. . ) EMR (Shortcuts, Reminders, CDS, and Reports) ▫ • Communication! Monthly staff meeting Daily huddles (First 15 minutes of the day with all staff to discuss workflow, ADT, and meetings for the day. ) Impromptu daily meeting Administrative meeting Clinical Management meeting Patient Focus Practice: Patient surveys reviewed monthly and changes made accordingly. Monthly staff training on building patient and staff relationships. Emphasize efforts to help patients feel valued. HINTS FOR OTHER PRACTICES ▫ Get everyone involved in all office process. ▫ Develop policies as a team and enforce it-don’t let it exist just on paper.
Winning Category: Best Overall- Adult and Family Practice Name: Lifetime Family Care • WHAT MADE A DIFFERENCE (Process Change, etc. ): ▫ ▫ Physician lead Practice ▫ Maximize use of Technology: Wellcentive (Active Data Entry, Care Summaries, Alerts, and etc. . ) EMR (Shortcuts, Reminders, CDS, and Reports) ▫ • Communication! Monthly staff meeting Daily huddles (First 15 minutes of the day with all staff to discuss workflow, ADT, and meetings for the day. ) Impromptu daily meeting Administrative meeting Clinical Management meeting Patient Focus Practice: Patient surveys reviewed monthly and changes made accordingly. Monthly staff training on building patient and staff relationships. Emphasize efforts to help patients feel valued. HINTS FOR OTHER PRACTICES ▫ Get everyone involved in all office process. ▫ Develop policies as a team and enforce it-don’t let it exist just on paper.
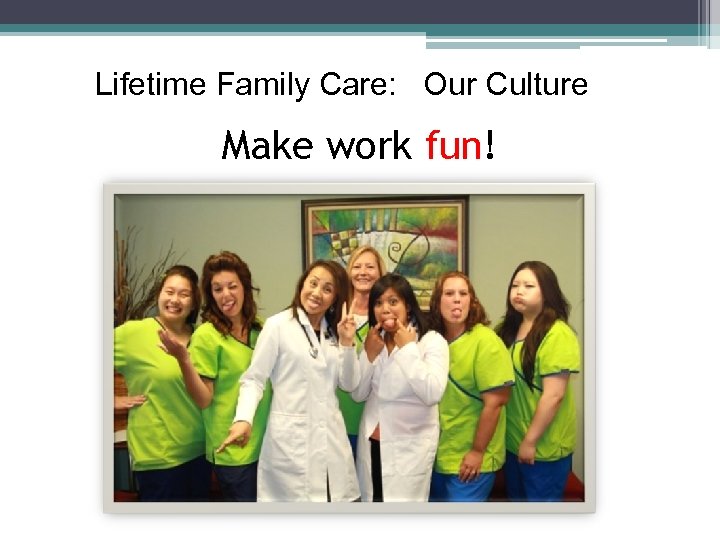 Lifetime Family Care: Our Culture Make work fun!
Lifetime Family Care: Our Culture Make work fun!
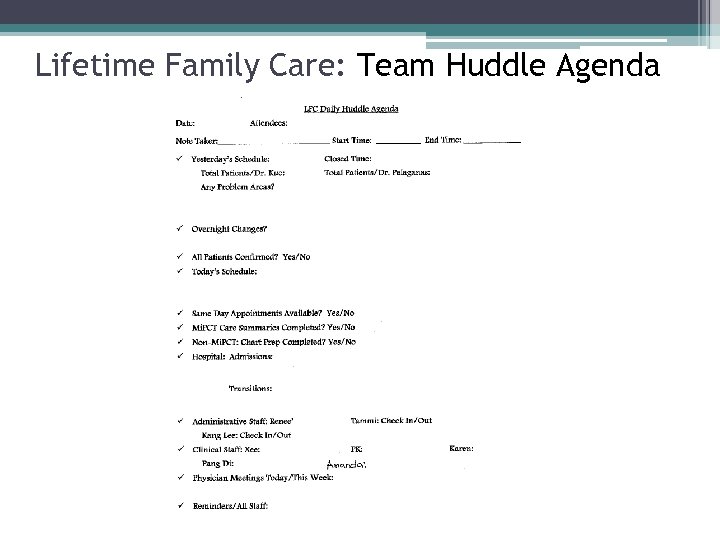 Lifetime Family Care: Team Huddle Agenda
Lifetime Family Care: Team Huddle Agenda
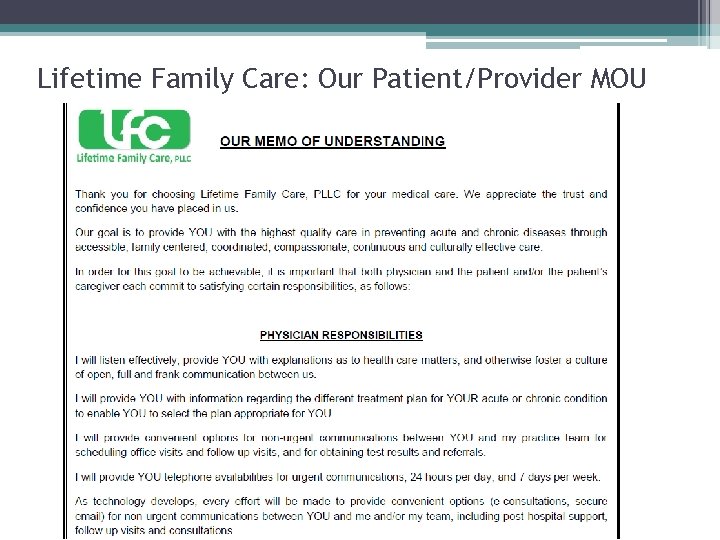 Lifetime Family Care: Our Patient/Provider MOU
Lifetime Family Care: Our Patient/Provider MOU
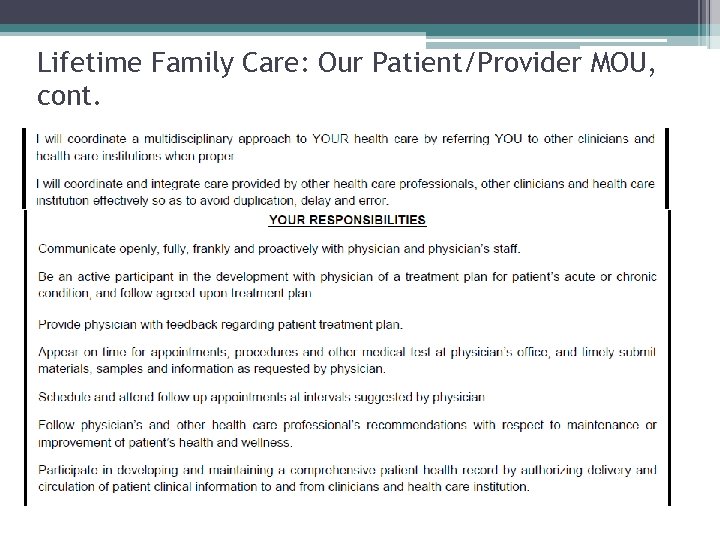 Lifetime Family Care: Our Patient/Provider MOU, cont.
Lifetime Family Care: Our Patient/Provider MOU, cont.
 Most Improved – Adult and Family Medicine • East Ann Arbor Adult Medicine and Pediatrics Clinic • Rivertown Internal Medicine and Pediatrics • Campustowne Family Medicine • Grand Rapids Internal Medicine and Pediatrics • Alpine Internal Medicine and Pediatrics
Most Improved – Adult and Family Medicine • East Ann Arbor Adult Medicine and Pediatrics Clinic • Rivertown Internal Medicine and Pediatrics • Campustowne Family Medicine • Grand Rapids Internal Medicine and Pediatrics • Alpine Internal Medicine and Pediatrics
 Winning Category: Most Improved – Adult and Family Practice Name: East Ann Arbor Adult Medicine and Pediatrics Clnic • WHAT MADE A DIFFERENCE: ▫ A Multidisciplinary Workgroup Approach The Chronic Care Team. Membership consists of Clinic Physicians, Navigator Team (Care Managers), Pharm. D (co-lead), Registered Dietitian, Social Worker, Nursing, Practice Management, Panel Manager, Medical Assistants, and Clerical staff)
Winning Category: Most Improved – Adult and Family Practice Name: East Ann Arbor Adult Medicine and Pediatrics Clnic • WHAT MADE A DIFFERENCE: ▫ A Multidisciplinary Workgroup Approach The Chronic Care Team. Membership consists of Clinic Physicians, Navigator Team (Care Managers), Pharm. D (co-lead), Registered Dietitian, Social Worker, Nursing, Practice Management, Panel Manager, Medical Assistants, and Clerical staff)
 Winning Category: Most Improved – Adult and Family Practice Name: East Ann Arbor Adult Medicine and Pediatrics Clnic, cont. WHAT MADE A DIFFERENCE – Chronic Care Team The team huddles for 15 minutes each Thursday to: Review Quality Management Programs (QMP) reports Set goals and review progress Divide the responsibility Medical Assistants play a significant role to assure Best Practice Alerts are ordered/pended for their providers, foot exams completed, etc.
Winning Category: Most Improved – Adult and Family Practice Name: East Ann Arbor Adult Medicine and Pediatrics Clnic, cont. WHAT MADE A DIFFERENCE – Chronic Care Team The team huddles for 15 minutes each Thursday to: Review Quality Management Programs (QMP) reports Set goals and review progress Divide the responsibility Medical Assistants play a significant role to assure Best Practice Alerts are ordered/pended for their providers, foot exams completed, etc.
 Winning Category: Most Improved – Adult and Family Practice Name: East Ann Arbor Adult Medicine and Pediatrics Clnic, cont. The Care Navigation Team • • • Jennifer Smith, NP Deborah Dahlgren, RN Carol Carnell, MAS Panel Manager Navigators Jennifer and Deb • Follow up on all the inpatient discharges • Manage patients with multiple complex diagnoses Coordination – The team meets weekly to focus on areas to accomplish. Lists are worked daily.
Winning Category: Most Improved – Adult and Family Practice Name: East Ann Arbor Adult Medicine and Pediatrics Clnic, cont. The Care Navigation Team • • • Jennifer Smith, NP Deborah Dahlgren, RN Carol Carnell, MAS Panel Manager Navigators Jennifer and Deb • Follow up on all the inpatient discharges • Manage patients with multiple complex diagnoses Coordination – The team meets weekly to focus on areas to accomplish. Lists are worked daily.
 Winning Category: Most Improved – Adult and Family Practice Name: East Ann Arbor Adult Medicine and Pediatrics Clnic, cont. HEALTH CENTER LPN TEAM Have key roles in assuring plans are in place for asthma and controlled substances. HEALTH CENTER RN TEAM Follow up patients recently discharged from Emergency and Urgent Care settings.
Winning Category: Most Improved – Adult and Family Practice Name: East Ann Arbor Adult Medicine and Pediatrics Clnic, cont. HEALTH CENTER LPN TEAM Have key roles in assuring plans are in place for asthma and controlled substances. HEALTH CENTER RN TEAM Follow up patients recently discharged from Emergency and Urgent Care settings.
 Winning Category: Most Improved – Adult and Family Practice Name: East Ann Arbor Adult Medicine and Pediatrics Clnic, cont. Adult Medicine & Pediatrics Clinic The Medicine Pediatric physicians (including 14 residents) partner with medical assistants, the clinic LPN, Patient Service Assistants, RNs and the Navigator Team to assure the best care for their patients.
Winning Category: Most Improved – Adult and Family Practice Name: East Ann Arbor Adult Medicine and Pediatrics Clnic, cont. Adult Medicine & Pediatrics Clinic The Medicine Pediatric physicians (including 14 residents) partner with medical assistants, the clinic LPN, Patient Service Assistants, RNs and the Navigator Team to assure the best care for their patients.
 Winning Category: Most Improved – Adult and Family Practice Name: East Ann Arbor Adult Medicine and Pediatrics Clnic, cont. HINTS FOR OTHER PRACTICES Flexibility is key to working with and lexibility meeting the needs of the team Collective Approach all clinic staff are Collective Approach responsible for meeting goals toward excellent patient care
Winning Category: Most Improved – Adult and Family Practice Name: East Ann Arbor Adult Medicine and Pediatrics Clnic, cont. HINTS FOR OTHER PRACTICES Flexibility is key to working with and lexibility meeting the needs of the team Collective Approach all clinic staff are Collective Approach responsible for meeting goals toward excellent patient care
 Diabetes Overall • Family Tree Medical Associates • St Johns Professional Associates • SMG De. Witt • Grand Blanc Family Medicine • Jane Castillo, MD
Diabetes Overall • Family Tree Medical Associates • St Johns Professional Associates • SMG De. Witt • Grand Blanc Family Medicine • Jane Castillo, MD
 Winning Category: Diabetes Overall Practice Name: Jane Castillo, MD WHAT MADE A DIFFERENCE • Dedicated staff member manages registry to focus on obtaining test results and closing gaps in care • Dr. Castillo calls patients with test results – even if normal • Focus is on patient self-management of blood sugar levels ▫ Dietary and exercise management ▫ Education and reinforcement on oral medication/insulin administration options
Winning Category: Diabetes Overall Practice Name: Jane Castillo, MD WHAT MADE A DIFFERENCE • Dedicated staff member manages registry to focus on obtaining test results and closing gaps in care • Dr. Castillo calls patients with test results – even if normal • Focus is on patient self-management of blood sugar levels ▫ Dietary and exercise management ▫ Education and reinforcement on oral medication/insulin administration options
 Diabetes Metric Improvement • Cherry Street Health Center • SMG Holt • St Johns Professional Associates • Premier Family Physicians • New Day Family Medicine
Diabetes Metric Improvement • Cherry Street Health Center • SMG Holt • St Johns Professional Associates • Premier Family Physicians • New Day Family Medicine
 Winning Category: Most Improved-Diabetes Practice Name: New Day • WHAT MADE A DIFFERENCE: ▫ A Flexible and “Eager to Adopt New Things” Culture -- The team takes care to make sure that everyone has “bought in” to a proposed change ▫ “Whole Practice Team” (coach, CM, physician, front desk lead) meets twice a month to go over their performance on measures, discuss gaps in care, etc. ) and uses IHP online registry ▫ Sustaining the Gains of the IHP Diabetes Collaboratives – Integrated successes into the practice workflow as expectations, and have spread the approach to asthma, hypertension ▫ Diabetic Eye Exam Excellence– Practice initiates and faxes the referral to the ophthalmologist. Two weeks later they follow up with the ophthalmologist and follow up if the patient has not gone using a referral tracking form they developed ▫ In-Office Diabetic AIC Testing – The practice has its own machine and can give the patient instantaneous testing and results
Winning Category: Most Improved-Diabetes Practice Name: New Day • WHAT MADE A DIFFERENCE: ▫ A Flexible and “Eager to Adopt New Things” Culture -- The team takes care to make sure that everyone has “bought in” to a proposed change ▫ “Whole Practice Team” (coach, CM, physician, front desk lead) meets twice a month to go over their performance on measures, discuss gaps in care, etc. ) and uses IHP online registry ▫ Sustaining the Gains of the IHP Diabetes Collaboratives – Integrated successes into the practice workflow as expectations, and have spread the approach to asthma, hypertension ▫ Diabetic Eye Exam Excellence– Practice initiates and faxes the referral to the ophthalmologist. Two weeks later they follow up with the ophthalmologist and follow up if the patient has not gone using a referral tracking form they developed ▫ In-Office Diabetic AIC Testing – The practice has its own machine and can give the patient instantaneous testing and results
 Winning Category: Most Improved-Diabetes Practice Name: New Day, cont. • HINTS FOR OTHER PRACTICES ▫ Everyone must be vested in a change (if the front desk, MA, etc. is not “bought in”, the change won’t work) ▫ Develop trust in your team –everyone is busy and needs a team that they can trust ▫ Incorporate prompts as cues – for example, when a chronic disease patient visits, the appointment system labels as a chronic disease visit, prompting the team to see if they need tests, etc.
Winning Category: Most Improved-Diabetes Practice Name: New Day, cont. • HINTS FOR OTHER PRACTICES ▫ Everyone must be vested in a change (if the front desk, MA, etc. is not “bought in”, the change won’t work) ▫ Develop trust in your team –everyone is busy and needs a team that they can trust ▫ Incorporate prompts as cues – for example, when a chronic disease patient visits, the appointment system labels as a chronic disease visit, prompting the team to see if they need tests, etc.
 Best Overall – Pediatric Practices • Pediatric Specialists of Bloomfield Hills PC • Pediatric Consultants of Troy PC • Joseph B. Luna, M. D. , P. C. • Cereal City Pediatrics PC • Moazami Pediatrics
Best Overall – Pediatric Practices • Pediatric Specialists of Bloomfield Hills PC • Pediatric Consultants of Troy PC • Joseph B. Luna, M. D. , P. C. • Cereal City Pediatrics PC • Moazami Pediatrics
 Winning Category: Best Overall Pediatric Practice Name: Pediatric Consultants of Troy WHAT MADE A DIFFERENCE • Access – Our Patients Know We Will Be Here for Them ▫ We are open SEVEN DAYS A WEEK (including Sat 8 -11 and Sunday 5 -8) ▫ Phones are personally answered (we don’t use an automated attendant), giving parents of asthmatics confidence about reaching the practice at times of need • Preparation and Scheduling ▫ We prepare charts the day before the visit ▫ Asthmatics get an initial 45 minute visit and we insert an asthma packet (with an asthma navigator and history, etc. ) with every pediatric asthmatic visit ▫ We use a Google calendar for dietician and social worker appointments ▫ Patients can’t get fills on their medications if they have not been seen in six months
Winning Category: Best Overall Pediatric Practice Name: Pediatric Consultants of Troy WHAT MADE A DIFFERENCE • Access – Our Patients Know We Will Be Here for Them ▫ We are open SEVEN DAYS A WEEK (including Sat 8 -11 and Sunday 5 -8) ▫ Phones are personally answered (we don’t use an automated attendant), giving parents of asthmatics confidence about reaching the practice at times of need • Preparation and Scheduling ▫ We prepare charts the day before the visit ▫ Asthmatics get an initial 45 minute visit and we insert an asthma packet (with an asthma navigator and history, etc. ) with every pediatric asthmatic visit ▫ We use a Google calendar for dietician and social worker appointments ▫ Patients can’t get fills on their medications if they have not been seen in six months
 Winning Category: Best Overall Pediatric Practice Name: Pediatric Consultants of Troy WHAT MADE A DIFFERENCE • Tracking Process – Our Checklist and our Tracking Book ▫ Our Checklist – The practice team designed a patient checklist that goes to the physician to make sure everything is done (self-management goal, etc. ), and is returned to the front staff for follow-up and gap closure if needed; also entered in Wellcentive ▫ Tracking Book – Contains things that require follow-up (e. g. , call to a no-show patient for rescheduling, etc. ) ▫ If there is an ER visit, the patient gets a letter with information about how to reach the practice and their office hours ▫ Good test tracking; we MCIR every patient who comes to the office (not just at the physical but at all appointments) HINTS FOR OTHERS • Take tracking seriously • Consider offering weekend hours – it makes a difference for our patients
Winning Category: Best Overall Pediatric Practice Name: Pediatric Consultants of Troy WHAT MADE A DIFFERENCE • Tracking Process – Our Checklist and our Tracking Book ▫ Our Checklist – The practice team designed a patient checklist that goes to the physician to make sure everything is done (self-management goal, etc. ), and is returned to the front staff for follow-up and gap closure if needed; also entered in Wellcentive ▫ Tracking Book – Contains things that require follow-up (e. g. , call to a no-show patient for rescheduling, etc. ) ▫ If there is an ER visit, the patient gets a letter with information about how to reach the practice and their office hours ▫ Good test tracking; we MCIR every patient who comes to the office (not just at the physical but at all appointments) HINTS FOR OTHERS • Take tracking seriously • Consider offering weekend hours – it makes a difference for our patients
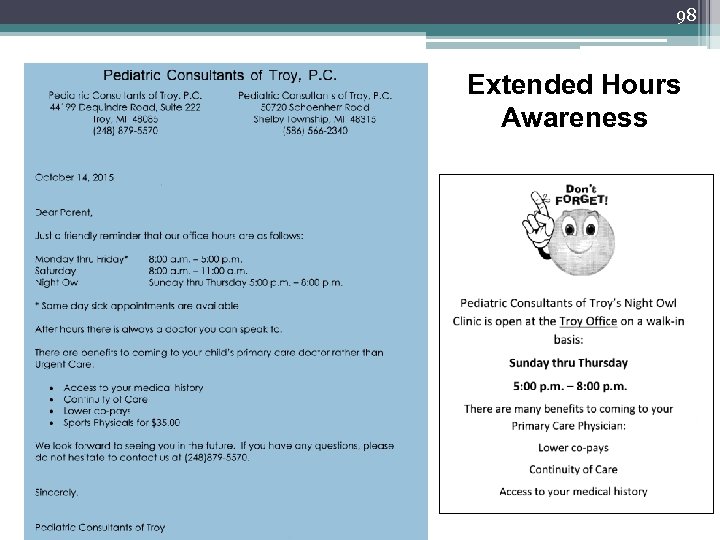 98 Extended Hours Awareness
98 Extended Hours Awareness
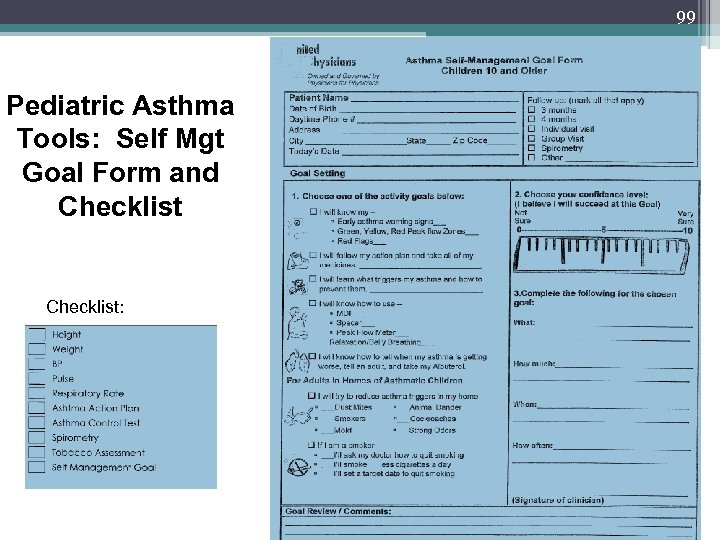 99 Pediatric Asthma Tools: Self Mgt Goal Form and Checklist:
99 Pediatric Asthma Tools: Self Mgt Goal Form and Checklist:
 100 Pediatric Asthma Tools: Asthma Navigator
100 Pediatric Asthma Tools: Asthma Navigator
 Winning Category: Best Practice Pediatrics Practice Name: Dr. Luna • WHAT MADE A DIFFERENCE: Asthma Patients ▫ Efficient at scheduling f/u appts before patient leaves ▫ Use of Wellcentive to check inpatient & ER admissions ▫ Good relationship with hospital which calls & makes f/u appt for pt before being discharged ▫ With asthma flare ups, will always have patient come back for recheck in 2 -3 days-1 week Preventive Care ▫ Efficient at scheduling ▫ Multiple calls to reschedule for no shows ▫ Send letter if unable to reach • HINTS FOR OTHER PRACTICES ▫ Staff has personal knowledge of families. They know which ones need extra reminders, preferences, likes/dislikes etc.
Winning Category: Best Practice Pediatrics Practice Name: Dr. Luna • WHAT MADE A DIFFERENCE: Asthma Patients ▫ Efficient at scheduling f/u appts before patient leaves ▫ Use of Wellcentive to check inpatient & ER admissions ▫ Good relationship with hospital which calls & makes f/u appt for pt before being discharged ▫ With asthma flare ups, will always have patient come back for recheck in 2 -3 days-1 week Preventive Care ▫ Efficient at scheduling ▫ Multiple calls to reschedule for no shows ▫ Send letter if unable to reach • HINTS FOR OTHER PRACTICES ▫ Staff has personal knowledge of families. They know which ones need extra reminders, preferences, likes/dislikes etc.
 Winning Category: Best Overall Pediatric Practice Names: Cereal City Pediatric and Moazami Pediatric WHAT MADE A DIFFERENCE • A Focus on Training ▫ The entire office (including front office) participated in in-service with an asthma educator; in-services from an Asthma Allergy Center on injections ▫ Physicians conducted an in service with the nursing staff on identifying respiratory distress. Now, the content of the in service has been included as part of the new hire training process. • Useful Standard Tools and Processes ▫ In 2012, a cough protocol/algorithm for the front desk and triage was created to screen phone calls and prioritize appointments. The office also purchased a spirometer and had the supplier conduct an in service on proper use. ▫ Annual well visits with an asthma action plan is required for all medication refills and notes for medication usage at school for patients with asthma. ▫ Medication follow-up appointment is required for patients w/frequent refills. ▫ Asthma patients are tracked and flagged in PCC and Gaps in Care reports and the office has a designated Asthma Champion.
Winning Category: Best Overall Pediatric Practice Names: Cereal City Pediatric and Moazami Pediatric WHAT MADE A DIFFERENCE • A Focus on Training ▫ The entire office (including front office) participated in in-service with an asthma educator; in-services from an Asthma Allergy Center on injections ▫ Physicians conducted an in service with the nursing staff on identifying respiratory distress. Now, the content of the in service has been included as part of the new hire training process. • Useful Standard Tools and Processes ▫ In 2012, a cough protocol/algorithm for the front desk and triage was created to screen phone calls and prioritize appointments. The office also purchased a spirometer and had the supplier conduct an in service on proper use. ▫ Annual well visits with an asthma action plan is required for all medication refills and notes for medication usage at school for patients with asthma. ▫ Medication follow-up appointment is required for patients w/frequent refills. ▫ Asthma patients are tracked and flagged in PCC and Gaps in Care reports and the office has a designated Asthma Champion.
 Winning Category: Best Overall Pediatric Practice Names: Cereal City Pediatric and Moazami Pediatric WHAT MADE A DIFFERENCE, cont. ▫ Priority calls are placed to patients with asthma when flu vaccine arrives, along with other high risk patients before reminder calls for the healthy. ▫ Refills are monitored for compliance. • Attention to Patient Education ▫ Patient Asthma Education folders are given to patients with a new asthma diagnosis. ▫ Individual care management education sessions are conducted to teach patients how to use a spacer, inhaler, or nebulizer. HINTS FOR OTHER PRACTICES ▫ Take time for training and incorporate processes and useful tools as aids to guide your work ▫ Watch for patterns (which patients are requesting frequent refills, are there repeating situations that cause rework, etc. ) and act on them
Winning Category: Best Overall Pediatric Practice Names: Cereal City Pediatric and Moazami Pediatric WHAT MADE A DIFFERENCE, cont. ▫ Priority calls are placed to patients with asthma when flu vaccine arrives, along with other high risk patients before reminder calls for the healthy. ▫ Refills are monitored for compliance. • Attention to Patient Education ▫ Patient Asthma Education folders are given to patients with a new asthma diagnosis. ▫ Individual care management education sessions are conducted to teach patients how to use a spacer, inhaler, or nebulizer. HINTS FOR OTHER PRACTICES ▫ Take time for training and incorporate processes and useful tools as aids to guide your work ▫ Watch for patterns (which patients are requesting frequent refills, are there repeating situations that cause rework, etc. ) and act on them
 Most Improved – Pediatric • Pediatric Consultants of Troy PC • CHC Fort Gratiot • Forest Hills Pediatric Associates PC • Briarwood Center For Women Children and Young Adults • Pediatric Care of Lansing
Most Improved – Pediatric • Pediatric Consultants of Troy PC • CHC Fort Gratiot • Forest Hills Pediatric Associates PC • Briarwood Center For Women Children and Young Adults • Pediatric Care of Lansing
 Winning Category: Most Improved – Pediatric Practice Name: Forest Hills Pediatrics • WHAT MADE A DIFFERENCE (Process Change, etc. ): ▫ Care Plan created with built in triggers for recall ▫ Phone calls within two days of all ED visits ▫ Recheck with educator after every asthma flare • HINTS FOR OTHER PRACTICES ▫ Never assume patients remember what you told them last time! Keep educating and empowering them to manage their own medications.
Winning Category: Most Improved – Pediatric Practice Name: Forest Hills Pediatrics • WHAT MADE A DIFFERENCE (Process Change, etc. ): ▫ Care Plan created with built in triggers for recall ▫ Phone calls within two days of all ED visits ▫ Recheck with educator after every asthma flare • HINTS FOR OTHER PRACTICES ▫ Never assume patients remember what you told them last time! Keep educating and empowering them to manage their own medications.
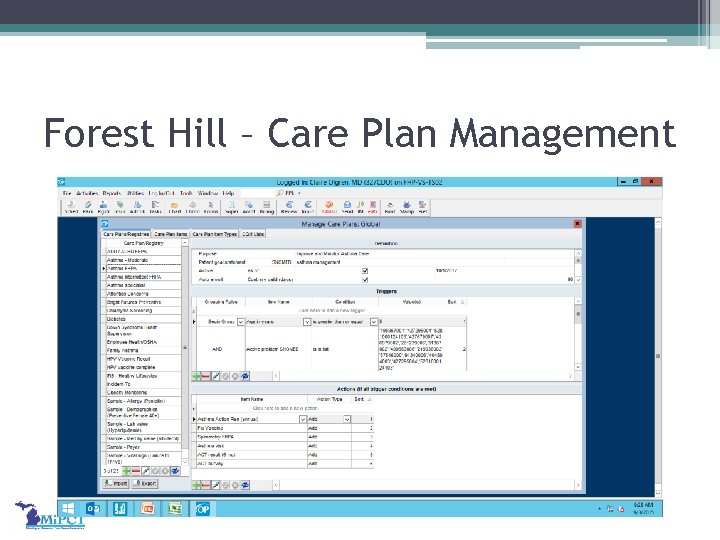 Forest Hill – Care Plan Management
Forest Hill – Care Plan Management
 Winning Category: Most Improved-Pediatric Practice Name: CHC Fort Gratiot • WHAT MADE A DIFFERENCE: ▫ Dedicated process and staff focus on closing gaps in care Office staff diligently follow up with parents by phone and via letters. Each visit (regardless of reason for visit) is used as an opportunity to close gaps in care ▫ ED calls are made to patients who visit the ED to remind them of extended access hours and arrange a follow-up visit, if appropriate ▫ Using data to identify opportunities for improvement Data analysis indicated that the most frequent driver of ED visits was constipation. Discussion with parents found that they didn’t know what to do when their child was in pain, or how to prevent constipation The practice offered a group visit that included how to prevent constipation (e. g. , with a high fiber diet that is appealing to kids), and offered information on what do if constipation reoccurs Care Managers and physicians identified patients who could benefit The group visit was held at a convenient time for parents (from 5: 30 to 7: 30) and was a hit! Now, group visits are conducted for asthma, nutrition, and ADHD
Winning Category: Most Improved-Pediatric Practice Name: CHC Fort Gratiot • WHAT MADE A DIFFERENCE: ▫ Dedicated process and staff focus on closing gaps in care Office staff diligently follow up with parents by phone and via letters. Each visit (regardless of reason for visit) is used as an opportunity to close gaps in care ▫ ED calls are made to patients who visit the ED to remind them of extended access hours and arrange a follow-up visit, if appropriate ▫ Using data to identify opportunities for improvement Data analysis indicated that the most frequent driver of ED visits was constipation. Discussion with parents found that they didn’t know what to do when their child was in pain, or how to prevent constipation The practice offered a group visit that included how to prevent constipation (e. g. , with a high fiber diet that is appealing to kids), and offered information on what do if constipation reoccurs Care Managers and physicians identified patients who could benefit The group visit was held at a convenient time for parents (from 5: 30 to 7: 30) and was a hit! Now, group visits are conducted for asthma, nutrition, and ADHD
 Winning Category: Most Improved-Pediatric Practice Name: CHC Fort Gratiot • WHAT MADE A DIFFERENCE: ▫ The Care Managers are centrally located but huddle once a week to discuss cases ▫ One Care Manager is a social worker and has good relationships with community mental health agencies and behavioral health resources ▫ Community resources are monitored and published on their website and in a hardcopy binder. All employees are trained on community resources and there are good relationships with local agencies. The practice helps the agencies by documenting activity for funders so that they can provide it to their funders as evidence of use • HINTS FOR OTHER PRACTICES ▫ The whole team must know they play important roles and that others depend on them ▫ Connect your offices with community resources ▫ Define and document processes. Create standard work and expectations. ▫ Use your data to find out what your issues are; Add a midlevel or increase your after-hours schedule if needed.
Winning Category: Most Improved-Pediatric Practice Name: CHC Fort Gratiot • WHAT MADE A DIFFERENCE: ▫ The Care Managers are centrally located but huddle once a week to discuss cases ▫ One Care Manager is a social worker and has good relationships with community mental health agencies and behavioral health resources ▫ Community resources are monitored and published on their website and in a hardcopy binder. All employees are trained on community resources and there are good relationships with local agencies. The practice helps the agencies by documenting activity for funders so that they can provide it to their funders as evidence of use • HINTS FOR OTHER PRACTICES ▫ The whole team must know they play important roles and that others depend on them ▫ Connect your offices with community resources ▫ Define and document processes. Create standard work and expectations. ▫ Use your data to find out what your issues are; Add a midlevel or increase your after-hours schedule if needed.
 Winning Category: Most Improved-Pediatric Practice Name: The Briarwood Center for Women, Children and Young Adults • WHAT MADE A DIFFERENCE: ▫ Support and direction from higher level leadership in Ambulatory Care ▫ Establishment of a multidisciplinary Medical Home Committee ▫ Set clear goals and objectives ▫ Obtain and understand reports and data ▫ Create standard workflows • HINTS FOR OTHER PRACTICES ▫ ▫ ▫ Invite the right people to the table Don’t wait for others to provide you with the answers Meet regularly, keep good notes and follow up Share your project with as many people as you can Celebrate improvements as you go
Winning Category: Most Improved-Pediatric Practice Name: The Briarwood Center for Women, Children and Young Adults • WHAT MADE A DIFFERENCE: ▫ Support and direction from higher level leadership in Ambulatory Care ▫ Establishment of a multidisciplinary Medical Home Committee ▫ Set clear goals and objectives ▫ Obtain and understand reports and data ▫ Create standard workflows • HINTS FOR OTHER PRACTICES ▫ ▫ ▫ Invite the right people to the table Don’t wait for others to provide you with the answers Meet regularly, keep good notes and follow up Share your project with as many people as you can Celebrate improvements as you go
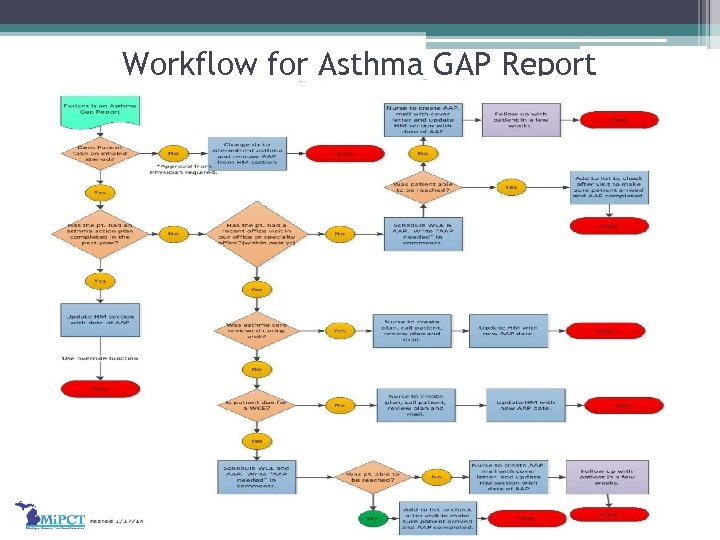 Workflow for Asthma GAP Report
Workflow for Asthma GAP Report
 Winning Category: Most Improved Pediatric Practice Name: Pediatric Care of Lansing • WHAT MADE A DIFFERENCE (Process Change, etc. ): ▫ Educating patients on disease management ▫ Improving access to the PCMH through extended hours • HINTS FOR OTHER PRACTICES ▫ Use your Care Manager!
Winning Category: Most Improved Pediatric Practice Name: Pediatric Care of Lansing • WHAT MADE A DIFFERENCE (Process Change, etc. ): ▫ Educating patients on disease management ▫ Improving access to the PCMH through extended hours • HINTS FOR OTHER PRACTICES ▫ Use your Care Manager!
 A Round of Applause for ALL Our 2015 Winners …. And Your Practice Could be Recognized in 2016!
A Round of Applause for ALL Our 2015 Winners …. And Your Practice Could be Recognized in 2016!
 113 THANK YOU FOR ATTENDING THE SUMMIT! • Please complete your online Summit Evaluation by November 12 at: http: //mipct. org/2015 -summit-prework-webinars/2015 -mipct-regional-annualsummit-evaluation-links/ (the link will also be emailed to attendees after the summit) • Care Managers, remember to be in your designated rooms by 1 pm to start the afternoon session! • All morning summit material is posted at mipctdemo. org • If you haven’t visited the Tiger Team chart to identify your PO’s current status, please do so! • If you are not staying for the afternoon sessions, please drop your name badges in the box at the exit of this room (or at the registration table). • Watch for a “Best of the Best” Compendium of the Best Practice Slides from All Three Mi. PCT 2015 Summits!
113 THANK YOU FOR ATTENDING THE SUMMIT! • Please complete your online Summit Evaluation by November 12 at: http: //mipct. org/2015 -summit-prework-webinars/2015 -mipct-regional-annualsummit-evaluation-links/ (the link will also be emailed to attendees after the summit) • Care Managers, remember to be in your designated rooms by 1 pm to start the afternoon session! • All morning summit material is posted at mipctdemo. org • If you haven’t visited the Tiger Team chart to identify your PO’s current status, please do so! • If you are not staying for the afternoon sessions, please drop your name badges in the box at the exit of this room (or at the registration table). • Watch for a “Best of the Best” Compendium of the Best Practice Slides from All Three Mi. PCT 2015 Summits!


