1931dd484ea72dfa9df35a375f37b90f.ppt
- Количество слайдов: 53
 The Medical Practitioner’s Role in Facilitating the Recovery Process “It’s not ALL about the medicine. ” James Finch, MD, FASAM Director of Physician Education: Governor’s Institute on Alcohol and Substance Abuse Changes By Choice Durham, NC
The Medical Practitioner’s Role in Facilitating the Recovery Process “It’s not ALL about the medicine. ” James Finch, MD, FASAM Director of Physician Education: Governor’s Institute on Alcohol and Substance Abuse Changes By Choice Durham, NC
 …Full Disclosure: No conflicts of interest. However… Arrested for public intoxication: 1967 “…but officer, I only had two beers…” Arrested for “curfew violation”: 1972 “oooh man…but I just got out of the concert…” Leash-law violation: 2008: “…you’re giving me a ticket for what…? !”
…Full Disclosure: No conflicts of interest. However… Arrested for public intoxication: 1967 “…but officer, I only had two beers…” Arrested for “curfew violation”: 1972 “oooh man…but I just got out of the concert…” Leash-law violation: 2008: “…you’re giving me a ticket for what…? !”
 Workshop Objectives n n Define what are reasonable counseling expectations of the clinician during brief clinical encounters, such as the typical “med management visit”. Outline common elements of the addiction recovery process that can be facilitated by attention from the clinician. Define basic elements of Cognitive Behavioral and Motivational Interventions as they apply to these time-limited but longitudinal encounters. Outline brief clinical strategies that apply to helping the patient cope with dysphoric mood states and interpersonal stressors. Premise: No clinical encounter is too brief for a little counseling!
Workshop Objectives n n Define what are reasonable counseling expectations of the clinician during brief clinical encounters, such as the typical “med management visit”. Outline common elements of the addiction recovery process that can be facilitated by attention from the clinician. Define basic elements of Cognitive Behavioral and Motivational Interventions as they apply to these time-limited but longitudinal encounters. Outline brief clinical strategies that apply to helping the patient cope with dysphoric mood states and interpersonal stressors. Premise: No clinical encounter is too brief for a little counseling!
 Pivotal Developments in the Approach to Substance Abuse Treatment Potential for effective interventions improved by three major developments in the field: • • • Public Health “Continuum” Model Evidence Based Behavioral Therapies Neurophysiologic Research and Pharmacologic Adjuncts: Medication Assisted Therapy (MAT)
Pivotal Developments in the Approach to Substance Abuse Treatment Potential for effective interventions improved by three major developments in the field: • • • Public Health “Continuum” Model Evidence Based Behavioral Therapies Neurophysiologic Research and Pharmacologic Adjuncts: Medication Assisted Therapy (MAT)
 Presentation objectives: Provide context for medical practitioner’s role/s: Define public health paradigm of addiction Describe addictive disease progression Outline elements of treatment: med and non-med Propose basic counseling tools for the brief medical encounter: “CBT (Cognitive Behavioral Therapy) Lite” “psychotherapy delivered in small doses over time” Premise: No clinical encounter is too brief for a little counseling!
Presentation objectives: Provide context for medical practitioner’s role/s: Define public health paradigm of addiction Describe addictive disease progression Outline elements of treatment: med and non-med Propose basic counseling tools for the brief medical encounter: “CBT (Cognitive Behavioral Therapy) Lite” “psychotherapy delivered in small doses over time” Premise: No clinical encounter is too brief for a little counseling!
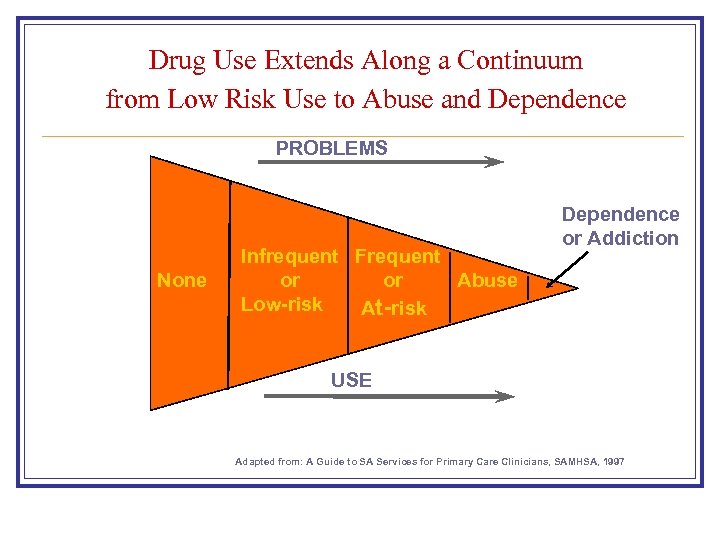 Drug Use Extends Along a Continuum from Low Risk Use to Abuse and Dependence PROBLEMS None Infrequent Frequent or or Abuse Low-risk At-risk Dependence or Addiction USE Adapted from: A Guide to SA Services for Primary Care Clinicians, SAMHSA, 1997
Drug Use Extends Along a Continuum from Low Risk Use to Abuse and Dependence PROBLEMS None Infrequent Frequent or or Abuse Low-risk At-risk Dependence or Addiction USE Adapted from: A Guide to SA Services for Primary Care Clinicians, SAMHSA, 1997
 Progression to Abuse and Dependence n Increased frequency of use and time involved with the drug n Evolving pattern of recurrent problems in multiple domains: Emotional/Interpersonal/Social Physical/Occupational/Legal n Continued use of the drug in spite of these problems n Increasing guilt/shame Increasing difficulty hiding, ignoring or denying problems n
Progression to Abuse and Dependence n Increased frequency of use and time involved with the drug n Evolving pattern of recurrent problems in multiple domains: Emotional/Interpersonal/Social Physical/Occupational/Legal n Continued use of the drug in spite of these problems n Increasing guilt/shame Increasing difficulty hiding, ignoring or denying problems n
 Neuro-adaptation: Progression to Dependence n Neuro-adaptation in reward (“survival”) system with increasing reliance on the drug to maintain hedonic tone. n Deterioration in pre-frontal cortical control system and transition from volitional control to compulsive, out of control use. n Transition from pleasurable use to maintenance use and need to avoid physical withdrawal.
Neuro-adaptation: Progression to Dependence n Neuro-adaptation in reward (“survival”) system with increasing reliance on the drug to maintain hedonic tone. n Deterioration in pre-frontal cortical control system and transition from volitional control to compulsive, out of control use. n Transition from pleasurable use to maintenance use and need to avoid physical withdrawal.
 Treatments Needed to Reverse Process: Bio-psycho-social-spiritual Interventions n Time abstinent: re-set neuro-adaptation/restore cortical function n Mitigate craving: MAT and behavioral interventions n Address reasons for use: How to respond to and avoid triggers and cues n Alternate means of coping with craving and dysphoria n Decrease social risks: situations/settings/associates
Treatments Needed to Reverse Process: Bio-psycho-social-spiritual Interventions n Time abstinent: re-set neuro-adaptation/restore cortical function n Mitigate craving: MAT and behavioral interventions n Address reasons for use: How to respond to and avoid triggers and cues n Alternate means of coping with craving and dysphoria n Decrease social risks: situations/settings/associates
 Treatment Elements: continued n Increase access and decrease resistence to non-using alternatives n Increase social support for sobriety: Connect and reconnect n Reinforce alternative sources of reward and pleasure n Re-establish connection with spiritual or other source of meaning (god/family/community/meaningful work)
Treatment Elements: continued n Increase access and decrease resistence to non-using alternatives n Increase social support for sobriety: Connect and reconnect n Reinforce alternative sources of reward and pleasure n Re-establish connection with spiritual or other source of meaning (god/family/community/meaningful work)
 Treatment Alternatives to Facilitate Recovery Mutual support/self-help groups AA, NA, Al-Anon, Smart Recovery, Women for Sobriety Psychosocial and non-pharmacologic treatments Cognitive Behavioral Therapy Motivational Enhancement Therapy Contingency or Incentive Based Therapy Community Reinforcement and Couples Based Therapies Individual and/or group therapy settings
Treatment Alternatives to Facilitate Recovery Mutual support/self-help groups AA, NA, Al-Anon, Smart Recovery, Women for Sobriety Psychosocial and non-pharmacologic treatments Cognitive Behavioral Therapy Motivational Enhancement Therapy Contingency or Incentive Based Therapy Community Reinforcement and Couples Based Therapies Individual and/or group therapy settings
 Treatment of Substance Abuse: Role of the Medical Practitioner Potential roles in variety of settings: n Management of acute withdrawal syndromes n Treatment of medical and/or psychiatric co-morbidities. n Providing medication assisted treatment (MAT). n Non-pharmacologic/behavioral treatment: Support and reinforce that provided by others Provide therapy directly: formal or brief counseling
Treatment of Substance Abuse: Role of the Medical Practitioner Potential roles in variety of settings: n Management of acute withdrawal syndromes n Treatment of medical and/or psychiatric co-morbidities. n Providing medication assisted treatment (MAT). n Non-pharmacologic/behavioral treatment: Support and reinforce that provided by others Provide therapy directly: formal or brief counseling
 Maximizing the Med Management Visitor Other Medical Encounter “Psychotherapy in small doses”
Maximizing the Med Management Visitor Other Medical Encounter “Psychotherapy in small doses”
 Med Management Visits: Routine and Potential Elements Assess response to medication/s: Efficacy/Side-Effects Assess abstinence from primary as well as other drugs Assess overall bio-psycho-social stability AND Reinforce steps toward engagement in recovery BY Applying elements of motivational interviewing and CBT
Med Management Visits: Routine and Potential Elements Assess response to medication/s: Efficacy/Side-Effects Assess abstinence from primary as well as other drugs Assess overall bio-psycho-social stability AND Reinforce steps toward engagement in recovery BY Applying elements of motivational interviewing and CBT
 Potential Roles for the Medical Practitioner n Medical clinician only Psychotherapist Counselor Coach Guide n Do we want to stay in a traditional medical role? n Do we want to accept and activate our counseling role? n n
Potential Roles for the Medical Practitioner n Medical clinician only Psychotherapist Counselor Coach Guide n Do we want to stay in a traditional medical role? n Do we want to accept and activate our counseling role? n n
 “Two-year experience with buprenorphine-naloxone for maintenance treatment of opioid-dependence within a private practice setting” < < < Office-based setting Mid-size urban community sample in North Carolina Mixed prescription opioid and illicit opioid dependent patients Minimal staff resources (solo practice) Standard visits: 45 -60 min initial, 15 -20 min follow-up Used standard community referral resources Finch JW, Kamien KB, Amass L, J of Addiction Medicine, 2007.
“Two-year experience with buprenorphine-naloxone for maintenance treatment of opioid-dependence within a private practice setting” < < < Office-based setting Mid-size urban community sample in North Carolina Mixed prescription opioid and illicit opioid dependent patients Minimal staff resources (solo practice) Standard visits: 45 -60 min initial, 15 -20 min follow-up Used standard community referral resources Finch JW, Kamien KB, Amass L, J of Addiction Medicine, 2007.
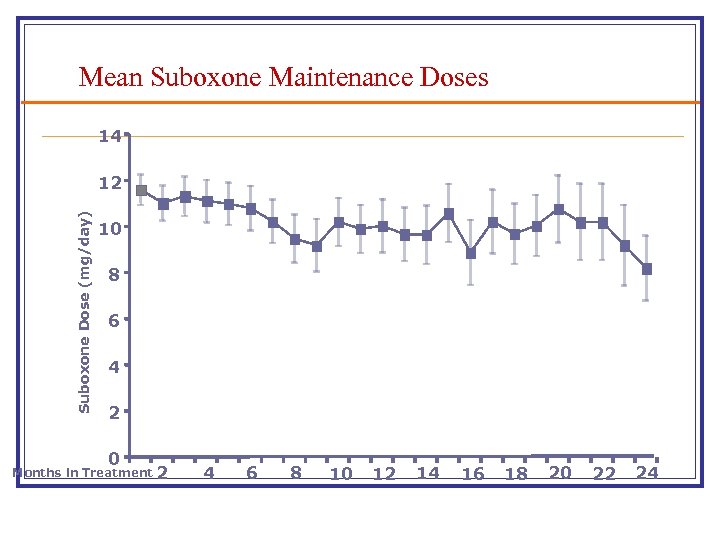 Mean Suboxone Maintenance Doses 14 Suboxone Dose (mg/day) 12 10 8 6 4 2 0 Months in Treatment 2 4 6 8 10 12 14 16 18 20 22 24
Mean Suboxone Maintenance Doses 14 Suboxone Dose (mg/day) 12 10 8 6 4 2 0 Months in Treatment 2 4 6 8 10 12 14 16 18 20 22 24
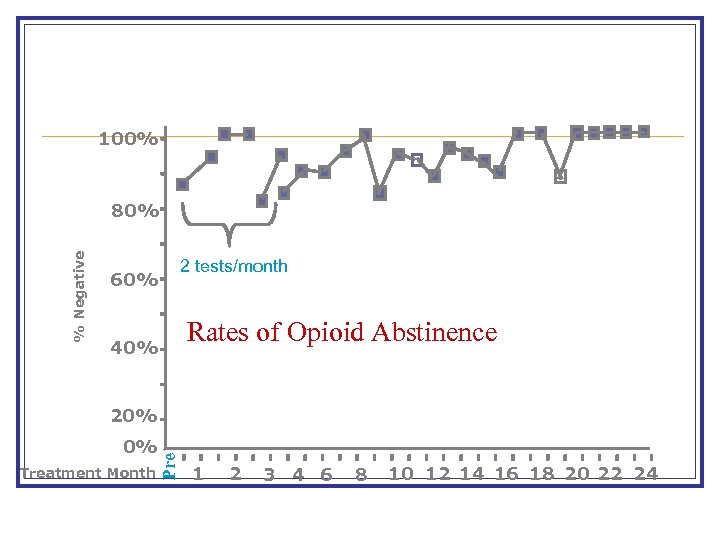 % Negative %Negative 100% 80% 2 tests/month 60% 40% Rates of Opioid Abstinence 20% 0% 0% Treatment Month Pre 20% 1 2 3 4 6 8 10 12 14 16 18 20 22 24
% Negative %Negative 100% 80% 2 tests/month 60% 40% Rates of Opioid Abstinence 20% 0% 0% Treatment Month Pre 20% 1 2 3 4 6 8 10 12 14 16 18 20 22 24
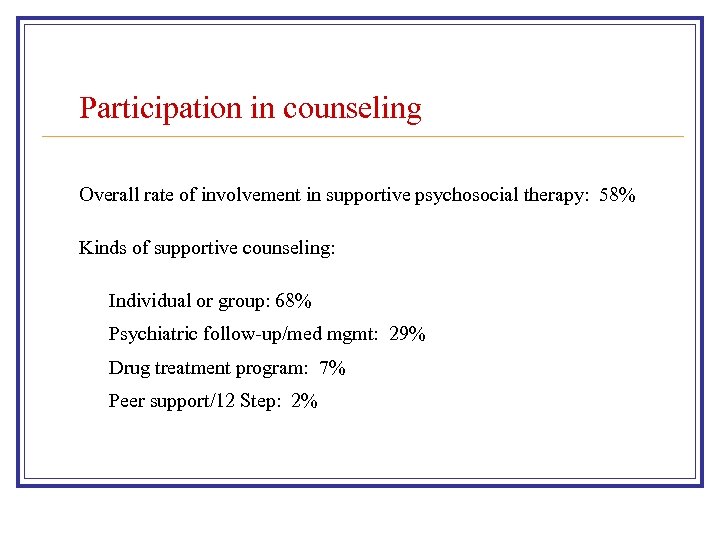 Participation in counseling Overall rate of involvement in supportive psychosocial therapy: 58% Kinds of supportive counseling: Individual or group: 68% Psychiatric follow-up/med mgmt: 29% Drug treatment program: 7% Peer support/12 Step: 2%
Participation in counseling Overall rate of involvement in supportive psychosocial therapy: 58% Kinds of supportive counseling: Individual or group: 68% Psychiatric follow-up/med mgmt: 29% Drug treatment program: 7% Peer support/12 Step: 2%
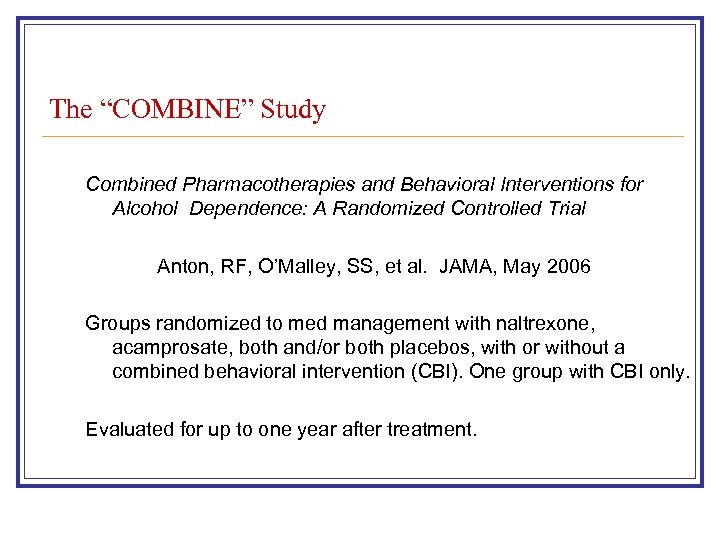 The “COMBINE” Study Combined Pharmacotherapies and Behavioral Interventions for Alcohol Dependence: A Randomized Controlled Trial Anton, RF, O’Malley, SS, et al. JAMA, May 2006 Groups randomized to med management with naltrexone, acamprosate, both and/or both placebos, with or without a combined behavioral intervention (CBI). One group with CBI only. Evaluated for up to one year after treatment.
The “COMBINE” Study Combined Pharmacotherapies and Behavioral Interventions for Alcohol Dependence: A Randomized Controlled Trial Anton, RF, O’Malley, SS, et al. JAMA, May 2006 Groups randomized to med management with naltrexone, acamprosate, both and/or both placebos, with or without a combined behavioral intervention (CBI). One group with CBI only. Evaluated for up to one year after treatment.
 The “Combine” Study: Outcomes n Patients receiving medical management with naltrexone, CBI or both fared better on drinking outcomes. n No combination produced better efficacy than naltrexone or CBI alone in the presence of medical management. n Placebo pills and meeting with a health care professional had a positive effect above that of CBI alone during treatment. n Medical Management (MD, RN, PA): Initial 45 min visit, followed by 20 min visits, on week 1 and 2 and then every 2 to 4 weeks.
The “Combine” Study: Outcomes n Patients receiving medical management with naltrexone, CBI or both fared better on drinking outcomes. n No combination produced better efficacy than naltrexone or CBI alone in the presence of medical management. n Placebo pills and meeting with a health care professional had a positive effect above that of CBI alone during treatment. n Medical Management (MD, RN, PA): Initial 45 min visit, followed by 20 min visits, on week 1 and 2 and then every 2 to 4 weeks.
 Basic Elements of Psychotherapy n n n Expectation of receiving help Therapeutic relationship Obtaining external perspective Encouraging corrective experiences Opportunity to test reality All available in the medical encounter.
Basic Elements of Psychotherapy n n n Expectation of receiving help Therapeutic relationship Obtaining external perspective Encouraging corrective experiences Opportunity to test reality All available in the medical encounter.
 Types of Power for Behavior Change n n n Reward: ability to give people what they want or need Coercive: disapproval, denying requests, not seeing Referent: the “admired other”, role-model Legitimate: validated authority Expert: access to knowledge, training, information All are inherent in the medical encounter.
Types of Power for Behavior Change n n n Reward: ability to give people what they want or need Coercive: disapproval, denying requests, not seeing Referent: the “admired other”, role-model Legitimate: validated authority Expert: access to knowledge, training, information All are inherent in the medical encounter.
 “the efficacy of psychotherapeutic methods lies in the shared belief of the participants that these methods will work. ” JD Frank That is…If you believe that what you’re doing when you talk to your patients is helpful…it is more likely that it will be.
“the efficacy of psychotherapeutic methods lies in the shared belief of the participants that these methods will work. ” JD Frank That is…If you believe that what you’re doing when you talk to your patients is helpful…it is more likely that it will be.
 To be or not to be…a psycho-therapist, counselor or guide…isn’t even the question… Your patients already expect it of you… and react to you like you’re already doing it… And one way or another…you are already doing it… you So, the only question is… what you need to help do what you’re doing… while you’re already doing it!
To be or not to be…a psycho-therapist, counselor or guide…isn’t even the question… Your patients already expect it of you… and react to you like you’re already doing it… And one way or another…you are already doing it… you So, the only question is… what you need to help do what you’re doing… while you’re already doing it!
 A Brief Psychotherapy “Primer” n n Applying core elements of CBT (Cognitive Behavioral Therapy) Incorporating a Motivational Interviewing style Supporting self-efficacy Adapting core elements of DBT (Dialectical Behavioral Therapy)
A Brief Psychotherapy “Primer” n n Applying core elements of CBT (Cognitive Behavioral Therapy) Incorporating a Motivational Interviewing style Supporting self-efficacy Adapting core elements of DBT (Dialectical Behavioral Therapy)
 Core Elements of Cognitive Behavioral Therapy: 1. Recognize: triggers-cues: external-internal 2. Anticipate/Avoid: high risk situations-people-places 3. Cope: relaxing-dealing with stress-dysphoria 4. Connect: options for support-socializing-fun-meaning
Core Elements of Cognitive Behavioral Therapy: 1. Recognize: triggers-cues: external-internal 2. Anticipate/Avoid: high risk situations-people-places 3. Cope: relaxing-dealing with stress-dysphoria 4. Connect: options for support-socializing-fun-meaning
 Recognize Triggers and Cues: External: “People/Places/Things” “Playmates/Playgrounds/Playthings” Internal: HALT: Hungry-Angry-Lonely-Tired “I slipped again…I don’t know what happened…” “I just started craving…I don’t know why…” Play the tape back: Where were you, who were you with, how did you feel…how is that like other slips?
Recognize Triggers and Cues: External: “People/Places/Things” “Playmates/Playgrounds/Playthings” Internal: HALT: Hungry-Angry-Lonely-Tired “I slipped again…I don’t know what happened…” “I just started craving…I don’t know why…” Play the tape back: Where were you, who were you with, how did you feel…how is that like other slips?
 Anticipate/Avoid Risk: “I get paid and cash in my hand is a huge trigger to buy some dope…” (Plan ahead…direct deposit, etc) go “I just ended up at this party. . . and when it’s in front of me I can’t say no…” (Play the tape back: When did you still have control? ) “If an old using buddy calls and “just wants to hang out. . . ” (Play the tape to the end: What’s likely to happen? ) “It is easier to avoid temptation, than to resist temptation”.
Anticipate/Avoid Risk: “I get paid and cash in my hand is a huge trigger to buy some dope…” (Plan ahead…direct deposit, etc) go “I just ended up at this party. . . and when it’s in front of me I can’t say no…” (Play the tape back: When did you still have control? ) “If an old using buddy calls and “just wants to hang out. . . ” (Play the tape to the end: What’s likely to happen? ) “It is easier to avoid temptation, than to resist temptation”.
 Connect: Re-expand dormant options to socialize and have fun: “Really, everybody uses? ” “Any old, non-using old friends to contact? ” “What did you use to do to have fun? Re-connect with sources of reward: “hedonic tone” “What do you want out of life? ” “What were your goals before you got into drugs? ” (I assume it wasn’t to still be living with your parents)
Connect: Re-expand dormant options to socialize and have fun: “Really, everybody uses? ” “Any old, non-using old friends to contact? ” “What did you use to do to have fun? Re-connect with sources of reward: “hedonic tone” “What do you want out of life? ” “What were your goals before you got into drugs? ” (I assume it wasn’t to still be living with your parents)
 Cope: Attention to basics: Sleep-diet-exercise Skills to relax/deal with stress “What’s a different option next time you’re upset? ” “Who can you call…who can you talk to? ” Mindfulness: Simple exercises to be in the moment/turn off the wheels/put space between feeling and acting “Thoughts are only thoughts…you don’t have to act on them. ”
Cope: Attention to basics: Sleep-diet-exercise Skills to relax/deal with stress “What’s a different option next time you’re upset? ” “Who can you call…who can you talk to? ” Mindfulness: Simple exercises to be in the moment/turn off the wheels/put space between feeling and acting “Thoughts are only thoughts…you don’t have to act on them. ”
 Motivationa. I Interviewing (MI) helps to: n Enhance intrinsic motivation for change n Mobilize person’s own resources n Resolve ambivalence and reach a decision n Build commitment to change
Motivationa. I Interviewing (MI) helps to: n Enhance intrinsic motivation for change n Mobilize person’s own resources n Resolve ambivalence and reach a decision n Build commitment to change
 Four Basic Principles n Express Empathy Focus on understanding the person’s dilemma n Roll with Resistance Don’t be the one arguing for change n Develop Discrepancy Evoke the person’s own arguments for change n Support Self Efficacy: Change is Possible
Four Basic Principles n Express Empathy Focus on understanding the person’s dilemma n Roll with Resistance Don’t be the one arguing for change n Develop Discrepancy Evoke the person’s own arguments for change n Support Self Efficacy: Change is Possible

 Support Self-Efficacy: Listen to the language of the patient’s story: generalizations/deletions/distortions “I always screw up. ” “I can’t stop using. ” “I’m just an addict. ” “My life is a mess. . . ”
Support Self-Efficacy: Listen to the language of the patient’s story: generalizations/deletions/distortions “I always screw up. ” “I can’t stop using. ” “I’m just an addict. ” “My life is a mess. . . ”
 Editing the Patient’s “Story” Challenging “learned helplessness” “Really…you always screw up…what’s something you did right…? Reinforcing the power of “yet” “Well, yes…you haven’t stopped… yet” “Your right…you haven’t re-earned peoples’ trust…yet” Your life isn’t where you want it to be…yet. ”
Editing the Patient’s “Story” Challenging “learned helplessness” “Really…you always screw up…what’s something you did right…? Reinforcing the power of “yet” “Well, yes…you haven’t stopped… yet” “Your right…you haven’t re-earned peoples’ trust…yet” Your life isn’t where you want it to be…yet. ”
 Provide perspective. Support strengths. Redefine self image: “You slipped with cocaine but you haven’t used dope in 3 months. ” “You thought about using every day but you only used once…what worked on those other days…” “How about instead of “just an addict”, try thinking of yourself as a person with an addiction who’s working hard to get better? ” “You may have to accept that you’re not a total screw-up after all. ” Find some positive behavior to reinforce every visit!.
Provide perspective. Support strengths. Redefine self image: “You slipped with cocaine but you haven’t used dope in 3 months. ” “You thought about using every day but you only used once…what worked on those other days…” “How about instead of “just an addict”, try thinking of yourself as a person with an addiction who’s working hard to get better? ” “You may have to accept that you’re not a total screw-up after all. ” Find some positive behavior to reinforce every visit!.
 n If that sounds like first grade…it is. n If you feel like you’re repeating yourself…that’s ok. n If you feel like a coach or a parent…that’s ok too.
n If that sounds like first grade…it is. n If you feel like you’re repeating yourself…that’s ok. n If you feel like a coach or a parent…that’s ok too.
 Communication Styles: A Continuum Directing Guiding Following “…when your goal is behavior change, the optimal style is usually guiding. ” William R Miller
Communication Styles: A Continuum Directing Guiding Following “…when your goal is behavior change, the optimal style is usually guiding. ” William R Miller
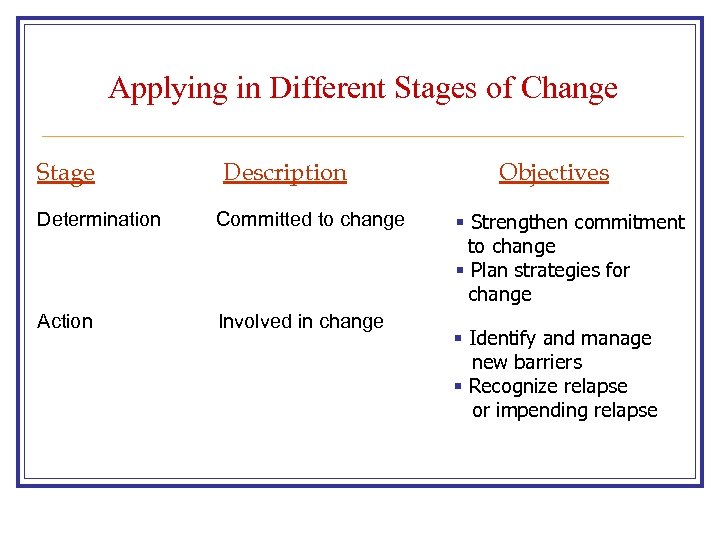 Applying in Different Stages of Change Stage Description Determination Committed to change Action Involved in change Objectives § Strengthen commitment to change § Plan strategies for change § Identify and manage new barriers § Recognize relapse or impending relapse
Applying in Different Stages of Change Stage Description Determination Committed to change Action Involved in change Objectives § Strengthen commitment to change § Plan strategies for change § Identify and manage new barriers § Recognize relapse or impending relapse
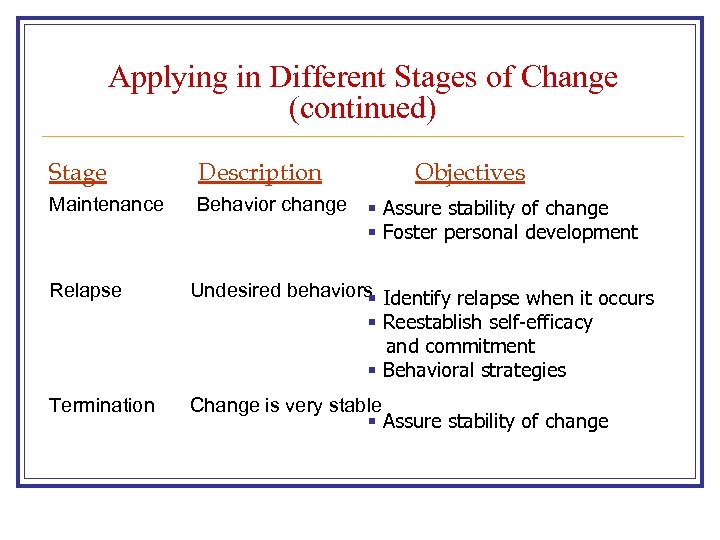 Applying in Different Stages of Change (continued) Stage Description Maintenance Behavior change Objectives § Assure stability of change § Foster personal development Relapse Undesired behaviors Identify relapse when it occurs § § Reestablish self-efficacy and commitment § Behavioral strategies Termination Change is very stable § Assure stability of change
Applying in Different Stages of Change (continued) Stage Description Maintenance Behavior change Objectives § Assure stability of change § Foster personal development Relapse Undesired behaviors Identify relapse when it occurs § § Reestablish self-efficacy and commitment § Behavioral strategies Termination Change is very stable § Assure stability of change
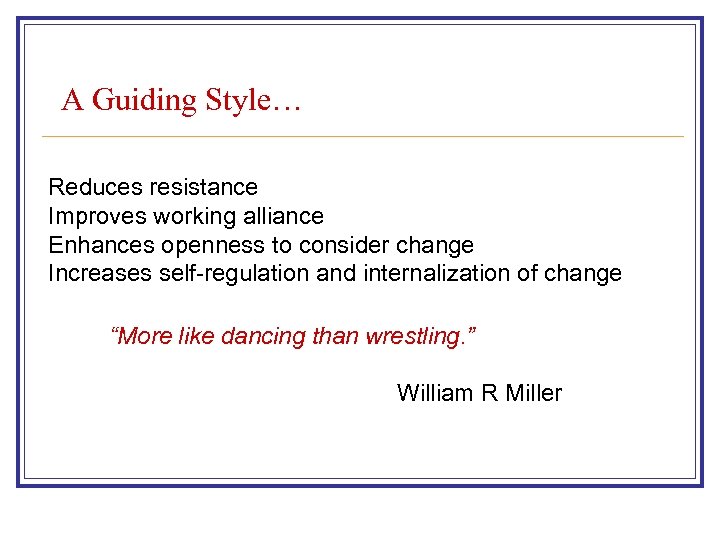 A Guiding Style… Reduces resistance Improves working alliance Enhances openness to consider change Increases self-regulation and internalization of change “More like dancing than wrestling. ” William R Miller
A Guiding Style… Reduces resistance Improves working alliance Enhances openness to consider change Increases self-regulation and internalization of change “More like dancing than wrestling. ” William R Miller
 Two Stages of Motivational Interviewing n Phase 1: Building Motivation for Change n Phase 2: Strengthening Commitment to Change Reinforcing positive changes
Two Stages of Motivational Interviewing n Phase 1: Building Motivation for Change n Phase 2: Strengthening Commitment to Change Reinforcing positive changes
 Change Talk n Change talk is speech linked to a particular behavior change target. n Three types: Sustaining talk Preparatory talk Implementing talk
Change Talk n Change talk is speech linked to a particular behavior change target. n Three types: Sustaining talk Preparatory talk Implementing talk
 Sustain Talk The other side change: n n n “I really like getting high” “I couldn’t give up…” “I need to use to be social” “I don’t think I need to stop” “I can use once in a while”
Sustain Talk The other side change: n n n “I really like getting high” “I couldn’t give up…” “I need to use to be social” “I don’t think I need to stop” “I can use once in a while”
 Preparatory Talk Implies continuing ambivalence: n. DESIRE: I want to…would like to… wish I could. . . n. ABILITY: Maybe I can…maybe I could. . . n. REASONS: If I stopped. . then. . . n. NEED: I need to… have to…I should…
Preparatory Talk Implies continuing ambivalence: n. DESIRE: I want to…would like to… wish I could. . . n. ABILITY: Maybe I can…maybe I could. . . n. REASONS: If I stopped. . then. . . n. NEED: I need to… have to…I should…
 Implementing Talk Reflects resolution of ambivalence and decision: n n n COMMITMENT (intention, decision, readiness) ACTIVATION (willing, trying, preparing) SPECIFIC (steps, actions) “I have decided to…” “I am ready to…” “I will…”
Implementing Talk Reflects resolution of ambivalence and decision: n n n COMMITMENT (intention, decision, readiness) ACTIVATION (willing, trying, preparing) SPECIFIC (steps, actions) “I have decided to…” “I am ready to…” “I will…”
 Resources n n n Motivational Interviewing by William Miller CSAT TIP 35: Enhancing Motivation for Change in Substance Abuse Treatment The 15 Minute Hour by Stuart and Lieberman Treating Alcohol Dependence: A Coping Skills Training Guide by Monti, et al. www. sa 4 docs website ASAM, TNSAM and NCSAM trainings
Resources n n n Motivational Interviewing by William Miller CSAT TIP 35: Enhancing Motivation for Change in Substance Abuse Treatment The 15 Minute Hour by Stuart and Lieberman Treating Alcohol Dependence: A Coping Skills Training Guide by Monti, et al. www. sa 4 docs website ASAM, TNSAM and NCSAM trainings
 Clinical Application: Demo/Role-play Scenario 1: I don’t know why I used… (Working backwards, identifying cues/triggers) I was at this party…and so showed up…and well, it was right under my nose, what could I do? (Identifying high-risk people/places, exploring alternative non-using activities/friends, reinforcing positive behaviors-even small steps)
Clinical Application: Demo/Role-play Scenario 1: I don’t know why I used… (Working backwards, identifying cues/triggers) I was at this party…and so showed up…and well, it was right under my nose, what could I do? (Identifying high-risk people/places, exploring alternative non-using activities/friends, reinforcing positive behaviors-even small steps)
 Clinical Application: Demo/Role-play n Scenario 2: I just had a terrible week…my girlfriend broke up with me/I lost my job…all this bad feeling just washed over me…and then I just dove into it…I had to use to deal with how bad I felt. (Dealing with craving, dysphoria, stress)
Clinical Application: Demo/Role-play n Scenario 2: I just had a terrible week…my girlfriend broke up with me/I lost my job…all this bad feeling just washed over me…and then I just dove into it…I had to use to deal with how bad I felt. (Dealing with craving, dysphoria, stress)
 Clinical Application: Discussion Final discussion: n n n Elicit other problematic aspects/encounters Informally play out alternatives What to do when it feels more like “wrestling” (when is the pt/when is it you/when is it time to move on) Next steps/how to get more training/fdbk (“supervision” for non-therapist docs? )
Clinical Application: Discussion Final discussion: n n n Elicit other problematic aspects/encounters Informally play out alternatives What to do when it feels more like “wrestling” (when is the pt/when is it you/when is it time to move on) Next steps/how to get more training/fdbk (“supervision” for non-therapist docs? )
 You can’t always get what you want… But if you try sometimes… You get what you need. JWF: The Vintage Image Gallery Mick Jagger, The Rolling Stones, 1969
You can’t always get what you want… But if you try sometimes… You get what you need. JWF: The Vintage Image Gallery Mick Jagger, The Rolling Stones, 1969


